Abstract
Background
Accurate glomerular filtration rate estimation informs drug dosing and risk stratification. Body composition heterogeneity influences creatinine production and the precision of creatinine-based estimated glomerular filtration rate (eGFRcr) in the elderly. We compared chronic kidney disease (CKD) categorization using eGFRcr and cystatin C-based estimated GFR (eGFRcys) in an elderly, racially/ethnically diverse cohort to determine their concordance.
Methods
The Northern Manhattan Study (NOMAS) is a predominantly elderly, multi-ethnic cohort with a primary aim to study cardiovascular disease epidemiology. We included participants with concurrently measured creatinine and cystatin C. eGFRcr was calculated using the CKD-EPI 2009 equation. eGFRcys was calculated using the CKD-EPI 2012 equation. Logistic regression was used to estimate odds ratios and 95% confidence intervals of factors associated with reclassification from eGFRcr≥60ml/min/1.73m2 to eGFRcys<60ml/min/1.73m2.
Results
Participants (n = 2988, mean age 69±10yrs) were predominantly Hispanic, female, and overweight/obese. eGFRcys was lower than eGFRcr by mean 23mL/min/1.73m2. 51% of participants’ CKD status was discordant, and only 28% maintained the same CKD stage by both measures. Most participants (78%) had eGFRcr≥60mL/min/1.73m2; among these, 64% had eGFRcys<60mL/min/1.73m2. Among participants with eGFRcr≥60mL/min/1.73m2, eGFRcys-based reclassification was more likely in those with age >65 years, obesity, current smoking, white race, and female sex.
Conclusions
In a large, multiethnic, elderly cohort, we found a highly discrepant prevalence of CKD with eGFRcys versus eGFRcr. Determining the optimal method to estimate GFR in elderly populations needs urgent further study to improve risk stratification and drug dosing.
Introduction
Accurate and reliable glomerular filtration rate (GFR) estimation has enabled the identification and classification of renal dysfunction in a manner that could not be done with the use of serum creatinine values in isolation.[1–3] The calculation of estimated GFR (eGFR) using creatinine, an endogenous amino acid derivative of muscle cells, can inform drug dosing and guide risk stratification.[4–6] By taking into account factors that impact creatinine generation, eGFR equations are able to provide an assessment of GFR without the cost or complexity associated with GFR “measurement” using exogenous substances such as inulin or iohexol.[7]
However, the use of creatinine is imperfect: because creatinine generation is dependent on muscle mass, factors that influence body composition, including age, sex, and race, adversely impact the reliability of creatinine-based GFR estimation.[8] Due to these limitations, Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend confirming creatinine-based chronic kidney disease (CKD) diagnosis using an alternative method of GFR estimation in select groups.[9] In the United States, the widely-used MDRD (Modification of Diet in Renal Disease) and CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) equations were initially developed from cohorts with a low prevalence of socio-demographic characteristics that may affect serum creatinine (mean age 50.6 years, 88% White and mean age 47 years, 95% White or Black race respectively).[10, 11]
Age-related body composition changes in the elderly lead to a decline in the relative proportion of muscle mass and a corresponding decrease in creatinine production. In this setting, stable renal function is reflected by decreasing serum creatinine concentrations over time, and thus a decline in GFR may not be reflected by significant increases in serum creatinine.[12] The uncertainty around creatinine-based estimates’ ability to adequately estimate GFR across a variety of body compositions, particularly at the extremes of age, has led to interest in using alternative biomarkers. Cystatin C is an endogenous protease inhibitor produced at a stable rate by most nucleated cells, and its generation has less inter-person variability than that of creatinine, especially as related to ethnicity, age, or sex.[8, 13, 14] Serum cystatin C values have been shown to be predictive of mortality, and cystatin C-based GFR estimating (eGFRcys) equations have been shown to outperform those using creatinine-based eGFR (eGFRcr) in prediction of CKD-associated morbidity and mortality.[10, 15–20] Notably, although eGFRcys does not significantly outperform eGFRcr in accuracy of GFR quantification in the general population, there appears to be a greater advantage in the elderly.[21, 22] Further, while efforts to develop new models for GFR estimation in the elderly have focused on European populations, the relative performance of creatinine- and cystatin-based equations remains unclear in Hispanics, which is concerning given that this is the fastest growing segments of the United States population.[21, 23, 24]
The objectives of this study are to determine the concordance of cystatin- and creatinine-based CKD diagnosis in the Northern Manhattan Study (NOMAS) cohort, an elderly, racially/ethnically diverse cohort in northern Manhattan. Given that these demographic characteristics were not well represented during the development of commonly used eGFR equations, we hypothesized that there would be significant discordance in CKD prevalence when using the two different GFR estimation methods.
Methods
Cohort
NOMAS is a prospective study with a primary aim to evaluate cardiovascular disease risk factors in an urban, racially/ethnically diverse community in northern Manhattan. Participants were eligible for enrollment if they were age≥40 years, had no prior history of stroke, had a telephone, and resided in Northern Manhattan for 3 months prior to completion of an enrollment phone interview.[25] All participants had serum creatinine measured at enrollment, and a subsample (n = 2988, 90.6%) had cystatin C measurements on stored blood samples as part of an ancillary study. All procedures performed were approved by and conducted in accordance with the ethical standards of the Columbia University Medical Center’s Institutional Review Board. Written informed consent was obtained from all participants.
Assessment of renal function, demographic variables, and risk factors
Blood samples were obtained during baseline enrollment (1993–2001). Creatinine and cystatin C values were measured on samples obtained at the same time point (baseline enrollment) for each patient. Laboratory testing was performed at Columbia University and the University of Miami. Serum creatinine (mg/dL) measurements used Olympus instrumentation with a Jaffe-based method. Although initial creatinine concentrations were measured prior to IDMS standardization, creatinine was re-measured in 100 samples stored at -80°C using an IDMS-traceable method for creatinine measurement in order to develop a correction factor similar to what has been done successfully by other cohorts.[26, 27] The mean difference between standardized and non-standardized creatinine was -0.056±0.079mg/dL (r = 0.98). (S1 and S2 Figs). In the absence of a meaningful difference, a calibration factor was not applied prior to using creatinine values for GFR estimation using the CKD-EPI 2009 equation.[28] However, a sensitivity analysis was performed by repeating the primary analysis using creatinine values after calibration factor application. Cystatin C (mg/L) was measured on samples (84% plasma, 14% serum, 2% unspecified) stored at -80°C using Roche Diagnostics Cystatin Reagents on a Roche analyzer, standardized against ERM-DA471/IFCC reference material (intra-assay coefficient of variation (CV) 2.8% and interassay CV 4.1%; reference range 0.5–1.3 mg/L). The eGFRcys estimation was based on the CKD-EPI 2012 equation.[10]
Height and weight were measured during the initial patient assessment; overweight was defined as BMI 25-30kg/m2 and obesity as BMI>30 kg/m2. Race, ethnicity, and smoking status were self-reported. Hypertension was defined as systolic blood pressure >140mmHg or diastolic blood pressure >90mmHg based on the mean of two blood pressure measurements or the patient's self-report of a history of hypertension/antihypertensive use. Diabetes mellitus was defined by self-report, fasting blood glucose level >126mg/dL, or insulin/oral hypoglycemic use. Hypercholesterolemia was based on self-report, lipid lowering therapy use, or fasting total cholesterol level >240mg/dL.
Statistical analysis
Calculated eGFRcr and eGFRcys were dichotomized at a clinical cutoff of 60ml/min/1.73m2 consistent with standard GFR-based definitions of CKD (i.e., eGFR<60ml/min/1.73m2 = CKD).[9] Discordance was defined as CKD diagnosis by only one of the two estimates. A Bland-Altman analysis was used to assess agreement between eGFRcr and eGFRcys by plotting the difference between the two estimates (eGFRcr—eGFRcys) against their mean ([eGFRcr + eGFRcys]/2) for each participant. Reclassification was defined as change in eGFRcr-based CKD diagnosis when using eGFRcys (ie. eGFRcr≥60ml/min/1.73m2 with eGFRcys<60ml/min/1.73m2 OR eGFRcr<60ml/min/1.73m2 with eGFRcys≥60ml/min/1.73m2). Given the uncertainty regarding which GFR estimate is more accurate in populations like ours and the absence of measured GFR data, we chose this definition of reclassification because creatinine-based GFR estimation is currently widely used in standard practice. We did, however, note that very few participants had eGFRcr<60ml/min/1.73m2 with eGFRcys>60ml/min/1.73m2 and therefore focused our analysis of reclassification on participants with eGFRcr≥60ml/min/1.73m2.
We first assessed reclassification among those with eGFRcr≥60ml/min/1.73m2. The proportion of reclassification was calculated and compared by baseline demographics and comorbidities using multivariate logistic regression with indication of reclassification [1 for reclassification (eGFRcys<60ml/min/1.73m2) and 0 for no reclassification (eGFRcys≥60ml/min/1.73m2)] as a dependent variable. We calculated the odds ratio and 95% confidence interval (OR, 95% CI) for the association with the proportion of reclassification. A similar analysis was not performed on those with eGFRcr<60ml/min/1.73m2 because only a small number (n = 43) were reclassified with eGFRcys≥60ml/min/1.73m2; these participants were manually reviewed.
We performed two sensitivity analyses. First, we rechecked the proportion of reclassification using eGFRcr recalculated after applying a calibration factor to SCr values (based on rechecking 100 samples using an IDMS-traceable method for creatinine, as above). Next, we rechecked the proportion of reclassification only among participants with age<65 years who self-identified as white race, a population more similar to the group in which the CKD-EPI equations were originally developed. Finally, we calculated eGFR using the combined creatinine-cystatin CKD-EPI 2012 equation (eGFRcr-cys) to determine the difference in eGFR-based CKD prevalence using each of the three estimates. Analyses were conducted using SAS version 9.3 (Cary, NC) and R version 3.5.0.
Results
Among the 3298 NOMAS cohort participants, 2988 (91%) had both serum creatinine and cystatin C measured at the same time point and were included in our analysis. The mean age of the final cohort was 69±10 years, with 61% individuals older than 65 years at the time of data collection. Participants were predominantly Hispanic (53%), female (63%), and either overweight (41%) or obese (28%) (Table 1).
Table 1. Baseline characteristics of cohort.
| Age (years), mean (sd) | 69 (10.2) |
|---|---|
| Sex | |
| Female | 1887 (63%) |
| Male | 1101 (37%) |
| Race | |
| White | 619 (21%) |
| Black | 725 (24%) |
| Hispanic | 1577 (53%) |
| Other | 67 (2%) |
| BMI (kg/m2) | |
| <20 | 152 (5%) |
| 20–24 | 782 (26%) |
| 25–30 | 1232 (41%) |
| >30 | 822 (28%) |
| Smoking Status | |
| Never Smoker | 1404 (47%) |
| Former Smoker | 1084 (36%) |
| Current Smoker | 498 (17%) |
| Comorbidities | |
| Diabetes Mellitus | 634 (21%) |
| Hypertension | 2196 (73%) |
| Any Cardiac Disease | 704 (24%) |
| Estimated GFR (ml/min/1.73m2) | |
| eGFRcr, mean (sd) | 75 ± 19 |
| eGFRcys, mean (sd) | 52 ± 17 |
| Antihypertensive Use | |
| Diuretic | 465 (16%) |
| Beta blocker | 355 (12%) |
| Calcium channel blocker | 596 (20%) |
| ACE inhibitor | 491 (16%) |
sd = standard deviation, BMI = body mass index, GFR = glomerular filtration rate, eGFRcr = creatinine-based estimated GFR using the CKD-EPI 2009 equation, eGFRcys = cystatin C-based estimated GFR using the CKD-EPI 2012 equation, ACE = angiotensin converting enzyme
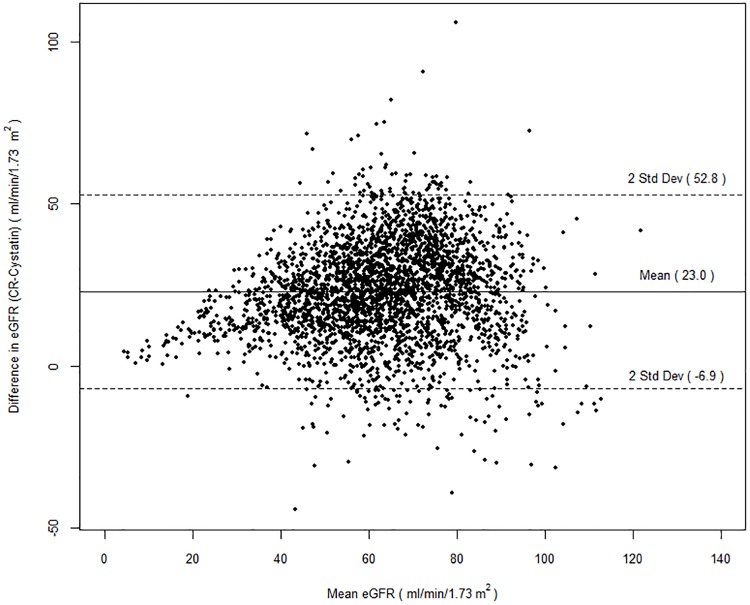
Mean SCr was 0.96 ± 0.4mg/dL and mean cystatin C was 1.4 ± 0.6mg/L, corresponding to mean eGFRcr 75 ± 19 ml/min/1.73m2 and mean eGFRcys 52 ± 17 ml/min/1.73m2. The creatinine- and cystatin-based GFR estimates (eGFRcr and eGFRcys, respectively) were correlated (r = 0.62, p<0.001) (S3 and S4 Figs). On average, eGFRcys was 23±15ml/min/1.73m2 lower than eGFRcr. The Bland-Altman plot shows that the participants primarily displayed difference between eGFRcr and eGFRcys of -7 to +53 (mean ± 2 standard deviations) with decreasing agreement noted at higher mean eGFR (Fig 1). Accordingly, there was a markedly higher prevalence of CKD (eGFR<60ml/min/1.73m2), using eGFRcys compared to eGFRcr (71% vs 22%, p<0.001) (Tables 2 and 3).
Fig 1. Bland-Altman plot of the difference in creatinine-based estimated glomerular filtration rate (eGFRcr) and cystatin C-based estimated glomerular filtration rate (eGFRcys) versus the mean of the two estimates.
Table 2. Comparison of CKD diagnosis by equation.
| eGFR (SCr) | eGFR (Cys) | ||
| ≥ 60 | < 60 | Total | |
| ≥ 60 | 838 | 1495 | 2333 |
| (28.1%) | (50%) | (78.1%) | |
| < 60 | 43 | 612 | 655 |
| (1.4%) | (20.5%) | (21.9%) | |
| Total | 881 | 2107 | 2988 |
| (29.5%) | (70.5%) | ||
CKD = chronic kidney disease, eGFR = estimated glomerular filtration rate
Table 3. Distribution of CKD stage by GFR-estimating equation.
| eGFRcr | eGFRcys | Total | |||||
| <15 | 15–29 | 30–59 | 60–89 | ≥90 | N | % | |
| <15 | 11 (92%) | 1 (8%) | 0 | 0 | 0 | 12 | 0.4 |
| 15–29 | 19 (56%) | 14 (41%) | 0 | 1 (3%) | 0 | 34 | 1.1 |
| 30–59 | 10 (2%) | 172 (28%) | 385 (63%) | 40 (7%) | 1 (<1%) | 608 | 20.4 |
| 60–89 | 2 (<1%) | 48 (3%) | 1181 (72%) | 380 (23%) | 19 (1%) | 1630 | 54.5 |
| ≥ 90 | 0 | 8 (1%) | 256 (36%) | 402 (57%) | 38 (5%) | 704 | 23.6 |
| Total | 42 | 243 | 1822 | 823 | 58 | 2988 | |
| % | 1.4 | 8.1 | 61 | 27.5 | 1.9 | ||
CKD = chronic kidney disease, eGFR = estimated glomerular filtration rate
The proportion of discordance between eGFRcr and eGFRcys-based CKD diagnosis was 51%. The highest discordance was observed among participants with eGFRcr≥60ml/min/1.73m2. Over half of the participants who were reclassified from eGFRcr≥60ml/min/1.73 m2 to eGFRcys<60ml/min/1.73 m2 had a difference in GFR estimates >30ml/min/1.73m2, while only 2.8% of participants displayed a difference ≤10ml/min/1.73m2 (Table 4). Only 43 participants had eGFRcr<60ml/min/1.73 m2 but eGFRcys>60ml/min/1.73 m2; manual review demonstrated that their GFR estimates were clustered around 60, with the majority (81%) displaying eGFRcr 50–59.9 but eGFRcys 60–69.9 (median eGFR difference 9.9ml/min/1.73m2).
Table 4. Distribution of eGFR discrepancy among those reclassified to CKD (i.e eGFRcr≥60 & eGFRcys<60).
| eGFRcr—eGFRcys | Frequency | Percent |
|---|---|---|
| 0–10 | 42 | 3% |
| 10–20 | 249 | 17% |
| 20–30 | 428 | 29% |
| 30–40 | 434 | 29% |
| 40–50 | 247 | 17% |
| 50–60 | 80 | 5% |
| 60–70 | 8 | 0.50% |
| >70 | 7 | 0.50% |
CKD = chronic kidney disease, eGFR = estimated glomerular filtration rate
49% of participants demonstrated CKD diagnosis concordance: 21% of the cohort had evidence of CKD by both estimates, while 45 patients (1.5% of the cohort) had evidence of severe CKD (eGFR<30ml/min/1.73m2) using both estimates. A minority of participants (28%) maintained the same CKD staging-based eGFR categories (ie. <15, 15–29, 30–59, 60–89, ≥90) using both estimates (Tables 2 and 3).
Reclassification among eGFRcr ≥60ml/min/1.73m2
Among those with eGFRcr≥60ml/min/1.73m2, the proportion of reclassification (eGFRcys<60ml/min/1.73 m2) was 64%. Reclassification was not limited to participants with borderline eGFRcr—although those with eGFRcr 60-89ml/min/1.73m2 were most likely to be reclassified (76%), many participants with eGFRcr≥90ml/min/1.73m2 were reclassified as well (38%). However, almost all (96%) of those reclassified were estimated to have eGFRcys 30-59ml/min/1.73m2. Most (81%) reclassified participants had ≥20mL/min/1.73m2 discrepancy between GFR estimates.
We examined the association of demographics and comorbidities with the proportion of reclassification (Table 5). In an adjusted model, the odds of reclassification were greater in those with age >65 years (vs. age ≤65, OR 5.67, 95% CI 4.61–6.99), obesity (OR 2.06 vs BMI≤30, 95% CI 1.64–2.59), current smokers (OR 1.66 vs non-smokers, 95% CI 1.26–2.18), non-diabetics (OR 1.64, 95% CI 1.30–2.08), females (OR 1.56, 95% CI 1.27–1.92), and white race (vs. African American, OR 2.04, 95% CI 1.49–2.78) (vs. Hispanic, OR 1.56, 95% CI 1.18–2.08).
Table 5. Factors associated with reclassification to eGFRcys <60 among participants with eGFRcr≥60.
| Parameter | Adjusted* | ||
|---|---|---|---|
| OR | 95% CI | ||
| Age>65 | 5.67 | 4.61 | 6.99 |
| Female (vs Male) | 1.56 | 1.27 | 1.92 |
| African American (vs. White) | 0.49 | 0.36 | 0.67 |
| Hispanic (vs. White) | 0.64 | 0.48 | 0.85 |
| Diabetics | 0.61 | 0.48 | 0.77 |
| Hypertension | 1.24 | 1.00 | 1.54 |
| Obese | 2.06 | 1.63 | 2.59 |
| Past Smoker (vs. non-smoker) | 1.08 | 0.87 | 1.35 |
| Current Smoker (vs. non-smoker) | 1.66 | 1.26 | 2.18 |
| Hypercholesterolemia | 0.93 | 0.76 | 1.14 |
| Any Cardiac Disease | 1.73 | 1.35 | 2.23 |
OR = odds ratio, CI = confidence interval;
*Adjusted for age, sex, race-ethnicity, education, medical insurance, diabetes, hypertension, BMI, smoking status, hypercholesterolemia and cardiac disease
Sensitivity analyses
Applying the calibration factor to serum creatinine values as described above yielded similar reclassification frequency (S1 Table). Next, we limited the analysis to participants aged <65 years with white race. These 110 participants continued to display a high frequency of reclassification: among the 88% of this subpopulation with eGFRcr≥60ml/min/1.73m2, 49% were reclassified to eGFRcys<60ml/min/1.73m2 (S2 Table). Finally, given the large difference in CKD prevalence observed above, we calculated eGFRcr-cys using the CKD-EPI 2012 formula that utilizes both biomarkers in a post-hoc analysis. Expectedly, we found that this method of GFR estimation yielded a CKD prevalence in between those provided using eGFRcr and eGFRcys (54.8%) (S3 Table).
Discussion
We compared creatinine- and cystatin-based GFR estimation in a large, elderly, racially/ethnically diverse cohort and found a large difference in the prevalence of CKD (defined as eGFR<60ml/min/1.73m2). While the direction of the findings was consistent with our hypothesis, the magnitude of the differences was striking. Over half of the participants did not retain the same CKD status using both GFR estimates, and the differences in CKD classification using eGFRcys and eGFRcr were not simply clustered around CKD class thresholds. In fact, even among participants with eGFRcr≥90ml/min/1.73m2 (classically considered a “normal” GFR), 37.5% were reclassified as having CKD using eGFRcys. This degree of discordance is greater than has been observed in other cohorts and raises potential concerns about the commonly used creatinine- and cystatin-based GFR estimates. The widely-used CKD-EPI eGFR equations were developed in a population with a median age of 47 years and only <4% of participants were aged ≥71 years.[28] In contrast, the mean participant age at the time of enrollment in NOMAS was 69 years. Further, over half of our participants self-identified as Hispanic. The cystatin C-based CKD-EPI eGFR equation may have an advantage in our cohort given the absence of inclusion of race and a smaller impact of age on the estimate.[10, 14]
Previous studies have compared creatinine- and cystatin-based eGFR in different elderly groups but have not demonstrated the degree of discordance that we observed.[29–32] The Sacramento Area Latino Study on Aging (SALSA), a cohort of Mexican-American participants with mean age 71 years, demonstrated that 10% of participants had discordant eGFRcr vs eGFRcys CKD classification.[29] However, the SALSA cohort had a much lower prevalence of CKD compared to the NOMAS cohort, with only 21% of participants having CKD based on any marker (whereas in our group 22% and 71% had CKD based on creatinine and cystatin C, respectively).[29] A smaller study comparing GFR estimates in 95 elderly Brazilian participants Brazil (mean age 85.3 years) suggested that although eGFRcr overestimated GFR, eGFRcys was more biased than eGFRcr, and the combined use of both markers performed better.[33] Similarly, estimating GFR with a combined creatinine and cystatin equation outperformed eGFRcys and eGFRcr in an elderly Icelandic cohort (n = 805, mean age 80.3 years).[32] A portion of another analysis with participants of primarily European ancestry (n = 394, mean age 80 years) found that while both equations overestimated GFR in those without decreased measured GFR, eGFRcys tended to underestimate GFR in patients with measured GFR<60ml/min/1.73m2, while eGFRcr overestimated GFR in the same group.[34] An additional study examined reclassification among participants in the Osteoporotic Fractures in Men Study (mean age 76.4 years) and found a large discrepancy between prevalence of eGFR<60ml/min/1.73m2 based on eGFRcys and eGFRcr (36% vs 23%), with eGFRcys providing superior prediction of mortality.[35]
The magnitude of the difference between the equations demonstrated in our study is large and, given the implications for incorrect medication dosing, particularly concerning. Our prevalence of eGFRcys-based CKD is consistent with prior data that used the creatinine-based Modification of Diet in Renal Disease (MDRD) Study formula and noted prevalent CKD Stages 1–4 in almost half of NHANES 1999–2004 participants age ≥70 years, with 37.8% of participants in this age group having CKD stages 3 or 4.[36, 37] Further, that analysis also showed a significant increase in CKD prevalence over time, supporting the plausibility of our findings.[36] The large discrepancies we observed in the absence of measured GFR data (using an exogenous marker) as a reference suggest that either one or both estimates lose precision in our elderly cohort. Several potential contributing factors should be considered as possible explanations.
First is a possible systematic overestimation of GFR using eGFRcr in our cohort. In our cohort, age was associated with reclassification of creatinine-based CKD status using cystatin C, whereas male sex was associated with decreased likelihood of reclassification. Prior investigators have suggested using age, cardiovascular disease, diabetes, hypertension, obesity, and smoking to identify patients who may have occult CKD not identified using eGFRcr alone and therefore warrant eGFRcys assessment.[38] With the exception of diabetes, our data is consistent with these prior findings. An increased prevalence of sarcopenia with age may be contributing to lower-than-expected serum creatinine independent of renal function and lead to the large discrepancy between eGFRcr and eGFRcys that we observed.
The other possibility is that eGFRcys systematically underestimates GFR in the NOMAS cohort instead of (or in addition to) the hypothesized mechanism above. Age, weight, and smoking are known to be associated with increased cystatin C levels even after controlling for creatinine clearance.[39] Consistent with this, these patient characteristics were all associated with increased reclassification in our cohort supporting the notion that a high prevalence of obesity and smoking would limit the ability of eGFRcys to accurately identify CKD in older cohorts.
Finally, currently available cystatin C assays vary significantly, underscoring the need for the ongoing development of reference material for cystatin C assays intended to improve this problem.[40–46] In contrast to the CKD-EPI group, which used a Siemens Dade Behring Nephelometer traceable to IFCC/IRMM reference materials, we used a Roche assay also standardized against ERM-DA471/IFCC reference material. Despite this difference, the cystatin C values we observed are quite plausible. The mean serum cystatin C was 1.4mg/L in the CKD-EPI study development/internal validation cohort.[10] Further, a previous investigation on cystatin C concentration in healthy elderly subjects (age ≥65 years) in Britain found a mean cystatin C of 1.48mg/L in females and 1.53mg/L in males, also similar to our observed mean of 1.4mg/L.[47] Other prior studies focusing elderly participants have demonstrated variable mean cystatin C values, ranging from 1.14–1.44 mg/L.[21, 32–34] While it is certainly possible that our cystatin C assay may be less reliable than expected, considering that our testing utilized a commercially-available cystatin C assay, these discrepancies underscore the need for further studies including measured GFR data to determine their etiology in addition to the need for better cystatin assay standardization. This uncertainty should similarly be considered when interpreting GFR estimates that utilize both creatinine and cystatin (eGFRcr-cys), and additional investigation is needed to determine whether the use of both biomarkers together improves the accuracy of GFR estimates in this population.
Grubb, et al have proposed an alternative, assay-independent, cystatin-based eGFR equation (“CAPA”) developed using Swedish, Japanese, and Dutch cohorts.[24] However, given the limited demographic subgroups in which this equation was developed, its applicability to a broad section of the United States population remains uncertain. Similarly, the BIS (Berlin Initiative Study) equations designed for use in the elderly included only subjects living in Berlin, Germany.[21] Domestic initiatives are warranted to better address the need for improved GFR assessment in the United States, particularly in non-White populations.
Our findings have significant implications for clinical practice because the discrepant CKD categorizations would warrant different dose adjustments and carry significantly different prognostic implications. Currently, clinicians routinely receive eGFR data alongside serum creatinine results. Our observations suggest that these data could be misleading in populations similar to ours, potentially leading to inappropriate decisions regarding drug dosing, drug safety, risk stratification, and eligibility for advanced therapeutics. Accurate GFR ascertainment is critical for accurate dosing of medications cleared by the kidney, especially among elderly patients already at higher risk of polypharmacy-associated complications. This underscores the need for further study of the performance of different methods of GFR estimation in older, diverse populations.
In addition to changing the need for evaluation of CKD-associated complications including anemia and bone disease, accurately identifying decreased GFR can help clinicians better assess the contribution of CKD to patient outcomes such as cardiovascular events and mortality. Discrepant estimates using creatinine and cystatin may even be a marker for sarcopenia in the elderly and thus further inform the clinical care of these patients.[48] Finally, the timely CKD diagnosis and early referral to a nephrologist have been associated with improved outcomes.[49]
Our study confirms previous findings of significantly discrepant CKD diagnosis in elderly patients, but in a larger multiethnic cohort. The strengths of our study include a large sample size and diverse population. Limitations include the lack of measured GFR testing, as detailed above. These data would allow us to determine whether the differences between eGFRcr and eGFRcys result from lack of precision of one or both GFR estimates. Additionally, we lack information regarding albuminuria, an important component of CKD diagnosis, classification, and risk prediction, and our cross-sectional design relies on a single simultaneous creatinine and cystatin measurements for each participant. It should also be noted that the use of concordance of eGFR<60ml/min/1.73m2 (i.e. the established eGFR-based threshold for CKD diagnosis) as a primary endpoint is somewhat arbitrary, although the large differences in GFR estimates we observed emphasize the clinical importance of these findings. Further studies investigating differences in morbidity and mortality, as well as the development of clinically relevant kidney disease, among our participants whose CKD status was reclassified are also warranted, as the value of precise GFR estimates may not necessarily translate to improved prediction of adverse outcomes such as progression to end-stage renal disease or incidence of cardiovascular events.
Conclusions
In a large, racially/ethnically diverse, elderly population, we observed a dramatic increase in the prevalence of CKD and a significant amount of reclassification of CKD diagnosis when using cystatin C- rather than creatinine-based estimates of GFR. Given the aging of the population and the known associations between CKD and adverse cardiovascular events, our findings suggest that urgent further study is needed to clarify the accuracy of different methods of GFR estimation in the elderly. Improving GFR estimation in elderly patients can help identify unrecognized CKD, prevent CKD misdiagnosis, and promote management of CKD-associated complications at an earlier stage.
Supporting information
(TIF)
(TIF)
(TIF)
(TIF)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
Part of the analysis and results presented here were previously presented in abstract form at ASN Kidney Week 2016.
Data Availability
The data for this analysis is now available at Columbia's Academic Commons. The direct link to the dataset is https://doi.org/10.7916/D8VM5W5W.
Funding Statement
This study was supported by the National Institutes of Health grants R01 HL111195 (Cheung/Elkind), NS K23073104 (Willey), and R01 NS029993 (Sacco/Elkind). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.National Kidney F. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–266. [PubMed] [Google Scholar]
- 2.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Annals of internal medicine. 2003;139(2):137–47. [DOI] [PubMed] [Google Scholar]
- 3.Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005;67(6):2089–100. 10.1111/j.1523-1755.2005.00365.x [DOI] [PubMed] [Google Scholar]
- 4.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–305. 10.1056/NEJMoa041031 [DOI] [PubMed] [Google Scholar]
- 5.Hemmelgarn BR, Manns BJ, Lloyd A, James MT, Klarenbach S, Quinn RR, et al. Relation between kidney function, proteinuria, and adverse outcomes. JAMA. 2010;303(5):423–9. 10.1001/jama.2010.39 [DOI] [PubMed] [Google Scholar]
- 6.Stevens LA, Nolin TD, Richardson MM, Feldman HI, Lewis JB, Rodby R, et al. Comparison of drug dosing recommendations based on measured GFR and kidney function estimating equations. Am J Kidney Dis. 2009;54(1):33–42. 10.1053/j.ajkd.2009.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levey AS, Inker LA. Assessment of Glomerular Filtration Rate in Health and Disease: A State of the Art Review. Clin Pharmacol Ther. 2017;102(3):405–19. 10.1002/cpt.729 [DOI] [PubMed] [Google Scholar]
- 8.Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function—measured and estimated glomerular filtration rate. N Engl J Med. 2006;354(23):2473–83. 10.1056/NEJMra054415 [DOI] [PubMed] [Google Scholar]
- 9.Summary of Recommendation Statements. Kidney Int Suppl (2011). 2013;3(1):5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inker LA, Schmid CH, Tighiouart H, Eckfeldt JH, Feldman HI, Greene T, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367(1):20–9. 10.1056/NEJMoa1114248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Annals of internal medicine. 1999;130(6):461–70. [DOI] [PubMed] [Google Scholar]
- 12.Stevens LA, Levey AS. Chronic kidney disease in the elderly—how to assess risk. N Engl J Med. 2005;352(20):2122–4. 10.1056/NEJMe058035 [DOI] [PubMed] [Google Scholar]
- 13.Grubb AO. Cystatin C—properties and use as diagnostic marker. Adv Clin Chem. 2000;35:63–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foster MC, Levey AS, Inker LA, Shafi T, Fan L, Gudnason V, et al. Non-GFR Determinants of Low-Molecular-Weight Serum Protein Filtration Markers in the Elderly: AGES-Kidney and MESA-Kidney. Am J Kidney Dis. 2017;70(3):406–14. 10.1053/j.ajkd.2017.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salminen M, Laine K, Korhonen P, Wasen E, Vahlberg T, Isoaho R, et al. Biomarkers of kidney function and prediction of death from cardiovascular and other causes in the elderly: A 9-year follow-up study. Eur J Intern Med. 2016;33:98–101. 10.1016/j.ejim.2016.06.024 [DOI] [PubMed] [Google Scholar]
- 16.Shlipak MG, Matsushita K, Arnlov J, Inker LA, Katz R, Polkinghorne KR, et al. Cystatin C versus creatinine in determining risk based on kidney function. N Engl J Med. 2013;369(10):932–43. 10.1056/NEJMoa1214234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Menon V, Shlipak MG, Wang X, Coresh J, Greene T, Stevens L, et al. Cystatin C as a risk factor for outcomes in chronic kidney disease. Annals of internal medicine. 2007;147(1):19–27. [DOI] [PubMed] [Google Scholar]
- 18.Sarnak MJ, Katz R, Stehman-Breen CO, Fried LF, Jenny NS, Psaty BM, et al. Cystatin C concentration as a risk factor for heart failure in older adults. Annals of internal medicine. 2005;142(7):497–505. [DOI] [PubMed] [Google Scholar]
- 19.Shlipak MG, Sarnak MJ, Katz R, Fried LF, Seliger SL, Newman AB, et al. Cystatin C and the risk of death and cardiovascular events among elderly persons. N Engl J Med. 2005;352(20):2049–60. 10.1056/NEJMoa043161 [DOI] [PubMed] [Google Scholar]
- 20.Krolewski AS, Warram JH, Forsblom C, Smiles AM, Thorn L, Skupien J, et al. Serum concentration of cystatin C and risk of end-stage renal disease in diabetes. Diabetes Care. 2012;35(11):2311–6. 10.2337/dc11-2220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schaeffner ES, Ebert N, Delanaye P, Frei U, Gaedeke J, Jakob O, et al. Two novel equations to estimate kidney function in persons aged 70 years or older. Annals of internal medicine. 2012;157(7):471–81. 10.7326/0003-4819-157-7-201210020-00003 [DOI] [PubMed] [Google Scholar]
- 22.Inker LA, Levey AS, Tighiouart H, Shafi T, Eckfeldt JH, Johnson C, et al. Performance of glomerular filtration rate estimating equations in a community-based sample of Blacks and Whites: the multiethnic study of atherosclerosis. Nephrol Dial Transplant. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pottel H, Hoste L, Dubourg L, Ebert N, Schaeffner E, Eriksen BO, et al. An estimated glomerular filtration rate equation for the full age spectrum. Nephrol Dial Transplant. 2016;31(5):798–806. 10.1093/ndt/gfv454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grubb A, Horio M, Hansson LO, Bjork J, Nyman U, Flodin M, et al. Generation of a new cystatin C-based estimating equation for glomerular filtration rate by use of 7 assays standardized to the international calibrator. Clin Chem. 2014;60(7):974–86. 10.1373/clinchem.2013.220707 [DOI] [PubMed] [Google Scholar]
- 25.Sacco RL, Roberts JK, Boden-Albala B, Gu Q, Lin IF, Kargman DE, et al. Race-ethnicity and determinants of carotid atherosclerosis in a multiethnic population. The Northern Manhattan Stroke Study. Stroke. 1997;28(5):929–35. [DOI] [PubMed] [Google Scholar]
- 26.Kurella Tamura M, Wadley V, Yaffe K, McClure LA, Howard G, Go R, et al. Kidney function and cognitive impairment in US adults: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am J Kidney Dis. 2008;52(2):227–34. 10.1053/j.ajkd.2008.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stevens LA, Manzi J, Levey AS, Chen J, Deysher AE, Greene T, et al. Impact of creatinine calibration on performance of GFR estimating equations in a pooled individual patient database. Am J Kidney Dis. 2007;50(1):21–35. 10.1053/j.ajkd.2007.04.004 [DOI] [PubMed] [Google Scholar]
- 28.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Annals of internal medicine. 2009;150(9):604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peralta CA, Lee A, Odden MC, Lopez L, Zeki Al Hazzouri A, Neuhaus J, et al. Association between chronic kidney disease detected using creatinine and cystatin C and death and cardiovascular events in elderly Mexican Americans: the Sacramento Area Latino Study on Aging. J Am Geriatr Soc. 2013;61(1):90–5. 10.1111/jgs.12040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tsai CW, Grams ME, Inker LA, Coresh J, Selvin E. Cystatin C- and creatinine-based estimated glomerular filtration rate, vascular disease, and mortality in persons with diabetes in the U.S. Diabetes Care. 2014;37(4):1002–8. 10.2337/dc13-1910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Legrand H, Werner K, Christensson A, Pihlsgard M, Elmstahl S. Prevalence and determinants of differences in cystatin C and creatinine-based estimated glomerular filtration rate in community-dwelling older adults: a cross-sectional study. BMC Nephrol. 2017;18(1):350 10.1186/s12882-017-0759-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fan L, Levey AS, Gudnason V, Eiriksdottir G, Andresdottir MB, Gudmundsdottir H, et al. Comparing GFR Estimating Equations Using Cystatin C and Creatinine in Elderly Individuals. J Am Soc Nephrol. 2015;26(8):1982–9. 10.1681/ASN.2014060607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lopes MB, Araujo LQ, Passos MT, Nishida SK, Kirsztajn GM, Cendoroglo MS, et al. Estimation of glomerular filtration rate from serum creatinine and cystatin C in octogenarians and nonagenarians. BMC Nephrol. 2013;14:265 10.1186/1471-2369-14-265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kilbride HS, Stevens PE, Eaglestone G, Knight S, Carter JL, Delaney MP, et al. Accuracy of the MDRD (Modification of Diet in Renal Disease) study and CKD-EPI (CKD Epidemiology Collaboration) equations for estimation of GFR in the elderly. Am J Kidney Dis. 2013;61(1):57–66. 10.1053/j.ajkd.2012.06.016 [DOI] [PubMed] [Google Scholar]
- 35.Canales MT, Blackwell T, Ishani A, Taylor BC, Hart A, Barrett-Connor E, et al. Estimated GFR and Mortality in Older Men: Are All eGFR Formulae Equal. Am J Nephrol. 2016;43(5):325–33. 10.1159/000445757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–47. 10.1001/jama.298.17.2038 [DOI] [PubMed] [Google Scholar]
- 37.Garg AX, Papaioannou A, Ferko N, Campbell G, Clarke JA, Ray JG. Estimating the prevalence of renal insufficiency in seniors requiring long-term care. Kidney Int. 2004;65(2):649–53. 10.1111/j.1523-1755.2004.00412.x [DOI] [PubMed] [Google Scholar]
- 38.Peralta CA, Muntner P, Scherzer R, Judd S, Cushman M, Shlipak MG. A Risk Score to Guide Cystatin C Testing to Detect Occult-Reduced Estimated Glomerular Filtration Rate. Am J Nephrol. 2015;42(2):141–7. 10.1159/000439231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Knight EL, Verhave JC, Spiegelman D, Hillege HL, de Zeeuw D, Curhan GC, et al. Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement. Kidney Int. 2004;65(4):1416–21. 10.1111/j.1523-1755.2004.00517.x [DOI] [PubMed] [Google Scholar]
- 40.Eckfeldt JH, Karger AB, Miller WG, Rynders GP, Inker LA. Performance in Measurement of Serum Cystatin C by Laboratories Participating in the College of American Pathologists 2014 CYS Survey. Arch Pathol Lab Med. 2015;139(7):888–93. 10.5858/arpa.2014-0427-CP [DOI] [PubMed] [Google Scholar]
- 41.Li J, Dunn W, Breaud A, Elliott D, Sokoll LJ, Clarke W. Analytical performance of 4 automated assays for measurement of cystatin C. Clin Chem. 2010;56(8):1336–9. 10.1373/clinchem.2009.141531 [DOI] [PubMed] [Google Scholar]
- 42.Zhao Z, Sacks DB. Detrimental Effects of Not Using International Reference Materials to Calibrate Cystatin C Assays. Clin Chem. 2016;62(2):410–1. 10.1373/clinchem.2015.244988 [DOI] [PubMed] [Google Scholar]
- 43.Blirup-Jensen S, Grubb A, Lindstrom V, Schmidt C, Althaus H. Standardization of Cystatin C: development of primary and secondary reference preparations. Scand J Clin Lab Invest Suppl. 2008;241:67–70. 10.1080/00365510802150067 [DOI] [PubMed] [Google Scholar]
- 44.Ebert N, Delanaye P, Shlipak M, Jakob O, Martus P, Bartel J, et al. Cystatin C standardization decreases assay variation and improves assessment of glomerular filtration rate. Clin Chim Acta. 2016;456:115–21. 10.1016/j.cca.2016.03.002 [DOI] [PubMed] [Google Scholar]
- 45.Gonzalez-Antuna A, Rodriguez-Gonzalez P, Ohlendorf R, Henrion A, Delatour V, Garcia Alonso JI. Determination of Cystatin C in human serum by isotope dilution mass spectrometry using mass overlapping peptides. J Proteomics. 2015;112:141–55. 10.1016/j.jprot.2014.09.005 [DOI] [PubMed] [Google Scholar]
- 46.Grubb A, Blirup-Jensen S, Lindstrom V, Schmidt C, Althaus H, Zegers I, et al. First certified reference material for cystatin C in human serum ERM-DA471/IFCC. Clin Chem Lab Med. 2010;48(11):1619–21. 10.1515/CCLM.2010.318 [DOI] [PubMed] [Google Scholar]
- 47.Finney H, Bates CJ, Price CP. Plasma cystatin C determinations in a healthy elderly population. Arch Gerontol Geriatr. 1999;29(1):75–94. [DOI] [PubMed] [Google Scholar]
- 48.Kashani KB, Frazee EN, Kukralova L, Sarvottam K, Herasevich V, Young PM, et al. Evaluating Muscle Mass by Using Markers of Kidney Function: Development of the Sarcopenia Index. Crit Care Med. 2017;45(1):e23–e9. 10.1097/CCM.0000000000002013 [DOI] [PubMed] [Google Scholar]
- 49.Smart NA, Dieberg G, Ladhani M, Titus T. Early referral to specialist nephrology services for preventing the progression to end-stage kidney disease. Cochrane Database Syst Rev. 2014;6:CD007333. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
(TIF)
(TIF)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
The data for this analysis is now available at Columbia's Academic Commons. The direct link to the dataset is https://doi.org/10.7916/D8VM5W5W.