Abstract
Uncertainty in illness is regarded as a source of stress in many chronic diseases and is negatively related to health-related quality of life (HRQoL). However, studies on the relationship between uncertainty and HRQoL in patients with heart failure are limited. This study used Mishel’s theory of uncertainty in illness to investigate the mediating role of uncertainty in illness and depressive symptoms between symptom distress and HRQoL in patients with heart failure. This study used a cross-sectional correlation design. Participants were recruited by convenience sampling from outpatient services and medical wards of cardiology departments of a medical center in northern Taiwan. Data were collected for uncertainty, depressive symptoms, symptoms distress of heart failure, and HRQoL using self-report questionnaires. Demographics and clinical characteristics were analyzed with descriptive statistics. The mutual effects of disease characteristics, symptom distress, uncertainty in illness, depressive symptoms and HRQoL, as well as the overall model fitness, were analyzed by with structural equation modeling. We collected 147 qualified questionnaires. The mean score for the Mishel Uncertainty in Illness Scale for patients with heart failure was 73.5 (SD = 18.55); 65.3% of participants had a score of ≧13 on the Beck Depressive Inventory-II, indicating mild depression. Uncertainty, depressive symptoms, and HRQoL were directly related to symptom distress. Symptom distress and depressive symptoms were both mediators between uncertainty and depressive symptoms. Depressive symptoms also mediated emotional support and HRQoL. Uncertainty and depressive symptoms were important factors in the pathway between symptom distress and HRQoL for heart failure patients. We suggest providing heart failure patients with tailored interventions for effective self-management of symptoms based on Mishel’s theory of uncertainty in illness, which could help control disease symptoms, alleviate uncertainty and depression as well as improve HRQoL.
Introduction
Heart failure (HF) is one of the significant global health issues and a serious health condition impacting many developing and developed countries, including Taiwan. It is estimated that over 5.1 million people in the United States have HF and over 650,000 patients are diagnosed with HF for the first time each year. The total medical costs for treating HF amount to more than US$3.92 billion [1]. The prevalence of HF is 0.4% to 6.0% in Asia, while values 6% was reported from Taiwan [2]. The cost of hospitalization was up to US$ 96 million in patients with HF in Taiwan [2]. The increasing prevalence of HF has resulted in an increased concern for HF as a clinical issue [3]. Due to the advancement of medical care, many HF patients are surviving longer; however, their prognosis remains poor and the 1-month re-hospitalization rate is approximately 17.1% [4].
The heart is pivotal for the circulation of blood. When the heart malfunctions, symptoms related to HF and short of the self-care capabilities impact not only the physical health of the patients but also their health-related quality of life (HRQoL) [5]. The varied and uncontrollable symptoms caused by HF may result in recurrent hospitalization and social isolation [6], which can lead to experience of uncertainty in illness [7]. HF patients frequently experience depression, which has been linked to increased risk of hospitalization and death [8]. Although uncertainty in illness is regarded as a source of stress in many chronic disease patients [9] and negatively related to HRQoL [10], studies on the relationship between uncertainty and HRQoL in patients with HF are limited. One study on uncertainty in illness and HRQoL in patients waiting for coronary artery bypass grafting surgery found that the lack of available information provided by health care professionals and the symptom distress caused by diseases during the waiting period for surgery may increase the uncertainty in illness and affect HRQoL [11]. Another longitudinal study on patients waiting for coronary angiography showed that uncertainty in illness was negatively related to HRQoL [12]. The study of Flemme et al. (2005) on patients with implanted cardioverter defibrillators revealed that uncertainty in illness was a key predictor of HRQoL [13].
Improving HRQoL for patients with cardiovascular disease by alleviating symptom distress and decreasing uncertainty in illness are important in disease management. However, few studies have investigated the relationship between uncertainty in illness and HRQoL in patients with HF. Moreover, no study has investigated the mediating effect of emotional factors such as uncertainty and depressive symptoms on HRQoL. Therefore, the purpose of this study was to investigate the mutual relationships of uncertainty, depressive symptoms and HRQoL, based on Mishel's Uncertainty in Illness Theory (UIT). This study had three aims: (1) to explore uncertainty, depressive symptoms and HRQoL in HF patients; (2) to examine the relationships of uncertainty, depressive symptoms and HRQoL through testing a conceptual model based on Mishel’s UIT; and (3) to identify the mediating role of uncertainty and depressive symptoms in the relationship between symptom distress and HRQoL.
Theoretical framework
Michel’s UIT, proposed in 1988, is a theoretical framework for describing how an individual copes with a disease when unable to predict the outcome of an illness. Michel’s UIT consists of three principal themes: antecedents of uncertainty, appraisal of uncertainty and coping with uncertainty [14].
Antecedents of uncertainty refers to experiences that have occurred prior to the onset of an illness and affect a person’s thinking, such as perception of disease, exposure to pain, and prior experiences. This theme includes three components: stimuli frame, cognitive capacity, and structure providers. Stimuli frame is the personal perception of diseases and therapy-related events, which consists of symptom pattern, event familiarity and event congruence. Symptom pattern is the number, frequency, intensity, and duration of disease symptoms. If the symptom patterns have a high variability, the individual may perceive more uncertainty. Event familiarity means the individual familiarity with the scenario of disease and therapy-related events. The higher the familiarity, the less uncertainty the individual has about the therapy, care system, and the complexity of the disease. Event congruence is the consistency between the individual expectation of disease-related events and their actual experiences. Incongruence incurs unexpected uncertainty. Cognitive capacity and structure providers cause positive effects on stimuli frame. Cognitive capacity exhibits the individual capability of managing information. Structure providers disclose the resources assisting the individual to interpret stimuli frame, including education, social support and credible authority.
Appraisal of uncertainty refers to how a person evaluates an illness situation, which can be viewed as a danger or an opportunity. Danger is the probability of a negative outcome, while opportunity is the probability of a positive outcome.
‘Coping with uncertainty’ refers to how the strategies individual employs to manage the uncertainties of disease. Coping with a danger appraisal is regarded as a responsive action to decrease uncertainty, which deals with the emotion produced by a danger appraisal. Coping with a situation which is appraised as an opportunity, involves direct actions that will maintain positive feelings and hope.
Uncertainty always exists in the disease trajectory. When the role of the individual is changed, the daily functions are limited, the social communication is terminated, and the life of the individual is in danger because of the disease, uncertainty will show up naturally [15]. Under these circumstances, the individual may employ problem-focused or emotion-focused strategies to adapt to the difficult situations in order to maintain their quality of life [10].
The framework for this study is based on Mishel’s UIT to investigate the mediating role of uncertainty and depressive symptoms between symptom distress and HRQoL in HF patients. The disease characteristics, symptom distress and social support are regarded as the antecedent factors of uncertainty. HRQoL refer to the outcomes after adaptation. The symptoms of heart failure such as fatigue, dyspnea, and weight gain may negatively affect the patient’s psychological well-being [16,17]. Previous studies found that deterioration of physical symptoms was significantly associated with depressive symptoms [18,19] and approximately 50% of HF patients have depressive symptoms [20]. Depression significantly increased all-cause mortality and was related to poor HRQoL in HF patients [21,22]. Because depression as a predictor of HRQoL for HF patients and significantly associated with symptom distress [23,24], we also added depressive symptoms into the model to identify the mediator role of depressive symptoms between symptom distress and HRQoL. The model for this study is shown in Fig 1
Fig 1. Conceptual Framework of this study.
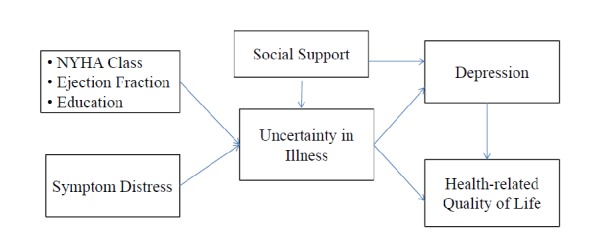
Conceptual Framework of uncertainty of illness and depressive symptoms in patients with heart failure. NHYA, New York Heart Association.
Methods
We conducted a cross-sectional correlation study to examine the relationships of uncertainty in illness, depressive symptoms and HRQoL based on Mishel's UIT. Uncertainty, depressive symptoms, and HRQoL were measured by using Chinese versions of standardized instruments.
Participants and procedure
We recruited study participants from a teaching hospital and medical center in northern Taiwan with convenience sampling. Patients diagnosed with HF were included if they met the following criteria: (1) older than 20 years, (2) with New York Heart Association (NYHA) Functional Class Ⅰ to Ⅳ, (3) without receiving heart transplant, permanent pacemaker or an implantable cardioverter defibrillator, (4) without addiction to drugs or alcohol, (5) not using antidepressants, and (6) without preexisting psychiatric diagnosis or cognitive impairment. The study was approved by the Institutional Review Board of the Tri-Service General Hospital National Defense Medical Centre. Prior to conducting the survey, patients were informed about the research purpose and procedure and were assured of anonymity. Written informed consent was obtained from all participants. A total of 147 HF patients participated in this study from January to June 2012. The estimates of power analysis revealed that the sample size provided the statistical power of 0.82 with the effect size at 0.15 and the significance (α) at 0.05 [25].
Instruments
Personal characteristics questionnaire
We designed a personal characteristics questionnaire to collect data regarding the demographics and health characteristics of the participants.
Mishel uncertainty in illness scale
Patients’ uncertainty of disease was measured with the Chinese version of the Mishel Uncertainty in Illness Scale (MUIS), which consists of 25 items rated on a 5-point Likert scale from "strongly disagree" to "strongly agree". The responses represent the patient’s perception of uncertainty about their symptoms, diagnosis, treatment, relationship with caregivers, and prognosis. There are 15 items related to factors of unpredictability, and 10 items to factors of multi-attributed ambiguity. A higher score indicates greater uncertainty. Cronbach’s α for the total scale was 0.87, and for the unpredictability subscale and the multi-attributed ambiguity subscale was 0.85 and 0.66, respectively [26]. In this study, Cronbach’s α for the total scale was 0.95, and for the unpredictability subscale and the multi-attributed ambiguity subscale was 0.94 and 0.86, respectively.
Beck depression inventory: Second Edition
The Chinese version of the Beck Depression Inventory- Second Edition (BDI-Ⅱ) is a 21-item self-administrated scale to assess the symptoms of depression. There are four symptom statements for each item. Responses to the item are rated from 0 to 3. The lower scores indicate less severity of depressive symptoms. A total score between 0 and 13 indicates a normal mood, between 14 and 19 indicates a mild level of depressive symptoms, between 20 and 28 indicates a moderate level of depressive symptoms, and between 26 and 63 indicates a severe level of depressive symptoms. The original scale had good convergent validity and discriminant validity, and the Cronbach’s α was from 0.86 to 0.88 [27]. The Chinese version of the BDI-II had an adequate internal consistency when tested in patients with end-stage renal disease (Cronbach’s α = .82) [28]. In this study, the Cronbach’s α was 0.95.
Heart failure symptom distress scale
Based on guidelines for the management of HF developed by the American College of Cardiology Foundation (ACCF) and the American Heart Association (AHA) as well as other studies [29–32], we designed a Heart Failure Symptom Distress Scale (HFSDS) to evaluate patient’s symptom distress resulting from HF. The HFSDS assesses 17 symptoms of HF: fatigue, weakness, head heavy, dyspnea on rapid exertion, weight gain, dry cough, swelling in the legs or ankles, orthopnea, palpitations, dizziness, syncope, memory decline, chest pain, insomnia, nausea, poor appetite and inability to concentrate. Responses to the items are rated on 6-point Likert scale from 0 = "no suffering from symptoms" to 5 = "severe suffering from symptoms". A higher score reflects greater symptom distress. In this study, the content validity index was 0.98 evaluated by five cardiovascular disease experts, and the Cronbach’s α for the total scale was 0.92.
Social support scale
Social support was measured by the Social Support Scale (SSS), which was modified from the Inventory of Social Support Behaviors by the authors [33]. SSS is a 19-item self-report scale rated with a 4-point Likert-type format. It contains four subscales: emotional support, informational support, instrumental support, and appraisal support. A higher the score indicates a greater perception of available support. Five experts proficient in cardiology examined the content validity of the SSS. The content validity index for the total scale was 0.91. The Cronbach’s α for the total scale was 0.96, and for the emotional support subscale, informational support subscale, instrumental support subscale, and appraisal support subscale was 0.94, 0.83, 0.92, and 0.92, respectively [34].
Minnesota living with heart failure questionnaire
Participants’ HRQoL was measured with the Chinese version of the Minnesota Living with Heart Failure Questionnaire (MLHFQ), which is a 21-item scale to assess patient’s perception of the impact of HF on the physical, psychological, and socioeconomic aspects of their life. The MLHFQ is a 6-point Likert scale from 0 to 5. A higher score reflects a worse HRQoL. The Chinese version of the MLHFQ has been identified to have appropriate construct validity and internal consistency reliability. Cronbach’s α for the total scale was 0.94 [35]. In this study, the Cronbach’s α for the total scale was 0.95.
Statistical analysis
Data were analyzed with the SPSS 18.0 and AMOS 8.0 statistical software packages. We analyzed demographic and health characteristics of participants through using the mean, standard deviation (SD), frequency and percentage. AMOS was used for SEM analysis. Left ventricular ejection fraction (LVEF), NYHA Class, education, symptom distress, social support and depressive symptoms were set as measured variables, while uncertainty in illness and HRQoL were set as latent variables. Modification indices (Wald test) were used to find a parsimonious model [36]. Goodness-of-fit tests were used to examine whether the research model fit well. The fit of the model was determined by using several methods including normalized Chi-square < 3 [37], goodness-of-fit index (GFI)>0.90, adjusted goodness-of-fit index (AGFI)>0.90 [38], comparative fit index (CFI)> 0.90 [39], and root mean squares error of approximation (RMSEA)<0.1 [40]. Furthermore, Sobel’s test was applied to identify whether both uncertainty and depressive symptoms were mediators. If we obtained a Z-value> 1.96, then the mediating effect was considered significant [41].
Results
Participant characteristics
A total of 147 HF patients participated in this study (male = 80, female = 67). The mean age was 71±13.29 years. Most of participants had completed elementary school (41%), and were unemployed (76.9%) and married (76.2%). Seventy participants were outpatients (47.6%) and 77 were inpatients (52.4%). Participants’ mean LVEF was 46.42% (SD = 17.20, range 10-80). Most proportion of the participants were in NYHA Class II (32.0%), followed by 31.3% in class III, 7.7% in Class IV and 9.5% in Class I. Participants’ characteristics are shown in (Table 1)。<}0{>SSSS outpatients (47.6%) and 77 were inpatients (52.4%). Participants’ mean LVEF was 46.42% (SD = 17.20, range 10–80). Most proportion of the participants were in NYHA Class II (32.0%), followed by 31.3% in class III, 7.7% in Class IV and 9.5% in Class I. Participants’ characteristics are shown in Table 1.
Table 1. Characteristics of participants (N = 147).
| Variable | n (%) | Mean (SD) |
|---|---|---|
| Age | 71.04 (13.29) | |
| Gender | ||
| Male | 80 (54.4%) | |
| Female | 67 (45.6%) | |
| Employment status | ||
| Unemployed | 113 (76.9%) | |
| Employed | 34 (23.1%) | |
| Education | ||
| None | 23 (15.6%) | |
| Elementary school | 60 (40.8%) | |
| Junior high school | 28 (19.2%) | |
| Senior high school | 22 (15.0%) | |
| University/college degree | 11 (7.5%) | |
| Master degree | 3 (2.0%) | |
| Marital status | ||
| Not married | 6 (4.1%) | |
| Married | 12 (76.2%) | |
| Divorced | 2 (1.4%) | |
| Widow | 25 (17.0%) | |
| Separated | 2 (1.4%) | |
| Treatment | ||
| Outpatient | 70(47.6%) | |
| Inpatient | 77(52.4%) | |
| NYHA Class | ||
| Class Ι | 14 (9.5%) | |
| Class Ⅱ | 47 (32.0%) | |
| Class Ⅲ | 46 (31.3%) | |
| Class Ⅵ | 40 (27.2%) | |
| Left ventricle ejection fraction | 46.42 (17.20) | |
| Comorbidities | ||
| Diabetes | 55(37.4%) | |
| Renal disease | 23(15.6%) | |
| Chronic obstructive pulmonary disease | 23(15.6%) |
Note: SD, Standard deviation; NYHA Class, New York Heart Association Functional Classification
Descriptive statistics of the measures
The mean, standard deviation, and score range of measures are presented in Table 2. The mean score of the HFSDS reported by the participants was 25.0 (SD = 13.25), indicating that participants had a low level of distress from disease symptoms. The highest distress mean scores among symptoms were for dyspnea on exertion (mean = 3.88, SD = 1.30), dyspnea while lying down (mean = 2.78, SD = 1.84) and sudden awaking due to dyspnea while sleeping (mean = 2.72, SD = 1.86). The mean score for the MUIS was 73.5 (SD = 18.55), indicating that participants had a moderate level of uncertainty in illness. The highest subscale score was unpredictability (mean = 52.06, SD = 13.73). The mean score of the SSS was 54.49 (SD = 11.51), suggesting that participants perceived a moderate level of social support. The highest subscale score was emotional support (mean = 16.03, SD = 3.05). The mean score of BDI-II was 19.42 (SD = 11.29), meaning that the participants had mild depressive symptoms. The mean score of the MLHFQ for participants was 54.41 (SD = 21.24), suggesting that participants had poor quality of life. The highest mean score between two domains was physical domain (mean = 25.44, SD = 11.30), indicating that participants perceived more impact from HF on the physical domain than on the psychosocial domain.
Table 2. Scores of measurements.
| Measurements | Mean (SD) | Range |
|---|---|---|
| Heart Failure Symptom Distress Scale | 25.03 (13.25) | 0–85 |
| Mishel Uncertainty in Illness Scale | ||
| Total score | 73.51 (18.55) | 25–125 |
| Unpredictability subscale score | 52.06 (13.73) | 15–75 |
| Multi-attributed ambiguity subscale score | 52.06 (13.73) | 10–50 |
| Social Support Scale | ||
| Total score | 54.14 (11.31) | 19–76 |
| Emotional support subscale score | 13.58 (3.65) | 5–20 |
| Information support subscale score | 16.03 (3.05) | 6–24 |
| Instrumental support subscale score | 12.88 (3.08) | 4–16 |
| Appraisal support subscale score | 11.65 (2.89) | 4–16 |
| BDI-Π | 19.42 (11.29) | 0–63 |
| MLHFQ | 54.41 (21.24) | 0–105 |
Note: SD, standard deviation; BDI-II, Beck Depression Inventory: Second Edition; MLHFQ, Minnesota living with heart failure questionnaire
Model testing and mediation model analysis
Our original model, based on Mishel's UIT, set the measured variables as education, NYHA class, LVEF, symptom distress, emotional support, and depressive symptoms. Uncertainty in illness and HRQoL were the latent variables. The original model had good fit indexes of χ2/df = 2.44, GFI = 0.92, AGFI = 0.84, CFI = 0.96, RMSEA = 0.10. However, the path coefficients between LVEF, NYHA class, education, and uncertainty were not significant (Table 3)(Fig 2). Therefore, we removed NYHA class, based on modification indexes. The modified model had better fitness indexes: χ2/df = 2.60, GFI = 0.93, AGFI = 0.85, CFI = 0.96, and RMSEA = 0.10 (Table 3) (Fig 3). Fifty-six percent of the variance in participants’ uncertainty was explained by symptom distress, emotional support and depressive symptoms. Eighty-nine percent of the variance in participants’ HRQoL was explained by symptom distress, emotional support, uncertainty and depressive symptoms. The results of Sobel's test showed that both uncertainty (Z value = 3.12; p value < 0.01) and depressive symptoms (Z value = 2.38; p value < 0.01) were mediators between symptom distress and HRQoL. In addition, the variable of depressive symptoms was also a mediator between emotional support and HRQoL (Z value = -2.25; p value < 0.01).
Table 3. The model fit indexes of structural equation models.
| Model Fit Indexes | |||||||
|---|---|---|---|---|---|---|---|
| Model | χ2 | df | χ2/df | GFI | AGFI | CFI | RMSEA |
| Original | 68.42 | 28 | 2.44 | 0.92 | 0.84 | 0.96 | 0.10 |
| Modified | 54.74 | 21 | 2.61 | 0.93 | 0.85 | 0.96 | 0.10 |
Note: χ2, Chi-square test value; df, degrees of freedom; GFI, goodness-of-fit index; AGFI, adjusted goodness-of- fit index; CFI, comparative fit index; RMSEA, root mean squares error of approximation.
Fig 2. The original model.

The original model of uncertainty to predict HRQoL for heart failure patients. NYHA, New York Heart Association functional class, EF, ejection fraction. *p-value < 0.05, **p-value<0.01, ***p-value < 0.001.
Fig 3. The modified model.
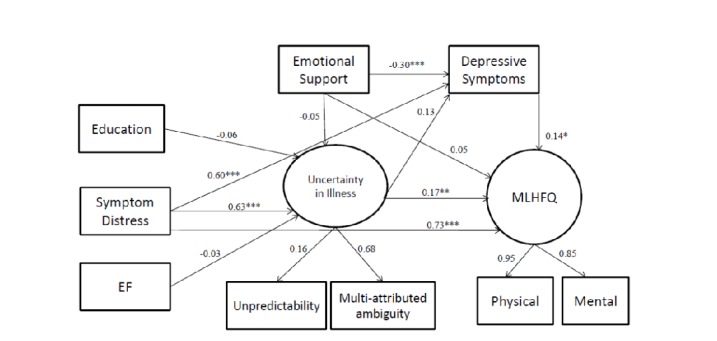
The modified model of uncertainty to predict HRQoL for heart failure patients. *p-value < 0.05, **p-value<0.01, ***p-value < 0.001.
Symptom distress had direct effects on uncertainty (β = 0.63, p < .001), depressive symptoms (β = 0.60, p < .001) and HRQoL (β = 0.73, p < .001) as well as indirect effects on HRQoL through uncertainty and depressive symptoms. Emotional support had direct effects on depressive symptoms (β = -0.30, p < .001), as well as indirect effects on HRQoL through depressive symptoms. The model in our study expressed more HF symptoms led to more uncertainty and depressive symptoms, which further bring about worse HRQoL. Otherwise, higher social support resulted in less depressive symptoms and then led to better HRQoL. The total, direct and indirect effects were shown in Table 4.
Table 4. Direct, indirect and total effects.
| Uncertainty | Depressive symptoms | HRQoL | |||||||
|---|---|---|---|---|---|---|---|---|---|
| IE | DE | TE | IE | DE | TE | IE | DE | TE | |
| Symptom distress | - | .63*** | .63*** | .08 | .60*** | .68 | 0.11*** | .73*** | .83 |
| Emotional support | - | -.05 | -.05 | - | -.30*** | -.30*** | - | .05 | .05 |
| Uncertainty | - | - | - | - | .13 | .13 | - | .17** | .17** |
| Depressive symptoms | - | - | - | - | - | - | - | .14* | .14* |
Note: HRQoL, Health related quality of life; IE, Indirect Effect; DE, Direct Effect; TE, Total Effect
*p-value < 0.05
**p-value<0.01
***p-value < 0.001
Discussion
The causal mechanism between symptom distress, uncertainty, depressive symptoms and HRQoL is rarely determined in patients with HF. The purpose of this study was to examine whether uncertainty and depressive symptoms are able to influence the relationship between symptom distress and HRQoL. Therefore, we conducted structural equation modeling analyses to test three hypotheses: (1) symptom distress, uncertainty, depressive symptoms and HRQoL were closely correlated in the structural equation model; (2) symptom distress showed a significant positive correlation with uncertainty and depressive symptoms, and a significant negative relationship with HRQoL, as well as an indirect influence on HRQoL through uncertainty and depressive symptoms; and (3) uncertainty and depressive symptoms mediated the relationship between symptom distress and HRQoL in HF patients.
The study results supported the first and second hypotheses. The symptom distress was significantly positively related to uncertainty and depressive symptoms, and negatively associated with HRQoL in patients with HF. Again, the symptom distress was able to indirectly influence HRQoL through uncertainty and depressive symptoms. The results are similar to the findings of a previous study showing that HF patients had moderate uncertainty (mean = 71.41, SD = 9.56) due to complex symptoms [42]. In the research of Kang also pointed out that atrial fibrillation patients with greater symptoms had more uncertainty (β = 0.21, p < 0.05) [43]. Bailey et al. [44] conducted a cross-sectional study in chronic Hepatitis C patients and showed that uncertainty was negatively associated with HRQoL. Because HF comprises a series of complex clinical symptoms, the symptoms are not only difficult to be treated, but also interfere with patients’ physical, psychological and social functions, and even HRQoL [45].
Our study also found that approximately 65.3% of HF patients scored over 13 on the BDI-II. This finding indicates that most HF patients had depressive symptoms, which is similar to a study showing 50% of HF patients suffer from depressive symptoms [22]. The findings of our study also show a positive relationship between symptom distress and depressive symptoms; indicating that patients with fewer symptoms had less depressive symptoms in our study. The findings are consistent with previous studies revealing a positive relationship between symptom distress and depressive symptoms [19,46]. Depressive symptoms are also a significant predictor of HRQoL in patients with HF [23,24]. In our study, a positive relationship between the score of BDI-II and the score of MLHFQ was detected. The outcomes in our study mean that patients with more depressive symptoms had a poor HRQoL. The HF patients with depressive symptoms have a poor adherence to medical treatments and healthy lifestyle, which lead to a decline in health status and affected their HRQOL [23,24, 46].
We also found a negative association between emotional support and depressive symptoms. This result is consistent with prior studies showing that HF patients with better emotional support had lower degree of depression. Social support is a buffering factor that can defend against such harmful events from HF or its treatments [47,48].
We found a mediator effect of uncertainty in the relationship between symptom distress and HRQoL. Mishel (1988) believed that uncertainty was generated when individuals were unclear about the disease treatment and outcome, and could not engage in proper sorting or compiling of information [49]. HF patients often face a load of symptoms such as fatigue, breathlessness, and functional impairment [19,50]. When the patient lacks information about the disease and feels a loss of control over the disease, uncertainty tends to increase as a result of its complex nature [12,43]. Jiang et al. exposed that uncertainty management intervention has a definite effect on decreasing emotional symptoms and improving HRQoL in chronic obstructive pulmonary disease patients [51]. The results showed that patients received uncertainty management intervention had significant lower degree of uncertainty than that of patients without receiving intervention. Again, the decrease of uncertainty resulted in the improvement of emotional symptoms and HRQoL [51].
Our findings demonstrated depressive symptom was the mediator between symptom distress and HRQoL, and also the mediator between emotional support and HRQoL. Hallas et al. indicated that HF patients with depression have more negative beliefs about their disease and more negative coping behaviors to cause poor quality of life [52]. Depressive symptoms will adversely influence HF patients’ adherence to the treatment regimen [46, 53]. The consequence will impair patients’ physical functioning, increase symptom distress, and worse HRQoL [8, 54]. Noroozi et al. reported the effectiveness of group cognitive behavior therapy on depression and quality of life in women with Type 2 diabetes [55]. They found that patients receiving cognitive behavior therapy had significant improvement on depression and HRQoL than those of the patients without receiving this intervention. Hence, the reduction of depression led to the improvement of mental condition and HRQoL [55].
Limitations
This study had some limitations. First, this was a cross-sectional design; a future study using a longitudinal research design is recommended to fully understand changes in patient's uncertainty in illness and quality of life on the whole course of a disease. Second, we only recruited patients from one medical center, which limits generalization of the findings. Future research should be conducted in multiple centers to make the research findings more representative of a larger population. Finally, our study framework is to take the educational level of the study subjects as the “cognitive capacity” mentioned in the theory of uncertainty in illness. We did not use additional questionnaires to test the cognitive capacity of the study subjects. We suggest that if future studies are based on Mishel’s theory of uncertainty in illness, a cognitive capacity test could be added in the cognitive capacity section of the theory.
Conclusions and implications
This study is the first study based on the Mishel’s UIT to indicate the mediation effect of uncertainty and depressive symptoms on the relationship between symptom distress and HRQoL in HF patients. These findings suggest that decreasing uncertainty and depressive symptoms could enhance HF patients’ HRQoL. Based on Mishel’s UIT, nurses and healthcare professionals should design systematic interventions to help HF patients control disease symptoms, alleviate or reduce uncertainty and depression, and improve their HRQoL.
Supporting information
(PDF)
Acknowledgments
The authors wish to express their most sincere appreciation to all participants in this study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014; 129: e28–e292. 10.1161/01.cir.0000441139.02102.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reyes EB, Ha JW, Firdaus I, Ghazi AM, Phrommintikul A, Sim D, et al. Heart failure across Asia: Same healthcare burden but differences in organization of care. Int J Cardiol. 2016; 223: 163–167. 10.1016/j.ijcard.2016.07.256 [DOI] [PubMed] [Google Scholar]
- 3.Huang TY, Moser DK, Hwang SL, Lennie TA, Chung M, Heo S. Comparison of Health-related Quality of Life between American and Taiwanese Heart Failure Patient. J of Trans Nurs. 2010; 21: 212–219. 10.1177/1043659609358779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-service program. N Engl J Med. 2009; 360:1418–1428. 10.1056/NEJMsa0803563 [DOI] [PubMed] [Google Scholar]
- 5.Buck HG, Lee CS, Moser DK, Albert NM, Lennie T, Bentley B, et al. Relationship between self-care and health-related quality of life in older adults with moderate to advanced heart failure. J Cardiovasc Nurs. 2012; 27: 8–15. 10.1097/JCN.0b013e3182106299 [DOI] [PubMed] [Google Scholar]
- 6.Bosworth HB, Steinhauser KE, Orr M, Lindquist JH, Grambow SC, Oddone EZ. Congestive heart failure patients' perceptions of quality of life: The integration of physical and psychosocial factors. Aging Ment Health. 2004; 8: 83–91. 10.1080/13607860310001613374 [DOI] [PubMed] [Google Scholar]
- 7.Falk K, Swedberg K, Gaston-Johansson F, Ekman I. Fatigue is a prevalent and severe symptom associated with uncertainty and sense of coherence in patients with chronic heart failure. Eur J Cardiovasc Nurs. 2007; 6: 99–104. 10.1016/j.ejcnurse.2006.05.004 . [DOI] [PubMed] [Google Scholar]
- 8.Moraska AR, Chamberlain AM, Shah ND, Vickers KS, Rummans TA, Dunlay SM, et al. Depression, Healthcare Utilization, and death in heart failure: A community study. Circ Heart Fail. 2013; 6: 387–394. 10.1161/CIRCHEARTFAILURE.112.000118 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mishel MH. Uncertainty in chronic illness. Annu Rev Nurs Resv. 1999; 17: 269–294. [PubMed] [Google Scholar]
- 10.Padilla GV, Mishel MH, Grant MM. Uncertainty, appraisal, and quality of life. Qual Life Res. 1992; 1: 155–165. [DOI] [PubMed] [Google Scholar]
- 11.McCormick KM, McClement S, Naimark BJ. A qualitative analysis of the experience of uncertainty while awaiting coronary artery bypass surgery. Can J Cardiovasc Nurs. 2005; 15: 10–22. [PubMed] [Google Scholar]
- 12.Eastwood JA, Doering L, Roper J, Hays RD. Uncertainty and Health-related quality of life 1 year after coronary angiography. Am J Crit Care. 2008; 17: 232–242. [PubMed] [Google Scholar]
- 13.Flemme I, Edvardsson N, Hinic H, Jinhage BM, Dalman M, Fridlund B. Long-term quality of life and uncertainty in patients living with an implantable cardioverter defibrillator. Heart Lung. 2005; 34: 386–392. 10.1016/j.hrtlng.2005.05.003 [DOI] [PubMed] [Google Scholar]
- 14.Mishel MH., Clayton MF. Theories of Uncertainty in Illness In: Smith MJ., Liehr PR, editors. Middle Range Theory of Nursing. Springer; 2008. pp. 55–84. [Google Scholar]
- 15.Mishel MH. The measurement of uncertainty in illness. Nurs Res. 1981; 30: 258–263. [PubMed] [Google Scholar]
- 16.Falk K, Patel H, Swedberg K, Ekman I. Fatigue in patients with chronic heart failure- a burden associated with emotional and symptom distress. Eur J Cardiovasc Nurs. 2008; 8: 91–96. 10.1016/j.ejcnurse.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 17.Song EK, Moser DK, Rayens MK, Lennie TA. Symptom clusters predict event-free survival in patients with heart failure. J Cardiovasc Nurs. 2101; 25: 284–291. 10.1097/JCN.0b013e3181cfbcbb . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bekelman DB, Havranek EP, Becker DM, Kutner JS, Peterson PN, Wittstein IS, et al. Symptoms, depression, and quality of life in patients with heart failure. J Card Fail. 2007; 13: 643–648. 10.1016/j.cardfail.2007.05.005 . [DOI] [PubMed] [Google Scholar]
- 19.Herr JK, Salyer J, Lyon DE, Goodloe L, Schubert C, Clement DG. Heart failure symptom relationships: a systematic review. J Cardiovasc Nurs. 2014; 29: 416–422. 10.1097/JCN.0b013e31829b675e [DOI] [PubMed] [Google Scholar]
- 20.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006; 48: 1527–1537. 10.1016/j.jacc.2006.06.055 [DOI] [PubMed] [Google Scholar]
- 21.Sokoreli I, de Vries JJ, Pauws SC, Steyerberg EW. Depression and anxiety as predictors of mortality among heart failure patients: systematic review and meta-analysis. Heart Fail Rev. 2016; 21: 49–63. 10.1007/s10741-015-9517-4 [DOI] [PubMed] [Google Scholar]
- 22.Aggelopoulou Z, Fotos NV, Chatziefstratiou AA, Giakoumidakis K, Elefsiniotis I, Brokalaki H. The level of anxiety, depression and quality of life among patients with heart failure in Greece. Appl Nurs Res. 2017; 34: 52–56. 10.1016/j.apnr.2017.01.003 [DOI] [PubMed] [Google Scholar]
- 23.Ege MR, Yılmaz N, Yılmaz MB. Depression and perceptions about heart failure predict quality of life. Heart Lung. 2011; 40: 111–121. 10.1016/j.hrtlng.2009.12.008 [DOI] [PubMed] [Google Scholar]
- 24.Loo DW, Jiang Y, Koh KW, Lim FP, Wang W. Self-efficacy and depression predicting the health-related quality of life of outpatients with chronic heart failure in Singapore. Appl Nurs Res. 2016; 32: 148–155. 10.1016/j.apnr.2016.07.007 [DOI] [PubMed] [Google Scholar]
- 25.Erdfelder E, Faul F, Buchner A. G POWER: A general power analysis program. Behav Res Methods Instrum Comput. 1996; 28: 1–11. [Google Scholar]
- 26.Sheu S, Hwang SL. Validation of Chinese Version of Mishel's Uncertainty in Illness Scale. J Nurs Res. 1996; 4:59–67. [Google Scholar]
- 27.Beck AT, Steer RA, Brown GK. BDI-II, Beck depression inventory: manual San Antonio: The Psychological Corporation; 1996. [Google Scholar]
- 28.Cho YC, Tsay SL. The effect of acupressure with massage on fatigue and depression in patients with end-stage renal disease. J Nurs Res. 2004; 12: 51–59. [DOI] [PubMed] [Google Scholar]
- 29.Carlson B, Riegel B, Moser DK. Self-care abilities of patients with heart failure. Heart Lung. 2001; 30: 351–359. 10.1067/mhl.2001.118611 [DOI] [PubMed] [Google Scholar]
- 30.Goodlin SJ, Hauptman PJ, Arnold R, Grady K, Hershberger RE, Kutner J, et al. Consensus statement: Palliative and supportive care in advanced heart failure. J Card Fail. 2004; 10: 200–209. [DOI] [PubMed] [Google Scholar]
- 31.Oliva AP, Monteiro da Cruz Dde A. Decreased cardiac output validation with postoperative heart surgery patients. Dimens Crit Care Nurs. 2003; 22: 39–44. . [DOI] [PubMed] [Google Scholar]
- 32.Rasmusson KD, Hall JA, Renlund DG. Heart failure epidemic: Boiling to the surface. Nurse Pract. 2006; 31; 12–21. [DOI] [PubMed] [Google Scholar]
- 33.Barrera M, Sandler IN, Ramsy TB. Preliminary development of a scale of social support: Studies on college students. Am J Community Psychol. 1981; 9: 435–447. [Google Scholar]
- 34.Kao CW, Chen TY, Cheng SM, Lin WS, Friedmann E, Thomas SA. Gender differences in the predictors of depression among patients with heart failure. Eur J Cardiovasc Nurs. 2014; 13:320–328. 10.1177/1474515113496493 [DOI] [PubMed] [Google Scholar]
- 35.Heo S, Moser DK, Riegel B, Hall LA, Christman N. Testing the psychometric properties of the Minnesota Living with Heart Failure Questionnaire. Nurs Res. 2005; 54: 265–272. [DOI] [PubMed] [Google Scholar]
- 36.Sörbom D. Model modification. Psychometrika. 1989; 54: 371–384. [Google Scholar]
- 37.Bagozzi RP, Yi Y. On the evaluation for structural equation models. JAMS. 1988; 16: 74–94. [Google Scholar]
- 38.Shevlin M, Miles JNV. Effects of sample size, model specification and factor loadings on the GFI in confirmatory factor analysis. Pers Indiv Differ. 1998; 25: 85–90. 10.1016/S0191-8869(98)00055-5 [DOI] [Google Scholar]
- 39.Bentler PM. Comparative fit index in structural models. Psychol Bull. 1990; 107: 238–246. [DOI] [PubMed] [Google Scholar]
- 40.MacCallum RC, Browne MW, Sugawara HM. Power Analysis and Determination of Sample Size for Covariance Structure Modeling. Psychol Methods. 1996; 1:130–149. 10.1037/1082-989X.1.2.130 [DOI] [Google Scholar]
- 41.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instruments Comput. 2004; 36: 717–731. [DOI] [PubMed] [Google Scholar]
- 42.Jurgens CY. Somatic awareness, uncertainty, and delay in care-seeking in acute heart failure. Res Nurs Health. 2006; 29: 74–86. 10.1002/nur.20118 [DOI] [PubMed] [Google Scholar]
- 43.Kang Y. The relationships between uncertainty and its antecedents in Korean patients with atrial fibrillation. J Clin Nurs. 2011; 20: 1880–1886. 10.1111/j.1365-2702.2010.03416.x [DOI] [PubMed] [Google Scholar]
- 44.Bailey DE Jr, Landerman L, Barroso J, Bixby P, Mishel MH, Muir AJ, et al. Uncertainty, symptoms, and quality of life in persons with chronic hepatitis C. Psychosomatics. 2009;50:138–146. 10.1176/appi.psy.50.2.138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heo S, Lennie TA, Moser DK, Kennedy RL. Types of social support and their relationships to physical and depressive symptoms and health-related quality of life in patients with heart failure. Heart Lung. 2014; 43: 299–305. 10.1016/j.hrtlng.2014.04.015 [DOI] [PubMed] [Google Scholar]
- 46.Luyster FS, Hughes JW, Gunstad J. Depression and anxiety symptoms are associated with reduced dietary adherence in heart failure patients treated with an implantable cardioverter defibrillator. J Cardiovasc Nurs. 2009; 24:10–17. 10.1097/01.JCN.0000317469.63886.24 [DOI] [PubMed] [Google Scholar]
- 47.Chung ML, Moser DK, Lennie TA, Frazier SK. Perceived social support predicted quality of life in patients with heart failure, but the effect is mediated by depressive symptoms. Qual Life Res. 2013; 22: 1555–1563. 10.1007/s11136-012-0294-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Graven LJ, Grant J. The impact of social support on depressive symptoms in individuals with heart failure: update and review. J Cardiovasc Nurs. 2013; 28: 429–443. 10.1097/JCN.0b013e3182578b9d [DOI] [PubMed] [Google Scholar]
- 49.Mishel MH. Uncertainty in illness. J Nurs Scholarship. 1988; 20: 225–232. 10.1111/j.1547-5069.1988.tb00082.x [DOI] [PubMed] [Google Scholar]
- 50.Chu SH, Lee WH, Yoo JS, Kim SS, Ko IS, Oh EG, et al. Factors affecting quality of life in Korean patients with chronic heart failure. Jpn J Nurs Sci. 2014;11:54–64. 10.1111/jjns.12002 [DOI] [PubMed] [Google Scholar]
- 51.Jiang X, He G. Effects of an uncertainty management intervention on uncertainty, anxiety, depression, and quality of life of chronic obstructive pulmonary disease outpatients. Res Nurs Health. 2012; 35: 409–418. 10.1002/nur.21483 [DOI] [PubMed] [Google Scholar]
- 52.Hallas CN, Wray J, Andreou P, Banner NR. Depression and perceptions about heart failure predict quality of life in patients with advanced heart failure. Heart Lung. 2011; 40: 111–121. 10.1016/j.hrtlng.2009.12.008 [DOI] [PubMed] [Google Scholar]
- 53.Corotto PS, McCarey MM, Adams S, Khazanie P, Whellan DJ. Heart failure patient adherence: epidemiology, cause, and treatment. Heart Fail Clin. 2013; 9: 49–58. 10.1016/j.hfc.2012.09.004 [DOI] [PubMed] [Google Scholar]
- 54.Samartzis L, Dimopoulos S, Tziongourou M, Nanas S. Effect of psychosocial interventions on quality of life in patients with chronic heart failure: a meta-analysis of randomized controlled trials. J Card Fail. 2013; 19: 125–134. 10.1016/j.cardfail.2012.12.004 [DOI] [PubMed] [Google Scholar]
- 55.Noroozi Z, Hamidian S, Khajeddin N, Mehrabi Zadeh Honarmand M, Zargar Y, Rashidi H, et al. Improving Depression, and Quality of Life in Patients with Type 2 Diabetes: Using Group Cognitive Behavior Therapy. Iran J Psychiatry. 2017; 12: 281–286. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.


