Abstract
Background/Objective
Older adults frequently use the emergency department (ED) for care, but the ED-to-home transition often goes poorly, with up to 20% experiencing adverse outcomes, including return to the ED for further care. We describe a novel model of care that uses community-based paramedics to deliver a modified version of the evidence-based hospital-to-home Care Transitions Intervention (CTI) to a new context: the ED-to-home transition.
Design
Single blinded randomized controlled trial.
Setting
Three EDs in two cities.
Participants
Through June 2017, 422 patients discharged home from the EDs who were consented and randomized to receive the modified CTI.
Intervention
We modified the hospital-to-home CTI, applying it to the ED-to-home transition and delivering services through community paramedics, thus allowing the program to benefit from the unique attributes of paramedics to deliver care.
Measurements
Through surveys of participants, medical record review, and documentation of activities by CTI coaches, we characterize the participants and program, including feasibility and acceptability.
Results
The median age of patient participants was 70.7 years; 241 (57.1%) subjects were female; and 385 (91.2%) were white. Coaches successfully completed 354 (83.9%) home visits and 92.7%, 90.9%, and 85.8% of planned telephone follow-up for call 1, 2, and 3, respectively. We found high levels of acceptability among participants, with most patients (76.2%) and caregivers (83.1%) reporting themselves likely or extremely likely to choose an ED featuring the CTI Program in the future. Coaches reported delivering expected services during patient contact at least 88% of the time.
Conclusion
While finalized conclusions about program effectiveness must await the results of the randomized controlled trial, the findings reported here are promising and provide preliminary support for an ED-to-home CTI Program’s ability to improve patient outcomes. The coaches’ identity as community paramedics is particularly noteworthy, as this is a unique role for this provider type.
Keywords: Care transitions, community paramedicine, emergency department, older adults
INTRODUCTION
The emergency department (ED) is a crucial source of care for the 43.3 million older adults living in the United States.1 In 2013, older adults made 20.8 million ED visits, with the majority being discharged home.2 Unfortunately, the ED-to-home transition is frequently associated with adverse events. Studies have demonstrated that within 30 days of an ED visit, up to 20% of older adults require further ED care, experience hospitalization or nursing home placement, or die.3,4,5,6,7,8,9,10
Sub-optimal care transition quality is one critical factor that likely contributes to these poor outcomes. The discharge process often fails to ensure that patients leaving the ED understand essential next steps such managing medications, obtaining follow-up care, and identifying warning-sign symptoms requiring immediate medical attention. Although the ED discharge process does deliver verbal and written instructions to patients pertaining to these issues, it lasts on average only four minutes.11 Not surprisingly, comprehension is deficient in 78% of patients, regardless of age.12 As few as 32% of ED patients follow up with their primary care physician (PCP) in the 30 days following discharge.13,14
Interventions to improve the transition include telephone follow-up, discharge planning, case management, and comprehensive assessments, but few have demonstrated a consistent and statistically significant benefit. 13,15,16,17,18,19 Furthermore, those interventions with benefit are difficult to implement without interfering with care processes in the time-pressured ED, limiting the ability for widespread uptake and sustainability.
We describe an innovative approach to improve the ED-to-home transition. By modifying the Care Transitions Intervention (CTI), an evidence-based, commonly used hospital-to-home transitions program, to the ED-to-home context, we sought to improve this transition for older adults.20,21 Using paramedics to serve as coaches who deliver the CTI, leverages unique features of this type of care provider such as wide availability, advanced training, and community respect. We outline our modified ED-to-home CTI Program and describe its feasibility, acceptability, and ability to support older adults experiencing the ED-to-home care transition. We conclude by discussing lessons learned from this intervention.
MODEL OF CARE
Program Setting and Research Context
We implemented the ED-to-home CTI Program in Dane County, WI, and Monroe County, NY, in the context of a randomized controlled trial evaluating its effectiveness. The study began in January 2016 in Monroe County (two EDs), and February 2016 in Dane County (one ED), and will continue through 2019.
In the trial, ED patients age≥60 years receiving discharge home are approached and, if consenting to participate, randomized to the CTI Program or usual care. The key investigators are blinded to whether patients receive the intervention. Staff are blinded unless patients reveal whether they received coaching. A single informal caregiver per patient who is present may participate. We survey all patient participants in the ED (demographic and clinical characteristics), and 4 and 30 days after discharge (health utilization and opinions). We survey caregiver subjects in the ED (demographics) and 30 days after discharge (opinions). Additionally, we review medical records for patient subjects to measure health care use. Participants do not have to arrive at the ED via the ambulance-based emergency medical services (EMS) system. Thus, while possible that the paramedics provide EMS services in the context of a 911 call for control group patients, it is unlikely due to the large number of paramedics in the affiliated program agencies. The University of Wisconsin and University of Rochester Institutional Review Boards approved the study with written informed consent.
A Pragmatic Application of the CTI to the ED-to-Home Context
The hospital-to-home CTI Program is a four-week program supporting patients discharged from the hospital, with a trained “coach” providing one in-person visit in the hospital prior to discharge, one in-person home visit, and up to three phone calls.21 During these encounters, the coach uses motivational interviewing techniques, behavior modelling, skill transfer, and role playing to improve self-management. Key areas of focus include ensuring effective medication management, PCP follow-up, red flags awareness, and maintenance of a personal health record. Of note, coaches do not deliver services (e.g., make appointments). We made two changes to the CTI, driven by pragmatic considerations described below. By retaining other CTI features we pursued a balance between modifications necessary for success in the ED-to-home transition and preservation of characteristics of the validated CTI.
Through discussions among members of the research team, which includes CTI experts, geriatricians, emergency physicians, EMS physicians, and paramedics, we first determined that the in-person coach visit in the ED would be impractical. Therefore, we briefly introduce the program in the ED as part of obtaining consent, and schedule a home visit to occur rapidly following ED discharge, ideally within 48 hours.
Second, we centered program delivery on paramedics instead of nurses, as used in the original validation.20 Paramedics were chosen because, if implemented broadly, an ED-to-home CTI program would require home visits to occur in urban, suburban, and rural communities, on any day of the week. The wide availability of the EMS system fits such demanding requirements. The national movement to leverage the EMS-system and paramedics to improve community health, known as community paramedicine, has led to many EMS agencies displaying interest in such activities.22 Accordingly, we work with the Madison Fire Department in Dane County and CHS Mobile Integrated Healthcare in Monroe County to supply and manage the program’s community paramedic coaches.
EMS providers possess certifications at different levels. For this program, we chose to use paramedics, as they require the greatest training (approximately 1,500 hours) to achieve certification. We considered EMS providers with other certifications, but decided to include staff with a greater depth of healthcare experience and training. In this first study, paramedics at either agency were able to apply to participate. Agency leadership and research staff interviewed applicants and chose a team of four in each city to receive training and serve as community paramedic coaches.
Community Paramedic Coach Training
The CTI requires that paramedics shift from solving problems (e.g., when the patient is not breathing, intubate the patient) to coaching. Thus, we provided specific training to reinforce the knowledge, skills, and attitudes necessary for successful coaching through a curriculum for participating community paramedics (Table 1). Because we used paramedics, we did not feel the need to provide medical education other than in aging-specific topics. We required coaches to complete readings, video podcasts, and experiences such as CTI coach, emergency physician, and geriatrician shadowing, simulation, and mentored coaching, in addition to the standard in-person CTI training by the Care Transitions Program (University of Colorado-Denver, Aurora, Colorado).23 An evaluation of this training program has been published.24 We also provided continuing education through regular review sessions that discussed patients and challenges that coaches encountered and annual trainings from the Care Transitions Program to reinforce concepts.
Table 1.
Community Paramedic Coach Training Curriculum
| Topic | Time | Resources |
|---|---|---|
| Care Transitions Intervention | 10–12 hours | Care Transitions Program®
|
| 1 day + travel | Onsite training at the University of Colorado: https://caretransitions.org/about-our-training/ | |
| Coaching | 10–15 hours | Motivational interviewing training and mentored coaching training
|
| Geriatrics | 4 hours | Readings on caring for older patients |
| Video podcasts on caring for older adults to better understand clinical issues faced by older patients | ||
| 6 hours | Geriatrician shadowing to understand clinical issues faced by older patients and to obtain education on key aging concepts such as delirium and dementia | |
| ED Discharge Process | 6 hours | Shadowing an ED physician and patient to particularly observe ED discharge processes |
| 2 hours | Readings on failures of the ED discharge process to understand patients’ challenges resulting from the discharge process | |
| Review of patient discharge handouts to gain familiarity with discharge information | ||
| Community Paramedicine | 2 hours | Readings on the role of community paramedicine to understand concepts underlying community paramedicine |
Program Features: Enrollment
Our study only included community-dwelling older adults (age≥60) who lived in Dane or Monroe Counties and received primary care from either University-associated health system. We avoided focusing on specific subgroups because a study aim is to determine which types of patients would benefit from the ED-to-home CTI.
Integrating the CTI into the fast-paced ED environment required coordination with the ED operations. We queried each eligible patient’s ED care provider to determine if the patient would be discharged home. Research assistants approached those patients likely to be discharged home and obtained informed consent to participate, either from the patients or their legally authorized representative. To minimize program attrition, research assistants scheduled the patient’s home visit in the ED, and gave patients a card with the coach’s photo and scheduled visit time. We provided the coach with the patient’s demographic information and ED discharge instructions (included in the AfterVisit Summary: Epic Corporation, Verona, WI), but not the physician note, since the program’s purpose is coaching rather than direct medical care.
Program Features: Home Visit
Paramedic coaches traveled to the patient in a marked vehicle and in uniform, but without emergency medical equipment. This approach differentiated coaching from delivery of direct medical care. For personal safety, coaches checked public safety databases for any alerts (e.g., violent dogs). They called the patient shortly before the visit to ensure that the patient was at home and the visit time was still convenient. Such contact eliminated unnecessary travel and served as a patient reminder. Upon arrival at the residence, if coaches identified an emergency situation they would contact a physician member of the study team at each site and, if necessary, request an ambulance, although this event has not happened to date.
During the visit itself, coaches delivered the CTI as detailed by the Care Transitions Program.20,21 The agenda for the visit was driven by each patient’s personal goal, which may be related to the reason for his/her ED visit. Conversations during the coaching visit included the patient reconciling medications using the Medication Discrepancy Tool (MDT), maintaining the personal health record to facilitate communication, understanding the role of follow-up visits, and demonstrating awareness of red flags.20,21,31,32
Program Features: Follow-Up
Finally, coaches performed up to 3 follow-up phone calls, supporting patients by discussing progress towards each patient’s goals, recapping encounters with health professionals, and reinforcing previous discussions. We did not require that coaches complete three calls with all patients. We gave coaches, in conjunction with patients, the discretion to determine whether additional calls would have value. Coaches logged each home visit and phone call.
Evaluation
Our preliminary evaluation of the ED-to-home CTI Program focuses on feasibility, which we defined as the ability to enroll and retain patients and complete recommended contacts, acceptability, which we defined as satisfaction with the Program, and fidelity to the CTI model. We first report characteristics of intervention-group participants, including the Generalized Anxiety Disorder-2,25 Patient Health Questionnaire-9,26 PROMIS Social Isolation,27 Blessed Orientation-Memory-Concentration score,28 Activities of Daily Living deficiencies29 and Perceived Health Competence Scale.30 To evaluate feasibility, we report the overall eligibility and enrollment rates as of June 2017, proportion of coaching home visits and telephone calls completed, and program operational information (e.g., time metrics). For acceptability, we provide patient and caregiver reported satisfaction on surveys.
To evaluate program fidelity, we characterize the data on coaching services delivered to patients originating in logs completed by community paramedic coaches, as well as frequency and duration of calls. Finally, we present outcomes regarding medication discrepancies through the Medication Discrepancy Tool,31 physician follow-up, patient activation through the Perceived Health Competence Scale,32 and the quality of the care transition through the Care Transitions Measure-3 (0–100, higher scores indicate a better transition).33 Evaluation data pertain to the period from the program start to June 30, 2017 (University of Wisconsin) or June 28, 2017 (University of Rochester).
RESULTS
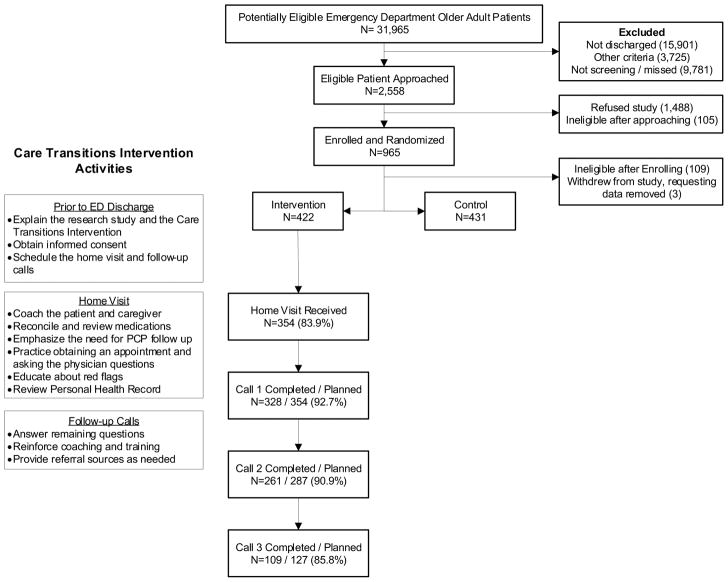
Of the 2,558 eligible patients approached, 853 were eligible, enrolled, and randomized, with 422 allocated to receive the CTI Program (Figure 1). Additionally, 98 caregivers consented to participate. Table 2 characterizes the participants in these groups, and describes the post-transition outcomes, including physician follow-up.
Figure 1.
Flow of subjects through the study, with detail regarding Care Transitions Intervention activities.
Table 2.
Characteristics of Intervention Participants and Program Outcomes
| Patients (N=422) | Caregivers (N=98) | ||
|---|---|---|---|
| Characteristics | Age years, median (IQR) | 70.7 (64.8, 79.3) | 67.5 (61.9, 73.5) |
| Female | 241 (57.1%) | 56 (60.2%) | |
| Race, White | 385 (91.2%) | 91 (92.9%) | |
| Ethnicity, Hispanic | 4 (0.9%) | 0 (0%) | |
| Marital status, married | 241 (57.1%) | 83 (84.7%) | |
| Education, >High school | 336 (79.6%) | 90 (91.8%) | |
| Lives alone | 139 (32.9%) | n/a | |
| Comorbidities, patient reported | n/a | ||
| Heart disease | 146 (34.6%) | n/a | |
| Depression | 125 (29.6%) | n/a | |
| Asthma / Chronic obstructive pulmonary disease | 89 (21.1%) | n/a | |
| Diabetes | 89 (21.1%) | n/a | |
| Cancer | 78 (18.5%) | n/a | |
| Stroke | 32 (7.6%) | n/a | |
| Dementia | 19 (4.5%) | n/a | |
| Generalized Anxiety Disorder-2 score, median (IQR) | 1 (0, 2) | n/a | |
| Categorized as anxiety disorder | 59 (14.0%) | n/a | |
| Patient Health Questionnaire-9 Score, median (IQR) | 3 (1, 6) | n/a | |
| Categorized as moderate depression or greater | 62 (14.7%) | n/a | |
| PROMIS Social Isolation, median (IQR) | 8 (6, 9) | n/a | |
| Categorized as medium or high isolation | 298 (70.6%) | n/a | |
| Activities of Daily Living deficiencies, median (IQR) | 0 (0, 1) | n/a | |
| 1 or more Deficiency | 172 (40.8%) | n/a | |
| Blessed Orientation-Memory-Concentration Test | n/a | ||
| Normal | 337 (79.9%) | n/a | |
| Questionable impairment / Impairment | 77 (18.3%) | n/a | |
| Unable to complete | 8 (1.9%) | n/a | |
| Outcomes | Physician follow-up within 4 days of ED visit (N=354) | 129 (38.9%) | n/a |
| Physician follow-up within 30 days of ED visit (N=320) | 282 (88.7%) | n/a | |
| Patient Activation Assessment (mean (SD)) | n/a | ||
| At Home Visit (n=354) | 5.97 (1.68) | n/a | |
| At Call 1 (n=328) | 7.22 (1.67) | n/a | |
| At Call 2 (n=261) | 7.79 (1.72) | n/a | |
| At Call 3 (n=109) | 7.70 (1.72) | n/a | |
| Care Transitions Measure-3 (4 day follow up, mean (SD), N=354)) | 85.9 (15.9) | n/a | |
| Health preferences (agree or strongly agree) | 298 (84.7%) | n/a | |
| Purpose meds (agree or strongly agree) | 335 (95.2%) | n/a | |
| Understanding responsibility (agree or strongly agree) | 340 (96.5%) | n/a |
IQR=Interquartile Range; PROMIS=Patient-Reported Outcomes Measurement Information System; ED=emergency department
Figure 1 and Table 3 provide measures of program feasibility. Notably, coaches successfully completed home visits and telephone coaching at high rates. On average, the home visit required nearly one hour and transport and preparation required an additional hour. We queried the paramedic coaches whether the initial home visit had to be an in-person visit, as opposed to a telephone call. For 324 (91.5%) of patients, the coaches responded that they felt that the initial home visit could not be replaced by a phone call.
Table 3.
Care Transitions Intervention Program Activity and Services Delivered
| Characteristic | Value | |
|---|---|---|
| Timing of home visit (n=354) | ≤48 hours | 320 (90.3%) |
| ≤72 hours | 33 (9.3%) | |
| Home visit effort (n=354) | Preparation time minutes, mean (SD) | 9.7 (6.5) |
| Coaching time minutes, mean (SD) | 54.0 (16.7) | |
| Driving time minutes, mean (SD) | 40.9 (18.9) | |
| Post visit documentation minutes, mean (SD) | 22.4 (11.8) | |
| Follow-up call 1 effort (n=328) | Preparation time minutes, mean (SD) | 5.2 (2.9) |
| Coaching time minutes, mean (SD) | 11.1 (5.1) | |
| Post visit documentation minutes, mean (SD) | 11.9 (5.8) | |
| Follow-up call 2 effort (n=261) | Preparation time minutes, mean (SD) | 5.1 (2.8) |
| Coaching time minutes, mean (SD) | 10.7 (4.8) | |
| Post visit documentation minutes, mean (SD) | 11.4 (4.4) | |
| Follow-up call 3 effort (n=109) | Preparation time minutes, mean (SD) | 5.2 (2.4) |
| Coaching time minutes, mean (SD) | 10.8 (4.5) | |
| Post visit documentation minutes, mean (SD) | 11.3 (3.4) | |
| Services provided during the home visit (n=354) | Discuss the patient’s personal goals | 349 (98.6%) |
| Perform medication management and discrepancy review | 337 (95.2%) | |
| Develop / update a personal health record | 343 (96.3%) | |
| Discuss physician follow-up | 327 (92.3%) | |
| Discuss what to do if red flags arise | 347 (98.0%) | |
| Medication discrepancies on home visit | Patients with at least one medication discrepancy | 119 (33.6%) |
| Factors Contributing to medication discrepancy (n=348) | ||
| Conflicting information from different sources | 139 (39.9%) | |
| Discharge instructions incomplete/inaccurate | 65 (18.6%) | |
| Intentional non-adherence | 58 (16.7%) | |
| Didn’t need prescription | 40 (11.5%) | |
| Services provided during follow-up call 1 (n=328) | Discuss the patient’s personal goals | 318 (97.0%) |
| Perform medication management and discrepancy review | 304 (92.7%) | |
| Develop / update a personal health record | 304 (92.7%) | |
| Discuss physician follow-up | 305 (93.0%) | |
| Discuss what to do if red flags arise | 304 (92.7%) | |
| Services provided during follow-up call 2 (n=261) | Discuss the patient’s personal goals | 252 (96.6%) |
| Perform medication management and discrepancy review | 242 (92.7%) | |
| Develop / update a personal health record | 239 (91.6%) | |
| Discuss physician follow-up | 241 (92.3%) | |
| Discuss what to do if red flags arise | 232 (88.9%) | |
| Services provided during follow-up call 3 (n=109) | Discuss the patient’s personal goals | 107 (98.2%) |
| Perform medication management and discrepancy review | 105 (96.3%) | |
| Develop / update a personal health record | 105 (96.3%) | |
| Discuss physician follow-up | 104 (95.5%) | |
| Discuss what to do if red flags arise | 100 (91.7%) |
Participants reported the CTI Program as highly acceptable, with patient and caregiver participants reporting being likely or extremely likely in the future to choose an ED with the CTI Program over one without the program (244 (76.2%); 69 (83.1%) respectively).
Finally, we report the services delivered as part of the CTI in Table 3. Fidelity with the CTI services were greater than 90% on all measures except for one.
DISCUSSION
We found that delivering the CTI for the ED-to-home transition is feasible and acceptable (Table 3). Particularly notable is the CTI coaches’ identity as community paramedics, as this is the first published evaluation of them in this role. While the effectiveness of the program will remain unclear until the results of the randomized controlled trial become available, the findings reported herein are promising and provide preliminary support of an ED-to-home CTI Program.
Care transitions has been a key focus to improve patient care.4,5,6,7,8,9,10,34 Coleman and colleagues developed the CTI to address hazards during the hospital-to-home transition through coaching, and they found that this approach reduced hospital readmissions and costs.35,36 This success accounts for our approach to apply the CTI approach to the ED-to-home context while making as few changes as possible. Coaches successfully provided patients coaching in the key focus areas (Table 3) and the coaches identified common needs (e.g., medication discrepancies, Table 3). These findings generally indicate strong fidelity with the program.
Other researchers have worked to improve the ED-to-home transition by identifying problems and directly addressing them, but have encountered challenges related to the feasibility and effectiveness of their programs. For instance, Guttman implemented a discharge planning and follow-up program that lasted 30 minutes/patient during the ED stay. Although her program increased patient satisfaction, it did not decrease in ED revisits within 14 days.17 A number of other researchers have similarly developed and implemented assessment and intervention programs, only to find no significant decrease in ED visits.18,19,37,38 In contrast, Schumacher and colleagues have developed a promising ED-to-home intervention modeled on the CTI using coaches from community area agencies on aging.39 While the exact details of the modification are not published, in a randomized controlled trial with 69 subjects, they found that those receiving the intervention showed improved patient activation. However, outcomes such as ED revisits were not reported. Finally, the concept of a geriatric ED has received much attention in discussions on how to improve care for older ED patients.3,40 While this concept has face validity, the only study to date assessing outcomes found only a negligible reduction in the ED revisit rate.41
Our approach of delivering the ED-to-home CTI Program using community paramedics is particularly novel. Community paramedics have already acted to deliver acute illness care, to screen patients for conditions, and to help patients navigate the health care system.42,43,44,45 To our knowledge, this is the first use of community paramedics in the CTI coaching role, suggesting that an additional type of healthcare provider may serve successfully as the CTI coach. Given their presence in most communities, the availability of paramedics to provide these services adds to the ability to deliver the ED-to-home CTI Program in underserved communities.46
Through our experiences in developing and implementing the ED-to-home CTI Program, we have found four important issues that must be considered. First, community paramedic coaches must be chosen for their commitment to the program and the approach. They then require training to deliver the CTI services, which differ significantly from the typical services offered by EMS providers. Although we did not experience significant challenges with this frame shift to coaching, an organization replicating our approach should be cognizant of this potential challenge and ensure careful selection of coaches such that the knowledge, skills, and attitudes of those placed in this role are sufficient to ensure success of the program. Additionally, future iterations of this program should consider using EMS providers with alternate certifications, as their EMS training may be sufficient, would reduce costs, and would make the program easier to implement more broadly in communities with more limited numbers of paramedics, such as rural settings.
Second, the ED-to-home CTI Program must work closely with EDs and health systems to establish an efficient process of identifying the participants, presenting the program, and communicating the necessary information to the coaches, as well as notifying PCPs. Likewise, we recommend working with strong EMS agencies with a commitment to community paramedicine training and programs. This mission alignment will help overcome the inevitable challenges that arise in any novel endeavor. For instance, in this study, research assistants scheduled home visits. This scheduling process will be a challenge without close collaboration of researchers and EMS.
Third, delivering the CTI Program involves significant effort: each patient requires almost three hours of coach time, including preparation and travel. Although leveraging the existing EMS infrastructure may reduce the cost of the ED-to-home CTI Program, the cost will remain significant and pose a major challenge, even if insurance plans agree to cover the cost. We hope our research can help target patients most able to benefit from this program. To manage costs and maximize the number of patients who can benefit from services, efficiency also needs to be maximized. For instance, the CTI Program is based on a home visit, and the coaches for this program feel strongly about the value of the home visit, reporting that it could have been substituted with a phone call only 9% of the time. In future work, we need to consider whether a home visit is necessary for all patients, or whether a telephone call or video conferencing would suffice, given local circumstances and goals.
Finally, if we demonstrate that a community paramedic-delivered ED-to-home CTI Program is effective, sustainability will be a major consideration for those establishing similar programs. We recommend working closely with local funders, including insurers and accountable care organizations. These groups will accrue cost benefits, and may express willingness to serve as the future funding resources for such programs.
Limitations
While we document the feasibility and acceptability of an ED-to-home CTI Program delivered through community paramedics and services provided, we do not demonstrate effectiveness. Also, this program takes place in two mid-sized communities, and it may have limited generalizability to other communities (e.g., rural, large urban cities), populations (e.g., homeless, institutionalized), or interventions, as well as to other types of coaches.
Conclusion
This program addresses the critically important need to improve the ED-to-home transition by translating the validated hospital-to-home CTI to a new setting. By leveraging community paramedics as CTI coaches, we demonstrate a model of care with characteristics to enhance implementation in a difficult transition period and in communities with limited health care resources.
Acknowledgments
Funding Source: esearch reported in this publication received support from the National Institute on Aging of the National Institutes of Health under Award Number R01AG050504 and the Clinical and Translational Science Award program, through the NIH National Center for Advancing Translational Sciences award UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Sponsor’s Role: The sponsor had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of the paper.
Footnotes
Conflict of Interest: The authors have no conflicts of interest.
Author Contributions: All listed authors have contributed significantly to this paper, including study concept and design (MNS, TVC, YC, JTC, CMCJ, EAC), acquisition of subjects and data (MNS, JTC, CMCJ, ML, RM), analysis and interpretation of data (MNS, MMH, TVC, YC, JTC, EHD, CMCJ, AJHK, ML, RM, EAC), and preparation of manuscript (MNS, MMH, JTC, EHD, CMCJ, AJHK, RM, EAC).
References
- 1.U.S. Census Bureau. [Accessed November 24, 2017];Selected Social Characteristics in the United States. Available at: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_5YR_DP02&src=pt.
- 2.Rui P, Kang K, Albert M. [Accessed October 14, 2017];National Hospital Ambulatory Medical Care Survey: 2013 Emergency Department Summary Tables. Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2013_ed_web_tables.pdf.
- 3.Hwang U, Shah MN, Han JH, et al. Transforming emergency care for older adults. Health Aff Proj Hope. 2013;32(12):2116–2121. doi: 10.1377/hlthaff.2013.0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCusker J, Cardin S, Bellavance F, et al. Return to the emergency department among elders: Patterns and predictors. Acad Emerg Med. 2000;7(3):249–259. doi: 10.1111/j.1553-2712.2000.tb01070.x. [DOI] [PubMed] [Google Scholar]
- 5.Caplan GA, Brown A, Croker WD, et al. Risk of admission within 4 weeks of discharge of elderly patients from the emergency department–the DEED study. Age Ageing. 1998;27(6):697–702. doi: 10.1093/ageing/27.6.697. [DOI] [PubMed] [Google Scholar]
- 6.Friedmann PD, Jin L, Karrison TG, et al. Early revisit, hospitalization, or death among older persons discharged from the ED. Am J Emerg Med. 2001;19(2):125–129. doi: 10.1053/ajem.2001.21321. [DOI] [PubMed] [Google Scholar]
- 7.Hastings SN, Oddone EZ, Fillenbaum G, et al. Frequency and predictors of adverse health outcomes in older Medicare beneficiaries discharged from the emergency department. Med Care. 2008;46(8):771–777. doi: 10.1097/MLR.0b013e3181791a2d. [DOI] [PubMed] [Google Scholar]
- 8.Moons P, De Ridder K, Geyskens K, et al. Screening for risk of readmission of patients aged 65 years and above after discharge from the emergency department: Predictive value of four instruments. Eur J Emerg Med. 2007;14(6):315–323. doi: 10.1097/MEJ.0b013e3282aa3e45. [DOI] [PubMed] [Google Scholar]
- 9.Hastings SN, Schmader KE, Sloane RJ, et al. Adverse health outcomes after discharge from the emergency department–incidence and risk factors in a veteran population. J Gen Intern Med. 2007;22(11):1527–1531. doi: 10.1007/s11606-007-0343-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lowenstein SR, Crescenzi CA, Kern DC, et al. Care of the elderly in the emergency department. Ann Emerg Med. 1986;15(5):528–535. doi: 10.1016/s0196-0644(86)80987-8. [DOI] [PubMed] [Google Scholar]
- 11.Vashi A, Rhodes KV. “Sign right here and you’re good to go”: a content analysis of audiotaped emergency department discharge instructions. Ann Emerg Med. 2011;57:315–322. doi: 10.1016/j.annemergmed.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 12.Engel KG, Heisler M, Smith DM, et al. Patient comprehension of emergency department care and instructions: Are patients aware of when they do not understand? Ann Emerg Med. 2009;53(4):454–461. doi: 10.1016/j.annemergmed.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 13.Katz EB, Carrier ER, Umscheid CA, et al. Comparative effectiveness of care coordination interventions in the emergency department: a systematic review. Ann Emerg Med. 2012;60:12–23. doi: 10.1016/j.annemergmed.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 14.Barlas D, Homan CS, Rakowski J, et al. How well do patients obtain short term follow up after discharge from the emergency department. Ann Emerg Med. 1999;34:610–614. doi: 10.1016/s0196-0644(99)70163-0. [DOI] [PubMed] [Google Scholar]
- 15.Biese KJ, Busby-Whitehead J, Cai J, et al. Telephone follow-up for older adults discharged to home from the emergency department: a pragmatic randomized controlled trial. J Am Geriatr Soc. 2018;66(3):452–458. doi: 10.1111/jgs.15142. [DOI] [PubMed] [Google Scholar]
- 16.Caplan GA, Williams AJ, Daly B, et al. A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department–the DEED II study. J Am Geriatr Soc. 2004;52(9):1417–1423. doi: 10.1111/j.1532-5415.2004.52401.x. [DOI] [PubMed] [Google Scholar]
- 17.Guttman A, Afilalo M, Guttman R, et al. An emergency department-based nurse discharge coordinator for elder patients: Does it make a difference? Acad Emerg Med. 2004;11(12):1318–1327. doi: 10.1197/j.aem.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 18.Mion LC, Palmer RM, Meldon SW, et al. Case finding and referral model for emergency department elders: A randomized clinical trial. Ann Emerg Med. 2003;41:57–68. doi: 10.1067/mem.2003.3. [DOI] [PubMed] [Google Scholar]
- 19.McCusker J, Dendukuri N, Tousignant P, et al. Rapid two-stage emergency department intervention for seniors: Impact on continuity of care. Acad Emerg Med. 2003;10:233–243. doi: 10.1111/j.1553-2712.2003.tb01997.x. [DOI] [PubMed] [Google Scholar]
- 20.Coleman EA, Parry C, Chalmers S, et al. The care transitions intervention: Results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 21.Coleman EA, Smith JD, Frank JC, et al. Preparing patients and caregivers to participate in care delivered across settings: The Care Transitions Intervention. J Am Geriatr Soc. 2004;52(11):1817–1825. doi: 10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- 22.Choi BY, Blumberg C, Williams K. Mobile integrated health care and community paramedicine: An emerging emergency medical services concept. Ann Emerg Med. 2016;67(3):361–366. doi: 10.1016/j.annemergmed.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 23.The Care Transitions Program. [Accessed on March 24, 2018];About Our Training. https://caretransitions.org/about-our-training/
- 24.Lau HS, Hollander MM, Cushman JT, et al. A qualitative evaluation of the coach training within a community paramedicine care transitions intervention. Prehosp Emerg Care. doi: 10.1080/10903127.2017.1419325. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wild B, Eckl A, Herzog W, et al. Assessing generalized anxiety disorder in elderly people using the GAD-7 and GAD-2 scales: results of a validation study. The American Journal of Geriatric Psychiatry. 2014;22(10):1029–1038. doi: 10.1016/j.jagp.2013.01.076. [DOI] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. [Accessed on March 23, 2018];PROMIS Short Form v2.0. Available at: http://www.healthmeasures.net/search-viewmeasures?task=Search.search.
- 28.Katzman R, Brown T, Fuld P, et al. Validation of a short orientation-memory-concentration test of cognitive impairment. The American Journal of Psychiatry. 1983;140:734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- 29.Katz S, Downs TD, Cash HR, et al. Progress in development of ADL. Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 30.Smith MS, Wallston KA, Smith CA. The development and validation of the Perceived Health Competence Scale. Health Education Research. 1995;10(1):51–64. doi: 10.1093/her/10.1.51. [DOI] [PubMed] [Google Scholar]
- 31.Smith JD, Coleman EA, Min SJ. A new tool for identifying discrepancies in postacute medications for community-dwelling older adults. American Journal of Geriatric Pharmacotherapy. 2004;2:141–148. doi: 10.1016/s1543-5946(04)90019-0. [DOI] [PubMed] [Google Scholar]
- 32.Smith MS, Wallston KA, Smith CA. The development and validation of the Perceived Health Competence Scale. Health Education Research. 1995;10(1):51–64. doi: 10.1093/her/10.1.51. [DOI] [PubMed] [Google Scholar]
- 33.Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patient’s perspective. The Care Transitions Measure. Med Care. 2005;43:246–255. doi: 10.1097/00005650-200503000-00007. [DOI] [PubMed] [Google Scholar]
- 34.National Transitions of Care Council. [Accessed November 24, 2017]; Available at: http://www.ntocc.org/
- 35.Coleman EA, Smith JD, Frank JC, et al. Development and testing of a measure designed to assess the quality of care transitions. Int J Integr Care. 2002;2(2):e02. doi: 10.5334/ijic.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coleman EA, Berenson RA. Lost in transition: Challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141:533–536. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 37.Runciman P, Currie CT, Nicol M, et al. Discharge of elderly people from an accident and emergency department: Evaluation of health visitor follow-up. J Adv Nurs. 1996;24:711–718. doi: 10.1046/j.1365-2648.1996.02479.x. [DOI] [PubMed] [Google Scholar]
- 38.Miller DK, Lewis LM, Nork MJ, et al. Controlled trial of a geriatric case finding and liaison service in an emergency department. J Am Geriatr Soc. 1996;44:513–520. doi: 10.1111/j.1532-5415.1996.tb01435.x. [DOI] [PubMed] [Google Scholar]
- 39.Schumacher JR, Lutz BJ, Hall AG, et al. Feasibility of an ED-to-home intervention to engage patients: A mixed-methods investigation. West J Emerg Med. 2017;18(4):743–751. doi: 10.5811/westjem.2017.2.32570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rosenberg M, Rosenberg L. Improving outcomes of elderly patients presenting to the emergency department. Ann Emerg Med. 2011;58:4979–4981. doi: 10.1016/j.annemergmed.2011.06.544. [DOI] [PubMed] [Google Scholar]
- 41.Hwang U, Dresden SM, Rosenberg MS, et al. Geriatric emergency department innovations: Transitional care nurses and hospital use. J Am Geriatr Soc. 2018 doi: 10.111/jgs.15235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O’Meara P, Stirling C, Ruest M, et al. Community paramedicine model of care: An observational, ethnographic case study. BMC Health Services Research. 2016;16:39. doi: 10.1186/s12913-016-1282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shah MN, Schoenwetter DJ. Community paramedicine: The Geisinger experience. In: Wiler J, Pines J, Ward M, editors. Value and Quality Innovations in Acute and Emergency Care. Cambridge, UK: Cambridge University Press; 2017. pp. 186–194. [Google Scholar]
- 44.Nejtek VA, Aryal S, Talari D, et al. A pilot mobile integrated healthcare program for frequent utilizers of emergency department services. Am J Emerg Med. 2017;35:1702–1705. doi: 10.1016/j.ajem.2017.04.061. [DOI] [PubMed] [Google Scholar]
- 45.Tadros AS, Castillo EM, Chan TC, et al. Effects of an emergency medical services-based resource access program on frequent users of health services. Prehosp Emerg Care. 2012;16(4):541–547. doi: 10.3109/10903127.2012.689927. [DOI] [PubMed] [Google Scholar]
- 46.Tavares W, Drennan I, Van Diepen K, et al. Building capacity in healthcare by reexamining clinical services in paramedicine. Prehosp Emerg Care. 2017;21(5):652–661. doi: 10.1080/10903127.2017.1311391. [DOI] [PubMed] [Google Scholar]