Abstract
BACKGROUND:
Cefixime is a widely used third-generation cephalosporin schedule H1 drug, which is prescribed for the treatment of otitis media, respiratory tract infections, and uncomplicated urinary tract infections and is effective against infections caused by Enterobacteriaceae and Haemophilus influenzae species in India. The National Coordination Centre (NCC)-Pharmacovigilance Programme of India (PvPI), Indian Pharmacopoeia Commission (IPC), has received rare individual case safety reports (ICSRs) for acute generalized exanthematous pustulosis (AGEP) associated with the use of cefixime.
MATERIALS AND METHODS:
IPC, NCC-PvPI also acts as a national collaborating center for pharmacovigilance activities under the aegis of Ministry of Health and Family Welfare, Government of India; moreover, it is a member country in global pharmacovigilance system, World Health Organization-Uppsala Monitoring Centre, Sweden. There are more than 250 government/corporate medical colleges and hospitals acting as regional adverse drug reaction monitoring centers, actively functioning under PvPI. Furthermore, various stakeholders including consumers and pharmaceutical industries also play a significant contribution. NCC-PvPI receives spontaneous ICSRs from various stakeholders.
RESULTS:
NCC-PvPI, IPC has received a total of four spontaneous ICSRs for cefixime-induced AGEP. After clinical evaluation of reported ICSRs, a strong causal relationship was established between AGEP and cefixime and was supported by published literature and histopathological examination of skin. Based on the statistics with positive information component (IC025 Value: 0.17) and proportionality relative risk (PRR:3.4), PvPI considered cefixime-associated AGEP may be a potential signal.
CONCLUSION:
Hence, initially, AEGP is considered by PvPI as drug safety alert in July 2016. Therefore, to enhance the safety of population in rational usage of medication, as a result, there is a need for physicians and health-care professionals to sensitize about serious adverse reaction while prescribing the cefixime as signal in India.
Keywords: Acute generalized exanthematous pustulosis, cefixime, National Coordination Centre-Pharmacovigilance Programme of India, World Health Organization-Uppsala Monitoring Centre
Introduction
Acute generalized exanthematous pustulosis (AGEP) is a rare cutaneous reaction which advances with multiple pustular lesions on erythematous and edematous surface accompanying with a systemic fever.[1] The European Study of Severe Cutaneous Adverse Reactions study uses scoring scale to distinguish the pustular psoriasis from other pustular eruptions. Approximately 90% AGEP cases were due to the systemic drugs, of which antibiotics are proclaimed to be primary etiology. In addition to this viral and bacterial infections may serve as occasional causes.[2,3,4] The current study is in contrast to the above-stated causes. When all causal associations are ruled out, hence the disease is limited to bias. Symptomatic treatment can be given by using steroids for short term period.[5]
Cefixime is a broad-spectrum antibiotic, mainly used for the treatment of infection-associated bacteria, and it comes under category of third-generation cephalosporin antibiotic. Which involves in mechanism of action by inhibition of bacterial growth. The common side effects include diarrhea, abdominal pain, and nausea, and serious adverse reaction may include allergic reactions.[6] Although AGEP associated with cefixime is not well known adverse reaction also not labeled in drug safety information. However, evidence of safety information reveals that this suspected medication causes various cutaneous reactions. The current article demonstrates a case of cefixime-induced AGEP.
Materials and Methods
NCC-PvPI has been received spontaneous cases from healthcare professionals from four different hospital in India during period of 2013-2018. The data is collated in national Pharmacovigilance database. Patient demographic data, laboratory and clinical investigation data, pre-existing conditions, and disease signs and symptoms were analysed. Causality assessment had been done by considering all other histopathological conditions.
Patients admitted to four different hospitals which are taking part in PvPI and diagnosed with AEGP were analyzed. All cases were evaluated by dermatologist who assessed the patients directly. Information regarding medical history, laboratory investigations, suspected medication(s) and concomitant medication(s), and other relevant information were recorded. AEGP was diagnosed based on the clinical features and histopathology.[7] Causality assessment for suspected adverse reactions was done using the World Health Organization-Uppsala Monitoring Centre (WHO-UMC) causality assessment scale. Out of four spontaneous cases, causality assessment for two cases were found to probable or likely and other two cases found to be possible causal association with the suspected medication. Concisely assessment method includes temporal drug usage, onset of reaction, and clinical manifestation of drug and past history of medication, Rechallenge and dechallenge information. There are certain parameters such as concomitant medication and other possible signs and symptoms were also assessed.
Results
A total of four cases fulfilled the AEGP diagnostic criteria with clinical and histopathological report. Reports from two age groups, adolescent and adults in equal percentage, were received spontaneously. There is only one female report from the total reports. From the interpretation of data, Indication for cefixime for majority reports were reported fever followed by vomiting and acute nasopharyngitis. In our data, only two reports state usage of concomitant medications along with suspected medication. No history of psoriasis was recorded and no other clinical manifestations also noticed. In all cases dechallenge was done subsequently improvement in patient condition were noticed. Outcome were recovering or resolving at the time of report in majority cases, knowingly outcome of one case was recovered/resolved at the time of report. We failed to take follow-up from the patient's whose outcome was under recovering. Causality assessment were done for all four cases by considering the all relevant information. The signal review panel (SRP) of PvPI was considered and approved this drug-ADR combination as Indian centric potential drug safety signal based by adopting quantitative and qualitative methods for the identification of signals for Individual case safety reports (ICSRs) (Ncom= 4, IC025= 0.17 and PRR 3.4).[8]
Discussion
Drugs particularly antibiotics are primary causal association for this etiopathogenesis. The evidence from the literature reports reveals that drug-induced AGEP progress within 24 h.[9,10,11,12,13] Similar onset of time was reported in all reported adverse reaction reports. Scientifically, it is identified by certain clinical parameters such as immediate course of action, type of eruptions, single episode, without any history of arthritis, and perpetual administration of drugs. The latency period of AGEP in all reported cases was 24–48 h without any history of psoriasis. No patient developed AGEP with known drug allergy. Although cefixime is a class of cephalosporin antibiotics, however AGEP not commonly seen with cefixime. The pustular eruption spreads rapidly and tends to unite within less time. In our present reported cases, the onset of the adverse reaction was consistent with the literature. Furthermore, no mucosal involvement and no lesions were observed apart from the erythematous skin.
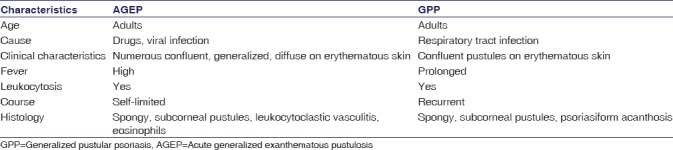
AGEP and generalized pustular psoriasis having clinical and histological similarities, However there are certain major differences between the two conditions are depicted in Table 1.[10,15] Initially, the lesion of AGEP develops on the face, followed by proliferating to the trunk and limbs. It is very hard to distinguish AGEP from GPP, although there are certain limitations to find out the case. The presence of eosinophils and neutrophils, necrotic keratinocytes, which describes as a major epidermal features and a conspicuously high prevalence of dermal infiltrates and absence of tortuous or dilated blood vessels aids AGEP. Histopathological examination of skin biopsy in reported cases showed the presence of epidermis showing intraepidermal pustules formation containing acute inflammatory cell exudates, surrounding epidermis showing spongiosis, vacuolization, and exocytosis. Superficial dermis showed perivascular and periadnexal mixed inflammatory cell infiltrate. The features are consistent with AGEP in all reported cases.
Table 1.
Factors outweigh diagnosis of acute generalized exanthematous pustulosis over generalized pustular psoriasis
AGEP is an uncommon adverse reaction associated with the medication, with the reported rate not more than 5 cases/million people/year.[15] By considering global data pertaining to current study following ICSR's reported till date, that is 01 report identified from Asia (Turkey), followed by two cases from Europe (Italy).[16] AGEP is not listed in summary of product characteristics and patient information leaflet of cefixime marketed in India, the United Kingdom,[17] and also in the United States.[18] Initially NCC-PvPI issued a drug safety alert based on the information received till July 2016[19] same shall be intimated through website and newsletter to HCP's and consumers to implement targeted or stimulated spontaneous reporting system in India.[20] After implementation of stimulated reporting system, few more cases were received. Subsequent profound assessment of this cases done by adopting signal identification criteria of NCC. Signal proposal were suggested to signal review panel of PvPI followed by Central drugs standard control organisation for regulatory intervention. The Indian regulatory requested for the revision of drug safety labels of Cefixime with the prevailing adverse drug reaction,[21] where it being marketed by generic & various brand names in India.
Conclusion
Spontaneous reported cases of AGEP associated with the treatment using Cefixim deduce that there is a potential risk for systemic involvement in patients with AEGP. Hence all prescribers should be aware about the potential risk of adverse reaction while prescribing cefixime in order to ensure the patient safety.
Limitation of the study
All 04 spontaneous cases reported to NCC-PvPI through spontaneous reporting system in India, however same study shall be extended by adopting complementing spontaneous reporting system i.e. targeted spontaneous reporting.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors acknowledge NCC-PvPI, Indian Pharmacopeia Commission, Department of Pharmacology, Postgraduate Institute of Medical Education and Research, Chandigarh, and IKG Punjab Technical University, Kapurthala, for Scientific and Technical support.
References
- 1.Chaabane A, Aouam K, Gassab L, Njim L, Boughattas NA. Acute generalized exanthematous pustulosis (AGEP) induced by cefotaxime. Fundam Clin Pharmacol. 2010;24:429–32. doi: 10.1111/j.1472-8206.2009.00794.x. [DOI] [PubMed] [Google Scholar]
- 2.Beylot C, Bioulac P, Doutre MS. Acute generalized exanthematic pustuloses (four cases) (author's transl) Ann Dermatol Venereol. 1980;107:37–48. [PubMed] [Google Scholar]
- 3.Lowell AG, Stephen IK, Barbara AG, Amy SP, David JL, Wolff K, et al. Fitzpatrick's Dermatology in General Medicine. 6th ed. New York: McGraw-Hill; 2003. pp. 625–7. [Google Scholar]
- 4.Roujeau JC, Bioulac-Sage P, Bourseau C, Guillaume JC, Bernard P, Lok C, et al. Acute generalized exanthematous pustulosis. Analysis of 63 cases. Arch Dermatol. 1991;127:1333–8. [PubMed] [Google Scholar]
- 5.Won JH, Yun SJ, Kim SJ, Lee SC, Won YH, Lee JB, et al. A case of acute generalized exanthematous pustulosis possibly induced by ritodrine. Ann Dermatol. 2009;21:323–5. doi: 10.5021/ad.2009.21.3.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brogden RN, Campoli-Richards DM. Cefixime. A review of its antibacterial activity. Pharmacokinetic properties and therapeutic potential. Drugs. 1989;38:524–50. doi: 10.2165/00003495-198938040-00004. [DOI] [PubMed] [Google Scholar]
- 7.Nacaroglu HT, Celegen M, Ozek G, Umac O, Karkıner CS, Yıldırım HT, et al. Acute generalized exanthematous pustulosis induced by ceftriaxone use. Postepy Dermatol Alergol. 2014;31:269–71. doi: 10.5114/pdia.2014.40938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalaiselvan V, Tripathi A, Archana S, Ranvir K, Rishi K, Prasad T, et al. Quantitative Methods for the Identification of Signals for Individual Case Safety Reports in India, Therapeutic Innovation & Regulatory Sciences. 2015 Jun 25; doi: 10.1177/2168479015589822. [DOI] [PubMed] [Google Scholar]
- 9.Sidoroff A, Dunant A, Viboud C, Halevy S, Bavinck JN, Naldi L, et al. Risk factors for acute generalized exanthematous pustulosis (AGEP)-results of a multinational case-control study (EuroSCAR) Br J Dermatol. 2007;157:989–96. doi: 10.1111/j.1365-2133.2007.08156.x. [DOI] [PubMed] [Google Scholar]
- 10.Sidoroff A, Halevy S, Bavinck JN, Vaillant L, Roujeau JC. Acute generalized exanthematous pustulosis (AGEP) – A clinical reaction pattern. J Cutan Pathol. 2001;28:113–9. doi: 10.1034/j.1600-0560.2001.028003113.x. [DOI] [PubMed] [Google Scholar]
- 11.Litt JZ. Drug Eruptions & Reactions Manual. 16th ed. New York: Informa Healthcare; 2010. p. 572. [Google Scholar]
- 12.Auer-Grumbach P, Pfaffenthaler E, Soyer HP. Pustulosis acuta generalisata is a post-streptococcal disease and is distinct from acute generalized exanthematous pustulosis. Br J Dermatol. 1995;133:135–9. doi: 10.1111/j.1365-2133.1995.tb02508.x. [DOI] [PubMed] [Google Scholar]
- 13.Belda Junior W, Ferolla AC. Acute generalized exanthematous pustulosis (AGEP). Case report. Rev Inst Med Trop Sao Paulo. 2005;47:171–6. doi: 10.1590/s0036-46652005000300011. [DOI] [PubMed] [Google Scholar]
- 14.Sampaio SA, Rivitti EA. Brazil: Dermatologia São Paulo, Artes Médicas; 1998. Erupções Pustulosas. [Google Scholar]
- 15. [Last accessed on 2017 May 25]. Available from: https://www.signin.who-umc.org/core/login?signin=87a15c1e006f1cd14fd20b95c6524852 .
- 16. [Last accessed on 2017 May 29]. Available from: http://www.medicines.org.uk/emc/search .
- 17. [Last accessed on 2017 May 29]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2017/206939Orig1s000lbl.pdf .
- 18.Drug Safety Alerts of Pharmacovigilance Programme of India. [Last accessed on 2017 Aug 23]. Available from: http://www.ipc.nic.in/index2.asp?slid=541&sublinkid=449&lang=1&EncHid=
- 19.Thota P, Thota A, Medhi B, Sidhu S, Kumar P, Selvan VK, et al. Drug safety alerts of pharmacovigilance programme of India: A scope for targeted spontaneous reporting in India. Perspect Clin Res. 2018;9:51–5. doi: 10.4103/picr.PICR_29_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Cefixime- Risk of acute generalized exanthematous pustulosis, India. [Last accessed on 2016 Nov 23];Pharm News Lett. 2016 5:7. Available from: http://www.who.int/medicines/publications/PharmaNewsletter5_16.pdf . [Google Scholar]
- 21.Central Drugs Standard Control Organisation. [Last accessed on 2016 Dec 23]. Available from: http://www.cdsco.nic.in/forms/Default.aspx .


