Abstract
Objective
To describe variation in payer and outcomes in Veterans’ births.
Data/Setting
Secondary data analyses of deliveries in California, 2000–2012.
Study Design
We performed a retrospective, population‐based study of all live births to Veterans (confirmed via U.S. Department of Veterans Affairs (VA) enrollment records), to identify payer and variations in outcomes among: (1) Veterans using VA coverage and (2) Veteran vs. all other births. We calculated odds ratios (aOR) adjusted for age, race, ethnicity, education, and obstetric demographics.
Methods
We anonymously linked VA administrative data for all female VA enrollees with California birth records.
Principal Findings
From 2000 to 2012, we identified 17,495 births to Veterans. VA covered 8.6 percent (1,508), Medicaid 17.3 percent, and Private insurance 47.6 percent. Veterans who relied on VA health coverage had more preeclampsia (aOR 1.4, CI 1.0–1.8) and more cesarean births (aOR 1.2, CI 1.0–1.3), and, despite similar prematurity, trended toward more neonatal intensive care (NICU) admissions (aOR 1.2, CI 1.0–1.4) compared to Veterans using other (non‐Medicaid) coverage. Overall, Veterans’ birth outcomes (all‐payer) mirrored California's birth outcomes, with the exception of excess NICU care (aOR 1.15, CI 1.1–1.2).
Conclusions
VA covers a higher risk fraction of Veterans’ births, justifying maternal care coordination and attention to the maternal–fetal impacts of Veterans’ comorbidities.
Keywords: Maternal care, pregnancy, Veterans, health services, California
Rapid growth in the number of women serving in the U.S. military in the post 9/11 era (Street, Vogt, and Dutra 2009; McGraw, Koehlmoos, and Ritchie 2016) has been accompanied by an increasing number of reproductive‐aged Veterans using health care benefits from the U.S. Department of Veterans Affairs (VA) Health Care System after separation from service. While women remain a distinct minority, <7 percent, of the patient population cared for by the VA, the absolute number nearly doubled from 2003 to 2012 and likely will continue to rise (Frayne et al. 2014). Accordingly, the past decade has witnessed significant growth in VA's attention (programmatic and research) to women Veterans’ health care needs (Vogt, Barry, and King 2008; Yano et al. 2010, 2011; Bean‐Mayberry et al. 2011; Hayes 2011; Yano and Frayne 2011; Frayne et al. 2013; Maisel et al. 2015; Fox et al. 2016; Zephyrin 2016). At the same time, changes in VA's role as insurer (U.S. Congress 1996) led to the coverage of maternity care, and subsequent expansion (U.S. Congress 2010) to include newborns’ health care coverage in the first 7 days of life. The number of Veterans relying on VA for maternity benefits has steadily grown to a few thousand per year (Mattocks et al. 2014; Shaw et al. 2014). Any VA‐enrolled Veteran who becomes pregnant is eligible to use the VA maternity benefit, yet many may also have private insurance or are eligible for public Medicaid coverage once pregnant. Little is known about which Veterans opt to rely on VA coverage for their primary health insurance once pregnant.
Nearly all VA‐covered maternity care is provided as non‐VA services covered by the VA—that is, care provided by non‐VA community and/or academic obstetrical providers, but reimbursed by the VA (Mattocks et al. 2017a). Therefore, for a growing number of women Veterans, the VA has over a decade of experience acting as insurer for non‐VA maternity care. This provides a unique opportunity to explore differences in characteristics of Veterans, and their outcomes, stratified by whether they opt to use VA coverage for this specialty care. Such exploration is timely and might hold lessons directly relevant to the broader VA population, in light of the 2014 Veterans Choice Act (Farmer, Hosek, and Adamson 2016; Mattocks et al. 2017b) that has rapidly expanded eligibility for non‐VA care to be covered by the VA and ongoing plans (VA 2017b) to make it easier for Veterans to get care outside the VA.
Recognizing the challenges and unique needs of pregnant Veterans seeking VA maternity benefits, the VA developed guidelines for maternity health care coordination in 2012 (VA 2012). Care coordination is important because Veteran women have unique health considerations (Committee on Health Care for Underserved Women 2012). It is known that Veterans (Lehavot et al. 2012), and those engaged in the VA in particular (Agha et al. 2000), often have higher physical and mental health comorbidities and that the most recent wars’ era of female Veterans have high rates of psychiatric diagnoses (Street, Vogt, and Dutra 2009). Two recent studies of all VA‐covered births describe high mental health burden and find PTSD uniquely linked to pregnancy complications (Shaw et al. 2014, 2017). More broadly, there is concern that deployed servicewomen might face unrecognized reproductive health risks from exposures and stressors (physical and psychological) (Copper et al. 1996; Institute of Medicine 2007; Ryan et al. 2008; Holzman et al. 2009; Class et al. 2011; Okun, Schetter, and Glynn 2011; Conlin et al. 2012; Kajeepeta et al. 2014; Vadillo‐Ortega et al. 2014; Basu et al. 2017) encountered in the field of active combat.
Many pregnant Veterans, even those eligible and/or enrolled in the VA, turn to other sources of insurance for maternity care coverage and thus do not stand to benefit from the maternity care coordination efforts extended to VA‐covered pregnancies. However, methodological difficulties linking VA medical records to non‐VA claims data have limited the ability to examine such issues. Prior work looking at Veterans’ pregnancy complications or outcomes has been limited to the fraction of Veterans who are using VA to cover their care (Katon et al. 2014, 2017a; Shaw et al. 2014, 2017; Kroll‐Desrosiers et al. 2016) or relied on survey data limited to small subsample of Veteran mothers and focused on self‐reported outcomes (Katon et al. 2015). It remains unknown what fraction of eligible Veterans’ pregnancies the VA is covering, and how the health risks and pregnancy outcomes of mothers using VA maternity resources compare to their Veteran and non‐Veteran peers.
We aimed to better understand the needs of Veteran mothers by understanding their characteristics and risk profiles. Specifically, we examined linked California and VA data to describe: (1) fraction of eligible Veteran mothers for whom the VA provides maternity care coverage, (2) trends in other maternity care payers coverage for Veterans’ obstetric care over the past decade, (3) trends in preterm birth in Veterans, and (4) differences in obstetric risk profile and outcomes among Veteran pregnancies (VA and non‐VA covered) and the general population.
Methods
Study Design
This was a retrospective, population‐based observational study of all live births to confirmed Veterans in California from 2000 to 2012 (Figure S1). Veteran status was specified at the individual birth level and confirmed if the Veteran's VA recorded separation date from military service preceded the date of the delivery in question (i.e., for mothers with repeat deliveries, Veteran status was a time‐varying indicator). For all births to confirmed Veterans, we first compared characteristics (demographic, obstetric, and insurance payer) to all other California births; for comparability, the cohort was restricted to mothers aged 19 to 49. To broadly explore changes in characteristics of our cohort over time, we examined unadjusted trends in the fraction of Veterans’ births covered by each category of payer (VA, Medicaid, Private insurance, Military insurance, Other government payer, or Self‐pay/unknown). Similarly, to observe any gross changes in outcomes we examined unadjusted trends over time in preterm birth rates, comparing Veteran to all other California births. To understand differences in women Veterans who did and did not rely on VA maternity coverage, we first compared their characteristics. We then used multivariable regression to perform adjusted comparisons of Veterans’ obstetric outcomes by payer status (VA, Medicaid, or Private/other). Lastly, to understand Veteran mothers’ obstetric risk profile, we compared obstetric outcomes for all Veteran births (regardless of payer) to outcomes for all other California births.
Data Sources/Study Setting
Secondary data analyses were used to identify all in‐hospital deliveries in California to VA‐enrolled Veterans, using linked California birth data and VA administrative data. For obstetric and demographic data, we used a previously described (Herrchen, Gould, and Nesbitt 1997; Phibbs et al. 2007) combined state database maintained by the California Office of Statewide Health Planning and Development that consists of all obstetric discharge claims linked to birth certificate data (2000–2012, n = 6,605,973). For Veteran‐specific data, we used several data sources previously described and available through the VA Corporate Data Warehouse (Fihn et al. 2014). Status as a VA‐enrolled Veteran (subsequently referred to as “Veteran” for simplicity) was identified and confirmed based on VA enrollment files (VA Information Resource Center 2011) (last queried February 5, 2017), as well as the Beneficiary Identification Records Locator Subsystem (BIRLS)(Page 1991) death file, Veterans Services Network Corporate Mini Master file (VETSNET)(VA Information Resource Center 2011; Maynard et al. 2018), and files from the VA Corporate Data Warehouse Patient 2.0 domain (VA 2017a) (all last queried August 9, 2017). The remaining Veteran‐specific covariates were also obtained from the VA Corporate Data Warehouse and included files such as clinical encounter‐derived datasets for VA inpatient and outpatient care, and purchased care files (i.e., non‐VA care covered by the VA), most from 1998 onward.
Data Collection/Extraction Methods
Data Linkage
VA enrollment data for all reproductive‐age female VA enrollees were linked with California birth records (birth certificate and hospital discharge summary abstracts derived from claims data), which provided key descriptive characteristics and obstetric diagnoses. All analysis was done on a dataset that had been anonymized after linkage. Linkage was done by an independent third party, using access to minimal necessary confidential information (i.e., no analytic variables were in the data files for the linkages), in a partitioned VA environment accessible only to this third party, using previously developed, but modified probabilistic match techniques (Herrchen, Gould, and Nesbitt 1997; Danielsen 2000) which first match Social Security Number (SSN) and second match maternal date of birth and name. Our match technique (Herrchen, Gould, and Nesbitt 1997; Danielsen 2000) retains all matches above a critical match threshold that was based on extensive clerical review of linked records (i.e., we did not only retain perfect matches). Due to our inability to determine a base population (i.e., not knowing the true denominator of the number of VA‐enrolled women who have given birth in California in a year), it was not possible to generate match percentages to describe the overall success of the linkage. However, we were able to use the subcohort of known VA‐covered births that occurred in Veterans with evidence of residency or VA‐assigned care in California, and use that denominator to determine linkage yield, as an estimate for overall linkage success: 95.3 percent. The third party's linkage result consisted of a crosswalk of the anonymized VA and birth record identifiers. The finder file was then destroyed, after it had been used to create the crosswalk file, which replaced SSNs with anonymized VA identifiers and paired each with the unique identifier for the matched birth records from the California database.
We used both VA claims data (indicating the VA paid for the maternity care) and insurance codes from California birth data (Braveman et al. 1998) to identify the payer. We used VA data to identify and confirm Veteran status and determine the date of termination of military service. We obtained approval from the VA (via the Stanford University Institutional Review Board) and the State of California Health and Human Services Agency (via the Office of Statewide Health Planning and Development, Committee for the Protection of Human Subjects, and the California Department of Public Health's Vital Statistics Advisory Committee) to perform the linkage and study.
Covariates
Maternal age, parity, race, ethnicity (Baumeister et al. 2000), and highest education level (as an indicator of socioeconomic status) were derived from birth certificate data and were considered relevant covariates as they are known to strongly associate with pregnancy outcomes, especially preterm birth. Likewise, gestations involving multiples (twins or higher order) were identified using birth certificate and maternal and infant hospital discharge summaries.
Obstetric Outcomes
For obstetric outcomes, we focused on the two most common and high cost outcomes—preterm and cesarean births—and the most prevalent subacute antepartum complications—gestational diabetes and preeclampsia. Additionally, as a proxy for infant complications we identified newborns with admission to the neonatal intensive care unit (NICU).
We principally relied on birth certificate data to identify estimated gestational age. For our primary analysis, we used the gestational age estimate derived from reported last menstrual period, as this value was available across all study years. In instances where the gestational age was missing, we applied the Kotelchuck algorithm (Kotelchuck 1994; Remy and Oliva 2006) to impute gestational age from birthweight and gender values. In sensitivity analysis, we explored alternative use of “best obstetric estimate” of gestational age, which is a relatively new variable (Dietz et al. 2007) only available in our California birth certificate data from 2007 onward. Throughout, we identified preterm birth as delivery prior to 37 weeks’ gestation and further subcategorized preterm birth by gestational age into very preterm (<32 weeks) and moderate to late preterm (32 to <37 weeks). To further examine variation in preterm birth, we attempted to characterize any observed increased risk as attributable to spontaneous or medically induced preterm births, using a previously developed algorithm (Shachar et al. 2016) that combines birth certificate and discharge summary data to subtype preterm births as “spontaneous,” “medically indicated,” or “unknown.” Cesarean deliveries were identified by the presence of any indication of cesarean section within either the birth certificate or the discharge summary data (i.e., DRG or ICD‐9 procedure codes) (Lydon‐Rochelle et al. 2005; Yasmeen et al. 2006). For gestational diabetes (GDM) and preeclampsia, we relied on discharge summary abstract data as the most reliable source (Devlin, Desai, and Walaszek 2009; Haghighat et al. 2016). To identify newborns with more than routine newborn care, we used an algorithm (see Table S1) to estimate use of neonatal intensive care (NICU) services; the algorithm uses an approach that combines infant length of stay with birth certificate and/or discharge data indicating NICU level of care was likely provided.
Analysis
The analytic cohort was restricted to births at maternal age 19 to 49 and gestational age >20 weeks (to remove likely fetal demise). Analyses were performed using SAS 9.3 and STATA 14.0. We performed unadjusted statistical comparison of maternal characteristics between Veteran and all other California births, and between VA‐covered, Medicaid‐covered, and Private/other payer Veteran births. Comparisons of obstetric outcomes were modeled using generalized estimating equation models, with clustering by maternal identifier and robust standard errors to account for repeated measures (i.e., mothers with repeat births), to estimate adjusted odds ratios (aOR) and 95 percent confidence intervals (CIs). All models were adjusted for age, education, race, ethnicity, maternal parity, and higher order gestations. The regression models for preterm birth were analyzed first for any preterm birth (<37 weeks) and then separately for moderately preterm (32 to <37 weeks) and very preterm (<32 weeks). If the predictor of interest was associated with preterm birth, we then explored whether the excess risk was suggested to be due to spontaneous preterm birth, by running three additional models for each of the algorithmically assigned outcomes of “spontaneous,” “medically indicated,” or “unknown.” Lastly, in sensitivity analysis, we reran all models of preterm birth restricted to births in years 2007–2012, first with the gestational age derived from the last menstrual period estimate, then with the gestational age derived from the more recently introduced birth certificate field “best obstetric estimate.”
Results
From 2000 to 2012, there were 17,495 births to 13,032 confirmed Veterans representing 0.3 percent of the 6.6 million births to women aged 19–49 in California. Roughly half were covered by Private insurance, which decreased (from 58 percent to 40 percent) gradually (Figure 1). Medicaid, the next most common payer for Veteran births, remained relatively stable (from 17 percent to 15 percent) while coverage by the military health care system (TRICARE) increased from 16 percent to 25 percent. From 2000 to 2012, the proportion of VA‐covered births grew linearly from <2 percent to 14 percent. Overall, VA was the payer for 9 percent (n = 1,508). The trends in preterm birth prevalence among Veterans (starting at 94 and ending at 92 per 1,000 live births) generally mirrored California's overall (starting at 101 and ending at 93 per 1,000 live births), with a similar peak midway through the decade at 119 per 1,000 live births (vs. 111 per 1,000 for California overall) (Figure S2). Veterans, compared to all other California mothers, were just slightly older on average, more frequently black, and much less likely to be Hispanic or lack a high school diploma, all at level of significance p < .001 (Table 1).
Figure 1.
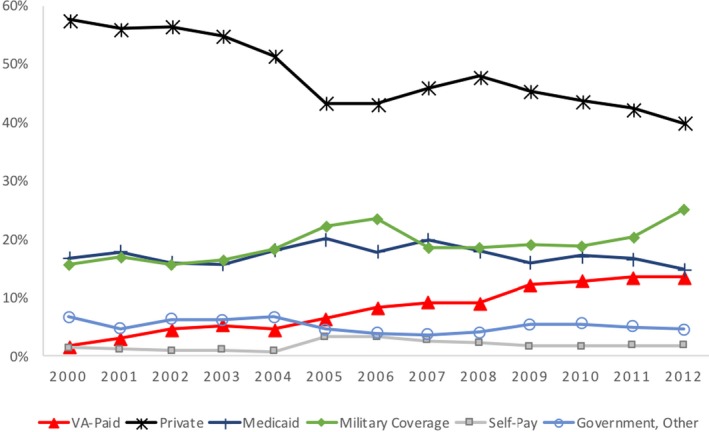
- Note: *Based on 17,495 births representing the successful linkage of California birth records to VA enrollee records, the linkage yield is an estimated 95 percent, based on proxy of the successful linkage rate observed among the subpopulation of VA‐covered births (i.e., the subpopulation for which the true total of California Veteran births was known). [Color figure can be viewed at http://www.wileyonlinelibrary.com/]
Table 1.
Characteristics of California Births, among VA‐enrolled Veterans and the General Population (aged 19–49), 2000–2012
| VA‐enrolled Veterans’ Births | All Other Births | |||
|---|---|---|---|---|
| 17,495 (0.3%) | 6,588,478 (99.7%) | |||
| n | % | n | % | |
| Unique mothersa | 13,032 | n/a | 4,825,676 | n/a |
| Maternal Age in years, Mean (SD)b | 28.9 (5.3) | 28.3 (6) | ||
| 19–24 | 3,028 | 23.2 | 1,505,631 | 31.2 |
| 25–29 | 4,602 | 35.3 | 1,316,749 | 27.3 |
| 30–34 | 3,295 | 25.3 | 1,189,311 | 24.6 |
| 35–39 | 1,631 | 12.5 | 640,889 | 13.3 |
| 40–49 | 476 | 3.7 | 173,096 | 3.6 |
| Maternal race | ||||
| Black | 1,848 | 14.2 | 246,635 | 5.1 |
| White | 9,371 | 71.9 | 3,742,676 | 77.5 |
| Asian/Pacific Islander | 801 | 6.2 | 607,290 | 12.6 |
| Other/Unknown | 463 | 3.6 | 149,240 | 3.1 |
| Multiracec | 549 | 4.2 | 79,835 | 1.7 |
| Maternal ethnicity: Hispanic | 3,182 | 24.4 | 2,524,406 | 52.3 |
| Maternal educationd | ||||
| <High school | 256 | 2 | 1,322,699 | 27.4 |
| High school graduate | 3,298 | 25.3 | 1,247,418 | 25.9 |
| Some college, but <4 years | 5,864 | 45 | 988,414 | 20.5 |
| College graduate | 2,148 | 16.5 | 671,738 | 13.9 |
| Some graduate education | 1,099 | 8.4 | 453,463 | 9.4 |
| Payer | ||||
| VA | 1,508 | 8.6 | n/a | n/a |
| Medicaid | 3,026 | 17.3 | 2,868,960 | 43.5 |
| Private Insurance | 8,325 | 47.6 | 3,316,599 | 50.3 |
| TRICARE/Birth in DoD Hospital | 3,403 | 19.5 | 96,360 | 1.5 |
| Self‐Pay or Unknown | 337 | 1.9 | 231,287 | 3.5 |
| Other Government Payer | 892 | 5.1 | 70,532 | 1.1 |
| Unattended birth | 4 | <0.1 | 4,740 | 0.1 |
| Obstetric profile | ||||
| Twins/higher order | 657 | 3.8 | 213,399 | 3.2 |
| Paritye: Multiparous | 10,758 | 61.5 | 4,190,121 | 63.6 |
All comparisons were p ≤ .001 aside from payer: Unattended birth (p = .01); p‐values were derived using chi‐square/Fisher's exact test for categorical, and t‐test for continuous variables.
1,133 mothers had ≥1 VA‐enrolled Veteran birth(s) and ≥1 all other birth(s), suggesting they had deliveries both before and after obtaining Veteran status. Statistical testing shown for unadjusted comparisons excludes those individuals; subsequent adjusted models take into account within‐subject correlation for repeated individuals.
Age restricted to >18 for comparability; for mothers with >1 birth in data, statistics are based on age at first birth.
This category was introduced newly to birth data in 2003, so applies only for births 2003–2012
Missing for VA 367 (2.8%); all other 141,944 (2.9%)
Missing for VA 7 (0.04%); all other 5,749 (0.09%)
DoD, Department of Defense; TRICARE, US Military insurance for service members and beneficiaries; VA, Department of Veterans Affairs Health Care System
Comparing Veterans who relied on VA coverage, Medicaid coverage, or Private/other coverage for maternity care, there was only minimal difference in age, race, and ethnicity; those using VA coverage were most similar to those using Private/other coverage. Veterans using Medicaid were slightly younger and more likely to be black and Hispanic. For those using VA coverage, there were more marked differences in past experience (Table 2). Specifically, Veterans who relied on VA coverage for their pregnancy were most likely (49 percent) to be first time mothers, and nearly twice as likely (28 percent vs 17 percent, p < .001) to have deployed in support of combat Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) than those Veterans who relied on Medicaid. Almost all Veterans using VA coverage had also recently engaged in VA outpatient clinical care, in contrast to the VA‐enrolled Veterans who used Medicaid or Private/other coverage for their maternity care (98 percent vs. 35 percent and 28 percent, respectively, had VA encounters in the two years prior to delivery, p < .001).
Table 2.
Characteristics of Births among VA‐enrolled Veterans in California, 2000–2012: VA versus Medicaid versus Private/other Covered
| VA‐covered Veteran Births | Medicaid‐covered Veteran Births | Private/other covered Veteran Births | ||||
|---|---|---|---|---|---|---|
| 1,508 (8.6%) | 3,026 (17.3%) | 12,961 (74.1%) | ||||
| n | % | n | % | n | % | |
| Unique mothersa | 1,297 | n/a | 2,462 | n/a | 10,083 | n/a |
| Maternal age in years, mean (SD)b | 28.8 (4.9) | n/a | 27.4 (5.2) | n/a | 29.4 (5.3) | n/a |
| 19–24 | 249 | 19.2 | 834 | 33.9 | 2,028 | 20.1 |
| 25–29 | 560 | 43.2 | 895 | 36.3 | 3,492 | 34.6 |
| 30–34 | 301 | 23.2 | 464 | 18.9 | 2,777 | 27.5 |
| 35–39 | 145 | 11.2 | 205 | 8.3 | 1,389 | 13.8 |
| 40–49 | 42 | 3.2 | 64 | 2.6 | 397 | 3.9 |
| Maternal race | ||||||
| Black | 165 | 12.7 | 457 | 18.6 | 1,330 | 13.2 |
| White | 876 | 67.5 | 1,694 | 68.8 | 7,378 | 73.2 |
| Asian/Pacific Islander | 98 | 7.6 | 113 | 4.6 | 637 | 6.3 |
| Other/Unknown | 74 | 5.7 | 89 | 3.6 | 335 | 3.3 |
| Multiracec | 84 | 6.5 | 109 | 4.4 | 403 | 4 |
| Maternal Ethnicity: Hispanic | 332 | 25.6 | 832 | 33.8 | 2,282 | 22.6 |
| Maternal educationd | ||||||
| <High school | 8 | 0.6 | 183 | 7.4 | 83 | 0.8 |
| High school graduate | 244 | 18.8 | 865 | 35.1 | 2,363 | 23.4 |
| Some college, but <4 years | 688 | 53.1 | 1,144 | 46.5 | 4,480 | 44.4 |
| College graduate | 229 | 17.7 | 157 | 6.4 | 1,867 | 18.5 |
| Some graduate education | 68 | 5.2 | 40 | 1.6 | 1,027 | 10.2 |
| Payer | ||||||
| VA | 1,508 | 100.0 | – | – | – | – |
| Medicaid | – | – | 3,026 | 100.0 | – | – |
| Private insurance | – | – | – | – | 8,325 | 64.2 |
| TRICARE/Birth in DoD Hospital | – | – | – | – | 3,403 | 26.3 |
| Self‐pay or Unknown | – | – | – | – | 337 | 2.6 |
| Other Government Payer | – | – | – | – | 892 | 6.9 |
| Unattended birth | – | – | – | – | 4 | <1 |
| Obstetric profile | ||||||
| Twins/higher order | 54 | 3.6 | 82 | 2.7 | 521 | 4 |
| Paritye: Multiparous | 773 | 51.3 | 2,027 | 67.0 | 7,958 | 61.4 |
| VA status prior to delivery | ||||||
| VA health care usef | ||||||
| Use within 2 years prior to delivery | 1,470 | 97.5 | 1,055 | 34.9 | 3,605 | 27.8 |
| Use within gestational period | 1,396 | 92.6 | 722 | 23.9 | 2,063 | 15.9 |
| Deployment History | ||||||
| OEF/OIF | 428 | 28.4 | 521 | 17.2 | 2,094 | 16.2 |
| Persian Gulf | 66 | 4.4 | 96 | 3.2 | 448 | 3.5 |
All comparisons were p ≤ .001 aside from Obstetric Profile: Twins/higher order (p = .003) and VA Status prior to Delivery: Deployment History—Persian Gulf (p = .11); p‐values were derived using chi‐square for categorical, and analysis of variance for continuous variables.
Eighty‐two mothers had ≥1 VA‐covered birth(s) and ≥1 Medicaid‐covered birth(s); 208 mothers had ≥1 VA‐covered birth(s) and ≥1 other birth(s). The above statistical testing for unadjusted comparisons exclude those individuals; subsequent adjusted models take into account within‐subject correlation for repeated individuals.
Age restricted to >18 for comparability; for mothers with >1 birth in data, statistics are based on age at first birth.
This category was introduced newly to birth data in 2003, so applies only for births 2003–2012.
Missing for VA‐covered n = 60 (4.6%), Medicaid n = 73 (3%), and for other payer n = 263 (2.6%).
Missing for Medicaid n = 1 (0.03%) and for other payer n = 6 (0.05%).
Indicated by at least 1 face‐to‐face mental health, substance use disorder, women's health clinic, and/or general primary care clinic visit.
DoD, Department of Defense; OEF/OIF, Operation Enduring Freedom and Operation Iraqi Freedom; TRICARE, US Military insurance for service members and beneficiaries; VA, Department of Veterans Affairs.
Comparison of obstetric outcomes for Veterans who used VA maternity coverage to those using Medicaid or those using Private/other coverage showed roughly similar prevalence of preterm birth by subtypes and overall (Table 3). After full adjustment, only those using Medicaid coverage demonstrated increased risk or preterm birth (aOR 1.29, CI 1.11–1.49), apparently driven predominantly by increased moderate–mild preterm (32–37 weeks; aOR 1.28, CI 1.10–1.50) and spontaneous preterm deliveries (aOR 1.39, CI 1.14–1.69), when compared to Private/other covered Veterans (Table 3). In sensitivity analysis (Table S2), using the newer birth certificate‐derived “best obstetric estimate” for gestational age, the observed risk of preterm birth for Medicaid‐covered Veterans disappeared (aOR 0.94, CI 0.75–1.19). For VA‐covered births, when compared to Private/other covered births, there was no significant difference in preterm birth risk, in the main adjusted models (Table 3) or in the sensitivity analyses (Table S3).
Table 3.
Unadjusted and Adjusted Birth Outcomes in California, 2000–2012, among VA‐enrolled Veterans: VA vs Medicaid vs Private/other Covered
| VA‐Covered, n = 1,508 (8.6%) | Medicaid‐Covered, n = 3,026 (17.3%) | Private/other Covered, n = 12,961 (74.1%) | Adjusted Model (Reference = Private/Other Covered) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VA‐Covered | Medicaid‐Covered | |||||||||||
| n | % | n | % | n | % | OR | 95% CI | OR | 95% CI | |||
| Preterm birtha | 148 | 9.8 | 355 | 11.7 | 1,306 | 10.1 | 1.00 | 0.82 | 1.22 | 1.29*** | 1.11 | 1.49 |
| 32 to <37 weeks | 123 | 8.2 | 296 | 9.8 | 1,104 | 8.5 | 0.99 | 0.80 | 1.22 | 1.28** | 1.10 | 1.50 |
| <32 weeks | 25 | 1.7 | 59 | 2 | 202 | 1.6 | 1.03 | 0.63 | 1.66 | 1.21 | 0.84 | 1.73 |
| Preterm subtype | Not Applicableb | |||||||||||
| Spontaneous | 83 | 5.5 | 179 | 5.9 | 650 | 5.0 | 1.39*** | 1.14 | 1.69 | |||
| Medically indicated | 49 | 3.3 | 123 | 4.1 | 438 | 3.4 | 1.31* | 1.03 | 1.67 | |||
| Unknown | 16 | 1.1 | 53 | 1.7 | 218 | 1.7 | 0.90 | 0.65 | 1.25 | |||
| Cesarean delivery | 533 | 35.3 | 972 | 32.1 | 4,148 | 32 | 1.18** | 1.05 | 1.32 | 1.10* | 1.01 | 1.20 |
| Gestational diabetesc | 109 | 7.2 | 171 | 5.6 | 677 | 5.2 | 1.15 | 0.91 | 1.45 | 0.96 | 0.79 | 1.16 |
| Preeclampsiac | 68 | 4.5 | 97 | 3.2 | 360 | 2.8 | 1.37* | 1.03 | 1.81 | 1.01 | 0.78 | 1.31 |
| Infant NICU stayd | 197 | 13.1 | 303 | 10 | 1,199 | 9.3 | 1.17 | 0.97 | 1.40 | 0.96 | 0.82 | 1.12 |
*p ≤ .05; **p ≤ .01; ***p ≤ .001.
All models adjust for age, race, ethnicity, education level, parity, and twins/higher order gestation.
High rates of missingness for the last three rows, which are discharge data derived outcomes, are predominantly (>90%) attributable to births at Military hospitals and/or under Military insurance, as the database maintained by the California Office of Statewide Health Planning and Development lacks discharge claims data for these federally covered births.
Records of preterm birth and preterm subtype missing for 38 (2.5%) VA paid births, 113 (3.7%) Medicaid paid births, and 419 (3.2%) other payer births.
Preterm subtype is not modeled because the predictor was not associated with an overall increased risk of preterm birth.
Missing for 11 (0.7%) VA paid births, 27 (0.9%) Medicaid paid births, and 2,991 (23.1%) other payer births.
Missing for 65 (4.3%) VA paid births, 176 (5.8%) Medicaid paid births, and 3,236 (25%) other payer births.
VA‐covered mothers were significantly more likely to suffer preeclampsia (4.5 percent) than their Medicaid‐covered (3.2 percent) or Private/other covered (2.8 percent) peers, and this remained after adjustment (aOR 1.37, CI 1.03–1.81, reference = Private/other coverage) (Table 3). Rates of gestational diabetes among VA covered (7.2 percent), Medicaid‐covered (5.6 percent) and Private/other covered (5.2 percent) did not significantly differ in adjusted models. Both VA‐covered (aOR 1.18, CI 1.05–1.32) and Medicaid‐covered (aOR 1.10, CI 1.01–1.20) Veterans were more likely to deliver by cesarean delivery than those with Private/other coverage. Despite similar rates of preterm birth, 13.1 percent of newborns delivered under VA coverage received NICU‐level care vs. 9.3 percent under Private/other coverage, a difference which trended toward significance (aOR 1.17, CI 0.97–1.40). No increased risk of NICU care was observed for the infants of Medicaid‐covered Veterans, despite them having the highest prevalence of preterm birth.
Lastly, to understand how the obstetric risk profile of VA‐enrolled Veterans compared to the general population, we examined differences for all‐payer birth outcomes. On average, there were few differences in maternal outcomes between VA‐enrolled Veterans and other California women (Table 4), with identical prevalence of preterm birth and similar rates of cesarean. There was suggestion of lower rates of gestational diabetes among Veterans (5.5 percent vs. 7.3 percent), which was initially observed to be significant when risk was only age‐adjusted (aOR 0.81, CI 0.75–0.87, not shown), but appeared to be explained by variation in baseline risk by race and ethnicity, as the effect disappeared after further adjustment, and was null in the fully adjusted model (Table 4). Similarly, an increased risk of preeclampsia was found for Veterans when risk was only age‐adjusted (aOR 1.14, CI 1.04–1.24, not shown) that attenuated markedly (Table 4) once full adjustment accounted for the markedly higher black, non‐Hispanic make‐up of the Veteran cohort. NICU‐level care was a notable exception among the outcomes examined, as it remained slightly elevated for Veteran births, even after full adjustment (aOR 1.15, CI 1.09–1.22).
Table 4.
Unadjusted and Adjusted Birth Outcomes in California, 2000–2012: VA‐enrolled Veterans vs General Population
| Veteran Births, n = 17,495 (0.3%) | All other California Births, n = 6,588,478 (99.7%) | Adjusted Model (Reference = All other CA births) | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | OR | 95% CI | ||
| Preterm birtha | 1,809 | 10.3 | 680,891 | 10.3 | 0.99 | 0.94 | 1.05 |
| 32 to <37 weeks | 1,523 | 8.7 | 574,100 | 8.7 | 1.00 | 0.94 | 1.06 |
| <32 weeks | 286 | 1.6 | 106,791 | 1.6 | 0.96 | 0.84 | 1.09 |
| Cesarean delivery | 5,653 | 32.3 | 2,069,741 | 31.4 | 1.02 | 0.99 | 1.06 |
| Gestational Diabetesb | 957 | 5.5 | 480,932 | 7.3 | 0.96 | 0.90 | 1.04 |
| Preeclampsiab | 525 | 3.0 | 205,514 | 3.1 | 1.04 | 0.94 | 1.15 |
| Infant NICU stayc | 1,699 | 9.7 | 632,778 | 9.6 | 1.15*** | 1.09 | 1.22 |
*p ≤ .05; **p ≤ .01; ***p ≤ .001.
All models adjusted for age, race, ethnicity, education level, parity, and twins/higher order gestation.
High rate of missingness for the last three discharge data derived outcomes is predominantly (>90%) attributable to births at Military hospitals and/or under Military insurance, as the database maintained by the California Office of Statewide Health Planning and Development lacks discharge claims data for these federally covered births.
Records of preterm birth and preterm subtype missing for 570 (3.3%) Veteran births and 261,997 (4%) of other births.
Missing for 3,029 (17.3%) Veteran births and 177,721 (2.7%) of other births
Missing for 3,477 (19.9%) Veteran births and 467,255 (7.1%) other births.
Discussion
In this, the first study to link VA and state‐level birth data to explicitly examine obstetric care and outcomes, we find that for every VA‐covered birth there are more than 10 additional births to VA‐enrolled Veterans using other sources of coverage (e.g., Private insurance, Medicaid, or Military TRICARE). Thus, the VA has no birth data for the vast majority of enrolled Veterans’ pregnancies. For VA‐enrolled Veterans, Private insurance remains the leading source of coverage for maternity care, with the Military TRICARE insurance and Medicaid being the next most common sources of coverage. Still, over the past decade the fraction using VA has significantly increased, such that the proportion of Veteran births covered by VA (14 percent) nearly equaled those covered by Medicaid (15 percent) in 2012. Reassuringly, across that same period, outcomes for Veterans’ births, including preterm birth, appear largely on par with outcomes for the age‐comparable population.
Strikingly, however, when comparing Veterans who rely on VA coverage to their peers who use other coverage for their pregnancies, we encounter compelling evidence that as a maternity care payer, the VA is covering a disproportionately higher obstetric risk group of Veteran mothers. This is true not only in comparing VA‐covered Veterans to those using Private insurance, but also when comparing them to Veterans relying on Medicaid—a population that is typically lower socioeconomic status and might be expected to be more comparable in risk. We find that preeclampsia is uniquely elevated among the VA‐covered, but not the Medicaid‐covered Veteran. Similarly, we see a trend toward greater NICU use by infants of VA‐covered births. It is only thanks to the unique linkage of state‐level vital statistics and birth data that we gained insight, not only into the Veteran mothers for whom the VA is providing care, but also those Veterans for whom it does not. Our findings reiterate the importance of not simply relying on VA data (Halanych et al. 2006) when exploring disparities in care or outcomes for VA‐eligible Veterans.
In our study, Veterans using VA for maternity care coverage were much more likely to be users of VA health care services prior to and during pregnancy. In a survey of VA Veteran mothers eligible for VA maternity benefits from 2008 to 2009 (n = 324) (Katon et al. 2015), users of VA maternity benefits appeared to be a “higher risk” population based on 2.5‐fold rates of depression diagnosis, and 3 to 5 times higher reported rates of current symptoms of PTSD or depression as compared to VA Veterans who used other insurance for maternity coverage. Those findings of disproportionate mental health comorbidity among VA‐reliant mothers, combined with our documentation of increased risk in actual obstetric outcomes, strengthen the plausibility that such mental health diagnoses contribute to a poorer reproductive health profile for VA‐covered mothers.
The nearly 40 percent relative increase in risk of preeclampsia in VA‐covered Veterans is clinically significant. Preeclampsia remains difficult to predict or prevent, but its impacts can be greatly modified by early detection and management. Similarly of concern is the high absolute proportion of infants of VA‐covered mothers that experience NICU admission, despite no apparent increased risk of prematurity (typically the biggest driver of NICU admission). When combined with the observations that users of VA maternity care are more likely to have experienced combat deployment, and are more likely to be users of VA primary and mental health care services, it raises the concern that the heavy burden of mental and physical health conditions VA‐engaged Veterans carry may put them at increased risk of poorer birth outcomes.
Our preeclampsia finding is consistent with prior works documenting that OEF/OIF‐deployed Veterans have above average risk of complications (Katon et al. 2017a) and hypertensive disorders of pregnancy (Katon et al. 2014) and that active PTSD in Veterans specifically predicts increased risk of preeclampsia (Shaw et al. 2017). Our finding of increased preeclampsia in the VA‐covered populations suggests that PTSD, as a novel, but widespread, risk factor might plausibly translate to a detectable increased prevalence of preeclampsia across the VA‐engaged population. As the VA disproportionately serves and engages Veterans with high mental health needs, these findings suggest a need for more nuanced research and clinical attention to Veterans' newborn outcomes, with focus on potential physiologic (e.g., preeclampsia) and pharmaceutical (e.g., psychotropic medication) maternal–fetal exposures associated with psychiatric comorbidity.
Our study's confirmation that VA‐covered pregnancies are higher risk for both mother and newborn has clear policy implications. It highlights that program cost planning should account for higher obstetric care costs for these Veterans, and it reinforces the importance of tailoring care for Veterans and care coordination between VA care providers and non‐VA obstetric care providers. Our observation that 2 percent of Veteran births had no evidence of any payer (i.e., “Self‐pay or unknown”) might also suggest a subgroup of Veterans important for the VA to reach in maternity care coordination efforts, and highlights the importance of VA and non‐VA data linkages to identify gaps in Veterans coverage and care.
In 2012, the VA Office of Women's Health Services issued a Maternity Health Care and Coordination policy that mandated creation of a maternity care coordinator within each regional VA health care system to ensure appropriate care including screening and provision for mental health needs (VA 2012). Early efforts to evaluate implementation of this novel maternity care coordination role within the VA are ongoing and, appropriately, include significant focus on addressing mental and psychosocial needs in the antepartum and postpartum period (Katon et al. 2017b; Mattocks et al. 2017a). Our findings highlight the importance of such efforts and reinforce prior calls (Mattocks 2015; Shivakumar, Anderson, and Surís 2015) to ensure that common mental health conditions among Veterans, such as depression and PTSD, receive appropriate ongoing treatment around pregnancy (including preconception counseling and during the susceptible period postpartum) and aspirations for an overarching system of maternity care coordination that spans VA providers and community‐based obstetrical providers.
More broadly, this work holds lessons directly relevant to the general VA population, in light of ongoing policy shifts including the Veterans Choice Act (Farmer, Hosek, and Adamson 2016; Mattocks et al. 2017b; VA 2017b) that expand the opportunities and likelihood that Veterans (beyond those requiring maternity care) will seek VA‐reimbursed care in non‐VA health care settings. Early research of 3 years of experience of the Veterans Choice Act has demonstrated some of the complexities, gaps, and inefficiencies in this effort to expand Veterans’ care into the community (Mattocks and Yehia 2017). For more than a decade prior to the Veterans Choice Act, VA‐covered maternity care has analogously reimbursed non‐VA providers for specialty care and faced the challenges inherent in tracking and coordinating care provided for covered Veterans. In the face of these challenges, the VA Office of Women's Health Services developed clinically relevant “Health Care and Coordination” policies (VA 2012) that mandate staffing with Maternity Care Coordinator roles, in acknowledgment that pregnant women using VA coverage may have unique and complex care needs. Our study demonstrates that, indeed, risk profiles of Veterans vary importantly for those who engage and opt to use VA coverage.
Our work faces several limitations. First, our ability to identify Veterans remains limited to those women who at some time in the past two decades have enrolled in the VA. We inevitably miss upwards of half of the recent era of women Veterans who never enroll in VA (VA 2015). Nonetheless, the VA‐enrolled population is who the VA should reach out to first in its maternal care coordination efforts, and thus, the data shared in our study are of direct value to understanding who the VA serves. Second, California's Veterans' care patterns and needs may not be generalizable to other states. Internal factors, such as regional and local variation in the degree to which VA facilities have implemented gender‐specific Veteran care (Oishi et al. 2011; Reddy et al. 2016) may impact women Veterans' experience and thereby the rate of uptake of VA gender‐specific benefits such as maternity coverage. External social and policy factors likely also affect the generalizability of our single‐state study. For example, there is good reason to suspect that in other states with higher unemployment and/or less comprehensive state public insurance (Medicaid) benefits, there may be more need and use of VA coverage for maternity care. Third, while maternal discharge data are generally of high validity, for some obstetric conditions there is known to be moderate misclassification (Romano et al. 2005; Yasmeen et al. 2006); however, we have no reason to believe any such misclassification would be more prevalent in the discharge data of women relying on VA coverage. Lastly, we lacked hospital claims‐derived data for those Veterans who gave birth in Federal Department of Defense hospitals in California, and thus for outcomes that require discharge data for accuracy (e.g., preeclampsia and gestational diabetes), we were unable to include those births.
Despite these limitations, our novel methodology linking VA data with state‐level birth and obstetric discharge data in California, the most populous U.S. state, allowed a breadth of assessment of Veteran mothers and outcomes not previously feasible. Veterans are confirmed to be a higher risk obstetric population, with the VA covering an even higher risk subpopulation, and the fraction of Veterans using VA maternity coverage is now shown to rival the fraction relying on Medicaid for such benefits. As the VA disproportionately serves those with high mental and physical health needs, these findings reinforce the importance of current efforts (VA 2012; Katon et al. 2017b; Mattocks et al. 2017a) to coordinate on‐site VA care with off‐site maternity care, and suggest a need for more nuanced research and clinical attention to Veterans’ maternal and newborn outcomes.
Supporting information
Appendix SA1: Author Matrix.
Figure S1. Analytic Cohort.
Figure S2. Preterm Birth Rate (per 1,000 live births) among VA‐enrolled Veterans and All Mothers Age 19‐49, in California, 2000–2012.
Table S1. Algorithm to Estimate Use of Neonatal Intensive Care Unit (NICU).
Table S2. Sensitivity Test Using “Best Obstetric Estimate” versus “Last Menstrual Period” Variable for Estimated Gestational Age, to Model Preterm Birth Outcomes in California, 2007–2012, among VA‐enrolled Veterans.
Table S3. Sensitivity Test Using “Best Obstetric Estimate” versus “Last Menstrual Period” Variable for Estimated Gestational Age, to Model Preterm Birth Outcomes in California, 2007‐2012, VA‐enrolled Veterans vs General Population.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was funded by the U.S. Department of Veterans Affairs, Health Services Research and Development Grant # IIR 14‐099. We additionally would like to thank Jonathan Mayo of Stanford University, Jodie Katon of the University of Washington and the Puget Sound VA, and the VA Women's Health Services for their technical support in this work. An early version of this work was orally presented at the Department of Veterans Affairs HSR&D/QUERI National Conference, July 19, 2017, in Arlington, Virginia. All authors contributed substantially to the design, analysis, or interpretation of results of the study, as well as to editing of the final manuscript.
Disclosures: None.
Disclaimer: The content is solely the responsibility of the authors and does not represent the official views of the Department of Veterans Affairs.
References
- Agha, Z. , Lofgren R. P., VanRuiswyk J. V., and Layde P. M.. 2000. “Are Patients at Veterans Affairs Medical Centers Sicker? A Comparative Analysis of Health Status and Medical Resource Use.” Archives of Internal Medicine 160 (21): 3252–7. [DOI] [PubMed] [Google Scholar]
- Basu, R. , Pearson D., Ebisu K., and Malig B.. 2017. “Association Between PM 2.5 and PM 2.5 Constituents and Preterm Delivery in California, 2000–2006.” Paediatric and Perinatal Epidemiology 31 (5): 424–34. [DOI] [PubMed] [Google Scholar]
- Baumeister, L. , Marchi K., Pearl M., Williams R., and Braveman P.. 2000. “The Validity of Information on ‘Race’ and ‘Hispanic Ethnicity’ in California Birth Certificate Data.” Health Services Research 35 (4): 869–83. [PMC free article] [PubMed] [Google Scholar]
- Bean‐Mayberry, B. , Yano E. M., Washington D. L., Goldzweig C., Batuman F., Huang C., Miake‐Lye I., and Shekelle P. G.. 2011. “Systematic Review of Women Veterans’ Health: Update on Successes and Gaps.” Women's Health Issues 21 (4 Suppl): S84–97. [DOI] [PubMed] [Google Scholar]
- Braveman, P. , Pearl M., Egerter S., Marchi K., and Williams R.. 1998. “Validity of Insurance Information on California Birth Certificates.” American Journal of Public Health 88 (5): 813–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Class, Q. A. , Lichtenstein P., Långström N., and D'Onofrio B. M.. 2011. “Timing of Prenatal Maternal Exposure to Severe Life Events and Adverse Pregnancy Outcomes: A Population Study of 2.6 Million Pregnancies.” Psychosomatic Medicine 73 (3): 234–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Health Care for Underserved Women, American College of Obstetricians and Gynecologists . 2012. “Committee Opinion No. 547: Health Care for Women in the Military and Women Veterans.” Obstetrics and Gynecology 120 (6): 1538–42. [DOI] [PubMed] [Google Scholar]
- Conlin, A. M. S. , DeScisciolo C., Sevick C. J., Bukowinski A. T., Phillips C. J., and Smith T. C.. 2012. “Birth Outcomes Among Military Personnel After Exposure to Documented Open‐Air Burn Pits Before and During Pregnancy.” Journal of Occupational and Environmental Medicine 54 (6): 689–97. [DOI] [PubMed] [Google Scholar]
- Copper, R. L. , Goldenberg R. L., Das A., Elder N., Swain M., Norman G., Ramsey R., Cotroneo P., Collins B. A., Johnson F., Jones P., and Meier A. M.. 1996. “The Preterm Prediction Study: Maternal Stress Is Associated With Spontaneous Preterm Birth at Less Than Thirty‐Five Weeks’ Gestation. National Institute of Child Health and Human Development Maternal‐Fetal Medicine Units Network.” American Journal of Obstetrics and Gynecology 175 (5): 1286–92. [DOI] [PubMed] [Google Scholar]
- Danielsen, B . 2000. Probabilistic Record Linkages for Generating a Comprehensive Epidemiological Research File on Maternal and Infant Health. Rocklin, CA: Health Information Solutions. [Google Scholar]
- Devlin, H. M. , Desai J., and Walaszek A.. 2009. “Reviewing Performance of Birth Certificate and Hospital Discharge Data to Identify Births Complicated by Maternal Diabetes.” Maternal and Child Health Journal 13 (5): 660–6. [DOI] [PubMed] [Google Scholar]
- Dietz, P. M. , England L. J., Callaghan W. M., Pearl M., Wier M. L., and Kharrazi M.. 2007. “A Comparison of LMP‐Based and Ultrasound‐Based Estimates of Gestational Age Using Linked California Livebirth and Prenatal Screening Records.” Paediatric and Perinatal Epidemiology 21 (Suppl 2): 62–71. [DOI] [PubMed] [Google Scholar]
- Farmer, C. M. , Hosek S. D., and Adamson D. M.. 2016. “Balancing Demand and Supply for Veterans’ Health Care.” Rand Health Quarterly 6 (1). Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5158276/. [PMC free article] [PubMed] [Google Scholar]
- Fihn, S. D. , Francis J., Clancy C., Nielson C., Nelson K., Rumsfeld J., Cullen T., Bates J., and Graham G. L.. 2014. “Insights From Advanced Analytics At The Veterans Health Administration.” Health Affairs 33 (7): 1203–11. [DOI] [PubMed] [Google Scholar]
- Fox, A. B. , Hamilton A. B., Frayne S. M., Wiltsey‐Stirman S., Bean‐Mayberry B., Carney D., Di Leone B. A. L., Gierisch J. M., Goldstein K. M., Romodan Y., Sadler A. G., Yano E. M., Yee E. F., and Vogt D.. 2016. “Effectiveness of an Evidence‐Based Quality Improvement Approach to Cultural Competence Training: The Veterans Affairs’ ‘Caring for Women Veterans’ Program.” Journal of Continuing Education in the Health Professions 36 (2): 96–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frayne, S. M. , Carney D. V., Bastian L., Bean‐Mayberry B., Sadler A., Klap R., Phibbs C. S., Kimerling R., Vogt D., Yee E. F., Lin J. Y., and Yano E. M.. 2013. “The VA Women's Health Practice‐Based Research Network: Amplifying Women Veterans’ Voices in VA Research.” Journal of General Internal Medicine 28 (Suppl 2): S504–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frayne, S. M. , Phibbs C. S., Saechao F., Maisel N. C., Friedman S. A., Finlay A., Berg E., Balasubramanian V., Dally S. K., Ananth L., Romodan Y., Lee J., Iqbal S., Hayes P. M., Zephyrin L., Whitehead A., Torgal A., Katon J. G., and Haskell S.. 2014. Sourcebook: Women Veterans in the Veterans Health Administration. Volume 3. Sociodemographics, Utilization, Costs of Care, and Health Profile. Washington DC: Women's Health Evaluation Initiative, Women's Health Services, Veterans Health Administration, Department of Veterans Affairs.
- Haghighat, N. , Hu M., Laurent O., Chung J., Nguyen P., and Wu J.. 2016. “Comparison of Birth Certificates and Hospital‐Based Birth Data on Pregnancy Complications in Los Angeles and Orange County, California.” BMC Pregnancy and Childbirth 16: 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halanych, J. H. , Wang F., Miller D. R., Pogach L. M., Lin H., Berlowitz D. R., and Frayne S. M.. 2006. “Racial/Ethnic Differences in Diabetes Care for Older Veterans: Accounting for Dual Health System Use Changes Conclusions.” Medical Care 44 (5): 439–45. [DOI] [PubMed] [Google Scholar]
- Hayes, P. M . 2011. “Leading the Nation in Women's Health: The Important Role of Research.” Women's Health Issues, 21 (4, Supplement): S70–2. [DOI] [PubMed] [Google Scholar]
- Herrchen, B. , Gould J. B., and Nesbitt T. S.. 1997. “Vital Statistics Linked Birth/Infant Death and Hospital Discharge Record Linkage for Epidemiological Studies.” Computers and Biomedical Research 30 (4): 290–305. [DOI] [PubMed] [Google Scholar]
- Holzman, C. , Senagore P., Tian Y., Bullen B., Devos E., Leece C., Zanella A., Fink G., Rahbar M. H., and Sapkal A.. 2009. “Maternal Catecholamine Levels in Midpregnancy and Risk of Preterm Delivery.” American Journal of Epidemiology 170 (8): 1014–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (U.S.) . 2007. Preterm Birth: Causes, Consequences, and Prevention. Washington, D.C: National Academies Press. [PubMed] [Google Scholar]
- Kajeepeta, S. , Sanchez S. E., Gelaye B., Qiu C., Barrios Y. V., Enquobahrie D. A., and Williams M. A.. 2014. “Sleep Duration, Vital Exhaustion, and Odds of Spontaneous Preterm Birth: A Case–Control Study.” BMC Pregnancy and Childbirth, 14 (1). Available at: http://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/1471-2393-14-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon, J. , Mattocks K., Zephyrin L., Reiber G., Yano E. M., Callegari L., Schwarz E. B., Goulet J., Shaw J., Brandt C., and Haskell S.. 2014. “Gestational Diabetes and Hypertensive Disorders of Pregnancy Among Women Veterans Deployed in Service of Operations in Afghanistan and Iraq.” Journal of Women's Health 23 (10): 792–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon, J. G. , Washington D. L., Cordasco K. M., Reiber G. E., Yano E. M., and Zephyrin L. C.. 2015. “Prenatal Care for Women Veterans Who Use Department of Veterans Affairs Health Care.” Women's Health Issues 25 (4): 377–81. [DOI] [PubMed] [Google Scholar]
- Katon, J. , Cypel Y., Raza M., Zephyrin L., Reiber G., Yano E. M., Barth S., and Schneiderman A.. 2017a. “Deployment and Adverse Pregnancy Outcomes: Primary Findings and Methodological Considerations.” Maternal and Child Health Journal 21 (2): 376–86. 10.1007/s10995-016-2122-x. [DOI] [PubMed] [Google Scholar]
- Katon, J. G. , Lewis L., Hercinovic S., McNab A., Fortney J., and Rose S. M.. 2017b. “Improving Perinatal Mental Health Care for Women Veterans: Description of a Quality Improvement Program.” Maternal and Child Health Journal 21 (8): 1598–605. [DOI] [PubMed] [Google Scholar]
- Kotelchuck, M. 1994. “An Evaluation of the Kessner Adequacy of Prenatal Care Index and a Proposed Adequacy of Prenatal Care Utilization Index.” American Journal of Public Health 84 (9): 1414–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroll‐Desrosiers, A. R. , Skanderson M., Bastian L. A., Brandt C. A., Haskell S., Kerns R. D., and Mattocks K. M.. 2016. “Receipt of Prescription Opioids in a National Sample of Pregnant Veterans Receiving Veterans Health Administration Care.” Women's Health Issues: Official Publication of the Jacobs Institute of Women's Health 26 (2): 240–6. [DOI] [PubMed] [Google Scholar]
- Lehavot, K. , Hoerster K. D., Nelson K. M., Jakupcak M., and Simpson T. L.. 2012. “Health Indicators for Military, Veteran, and Civilian Women.” American Journal of Preventive Medicine 42 (5): 473–80. [DOI] [PubMed] [Google Scholar]
- Lydon‐Rochelle, M. T. , Holt V. L., Nelson J. C., Cárdenas V., Gardella C., Easterling T. R., and Callaghan W. M.. 2005. “Accuracy of Reporting Maternal In‐Hospital Diagnoses and Intrapartum Procedures in Washington State Linked Birth Records.” Paediatric and Perinatal Epidemiology 19 (6): 460–71. [DOI] [PubMed] [Google Scholar]
- Maisel, N. C. , Haskell S., Hayes P. M., Balasubramanian V., Torgal A., Ananth L., Saechao F., Iqbal S., Phibbs C. S., and Frayne S. M.. 2015. “Readying the Workforce: Evaluation of VHA's Comprehensive Women's Health Primary Care Provider Initiative.” Medical Care 53 (4 Suppl 1): S39–46. [DOI] [PubMed] [Google Scholar]
- Mattocks, K. 2015. “Mental Health Care Screening and Care Coordination During Pregnancy and Postpartum for Women Veterans.” Journal of Women's Health 24 (1): 1–2. [DOI] [PubMed] [Google Scholar]
- Mattocks, K. M. , and Yehia B.. 2017. “Evaluating the Veterans Choice Program: Lessons for Developing a High‐Performing Integrated Network.” Medical Care 55 Suppl 7 Suppl 1: 1–3. [DOI] [PubMed] [Google Scholar]
- Mattocks, K. M. , Frayne S., Phibbs C. S., Yano E. M., Zephyrin L., Shryock H., Haskell S., Katon J., Sullivan J. C., Weinreb L., Ulbricht C., and Bastian L. A.. 2014. “Five‐Year Trends in Women Veterans’ Use of VA Maternity Benefits, 2008–2012.” Women's Health Issues 24 (1): e37–42. [DOI] [PubMed] [Google Scholar]
- Mattocks, K. M. , Kuzdeba J., Baldor R., Casares J., Lombardini L., and Gerber M. R.. 2017a. “Implementing and Evaluating a Telephone‐Based Centralized Maternity Care Coordination Program for Pregnant Veterans in the Department of Veterans Affairs.” Women's Health Issues: Official Publication of the Jacobs Institute of Women's Health 27 (5): 579–85. [DOI] [PubMed] [Google Scholar]
- Mattocks, K. M. , Mengeling M., Sadler A., Baldor R., and Bastian L.. 2017b. “The Veterans Choice Act: A Qualitative Examination of Rapid Policy Implementation in the Department of Veterans Affairs.” Medical Care, 55 Suppl 7 Suppl 1: S71–5. [DOI] [PubMed] [Google Scholar]
- Maynard, C. , Trivedi R., Nelson K., and Fihn S. D.. 2018. “Disability Rating, Age at Death, and Cause of Death in U.S. Veterans With Service‐Connected Conditions.” Military Medicine Available at: https://academic.oup.com/milmed/advance-article/doi/10.1093/milmed/usy040/4954108. [DOI] [PubMed] [Google Scholar]
- McGraw, K. , Koehlmoos T. P., and Ritchie E. C.. 2016. “Women in Combat: Framing the Issues of Health and Health Research for America's Servicewomen.” Military Medicine 181 (1S): 7–11. [DOI] [PubMed] [Google Scholar]
- Oishi, S. M. , Rose D. E., Washington D. L., MacGregor C., Bean‐Mayberry B., and Yano E. M.. 2011. “National Variations in VA Mental Health Care for Women Veterans.” Women's Health Issues, 21(4, Supplement): S130–7. [DOI] [PubMed] [Google Scholar]
- Okun, M. L. , Schetter C. D., and Glynn L. M.. 2011. “Poor Sleep Quality Is Associated With Preterm Birth.” Sleep Available at: http://www.journalsleep.org/ViewAbstract.aspx?pid=28329, 10.5665/sleep.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page, W. F . ed. 1991. Epidemiology in Military and Veteran Populations: Proceedings of the Second Biennial Conference, March 7, 1990, Washington, DC: National Academy Press. [PubMed] [Google Scholar]
- Phibbs, C. S. , Baker L. C., Caughey A. B., Danielsen B., Schmitt S. K., and Phibbs R. H.. 2007. “Level and Volume of Neonatal Intensive Care and Mortality in Very‐Low‐Birth‐Weight Infants.” New England Journal of Medicine 356 (21): 2165–75. [DOI] [PubMed] [Google Scholar]
- Reddy, S. M. , Rose D. E., Burgess J. F., Charns M. P., and Yano E. M.. 2016. “The Role of Organizational Factors in the Provision of Comprehensive Women's Health in the Veterans Health Administration.” Women's Health Issues: Official Publication of the Jacobs Institute of Women's Health 26 (6): 648–55. [DOI] [PubMed] [Google Scholar]
- Remy, L. , and Oliva G.. 2006. Impact of Data Quality on Birth Related Indicators. San Francisco, CA: The Family Health Outcomes Project, University of California, San Francisco [accessed on November 28, 2017]. Available at: https://fhop.ucsf.edu/sites/fhop.ucsf.edu/files/wysiwyg/dATAQUAL7.pdf. [Google Scholar]
- Romano, P. S. , Yasmeen S., Schembri M. E., Keyzer J. M., and Gilbert W. M.. 2005. “Coding of Perineal Lacerations and Other Complications of Obstetric Care in Hospital Discharge Data.” Obstetrics and Gynecology 106 (4): 717–25. [DOI] [PubMed] [Google Scholar]
- Ryan, M. A. K. , Gumbs G. R., Conlin A. M. S., Sevick C. J., Jacobson I. G., Snell K. J., Spooner C. N., and Smith T. C., and for the Department of Defense Birth and Infant Health Registry Team . 2008. “Evaluation of Preterm Births and Birth Defects in Liveborn Infants of US Military Women Who Received Smallpox Vaccine.” Birth Defects Research Part A: Clinical and Molecular Teratology, 82 (7): 533–9. [DOI] [PubMed] [Google Scholar]
- Shachar, B. , Mayo J., Lyell D., Baer R., Jeliffe‐Pawlowski L., Stevenson D., and Shaw G.. 2016. “Interpregnancy Interval After Live Birth or Pregnancy Termination and Estimated Risk of Preterm Birth: A Retrospective Cohort Study.” BJOG: An International Journal of Obstetrics & Gynaecology 123 (12): 2009–17. [DOI] [PubMed] [Google Scholar]
- Shaw, J. G. , Asch S. M., Kimerling R., Frayne S. M., Shaw K. A., and Phibbs C. S.. 2014. “Posttraumatic Stress Disorder and Risk of Spontaneous Preterm Birth.” Obstetrics and Gynecology 124 (6): 1111–9. [DOI] [PubMed] [Google Scholar]
- Shaw, J. G. , Asch S. M., Katon J. G., Shaw K. A., Kimerling R., Frayne S. M., and Phibbs C. S.. 2017. “Post‐Traumatic Stress Disorder and Antepartum Complications: A Novel Risk Factor for Gestational Diabetes and Preeclampsia.” Paediatric and Perinatal Epidemiology 31 (3): 185–94. [DOI] [PubMed] [Google Scholar]
- Shivakumar, G. , Anderson E. H., and Surís A. M.. 2015. “Managing Posttraumatic Stress Disorder and Major Depression in Women Veterans During the Perinatal Period.” Journal of Women's Health 24 (1): 18–22. [DOI] [PubMed] [Google Scholar]
- Street, A. E. , Vogt D., and Dutra L.. 2009. “A New Generation of Women Veterans: Stressors Faced by Women Deployed to Iraq and Afghanistan.” Clinical Psychology Review 29 (8): 685–94. [DOI] [PubMed] [Google Scholar]
- United States Congress . 1996. “Veterans’ Health Care Eligibility Reform Act of 1996 (1996 – H.R. 3118),” GovTrack.us, [accessed on May 4, 2018]. Available at: https://www.govtrack.us/congress/bills/104/hr3118.
- United States Congress . 2010. “111th Congress Public Law 163. Page 124 STAT. 1145,” Caregivers and Veterans Omnibus Health Services Act of 2010 [accessed on November 25, 2013]. Available at: http://www.gpo.gov/fdsys/pkg/PLAW-111publ163/html/PLAW-111publ163.htm.
- VA . 2012. “Maternity Health Care and Coordination,” VHA Handbook 1330.03, Washington, DC: Veterans Health Administration; [accessed on July 8, 2013]. Available at: http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2803. [Google Scholar]
- VA . 2015. Women Veterans Health Care: Facts and Statistics about Women Veterans. Washington, DC: U.S. Department of Veterans Affairs; Available at: http://www.womenshealth.va.gov/WOMENSHEALTH/latestinformation/facts.asp#5. [Google Scholar]
- VA . 2017a. “172VA10P2: VHA Corporate Data Warehouse – VA. 79 FR 4377. Updated August 9, 2017,” [accessed on November 7, 2017].
- VA, Office of Public and Intergovernmental Affairs . 2017b. “VA Announces Veterans Coordinated Access & Rewarding Experiences (‘CARE’) Act: Replaces Current ‘30‐Day/40‐Mile’ System With Patient/Provider‐Centric Decision‐Making,” News, [accessed on December 1, 2017]. Available at: https://www.va.gov/opa/pressrel/pressrelease.cfm?id=2963.
- VA Information Resource Center . 2011. “VIReC Data Investigation: VETSNET File,” Hines, IL: U.S. Dept. of Veterans Affairs, Health Services Research and Development Service, VA Information Resource Center; [accessed on February 5, 2017]. Available at: http://vaww.virec.research.va.gov/Reports/DI/DI-VETSNET-Jan-CY11-RA.pdf. [Google Scholar]
- Vadillo‐Ortega, F. , Osornio‐Vargas A., Buxton M. A., Sánchez B. N., Rojas‐Bracho L., Viveros‐Alcaráz M., Castillo‐Castrejón M., Beltrán‐Montoya J., Brown D. G., and O'Neill M. S.. 2014. “Air Pollution, Inflammation and Preterm Birth: A Potential Mechanistic Link.” Medical Hypotheses 82 (2): 219–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt, D. S. , Barry A. A., and King L. A.. 2008. “Toward Gender‐Aware Health Care: Evaluation of an Intervention to Enhance Care for Female Patients in the VA Setting.” Journal of Health Psychology 13 (5): 624–38. [DOI] [PubMed] [Google Scholar]
- Yano, E. M. , and Frayne S. M.. 2011. “Health and Health Care of Women Veterans and Women in the Military: Research Informing Evidence‐Based Practice and Policy.” Women's Health Issues, 21(4, Supplement): S64–6. [DOI] [PubMed] [Google Scholar]
- Yano, E. M. , Hayes P., Wright S., Schnurr P. P., Lipson L., Bean‐Mayberry B., and Washington D. L.. 2010. “Integration of Women Veterans Into VA Quality Improvement Research Efforts: What Researchers Need to Know.” Journal of General Internal Medicine 25 (Suppl 1): 56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yano, E. M. , Bastian L. A., Bean‐Mayberry B., Eisen S., Frayne S., Hayes P., Klap R., Lipson L., Mattocks K., McGlynn G., Sadler A., Schnurr P., and Washington D. L.. 2011. “Using Research to Transform Care for Women Veterans: Advancing the Research Agenda and Enhancing Research–Clinical Partnerships.” Women's Health Issues, 21(4, Supplement): S73–83. [DOI] [PubMed] [Google Scholar]
- Yasmeen, S. , Romano P. S., Schembri M. E., Keyzer J. M., and Gilbert W. M.. 2006. “Accuracy of Obstetric Diagnoses and Procedures in Hospital Discharge Data.” American Journal of Obstetrics and Gynecology 194 (4): 992–1001. [DOI] [PubMed] [Google Scholar]
- Zephyrin, L. C. 2016. “Reproductive Health Management for the Care of Women Veterans.” Obstetrics & Gynecology 127 (2): 383–92. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Figure S1. Analytic Cohort.
Figure S2. Preterm Birth Rate (per 1,000 live births) among VA‐enrolled Veterans and All Mothers Age 19‐49, in California, 2000–2012.
Table S1. Algorithm to Estimate Use of Neonatal Intensive Care Unit (NICU).
Table S2. Sensitivity Test Using “Best Obstetric Estimate” versus “Last Menstrual Period” Variable for Estimated Gestational Age, to Model Preterm Birth Outcomes in California, 2007–2012, among VA‐enrolled Veterans.
Table S3. Sensitivity Test Using “Best Obstetric Estimate” versus “Last Menstrual Period” Variable for Estimated Gestational Age, to Model Preterm Birth Outcomes in California, 2007‐2012, VA‐enrolled Veterans vs General Population.


