Removal of a circumferential shell of casting material (plaster of Paris or synthetic) is an important skill for physicians who might expect to see patients for routine follow-up or more emergently. It is the first step in assessment and management of possible compartment syndrome with the cast in situ and it is an essential skill in the emergency room and urgent care setting.
Although a straightforward piece of equipment, cast saws can be dangerous in unprepared hands. In February 2017, Canadian national media reported on 2 children injured during the simple procedure of removing a cast.1,2
Injuries occur owing to direct trauma and to thermal injury to underlying skin. The risk of the latter increases when long duration cuts are attempted without allowing the blades to cool, with recently applied casts that have not completely cured, or with wet casts that are still soft and sticky, creating more friction.
Indications
The following are examples of cases in which skills with a cast saw will be needed:
removal of a cast for reassessment;
splitting open a tight cast;
removal of a wet cast or where history suggests a foreign body underneath;
removal of a cast to exclude underlying infection in the context of sepsis;
splitting of a cast for airline travel (often mandated by airlines before boarding);
splitting or removal of a cast for suspected compartment syndrome; and
removal or trimming of a cast that has been applied incorrectly.
Steps for removal
Follow the steps outlined in Figures 1 to 6.3 The patient should be sitting or, preferably, lying (for leg casts and because in rare cases the patient can experience vasovagal syncope) in a position that allows the operator to use the saw with full control.
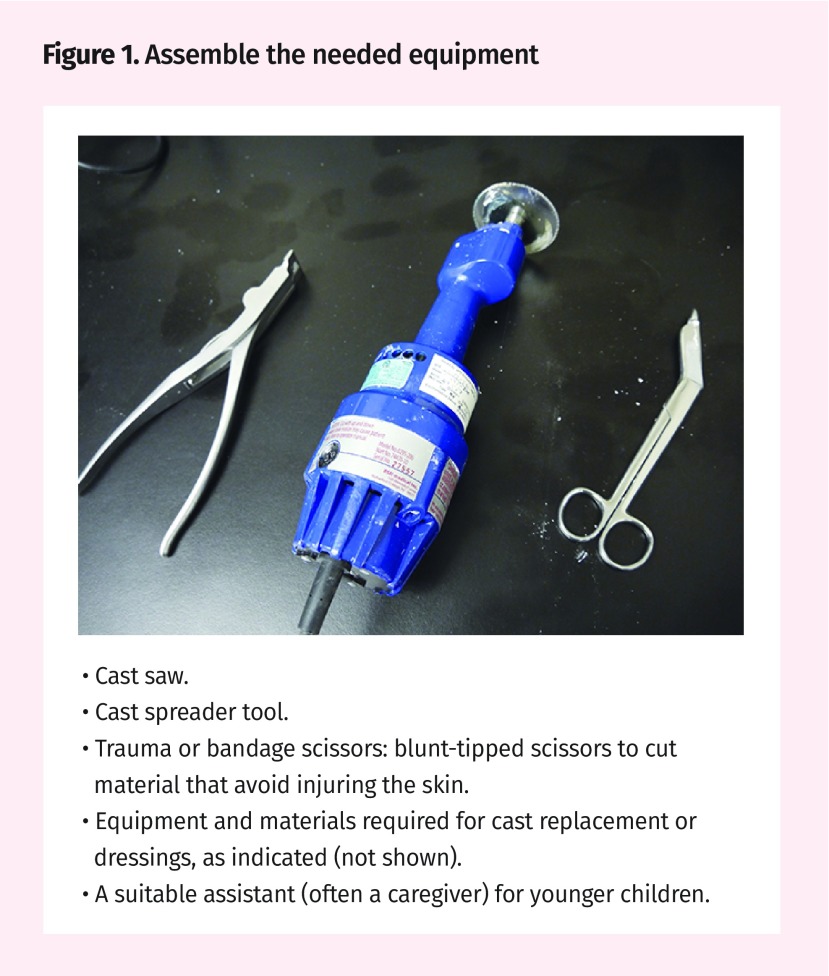
Figure 1.
- Cast saw.
- Cast spreader tool.
- Trauma or bandage scissors: blunt-tipped scissors to cut material that avoid injuring the skin.
- Equipment and materials required for cast replacement or dressings, as indicated (not shown).
- A suitable assistant (often a caregiver) for younger children.
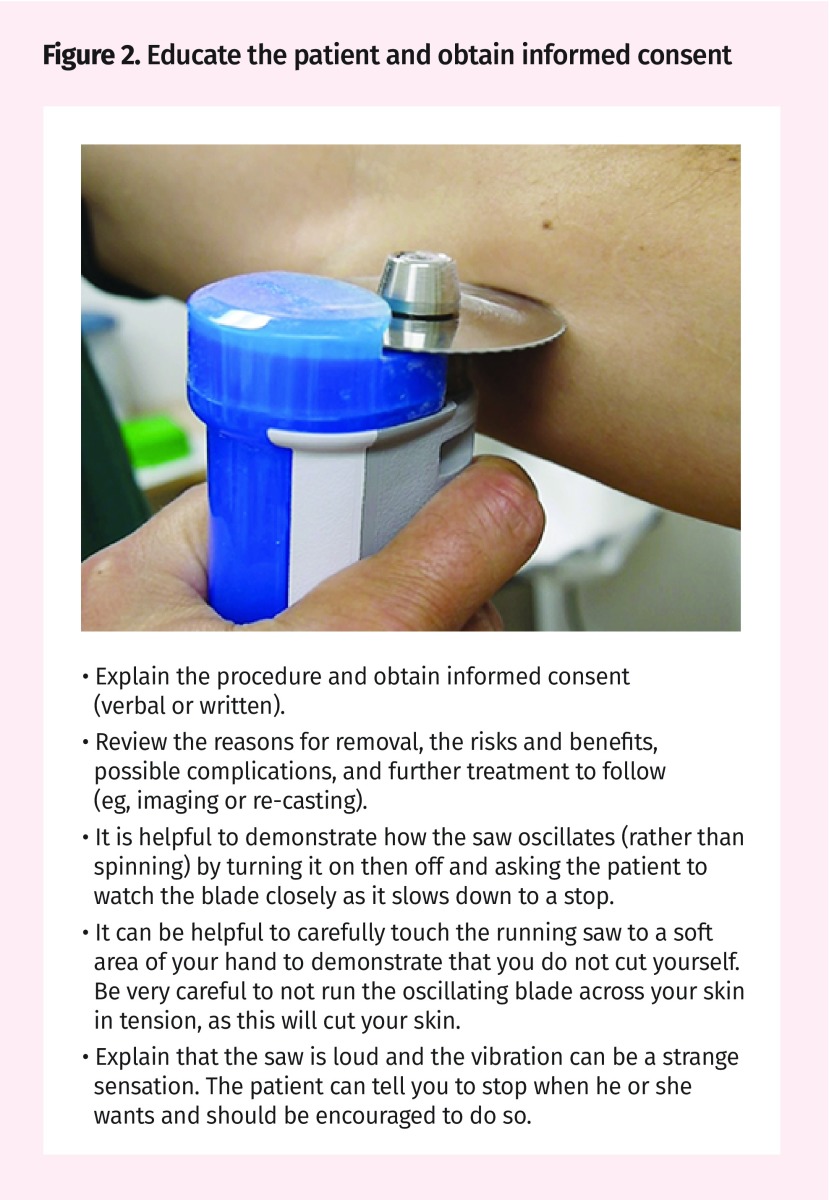
Figure 2.
- Explain the procedure and obtain informed consent (verbal or written).
- Review the reasons for removal, the risks and benefits, possible complications, and further treatment to follow (eg, imaging or re-casting).
- It is helpful to demonstrate how the saw oscillates (rather than spinning) by turning it on then off and asking the patient to watch the blade closely as it slows down to a stop.
- It can be helpful to carefully touch the running saw to a soft area of your hand to demonstrate that you do not cut yourself. Be very careful to not run the oscillating blade across your skin in tension, as this will cut your skin.
- Explain that the saw is loud and the vibration can be a strange sensation. The patient can tell you to stop when he or she wants and should be encouraged to do so.
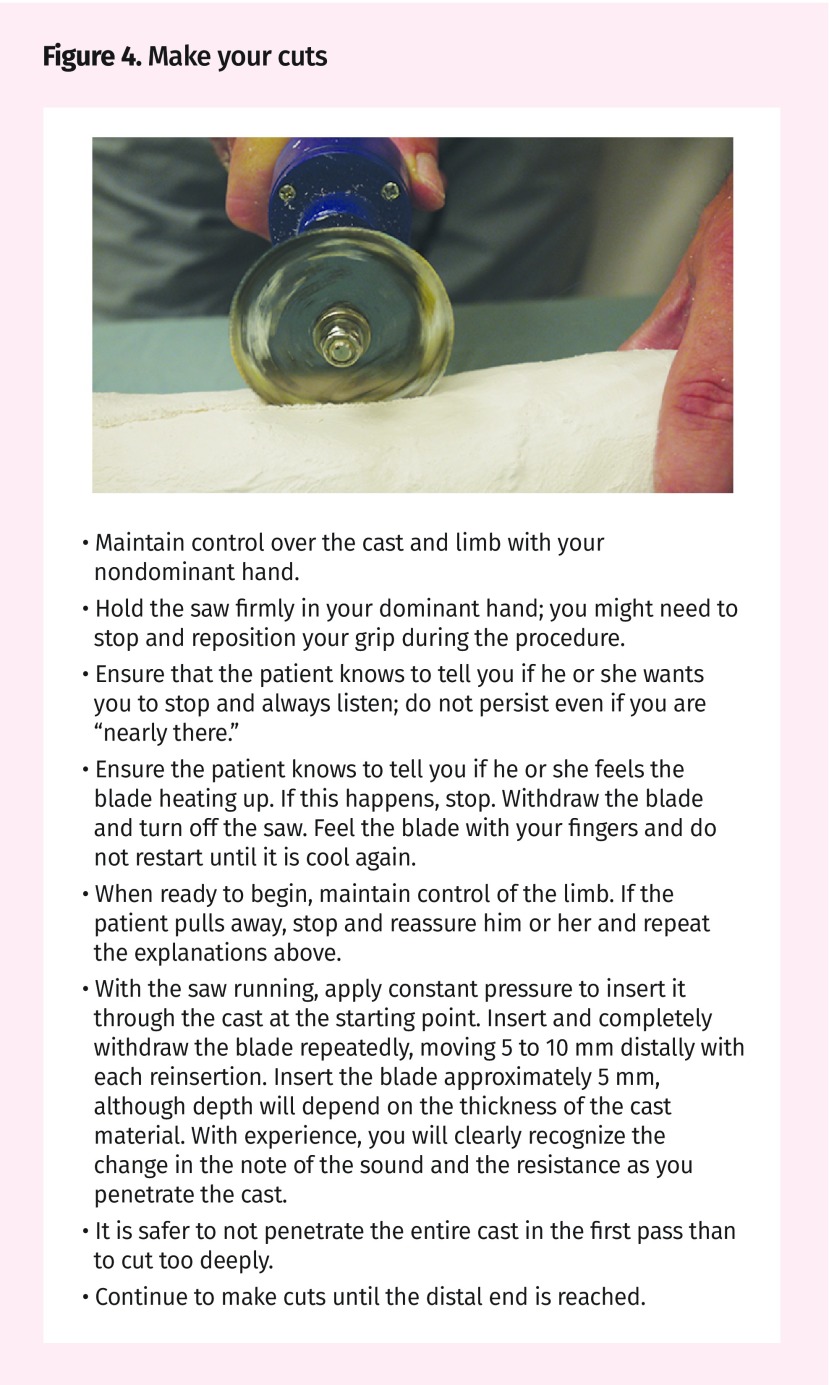
Figure 4.
- Maintain control over the cast and limb with your nondominant hand.
- Hold the saw firmly in your dominant hand; you might need to stop and reposition your grip during the procedure.
- Ensure that the patient knows to tell you if he or she wants you to stop and always listen; do not persist even if you are “nearly there.”
- Ensure the patient knows to tell you if he or she feels the blade heating up. If this happens, stop. Withdraw the blade and turn off the saw. Feel the blade with your fingers and do not restart until it is cool again.
- When ready to begin, maintain control of the limb. If the patient pulls away, stop and reassure him or her and repeat the explanations above.
- With the saw running, apply constant pressure to insert it through the cast at the starting point. Insert and completely withdraw the blade repeatedly, moving 5 to 10 mm distally with each reinsertion. Insert the blade approximately 5 mm, although depth will depend on the thickness of the cast material. With experience, you will clearly recognize the change in the note of the sound and the resistance as you penetrate the cast.
- It is safer to not penetrate the entire cast in the first pass than to cut too deeply.
- Continue to make cuts until the distal end is reached.
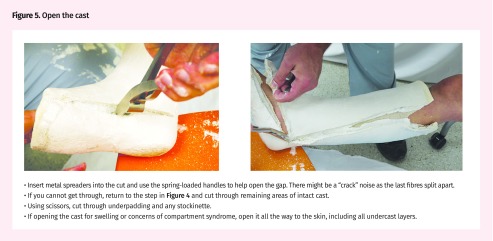
Figure 5.
- Insert metal spreaders into the cut and use the spring-loaded handles to help open the gap. There might be a “crack” noise as the last fibres split apart.
- If you cannot get through, return to the step in Figure 4 and cut through remaining areas of intact cast.
- Using scissors, cut through underpadding and any stockinette.
- If opening the cast for swelling or concerns of compartment syndrome, open it all the way to the skin, including all undercast layers.
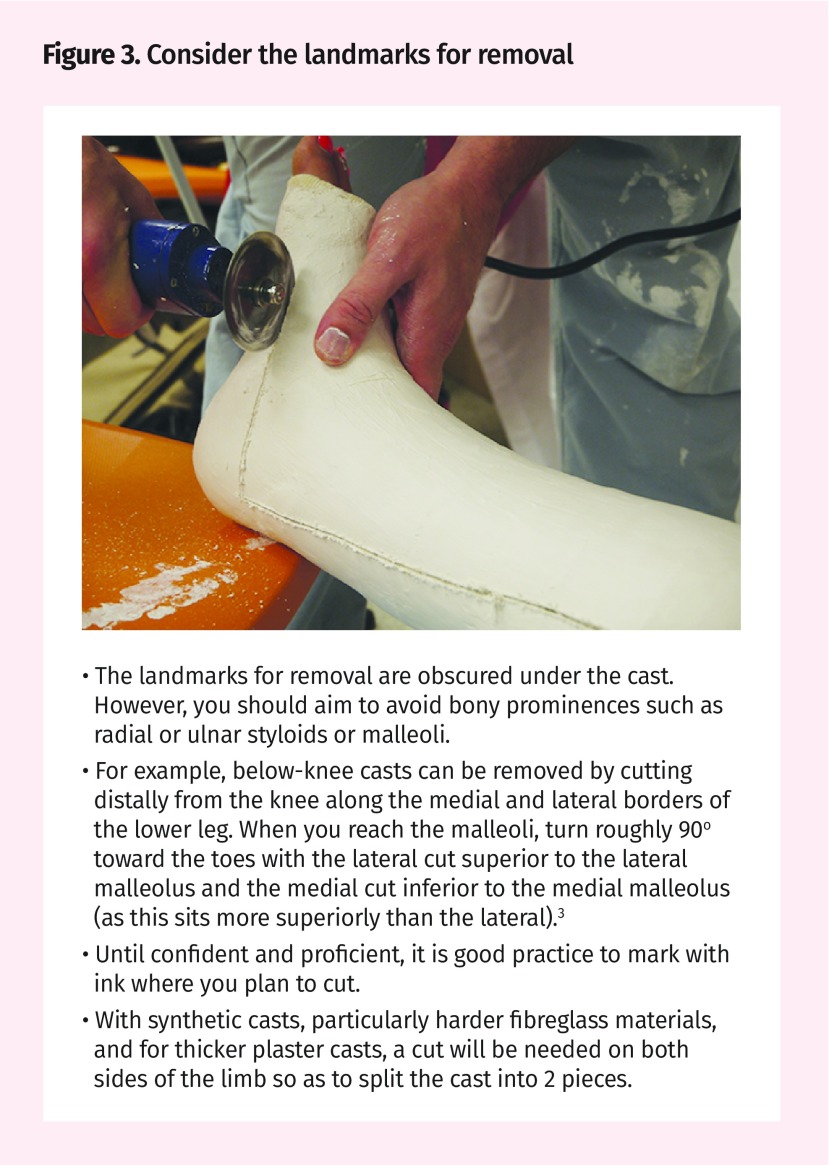
Figure 6.
- Carefully slide the cast out from the limb (not the other way around).
- Be wary of any operative fixation undertaken, as percutaneous Kirschner wires might get caught on cast material and could become displaced.
- Place the limb on a pillow to rest while completing your assessment.
Notable points
The following are some important considerations:
Take your time to prepare your patient and stop when he or she asks. It is much quicker and safer to remove a cast with the patient cooperating and at ease.
If the cast removal is because of concerns about compartment syndrome and clinical improvement is not swift, urgent orthopedic consultation is indicated.
Potential complications
We caution readers to be extremely careful when removing casts if they are uncertain about the undercast padding and skin protection in place. Casts with merely thin paper between skin and cast have been seen in travelers returning from countries with less well developed health care. Even with extreme care, skin can be damaged in these circumstances, and patients should be counseled about this possibility before commencing.
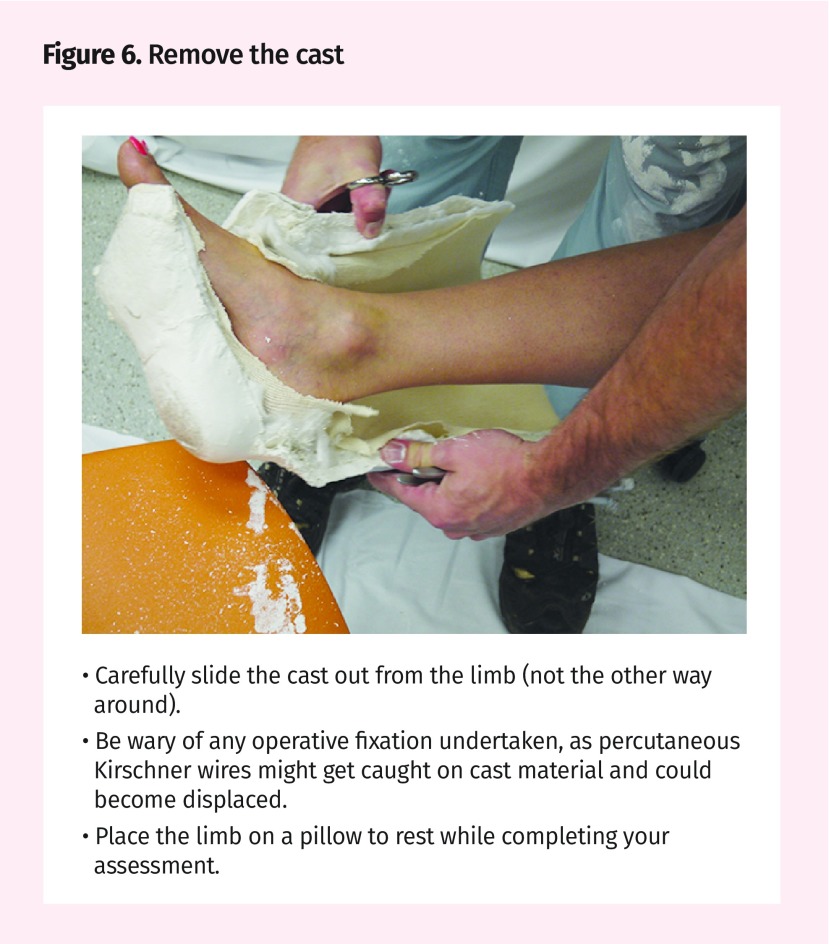
Figure 3.
- The landmarks for removal are obscured under the cast. However, you should aim to avoid bony prominences such as radial or ulnar styloids or malleoli.
- For example, below-knee casts can be removed by cutting distally from the knee along the medial and lateral borders of the lower leg. When you reach the malleoli, turn roughly 90° toward the toes with the lateral cut superior to the lateral malleolus and the medial cut inferior to the medial malleolus (as this sits more superiorly than the lateral).3
- Until confident and proficient, it is good practice to mark with ink where you plan to cut.
- With synthetic casts, particularly harder fibreglass materials, and for thicker plaster casts, a cut will be needed on both sides of the limb so as to split the cast into 2 pieces.
We encourage readers to share some of their practice experience: the neat little tricks that solve difficult clinical situations. Praxis articles can be submitted online at http://mc.manuscriptcentral.com/cfp or through the CFP website (www.cfp.ca) under “Authors and Reviewers.”
Footnotes
Competing interests
None declared
References
- 1.Brohman E. Manitoba toddler’s arm burned during cast removal, mom says. CBC News. 2017. Feb 21, Available from: www.cbc.ca/news/canada/manitoba/lana-roulette-arm-cast-toddler-burns-1.3991572. Accessed 2017 Dec 15.
- 2.Bridges A. Sask. mom speaks out after boy, 12, severely burned having cast removed. CBC News. 2017 Feb 21; Available from: www.cbc.ca/news/canada/saskatoon/boy-burns-cast-removal-warman-sask-1.3993314. Accessed 2017 Dec 15. [Google Scholar]
- 3.Court-Brown CM. Fractures of the tibia and fibula. In: Rockwood CA, Green DP, Buchholz RW, editors. Rockwood and Green’s fractures in adults. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. pp. 2079–146. [Google Scholar]