Abstract
Objective
To identify the most commonly presenting conditions in primary care globally, and to compare common reasons for visits (RFVs) as reported by clinicians and patients, as well as among countries of different economic classifications.
Data sources
Twelve scientific databases were searched up to January 2016, and a dual independent review was performed to select primary care studies.
Study selection
Studies were included if they contained 20 000 visits or more (or equivalent volume by patient-clinician interactions) and listed 10 or more RFVs. Dual independent data extraction of study characteristics and RFV rankings was performed. Data analysis was descriptive, with pooled rankings of RFVs across studies.
Synthesis
Eighteen studies met inclusion criteria (median 250 000 patients or 83 161 visits). Data were from 12 countries across 5 continents. The 10 most common clinician-reported RFVs were upper respiratory tract infection, hypertension, routine health maintenance, arthritis, diabetes, depression or anxiety, pneumonia, acute otitis media, back pain, and dermatitis. The 10 most common patient-reported RFVs were symptomatic conditions including cough, back pain, abdominal symptoms, pharyngitis, dermatitis, fever, headache, leg symptoms, unspecified respiratory concerns, and fatigue. Globally, upper respiratory tract infection and hypertension were the most common clinician-reported RFVs. In developed countries the next most common RFVs were depression or anxiety and back pain, and in developing countries they were pneumonia and tuberculosis. There was a paucity of available data, particularly from developing countries.
Conclusion
There are differences between clinician-reported and patient-reported RFVs to primary care, as well as between developed and developing countries. The results of our review are useful for the development of primary care guidelines, the allocation of resources, and the design of training programs and curricula.
Résumé
Objectif
Déterminer l’ensemble des raisons de consulter (RDC) les plus fréquentes dans les cliniques de soins primaires et comparer celles que mentionnent les médecins et les patients ainsi que celles qu’on rencontre dans des pays de différentes classifications économiques.
Source des données
On a consulté 12 bases de données scientifiques jusqu’en janvier 2016, pour ensuite effectuer une revue indépendante double afin de retenir les études qui portaient sur les soins primaires.
Choix des études
Pour être retenues, les études devaient contenir au moins 20 000 visites (ou un nombre équivalent d’interactions patient-médecin) et mentionner au moins les 10 RDC les plus fréquentes. On a effectué une extraction indépendante double des données sur les caractéristiques des études et sur le classement des RDC les plus fréquentes. L’analyse des données était descriptive avec une mise en commun des classements des RDC les plus fréquentes dans les diverses études.
Synthèse
Dix-huit études (avec une médiane de 250 000 patients ou de 83 161 visites) respectaient les critères d’inclusion. Les données provenaient de 12 pays répartis sur 5 continents. Les RDC les plus fréquentes rapportées par les médecins étaient les infections des voies respiratoires supérieures, l’hypertension, les examens de santé périodiques, l’arthrite, le diabète, la dépression ou l’anxiété, la pneumonie, l’otite moyenne aigue, le mal de dos et les dermatites. Les RDC les plus fréquemment rapportées par les patients étaient des entités symptomatiques comme la toux, le mal de dos, des symptômes abdominaux, les pharyngites, les dermatites, la fièvre, les céphalées, les symptômes des membres inférieurs, des inconforts respiratoires mal définis et de la fatigue. Dans l’ensemble, les infections des voies respiratoires supérieures et l’hypertension étaient les RDC les plus fréquentes selon les médecins. Dans les pays développés, les RDC qui occupaient les prochains rangs étaient la dépression ou l’anxiété et le mal de dos, tandis que dans les pays en développement, c’était la pneumonie et la tuberculose. Il y avait très peu de données disponibles, en particulier dans les pays en voie de développement.
Conclusion
Il y a des différences entre ce que rapportent les médecins et les patients sur les raisons de consulter un service de soins primaires, mais aussi entre ce qu’on observe dans les pays développés et dans les pays en voie de développement. Les résultats de la présente revue devraient permettre l’élaboration de directives pour les soins primaires, l’allocation de ressources appropriées, et l’instauration de programmes de formation et de curricula spécifiques.
Primary care is an important point of access to health care systems.1–3 Primary care also provides care for the greatest variety of patients and complexity of illness.4 Primary care infrastructure is positively associated with better health outcomes5,6 and reduced health care costs.7 However, it has been estimated that a primary care clinician with an average practice would need 18 hours per day to provide guideline-based care for chronic disease and preventive care alone.8,9 Furthermore, the workload of primary care continues to increase.10 Given the considerable demands on primary care clinicians, it is essential to understand which conditions present most commonly in primary care settings. This information can assist with planning, allocating resources, determining research priorities, policy making, developing guidelines, and training of primary care professionals.11
While some studies present the most common reasons for visiting primary care in a particular country or region of a country,12,13 there is currently no systematic review of common conditions in primary care globally. Our primary objective was to systematically identify the reasons unreferred patients visit their primary care practitioners. Our secondary objective was to compare common reasons for visits (RFVs) as reported by clinicians and patients, as well as among countries of differing economic classifications.
METHODS
Data sources
This systematic review was performed and reported according to MOOSE (Meta-analysis Of Observational Studies in Epidemiology) guidelines,14 augmented by the more updated PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).15
In January 2016 a medical librarian (S.C.) searched databases using both controlled vocabulary (eg, MeSH terms and EMTREE subject headings) and text words describing the concepts of “primary health care” and “reasons for consulting.” Twelve databases were searched with no limits applied. A complete list of databases and details about the search strategy are available at CFPlus.* Google was searched on January 21, 2016, and the first 10 pages were reviewed. References were exported to RefWorks bibliographic management software. Reference lists of included studies were hand searched.
Study selection
Title or abstract screening and full-text review of articles was performed by 3 independent reviewers (D.S.C., C.R.F., and A.J.L.). Inclusion criteria were as follows: the study setting was general practice or primary care; the study reported a minimum of 10 RFVs; and the study’s population included a minimum 20 000 visits or 5 clinicians over a period of 1 year or more, or 7500 patients over a period of 1 year or more. The rationale for the minimum number of visits was based on a practice with 5 clinicians each seeing 20 patients per day, with 200 working days per year, which would result in 20 000 visits. Equivalencies were determined based on 1500-patient practice panels per physician, which among 5 physicians would result in 7500 patients. Studies were observational in design.
Studies were excluded if they focused on a specific type of visit or presentation (eg, periodic health examination visits), focused on specific conditions or problems (eg, acute conditions only), selected specific populations (eg, adolescents), indicated that visits resulted from referrals (eg, to pediatrics or internal medicine), or were published before 1996. When there were multiple publications using data from the same source or database, priority was given to the most recent data and to complete data sets with the most specific information. Multiple publications using the same source were only included if they analyzed the data differently (eg, subgroup analysis). Disagreement was resolved by consensus or third party review (G.M.A.). Attempts were made to contact authors of studies if additional data were required (eg, unpublished data). Google Translate was used for non-English articles.
Two reviewers extracted data independently (D.S.C., C.R.F.). The reported RFV was the primary outcome of interest. Reasons for visits were defined as the reasons patients presented to primary care or the problems managed by physicians. For each of the top RFVs (up to 20 per study), the number, percent, or rate of visits associated with each condition were recorded. Descriptive characteristics of each study were also collected, including whether the RFV was patient- or clinician-reported, the total number of visits, the number of clinicians or practices sampled, the location and duration of data collection, the percent of female patients, the percent of patients aged 65 and older, and the coding system used (eg, the International Classification of Primary Care, ICD-9, ICD-10).
To assess the risk of bias, 5 characteristics of each study were scored, with 0 indicating high risk of bias and 1 indicating low risk of bias. The characteristics were as follows: representative sample of clinicians (≥ 2 of the following 3: having both male and female clinicians; not limited to specific number of years in practice; and not limited to specific practice size); representative sample of patients (≥ 2 of the following 3: having both male and female patients; mixture of urban and rural settings; and not limited to specific age group); prospective (score = 1) or retrospective (score = 0) data collection; specified coding system (yes = 1, no = 0); and duration of data collection (≥ 1 year = 1, < 1 year = 0). Discrepancies were resolved by consensus or third party review (G.M.A.).
Data were separated into “general” and “specific” reported RFVs. General categories were broad descriptive groupings (eg, respiratory), while specific categories were more exact diagnoses (eg, pneumonia). Within each category (general or specific), a standardized coding scheme was applied. For example, using our coding scheme for specific RFVs, “back complaint,” “dorsopathies,” “back symptoms,” “dorsalgia,” “low back symptoms,” and “neck pain” were all coded as “back pain/spinal pain.” Diagnostic coding legends for the general and specific conditions are available at CFPlus.*
To analyze and pool the most common visits, RFVs from each study were ranked from most to least common. The reporting of frequency of visits for particular RFVs was inconsistent between studies (variably using number of visits, percent of visits, rate of visits, and others). Thus, the rank of each reported RFV was used as our measure of relative frequency. Using the top 20 ranked RFVs in each study, the first most common condition in each study was assigned the number 20, the second was 19, and so on. Therefore, an RFV not in the top 20 in a particular study would be assigned a zero ranking. Rankings were then combined and mean ranks were determined for each RFV. The most commonly seen RFVs were those with the highest mean rank. An RFV was excluded from combining if it was present in only 1 study.
To analyze the secondary outcome, countries were categorized by economic classification as either developed or developing, using the United Nations classification system,16 and the mean ranks of clinician-reported RFVs were compared. Also, when subgroup analyses from included studies were available (eg, clinician or patient sex, practice setting), data from each study were combined using the same approach (for subgroups with ≥ 2 studies).
SYNTHESIS
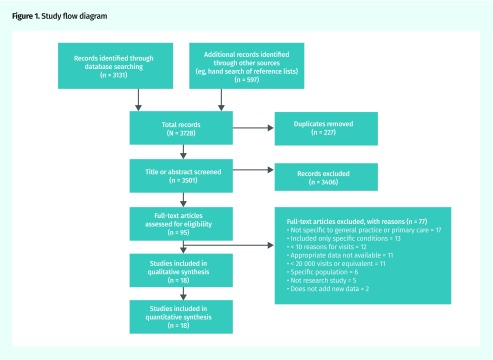
We identified 18 studies (Table 1)11–13,17–31 for inclusion from a total of 3501 original articles retrieved in our search (Figure 1). (National Center for Health Statistics data were also reported by the Centers for Disease Control and Prevention [Akintunde Akinseye, personal communication, April 2017].) Agreement was 99% for study selection and 95% for data extraction.
Table 1.
Study characteristics
| STUDY | OA OR SG DATA | YEARS OF DATA COLLECTION | SAMPLING DURATION, WK | COUNTRY | TOTAL PATIENT POPULATION SERVED | TOTAL NO. OF VISITS INCLUDED | GENERAL OR SPECIFIC CODING CATEGORY | PATIENT REPORTED OR CLINICIAN REPORTED | QUALITY SCORE* (OUT OF 5) |
|---|---|---|---|---|---|---|---|---|---|
| Binns et al,11 2007 | OA | 2002 | 32 (continuous) | USA | NA | 597 176 | General and specific | Clinician | 4 |
| Britt et al,17 1996 | SG (physician sex) | 1990–1991 | 2 (per physician, over a 12-mo period) | Australia | NA | 113 468 | General† | Patient and clinician | 5 |
| Britt et al,12 2015 | OA | 2014–2015 | NA (up to 100 encounters) | Australia | NA | 98 728 | Specific | Patient and clinician | 5 |
| Brueton et al,18 2010 | OA (SG: practice setting) | 2001–2002 | 26 | South Africa | 250 000 | 4383 | General and specific | Patient and clinician | 3 |
| Fleming et al,19 2005 | OA (SG: patient sex) | 2001 | 52 (continuous) | England, Wales | 325 850 | NA | Specific | Clinician | 3 |
| Harrison et al,20 2011 | SG (physician sex) | 2009–2010 | NA (up to 100 encounters) | Australia | NA | 101 349 | General† | Patient and clinician | 5 |
| Mash et al,21 2012 | OA (SG: patient age) | 2010 | 1 (5 d over a 1-y period) | South Africa | 2 780 270 | 18 856 | General and specific | Patient and clinician | 4 |
| Ministry of Health,22 2004 | OA (SG: practice type reimbursement, season) | 2001–2002 | 2 (per physician, over an 18-mo period) | NZ | NA | 8258 | General | Clinician | 5 |
| Mohan and Nagavi,23 2003 | OA | 2000 | 52 (continuous) | India | NA | NA | Specific | Clinician | 1 |
| Murphy et al,24 2015 | OA (SG: patient sex, public vs private payment methods) | 2008–2010 | NA (up to 100 encounters) | Ireland | 503 823 | 16 899 | General | Patient | 3 |
| National Center for Health Statistics,25 2017 | OA | 2014 | 52 (1 wk per physician) | USA | NA | 6386 | Specific | Clinician | 5 |
| Pace et al,26 2004 | OA (SG: season) | 1995–1998 | 208 (continuous) | USA | NA | 13 149 | Specific† | Clinician | 5 |
| Pearson et al,27 1996 | SG (patient sex) | 1994–1995 | 52 (continuous) | England | 65 000 | 4685 | General† | Clinician | 5 |
| Probst et al,28 2002 | SG (urban or rural) | 1996–1997 | 104 (continuous) | USA | NA | 19 409 | Specific† | Patient | 5 |
| Salvi et al,29 2015 | OA (SG: practice setting) | 2011 | 1 d | India | NA | 204 912 | Specific | Clinician | 2 |
| Sayer and Britt,30 1996 | SG (patient sex) OA | 1990–1991 | 2 (per physician, over a 12-mo period) | Australia | NA | 96 144 | General | Patient and clinician | 5 |
| Soler et al,31 2012 | OA | 1995–2005 (Neth), 2001–2005 (Malta), and 2003 (Serbia) | 132 (Neth), 60 (Malta), and 12 (Serbia) (all continuous) | Neth, Malta, and Serbia | 15 318 (Neth), 9896 (Malta), 72 673 (Serbia) | 838 896 (Neth), 70 177 (Malta), 207 323 (Serbia) | Specific | Patient | 4 |
| Wändell et al,13 2013 | OA | 2009–2011 | 104 (continuous) | Sweden | 1 987 827 | 3 810 843 | Specific | Clinician | 4 |
NA—not available, Neth—the Netherlands, NZ—New Zealand, OA—overall, SG—subgroup, USA—United States of America.
Higher scores represent higher quality.
These studies could not be included in the general or specific analysis.
Figure 1.
Study flow diagram
Included articles represented 12 countries: Australia, England and Wales, India, Ireland, Malta, the Netherlands, New Zealand, Serbia, South Africa, Sweden, and the United States. Seven studies provided the size of the included population, ranging from 9896 to 2 780 270 (median was 250 000). Sixteen studies provided the total number of included visits, ranging from 4383 to 3 810 843 (median was 83 161) (Table 1).11–13,17–31 Overall, the risk of bias was low, with 72% (13 of 18) of articles scoring at least 4 out of 5 on our assessment. Further details regarding the characteristics and quality assessment of included studies are available at CFPlus.*
Of the 18 included studies, 6 reported general categories of RFVs.11,18,21,22,24,30 Three of these studies11,18,21 also reported specific RFVs, as did an additional 7 studies.12,13,19,23,25,29,31 The remaining 5 studies17,20,26–28 could not be included in either the general or specific analysis but were kept in the review, as they provided additional subgroups for analysis.
Six studies were analyzed for general categories of RFVs in primary care.11,18,21,22,24,30 The most common categories of RFVs in descending order were respiratory, nervous system or sense organs, cardiovascular or circulatory, skin or subcutaneous, and musculoskeletal conditions. The proportion of RFVs and problems managed are further described at CFPlus.* Each of these categories was included in the top 20 reported RFVs in all 6 included studies, providing high consistency with the ranking.
Fourteen RFV lists from 10 studies were analyzed for specific RFVs to primary care.11–13,18,19,21,23,25,29,31 Nine RFV lists were “clinician-reported” and 5 were “patient-reported.” Two studies reported data from both clinicians and patients.12,21 One study provided data from 3 countries, which were analyzed as distinct sets of data.31 Table 211–13,18,19,21,23,25,29,31 provides the most common clinician-reported and patient-reported RFVs. None of the most common clinician-reported RFVs was found in all 9 included studies, but the top 2 (upper respiratory tract infection [URTI] and hypertension [HTN]) were found in 8 studies. Of the top 18 patient-reported RFVs, 10 appeared in all 5 data sets.
Further analysis of clinician-reported RFVs according to country classification showed specific differences (Table 3).11–13,18,19,21,23,25,29 Five studies with information on clinician-reported RFVs were classified as developed countries (Australia, England and Wales, Sweden, and the United States),11–13,19,25 and 4 studies were classified as developing (India and South Africa).18,21,23,29 For both developed and developing countries, the top 2 most common reported RFVs were URTI and HTN, consistent with the overall rankings. In developed countries, the third and fourth most common RFVs were depression or anxiety and back pain, neither of which appeared in the developing countries list. In developing countries, the third and fourth most common RFVs were pneumonia and tuberculosis, neither of which appeared in the developed countries list.
Table 3.
Ranking of RFVs presenting to primary care among developed and developing countries
| RANK | DEVELOPED COUNTRIES* | DEVELOPING COUNTRIES † | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| CONDITION | RANK SCORE‡ (MAXIMUM SCORE OF 20) | NO. OF ANALYSES THAT INCLUDED THE CONDITION (OUT OF 5) | CONDITION | RANK SCORE‡ (MAXIMUM SCORE OF 20) | NO. OF ANALYSES THAT INCLUDED THE CONDITION (OUT OF 4) | |
| 1 | Hypertension | 17.4 | 5 | Upper respiratory tract infection, unspecified | 18.5 | 4 |
| 2 | Upper respiratory tract infection, unspecified | 15.2 | 4 | Hypertension | 14.5 | 3 |
| 3 | Depression or anxiety | 12.0 | 5 | Pneumonia | 11.5 | 4 |
| 4 | Back pain | 12.0 | 4 | Tuberculosis | 10.0 | 3 |
| 5 | Routine health maintenance | 11.6 | 3 | Parasites | 9.0 | 2 |
| 6 | Arthritis (not back) | 10.0 | 4 | Anemia | 8.3 | 2 |
| 7 | Dermatitis | 8.6 | 4 | Diabetes | 8.3 | 2 |
| 8 | Acute otitis media | 8.6 | 4 | Arthritis (not back) | 6.5 | 2 |
| 9 | Diabetes | 8.6 | 3 | Bronchitis or bronchiolitis | 6.3 | 2 |
| 10 | Cough | 7.0 | 2 | Epilepsy | 6.0 | 2 |
| 11 | Medication | 5.8 | 2 | Urinary tract infection | 5.5 | 2 |
| 12 | Urinary tract infection | 5.4 | 3 | Tonsillitis | 5.5 | 2 |
RFV—reason for visit.
Studies in this analysis included the following: Binns et al,11 2007; Britt et al,12 2015; Fleming et al,19 2005; National Center for Health Statistics,25 2017; and Wändell et al,13 2013.
Studies in this analysis included the following: Brueton et al,18 2010; Mash et al,21 2012; Mohan and Nagavi,23 2003; and Salvi et al,29 2015.
Higher scores mean the condition was reported as a more common RFV in more studies.
Subgroup analyses were provided in 9 studies.17,20,22,24,26–30 Subgroups included seasonality,22,26 physician17,20 and patient sex,19,24,27,30 urban versus rural setting,28 methods of reimbursement or payment,22,24 and practice setting18,29 (Table 1).11–13,17–31 The information on methods of reimbursement or payment and practice settings was frequently not well described and inconsistent among studies and, therefore, was not pooled or included. Summaries of the remaining subgroup data are available at CFPlus.*
DISCUSSION
This review includes primary care visit data from 18 studies with a median of 250 000 patients or 83 161 visits per study. Twelve countries provided data from 5 of 6 populated continents. Data on specific RFVs were robust and provided a number of important results.
The 10 most common clinician-reported RFVs encapsulate the breadth of medical management provided by primary care, including acute, chronic, and preventive care. Policy makers and administrators must balance increasing demand for primary care services with finite resources. For example, while routine health maintenance examinations are the third most common clinician-reported RFV, there is considerable debate as to the merit of these appointments.32 Researchers and guideline developers can be reminded of priorities in primary care. For example, common RFVs should be reflected in guideline recommendations and associated opportunity costs within primary care. Additionally, training and evaluating clinicians on their clinical abilities should reflect the relative frequency of conditions that they will see in practice. For example, many primary care clinicians report feeling unprepared to manage mental health problems,33 yet depression or anxiety is the sixth most common clinician-reported RFV.
The 10 most common patient-reported RFVs were dominated by symptomatic conditions with no preventive care or management of asymptomatic chronic conditions. This intuitively makes sense as patients seek help for symptoms, but it might also suggest a difference in clinician and patient care priorities. Regardless, the differences remind us that interpretation of RFV data requires examination of both clinician- and patient-reported data.
When comparing clinician-reported RFVs in developed and developing countries, URTI and HTN are consistently the 2 most common RFVs. However, some highly ranking RFVs in developed countries were absent from developing countries, and vice versa. Notably, depression or anxiety and back pain ranked as third and fourth in developed countries but did not appear in developing countries. This might be owing to a paucity of data from developing countries and thus not reflect reality. Alternatively, clinician-reported RFVs might not reflect the prevalence of conditions if patients do not present for depression or anxiety and back pain, or if clinicians under-reported or recorded these conditions differently. Thus, depression or anxiety and back pain might be more common in developing countries than identified. The World Health Organization estimates that more than 75% of people with mental illness are untreated in developing countries.34 Furthermore, certain cultures are more likely to report somatic symptoms than emotional symptoms, affecting how mental illness presents and is diagnosed by clinicians.35 Back pain is also likely underrepresented in these studies, as 1-month prevalence estimates of back pain in South Africa and India are 39%.36 Additionally, several infectious conditions such as pneumonia, tuberculosis, parasites, and HIV are considerably more prevalent in primary care in developing nations, which was reflected in our results.
Limitations
The use of different coding systems (ie, the International Classification of Primary Care, ICD-9, ICD-10, and the Read codes) by each study presented challenges for combining data while retaining adequate detail. Also, studies recorded data with varying levels of specificity, which limited the number of data sets that could be combined. The biggest limit to our study was the paucity of published literature meeting our inclusion criteria; there were notable omissions from Canada, Europe, and South America, and only 2 developing countries provided data.
Conclusion
While examining large-scale studies encompassing 12 countries on 5 continents, we found that globally primary care clinicians manage a range of clinical presentations. Despite a high degree of consistency in the 10 most common RFVs to primary care, we identified important differences in RFVs reported by clinicians or patients. Differences might also exist between developed and developing countries. Our findings demonstrate the need for more large-scale primary care studies and serve as a call for primary care researchers around the globe to investigate common conditions in their regions.
Table 2.
Ranking of RFVs to primary care as reported by clinicians and patients
| RANK | CLINICIAN REPORTED* | PATIENT REPORTED† | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| CONDITION | RANK SCORE‡ (MAXIMUM SCORE WAS 20) | NO. OF ANALYSES THAT INCLUDED THE CONDITION (OUT OF 9) | CONDITION | RANK SCORE‡ (MAXIMUM SCORE WAS 20) | NO. OF ANALYSES THAT INCLUDED THE CONDITION (OUT OF 5) | |
| 1 | Upper respiratory tract infection, unspecified | 16.7 | 8 | Cough | 19.0 | 5 |
| 2 | Hypertension | 16.1 | 8 | Back pain or spinal pain | 16.8 | 5 |
| 3 | Routine health maintenance | 8.7 | 4 | Abdominal, unspecified | 16.6 | 5 |
| 4 | Arthritis (not back) | 8.6 | 6 | Pharyngitis | 14.4 | 5 |
| 5 | Diabetes | 8.4 | 5 | Dermatitis | 13.4 | 5 |
| 6 | Depression or anxiety | 7.7 | 6 | Fever | 12.6 | 5 |
| 7 | Pneumonia | 7.2 | 6 | Headache | 12.4 | 5 |
| 8 | Acute otitis media | 6.8 | 6 | Leg symptoms | 9.4 | 5 |
| 9 | Back pain or spinal pain | 6.7 | 4 | Respiratory, unspecified | 8.8 | 4 |
| 10 | Dermatitis | 6.4 | 5 | Fatigue | 8.4 | 5 |
| 11 | Cough | 5.6 | 3 | Depression or anxiety | 8.0 | 4 |
| 12 | Urinary tract infection | 5.4 | 5 | Arthritis (not back) | 6.8 | 5 |
| 13 | Tuberculosis | 4.4 | 3 | Sinusitis | 6.2 | 3 |
| 14 | Dyspepsia | 4.3 | 4 | Cardiovascular | 6.0 | 4 |
| 15 | Tonsillitis | 4.2 | 3 | Acute otitis media | 5.8 | 4 |
| 16 | Parasites | 4.0 | 2 | Urinary tract infection | 5.4 | 4 |
| 17 | Asthma | 4.0 | 4 | Vertigo or dizziness | 5.4 | 4 |
| 18 | Abdominal, unspecified | 4.0 | 5 | Skin, unspecified | 4.8 | 4 |
RFV—reason for visit.
Studies in this analysis included the following: Binns et al,11 2007; Britt et al,12 2015; Brueton et al,18 2010; Fleming et al,19 2005; Mash et al,21 2012; Mohan and Nagavi,23 2003; National Center for Health Statistics,25 2017; Salvi et al,29 2015; and Wändell et al,13 2013.
Studies in this analysis included the following: Britt et al,12 2015; Mash et al,21 2012; and Soler et al,31 2012 (which had 3 data sets).
Higher scores mean the condition was reported as a more common RFV in more studies.
Editor’s key points
▸ This systematic review of several large-scale studies from 12 countries found that the most common clinician-reported reasons for visits (RFVs) (eg, upper respiratory tract infection, hypertension) encapsulate the breadth of medical management provided by primary care, including acute, chronic, and preventive care. Clinicians’ training should reflect the relative frequency of conditions that they will see in practice; for example, depression or anxiety was the sixth most common clinician-reported RFV, so clinicians should be trained to manage mental health problems.
▸ The most common patient-reported RFVs (eg, cough, back pain, abdominal symptoms) were dominated by symptomatic conditions.
▸ Developed and developing countries shared the 2 most common RFVs: upper respiratory tract infection and hypertension. In developed countries, the third and fourth most common RFVs were depression or anxiety and back pain, neither of which appeared in the developing countries list. In developing countries, the third and fourth most common RFVs were pneumonia and tuberculosis, neither of which appeared in the developed countries list.
Points de repère du rédacteur
▸ Cette revue systématique de plusieurs grandes études provenant de 12 pays a trouvé que les raisons de consulter (RDC) les plus fréquentes (p. ex. les infections des voies respiratoires supérieures et l’hypertension) étaient à l’origine de la plupart des traitements médicaux dispensés dans les institutions de soins primaires, y compris les soins aigus, chroniques et préventifs. La formation des médecins devrait donc tenir compte de la fréquence relative des problèmes de santé auxquels ils auront à faire face; par exemple, la dépression et l’anxiété étaient les sixièmes RDC rapportées par les médecins, si bien qu’ils devraient être formés pour traiter les problèmes de santé mentale.
▸ Les RDC les plus fréquemment rapportées par les patients (c.-à-d. la toux, le mal de dos et les douleurs abdominales) étaient essentiellement des conditions symptomatiques.
▸ Les pays développés et les pays en voie de développement avaient les mêmes RDC les plus fréquentes, soit les infections des voies respiratoires supérieures et l’hypertension. Toutefois, dans les pays développés, les troisièmes et quatrièmes choix étaient la dépression ou l’anxiété et le mal de dos, alors que ces problèmes n’étaient pas mentionnés dans les pays en développement. Dans les pays développés, les troisièmes et quatrièmes RDC étaient les pneumonies et la tuberculose, des problèmes de santé non inscrits sur la liste des pays en voie de développement.
Footnotes
The search strategy, the diagnostic coding legends for general and specific conditions, the characteristics and quality assessment of included studies, the proportion of reasons for visits and problems managed, and summaries of the subgroup data are available at www.cfp.ca. Go to the full text of the article online and click on the CFPlus tab.
Contributors
All authors made substantial contributions to the design of the study, conducting the study, and writing and editing the manuscript.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Green LA, Fryer GE, Jr, Yawn BP, Lanier D, Dovey SM. The ecology of medical care revisited. N Engl J Med. 2001;344(26):2021–5. doi: 10.1056/NEJM200106283442611. [DOI] [PubMed] [Google Scholar]
- 2.Stewart M, Ryan B. Ecology of health care in Canada. Can Fam Physician. 2015;61:449–53. [PMC free article] [PubMed] [Google Scholar]
- 3.Roland M, Guthrie B, Thomé DC. Primary medical care in the United Kingdom. J Am Board Fam Med. 2012;25(Suppl 1):S6–11. doi: 10.3122/jabfm.2012.02.110200. [DOI] [PubMed] [Google Scholar]
- 4.Starfield B, Lemke KW, Bernhardt T, Foldes SS, Forrest CB, Weiner JP. Comorbidity: implications for the importance of primary care in ‘case’ management. Ann Fam Med. 2003;1(1):8–14. doi: 10.1370/afm.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang CH, Stukel TA, Flood AB, Goodman DC. Primary care physician workforce and Medicare beneficiaries’ health outcomes. JAMA. 2011;305(20):2096–104. doi: 10.1001/jama.2011.665. Erratum in: JAMA 2011;306(2):162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi L, Macinko J, Starfield B, Wulu J, Regan J, Politzer R. The relationship between primary care, income inequality, and mortality in US States, 1980–1995. J Am Board Fam Pract. 2003;16(5):412–22. doi: 10.3122/jabfm.16.5.412. [DOI] [PubMed] [Google Scholar]
- 7.Starfield B, Shi L. Policy relevant determinants of health: an international perspective. Health Policy. 2002;60(3):201–18. doi: 10.1016/s0168-8510(01)00208-1. [DOI] [PubMed] [Google Scholar]
- 8.Østbye T, Yarnall KS, Krause KM, Pollak KI, Gradison M, Michener JL. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3(3):209–14. doi: 10.1370/afm.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yarnall KS, Pollak KI, Østbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–41. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hobbs FDR, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, et al. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet. 2016;387(10035):2323–30. doi: 10.1016/S0140-6736(16)00620-6. Epub 2016 Apr 5. Erratum in: Lancet 2016;387(10035):2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Binns HJ, Lanier D, Pace WD, Galliher JM, Ganiats TG, Grey M, et al. Describing primary care encounters: the Primary Care Network survey and the National Ambulatory Medical Care survey. Ann Fam Med. 2007;5(1):39–47. doi: 10.1370/afm.620. Erratum in: Ann Fam Med 2007;5(2):179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Britt H, Miller GC, Henderson J, Bayram C, Harrison C, Valenti L, et al. General practice activity in Australia 2014–15. Sydney, Aust: Sydney University Press; 2015. General practice series no. 38. Available from: http://sydney.edu.au/medicine/fmrc/publications/BEACH-feature-chapter-2015.pdf. Accessed 2018 Sep 21. [Google Scholar]
- 13.Wändell P, Carlsson AC, Wettermark B, Lord G, Cars T, Ljunggren G. Most common diseases diagnosed in primary care in Stockholm, Sweden, in 2011. Fam Pract. 2013;30(5):506–13. doi: 10.1093/fampra/cmt033. [DOI] [PubMed] [Google Scholar]
- 14.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 15.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. Epub 2009 Jul 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.United Nations . World economic situation and prospects 2012. New York, NY: United Nations; 2012. Country classification. In: United Nations; pp. 131–40. Available from: www.un.org/en/development/desa/policy/wesp/wesp_archive/2012wesp.pdf. Accessed 2018 Sep 21. [Google Scholar]
- 17.Britt H, Bhasale A, Miles DA, Meza A, Sayer GP, Angelis M. The sex of the general practitioner: a comparison of characteristics, patients, and medical conditions managed. Med Care. 1996;34(5):403–15. doi: 10.1097/00005650-199605000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Brueton V, Yogeswaran P, Chandia J, Mfenyana K, Modell B, Modell M, et al. Primary care morbidity in Eastern Cape province. S Afr Med J. 2010;100(5):309–12. doi: 10.7196/samj.3427. [DOI] [PubMed] [Google Scholar]
- 19.Fleming DM, Cross KW, Barley MA. Recent changes in the prevalence of diseases presenting for health care. Br J Gen Pract. 2005;55(517):589–95. [PMC free article] [PubMed] [Google Scholar]
- 20.Harrison CM, Britt HC, Charles J. Sex of the GP - 20 years on. Med J Aust. 2011;195(4):192–6. doi: 10.5694/j.1326-5377.2011.tb03278.x. [DOI] [PubMed] [Google Scholar]
- 21.Mash B, Fairall L, Adejayan O, Ikpefan O, Kumari J, Mathee S, et al. A morbidity survey of South African primary care. PLoS One. 2012;7(3):e32358. doi: 10.1371/journal.pone.0032358. Epub 2012 Mar 16. Erratum in: PLoS One 2012;7(5): 10.1371/annotation/3545077e-aded-4eef-a460-be1edbd1845c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ministry of Health – Manatū Hauora [website] Family doctors: methodology and description of the activity of private GPs. The national primary medical care survey (NatMedCa): 2001/02. Report 1. Wellington, NZ: Ministry of Health; 2004. Available from: www.health.govt.nz/publication/family-doctors-methodology-and-description-activity-private-gps. Accessed 2018 Sep 24. [Google Scholar]
- 23.Mohan N, Nagavi BG. Development of standard therapeutic guidelines for selected common diseases for the primary health care centres of a south Indian district. Int J Pharm Pract. 2003;11(3):169–74. [Google Scholar]
- 24.Murphy M, Brodie G, Byrne S, Bradley C. An observational study of public and private general practitioner consultations in the Republic of Ireland. Ir J Med Sci. 2015;184(1):147–52. doi: 10.1007/s11845-014-1078-3. Epub 2014 Feb 20. [DOI] [PubMed] [Google Scholar]
- 25.NAMCS and NHAMCS Web tables. 2014. Atlanta, GA: Centers for Disease Control and Prevention; 2017. National Center for Health Statistics. Available from: www.cdc.gov/nchs/data/ahcd/namcs_summary/2014_namcs_web_tables.pdf. Accessed 2018 Sep 21. [PubMed] [Google Scholar]
- 26.Pace WD, Dickinson LM, Staton EW. Seasonal variation in diagnoses and visits to family physicians. Ann Fam Med. 2004;2(5):411–7. doi: 10.1370/afm.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pearson N, O’Brien J, Thomas H, Ewings P, Gallier L, Bussey A. Collecting morbidity data in general practice: the Somerset morbidity project. BMJ. 1996;312(7045):1517–20. doi: 10.1136/bmj.312.7045.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Probst JC, Moore CG, Baxley EG, Lammie JJ. Rural-urban differences in visits to primary care physicians. Fam Med. 2002;34(8):609–15. [PubMed] [Google Scholar]
- 29.Salvi S, Apte K, Madas S, Barne M, Chhowala S, Sethi T, et al. Symptoms and medical conditions in 204 912 patients visiting primary health-care practitioners in India: a 1-day point prevalence study (the POSEIDON study) Lancet Glob Health. 2015;3(12):e776–84. doi: 10.1016/S2214-109X(15)00152-7. [DOI] [PubMed] [Google Scholar]
- 30.Sayer GP, Britt H. Sex differences in morbidity: a case of discrimination in general practice. Soc Sci Med. 1996;42(2):257–64. doi: 10.1016/0277-9536(95)00097-6. [DOI] [PubMed] [Google Scholar]
- 31.Soler JK, Okkes I, Oskam S, van Boven K, Zivotic P, Jevtic M, et al. An international comparative family medicine study of the Transition Project data from the Netherlands, Malta and Serbia. Is family medicine an international discipline? Comparing incidence and prevalence rates of reasons for encounter and diagnostic titles of episodes of care across populations. Fam Pract. 2012;29(3):283–98. doi: 10.1093/fampra/cmr098. Epub 2012 Feb 3. [DOI] [PubMed] [Google Scholar]
- 32.Choosing Wisely . Five things physicians and patients should question. Choosing Wisely: Society of General Internal Medicine; 2013. Available from: www.choosingwisely.org/wp-content/uploads/2015/02/SGIM-Choosing-Wisely-List.pdf. Accessed 2018 Sep 25. [Google Scholar]
- 33.Osborn R, Moulds D, Schneider EC, Doty MM, Squires D, Sarnak DO. Primary care physicians in ten countries report challenges caring for patients with complex health needs. Health Aff (Millwood) 2015;34(12):2104–12. doi: 10.1377/hlthaff.2015.1018. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization [website] Millions with mental disorders deprived of treatment and care. Geneva, Switz: World Health Organization; 2008. Available from: www.who.int/mediacentre/news/releases/2008/pr37/en. Accessed 2018 Sep 25. [Google Scholar]
- 35.Office of the Surgeon General. Center for Mental Health Services. National Institute of Mental Health . Mental health: culture, race, and ethnicity. A supplement to mental health: a report of the Surgeon General. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2001. [PubMed] [Google Scholar]
- 36.Stewart Willams J, Ng N, Peltzer K, Yawson A, Biritwum R, Maximova T, et al. Risk factors and disability associated with low back pain in older adults in low- and middle-income countries. Results from the WHO study on global AGEing and adult health (SAGE) PLoS One. 2015;10(6):e0127880. doi: 10.1371/journal.pone.0127880. [DOI] [PMC free article] [PubMed] [Google Scholar]