Abstract
This study aims to compare demographic and clinical characteristics of chronic obstructive pulmonary disease (COPD) patients who complete and fail to complete outpatient pulmonary rehabilitation (PR) program and to determine the reasons for not completing the program. Patients with COPD referred to the PR program were divided into two groups: Those who completed the program were classified as group 1 and those who did not complete were classified as group 2, and their data were compared. Patients who failed to complete the program were contacted through phone and asked why they ceased their participation in the program. In group 2, number of smoker patients and patients using nebulizer and receiving long-term oxygen treatment, emergency admissions, and dyspnea perception were higher (p = 0.003, p < 0.001, p = 0.033, p = 0.011, p < 0.001, respectively); forced expiratory volume in one second (%) value, exercise capacity, and quality of life were lower (p = 0.024, p = 0.001, p = 0.014, respectively). When considered from the sociodemographic perspective, group 2 had a lower education level and a higher rate of living alone (p < 0.001). Factors impairing the program compliance were lack of motivation (49.0%), transportation problems (23.8%), COPD exacerbation (18.4%), work-related reasons (4.8%), and hospitalization (4.1%), respectively. Smokers and severe COPD patients fail to complete PR program due to various reasons, especially lack of motivation. It is very important for health practitioners to inform patients accurately and adopt a positive attitude.
Keywords: COPD, pulmonary rehabilitation, patient compliance, lack of motivation, transportation problems, COPD exacerbation
Introduction
Chronic obstructive pulmonary disease (COPD) is an important mortality and morbidity cause in the world and has great significance due to its increasing prevalence despite the presence of medical treatment.1 Multidisciplinary pulmonary rehabilitation (PR) programs are very effective as non-pharmacological treatment modalities in COPD patients with its positive effects on dyspnea, exercise capacity, and quality of life (QOL).2 In addition, such programs provide the best opportunity for patients to regain their physical and social functions and become independent.3
Although international guidelines recommend PR as part of COPD patient management, participation in PR programs is very low.4 There are many problems with regards to participation in and completion of PR. Awareness for accessibility and benefits of PR is very low among patients as well as health practitioners.5 Only a small percentage (3–16%) of patients, who are eligible for PR, are referred to PR program by physicians.4 Some of the patients who are referred to PR program refuse to participate in the program from the beginning, while others fail to complete.6 Factors affecting program participation and/or completion are transportation problems, feeling too sick or too healthy to participate in the program, having some obligations or priorities, and fearing that PR will provide less benefit or cause harm to their health.7,8 In addition, smoking history, level of dyspnea, and social support may affect PR participation.7
Studies investigating the problems related to PR program are limited in numbers. Participation problems may vary from country to country. In our country, where PR practices are progressing, there are no published studies in this regard. There are two aims in this study: (1) Comparison of demographic and clinical characteristics of COPD patients who complete and fail to complete outpatient PR program and (2) determination of reasons for not attending to or not completing the program.
Methods
COPD patients who were referred to PR Unit from chest disease outpatient clinic of our hospital located in the center of Izmir at the west of Turkey, between January 2013 and June 2017, and who, upon preliminary examination, were considered eligible for 8-week outpatient PR program were included in the study. Our eligibility criteria for PR program were to be dyspneic at rest or during effort even though using bronchodilator medications, to have increased emergency admissions or hospitalizations, to have reduced activities of daily living, and to have no contraindications for the exercise training program according to cardiology department.9
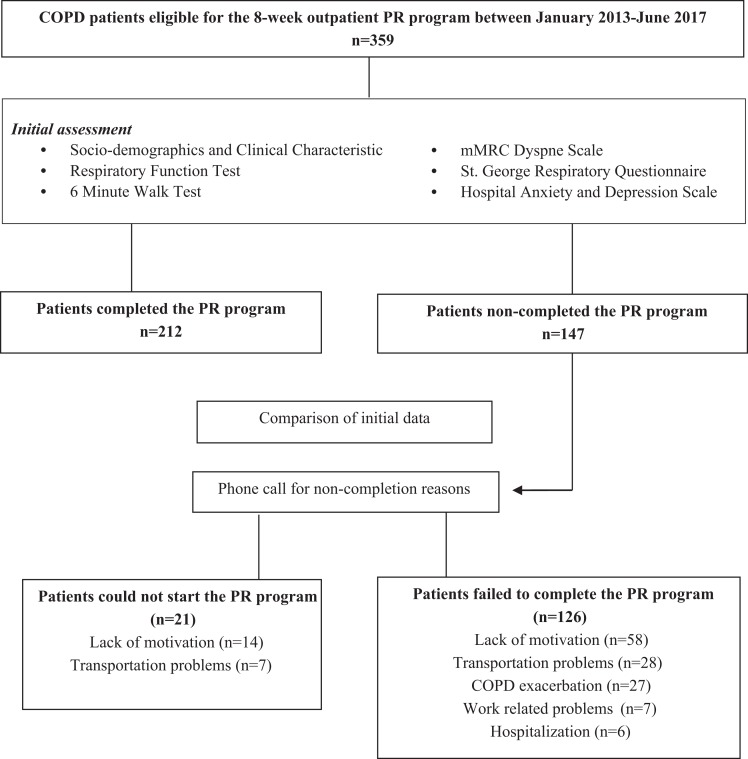
Patients completing the 8-week PR program were classified as group 1 and patients failing to complete were classified as group 2. We considered “non-completion” for patients who were referred to the 8-week PR program and whose initial evaluations were performed but did not start the program at all or did not come for three consecutive sessions. The data of both groups were compared. Patients who failed to complete the program were called by phone and asked for the reasons impairing their compliance with the program (Figure 1).
Figure 1.
Flowchart. COPD: chronic obstructive pulmonary disease, PR: pulmonary rehabilitation; mMRC: Modified Medical Research Council.
The study was approved by the local institutional review board. Patients included in the PR program completed an informed written consent form.
Measurements
Demographic and clinical characteristics of the patients were recorded prior to the program. The education levels of the patients were examined in three groups: primary school (age: 6–11 years), high school (age: 11–18 years), and university (age: 18 years and above). For our country, the hunger limit is 1.608 Turkish Liras (TL) and the poverty line is 5.238 TL per month. Therefore, for income level, those with income below 1.608 TL per month were classified as low, between 1.608 and 5.238 TL as medium, and above 5.238 TL as high income.10 Smoking histories were taken. Patients using the nebulizer, long-term oxygen treatment, and noninvasive mechanical ventilation were identified. Number of emergency admissions and hospitalizations during last year were examined. Patients with comorbidity were given scores based on Charlson Comorbidity Index (CCI).11
Respiratory functions
Body plethysmography (Zan 500, Germany) and carbon monoxide diffusion capacity (TLCO) (Zan 300, Germany) were measured and evaluated.12
Six-minute walk distance
The distance that the patients were able to walk in 6 minutes at their maximum possible pace was measured.13
Dyspnea evaluation
“Modified Medical Research Council” (mMRC) dyspnea scale, consisted of five articles, was used to determine dyspnea severity of patients: “0” represents the best level and “4” represents the worst level.14
Quality of life
“St. George Respiratory Questionnaire” (SGRQ) was used to determine disease-specific QOL. Higher scores indicate worsening of the disease and increase in symptoms. Change of four units in the total score and each subsection was considered to be statistically significant.15
Psychological symptoms
Hospital Anxiety and Depression (HAD), consisted of 14 questions, was used to determine psychological state of the patients.16
Statistical analysis
Statistical analysis of the data was performed by using “Statistical Package for Social Science (SPSS) for Windows version 17” statistics software. Distribution normality of the data was checked using the Kolmogorov–Smirnov analysis. Continuous variables were represented as median (interquartile range) and categorical variables were represented as percentage (%).
The Mann–Whitney U test was used for the comparison of values determined by measurement, and Fisher’s exact test was used for the comparison of categorical variables. Binary logistic regression analysis of Wald backward elimination method was used to predict noncompletion adjusting variables. Test results were interpreted according to p = 0.05 significance level.
Results
A total of 359 patients participated in the study and 325 of them were male (90.52%); 212 patients (59%) completed the program and 147 patients (41%) failed to complete. Age, body mass index, and disease duration of the patients were similar (p > 0.05). When the groups were compared for smoking history, cigarette consumption was similar (p = 0.965) in both groups; however, group 2 had a higher number of current smokers (p = 0.003). Both groups had similar CCI scores (p = 0.455). Although noninvasive mechanical ventilation use was similar in both groups (p = 0.069), the percentage of patients using the nebulizer and receiving long-term oxygen treatment was significantly higher in group 2 (p < 0.001 and p = 0.033, respectively). The number of hospitalization was similar for both groups (p = 0.198); however, group 2 had significantly higher number of hospital admissions (p = 0.011). When sociodemographic data are examined, in group 1, the number of high school graduates and in group 2, consequently, the number of primary school graduates was significantly higher (p < 0.001). The number of university graduates was very small and there was no difference between the groups (p = 0.610). Most of our patients had middle-income levels per month. Patients with low incomes were more likely to be in group 2, while those with high incomes were more likely in group 1. However, there was no significant difference between the two groups in terms of income levels per month (p > 0.05). The number of patients living alone was significantly higher in group 2 (p < 0.001; Table 1).
Table 1.
Comparison of demographic and clinical features of patients.a
| Variables | All patients (n = 359) | Group 1 (n = 212) | Group 2 (n = 147) | p valueb |
|---|---|---|---|---|
| Age (years) | 64 (58, 69) | 63 (59, 63) | 65 (58, 70) | 0.609 |
| Disease durations (years) | 7 (4, 11) | 7 (4, 10) | 7 (5, 12) | 0.350 |
| Body mass index (kg/m2) | 25 (22, 30) | 25 (22, 30) | 25 (21, 29) | 0.184 |
| Men n (%) | 325 (90.5) | 188 (88.7) | 137 (93.2) | 0.286 |
| Education n (%) | ||||
| Primary school* | 158 (44.0) | 64 (30.2) | 93 (63.3) | <0.001** |
| High school* | 191 (53.2) | 142 (67.0) | 50 (34.0) | <0.001** |
| University | 10 (2.8) | 6 (2.2) | 4 (2.7) | 0.610 |
| Income n (%) | ||||
| Low | 82 (22.8) | 41 (19.3) | 41 (27.9) | 0.057 |
| Middle | 261 (72.7) | 158 (74.5) | 103 (70.1) | 0.350 |
| High | 16 (4.5) | 13 (6.1) | 3 (2.0) | 0.064 |
| Living alone n (%)* | 37 (10.3) | 12 (5.7) | 25 (17.0) | <0.001** |
| Smoking history n (%) | ||||
| Smoker | 14 (3.9) | 3 (1.4) | 11 (7.5) | 0.003** |
| Ex-smoker | 314 (87.5) | 189 (89.1) | 125 (85.0) | 0.246 |
| Never smoked | 31 (8.6) | 20 (9.5) | 11 (7.5) | 0.517 |
| Smoking consumption (person-years) | 60 (40, 80) | 60 (40, 80) | 55 (35, 90) | 0.965 |
| CCI | 3 (3, 4) | 3 (3, 4) | 3 (3, 4) | 0.455 |
| Devices n (%) | ||||
| Nebulizer | 73 (20.3) | 25 (11.8) | 48 (32.7) | <0.001** |
| LTOT | 80 (22.3) | 39 (18.4) | 41 (27.9) | 0.033** |
| NIMV | 19 (5.3) | 15 (7.1) | 4 (2.7) | 0.069 |
| Hospital admission (n/last year) | 2 (0, 5) | 1 (0, 3) | 3 (1, 7) | 0.011** |
| Hospitalization (n/last year) | 0 (0, 1) | 0 (0, 1) | 0 (0, 2) | 0.198 |
CCI: Charlson Comorbidity Index; LTOT: long-term oxygen treatment; NIMV: noninvasive mechanical ventilation.
aData are expressed as median (interquartile range) or number (percentage).
bMann–Whitney U test and Fisher's Exact Test.
*p < 0.001, **p < 0.05.
When respiratory function test results were compared, group 2 had significantly lower forced expiratory volume in 1 second (FEV1) value (p = 0.024). FEV1/forced vital capacity (FVC) and TLCO values were similar in both groups (p > 0.05). Arterial blood gas values had no significant difference between two groups (p > 0.05). Six-minute walk distance (6-MWD) was significantly lower in group 2 (p = 0.001). Anxiety and depression scores of the groups had no significant difference (p > 0.05); however, activity, effect, and total scores of SGRQ QOL survey were significantly worse in group 2 (p = 0.015, p = 0.010, and p = 0.014, respectively; Table 2).
Table 2.
Comparison of pulmonary function test, arterial blood gas, exercise capacity, dyspnea, QOL, anxiety and depression scores of patients.a
| Variables | All patients (n = 359) | Group 1 (n = 212) | Group 2 (n = 147) | p valueb |
|---|---|---|---|---|
| PFT | ||||
| FEV1 (%) | 39 (29, 52) | 40 (30, 59) | 37 (28, 48) | 0.024** |
| FEV1/FVC | 56 (48, 66) | 56 (48, 67) | 57 (47, 64) | 0.363 |
| TLCO (%) | 33 (20, 45) | 34 (21, 47) | 32 (17, 42) | 0.181 |
| ABGA | ||||
| PaO2 (mmHg) | 72 (63, 80) | 72 (63, 80) | 71 (63, 80) | 0.859 |
| PaCO2 (mmHg) | 40 (38, 45) | 40 (37, 45) | 41 (38, 46) | 0.578 |
| SaO2 (mmHg) | 95 (93, 96) | 95 (93,96) | 95 (92, 96) | 0.960 |
| 6-MWD (m) | 340 (258, 401) | 350 (290, 410) | 310 (220, 390) | 0.001** |
| mMRC dyspnea score | 3 (2, 3) | 2 (2, 3) | 3 (2, 4) | <0.001** |
| SGRQ | ||||
| Symptom | 59 (44, 73) | 58 (42, 74) | 61 (45, 72) | 0.986 |
| Activity | 67 (54, 86) | 66 (54, 86) | 80 (59, 87) | 0.015** |
| Impact | 49 (33, 67) | 46 (31, 65) | 54 (43, 73) | 0.010** |
| Total | 57 (42, 72) | 55 (41, 71) | 63 (49, 72) | 0.014** |
| HAD | ||||
| Anxiety | 8 (5, 11) | 8 (4, 11) | 8 (5, 12) | 0.203 |
| Depression | 7 (4, 10) | 7 (4, 10) | 7 (5, 11) | 0.318 |
QOL: quality of life; PFT: pulmonary function test, FEV1: forced expiratory volume in 1 second; FVC: forced vital capacity; TLCO: carbon monoxide diffusing capacity; ABGA: arterial blood gas analysis; PaO2: partial arterial oxygen pressure; PaCO2: partial arterial oxygen pressure; SaO2: arterial oxygen saturation; 6-MWD: 6-minute walk distance; mMRC: Modified Medical Research Council; SGRQ: St George Respiratory Questionnaire, HAD: Hospital Anxiety and Depression.
aData are expressed as median (interquartile range) and Δ values show changes between pre- and posttest.
bMann–Whitney U test.
**p < 0.05.
In logistic regression model, education level, using nebulizer, and mMRC dyspnea score were found to be effective on completion (Table 3). Primary school graduates were 3.7 times more likely than non–high school graduates to nonparticipate (95% CI: 0.169%–0.433%, p < 0.001). Using nebulizer had a risk of not participating 2.48 times more than those who did not use it (95% CI: 1.385%–4.459%, p = 0.002). The risk of not participating in the program increased by 1.33 times as the MRC score increased by 1 point (95% CI: 1.904%–1.682%, p = 0.005).
Table 3.
Logistic regression model of variables affecting PR program non-completion.
| Odds ratio | 95% confidence interval | p value | |
|---|---|---|---|
| Education | |||
| Primary school | 1 | ||
| High school | 0.271 | 0.169–0.433 | <0.001 |
| University | 0.632 | 0.161–2.478 | 0.510 |
| Using nebulizer | |||
| No | 1 | ||
| Yes | 2.485 | 1.385–4.459 | 0.002 |
| mMRC dyspnea score | 0.751 | 1.094–1.682 | 0.005 |
PR: pulmonary rehabilitation; mMRC: Modified Medical Research Council.
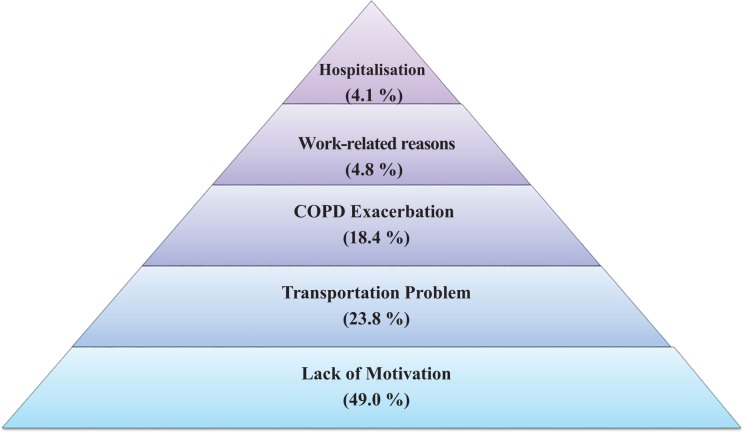
Reasons shared during the phone calls were examined under five main groups: (1) lack of motivation, (2) transportation problems, (3) COPD exacerbations, (4) work-related problems, and (5) hospitalization (for reasons other than COPD exacerbation). Of 147 patients who failed to complete the program, 21 patients (14.3%) did not start the program. Reasons for these patients not to participate were identified to be 75% lack of motivation (14 patients) and 25% transportation problems (7 patients). When patients who did not start the program and patients who failed to complete were evaluated together, factors impairing program compliance were found to be lack of motivation in 72 patients (49.0%), transportation problems in 35 patients (23.8%), COPD episode in 27 patients (18.4%), work-related problems in 7 patients (4.8%), and conditions requiring hospitalization in 6 patients (4.1%), respectively (Figure 2).
Figure 2.
Reasons of patients for not participating in the PR program. PR: pulmonary rehabilitation.
Discussion
In our study, the number of patients who smoke and receive long-term oxygen therapy, the emergency admissions in the last year and living alone was higher, while low education level was lower in patients who did not complete the PR program. In addition, FEV1 and 6-MWD were lower, perceived dyspnea was higher, and QOL was poorer in that group. Upon investigation of causes for the program completion failure, lack of motivation was observed to be the most important factor. Other reasons included transportation problems, COPD exacerbations, work-related reasons, and hospitalization, respectively.
Treatment compliance of COPD patients may be affected by sociodemographic, psychological, physiological characteristics, and QOL.17 There is only one study reporting that young patients have lower participation rate in PR programs.18 As with other studies, factors such as age, gender, and body mass index2,19 were not considered in the PR program participation of our study. Unlike a study that showed that education did not affect program adjustment,2 in our study, the number of patients with low levels of education was higher in the group that could not complete the program.
In one study, it was shown that patients living in more deprived areas are less likely to complete PR.20 In our study, the difference between the two groups was not significant, although the proportion of those with low income levels was higher in group 2. Similar to studies showing that patients living alone have a poor program compliance,2,17,21 the rate of patients living alone in our study was higher in group 2.
Smoking is considered to be one of the factors that adversely affect patients’ compliance with the PR program.19 According to a study where the results of those who complete the program with dropouts, it was shown that the majority of smokers could not complete the program.22 In a prospective study, the rate of failure to complete the program was higher in patients who smoke. Moreover, smoker patients benefited from the program in a similar way to ex-smoker patients if they had completed the program. And, it was recorded that nicotine addictions and daily cigarette consumption of smokers were decreased significantly.23 This result can be an unrecognized achievement of PR, and more work is needed on this issue. Consistent with the literature, in our study, it was found that the number of smoker patients was significantly higher in group 2 and there was no difference between the groups in terms of cigarette consumption.
Effects of comorbidities on PR participation and completion rates are not clear yet.9 In a study, where patients were classified as “good” and “bad” participants, the percentage of patients with major comorbidity was similar between groups.18 Similar to a study which did not find any difference between patient groups that are scored according to CCI,22 comorbidity score did not differ between groups in our study as well. Studies show that long-term oxygen use is an independent determinant of poor compliance.7,22 In addition to long-term oxygen use, nebulizer use was also found to be higher in group 2; however, noninvasive mechanical ventilation use had no effect in our study. There are studies reporting the higher number of hospital admissions during last year for patients with poor compliance.7,19 Our study also found higher hospital admissions for patients failing to complete; however, no difference was observed in terms of hospitalization.
Majority of studies suggest that FEV1 value had no effect on program compliance;2,17,19 however, one study showed that low FEV1 impaired PR program compliance.19 In our study, we concluded that FEV1 value was lower in patients who fail to complete the program; however, FEV1/FVC and TLCO values were similar between patients. As with other studies,22 arterial blood gas values had no effect. Only one study reported that dyspnea score did not affect program compliance.2 Other studies show that patients with higher dyspnea score had worse program compliance.19,22 Our study also found higher mMRC scores in patients who failed to complete the program. Some studies showed that patients failing to complete PR program had shorter 6-MWD17,22,23 and shuttle walking distance.7 As with all other studies, our study found shorter 6-MWD in patients who failed to complete. In some studies, QOL adversely affected treatment compliance,17,18 whereas it had no effect in other studies.7,19 In our study, all parameters in SGRQ survey, except for “symptom”, were higher in patients who failed to complete the program. To the contrary of a study that suggests depressed patients had a higher risk for quitting the program,24 our study showed anxiety and depression scores had no effect on treatment compliance and this was in line with two other studies.7,17
Conducted studies determined that approximately 50% of COPD patients, who were referred to PR program, did not participate in the program.6,7,18,21 According to another study, patients with transportation problems, with very low exercise capacity, and who feel great and think that program would not benefit them did not participate in the program at all.7 In our study, of all COPD patients enrolled in the program, 41% did not complete the program.
Factors such as transportation problems, lack of motivation, thoughts of being very good or very bad, other obligations and priorities, and absence of social support adversely affected program compliance.7,8 Doctors who refer patients to PR program play an important role; positive attitude of doctors increases the program compliance.21 In a study, researchers conducted face-to-face interviews with patients who failed to complete the PR program and majority of them stated that they were not sufficiently informed, they cannot breathe, and they lack the strength to exercise.8 Nearly half of the patients included in our study, who did not complete the program, had lack of motivation. Transportation problems adversely affect compliance with the program.7,25,26 In this study, transportation problems are second among the reasons impairing program participation or completion. COPD exacerbations that occur while patients are participating in the program also prevent them from program completion.2,7,25 Some of our patients could not complete the program because of receiving outpatient or inpatient treatment for COPD exacerbations. Especially young patients could not participate in the program due to work.8 In our study, working patients could not continue their participation in the program because of not being able to take leave from their jobs. Hospitalization prevents patients from completing the program.2,7 The small part of our patients could not complete the program due to being hospitalized (for reasons other than COPD exacerbation). It was learned that patients who never started the program had lack of motivation and transportation problems.
In our study, we could not measure motivation via a scale because the patients did not come to our unit. We could only get information from the patients through phone. Inconsistent with the literature, if the patient had feasibility but did not want to come and find some pretexts, we considered it as “lack of motivation.” However, we believe that having an idea about the level of motivation before starting PR programs can increase participation rates in patients.
Our hospital is located in the center of Izmir at the west of Turkey. Since there are not many PR centers in our country, our center also accepts patients from the surrounding provinces and districts.
Our PR unit, where we conducted the study, is part of a hospital that is among hospitals that perform follow-ups for the highest number of chronic pulmonary patients in our country; therefore, despite a likelihood of regional differences, our results may reflect the overall patient population in our country. Therefore, we believe our study will contribute to the literature. Multicenter studies are needed for this issue.
Conclusion
Other components of the program should also be explained to the patients who are referred to the PR program. Patients should be informed well about their disease and its treatment, and they should be assisted for quitting smoking. It is not possible to change the educational status and income levels of patients but it is possible to increase participation rates by providing social support. It must be highlighted that this is a patient-specific program that can be applied to all the patients regardless of their disease severity. Sociodemographic and clinical characteristics of the patient must be considered for correct determination of the program type. Home programs and programs related to physical activity development strategies are needed for patients who cannot participate in the program due to reasons such as economic problems, transportation problems, or personal issues. To summarize, physicians and other health practitioners have a great responsibility for improving the program compliance of COPD patients.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Wedzicha JA, Wilkinson T. Impact of chronic obstructive pulmonary disease exacerbations on patients and payers. Proc Am Thorac Soc 2006; 3: 218–221. [DOI] [PubMed] [Google Scholar]
- 2. Fischer MJ, Scharloo M, Abbink JJ, et al. Drop-out and attendance in pulmonary rehabilitation: the role of clinical and psychosocial variables. Respir Med 2009; 103: 1564–1571. [DOI] [PubMed] [Google Scholar]
- 3. Guo SE, Bruce A. Improving understanding of and adherence to pulmonary rehabilitation in patients with COPD: a qualitative inquiry of patient and health professional perspectives. PLoS One 2014; 9(10): e110835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Johnston K, Grimmer-Somers K. Pulmonary rehabilitation: overwhelming evidence but lost in translation? Physiother Can 2010; 62: 368–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. GOLD executive committee. Global strategy for diagnosis, management and prevention of COPD, http://www.goldcopd.com (2017, accessed 15 June 2017).
- 6. Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis 2011; 8: 89–99. [DOI] [PubMed] [Google Scholar]
- 7. Hayton C, Clark A, Olive S, et al. Barriers to pulmonary rehabilitation: characteristics that predict patient attendance and adherence. Respir Med 2013; 107: 401–407. [DOI] [PubMed] [Google Scholar]
- 8. Mathar H, Fastholm P, Lange P, et al. Why do patients decline participation in offered pulmonary rehabilitation? A qualitative study. Clin Rehabil 2017; 1: 269215517708821. [DOI] [PubMed] [Google Scholar]
- 9. Spruit MA, Singh SJ, Garvey C, et al. ATS/ERS task force on pulmonary rehabilitation. An official American thoracic society/European respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013; 188: e13–e64. [DOI] [PubMed] [Google Scholar]
- 10. Report of Confederation of Turkish Trade Unions, available at: http://www.turkis.org.tr/LIMIT-OF-HUNGER-AND-POVERTY---DECEMBER-2017-d11679
- 11. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383. [DOI] [PubMed] [Google Scholar]
- 12. Miller MR, Crapo R, Hankinson J, et al. ATS/ERS task force. General considerations for lung function testing. Eur Respir J 2005; 26: 153–161. [DOI] [PubMed] [Google Scholar]
- 13. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111–117. [DOI] [PubMed] [Google Scholar]
- 14. Sweer L, Zwillich CW. Dyspnea in the patient with chronic obstructive pulmonary disease. Etiology and management. Clin Chest Med 1990; 11: 417–445. [PubMed] [Google Scholar]
- 15. Polatlı M, Yorgancıoğlu A, Aydemir Ö, et al. Validity and reliability of Turkish version of St. George’s respiratory questionnaire. Tuberk Toraks 2013; 61: 81–87. [DOI] [PubMed] [Google Scholar]
- 16. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370. [DOI] [PubMed] [Google Scholar]
- 17. Young P, Dewse M, Fergusson W, et al. Respiratory rehabilitation in chronic obstructive pulmonary disease: predictors of nonadherence. Eur Respir J 1999; 13: 855–859. [DOI] [PubMed] [Google Scholar]
- 18. Selzler AM, Simmonds L, Rodgers WM, et al. Pulmonary rehabilitation in chronic obstructive pulmonary disease: predictors of program completion and success. COPD 2012; 9: 538–545. [DOI] [PubMed] [Google Scholar]
- 19. Sabit R, Griffiths TL, Watkins AJ, et al. Predictors of poor attendance at an outpatient pulmonary rehabilitation programme. Respir Med 2008; 102: 819–824. [DOI] [PubMed] [Google Scholar]
- 20. Steiner MC, Lowe D, Beckford K, et al. Socioeconomic deprivation and the outcome of pulmonary rehabilitation in England and Wales. Thorax 2017; 1–8. DOI: 10.1136/thoraxjnl-2016-209376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Arnold E, Bruton A, Ellis-Hill C. Adherence to pulmonary rehabilitation: a qualitative study. Respir Med 2006; 100: 1716–1723. [DOI] [PubMed] [Google Scholar]
- 22. Cote CG, Celli BR. Pulmonary rehabilitation and the BODE index in COPD. Eur Respir J 2005; 26: 630–636. [DOI] [PubMed] [Google Scholar]
- 23. Santana VT, Squassoni SD, Neder JA, et al. Influence of current smoking on adherence and responses to pulmonary rehabilitation in patients with COPD. Rev Bras Fisioter 2010; 14: 16–23. [PubMed] [Google Scholar]
- 24. Garrod R, Marshall J, Barley E, et al. Predictors of success and failure in pulmonary rehabilitation. Eur Respir J 2006; 27: 788–794. [DOI] [PubMed] [Google Scholar]
- 25. Wadell K, Janaudis Ferreira T, Arne M, et al. Hospital-based pulmonary rehabilitation in patients with COPD in Sweden–a national survey. Respir Med 2013; 107: 1195–1200. [DOI] [PubMed] [Google Scholar]
- 26. Benzo R, Wetzstein M, Neuenfeldt P, et al. Implementation of physical activity programs after COPD hospitalizations: lessons from a randomized study. Chron Respir Dis 2015; 12: 5–10. [DOI] [PubMed] [Google Scholar]