Abstract
Background
The ProPrems trial, a multi-center, double-blind, placebo-controlled randomized trial, previously reported a 54% reduction in necrotizing enterocolitis (NEC) of Bell stage 2 or more from 4.4 to 2.0% in 1099 infants born before 32 completed weeks’ gestation and weighing < 1500 g, receiving probiotic supplementation (with Bifidobacterium longum subsp. infantis BB-02, Streptococcus thermophilus TH-4 and Bifidobacterium animalis subsp. lactis BB-12). This sub-study investigated the effect of probiotic supplementation on the gut microbiota in a cohort of very preterm infants in ProPrems.
Results
Bifidobacterium was found in higher abundance in infants who received the probiotics (AOR 17.22; 95% CI, 3.49–84.99, p < 0.001) as compared to the placebo group, and Enterococcus was reduced in infants receiving the probiotic during the supplementation period (AOR 0.27; 95% CI, 0.09–0.82, p = 0.02).
Conclusion
Probiotic supplementation with BB-02, TH-4 and BB-12 from soon after birth increased the abundance of Bifidobacterium in the gut microbiota of very preterm infants. Increased abundance of Bifidobacterium soon after birth may be associated with reducing the risk of NEC in very preterm infants.
Electronic supplementary material
The online version of this article (10.1186/s12866-018-1326-1) contains supplementary material, which is available to authorized users.
Keywords: Probiotics, Very preterm infants, Gut microbiota, Necrotizing enterocolitis
Background
Very preterm infants (born < 32 weeks’ gestation and weighing < 1500 g) are at increased risk of late-onset sepsis and necrotizing enterocolitis (NEC), with the associated potential for lifelong adverse health effects or death [1]. Preterm infants have a different gut microbiota than term newborns, including reduced species diversity, higher numbers of Enterobacteriaceae (including Klebsiella pneumoniae and Escherichia coli) and Clostridium difficile, and reduced numbers of Bifidobacteria and Lactobacilli [2, 3]. These differences may be a result of host factors associated with immaturity as well as various environmental factors including delivery mode, reduced exposure to maternal microbiota, exposure to antibiotic treatment, reduced breastfeeding, and prolonged stays in neonatal intensive care units [2, 4].
Necrotizing enterocolitis is a devastating inflammatory disease of the intestine that affects approximately 7% of infants born weighing < 1500 g [5]. Up to 30% of affected infants die, with increased rates of neurodevelopmental impairment in surviving NEC-affected infants compared to their unaffected peers [6]. The etiology of NEC is unknown and the current consensus is that it is likely to be multifactorial [5, 7, 8]. Non-microbial factors such as intestinal immaturity, genetic predisposition, and hypoxia-ischemia may contribute to the development of NEC [5, 7]. As NEC outbreaks have been reported, some hypothesize that the condition is caused by an infectious agent, although to date none has been found [9, 10]. It is generally accepted that a disturbance of the normal gut microbiota is a contributing factor to the development of NEC [8, 11, 12], with various associated dysbioses including reduced microbial diversity [13, 14], delayed colonization of commensals including Bifidobacterium, Bacteroidetes, and Firmicutes (including Negativicutes and Clostridia), and increased abundance of Gammaproteobacteria (with reports of increased Enterobacteriaceae, Klebsiella and Escherichia/Shigella in NEC infants compared to healthy controls) [13, 15–17].
There is strong evidence supporting the use of probiotic prophylaxis for the prevention of NEC. A recently published meta-analysis of 20 randomized controlled trials investigating the use of probiotics for prevention of NEC in preterm infants reported a 49.1% reduction in risk of NEC in probiotic supplemented infants (risk ratio [RR] = 0.509; 95% CI, 0.385–0.672; p < 0.001) [18]. In the ProPrems trial, a placebo-controlled randomized trial of 1099 infants, our group reported a 54% reduction in NEC of Bell stage 2 or more from 4.4 to 2.0% in very preterm infants receiving a three-strain probiotic (relative RR = 0.46; 95% CI 0.23–0.93; p = 0.03 [19]. In contrast, a large multicenter study of 1315 preterm infants found no reduction in the incidence of NEC following supplementation with a single-strain probiotic (adjusted RR = 0.93; 95% CI 0.68–1.27 [20]). This could suggest that not all probiotics have equivalent efficacy in preventing NEC and further work is needed to better understand how and why some probiotic combinations work and others do not.
In this sub-study, we investigated the effect of probiotic supplementation on the development of the gut microbiota of preterm infants by examining the gut bacterial communities in a cohort of very preterm infants enrolled in the ProPrems trial [19].
Methods
Participants and specimen collection
ProPrems [19, 21] was a large multi-center, double blind, placebo controlled randomized trial where very preterm infants (born < 32 weeks’ gestation and weighing < 1500 g) were randomized to receive either a probiotic combination (Bifidobacterium longum subsp. infantis (BB–02, 300 × 106), Streptococcus thermophilus (TH–4, 350 × 106) and Bifidobacterium animalis subsp. lactis (BB-12, 350 × 106) (ABC Dophilus Probiotic Powder for Infants; Solgar, Leonia, New Jersey) with 1 × 109 total organisms per 1.5 g, in a maltodextrin base powder) or placebo (maltodextrin powder) once enteral feeds were commenced, until discharge from hospital or term corrected age. Stool swabs (or perianal swabs if the infant had not passed feces) were collected from Victorian ProPrems participants as close to the following time points as possible: prior to commencement of the study powder, after one, four and eight weeks of treatment, at six and 12 months of age corrected for prematurity. Due to logistic limitations, only infants enrolled at The Royal Women’s Hospital, Melbourne, Australia with at least one swab available were eligible for inclusion in this sub-study. A total of 253 swabs (nine perianal swabs and 244 fecal swabs) from 68 infants were available for this sub-study.
DNA extraction, PCR amplification, and pyrosequencing
DNA was extracted from the specimens using the MagNA Pure 96 System (Roche Diagnostics, Branchburg, NJ); stool swabs and perianal swabs were processed in the same way. The extracted DNA was used to generate an amplicon based library using bifidobacteria optimized PCR primers that amplify the V3-V5 hypervariable regions of the 16S rRNA gene as described by Sim et al. [22]. Sequencing of amplicons was performed on a Roche 454 Genome Sequencer instrument (GS FLX Titanium Chemistry) at Macrogen Inc. (Seoul, South Korea) generating single end reads. Multiplex Identification tags were incorporated during preparation.
Sequence analysis
Sequence analysis was performed with QIIME (Version 1.8.0). Reads shorter than 250 bases, with homopolymer base runs of more than eight bases, containing more than eight ambiguously called bases or with an average phred quality score of less than 25 were removed from read sets. Chimeric reads were removed using UCHIME [23] in conjunction with the ‘gold’ 16S rRNA database [24]. Operational taxonomic unit (OTU) picking was performed using the default UCLUST algorithm and a similarity threshold of 97%. A representative sequence for each OTU was used to assign taxonomy, using the default UCLUST consensus taxonomy assigner and SILVA reference database [25]. Specimens with fewer than 100 reads following quality control were excluded from analysis.
Data analysis
All statistical analyses and diversity calculations were completed with R Studio (version 0.98.1103, Boston, USA) employing R 3.2.0 [26].
Baseline characteristics were compared between allocation groups using the Chi-Square test or Fisher’s exact test for categorical variables, and the Wilcoxon rank sum test for continuous variables.
To test if bacterial abundance differed significantly between the allocation groups and with age, a logistic regression analysis using a mixed effects model was performed for each genus that had a mean abundance of at least 1% in one allocation group. Proportional abundances of each genera were converted to a binary variable (based on the median value) and were regressed against allocation, adjusting for age at sampling (i.e. time from birth; expressed in days as a continuous variable) and gestation (expressed as above or below 28 weeks’ gestation as a binary variable), clustering by participant number to account for multiple specimens from the same infant.
The prevalence of key bacteria was calculated in two ways: 1) the number of infants who had at least one specimen over the study period test positive for a specific genus as a proportion of the total number of infants in each allocation group, 2) the number of specimens positive for a specific genus as a proportion of the total number of specimens in each allocation group.
Bacterial diversity was defined as effective number of genera (which is the exponential of the Shannon diversity index) and was calculated using the vegan package [27]. Reads that could not be classified to a genus level were omitted from diversity analyses. Effect of probiotic treatment on diversity was examined using a mixed effects linear regression model, adjusting as above. All regression analyses were implemented using the lme4 package [28]. P-value false discovery rate adjustment for multiple testing was performed where required using the Benjamini-Hochberg method. An adjusted p-value < 0.05 was deemed significant.
A heatmap and associated dendrogram was generated using the vegan and gplots packages [27, 29] and were based on Bray-Curtis dissimilarities and Ward’s method for hierarchical clustering.
Results
Specimen and participant data
From the 253 specimens eligible for processing from 68 infants, a total of 1,064,333 reads were generated. Thirty-eight read sets (from a total of 30 infants) were excluded from analysis; twelve specimens failed to produce a PCR product and were not sequenced, and 26 specimens had fewer than 100 reads following quality control. The remaining 215 read sets (seven perianal swabs and 208 fecal swabs) from 66 infants (730,861 reads) were analyzed using QIIME. The median number of reads per specimen was 3263 (IQR = 1665–4657) and did not differ between the probiotic (median 3296 reads) and placebo group (median 3076 reads; Z = − 0.87, p > 0.05; Table 1). The probiotic group comprised 124 specimens from 38 infants and the placebo group comprised 91 specimens from 28 infants. A range of one to five specimens was obtained from each infant (average three specimens (SD = 0.8)). Details of specimen collection are in Table 1.
Table 1.
Overview of study participants
| Probiotic, n = 38 | Placebo, n = 28 | P valuea | |
|---|---|---|---|
| Demographics | |||
| Male, n (%) | 19 (50.0) | 14 (50.0) | 1.0 |
| Gestational age, wk., mean (SD) | 28.6 (1.81) | 27.5 (1.72) | 0.02 |
| Birth weight, g, mean (SD) | 1040 (285) | 1000 (253) | 0.53 |
| Maternal antibiotics, n (%)b | 20 (52.6) | 12 (42.9) | 0.43 |
| Infant antibiotics: | |||
| Courses of antibiotics, median (IQR)) | 1 (0–2) | 1 (0–2) | 0.48 |
| Days of antibiotic exposure, d, median (IQR) | 2 (0–8) | 5 (0–10) | 0.38 |
| Infants with at least 1 episode of definite late-onset sepsis with pathogen, n(%)c | 3 (7.9) | 2 (7.1) | 1.0 |
| Infants with at least 1 episode of definite late-onset sepsis with CoNS, n(%)c | 2 (5.3) | 4 (14.3) | 0.39 |
| Caesarean delivery, n (%) | 27 (71.1) | 19 (60.7) | 0.78 |
| Any breast milk feeding, n (%) | 37 (97.4) | 28 (100.0) | 1.0 |
| Age commenced study powder, d, median (IQR) | 3.0 (2.0–5.0) | 3.5 (2.0–5.5) | 0.51 |
| Age finished study powder, d, median (IQR) | 67.5 (54.0–85.0) | 73.0 (64.0–89.5) | 0.14 |
| Length of supplementation, d, median (IQR) | 62.5 (48.5–81.8) | 69.5 (62.0–83.3) | 0.17 |
| Sequencing data | |||
| Specimens included, n | 124 | 91 | |
| Specimens collected before supplementation commenced, n | 3 | 8 | |
| DOL, median (range) | 3 (3–4) | 4 (1–8) | |
| Specimens collected during supplementation period, n | 80 | 62 | |
| DOL, median (range) | 30 (6–72) | 31 (4–96) | |
| Specimens collected post supplementation period, n | 41 | 21 | |
| DOL, median (range) | 256 (58–529) | 285 (61–613) | |
| Specimens collected per baby, mean (SD) | 3 (0.8) | 3 (0.8) | |
| Number of reads per specimen, median (IQR) | 3296 (1729–5136) | 3076 (1654–4472) | 0.39 |
Abbreviations: DOL Day of life of specimen collection, IQR interquartile range, CoNS Coagulase-negative Staphylococcus, SD standard deviation
aP value is based on Chi-Square test or Fisher’s exact test for categorical variables and Wilcoxon rank sum test for continuous variables. b maternal antibiotics is presented as the number (%) of mothers reporting antibiotic use before or during labor. c late-onset sepsis > 48 h after birth and before discharge home or term postmenstrual age
Baseline patient demographic characteristics were similar between the probiotic and placebo group, except that gestational age was lower in the placebo group (p = 0.02) (Table 1). The 66 infants included in this sub-study are representative of the entire ProPrems cohort with regard to the demographic characteristics including gender, gestational age, birth weight, and caesarean delivery (Additional file 1). However, the rate of NEC was lower in the sub-study population (one infant included in this sub-study developed NEC (Bell Stage 2 or more) (1.5%), compared to 35 infants (3.2%) in the wider ProPrems cohort).
The impact of probiotic supplementation on the gastrointestinal microbiota
A total of 102,050 reads (14.0%) could not be assigned to a genus; this included 400 reads that could not be assigned any bacterial phylum. The majority of reads that could not be classified to a bacterial genus were from the Enterobacteriaceae family (60.5%).
Bifidobacterium was the most prevalent genus in specimens from probiotic supplemented infants (detected in 90% of specimens collected from probiotic infants vs 55% of specimens collected from control infants). Streptococcus was present in 75% of specimens collected from probiotic infants vs 53% of specimens collected from control infants. Enterobacter was the most prevalent genus in specimens from control infants (detected in 85% of specimens collected from control infants vs 77% of specimens collected from probiotic infants). Bifidobacterium and Streptococcus were detected in at least one specimen from all probiotic supplemented infants; conversely, Enterobacter, Escherichia/Shigella and Enterococcus were detected in at least one specimen from all control infants (Table 2).
Table 2.
Logistic mixed model regression analysis for examining the effect of probiotic supplementation on bacterial genera abundance
| Probiotic (n = 38 infants, 124 specimens) |
Placebo (n = 28 infants, 91 specimens) |
||||||
|---|---|---|---|---|---|---|---|
| Genusa | Prevalence n infants (%)b; n specimens (%)c |
Relative abundance Mean % (SD) |
Prevalence n infants (%)b; n specimens (%)c |
Relative abundance Mean % (SD) |
AORd (95% CI) | P value | Adjusted P valuee |
| Bifidobacterium | 38 (100); 111 (90) | 36.4 (32.5) | 25 (89); 50 (55) | 17.5 (27.4) | 4.28 (2.02–9.10) | < 0.001 | 0.002 |
| Enterobacter | 37 (97); 95 (77) | 14.8 (24.6) | 28 (100); 77 (85) | 18.7 (25.1) | 0.75 (0.40–1.41) | 0.37 | 0.45 |
| Escherichia/Shigella | 37 (97); 84 (68) | 9.1 (19.1) | 28 (100); 74 (81) | 7.5 (17.2) | 0.69 (0.34–1.43) | 0.32 | 0.43 |
| Staphylococcus | 36 (95); 65 (52) | 8.1 (24.0) | 24 (86); 48 (53) | 7.5 (20.4) | 0.85 (0.47–1.55) | 0.60 | 0.60 |
| Enterococcus | 37 (97); 76 (61) | 3.7 (11.0) | 28 (100); 71 (78) | 8.8 (19.3) | 0.37 (0.20–0.71) | 0.003 | 0.02 |
| Streptococcus | 38 (100); 93 (75) | 4.7 (15.0) | 25 (89); 48 (53) | 2.9 (9.4) | 1.57 (0.88–2.80) | 0.13 | 0.31 |
| Veillonella | 32 (84); 56 (45) | 2.4 (7.2) | 25 (89); 46 (51) | 3.3 (7.9) | 0.74 (0.42–1.33) | 0.32 | 0.43 |
| Clostridium | 32 (84); 53 (43) | 0.5 (2.4) | 27 (96); 45 (49) | 3.0 (9.0) | 0.68 (0.38–1.21) | 0.19 | 0.31 |
| Lactobacillus | 23 (61); 41 (33) | 0.9 (3.7) | 13 (46); 19 (21) | 2 (7.6) | 1.85 (0.78–4.41) | 0.16 | 0.31 |
| Citrobacter | 20 (53); 27 (22) | 0.8 (3.4) | 21 (75); 34 (37) | 1.7 (10.1) | 0.44 (0.19–1.02) | 0.06 | 0.21 |
| Akkermansia | 6 (16); 6 (5) | 0.1 (0.5) | 3 (11); 3 (3) | 1.4 (9.2) | 1.87 (0.41–8.59) | 0.42 | 0.47 |
| Pantoea | 11 (29); 14 (11) | 0.1 (0.8) | 12 (43); 18 (20) | 1.1 (10.1) | 0.45 (0.15–1.35) | 0.15 | 0.31 |
Abbreviations: AOR adjusted odds ratio, CI confidence interval, IQR interquartile range; P values <0.05 are bolded to indicate statistically significant associations.
aProportional abundances of each genera were converted to a binary variable (based on the median value). Only genera that had a mean abundance of at least 1% abundant in one (or both) allocation group were included in regression analysis; b Presents the number (and percent) of infants who had at least on specimen over the study period test positive for genus; c Presents the number (and percent) of total specimens test positive for genus d Odds ratio for mixed effects regression model association between allocation group and bacterial abundance adjusted for gestation and age at sampling, clustering by participant number to account for multiple specimens from infants (66 clusters). e P-value false discovery rate adjustment for multiple testing was performed using the Benjamini-Hochberg method
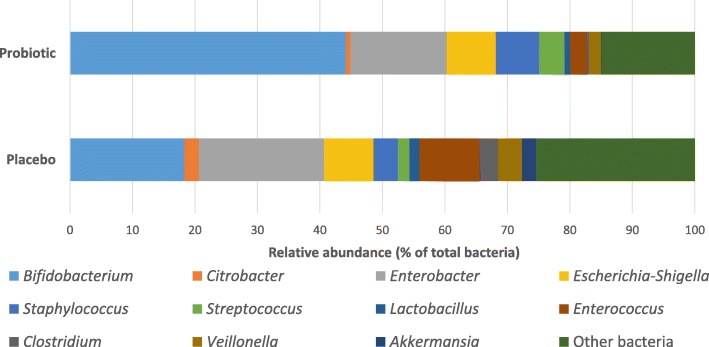
Twelve genera had a mean abundance of at least 1% in one (or both) allocation groups (Fig. 1) and these were the focus for regression analyses. After adjusting for age and gestation, babies receiving the probiotic had an increased abundance of Bifidobacterium (AOR 4.28; 95% CI, 2.02–9.10, adjusted p-value =0.002) and decreased abundance of Enterococcus (AOR 0.37; 95% CI, 0.20–0.71, adjusted p-value =0.02). Despite being detected more frequently in probiotic supplemented infants compared to control infants no significant difference in the abundance of Streptococcus was observed between allocation groups after adjusting for age and gestation (AOR 1.57; 95% CI, 0.88–2.79, adjusted p-value > 0.05; Table 2). Additional file 2 provides a graphical representation of the relative abundance of the 20 most abundant genera found in study specimens. Abundance data at the genus level for each specimen is provided in Additional file 3.
Fig. 1.
Compares the percent abundance of specific genera between the probiotic and placebo infants. The 12 genera included had a mean abundance of at least 1% in one (or both) allocation group and were included in the regression analysis. Bacteria not included in the regression analysis are grouped under “Other bacteria”
Given these findings, additional post-hoc logistic regression analyses were conducted. Specimens were grouped into two categories: collected during the supplementation period and collected post supplementation period. Supplementation on average started at four days of age and stopped at 68 days from birth. Eleven specimens collected before supplementation commenced were excluded from this analysis. Bifidobacterium and Enterococcus were regressed against allocation, adjusting for age, gestation and multiple specimens from each infant as above. The difference in abundance of Bifidobacterium and Enterococcus between the allocation groups was only evident during the supplementation period (AOR 17.22; 95% CI, 3.49–84.99, p < 0.001 and AOR 0.27; 95% CI, 0.09–0.82, p = 0.02 respectively) (Table 3).
Table 3.
Logistic mixed model regression analysis for examining the effect of probiotic supplementation on abundance of Bifidobacterium and Enterococcus during and following the supplementation period
| Specimens collected during supplementation period N=142a |
Specimens collected post supplementation period N=62a |
|||||||
|---|---|---|---|---|---|---|---|---|
| Genus | Probiotic % abundance mean (SD) (N = 80) |
Placebo % abundance mean (SD) (N = 62) |
AORb (95% CI) | P value | Probiotic % abundance mean (SD) (N = 41) |
Placebo % abundance mean (SD) (N = 21) |
AORc (95% CI) | P value |
| Bifidobacterium | 40.5 (31.9) | 14.4 (26.7) | 17.22 (3.49–84.99) | < 0.001 | 28.7 (31.2) | 26.9 (27.0) | 0.99 (0.30–3.26) | 0.99 |
| Enterococcus | 3.3 (8.9) | 10.0 (20.8) | 0.27 (0.09–0.82) | 0.02 | 4.9 (14.6) | 1.7 (1.9) | 0.36 (0.11–1.17) | 0.09 |
Abbreviations: AOR adjusted odds ratio, CI confidence interval, IQR interquartile range;
aA total of 204 specimens were included in this analysis. Specimens collected prior to the supplementation commenced (n = 11) were excluded from this analysis; b Odds ratio for adjusted mixed effects regression model for association between allocation group and bacterial abundance during the supplementation period, clustering by participant number to account for multiple specimens from infants (63 clusters); c Odds ratio for adjusted mixed effects regression model association between allocation group and bacterial abundance following the supplementation period, clustering by participant number to account for multiple specimens from infants (51 clusters)
Of note several genera were more abundant at different ages. Staphylococcus and Enterobacter were found in higher abundance in specimens collected closer to birth, compared to those collected later. Veillonella, Clostridium, Streptococcus, Akkermansia and Citrobacter were found in higher abundance in specimens collected later (Additional file 4).
No difference in effective number of genera was observed between the probiotic and placebo groups (adjusted coef − 0.3; 95% CI, − 0.7-0.1, p > 0.05).
Discussion
This sub-study investigated the effect of probiotic supplementation with B. longum subsp. infantis BB-02, S. thermophilus TH-4 and B. animalis subsp. lactis BB-12 on the gut microbiota of a subset of very preterm infants enrolled in the ProPrems trial and found that infants supplemented with probiotics had a higher abundance of Bifidobacterium compared to control infants.
ProPrems demonstrated that probiotic supplementation with BB-02, TH-4 and BB-12 resulted in a 54% relative risk reduction in NEC of Bell stage 2 or more [19]. However, as the incidence of NEC in the ProPrems control infants was low (4.4%) and only one infant who developed NEC was included in this sub-study, few conclusions can be made about the mechanism/s by which the probiotics may work to prevent NEC. Nevertheless, it is noteworthy that the increased abundance of Bifidobacterium in probiotic-supplemented infants was only observed during the supplementation period. This may suggest that increased abundance of Bifidobacterium when the gut and immune system are most immature is important in reducing the risk of NEC in very preterm infants.
Bifidobacterium spp. are known inhabitants of the adult and full term infant gut, but their presence is often reduced or delayed in preterm infants [30, 31]. Probiotic supplementation with Bifidobacterium spp. has been shown to promote colonization of Bifidobacterium spp. in preterm and low birth weight infants [20, 32–36], often resulting in positive effects including weight gain, decreased intestinal permeability, reduction in abundance of potentially pathogenic bacteria, and establishment of a gut microbiota similar to that of healthy full term infants [33, 35, 36].
Interestingly, the PiPs Study found no reduction in the incidence NEC in infants supplemented with Bifidobacterium breve BBG-001, despite confirmation of B. breve colonization by culture and qPCR in 85% of probiotic supplemented infants and 37% of control infants at 2 weeks postnatal age [20]. The results of the PiPs Study highlight the importance of Bifidobacterium strain/s selection in developing an effective probiotic for preventing NEC [37]. Given the multifactorial nature of NEC, and that different bacterial strains are thought to exert probiotic effects by different mechanisms, multi-strain probiotics may be more beneficial than single-strain formulations in the prevention of NEC [38]. This is supported by a recent meta-analysis that reported a lower incidence of NEC in infants supplemented with multi-strain probiotics compared with infants supplemented with single strain combinations using Lactobacillus spp., Bifidobacterium spp. and Saccharomyces boulardii [39].
Despite detecting a difference in the abundance of Bifidobacterium between the allocation groups, no similar effect was observed for Streptococcus. This is despite the probiotic comprising both Bifidobacterium and Streptococcus, and the prevalence of Streptococcus being higher in the probiotic group compared to the placebo group. This may indicate that Bifidobacterium has a more intimate interaction with the gut mucosa than Streptococcus [40, 41]. The increased abundance of Bifidobacterium compared to Streptococcus could also be a result of the greater quantity of Bifidobacterium in the probiotic formulation compared to Streptococcus.
Excluding Bifidobacterium, the most abundant bacterial taxonomic groups identified were the genera Enterococcus, Staphylococcus and Streptococcus and the Enterobacteriaceae family, which is consistent with current literature for preterm infants [32, 42, 43]. Enterococcus was the only genus found in significantly higher abundance in the control infants. Enterococci are known colonizers of the preterm gut, and have been identified in both healthy infants and infants who go on to develop NEC [44–47].
This study has a number of limitations. First, 16S rRNA gene sequencing only allowed allocation of reads to genus level. As a result, it cannot be determined if the increase in Bifidobacterium in the probiotic-supplemented infants comprised the probiotic BB-12 and BB-02 strains. Furthermore, we observed an overall high abundance of Bifidobacterium in both allocation groups compared to other studies of the infant gut microbiota [13, 48, 49]. This could be a result of the bifidobacteria optimised primers used for 16S rRNA gene amplification, which have been shown to improve the amplification of Bifidobacterium in fecal samples [22]. Cross-colonization may also have accounted for the higher than expected abundance of Bifidobacterium observed in controls. We previously reported a low occurrence of probiotic cross-colonization of infants in a neonatal unit during and after the ProPrems study [50]. However, this study was limited by a small number of ProPrems participants (twelve of the 87 infants analyzed were ProPrems participants) and several studies have reported cross-colonization in up to 44% of control infants during and/or after supplementation [20, 33]. Future research utilizing a whole metagenome approach will provide species and strain level information, as well as identify whether cross-colonization or primer selection may have influenced the microbial profiles presented here.
Second, infants included in this study contributed variable numbers of specimens, so colonization patterns could not be established for all infants. Additionally, only eleven specimens collected before supplementation commenced were available for analysis. As a result, we do not know if there was a difference in the pre-supplementation gut microbiota between the two allocation groups. Finally, the 66 infants included in this sub-study represent only a small proportion of the 1099 total ProPrems study population. Though the infants in this sub-study are representative of the wider ProPrems cohort in terms of demographic details, they did have a lower incidence of NEC (Bell Stage 2 or more). Specimens from only one infant who developed NEC were available for inclusion in this sub-study. As such, we cannot compare the gut microbiota of infants who developed NEC with those who remained healthy.
Conclusion
Probiotic supplementation with BB-02, BB-12, and TH-4 increased the abundance of Bifidobacterium in the gut microbiota of very preterm infants during probiotic supplementation. Increased abundance of Bifidobacterium shortly after birth may be protective against NEC. A detailed understanding of the impact of probiotic supplementation on the gut microbiota at a strain level is required given current research has highlighted that selecting the appropriate Bifidobacterium strain/s for probiotic supplementation in very preterm infants is crucial.
Additional files
Comparison of demographics of sub-study participants and the wider ProPrems cohort (DOCX 13 kb)
Heatmap of bacterial abundance in all study specimens. Each vertical line represents the bacterial composition of one specimen. The 20 most abundant taxa found in specimens are included in the heatmap. Allocation group is displayed above the heatmap in red (probiotic) and blue (placebo). The stage of study is also displayed above the heatmap in purple (before supplementation), pink (during supplementation) and cyan (post supplementation). (PDF 116 kb)
Relative abundance of all detected genera for each specimen (XLSX 120 kb)
Logistic mixed model regression analysis for examining the effect of time from birth on bacterial genera abundance. (DOCX 16 kb)
Acknowledgments
We acknowledge Dr. Jimmy Twin for the sample preparation and laboratory work completed in this study. Members of The ProPrems Study Group are as follows: ProPrems Steering Group – S.M. Garland (principal investigator), S.E. Jacobs (chief investigator), J.M. Tobin (chief investigator), S.N. Tabrizi (chief investigator), M. Pirotta (chief investigator), S. Donath (associate investigator), G.F. Opie (associate investigator), M.L.K. Tang (associate investigator), C.J. Morley (associate investigator); Participating Hospitals and Investigators – S.M. Garland, S.E. Jacobs, C.J. Morley, S.N. Tabrizi, L. Hickey, The Royal Women’s Hospital; G.F. Opie, Mercy Hospital for Women; K. Tan, A. Lewis, A. Veldman, Monash Medical Centre; M.L.K. Tang, Royal Children’s Hospital, all in Melbourne, Australia; J. Travadi, I.M. R. Wright, John Hunter Children’s Hospital; D.A. Osborn, Royal Prince Alfred Hospital; J. Sinn, Royal North Shore Hospital; J. Levison, J.A. Stack, Liverpool Hospital, all in New South Wales, Australia; A.G. DePaoli, Royal Hobart Hospital, Tasmania, Australia; N.C. Austin, B.A. Darlow, Christchurch Women’s Hospital, University of Otago, Christchurch, New Zealand; J.M. Alsweiler, M.J Buksh, Auckland City Hospital and The Liggins Institute, University of Auckland, Auckland, New Zealand.
Funding
Supported by the National Health and Research Medical Council of Australia (project grant 454629), The Royal Women’s Hospital Foundation, Melbourne, Australia, and The Angior Family Foundation, Melbourne, Australia. ELP received a bursary scholarship from Victorian Life Science Computation Initiative. Solgar, USA supplied the probiotic combination “ABC Dophilus Powder for Infants” at cost, but did not provide the study with support of any kind. The funders had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript. The authors have no other financial relationships relevant to this article to disclose.
Availability of data and materials
Raw sequencing data have been deposited in NCBI’s Short Read Archive (SRA) under BioProject PRJNA353658, https://www.ncbi.nlm.nih.gov/bioproject/PRJNA353658/.
Abbreviations
- AOR
Adjusted odds ratio
- CI
Confidence interval
- NEC
Necrotizing enterocolitis
- rRNA
ribosomal RNA
Authors’ contributions
SMG conceptualized and designed this sub-study. SMG and SEJ contributed equally to the coordination of the ProPrems trial from which the samples used in this sub-study were collected. ELP generated the microbiota data, carried out data analysis and drafted the initial manuscript under the supervision of SMG, SNT and DMB. SNT coordinated and supervised the laboratory work. ELP, DMB, GLM, SEJ, SNT and SMG contributed significantly to data interpretation, manuscript writing and editing of the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The ProPrems study was approved by The Royal Women’s Hospital (Melbourne) Human Research and Ethics Committees, and specimens were collected after obtaining written informed consent from parents or guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Erica L. Plummer, Email: erica.plummer@mcri.edu.au
Dieter M. Bulach, Email: dieter.bulach@unimelb.edu.au
Gerald L. Murray, Email: gerald.murray@mcri.edu.au
Susan E. Jacobs, Email: Sue.Jacobs@thewomens.org.au
Sepehr N. Tabrizi, Email: sepehr.tabrizi@gmail.com
Suzanne M. Garland, Email: suzanne.garland@thewomens.org.au
for the ProPrems Study Group:
S. M. Garland, S. E. Jacobs, J. M. Tobin, S. N. Tabrizi, M. Pirotta, S. Donath, G. F. Opie, M. L. K. Tang, C. J. Morley, L. Hickey, K. Tan, A. Lewis, A. Veldman, J. Travadi, I. M. R. Wright, D. A. Osborn, J. Sinn, J. Levison, J. A. Stack, A. G. DePaoli, N. C. Austin, B. A. Darlow, J. M. Alsweiler, and M. J. Buksh
References
- 1.Chang HH, Larson J, Blencowe H, Spong CY, Howson CP, Cairns-Smith S, Lackritz EM, Lee SK, Mason E, Serazin AC, et al. Preventing preterm births: analysis of trends and potential reductions with interventions in 39 countries with very high human development index. Lancet. 2013;381:223–234. doi: 10.1016/S0140-6736(12)61856-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cilieborg MS, Boye M, Sangild PT. Bacterial colonization and gut development in preterm neonates. Early Hum Dev. 2012;88(Suppl 1):S41–S49. doi: 10.1016/j.earlhumdev.2011.12.027. [DOI] [PubMed] [Google Scholar]
- 3.Matamoros S, Gras-Leguen C, Le Vacon F, Potel G, de La Cochetiere MF. Development of intestinal microbiota in infants and its impact on health. Trends Microbiol. 2013;21:167–173. doi: 10.1016/j.tim.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Underwood MA, Sohn K. The microbiota of the extremely preterm infant. Clin Perinatol. 2017;44:407–427. doi: 10.1016/j.clp.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011;364:255–264. doi: 10.1056/NEJMra1005408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luedtke SA, Yang JT, Wild HE. Probiotics and necrotizing enterocolitis: finding the missing pieces of the probiotic puzzle. J Pediatr Pharmacol Ther. 2012;17:308–328. doi: 10.5863/1551-6776-17.4.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samuels N, van de Graaf RA, de Jonge RCJ, Reiss IKM, Vermeulen MJ. Risk factors for necrotizing enterocolitis in neonates: a systematic review of prognostic studies. BMC Pediatr. 2017;17:105. doi: 10.1186/s12887-017-0847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel RM, Denning PW. Intestinal microbiota and its relationship with necrotizing enterocolitis. Pediatr Res. 2015;78:232–238. doi: 10.1038/pr.2015.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wendelboe AM, Smelser C, Lucero CA, McDonald LC. Cluster of necrotizing enterocolitis in a neonatal intensive care unit: New Mexico, 2007. Am J Infect Control. 2010;38:144–148. doi: 10.1016/j.ajic.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boccia D, Stolfi I, Lana S, Moro ML. Nosocomial necrotising enterocolitis outbreaks: epidemiology and control measures. Eur J Pediatr. 2001;160:385–391. doi: 10.1007/s004310100749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Torrazza RM, Neu J. The altered gut microbiome and necrotizing enterocolitis. Clin Perinatol. 2013;40:93–108. doi: 10.1016/j.clp.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hosny M, Cassir N, La Scola B. Updating on gut microbiota and its relationship with the occurrence of necrotizing enterocolitis. Human Microbiome Journal. 2017;4:14–19. doi: 10.1016/j.humic.2016.09.002. [DOI] [Google Scholar]
- 13.Warner BB, Deych E, Zhou Y, Hall-Moore C, Weinstock GM, Sodergren E, Shaikh N, Hoffmann JA, Linneman LA, Hamvas A, et al. Gut bacteria dysbiosis and necrotising enterocolitis in very low birthweight infants: a prospective case-control study. Lancet. 2016;387:1928–1936. doi: 10.1016/S0140-6736(16)00081-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McMurtry VE, Gupta RW, Tran L, EEt B, Penn D, Taylor CM, Ferris MJ. Bacterial diversity and clostridia abundance decrease with increasing severity of necrotizing enterocolitis. Microbiome. 2015;3:11. doi: 10.1186/s40168-015-0075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou Y, Shan G, Sodergren E, Weinstock G, Walker WA, Gregory KE. Longitudinal analysis of the premature infant intestinal microbiome prior to necrotizing enterocolitis: a case-control study. PLoS One. 2015;10:e0118632. doi: 10.1371/journal.pone.0118632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sim K, Shaw AG, Randell P, Cox MJ, McClure ZE, Li MS, Haddad M, Langford PR, Cookson WO, Moffatt MF, Kroll JS. Dysbiosis anticipating necrotizing enterocolitis in very premature infants. Clin Infect Dis. 2015;60:389–397. doi: 10.1093/cid/ciu822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Torrazza RM, Ukhanova M, Wang X, Sharma R, Hudak ML, Neu J, Mai V. Intestinal microbial ecology and environmental factors affecting necrotizing enterocolitis. PLoS One. 2013;8:e83304. doi: 10.1371/journal.pone.0083304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lau CS, Chamberlain RS. Probiotic administration can prevent necrotizing enterocolitis in preterm infants: a meta-analysis. J Pediatr Surg. 2015;50:1405–1412. doi: 10.1016/j.jpedsurg.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Jacobs SE, Tobin JM, Opie GF, Donath S, Tabrizi SN, Pirotta M, Morley CJ, Garland SM, ProPrems Study G. Probiotic effects on late-onset sepsis in very preterm infants: a randomized controlled trial. Pediatrics. 2013;132:1055–1062. doi: 10.1542/peds.2013-1339. [DOI] [PubMed] [Google Scholar]
- 20.Costeloe K, Hardy P, Juszczak E, Wilks M, Millar MR, Probiotics in Preterm Infants Study Collaborative G Bifidobacterium breve BBG-001 in very preterm infants: a randomised controlled phase 3 trial. Lancet. 2016;387:649–660. doi: 10.1016/S0140-6736(15)01027-2. [DOI] [PubMed] [Google Scholar]
- 21.Garland SM, Tobin JM, Pirotta M, Tabrizi SN, Opie G, Donath S, Tang ML, Morley CJ, Hickey L, Ung L, et al. The ProPrems trial: investigating the effects of probiotics on late onset sepsis in very preterm infants. BMC Infect Dis. 2011;11:210. doi: 10.1186/1471-2334-11-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sim K, Cox MJ, Wopereis H, Martin R, Knol J, Li MS, Cookson WO, Moffatt MF, Kroll JS. Improved detection of bifidobacteria with optimised 16S rRNA-gene based pyrosequencing. PLoS One. 2012;7:e32543. doi: 10.1371/journal.pone.0032543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edgar RC, Haas BJ, Clemente JC, Quince C, Knight R. UCHIME improves sensitivity and speed of chimera detection. Bioinformatics. 2011;27:2194–2200. doi: 10.1093/bioinformatics/btr381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haas BJ, Gevers D, Earl AM, Feldgarden M, Ward DV, Giannoukos G, Ciulla D, Tabbaa D, Highlander SK, Sodergren E, et al. Chimeric 16S rRNA sequence formation and detection in sanger and 454-pyrosequenced PCR amplicons. Genome Res. 2011;21:494–504. doi: 10.1101/gr.112730.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Quast C, Pruesse E, Yilmaz P, Gerken J, Schweer T, Yarza P, Peplies J, Glockner FO. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 2013;41:D590–D596. doi: 10.1093/nar/gks1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2017. https://www.R-project.org/.
- 27.Oksanen J, Blanchet FG, Friendly M, Kindt R, Legendre P, McGlinn D, Minchin PR, O'Hara RB, Simpson GL, Solymos P, et al. vegan: community ecology package. R package version 2.0-10 edition. 2013. [Google Scholar]
- 28.Bates D, Maechler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- 29.Warnes G, Bolker B, Bonebakker L, Gentleman R, Liaw W, Lumley T, Maechler M, Magnusson A, Moeller S, Schwartz M, Venables B. gplots: various R programming tools for plotting data., R package version 3.0.1 edition. 2016. [Google Scholar]
- 30.Buccigrossi V, Nicastro E, Guarino A. Functions of intestinal microflora in children. Curr Opin Gastroenterol. 2013;29:31–38. doi: 10.1097/MOG.0b013e32835a3500. [DOI] [PubMed] [Google Scholar]
- 31.Hallab JC, Leach ST, Zhang L, Mitchell HM, Oei J, Lui K, Day AS. Molecular characterization of bacterial colonization in the preterm and term infant's intestine. Indian J Pediatr. 2013;80:1–5. doi: 10.1007/s12098-012-0753-5. [DOI] [PubMed] [Google Scholar]
- 32.Abdulkadir B, Nelson A, Skeath T, Marrs EC, Perry JD, Cummings SP, Embleton ND, Berrington JE, Stewart CJ. Routine use of probiotics in preterm infants: longitudinal impact on the microbiome and metabolome. Neonatology. 2016;109:239–247. doi: 10.1159/000442936. [DOI] [PubMed] [Google Scholar]
- 33.Kitajima H, Sumida Y, Tanaka R, Yuki N, Takayama H, Fujimura M. Early administration of Bifidobacterium breve to preterm infants: randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 1997;76:F101–F107. doi: 10.1136/fn.76.2.F101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Y, Shimizu T, Hosaka A, Kaneko N, Ohtsuka Y, Yamashiro Y. Effects of bifidobacterium breve supplementation on intestinal flora of low birth weight infants. Pediatr Int. 2004;46:509–515. doi: 10.1111/j.1442-200x.2004.01953.x. [DOI] [PubMed] [Google Scholar]
- 35.Mohan R, Koebnick C, Schildt J, Schmidt S, Mueller M, Possner M, Radke M, Blaut M. Effects of Bifidobacterium lactis Bb12 supplementation on intestinal microbiota of preterm infants: a double-blind, placebo-controlled, randomized study. J Clin Microbiol. 2006;44:4025–4031. doi: 10.1128/JCM.00767-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stratiki Z, Costalos C, Sevastiadou S, Kastanidou O, Skouroliakou M, Giakoumatou A, Petrohilou V. The effect of a bifidobacter supplemented bovine milk on intestinal permeability of preterm infants. Early Hum Dev. 2007;83:575–579. doi: 10.1016/j.earlhumdev.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 37.Abrahamsson TR. Not all probiotic strains prevent necrotising enterocolitis in premature infants. Lancet. 2016;387:624–625. doi: 10.1016/S0140-6736(15)01090-9. [DOI] [PubMed] [Google Scholar]
- 38.Di Gioia D, Aloisio I, Mazzola G, Biavati B. Bifidobacteria: their impact on gut microbiota composition and their applications as probiotics in infants. Appl Microbiol Biotechnol. 2014;98:563–577. doi: 10.1007/s00253-013-5405-9. [DOI] [PubMed] [Google Scholar]
- 39.Chang HY, Chen JH, Chang JH, Lin HC, Lin CY, Peng CC. Multiple strains probiotics appear to be the most effective probiotics in the prevention of necrotizing enterocolitis and mortality: an updated meta-analysis. PLoS One. 2017;12:e0171579. doi: 10.1371/journal.pone.0171579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elli M, Callegari ML, Ferrari S, Bessi E, Cattivelli D, Soldi S, Morelli L, Goupil Feuillerat N, Antoine JM. Survival of yogurt bacteria in the human gut. Appl Environ Microbiol. 2006;72:5113–5117. doi: 10.1128/AEM.02950-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.He F, Ouwehand AC, Isolauri E, Hashimoto H, Benno Y, Salminen S. Comparison of mucosal adhesion and species identification of bifidobacteria isolated from healthy and allergic infants. FEMS Immunol Med Microbiol. 2001;30:43–47. doi: 10.1111/j.1574-695X.2001.tb01548.x. [DOI] [PubMed] [Google Scholar]
- 42.Millar M, Seale J, Greenland M, Hardy P, Juszczak E, Wilks M, Panton N, Costeloe K, Wade WG. The microbiome of infants recruited to a randomised placebo-controlled probiotic trial (PiPS trial) EBioMedicine. 2017;20:255–262. doi: 10.1016/j.ebiom.2017.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mshvildadze M, Neu J, Mai V. Intestinal microbiota development in the premature neonate: establishment of a lasting commensal relationship? Nutr Rev. 2008;66:658–663. doi: 10.1111/j.1753-4887.2008.00119.x. [DOI] [PubMed] [Google Scholar]
- 44.Arboleya S, Binetti A, Salazar N, Fernandez N, Solis G, Hernandez-Barranco A, Margolles A, de Los Reyes-Gavilan CG, Gueimonde M. Establishment and development of intestinal microbiota in preterm neonates. FEMS Microbiol Ecol. 2012;79:763–772. doi: 10.1111/j.1574-6941.2011.01261.x. [DOI] [PubMed] [Google Scholar]
- 45.Moles L, Gomez M, Heilig H, Bustos G, Fuentes S, de Vos W, Fernandez L, Rodriguez JM, Jimenez E. Bacterial diversity in meconium of preterm neonates and evolution of their fecal microbiota during the first month of life. PLoS One. 2013;8:e66986. doi: 10.1371/journal.pone.0066986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morrow AL, Lagomarcino AJ, Schibler KR, Taft DH, Yu Z, Wang B, Altaye M, Wagner M, Gevers D, Ward DV, et al. Early microbial and metabolomic signatures predict later onset of necrotizing enterocolitis in preterm infants. Microbiome. 2013;1:13. doi: 10.1186/2049-2618-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stewart CJ, Marrs EC, Magorrian S, Nelson A, Lanyon C, Perry JD, Embleton ND, Cummings SP, Berrington JE. The preterm gut microbiota: changes associated with necrotizing enterocolitis and infection. Acta Paediatr. 2012;101:1121–1127. doi: 10.1111/j.1651-2227.2012.02801.x. [DOI] [PubMed] [Google Scholar]
- 48.Cong X, Xu W, Janton S, Henderson WA, Matson A, McGrath JM, Maas K, Graf J. Gut microbiome developmental patterns in early life of preterm infants: impacts of feeding and gender. PLoS One. 2016;11:e0152751. doi: 10.1371/journal.pone.0152751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jacquot A, Neveu D, Aujoulat F, Mercier G, Marchandin H, Jumas-Bilak E, Picaud JC. Dynamics and clinical evolution of bacterial gut microflora in extremely premature patients. J Pediatr. 2011;158:390–396. doi: 10.1016/j.jpeds.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 50.Hickey L, Garland SM, Jacobs SE, O'Donnell CP, Tabrizi SN, ProPrems Study G. Cross-colonization of infants with probiotic organisms in a neonatal unit. J Hosp Infect. 2014;88:226–229. doi: 10.1016/j.jhin.2014.09.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparison of demographics of sub-study participants and the wider ProPrems cohort (DOCX 13 kb)
Heatmap of bacterial abundance in all study specimens. Each vertical line represents the bacterial composition of one specimen. The 20 most abundant taxa found in specimens are included in the heatmap. Allocation group is displayed above the heatmap in red (probiotic) and blue (placebo). The stage of study is also displayed above the heatmap in purple (before supplementation), pink (during supplementation) and cyan (post supplementation). (PDF 116 kb)
Relative abundance of all detected genera for each specimen (XLSX 120 kb)
Logistic mixed model regression analysis for examining the effect of time from birth on bacterial genera abundance. (DOCX 16 kb)
Data Availability Statement
Raw sequencing data have been deposited in NCBI’s Short Read Archive (SRA) under BioProject PRJNA353658, https://www.ncbi.nlm.nih.gov/bioproject/PRJNA353658/.