Abstract
Objectives:
To study the impact of caregiver-focused interventions to support medication safety in older adults with chronic disease.
Design:
Systematic Review
Setting:
Studies published before 01/31/2017; searched through Ovid Medline, PubMed, EMBASE, Scopus, CINAHL, PsycInfo and Google Scholar.
Participants:
Caregivers with or without patients.
Measurements:
Inclusion criteria:
interventions focused on caregivers aiming to improve medication safety. Studies not focusing on older adults, not evaluating medication safety, failing to include caregivers, or without a comparison group were excluded.
Results:
The initial search revealed 1311 titles. Eight studies met inclusion criteria. The strategies employed among randomized trials were: a) a home-based medication review and adherence assessment by a clinical pharmacist (two home visits separated by 6–8 weeks, with pharmacist and physician meeting independently) showed no difference in non-elective hospital admissions (p=0.8), but reduced the number of medications (p=0.03); b) a 19-min educational DVD, an hour-long medication education and training improved caregiver satisfaction (p<0.04); c) another medication education and adherence intervention (2–3 home visits per patient and caregiver dyad over 8 weeks) showed no difference in knowledge, administration, and accessibility of medications (p=0.29); and d) a collaborative case management program (a 16-month program that includes assessment, meeting and monthly telephone follow-ups) reduced perceived caregiver burden (p=0.03). Quasi-experimental trials included: collaborative care transitional coaches, an outpatient collaborative care model, and education and training programs. Among these, educational interventions showed improvements in self-efficacy, confidence and preparedness. The collaborative care intervention reduced rehospitalization (p=0.04) and improved quality of care outcomes.
Conclusion:
While some interventions improved caregivers’ medication knowledge and self-efficacy, the impact on clinical outcomes or healthcare utilization was insufficiently studied. Two studies implementing collaborative care models with medication management components showed the potential for improvement in both quality of clinical care and reductions in healthcare visits and warrant further study with respect to medication safety.
Keywords: caregivers, medication safety, medication adherence, older adults, aged, chronic disease, systematic review
Introduction
Medication safety means reducing harm by maximizing the safe and prudent use of medications.1, 2 The process of managing medications safely from the patient perspective is complex and has various components including acquisition, storage, adherence, and monitoring of both safety and efficacy parameters. Managing all components of medication use is a challenging task for older adults who have chronic diseases. Older adults made up 13% of the US population in the 2010 census, and consumed 34% of prescription and 30% of over-the-counter (OTC) medications.3 The aging population is susceptible to adverse outcomes from medications due to multi-morbidity and physiologic changes with aging.3–6 Higher levels of medical complexity increase problems with adherence, drug-drug interactions, and adverse effects.3–8
Older adults often suffer from multiple chronic comorbidities.4, 8 Multi-morbidity often leads to use of multiple medications and polypharmacy. Polypharmacy is a term used to describe the unnecessary use of medications without an indication, have more risks than benefits, or have insufficient evidence supporting their use.5 Polypharmacy has been correlated with geriatric syndromes including falls, adverse drug effects and poor adherence.5 Prescribed medications are also further complicated by readily available OTC medications that increase risk of potentially harmful medication-related outcomes.3
In this paper, we define “vulnerable elders” as older adults with chronic disease. Vulnerable elders often have multiple barriers in adhering to their medications.7 Such barriers may include multiple medications with multiple doses and dosing times, lack of medication adherence support, adverse side effects, drug interactions, and cost. Many vulnerable elders, including those with early stages of cognitive impairment, often look to caregivers to support adherence to medications.8–10 The burden of caregiving in the U.S. is illustrated by the 30 billion hours in caring for elders that are spent by informal caregivers every year.11 An AARP study recently reported that nearly 50% of caregivers assist in the medication management of older adults, irrespective of their cognitive status.12 Another survey of 1002 informal caregivers revealed that nearly 40% of them were assisting in administration of medications but 18% of them reported that they did not receive any training or instructions from a healthcare professional regarding medication administration and related precaution.13 Poland and colleagues conducted a qualitative study to highlight caregiver-reported challenges of medication management in caring for patients with dementia. The study findings described themes on medication management, communication, shared responsibility, and assessing harms and usefulness of medications. Authors concluded that the emotional stress from these barriers represent an unmet need and may adversely influence the caregiver’s role in medication adherence and monitoring. .14 With a variety of medication-related challenges experienced by caregivers of vulnerable elders, our objective was to describe the design and impact of caregiver-focused interventions intended to support medication safety in vulnerable elders.
Methods:
We conducted a systematic evidence-based review of available literature to explore interventions for caregivers to improve the medication safety of vulnerable elders. We used key search terms to identify eligible studies, published before January 31, 2017, in Ovid Medline, PubMed, EMBASE, Scopus, CINAHL, PsycInfo and Google Scholar. Search terms included morbidity, chronic disease, dementia, cognitive disorder, medication adherence, patient safety, medication knowledge, elderly patients, polypharmacy, medication reconciliation, caregiver burden, caregivers, caregiver support, carer, aged, and vulnerable populations. Only English language studies were included. Inclusion criteria were a) age 65 years or older, b) chronic disease c) intervention focused on improving medication safety, d) intervention delivered at least in part to caregivers. Non-experimental designs without comparison groups were excluded.
The titles of studies identified by the initial search were reviewed against the inclusion and exclusion criteria by the lead author (KCW). After excluding those not meeting eligibility criteria, two authors (KCW, NLC) reviewed abstracts and manuscripts against the inclusion and exclusion criteria and removed those not meeting eligibility criteria. Disagreements on eligibility were resolved by discussion amongst all authors.
Results:
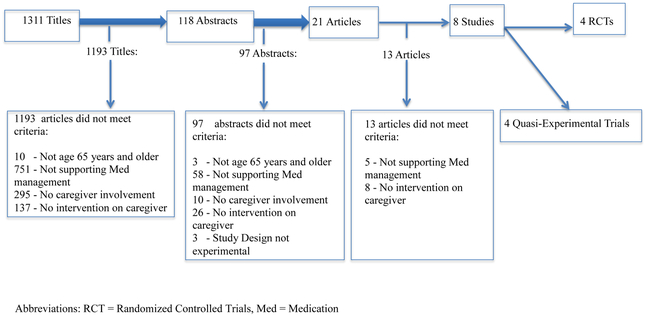
A total of 1311 studies met initial search criteria. See Figure 1 for the flow of screening and inclusion of identified studies. Due to the heterogeneity in the nature of interventions and outcomes assessed, studies are presented based on study design. A brief description of each study follows, while table 1 and 2 summarizes population, environment, intervention, and outcomes of the four RCTs and the four quasi-experimental trials respectively.
Figure 1:
Flow diagram of search results
Table 1.
Randomized Controlled Trials and their description
| Author (Yr.) Sample Size (N) |
Target of intervention* | Setting | Delivery of intervention | Intervention content | Outcomes measured | Results |
|---|---|---|---|---|---|---|
|
Lenaghan,
2007 N=136 |
Caregiver and patient Caregiver characteristics not published |
Community-dwelling older adults | Pharmacist | Med Review and education; recommendations delivered by pharmacist to primary/general provider | Non-elective hospital admissions, mortality,
Admission to nursing facility, Number of medicines prescribed, quality of life (EQ-5D) |
Med reduction of −0.87 in favor of the intervention group, 95% CI −1.66 to −0.08, P = 0.03; no statistically significant change in other outcomes: hospital admissions, nursing home admission, mortality, or quality of life |
|
Tsianakas,
2015 N=47 |
Caregiver of cancer
patient Mean age 53 years 65% female 44% spouse 26% children 30% others |
Hospital |
Chemo- therapy Nurse |
Education on Chemotherapy through group
session with DVD and booklet as follow-up resources |
Investigator-designed scales for: Med knowledge, Knowledge gaps, Care experience, and perceived confidence in caregiving. Also GHQ-12 for emotional wellbeing |
Improvement in knowledge of chemotherapy, proportion with information needs met, and satisfaction with care. No difference in experience of care, confidence of coping, and emotional well-being was found. |
|
Lingler,
2016 N=83 |
Caregiver 70% female 66+/−12.8 years 52% spouse 40% children 7% others |
Community | Nurse or Social Worker | Training caregivers on Med management; intervention group received home + telephone-based training of caregivers over 16 weeks. Usual Care group received reading materials on med safety | MedMaIDE Medication Deficiency Checklist |
Both groups showed reduction on MedMaIDE (p<0.01) and MDC (p < .01) scores compared to baseline but there was no difference between the groups in either measure (p =0.09, and p =0.29). 88% of the caregivers in the intervention group found the intervention to be useful and relevant |
|
Yu,
2016 N=60 |
Caregiver Mean age 61.3+/− 5.5 >70% female Half were children of the frail elders |
Community |
Collaborative model among a nurse, social
worker, care-recipient and caregiver |
Comprehensive assessment of caregiver including needs prioritization and access to elective training that includes med management and other physical, medical and psychological management workshops for 6 weeks | Caregiver Burden Inventory and the MOS SF-36 (Chinese) | Caregivers in intervention group showed
improvement on perceived caregiver burden (p = .03); no change in
measures of quality of life |
Available demographic information of caregivers are reported in the table. Abbreviations: Med = Medication(s), NP=Nurse Practitioner, SW=Social Worker, MedMaIDE=Med-Management Instrument for Deficiencies in the Elderly, MDC=Med Deficiency Checklist, EQ-5D=Standard Quality of Life measure developed by EuroQol group, CI= Confidence Interval
Table 2.
Quasi Experimental Trials and their description
| Author (Yr.) Sample size (N) Design |
*Target Interventions | Settings | Delivery of Intervention | Intervention content | Outcomes measured | Results |
|---|---|---|---|---|---|---|
|
Coleman,
2004 N=158 |
Caregivers and patients |
Transition from hospital to rehab or home | Geriatric NP | Medication self-management, personal (shared) health record, collaboration with primary and specialty physicians, symptoms management | Rehospitalization rates, ED visits | Rehospitalized within 30 days: 8.9% in
intervention vs. 13.8% in control, (p=0.04). Rehospitalized within 90 days: 13.5% in intervention vs. 22.9% in control, (p=0.002). Time to first rehospitalization 225.5 days in intervention vs. 217 days in control (p=0.003) |
|
Boustani,
2011 N=176 (first yr.) |
Caregivers |
Community dwelling older adults |
Dementia care coordinator through home-based and telephone-based communication | Education on behavior management, medication adherence support, care coordination, caregiver support, medication review by dementia expert | Acute care utilization, medication appropriateness, control of cardiovascular disease | Intervention group had lower proportion of inappropriate medications 16% vs. 32%; higher treatment of depression (68 % vs. 48%) and dementia medications (55% vs. 13%) and higher proportions meeting disease state control targets for cardiovascular disease |
|
Hendrix,
2011 N=50 |
Caregivers |
Hospitalized patients at time of discharge | Nurse | 70-minute face-to-face training with telephone follow-up at 1 week medication management education, symptom management, education on community resources, and personalized education about home care | Lorig’s Self-Efficacy Scale
(modified) Caregiving Preparedness Family Caregiving Inventory |
Improved self-efficacy (Modified
Lorig’s self-efficacy scale score) and preparedness (subscale of
the Family Caregiving Inventory) immediately following training and up
to four weeks (p-values not reported). |
|
Kimball,
2010 N=66 |
Caregivers and patients |
Hospital-based Rehabilitation unit | Nurse | Medication information delivered in three formats: 1) standardized med information; 2) Geragogy-based single session; 3) Geragogy-based dual session | Author-developed scale for Med Knowledge and confidence in medication administration | No difference in med knowledge between
teaching methods. Improved confidence in medication administration in family/caregivers regardless of the teaching method (p<0.001). |
All available demographic information of caregivers are reported in the table
Abbreviations: Med=Medication(s), NP=Nurse Practitioner, SW=Social Worker, Yr=Year, Rehab=Rehabilitation
Summary of Evidence from RCTs:
Home-Based Pharmacist Consultation:15
Lenaghan and colleagues described an intervention focused on older adults aged 80 and above living in their own homes, prescribed at least four oral daily medicines along with at least one of the following: living alone, record of confused mental state, impaired vision or hearing, prescribed medicines associated with medication-related morbidity, or prescribed more than 7 oral medicines. Participants randomized to the intervention received a one-time home visit by a clinical pharmacist who reviewed medications, provided medication specific education, addressed barriers to managing medications, and made prescribing recommendations to the primary care provider. At 6 months, there was no difference in the intervention group compared to usual care in the number of non-elective hospital admissions, admission to nursing facilities, mortality, or quality of life. However, participants in the intervention group experienced a reduction in the number of medications compared to those in the usual care group (p=0.03). Differences in adverse events, measures of adherence, or other clinical outcomes such as level of disease state control were not reported.
Supporting Caregivers of Cancer Patients:16
Tsianakas and colleagues described a study in which an intervention was developed for caregivers who were supporting patients undergoing chemotherapy for breast, lung or colon cancer. The intervention was developed through collaboration between both caregivers and the medical team based on the patient and caregiver’s needs. The intervention was delivered through an audiovisual aid (DVD), reading materials, and a group visit facilitated by chemotherapy nurses. The content focused on medication education of chemotherapy, including expected adverse effects, caregiver expectations and support. Compared to usual care, the intervention improved caregiver satisfaction and experience serving as a caregiver (p<0.04). The study did not report clinical outcomes such as chemotherapy adherence and tolerability.
Medication Management Training for Caregivers: 17
Lingler and colleagues studied an intervention developed to train caregivers to address medication management challenges in community dwelling elders with memory problems. Multiple disciplines met together to develop content for the training program, which was delivered in participant’s homes by a nurse or a social worker. The intervention was delivered over 2–3 home visits for each patient and caregiver dyad over an 8 week period. Each caregiver additionally received telephone follow up by the interventionists every 2 weeks for the subsequent 8 weeks (total 16-week intervention). This intervention group was compared to the usual care group who received only reading materials about resources on medication safety. The study used two medication management evaluation tools. One was the Medication Management Instrument for Deficiencies in the Elderly (MedMaIDE) which includes both survey as well as observation of caregivers on medication management, specifically reporting skills in medication knowledge, administration, and access. The second was the Medication Deficiency Checklist (MDC) which uses interviews with caregivers to assess medication administration errors and medication adherence. Although this training was perceived by the intervention group as helpful and relevant in their role as caregivers, there were no significant differences between groups on either the MedMaIDE (p=0.093) or MDC (p=0.292) scores. The study does not report differences in measures of adherence, disease state control, or health care utilization.
Collaborative Case Management to Support Family Caregivers of Vulnerable Elders:18
Yu and colleagues studied an intervention called Health and Social Collaborative Case Management (HSC-CM) to optimally support family caregivers of frail elders in the community. This 16-week intervention included a caregiver needs assessment, case management, medication management workshops and coordination of care support by multiple disciplines including nursing, social work, nutrition and physical therapy. Based on the needs assessment, caregivers are referred to workshops designed to address caregiving needs, such as nutritional management, stress management, or medication management, between the 5th to 11th weeks of the program. Specifically, medication management workshops were carried out by the nursing discipline. The authors reported an improvement in perceived caregiving burden among the intervention group compared to usual care according to the Caregiver Burden Inventory (p=0.03), and no difference in quality of life between groups as reported on the Medical Outcomes Study Short-Form Health Survey (p>0.04). No clinical outcomes related to differences in medication adherence, disease state control, and health care utilization were reported in the study.
Summary of Evidence of Quasi-Experimental Trials
Transitional Collaborative Care19:
Coleman and colleagues studied a transitional intervention by a geriatric nurse practitioner (NP) initiated during a hospital stay. The NP provided medication self-management tools, a personal health record with education on active health problems, and collaboration of care within primary and specialty care. The NP followed up with phone calls and visits either to a skilled nursing facility or the home setting to continue education of ongoing health issues and perform medication history with reconciliation. The intervention was conducted among patients discharged from the study hospital while the comparators were historical controls from administrative data. The intervention targeted the patient/caregiver dyad and included telephone calls and face-to-face visits to support transition to home after a skilled nursing facility stay. The intervention provided education and supported maintenance of a personal health record, medication self-management, coordination of care with providers, and monitoring of disease symptoms for acute decompensation. The intervention reduced non-elective re-hospitalization rates at 30, 90, and 180 days compared to the administrative control group, and reduced emergency room visits at 90 days, but not 30 or 180 days compared to control. Outcomes related to medication adherence were not reported, however the intervention resulted in high rates of medication knowledge and self-management compared to baseline, but no comparison with controls was available given the design of the study.
Collaborative Care Model for Caregivers of Patients with Dementia20:
Boustani and colleagues created an outpatient collaoborative care model targeting patients with cognitive impairment and supported by interdisciplinary team members. This intervention conducted a comprehensive assessment of caregiver’s knowledge of cognitive abilities, behavioral and supportive management strategies including medication adherence and medication appropriateness. Compared to the control group, the intervention group had lower use of high risk medications (19% vs. 40%) and higher pharmacologic treatment of depression (among those with depression; 68% vs. 48%) and higher pharmacologic treatment of dementia among patients with dementia (55% vs. 13%). Although no measures of medication adherence are reported, the authors reported higher rates of disease state control for hyperlipidemia and diabetes compared to a control group, and lower acute care utilization compared to the control group.
Teaching Hospitalized Patients and their Caregivers on Medication Management21:
Hendrix and colleagues studied an intervention that includes education of the patient caregiver dyad on medication management, symptom management, and availability of community healthcare resources prior to discharge from a hospital stay. The intervention was delivered by a trained nurse and occurred at a single point in time (up to 1.5 hours) prior to discharge. Compared to pre-intervention assessments, caregiver’s self-efficacy defined by a modified Lorig Self Efficacy score was improved (baseline score: 783.86; immediate post-training score: 903.64, 1 week post-training: 867.85, and 4 weeks post-training: 877.02). Similar increases were seen in measures of caregiver preparedness, however no comparisons of statistical significance were provided. Notably, no objective measures of medication adherence, disease state control, or healthcare utilization were reported, though participants reported satisfaction with the intervention.
Teaching caregivers and patients on discharge medications22:
Kimball and colleagues tested three approaches to teaching caregivers and patients about discharge medications in an inpatient rehabilitation setting. The three approaches were a standard medication information sheet with nurse review, medication information delivered in a geragogy format, and medication information delivered in a geragogy format with a follow-up session to reinforce education and answer questions. No differences in medication knowledge were reported between teaching methods, though all groups improved from baseline. Confidence in medication administration improved among caregivers (p<0.001) however no difference in method was reported. The authors did not report objective measures of medication adherence, measures of disease state control, or measures of re-hospitalization.
Discussion:
The findings from this systematic evidence-based review highlighted a paucity of data describing caregiver-focused interventions that improve medication safety and related clinical outcomes. Only three among the eight selected studies reported clinical outcomes such as reduced number of medicines, change in hospitalization, change in adverse outcomes, difference in use of inappropriate medications or medication adherence.15, 19, 20 Multi-component collaborative interventions that included medication management were able to improve rehospitalization rates, medication appropriateness, disease state control and acute care utilization among low-income elders.19,20
The variation in design, setting, population, intervention and outcome measures of the included studies are notable. Interventions were presumably developed from different stakeholder priorities, needs assessments, and intended applications. It was unclear in most manuscripts whether the logic model for the tested intervention was driven to improve a clinical outcome, patient-reported outcome, or caregiver-reported outcome. Further variability in setting could lead to an unknown impact on outcomes. As such, the quality of the evidence in generating a positive clinical impact was deemed to be weak. It is interesting to note that most interventions provided education and enhanced communication to the patient and caregiver, while interventions showing improved clinical outcomes enhanced communication amongst both the dyad and the healthcare team.
A systematic approach for review and reconciliation of medications was an integral part of several studies of the review. 15,18,19 It is worth noting that this component of the interventions was conducted either by a clinical pharmacist,15 a nurse,18 or a nurse practitioner;19 however the heterogeneity of the interventions precludes comparison of results based on the background of the interventionist. Two RCTs16, 17 and two quasi-experimental trials21, 22 highlighted training and education as caregiver interventions; they emphasized a need for such programs to occur in face-to-face formats either in a facility or at home. In these studies, nursing staff were the key personnel in delivering education and training, however in a study by Lingler et al,17 the training was performed by either a nurse or a social worker. Again, no comparison between disciplines was reported, but the study indicates a role for a social worker to be engaged in medication safety.17
While we believe that interventions improving caregiver knowledge are valuable, these activities are difficult to justify in the current payment models without an associated improvement in quality of care or clinical outcome. As such, it is also important to select appropriate clinical and quality measures for various populations and settings. For chronic care management, such clinical outcomes could include medication adherence, achievement of clinical targets, and healthcare utilization due to medication-related adverse events. In contrast, among patients in palliative care, reducing harm, improving quality of life and comfort are more appropriate clinical outcomes. Outcomes included in caregiver-based research should serve to both measure the impact of an intervention as well as correlate with a meaningful clinical outcome. Accuracy of medication administration and self-efficacy measures in managing chronic disease are ideal caregiver-reported outcomes that may improve medication management and safety. However, optimal measures for such outcomes have yet to be universally accepted.
Caregivers are the ones who observe the patient’s symptoms and signs closely; and this patient-specific knowledge can be important to consider in medication management.23 Importantly, caregivers may also influence medication management through their own sources of bias.23. A large study showed that caregivers who reside with a patient and have less stress levels will lead to higher medication adherence by 2.95 times compared to those caregivers who reside outside the patient’s residence and who have higher level of stress.24
Caregivers might have different needs based on characteristics and clinical needs of the patients they are supporting, such as dementia, cancer, or other chronic medical conditions. Similarly, characteristics about the caregiver’s personality, relationship with the patient, and health care literacy may also influence their needs. A common thread is a need for improved communication and skill sets specific to medications administration and monitoring. It is important to note that only highly motivated caregivers could be self-recruited for the trial and this may not reflect general caregiver characteristics including demographics, this is another example of limitation in caregiver research.17 Outcomes included in caregiver-based research should serve to both measure the impact of an intervention as well as correlate with a meaningful clinical outcome.
While some vulnerable elders may not be able to embrace technological assistance to aide in medication management, caregivers could be identified as alternative users of related technology. Studies of web-based interventions in the support of medication safety practices are promising 26,27 but failed to meet inclusion criteria for this review. Given the potential value of technology, further work will be needed to understand its role in supporting caregivers in medication safety and its impact on clinical outcomes.
Limitations of this review include small, mostly single site samples. Most studies investigated caregiver awareness, satisfaction, self-efficacy and knowledge rather than clinical outcomes.16, 22 Needs of those vulnerable elders with cognitive impairment may be different than those without cognitive impairment, and most studies did not report findings stratified by cognitive ability. As identified by Lingler and colleagues, caregivers and/or patient-caregiver dyads who are highly motivated to improve healthcare practices are the likely participants in this research, which may not be generalizable to all caregivers. Given heterogeneous outcomes of the included studies, a quantitative meta-analysis was not feasible. Because the intervention and the field in general, are limited by an underdeveloped assessment of clinical impact, it is premature to determine whether the cost is justified by the value. Additional work to understand clinical impact is warranted for this and other interventions, while considerations for cost are pursued among interventions showing meaningful clinical impact.
Conclusion:
This review illustrates that a variety of approaches executed by various members of the healthcare team have been attempted to improve medication management for vulnerable older adults. While interventions designed to improve medication knowledge and self-efficacy were successful, these interventions either had no impact on clinical outcomes or healthcare utilization, or the impact was insufficiently studied. In two studies, collaborative care models showed the potential for improvements in both quality of clinical care and reductions in healthcare visits. Interventions that reduce caregiver burden, improve satisfaction and confidence with medication management are valuable in quality-based care organization, however additional support from evidence establishing improvements in clinical outcomes will be critical for implementation. Interventions that showed reduction in number of medications, re-hospitalization, and improved quality of care of chronic diseases are potential strategies identified in this review that warrant further study. Understanding the essential components of caregiver-based interventions, including content, delivery, dose, and duration are important next steps to expand and optimize clinical, quality, and financial outcomes.
Acknowledgments:
The authors thank Steven R. Counsell, MD, from Indiana University School of Medicine, Department of Geriatrics and General Internal Medicine, for his comments and suggestions.
This study is presented in part, as a poster at the American Geriatrics Society Annual Scientific Meeting, Long Beach, California on, May 20, 2016.
Funding Source: John A. Hartford Foundation’s Center of Excellence and the National Institute on Aging (K23AG044440)
Sponsor’s Role: Dr. Wagle was supported by the John A. Hartford Foundation’s Center of Excellence in Geriatric Medicine and Training National Program Award to Indiana University School of Medicine as administered by the American Federation of Aging Research, New York, New York. Dr. Campbell was supported by award K23AG044440 from the National Institute on Aging. The sponsor had no role in the design or conduct of the study.
Footnotes
Conflict of Interest: The authors have no financial or any other personal or financial conflicts to report.
Author Contributions: Study concept and design: Wagle and Campbell. Literature search data extraction: Skopelja, Wagle and Campbell. Preparation of the manuscript: Wagle, Skopelja, and Campbell.
Impact Statement: We certify that this work is novel. As caregivers become an important workforce assisting older adults to manage their health, it is imperative to study what programs or interventions can support caregivers in improving medication safety. Our work reveals existing literature on this topic and suggests recommendations and directions for future studies.
Reference:
- 1.Canadian Patient Safety Institute. Medication Safety 2007. http://www.patientsafetyinstitute.ca/en/Topic/Pages/Medication-Safety.aspx. Accessed March 22, 2017.
- 2.http://www.who.int/patientsafety/medication-safety/en/, WHO; website accessed 11/20/17 [Google Scholar]
- 3.Qato DM, Alexander GC, Conti RM, et al. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA. 2008;300(24):2867–2878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83. [DOI] [PubMed] [Google Scholar]
- 5.Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. 2004;57(1):6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Campbell NL, Zhan J, Tu W, et al. Self-reported medication adherence barriers among ambulatory older adults with mild cognitive impairment. Pharmacotherapy. 2016;36(2):196–202 [DOI] [PubMed] [Google Scholar]
- 8.Jorm AF, Jolley D. The incidence of dementia: a meta-analysis. Neurology. 1998;51(3):728–733 [DOI] [PubMed] [Google Scholar]
- 9.Campbell NL, Boustani MA, Skopelja EN, et al. Medication adherence in older adults with cognitive impairment: a systematic evidence-based review. Am J Geriatr Pharmacother. 2012;10(3):165–177. [DOI] [PubMed] [Google Scholar]
- 10. [11/20/17]; https://www.ncbi.nlm.nih.gov/books/NBK396397/ accessed.
- 11.Chari AV, Engberg J, Ray KN, et al. The opportunity costs of informal elder-care in the United States: new estimates from the American Time Use Survey. Health Serv Res. 2015;50(3):871–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Alliance for Caregiving Public Policy Institute. Caregiving in the United States 2015. http://www.aarp.org/ppi/info-2015/caregiving-in-the-united-states-2015.html. Accessed March 22, 2017.
- 13.Donelan K, Hill CA, Hoffman C, et al. Challenged to care: informal caregivers in a changing health system. Health Aff (Millwood). 2002;21(4):222–231. [DOI] [PubMed] [Google Scholar]
- 14.Poland F, Mapes S, Pinnock H, et al. Perspectives of carers on medication management in dementia: lessons from collaboratively developing a research proposal; BMC Research Notes 2014, 7:463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lenaghan E, Holland R, Brooks A. Home-based medication review in a high risk elderly population in primary care--the POLYMED randomised controlled trial. Age Ageing. 2007;36(3):292–297. [DOI] [PubMed] [Google Scholar]
- 16.Tsianakas V, Robert G, Richardson A, et al. Enhancing the experience of carers in the chemotherapy outpatient setting: an exploratory randomised controlled trial to test impact, acceptability and feasibility of a complex intervention co-designed by carers and staff. Support Care Cancer. 2015;23(10):3069–3080. [DOI] [PubMed] [Google Scholar]
- 17.Lingler JH, Sereika SM, Amspaugh CM, et al. An intervention to maximize medication management by caregivers of persons with memory loss: Intervention overview and two-month outcomes. Geriatr Nurs. 2016;37(3):186–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu DSF. Effects of a Health and Social Collaborative Case Management Model on Health Outcomes of Family Caregivers of Frail Older Adults: Preliminary Data from a Pilot Randomized Controlled Trial. J Am Geriatr Soc 2016;64(10):2144–2148. [DOI] [PubMed] [Google Scholar]
- 19.Coleman EA, Smith JD, Frank JC, et al. Preparing patients and caregivers to participate in care delivered across settings: the care transitions intervention. J Am Geriatr Soc 2004;52(11):1817–1825. [DOI] [PubMed] [Google Scholar]
- 20.Boustani MA, Sachs GA, Alder CA, et al. Implementing innovative models of dementia care: The Healthy Aging Brain Center. Aging Ment Health. 2011;15(1):13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hendrix CC, Hastings SN, Van Houtven C, et al. Pilot study: individualized training for caregivers of hospitalized older veterans. Nurs Res. 2011;60(6):436–441. [DOI] [PubMed] [Google Scholar]
- 22.Kimball S, Buck G, Goldstein D, et al. Testing a teaching appointment and geragogy-based approach to medication knowledge at discharge. Rehabil Nurs. 2010;35(1):31–40. [DOI] [PubMed] [Google Scholar]
- 23.Conn VS, Taylor SG, Messina CJ. Older adults and their caregivers: the transition to medication assistance. J Gerontol Nurs. 1995:33–55. [DOI] [PubMed] [Google Scholar]
- 24.Foebel AD, Hirdes JP, Heckman GA. Caregiver status affects medication adherence among older home care clients with heart failure. Aging Clin Exp Res. 2012;24(6):718–721. [DOI] [PubMed] [Google Scholar]
- 25.Aikens JE, Zivin K, Trivedi R, et al. Diabetes self-management support using mHealth and enhanced informal caregiving. J Diabetes Complications. 2014;28(2):171–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kernisan LP, Sudore RL, Knight SJ. Information-seeking at a caregiving website: a qualitative analysis. J Med Internet Res 2010;12(3):e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steffen AM, Epstein J, George N, et al. The Sandwich Generation Diner: Development of a Web-Based Health Intervention for Intergenerational Caregivers. Jmir Research Protocols. 2016;5(2):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]