Abstract
Objective
Growing demand for VA dialysis exceeds its supply and travel distances prohibit many Veterans from receiving dialysis in a VA facility, leading to increased use of dialysis from non‐VA providers. This study compared utilization and hospitalization outcomes among Veterans receiving chronic dialysis in VA and non‐VA settings in 2008–2013.
Data Sources
VA, Medicare, and national disease registry data.
Study Design
National cohort of 27,301 Veterans initiating dialysis, observed for a period of 2 years after treatment initiation. We used multinomial logistic regression to examine associations between patient characteristics and dialysis use in VA, non‐VA community settings via VA Purchased Care (VA‐PC), community settings via Medicare, or Dual settings. Zero‐inflated negative binomial regression was used to compare risk of hospitalization and days spent in the hospital across dialysis settings.
Principal Findings
Sixty‐seven percent of Veterans obtained community‐based dialysis exclusively via Medicare, 11 percent in the community via VA‐PC, 4 percent in VA, and 18 percent in Dual settings. Financial and geographic access factors were important predictors of dialysis setting, but days spent in the hospital and risk of hospitalization did not differ meaningfully across settings.
Conclusions
Most Veterans obtained dialysis in the community. Dialysis setting appeared to have little impact on risk of hospitalization among Veterans.
Keywords: Dialysis, veteran, end‐stage renal disease, Medicare, VA, comparative effectiveness research
Veterans’ challenges in gaining access to Veterans Health Administration (VA) care have garnered significant attention in recent years, leading to the implementation of the Veterans Choice Act. However, it has been a longstanding concern to VA and federal policy makers. The VA has a long history of providing community care for Veterans, but the impact of VA and non‐VA care (including services purchased by VA) on outcomes is not well understood. This is particularly the case for Veterans on dialysis, who require highly specialized and ongoing chronic treatment and clinical management at significant time and cost.
Approximately 52,000 VA‐enrolled Veterans have end‐stage renal disease (ESRD), reflecting a higher prevalence in the VA patient population than in the general US population (US Renal Data System [USRDS] 2012, 2016; Veterans Health Administration [VHA] 2012; Watnick and Crowley 2014). The number of VA patients receiving maintenance dialysis under VA auspices almost doubled between 2000 and 2008, making this one of the fastest growing populations with chronic illness in the VA (Yoon et al. 2011). Veterans with ESRD have several different options for obtaining maintenance dialysis. Similar to non‐Veterans with ESRD, Veterans who have paid into Medicare are eligible for coverage under the ESRD entitlement 90 days after ESRD onset (if not already enrolled due to age or disability). However, Veterans may also be eligible to receive dialysis through the VA and, thus, often have a choice as to whether to obtain federally financed maintenance dialysis through either the VA or Medicare.
Where Veterans receive maintenance dialysis may be influenced by financial and non‐financial factors, non‐financial factors include travel distance (Wang et al. 2013, 2017), social support (Hynes et al. 2012; Wang et al. 2013), Veteran preference, prior care‐seeking in VA (Stroupe et al. 2011; Wang et al. 2013), and VA and community capacity. Financial factors include the relative generosity of VA and Medicare coverage. Unlike VA coverage, for new Medicare enrollees under the ESRD benefit, there is a 33‐month coordination period wherein Medicare serves as secondary payer to a Veteran's primary insurance coverage (e.g., private insurance). Differences in VA and Medicare cost‐sharing borne by the Veteran may also be a factor, as VA copayments (if not exempted due to military‐related disability or low income) are $15 per visit, compared to monthly Medicare Part B premiums and 20 percent copayment (roughly $30 per treatment) required under Medicare.
Dialysis services are a limited and costly resource within the VHA, which operates 71 units that provide outpatient maintenance dialysis, including 66 that also provide both inpatient acute and chronic dialysis services. When VA facilities are unable to meet Veteran demand for chronic dialysis due to insufficient capacity or geographic inaccessibility, local VA facilities authorize the use of outsourced dialysis care in the community through the VA Purchased Care program (VA‐PC, formerly known as VA Fee Basis). This system of procuring non‐VA dialysis under VA‐PC was in place before the introduction of the Veterans Choice Act. As chronic dialysis services are explicitly excluded from the Veterans Choice Program (VHA Office of Community Care 2017), VA‐PC remains the only source of VA‐financed dialysis in community settings and is the fastest growing source of dialysis for Veterans. The share of VA dialysis expenditures spent on VA‐PC community‐based dialysis increased from 17 percent in 1993 to 81 percent in 2017, and the proportion of Veterans receiving VA‐financed dialysis in the private sector increased from 56 percent in 2008 to 77 percent in 2017 (Health Economics Resource Center [HERC] 2009; VHA 2009; VHA Enrollment and Forecasting 2018).
Studies conducted more than a decade ago assessed general health care utilization among VA dialysis patients receiving care in different settings and payment sources or assessed dialysis costs among small regional samples (Hynes et al. 2007, 2012; Wang et al. 2013). Specifically, the prior study by Hynes and colleagues examined utilization, costs, quality of life, and mortality in 334 Veterans receiving maintenance dialysis from 2001 to 2004, while Wang and colleagues examined hospitalization and mortality in 1,388 maintenance dialysis patients from 2007 to 2008. Linkages of VA and Medicare administrative data to examine a more contemporary, national sample of patients reflecting utilization patterns and outcomes of the array of dialysis treatment and financial arrangements for dialysis services are needed. Elucidating the demographic, clinical, and financial determinants of Veterans’ use of VA, VA‐PC, or Medicare‐financed dialysis care and its implications for care and outcomes is information that is critical to forecasting and meeting the needs of future Veterans with ESRD.
In this study, we merged VA and Medicare data to examine a national cohort of 27,301 Veterans who initiated dialysis between 2008 and 2011, which was a time of exponential growth in VA spending for dialysis care and changing care and payment models. First, we examined Veterans’ utilization of outpatient maintenance dialysis and assessed the extent to which there were systematic differences in the characteristics of Veterans who obtained dialysis in VA and non‐VA settings. Second, we compared differences in the risk of hospitalization and days spent in the hospital across dialysis settings, which may be a function of many factors, including differences in patient characteristics across settings, quality of care, and care coordination across settings. Broadly, this study describes patient utilization in the VA's open health system model for providing care to a wide demographically and geographically distributed patient population. Examining these determinants is a critical foundation to understanding of potential sources of bias in comparative assessment of dialysis outcomes of VA versus Medicare‐financed dialysis care and to understanding the tradeoffs, implications, and value of alternative models of care for Veterans with ESRD (Department of Veteran Affairs [DVA] 2010, 2009; Government Accountability Office [GAO] 2012; VHA Chief Business Office 2012).
Methods
Conceptual Framework
This study is informed by Andersen's modified behavioral model of health services use (Andersen 1995). Briefly, this model posits that contextual factors (e.g., availability of VA dialysis, eligibility for insurance coverage) and individual characteristics (e.g., age, race) influence health care utilization, which in turn shape health outcomes. The relative importance of these factors may vary based on predisposing factors (e.g., employment, distance to care), other enabling factors (e.g., exemption from VA copayment, insurance status), and needs of a particular individual (e.g., comorbidity burden). Moreover, variations in these individual factors may provide insights into the underlying reasons for variations in utilization and outcomes of dialysis services in VA and non‐VA dialysis settings.
Hospitalization is common for patients with ESRD because dialysis initiation represents a major care transition often requiring hospitalization at the time of initiation and for subsequent complications (e.g., infection). Dialysis is an intensive and ongoing type of care (commonly 3 weekly visits to providers) that is quite different than health care received by most non‐dialysis patients. While some hospitalizations are necessary, others might be avoidable with better care coordination (i.e., a clotted dialysis access graft could be managed on an outpatient basis with better coordinated care). We hypothesized that those obtaining VA dialysis may experience better care coordination and lower rates of hospitalization than Veterans obtaining community‐based care funded by VA‐PC or Medicare due to co‐location of dialysis and non‐dialysis services and informational continuity of clinical information contained in the VA's seamless electronic medical record (Maciejewski et al. 2013). Hospitalization is an important dimension of dialysis quality and as a federal provider, however, the VA is systematically not included in the public reports on dialysis provider quality.
Study Design, Data, and Cohort
We conducted a retrospective cohort study of VA‐enrolled Veterans who initiated maintenance dialysis in 2008–2011. We used VA and Medicare administrative data from 2006 to 2013 to track Veterans’ use of health care services and their use of outpatient maintenance dialysis under VA, VA‐PC, and Medicare programs and hospitalization outcomes for up to 2‐years before and after dialysis initiation. VA data sources included information on Veteran enrollment (VHA Assistant Deputy Under Secretary for Health (ADUSH) Enrollment and VA MiniVitals files), inpatient and outpatient encounters (VA Patient Treatment and Outpatient Care files from the National Patient Care Database), and use of VA‐PC provided in community settings (VA Fee Basis outpatient and inpatient claims files). Medicare data included enrollment and claims files (i.e., Beneficiary Summary, MedPAR, Outpatient, and Carrier files) and the US Renal Data System (USRDS), a comprehensive national registry of all ESRD patients and providers in the United States (USRDS 2016).
After obtaining requisite approvals for the use of VA/CMS data, the analytic cohort was identified through a multi‐step data linkage process of VA and USRDS administrative files, coordinated between the study team and the VA Information Resource Center. Veterans were defined as those who enrolled in and obtained health care, compensation, or pension benefits from the VA (DVA 2014). Over 250,000 unique Veterans receiving dialysis in 2007–2013 were initially identified from VA and USRDS sources. We excluded patients who received a pre‐emptive kidney transplant, died within the first 90 days or recovered renal function within the first 180 days after dialysis initiation (because their exposure to financing options and dialysis treatment were too limited to derive meaningful associations); did not have a valid residential zip code or lived outside the US (i.e., Puerto Rico, Guam); or had incomplete or delayed recording of demographic or clinical information at dialysis initiation in the USRDS registry. We also excluded Veterans who were enrolled in Medicare Advantage or had unknown Medicare status at baseline; did not have any VA, VA‐PC, or Medicare recorded claims or encounters for outpatient dialysis; and patients who were hospitalized for the entire observed period of follow‐up. The final cohort included 27,301 Veterans (Appendix SA2).
Outcome and Covariates
We examined two outcomes of interest: utilization of dialysis setting and hospitalization in the 2 years following dialysis initiation. The dialysis setting outcome was one of four mutually exclusive dialysis settings/financing sources, ascertained from VA and Medicare claims: VA in‐house dialysis (VA), VA‐PC in community‐based dialysis units, Medicare‐financed dialysis (Medicare), and Dual dialysis from any combination of VA, VA‐PC, and/or Medicare arrangements. The outcome was initially identified in quarterly increments from the time of dialysis initiation up to the earlier instance of kidney transplantation, death, or end of follow‐up, but later constructed as a cross‐sectional observation per patient after we found little within‐patient variation in dialysis setting over the 2‐year observation period (Appendix SA3).
We also examined hospitalization, which is common for patients with ESRD, due to the generally high comorbidity burden and the major care transitions associated with dialysis initiation. Hospitalization was ascertained by VA, VA‐PC, and Medicare claims files and defined as the all‐cause total number of days spent in the hospital after dialysis initiation for up to 2 years of observation, with censoring at death or kidney transplantation. We also describe rates of cause‐specific hospitalizations: cardiac‐, dialysis access‐ or infection‐related.
Information from VA, USRDS, and Medicare administrative data was used to construct characteristics of each patient at the time of dialysis initiation (Table 1, Appendix SA4). We focused on eight explanatory variables of interest previously shown to consistently and systematically differ among Veterans who receive dialysis and other kinds of care in different settings (Hynes et al. 2007, 2012; Fischer et al. 2010; Stroupe et al. 2011; Wang et al. 2013) including demographic (age, race/ethnicity, US region of residence), clinical (baseline kidney function via estimated glomerular filtration rate or eGFR, mental health comorbidity), and access factors (insurance coverage: Medicare, Medicaid, private insurance, other, VA copayment exempt vs. non‐exempt status, and straight‐line distance to their nearest VA dialysis unit).
Table 1.
Veteran Patient Characteristics at Dialysis Initiation, Overall and by Veterans’ Dialysis Setting
| Overall | VA Dialysis | VA Purchased Care | Medicare | Dual | |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| Sample size | 27,301 (100) | 1,101 (4.0) | 3,085 (11.3) | 18,267 (66.9) | 4,848 (17.8) |
| Selected characteristics of interestc | |||||
| Agea,b | |||||
| <55 | 2,404 (8.8) | 179 (16.3) | 425 (13.8) | 1,068 (5.8) | 732 (15.1) |
| 55–64 | 6,544 (24.0) | 472 (42.9) | 1,377 (44.6) | 2,576 (14.1) | 2,119 (43.7) |
| 65–74 | 6,601 (24.2) | 230 (20.9) | 683 (22.1) | 4,567 (25.0) | 1,121 (23.1) |
| 75–84 | 8,624 (31.6) | 174 (15.8) | 503 (16.3) | 7,226 (39.6) | 721 (14.9) |
| ≥85 | 3,128 (11.5) | 46 (4.2) | 97 (3.1) | 2,830 (15.5) | 155 (3.2) |
| Racea,c | |||||
| White | 18,372 (67.3) | 404 (36.7) | 1,751 (56.8) | 13,667 (74.8) | 2,550 (52.6) |
| Black | 6,813 (25.0) | 555 (50.4) | 1,013 (32.8) | 3,462 (19.0) | 1,783 (36.8) |
| Hispanic | 1,333 (4.9) | 111 (10.1) | 210 (6.8) | 656 (3.6) | 356 (7.3) |
| Other | 783 (2.9) | 31 (2.8) | 111 (3.6) | 482 (2.6) | 159 (3.3) |
| US Regiona,b | |||||
| South | 11,947 (43.8) | 372 (33.8) | 1,685 (54.6) | 7,619 (41.7) | 2,271 (46.8) |
| Midwest | 6,235 (22.8) | 250 (22.7) | 580 (18.8) | 4,366 (23.9) | 1,039 (21.4) |
| Northeast | 4,502 (16.5) | 228 (20.7) | 222 (7.2) | 4,366 (23.9) | 431 (8.9) |
| West | 4,617 (16.9) | 251 (22.8) | 598 (19.4) | 2,661 (14.6) | 1,107 (22.8) |
| Nearest VAMC dialysisa,b | |||||
| Distance ≥30 miles | 17,479 (64.0) | 122 (11.1) | 2,668 (86.5) | 12,042 (65.9) | 2,647 (54.6) |
| Insurancea,c, a | |||||
| Medicaid | 4,140 (15.2) | 135 (12.3) | 374 (12.1) | 2,918 (16.0) | 713 (14.7) |
| Medicare | 25,561 (93.6) | 930 (84.5) | 2,617 (84.8) | 17,779 (97.3) | 4,235 (87.4) |
| Employer‐based | 3,950 (14.5) | 95 (8.6) | 212 (6.9) | 3,365 (18.4) | 278 (5.7) |
| Other | 9,321 (34.1) | 129 (11.7) | 606 (19.6) | 7,772 (42.5) | 814 (16.8) |
| VA copayment requiredb | 8,270 (30.3) | 104 (9.4) | 235 (7.6) | 7,475 (40.9) | 456 (9.4) |
| eGFRa | |||||
| <10 | 14,085 (51.6) | 679 (61.7) | 1,716 (55.6) | 8,838 (48.4) | 2,852 (58.8) |
| 10–15 | 9,084 (33.3) | 313 (28.4) | 976 (31.6) | 6,315 (34.6) | 1,480 (30.5) |
| ≥15 | 4,132 (15.1) | 109 (9.9) | 393 (12.7) | 3,114 (17.0) | 516 (10.6) |
| Comorbid conditiona,b,c, b | |||||
| Mental health | 10,225 (37.5) | 619 (56.2) | 1,661 (53.8) | 5,403 (29.6) | 2,542 (52.4) |
Data sources: (a) US Renal Data System (b) Veterans Health Administration (c) Medicare.
Category indicators of variables shown are not all mutually exclusive (e.g., insurance coverage).
Diagnosed mental health conditions used in this analysis refine the Gagne (Gagne et al. 2011) comorbidity index mental health conditions for evaluation of VA health care (Kilbourne et al. 2009; Holowka et al. 2014).
Descriptive statistics from the full set of Veteran patient characteristics incorporated in adjusted analyses are available in Appendix SA2.
eGFR, estimated glomerular filtration rate; VAMC,Veterans Affairs Medical Center.
Analyses were also adjusted for the following covariates: sex, urban vs. non‐urban residence, year of chronic dialysis start date, employment status, factors surrounding dialysis initiation that would influence treatment setting (e.g., pre‐ESRD nephrology care within or outside the VA, incident dialysis modality, type of vascular access at time of dialysis initiation, history of prior kidney transplant, cause of ESRD), distance to the nearest VA medical center (VAMC, i.e., the center most frequently used for non‐dialysis care, else the nearest VAMC to residence), and the extent of VA reliance for other outpatient care (Liu et al. 2011). VA reliance in our dialysis cohort was defined as the proportion of outpatient evaluation and management visits in or purchased by the VA, of all such visits identified from VA, VA‐PC, and Medicare sources in the year prior to dialysis initiation; and categorized as no VA or Medicare use (5.5 percent), 0–50 percent outpatient use relying on VA (60.3 percent), and >50–100 percent relying on VA (34.2 percent). We also determined whether patients initiated dialysis in the inpatient vs. outpatient setting, which may reflect severity and/or acuity of patient illness (i.e., complication resulting in kidney failure) or local practices (i.e., initiating dialysis as an inpatient to demonstrate physical tolerance for treatment) (Arif et al. 2017). The clinical burden of disease borne by the patient was characterized by 29 indicators of diagnosed physical health conditions (Gagne et al. 2011), body mass index (BMI), as well as hospitalization and institutionalization through VA or Medicare in the year before starting dialysis and hospice use in the 90 days before dialysis initiation. Finally, we included several characteristics of the VAMC most frequented by (or nearest to) each cohort member, including whether the VAMC had an on‐site nephrology services or dialysis unit, and the 2011 fiscal year occupancy rate of each Veteran's nearest VA outpatient dialysis unit as a rough proxy of VA clinical capacity.
We conducted regression imputation on 1,386 Veterans in our cohort (5 percent) with missing VA copayment status, based on baseline variables that predicted missing VA copayment status using IVEware in SAS (Raghunathan et al. 2001; Raghunathan, Solenberger, and Hoewyk 2007). All results presented use the copayment status including the imputed values. To assure fit in multivariable regression models and to simplify interpretation of point estimates, all continuous variables (e.g., age, body mass index, eGFR) were included as binary or categorical variables.
Statistical Analysis
Characteristics of Veterans receiving dialysis from the four settings (VA only, VA‐PC, Medicare, or Dual) were described via means and proportions. To examine the association between dialysis setting and Veteran characteristics, we used a multivariable multinomial logistic regression model in SAS version 9.4. Three odds ratios and their 95 percent confidence intervals are presented with an a priori selection of Medicare as the reference dialysis setting for each category of covariate. The model was reasonably fitted based on Hosmer and Lemeshow tests and McFadden's pseudo R 2 of 0.45 (McFadden 1974; Louviere, Hensher, and Swait 2000).
Our outcome of hospital days over the 2‐year period after each patient's first ESRD dialysis date of service is a count variable with overdispersion and excess zeros, so we fit Poisson, negative binomial, zero‐inflated Poisson, and negative binomial (ZINB) regression models that are appropriate for this type of outcome (McCullaugh and Nelder 1989; Neelon, O'Malley, and Smith 2016). The ZINB was the best fit model based on Akaike information criteria (AIC, Akaike 1974). The ZINB model is a mixture of the probability distribution for number of hospital days representing a subpopulation of Veterans at risk for hospitalization and the subpopulation not at risk for hospitalization (i.e., with no hospital days or “excess zeroes”). A higher probability of “excess zeroes” correlates with a lower probability of risk for hospitalization. An offset variable for time in the study was included to account for censoring due to death or kidney transplantation during follow‐up, and both parts of the zero‐inflated models adjusted for the aforementioned covariates. A deviance‐based R 2 for the ZINB (Martin and Hall 2016) was 0.14.
To aid with effect size interpretations for explanatory covariates of interest in both analyses, we present marginalized predicted probabilities of dialysis setting and expected number of days in the hospital and associated 95 percent confidence intervals (Austin 2010; Fang 2011). This study was approved by the Institutional Review Board of the Durham VA Health Care System.
Results
Characteristics of Patient Cohort
Veterans obtaining maintenance dialysis were predominantly male (98 percent), white (67 percent), retired (83 percent) and had a mean age of 71 years (Table 1, Appendix SA4). The overwhelming majority (94 percent) of Veterans in our cohort were already enrolled in Medicare at the time of dialysis initiation, and it is likely that most of the remaining 6 percent were subsequently eligible and enrolled in Medicare after the first 90 days of observation. A smaller proportion of patients were covered under Medicaid (15 percent), an employer group health plan (15 percent), or had other insurance (34 percent). Nearly, two‐thirds of Veterans (64 percent) lived ≥30 miles from the nearest VA dialysis unit. Over half of Veterans had very low levels of kidney function at the time of dialysis initiation (52 percent with eGFR <10 mL/min/1.73 m2) at the start of dialysis. Most Veterans were living in urban areas (85 percent) and 44 percent were living in Southern states. Overall, 38 percent had a mental health diagnosis and 6 percent had hepatitis. The overwhelming majority of Veterans had received nephrology care for up to 2 years (86 percent) before dialysis initiation, and 61 percent had been hospitalized under VA or Medicare during the year before initiation.
Utilization of Outpatient Dialysis Setting
Most (67 percent) Veterans received dialysis via Medicare exclusively throughout the 2‐year observation period (Table 1), 4 percent received VA‐only dialysis, 11 percent received dialysis outside the VA under VA‐PC only, while 18 percent received dialysis in more than one of these settings (Dual settings). Among the Veterans in this latter category, utilization patterns were generally stable over time. The majority of Dual dialysis patients used multiple settings for a relative short period of time over the 2‐year observation; half received dialysis in multiple settings only in the first 3 months after dialysis initiation and then settled in a distinct and single setting for the remainder of their observation. Moreover, Dual use most commonly involved VA‐PC (48 percent of Dual users received dialysis through VA and VA‐PC, 26 percent through VA‐PC and Medicare, and 12 percent through VA, VA‐PC, and Medicare). There was variation in setting/payment source across VISNs (Appendix SA5), with the percentage of patients receiving dialysis under Medicare ranging from roughly 50 percent in VISN A up to approximately 80 percent of Veterans in VISN S.
Higher observed percentages of Veterans with VA‐only dialysis were younger (aged <65), initiated dialysis with low levels of kidney function (e.g., eGFR < 10 mL/min/1.73 m2), were Black or Hispanic, were exempt from VA copayment, lived less than 30 miles from a VA facility providing maintenance dialysis, or had a mental health diagnosis as compared with Veterans with Medicare (and in some cases, VA‐PC) dialysis (Table 1).
In adjusted analyses, all explanatory variables of interest were associated with dialysis setting use (all p‐values < .0001; Figure 1, Appendix SA6). There was a substantial difference (7.8 percentage points) in predicted probabilities of Medicare use by VA copayment status (73.1 percent if required to pay VA copayments vs. 65.3 percent if exempted; Figure 2) and in the use of VA‐PC dialysis (9 percentage points) by Veterans’ residential distance <30 miles from their nearest VA dialysis unit compared to those living ≥30 miles away (5.6 percent vs. 14.5 percent). Veterans with a mental health diagnosis had higher odds of VA only, VA‐PC only, or Dual dialysis use compared to Medicare only (Figure 1). Compared to Medicare only users, Veterans with relatively higher baseline kidney function (e.g., eGFR ≥10 mL/min/1.73 m2) had a lower odds of dialyzing through VA‐only or Dual settings and those with eGFRs 10–15 mL/min/1.73 m2 had lower odds of VA‐PC dialysis (vs. eGFR <10, Figure 1).
Figure 1.
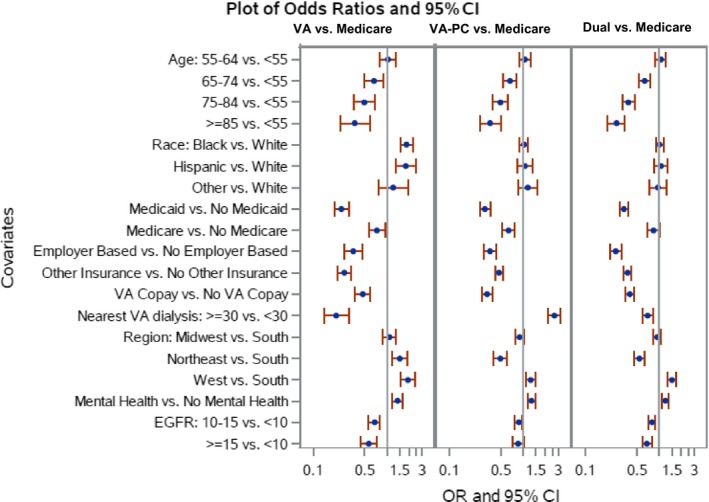
- Note. eGFR, estimated glomerular filtration rate; VA‐PC, VA Purchased Care. Selected estimates are presented here. Estimates from the full regression model are available in Appendix SA6.
Figure 2.
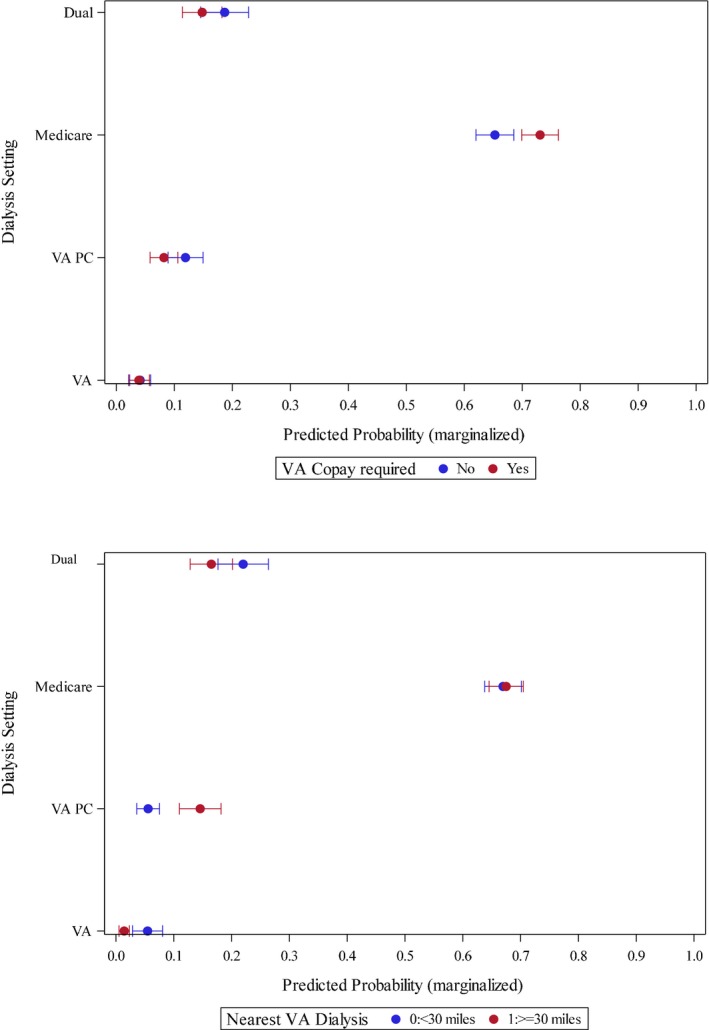
Adjusted Results: Marginalized Predicted Probabilities of Dialysis Setting Utilization, by Selected Veteran Characteristics [Color figure can be viewed at http://wileyonlinelibrary.com]
Hospitalization Rates and Number of Days by Dialysis Setting
Overall, 83 percent of Veterans were hospitalized at least once during the 2‐year period after initiating dialysis (Table 2) and spent a mean of 22.7 days (SD 28.8) and a median of 14.0 days (interquartile range = 28.0) in the hospital during this time period. Observed days spent in the hospital were similar across the four dialysis settings. Nearly, half of the cohort had at least one cardiac‐related hospitalization, and this was true for all four groups. Overall, 23 percent of Veterans had at least one access‐related hospitalization, ranging from 21 percent for those receiving dialysis in VA‐based to 28 percent in those receiving dialysis in Dual settings. The observed rate of infection‐related hospitalization for Veterans obtaining dialysis ranged from 41.2 percent for VA‐based to 45.1 percent in Dual settings.
Table 2.
Observed Hospital Days and Rates of Cause‐Specific Hospitalizations in the 2‐Years after Dialysis Initiationa, by Dialysis Setting
| Overall N = 27,301 | VA Dialysis N = 1,101 | VA‐PC N = 3,085 | Medicare N = 18,267 | Dual N = 4,848 | |
|---|---|---|---|---|---|
| All‐cause admissions, N (%) | 22,684 (83.1) | 905 (82.2) | 2,501 (81.1) | 15,161 (83.0) | 4,117 (84.9) |
| Overall hospital daysb, mean (SD) | 22.7 (28.8) | 24.1 (37.2) | 22.4 (29.3) | 21.9 (26.0) | 26.0 (35.1) |
| Overall hospital daysb, median (Q1, Q3) | 14.0 (4.0, 32.0) | 12.0 (3.0, 32.0) | 13.0 (3.0, 31.0) | 14.0 (4.0, 31.0) | 14.5 (4.0, 35.0) |
| Hospital daysc, mean (SD) | 27.4 (29.5) | 29.4 (39.1) | 27.7 (30.3) | 26.3 (26.4) | 30.6 (36.2) |
| Hospital daysc, median (Q1, Q3) | 18.0 (8.0, 36.0) | 17.0 (7.0, 39.0) | 18.0 (8.0, 37.0) | 18.0 (8.0, 36.0) | 19.0 (8.0, 40.0) |
| Cause‐specific hospitalizationd | |||||
| Cardiac, N (%) | 13,333 (48.8) | 524 (47.6) | 1,481 (48.0) | 8,770 (48.0) | 2,558 (52.8) |
| Access, N (%) | 6,382 (23.4) | 234 (21.3) | 779 (25.3) | 4,029 (22.1) | 1,340 (27.6) |
| Infection, N (%) | 12,031 (44.1) | 454 (41.2) | 1,293 (41.9) | 8,099 (44.3) | 2,185 (45.1) |
| Time in study, mean (SD) | 587.0 (211.8) | 631.3 (185.5) | 618.1 (192.6) | 562.2 (223.6) | 650.5 (159.8) |
| Time in study, median (Q1, Q3) | 727.0 (454.0, 727.0) | 727.0 (690.0, 727.0) | 727.0 (565.0, 727.0) | 727.0 (369.0, 727.0) | 727.0 (718.0, 727.0) |
Hospitalization outcomes (for admissions that occur following the 1st day of dialysis) and Time in study indexed on 1st day of dialysis and is <727 if Veterans received a kidney transplant or died).
Calculated mean and median hospital days include those in the sample with no observed hospitalization (i.e., hospital days=0).
Calculated mean and median hospital days, among those with any hospitalization (n = 22,684).
Cause‐specific hospitalization categories are not mutually exclusive (example: hospitalization for vascular access infection is both access‐related and infection‐related).
Q1, First quartile; Q3, Third quartile; SD, Standard deviation; VA‐PC, VA Purchased Care.
After adjustment for demographic, clinical, and access factors, risk for hospitalization (as reflected by probability of excess zeroes—lower probability of excess zeroes indicates higher risk of hospitalization) differed across dialysis settings (p < .0001; Appendix SA7). However, these differences were not clinically meaningful: upon examining marginalized estimates of risk for hospitalization, we found the range of estimates to be 0.10 to 0.14 across settings. Among the subpopulation at risk for hospitalization, there was no difference in the number of days spent in the hospital by dialysis setting (p = .80; Figure 3 and Appendix SA7).
Figure 3.
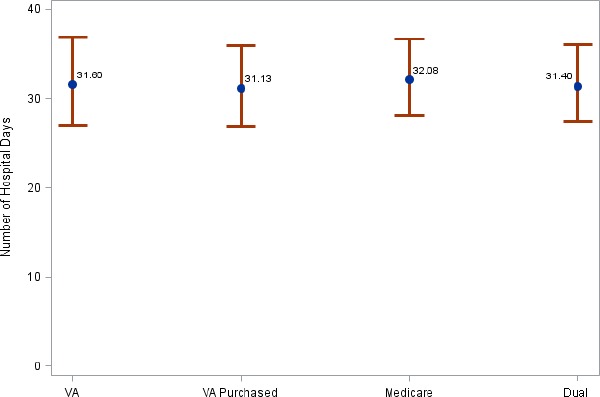
- Note. Marginalized Estimates from ZINB model that adjusted for patient baseline demographic, clinical and financial, and geographic access characteristics (full set of ZINB model estimates in Appendix SA7).
Discussion
Capitalizing on linkages of longitudinal VA, Medicare, and national disease registry data in a national cohort of Veterans who initiated dialysis in 2008–2011, we found that 67 percent received dialysis in the community exclusively under Medicare while only 4 percent received dialysis exclusively within the VA. The remaining 29 percent of patients received VA‐PC dialysis delivered in the community (11 percent) or received dialysis in more than one setting (18 percent). We found marked stability in Veterans’ dialysis utilization patterns where over three quarters of Veterans obtained dialysis in the same one setting through the entire observation period, indicating that Veterans’ dialysis setting was established early after initiation and that a community setting financed by Medicare was preferred by most Veterans. These findings—which reflect the most comprehensive contemporary analysis—are generally consistent with a prior study of Medicare and VA‐enrolled Veterans with ESRD, which showed use of both Medicare and VA programs for general health care needs (Hynes et al. 2003). Two earlier studies with smaller cohorts of regional samples (in 2001–2004 and 2007–2008) reported that Veterans had less frequent dialysis use in Medicare and greater use of VA financed or Dual dialysis (Hynes et al. 2007, 2012; Wang et al. 2013).
We also found that the risk of hospitalization and days spent in the hospital two years after initiation did not differ meaningfully by dialysis setting. We hypothesized that dialyzing across multiple settings involves transition of care and involvement of various providers across VA and non‐VA health systems might place patients higher risk for hospitalization, but our results suggest otherwise. Prior studies found differences in hospitalization rates between Veterans receiving dialysis in VA and non‐VA settings (Hynes et al. 2012; Wang et al. 2013), likely due to differences in study years, sampling strategy (regional vs. national sample), data used (VA vs. merged VA and Medicare enrollment and claims), and timeframe of observation (1‐ vs. 2‐year follow‐up).
Although risk of hospitalization and time spent in the hospital did not differ meaningfully across settings, we found that over three quarters of Veterans initiating dialysis maintained care through the same setting up to 2 years of observed follow‐up, which suggests that Veterans’ dialysis setting was established early after initiation. This finding raises important questions about whether current practices allow Veterans to exercise choice over where they dialyze, whether increasing VA capacity would lead more Veterans to obtain dialysis care in VA, and how shared decision making might be systematically introduced early in the course of dialysis treatment to insure that decisions about dialysis setting reflect the needs and preferences of individual Veterans. Given the often‐evolving needs of patients on dialysis and limited switching across settings, VA may want to develop feedback mechanisms and infrastructure to support accountability and responsiveness to patients’ needs.
With increasing prevalence of ESRD among Veterans, assessing the consequences of the VA Health Care System's make vs. buy decision‐making process for dialysis care is important, especially as improving Veterans’ access to community care has become a high priority among VA leaders (Vanneman et al. 2017). Our findings suggest that either option does not have adverse consequences on hospitalization outcomes. Veterans receiving dialysis in VA are more complex in several respects (more frequently African‐American with higher prevalence of diabetes, hypertension and mental health comorbidities, hepatitis, amputation) and therefore may receive more Veteran‐centric care in VA than those receiving dialysis care through Medicare. These results suggest that buying dialysis care in the community may be reasonable for most Veterans, but more complex Veterans may benefit from dialyzing in VA. Current policy does not allow VA to steer Veterans to community sources, so Veterans are likely to continue receiving dialysis from all of these sources for the foreseeable future.
If VA continues efforts to make additional VA capacity, our findings suggest it may do so without compromising patient outcomes while also improving patient access to VA care, aligning services to Veteran preferences, and reducing VA‐PC expenditures (GAO 2014). Veterans appear to largely utilize community‐based care, given that only 4 percent of Veterans dialyzed exclusively in VA and nearly three times as many Veterans were obtaining community‐based dialysis purchased by VA than were obtaining it from VA facilities. This demand for dialysis is likely to continue to outpace VA supply for some time, particularly if access to community dialysis care continues to increase. Future research is needed to understand whether outcomes for Veterans obtaining VA‐PC dialysis remain comparable to those of Veterans obtaining dialysis in VA facilities.
There are study limitations that should be noted. First, the scope of our analysis was limited to outpatient dialysis utilization and hospitalizations provided under financial auspices of the VA or Medicare. We did not have access to data on dialysis financed by Medicare Advantage or private insurance (approximately 9,000 patients). Therefore, our findings may not generalize to the entire population of patients or Veterans with ESRD. Second, despite all attempts for comprehensive covariate adjustment from VA and Medicare sources, unmeasured confounders may impact our results. For example, we were not able to control for social support or disease severity or to measure intermediate outcomes of dialysis treatment (e.g., urea reduction ratio, anemia treatment) that may influence dialysis utilization, reflect quality of dialysis care, and influence risk for hospitalization. Clinical measures obtained through laboratory results are not uniformly available across all settings and data systems. Third, we were not able to identify or characterize VA‐PC community dialysis providers from the VA‐PC claims data. This is important because the majority of private‐sector dialysis facilities are freestanding units and studies that found relationships between ESRD outcomes and dialysis facility characteristics have excluded VA's hospital‐based facilities (Garg et al. 1999; Hirth et al. 1999). Further research is needed to better understand whether observed differences in Veterans’ dialysis outcomes are attributable to the types of providers VA is outsourcing its services. Last, analyses were conducted on Veterans initiating dialysis from 2008 to 2011 and may not reflect current trends in CMS and VA payment and contracting policy, which has undergone significant change since 2012 (e.g., Medicare bundled payment for dialysis treatment, establishment of VA national contracting for dialysis services).
The ability to link VA, Medicare, and USRDS data enables a range of analyses in an extremely vulnerable and costly group of Veterans that can yield insights to help VA best structure and modify dialysis care and payment policies. Without Medicare and USRDS data linkage, it would be unknown specifically where a majority of Veterans initiating dialysis are getting their care or how hospitalization rates and other outcomes vary by dialysis care setting. As VA increases Veterans’ access to community care, these data linkages provide VA an ability to examine outcomes between VA dialysis and VA‐PC dialysis, which can inform future “make or buy” decisions about dialysis.
In conclusion, this study's linkage of VA and Medicare data and comprehensive assessment of Veterans’ utilization and hospital outcomes of chronic dialysis services identified important drivers of utilization patterns and hospital outcomes of Veterans receiving chronic dialysis in VA and non‐VA settings in 2008–2013. Veterans’ dialysis care patterns are established early after initiation. Most Veterans receive dialysis in the community through Medicare, and a minority receive treatment through the VA. There were no meaningful differences in hospitalization or days in the hospital, which is an important outcome but not the only outcome consideration for VA providers and federal policymakers. These results serve an important foundation for evaluating the comparative effectiveness of dialysis outcomes, assessing the consequences of the VA's make‐buy decision for dialysis care on the quality of care and health of Veterans, and allocation of federal (VA and Medicare) resources for life‐sustaining care for a growing population of Veterans with ESRD.
Supporting information
Appendix SA1: Author Matrix.
Appendix SA2: Sampling Frame.
Appendix SA3. Visualization of Veteran Dialysis Settings, by Quarter.
Appendix SA4. All Veteran Patient Characteristics at Dialysis Initiation, Overall and by Veterans’ Dialysis Setting.
Appendix SA5. Regional Variation in Cross‐Sectional (Overall) Dialysis Setting, by Veterans. Integrated Service Network (VISN).
Appendix SA6. Multinomial Regression Model Output for Dialysis Setting Utilization.
Appendix SA7. Technical Description and Full Set of Regression Results: Zero‐Inflated Negative Binomial Regression Model Examining Number of Hospital Days over 2 Years Follow‐Up Period from Chronic Dialysis Initiation.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors thank Drs. Susan Crowley, Michael Fischer, Wissam Kourany, and Rudy Rodriguez, the journal editors, and two anonymous reviewers for scientific counsel and helpful comments to this manuscript. This study was funded by the Department of Veterans Affairs (VA) Health Services Research & Development Service (IIR 12‐342) and a VA Research Career Scientist award (RCS 10‐391) and supported by the Center of Innovation for Health Services Research in Primary Care (CIN 13‐410) at the Durham VA Health Care System. Support for VA/CMS data is provided by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development, VA Information Resource Center (Project Numbers SDR 02‐237 and 98‐004).
Disclosures: Dr. Maciejewski reports ownership of Amgen stock due to his spouse's employment. Dr. O'Hare has received funding from VA, CDC, and NIH, as well as honoraria/speaker fees from Uptodate, Fresenius Medical Care, Dialysis Clinics Inc., the University of Alabama at Birmingham, and the Coalition for the Supportive Care of Kidney Patients. All other authors (VW, CJC, KMS, TSZB, PLH, DE, and HJW) report no potential conflict of interests.
Disclaimers: The interpretation and reporting of these data are the responsibility of the authors and do not reflect the official policy or interpretation of the US Government (US Renal Data System, National Institutes of Diabetes and Digestive and Kidney Diseases, Department of Veterans Affairs), Duke University, or University of Washington.
References
- Akaike, H. 1974. “A New Look at the Statistical Model Identification.” IEEE Transactions on Automatic Control 19: 716–23. [Google Scholar]
- Andersen, R. M. 1995. “Revisiting the Behavioral Model and Access to Medical Care: Does It Matter?” Journal of Health and Social Behavior 36 (1): 1–10. [PubMed] [Google Scholar]
- Arif, F. M. , Sumida K., Molnar M. Z., Potukuchi P. K., Lu J. L., Hassan F., Thomas F., Siddiqui O. A., Gyamlani G. G., Kalantar‐Zadeh K., and Kovesdy C. P.. 2017. “Early Mortality Associated with Inpatient versus Outpatient Hemodialysis Initiation in a Large Cohort of US Veterans with Incident End‐Stage Renal Disease.” Nephron 137 (1): 15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin, P. C. 2010. “Absolute Risk Reductions, Relative Risks, Relative Risk Reductions, and Numbers Needed to Treat Can Be Obtained from a Logistic Regression Model.” Journal of Clinical Epidemiology 63 (1): 2–6. [DOI] [PubMed] [Google Scholar]
- Department of Veteran Affairs (DVA) . 2010. “Payment for Inpatient and Outpatient Health Care Professional Services at Non‐Departmental Facilities and Other Medical Charges Associated with Non‐VA Outpatient Care. Final Rule.” Federal Register 75 (242): 78901–15. [PubMed] [Google Scholar]
- Department of Veterans Affairs (DVA) . 2009. Department of Veterans Affairs National Dialysis Pilot Study. Washington, DC: DVA National Dialysis Workgroup. [Google Scholar]
- Fang, J. 2011. Using SAS Procedures FREQ, GENMOD, LOGISTIC, and PHREG to Estimate Adjusted Relative Risks: A Case Study. Toronto, ON: Institute for Clinical Evaluative Sciences. [Google Scholar]
- Fischer, M. J. , Stroupe K. T., Kaufman J. S., O'Hare A. M., Browning M. M., Huo Z., and Hynes D. M.. 2010. “Predialysis Nephrology Care among Older Veterans Using Department of Veterans Affairs or Medicare‐Covered Services.” American Journal of Managed Care 16 (2): e57–66. [PubMed] [Google Scholar]
- Gagne, J. J. , Glynn R. J., Avorn J., Levin R., and Schneeweiss S.. 2011. “A Combined Comorbidity Score Predicted Mortality in Elderly Patients Better than Existing Scores.” Journal of Clinical Epidemiology 64 (7): 749–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg, P. P. , Frick K. D., Diener‐West M., and Powe N. R.. 1999. “Effect of the Ownership of Dialysis Facilities on Patients’ Survival and Referral for Transplantation.” New England Journal of Medicine 341 (22): 1653–60. [DOI] [PubMed] [Google Scholar]
- Government Accountability Office (GAO) . 2012. “VA Dialysis Pilot: Increased Attention to Planning, Implementation, and Performance Measurement Needed to Help Achieve Goals (GAO‐12‐584).”
- Government Accountability Office (GAO) . 2014. “VA Dialysis Pilot: Documentation of Plans for Concluding the Pilot Needed to Improve Transparency and Accountability (GAO‐14‐646).”
- Health Economics Resource Center (HERC) . 2009. “VHA Costs in Cost Distribution Report, FY1993–FY2003” [accessed on April 30, 2009]. Available at: http://vaww.herc.research.va.gov/files/MXLS_370.xls
- Hirth, R. A. , Held P. J., Orzol S. M., and Dor A.. 1999. “Practice Patterns, Case Mix, Medicare Payment Policy, and Dialysis Facility Costs.” Health Services Research 33 (6): 1567–92. [PMC free article] [PubMed] [Google Scholar]
- Holowka, D. W. , Marx B. P., Gates M. A., Litman H. J., Ranganathan G., Rosen R. C., and Keane T. M.. 2014. “PTSD Diagnostic Validity in Veterans Affairs Electronic Records of Iraq and Afghanistan Veterans.” Journal of Consulting and Clinical Psychology 82 (4): 569–79. [DOI] [PubMed] [Google Scholar]
- Hynes, D. M. , Cowper D. C., Manheim L., Sohn M. W., Stroupe K., Weaver F. M., and Freedman J.. 2003. Research Findings from the VA Medicare Data Merge Initiative: Veterans’ Enrollment, Access, and Use of Medicare and VA Health Services (XVA 69‐001). Report to the under Secretary for Health, Department of Veteran Affairs. Hines, IL: VA Information Resource Center, Health Services Research and Development Service. [Google Scholar]
- Hynes, D. M. , Koelling K., Stroupe K., Arnold N., Mallin K., Sohn M. W., Weaver F. M., Manheim L., and Kok L.. 2007. “Veterans’ Access to and Use of Medicare and Veterans Affairs Health Care.” Medical Care 45 (3): 214–23. [DOI] [PubMed] [Google Scholar]
- Hynes, D. M. , Stroupe K. T., Fischer M. J., Reda D. J., Manning W., Browning M. M., Huo Z., Saban K., and Kaufman J. S.. 2012. “Comparing VA and Private Sector Healthcare Costs for End‐Stage Renal Disease.” Medical Care 50 (2): 161–70. [DOI] [PubMed] [Google Scholar]
- Kilbourne, A. M. , Morden N. E., Austin K., Ilgen M., McCarthy J. F., Dalack G., and Blow F. C.. 2009. “Excess Heart‐Disease‐Related Mortality in a National Study of Patients with Mental Disorders: Identifying Modifiable Risk Factors.” General Hospital Psychiatry 31 (6): 555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, C. F. , Manning W. G., Burgess J. F. Jr, Hebert P. L., Bryson C. L., Fortney J., Perkins M., Sharp N. D., and Maciejewski M. L.. 2011. “Reliance on Veterans Affairs Outpatient Care by Medicare‐Eligible Veterans.” Medical Care 49 (10): 911–7. [DOI] [PubMed] [Google Scholar]
- Louviere, J. J. , Hensher A. D., and Swait D. J.. 2000. Stated Choice Methods. New York, NY: Cambridge University Press. [Google Scholar]
- Maciejewski, M. L. , Wang V., Burgess J. F. Jr, Bryson C. L., Perkins M., and Liu C. F.. 2013. “The Continuity and Quality of Primary Care.” Medical Care Research and Review: MCRR 70 (5): 497–513. [DOI] [PubMed] [Google Scholar]
- Martin, J. , and Hall D. B.. 2016. “R2 Measures for Zero‐Inflated Regression Models for Count Data with Excess Zeroes.” Journal of Statistical Computation and Simulation 86 (18): 3777–90. [Google Scholar]
- McCullaugh, P. , and Nelder J. A.. 1989. Generalized Linear Models. London: Chapman and Hall. [Google Scholar]
- McFadden, D. 1974. “Conditional Logit Analysis of Qualitative Choice Behavior” In Frontiers in Econometrics, edited by Zarembka P., pp. 105–42. Cambridge, MA: Academic Press. [Google Scholar]
- Neelon, B. , O'Malley A. J., and Smith V. A.. 2016. “Modeling Zero‐Modified Count and Semicontinuous Data in Health Services Research Part 1: Background and Overview.” Statistics in Medicine 35 (27): 5070–93. [DOI] [PubMed] [Google Scholar]
- Raghunathan, T. E. , Solenberger P. W., and Hoewyk J. V.. 2007. IVEware: Imputation and Variance Estimation Software, Version 0.1 Release. Ann Arbor, MI: Survey Methodology Program, Survey Research Center, Institute for Social Research, University of Michigan. [Google Scholar]
- Raghunathan, T. E. , Lepkowski J. M., Hoewyk J. V., and Solenberger P.. 2001. “A Multivariate Technique for Multiply Imputing Missing Values Using a Sequence of Regression Models.” Survey Methodology 27 (1): 85–95. [Google Scholar]
- Stroupe, K. T. , Fischer M. J., Kaufman J. S., O'Hare A. M., Sohn M. W., Browning M. M., Huo Z., and Hynes D. M.. 2011. “Predialysis Nephrology Care and Costs in Elderly Patients Initiating Dialysis.” Medical Care 49 (3): 248–56. [DOI] [PubMed] [Google Scholar]
- Tueller, S. J. , Van Dorn R. A., and Bobashev G. V.. 2016. “Visualization of Categorical Longitudinal and Times Series Data.” Methods report (RTI Press)(MR‐0033‐1602). [DOI] [PMC free article] [PubMed]
- US Department of Veterans Affairs . 2014. “VA Information Resource Center” [accessed on April 9, 2014]. Available at: http://www.virec.research.va.gov
- US Renal Data System . 2016. 2015 Researcher's Guide to the USRDS Database. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. [Google Scholar]
- US Renal Data System (USRDS) . 2012. USRDS 2012 Annual Data Report: Atlas of End‐stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (NIH‐NIDDK). [Google Scholar]
- US Renal Data System (USRDS) . 2016. USRDS 2016 Annual Data Report, Volume 1: Chronic Kidney Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (NIH‐NIDDK). [Google Scholar]
- Vanneman, M. E. , Harris A. H. S., Asch S. M., Scott W. J., Murrell S. S., and Wagner T. H.. 2017. “Iraq and Afghanistan Veterans’ Use of Veterans Health Administration and Purchased Care before and after Veterans Choice Program Implementation.” Medical Care 55(Suppl 7 Suppl 1): S37–44. [DOI] [PubMed] [Google Scholar]
- Veterans Health Administration (VHA) . 2009. Purchase of Non‐VA Hemodialysis Treatments, 2009. Washington, DC: Department of Veterans Affairs Chief Business Office. [Google Scholar]
- Veterans Health Administration (VHA) . 2012. “Allocation Resource Center: FY2011 Workload and Cost Report” [accessed on November 8, 2012]. Available at: http://vaww.arc.med.va.gov/vapublic/arci_sr4v3.asp?sDTP=11&sSO=2011FY
- Veterans Health Administration (VHA) Office of Community Care . 2017. Veterans Choice Program (VCP) Overview. Washington, DC: Department of Veteran Affairs. [Google Scholar]
- VHA Chief Business Office . 2012. “National Fee Program Office: Dialysis FY13 Contract Information” [accessed on November 8, 2012]. Available at: http://nonvacare.hac.med.va.gov/programs/dialysis-contract-information.asp
- VHA Enrollment and Forecasting . 2018. “Personal Communication: Dialysis Patients and Utilization by Care Location, 2006–2017.”
- Wang, V. , Maciejewski M. L., Patel U. D., Stechuchak K. M., Hynes D. M., and Weinberger M.. 2013. “Comparison of Outcomes for Veterans Receiving Dialysis Care from VA and Non‐VA Providers.” BMC Health Services Research 13: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, V. , Maciejewski M. L., Coffman C. J., Sanders L. L., Lee S. D., Hirth R., and Messana J.. 2017. “Impacts of Geographic Distance on Peritoneal Dialysis Utilization: Refining Models of Treatment Selection.” Health Services Research 52 (1): 35–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watnick, S. , and Crowley S. T.. 2014. “ESRD Care within the US Department of Veterans Affairs: A Forward‐Looking Program with an Illuminating Past.” American Journal of Kidney Diseases 63 (3): 521–9. [DOI] [PubMed] [Google Scholar]
- Yoon, J. , Scott J. Y., Phibbs C. S., and Wagner T. H.. 2011. “Recent Trends in Veterans Affairs Chronic Condition Spending.” Population Health Management 14 (6): 293–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Sampling Frame.
Appendix SA3. Visualization of Veteran Dialysis Settings, by Quarter.
Appendix SA4. All Veteran Patient Characteristics at Dialysis Initiation, Overall and by Veterans’ Dialysis Setting.
Appendix SA5. Regional Variation in Cross‐Sectional (Overall) Dialysis Setting, by Veterans. Integrated Service Network (VISN).
Appendix SA6. Multinomial Regression Model Output for Dialysis Setting Utilization.
Appendix SA7. Technical Description and Full Set of Regression Results: Zero‐Inflated Negative Binomial Regression Model Examining Number of Hospital Days over 2 Years Follow‐Up Period from Chronic Dialysis Initiation.


