Abstract
Objective
To examine the association of dual use of both Veterans Health Administration (VHA) and Medicare benefits with high‐risk opioid prescriptions among Veterans aged 65 years and older with a musculoskeletal disorder diagnosis.
Data Sources/Study Setting
Data were obtained from the VA Musculoskeletal Disorder (MSD) cohort and national Medicare claims data from 2008 to 2010.
Study Design
We conducted a retrospective analysis of Veterans enrolled in Medicare to examine the association of dual use with long‐term opioid use (>90 days of prescription opioids/year) and overlapping opioid prescriptions. Multivariable logistic regression was performed adjusting for demographic and clinical characteristics.
Data Collection/Extraction Methods
We identified 21,111 Veterans enrolled in Medicare who entered the MSD cohort in 2008 and received an opioid prescription in 2010. We linked VHA data with Medicare claims data to identify opioid prescriptions for these Veterans in 2010.
Principal Findings
As compared to Veterans who used only VHA or Medicare, Veterans with dual use of VHA and Medicare were significantly more likely to be prescribed long‐term opioid therapy (OR = 4.61 (95 percent CI 4.05–5.25) and were also found to have higher median number of opioid prescriptions and higher odds of overlapping opioid prescriptions in 1 year. Patients reporting moderate‐to‐severe pain, non‐white‐race/ethnicity, and higher scoring on the Charlson comorbidity index had significantly higher odds of long‐term opioid prescriptions.
Conclusions
Among Veterans aged 65 years or older, dual use of both VHA and Medicare was associated with higher odds of long‐term opioid therapy. Our findings suggest there may be benefit to combining VHA and non‐VHA electronic health record data to minimize exposure to high‐risk opioid prescribing.
Keywords: Dual use, patient safety, opioid analgesics, Veterans
The rise of opioid usage and opioid use disorder has recently been declared a public health emergency in the United States (“The White House” 2017). In 2016, an estimated 11.8 million Americans misused opioids and rates of death from prescription‐opioid overdoses have more than quadrupled in the past 15 years (Ahrnsbrak et al. 2017; CDC 2017). This issue is particularly pertinent to the Veterans Health Administration (VHA) as it is the largest integrated health care system in the United States, and Veterans are at increased risk of experiencing chronic pain and developing opioid use disorders (Bohnert et al. 2011; Nahin 2017). Chronic pain impacts nearly half of Veterans and almost 25 percent of Veterans received opioid prescriptions as an outpatient in 2012 (Dorflinger et al. 2014; Toblin et al. 2014; Nahin 2017). Although recent national initiatives by the VHA have decreased the number of Veterans with opioid prescriptions, there remains concern that patients may be obtaining medications from alternative sources (Gellad et al. 2018). These findings highlight the continual need to identify strategies to ensure Veterans with chronic pain are appropriately treated without an overreliance on opioid therapy.
One cohort of Veterans particularly at risk is those with musculoskeletal disorder diagnoses (MSD). MSD including joint, back, and neck disorders and osteoarthritis are some of the most prevalent, debilitating, and costly disorders affecting Veterans and the general population (Stewart et al. 2003; Woolf, Vos, and March 2010; Goulet et al. 2016). Many Veterans with MSD experience chronic pain, and traditional treatment strategies have revolved around long‐term opioid therapy despite limited evidence regarding its efficacy (Ballantyne and Mao 2003; Dowell, Hargerich, and Chou 2016). Although the VHA has spearheaded many opioid reducing initiatives, these efforts may have a more modest impact for patients who receive care outside the VHA. Providers from different health care services often have limited communication with other providers and are unable to share electronic health care records, thereby hampering efforts to provide coordinated care in pain management for Veterans with chronic pain (Stroupe et al. 2013).
There are nearly ten million US Veterans aged 65 years or older who are eligible for both VHA and Medicare benefits given their military service and age, respectively (American Community Survey 2016). While Veterans who utilize both VHA and Medicare may have access to wider sources of health care, they are also at risk of experiencing increased fragmentation in the care delivered to them (Wolinsky et al. 2006; Pizer and Gardner 2011; Gellad et al. 2015). In Veterans with chronic pain, having multiple providers from different health care systems may actually be a barrier to receiving a consistent and continuously coordinated care plan to address their pain without an overreliance on opioid therapy (Wilsey et al. 2010; Jena et al. 2014). It is currently unclear whether Veterans with musculoskeletal disorders who utilize both VHA and Medicare are at higher risk of being prescribed long‐term opioid therapy. Given this gap in knowledge, we utilized a national cohort of Veterans in VHA care who are 65 years and older with a new diagnosis of musculoskeletal diagnosis to determine whether there is an association between dual use of VHA and Medicare and opioid prescriptions. We hypothesized that Veterans with musculoskeletal disorders with dual use of VHA and Medicare benefits are at increased risk of being prescribed long‐term opioid therapy compared to Veterans only using VHA care.
Methods
Data Sources
In this analysis, we linked data from the VA Musculoskeletal Disorders Cohort with claims data from the Centers for Medicare and Medicaid Services (CMS) from VA Information Resource Center (VIReC) using patient scrambled SSN (VIReC 2016). The VA Musculoskeletal Disorders Cohort is a comprehensive registry of all Veterans with MSD diagnoses who received care in a VHA inpatient and/or outpatient medical facility between 2000 and 2013 (Goulet et al. 2016). To be eligible for the VA Musculoskeletal Disorders Cohort, a veteran had to have one of 1,685 distinct International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9CM) diagnoses representing a musculoskeletal disorder recorded at ≥2 outpatient visits occurring within 18 months of one another or at ≥1 inpatient stay. Additional demographic and clinical information was extracted from VHA electronic clinical and administrative data sources in the Corporate Data Warehouse (CDW) for all eligible Veterans both prior to and following the date of their first MSD diagnosis (index date) to enable the analysis of longitudinal outcomes (Fihn 2014).
Study Design and Population
We performed a cross‐sectional analysis of all Veterans who entered the MSD Cohort in 2008 who were aged 65 and older. The date of the first MSD diagnosis was used as the index date. Using data from the CDW Vital Status Mini and Medicare Beneficiary Annual Summary, Veterans were followed from their MSD index date to end of calendar year 2010 or until death (VA Information Resource Center 2015). Patients who died during our study period were excluded. Veterans not eligible for Medicare part D were excluded from our study cohort (e.g., Veterans not enrolled in Medicare Part A for 12 months). We furthermore restricted our study population to only Veterans who were prescribed an opioid from either source in 2010 (Figure 1).
Figure 1.
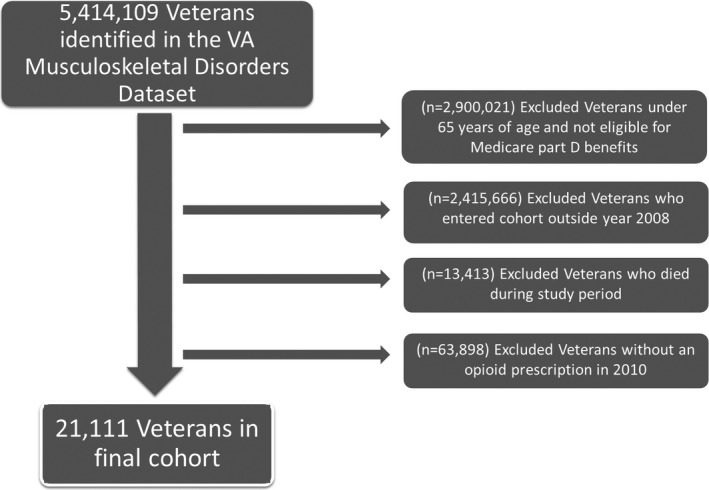
Cohort Selection Flowchart
- Notes. The final cohort included 21,111 Veterans in that entered the MSD cohort in 2008 and received an opioid prescription in 2010.
Dual Use Definition
Veterans were identified as VHA only if they did not have any Medicare opioid prescription in 2010, Medicare only if all of their opioid prescriptions were from Medicare providers, or dual use if they received opioid prescriptions from both VHA and Medicare in 2010.
Study Outcomes
Our outcome measures were the proportion of Veterans with long‐term opioid prescriptions, defined by >90 days of prescribed opioid therapy and overlap of concurrent opioid prescriptions in 2010. Greater than 90 days of opioid prescriptions has been previously used in prior studies as a marker for long‐term opioid therapy (Boscarino et al. 2010; Edlund et al. 2014) . Overlap of opioid prescriptions was defined as an opioid prescription that started before the end‐date of a prior prescription, inclusive of prescriptions outside the VHA. We also included as secondary outcomes the number of unique opioid prescriptions and the number of days associated with an opioid prescription. Opioid medications included the following: Codeine, Fentanyl, Hydrocodone, Hydromorphone, Levorphanol, Meperidine, Morphine, Oxycodone, Oxymorphone, Pentazocine, Propoxyphene, Tapentadol and Tramadol. Buprenorphine and Methadone were excluded as the majority of their use is to treat opioid use disorder.
Covariates
Covariates including age, sex, and ethnicity were derived from VHA data on the MSD index date. We also constructed a moderate‐to‐severe pain intensity variable as defined by a pain score from 4 to 10 in 2008 using the pain intensity numerical rating scale (NRS) score from the VA Vital Signs data on their MSD index date (Strong, Ashton, and Chant 1991; Dobscha et al. 2015).
We also identified comorbid diagnoses recorded at ≥2 outpatient visits or ≥1 inpatient stay up to 12 months before or 6 months after the MSD index date. We controlled for overall clinical severity by calculating the Charlson comorbidity index (CCI), with higher scores indicating greater comorbidity (Deyo, Cherkin, and Ciol 1992; Klabunde et al. 2000). We also included mental health diagnoses not included in the CCI: depressive disorder, substance use disorder (alcohol and illicit drug use disorders), and post‐traumatic stress disorder (PTSD). We controlled for these conditions because they have high prevalence among Veterans (Brennan, Schutte, and Moos 2005; Hooten et al. 2011; Seal et al. 2012).
Statistical Analyses
We first described the sample with respect to VHA only, CMS only and dual use of benefits. We then compared clinical and demographic characteristics of Veterans by prescription drug benefits utilization using analyses of variance (ANOVA) for continuous variables and a chi‐square test or Fisher's exact test for categorical variables. We then compared patterns of opioid prescriptions including total days’ supplied of opioid prescriptions, proportion of patients with >90 days supplied of prescriptions in a year, number of prescriptions in a year, and overlap of concurrent prescriptions. Finally, we used logistic regression modeling to examine factors associated with dual use of both VHA and Medicare benefits, the odds of receipt of long‐term opioid prescriptions, and odds of receipt of overlapping concurrent opioid prescriptions, adjusting for other demographic and clinical characteristics as described above.
All analyses were conducted using SAS 9.4 (SAS, Cary, NC). All p values are reported as two‐sided with significant at p < .05. The VA Connecticut Healthcare System Institutional Review Board approved the MSD Cohort study.
Results
Cohort Characteristics
We identified 21,111 Veterans who met inclusion criteria for this study. The mean age of the analytic sample was 75 with 83.6 percent white and 98.3 percent male. Sixty‐seven percent of Veterans received an opioid from VHA only, 26.5 percent Medicare only, and 6.8 percent of both VHA and Medicare. Veterans who used only VHA were significantly younger and had more medical and psychiatric comorbidities. The majority of Veterans in the cohort (58 percent) reported no or mild pain intensity on the NRS at MSD index date (2008), and Veterans with dual use of prescription drug benefits were more likely to report moderate‐to‐severe pain (Table 1).
Table 1.
Baseline Characteristics of Veterans with Opioid Prescriptions in 2010 by Prescription Drug Benefit Utilization
| Patient Characteristics | Prescription Drug Benefit Utilization | p‐Value | ||
|---|---|---|---|---|
| Both (n = 1,430) | CMS Only (n = 5,596) | VHA Only (n = 14,085) | ||
| Age | ||||
| 65–74 years old | 51.0 | 43.1 | 57.6 | <.001 |
| 75–84 years old | 38.5 | 43.1 | 32.9 | |
| 85+ years old | 10.5 | 13.8 | 9.5 | |
| Sex | ||||
| Female | 2.0 | 1.7 | 1.6 | 0.05 |
| Male | 98.0 | 98.2 | 98.4 | |
| Race | ||||
| White | 81.5 | 88.1 | 82.7 | <.001 |
| Black | 10.9 | 6.7 | 11.3 | |
| Hispanic | 5.3 | 3.5 | 4.0 | |
| Other/Unknown | 2.3 | 1.7 | 2.0 | |
| Moderate‐to‐severe pain intensity (pain scale 4–10) | 48.4 | 31.7 | 44.4 | <.001 |
| Pain intensity, median[IQR] | 3 [0–7] | 0 [0–5] | 3 [0–6] | <.001 |
| BMI, mean (SD) | 29.3 (5.7) | 29.1 (5.3) | 29.2 (6.0) | 0.40 |
| MSD diagnoses | ||||
| Nontraumatic joint | 65.0 | 52.0 | 69.5 | <.001 |
| Back pain | 47.6 | 26.6 | 44.0 | <.001 |
| Osteoarthritis | 38.5 | 30.6 | 41.4 | <.001 |
| Fracture | 7.1 | 3.2 | 9.1 | <.001 |
| Gout | 9.2 | 9.2 | 9.7 | 0.47 |
| Neck pain | 12.6 | 6.8 | 16.3 | <.001 |
| Fibromyalgia | 1.5 | 1.0 | 2.1 | <.001 |
| Temporomandibular joint dysfunction | 0.4 | 0.1 | 0.4 | <.001 |
| Comorbidities | ||||
| Substance Use (Illicit Drugs + Alcohol) | 8.0 | 3.8 | 8.6 | <.001 |
| Major depression | 6.4 | 3.2 | 6.4 | <.001 |
| Post‐traumatic stress disorder | 6.3 | 3.3 | 8.8 | <.001 |
| Charlson Comorbidity Score | ||||
| Score 0–1 | 63.4 | 76.0 | 55.0 | <.001 |
| Score 2 or more | 36.6 | 24.0 | 45.0 | |
BMI, body mass index; CMS, Center for Medicare and Medicaid Services; IQR, interquartile range; MSD, musculoskeletal disorder; SD, standard deviation; VHA, Veterans Health Administration.
Dual Use of Benefits and High‐Risk Opioid Prescriptions
Seven‐one percent of Veterans who used both VHA and Medicare were prescribed long‐term opioid therapy, whereas 43 percent and 22 percent of Veterans who used only VHA and Medicare respectively were prescribed long‐term opioid therapy. Veterans with dual VHA and Medicare use had more opioid prescriptions and more days of opioid prescriptions in 1 year. Overall, 76 percent of dual users had overlapping prescriptions, whereas 38 percent of VHA only and 24 percent of Medicare only users had overlapping prescriptions (Table 2).
Table 2.
Opioid Prescribing Patterns in Veterans with Opioid Prescriptions by Prescription Drug Benefit Utilization
| Opioid Prescribing Patterns | Prescription Drug Benefit Utilization in 2010 | p‐Value | ||
|---|---|---|---|---|
| Both (n = 1,430) | CMS Only (n = 5,596) | VHA Only (n = 14,085) | ||
| Total days supply in 2010, median [IQR] | 182 [72–303] | 15 [5–67] | 60 [24–169] | <.001 |
| Proportion of patients on long‐term opioid therapy (>90 days/year) | 0.71 | 0.22 | 0.43 | <.001 |
| Number of prescriptions, median [IQR] | 9 [4–15] | 2 [1–5] | 2 [1–6] | <.001 |
| Proportion of patients with overlapping concurrent opioid prescriptions | 0.76 | 0.24 | 0.38 | <.001 |
CMS, Centers for Medicare and Medicaid Services; IQR, interquartile range; VHA, Veterans Health Administration.
In multivariate modeling, Veterans who were non‐white [odds ratio (OR) = 1.28 (95 percent confidence interval (CI) = 1.11–1.49] or reported moderate/severe pain [OR = 1.37 (95 percent CI 1.22–1.54) (Table 3) were significantly more likely to be dual users. Dual use was associated with significantly higher odds of long‐term opioid use [OR = 4.61 (95 percent CI 4.05–5.25)] and concurrent overlapping opioid prescriptions [OR = 5.28 (95 percent CI 4.60–6.05)]. Non‐white race and older age were associated with lower odds of long‐term opioid use and concurrent overlapping opioid prescriptions. Moderate‐to‐severe pain intensity and major depression were independently associated with higher odds of long‐term opioid use and concurrent overlapping opioid prescriptions. Additionally, higher scores on the Charlson comorbidity index were significantly associated with higher odds of long‐term opioid use; substance use disorder was found to be significantly associated with higher odds for overlapping concurrent opioid prescriptions (Table 4).
Table 3.
Patient Characteristics Associated with Dual Use of VHA Pharmacy and Medicare Part D
| Patient Characteristics | OR (95% CI) | p‐Value |
|---|---|---|
| Age: 65–74 years old | REF | – |
| 75–84 years old | 1.12 (0.99–1.27) | .08 |
| 85+ years old | 1.09 (0.89–1.32) | .40 |
| Non‐white race (ref: white race) | 1.28 (1.11–1.49) | .002 |
| Female sex (ref: male sex) | 0.78 (0.52–1.17) | .23 |
| Moderate‐to‐severe pain intensity (pain scale 4–10) | 1.37 (1.22–1.54) | <.001 |
| CCI 2+ (ref: CCI score 0–1) | 0.90 (0.80–1.01) | .09 |
| Substance use disorder | 1.10 (0.90–1.39) | .31 |
| PTSD | 0.81 (0.63–1.04) | .09 |
| Major depression | 1.17 (0.91–1.51) | .22 |
CCI, Charlson comorbidity index; CI, confidence intervals; CMS, Centers for Medicare and Medicaid Services; OR, odds ratio; PTSD, post‐traumatic stress disorder; REF, reference; VHA, Veterans Health Administration.
Table 4.
Patient Characteristics Associated with Long‐Term Opioid Prescribing and Overlapping Concurrent Opioid Prescriptions
| Patient Characteristics | Long‐Term Opioid Use (>90 Days in 1 Year) | Overlapping Concurrent Opioid Prescriptions | ||
|---|---|---|---|---|
| OR (95% CI) | p‐Value | OR (95% CI) | p‐Value | |
| Age: 65–74 years old | REF | — | REF | — |
| 75–84 years old | 0.85 (0.79–0.91) | <.001 | 0.81 (0.76–0.87) | <.001 |
| 85+ years old | 0.85 (0.85–0.97) | 0.010 | 0.83 (0.74–0.92) | .001 |
| Non‐white race (ref: white race) | 0.82 (0.75–0.89) | <.001 | 0.77 (0.71–0.84) | <.001 |
| Female sex (ref: male sex) | 0.90 (0.71–1.15) | .406 | 0.97 (0.75–1.24) | .777 |
| Moderate‐to‐severe pain intensity (pain scale 4–10) | 1.48 (1.39–1.57) | <.001 | 1.40 (1.31–1.49) | <.001 |
| CCI 2+ (ref: CCI score 0–1) | 1.08 (1.01–1.15) | 0.019 | 0.96 (0.90–1.03) | .285 |
| Substance use disorder | 1.11 (0.99–1.25) | .082 | 1.18 (1.05–1.33) | .003 |
| PTSD | 1.05 (0.93–1.19) | .457 | 0.94 (0.82–1.05) | .307 |
| Major depression | 1.31 (1.14–1.51) | .001 | 1.32 (1.15–1.52) | .001 |
| Dual Use of VHA and Medicare part D | 4.61 (4.05–5.25) | <.001 | 5.28 (4.60–6.05) | <.001 |
CCI, Charlson comorbidity index; CI, confidence intervals; OR, odds ratio; PTSD, Post‐traumatic stress disorder; REF, reference; VHA, Veterans Health Administration.
Discussion
Our study demonstrates that in Veterans with a newly established musculoskeletal disorder diagnosis, those who used both VHA and Medicare benefits had fourfold higher odds of being prescribed long‐term opioid therapy. Furthermore, we found that dual use of VHA and Medicare was associated with higher total number of opioid prescription days and overlapping concurrent prescriptions. Our study suggests that dual use can potentiate high‐risk opioid patterns.
In this cohort of Veterans with an opioid prescription, with 11 percent being 85 years and older, we did not observe a consistent association between advancing age and long‐term opioid prescriptions in our study. However, the relatively high absolute number of opioid prescriptions in this elderly cohort is alarming. Recent studies have highlighted that opioid usage as compared to NSAIDs for pain management in the elderly can lead to higher rates of increased adverse events, such as medication interactions and falls, and all‐cause mortality rates (Dunn et al. 2010; Saunders et al. 2010; Solomon et al. 2010). Taken together, prescribers treating elderly Veterans for chronic nonmalignant pain should take extra precaution when prescribing opioids and consider other alternative treatment modalities that may prove equally or more efficacious (Otis, Keane, and Kerns 2003).The VHA has recognized the importance of multimodal treatments in patients with chronic pain. The recent VA Health Services Research and Development sponsored State‐Of‐The‐Art (SOTA) Conference, “nonpharmacological approaches to chronic musculoskeletal pain management,” identified a range of approaches categorized as psychological/behavioral (i.e., cognitive‐behavioral therapy, acceptance and commitment therapy, mindfulness‐based stress reduction), exercise/movement (i.e., structured exercise, tai chi, yoga), and manual (i.e., acupuncture, chiropractic/spinal manipulation, massage) as having sufficient evidence of effectiveness to encourage their routine availability in the VHA (2018). Despite recommendations for a multimodal approach, opioid medications have been used as a primary or sole treatment modality for many Veterans and general population with chronic pain, with the duration of therapy lasting potentially for many years (Ballantyne and Mao 2003; Edlund et al. 2007). The VHA is currently prioritizing various opportunities integrative of multimodal care for elderly Veterans with chronic musculoskeletal pain (Peterson et al. 2016).
Our analysis also found that in Veterans with musculoskeletal diagnoses, a diagnosis of depression was independently associated with higher odds of long‐term and overlapping opioid prescriptions. Our findings build upon the substantial literature supporting this relationship (Hooten et al. 2011; Phifer et al. 2011; Seal et al. 2012; Edlund et al. 2014; Zale, Maisto, and Ditre 2015). The association of depression with long‐term opioid prescribing suggests a potential concern that health care engagement may lead to an increase in opioid use in this patient population with mental illness as prescribers may be using opioids to treat both physical pain and psychological pain. Furthermore, our results support the complex relationship between substance use and opioid use for pain management (Brennan, Schutte, and Moos 2005; Zale, Maisto, and Ditre 2015). Despite VA guidelines that caution prescribers in prescribing opioids in Veterans with substance use disorders, our data reflect that substance use disorder is an independent risk factor in predicting overlapping opioid prescriptions. Given the inherent danger of severe central nervous system depression from simultaneous substance use, such as alcohol use and opioids, there needs to be further efforts to ensure Veterans with substance use histories undergo more thorough assessment of the need for opioid prescriptions (Morasco and Dobscha 2008).
Although our study cohort focused on elderly Veterans with musculoskeletal diagnoses, we believe that our findings are likely applicable to elderly Veterans in the general population that suffer from chronic pain. Our findings are complimentary to a recent study that also analyzed the association of dual use with risk of high‐dose opioid exposure and also found that Veterans who were dual users were more likely to receive opioids for more than 90 days in a year and overlapping prescriptions (Gellad et al. 2018). The joint findings from Gellad and colleague's study and ours emphasize several policy implications. First, the findings of increased overlap in prescription opioids in both our studies suggest potential fragmentation in care as there is little sharing of information across different EMRs allowing for simultaneous prescriptions of duplicate drugs. Second, studies have documented that health care for Veterans with dual use is associated with increased inefficiency and other patterns of high‐risk prescriptions in other drug classes suggesting potential risks associated with utilization of different health care systems that has often been hypothesized to be due to fragmentation in the delivery of care (Gellad et al. 2015; Becker et al. 2017). The importance of improving health care integration is even more important in patients receiving opioid prescriptions as multiple providers or payment sources may significantly place a patient at risk of being prescribed risky opioid therapy (Becker et al. 2017). Despite current CDC guidelines of recommending prescribing of opioids by a single provider, previous literature has shown that roughly 40–60 percent of Veterans obtain their opioids from multiple providers and those who do, are twice as likely to be admitted for an opioid overdose (Jena et al. 2014; Dowell, Hargerich, and Chou 2016).
Accordingly, many states have already begun mandatory prescription drug monitoring programs (PDMP) that have shown some degree of success in reducing prescription rates for opioids (Reifler et al. 2012). The Comprehensive Addiction and Recovery Act of 2016 mandated VA providers to check PDMPs prior to administering opioids and other controlled substances. However, there are no similar requirements outside the VHA with most states having different leniency and structures on controlled substance monitoring. The preliminary data from such programs have shown a decrease in high‐risk opioid prescription patterns such as overlapping opioid prescriptions, and our findings emphasize the potential of creating a national, systematic database that can serve as a platform to help improve coordination among different health care systems. This national database would facilitate a coordinated and integrative approach to treating Veterans and civilian patients with chronic pain without overreliance on opioid therapy.
Our study has several limitations that must be considered in interpreting the findings of our study. First, we only included Veterans who utilized VHA health care; therefore, our results may not be applicable to Veterans who did not utilize VHA care. Second, our study was based off VHA and Medicare claims data which is subject to clerical errors and miscoding. Third, our study presents data from 2010 and may not be reflective of current prescribing guidelines. However, our results are similar to more recent data (Gellad et al. 2018) and we believe our main findings regarding dual use of benefits remain currently relevant. Our study cohort was comprised of Veterans who were enrolled in Medicare Part A but not necessarily enrolled in part D benefits. This may have introduced potential bias given there may be heterogeneity in single use and dual use of prescription benefits. Additionally, information on comorbidities was from VHA data only and may have underestimated the comorbidities among Veterans who received their care predominantly outside the VHA. Furthermore, our dataset lacked certain variables such as socioeconomic status so there may be still residual cofounding in our results. In particular, although we appreciate that dual users may be using more care and thus potentially leading to higher prescription rates, we were unable to adjust for health care utilization in our analyses. Moreover, although we used the VA musculoskeletal cohort entry data as an anchor after which Veterans were followed for 1–2 years to define a cohort with at least one opioid prescription, our analysis remains a cross‐sectional examination of an observational dataset which limits our ability to draw conclusions about causation. Therefore, we were not able to determine a direction of causality. We also used a one‐item measure of current pain intensity. No other pain‐relevant variables are routinely collected in the electronic medical record, so other variables which capture the full complexity of pain as a construct such as type of pain (acute vs. chronic), location of the pain, and pain interference were not available to us. Finally, we were only able to capture opioid prescriptions patterns from the administrative data which is only a surrogate marker of opioid prescription intake by Veterans.
In summary, we found that Medicare‐eligible Veterans with musculoskeletal disorders using dual care were associated with higher rates of high‐risk opioid prescribing including chronic opioid therapy and overlapping opioid prescription. The implications of our study emphasize the value in linking VHA and non‐VHA data to improve the quality of care delivered to Veterans. Further research is needed to understand whether improving multisystem care can decrease reliance on opioid therapy for Veterans with chronic pain.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Funding Sources: This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, and Health Services Research and Development # CRE 12‐012, CIN 13‐407, and Office of Academic Affairs HSR&D Fellowship.
Disclosures: None.
Disclaimer: The views expressed in this manuscript are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- Ahrnsbrak, R. , Bose J., Hedden S. L., Lipari R. N., and Park‐Lee E.. 2017. Substance Abuse and Mental Health Services Administration. “Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17‐5044, NSDUH Series H‐52).”Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; [accessed on November 28, 2017]. Available at https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.pdf [Google Scholar]
- American Community Survey . 2016. “American FactFinder.” Suitland, MD: United States Census Bureau; [accessed on November 28, 2017]. Available at https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml [Google Scholar]
- Ballantyne, J. C. , and Mao J.. 2003. “Opioid Therapy for Chronic Pain.” New England Journal of Medicine 349: 1943–53. [DOI] [PubMed] [Google Scholar]
- Becker, W. D. , Fenton B. T., Brant C. A., Doyle E. L., Francis J., Goulet J. L., Moore B. A., Torrise V., Kerns R. D., and Kreiner P. W.. 2017. “Multiple Sources of Prescription Payment and Risky Opioid Therapy among Veterans.” Medical Care 55 (suppl 7): S33–6. [DOI] [PubMed] [Google Scholar]
- Bohnert, A. S. , Ilgen M. A., Galaea S., McCarthy J. F., and Blow F. C.. 2011. “Accidental Poisoning Mortality among Veterans in the Department of Veterans Affairs Health System.” Medical Care 49 (4): 393–6. [DOI] [PubMed] [Google Scholar]
- Boscarino, J. A. , Rukstalis M., Hoffman S. N., Han J. J., Erlich P. M., Gerhard G. S., and Stewart W. F.. 2010. “Risk Factors for Drug Dependence among Out‐Patients on Opioid Therapy in a Large US Health‐Care System.” Addiction 105 (10): 1776–82. [DOI] [PubMed] [Google Scholar]
- Brennan, P. L. , Schutte K. K., and Moos R. H.. 2005. “Pain and Use of Alcohol to Manage Pain: Prevalence and 3‐Year Outcomes among Older Problem and Non‐Problem Drinkers.” Addiction 100: 777–86. [DOI] [PubMed] [Google Scholar]
- CDC . 2017. “Wide‐Ranging Online Data for Epidemiologic Research (WONDER).” Atlanta, GA: CDC, National Center for Health Statistics; [accessed on November 26, 2017]. Available at https://wonder.cdc.gov/ [Google Scholar]
- Deyo, R. A. , Cherkin D. C., and Ciol M. A.. 1992. “Adapting a Clinical Comorbidity Index for Use with ICD‐9‐CM Administrative Databases.” Journal of Clinical Epidemiology 45 (6): 613–9. [DOI] [PubMed] [Google Scholar]
- Dobscha, S. K. , Morasco B. J., Kovas A. E., Peters D. M., Hart K., and McFarland B. H.. 2015. “Short‐Term Variability in Outpatient Pain Intensity Scores in a National Sample of Older Veterans with Chronic Pain.” Pain Med 16 (5): 855–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorflinger, L. , Moore B., Goulet J., Becker W., Heapy A. A., Sellinger J. J., and Kerns R. D.. 2014. “A Partnered Approach to Opioid Management, Guideline Concordant Care and the Stepped Care Model of Pain Management.” Journal of General Internal Medicine 29 (Supp 4): 870–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell, D. , Hargerich T. M., and Chou R.. 2016. “CDC Guideline for Prescribing Opioids for Chronic Pain‐United States, 2016.” Journal of the American Medical Association 315 (15): 1624–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn, K. M. , Saunders K. W., Rutter C. M., Banta‐Green C. J., Merrill J. O., Sullivan M. D., Weisner C. M., Silverberg M. J., Campbell C. I., Psaty B. M., and Von Korff M.. 2010. “Opioid Prescriptions for Chronic Pain and Overdose: A Cohort Study.” Annals of Internal Medicine 152 (2): 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund, M. J. , Steffick D., Hudson T., Harris K. M., and Sullivan M.. 2007. “Risk Factors for Clinically Recognized Opioid Abuse and Dependence among Veterans Using Opioids for Chronic Non‐Cancer Pain.” Pain 129 (3): 355–62. [DOI] [PubMed] [Google Scholar]
- Edlund, M. J. , Martin B. C., Russo J. E., DeVries A., Braden J. B., and Sullivan M. D.. 2014. “The Role of Opioid Prescription in Incident Opioid Abuse and Dependence among Individuals with Chronic Noncancer Pain: The Role of Opioid Prescription.” Clinical Journal of Pain 305: 57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fihn . 2014. “US Department of Veterans Affairs. 172VA10P2: VHA Corporate Data Warehouse – VA. 79 FR 4377. ” Updated January 27, 2014 [accessed on March 10, 2017].
- Gellad, W. F. , Zhao X., Thorpe C. T., Mor M. K., Good C. B., and Fine M. J.. 2015. “Dual Use of Department of Veterans Affairs and Medicare Benefits and Use of Test Strips in Veterans with type 2 Diabetes Mellitus.” JAMA Internal Medicine 175 (1): 26–34. [DOI] [PubMed] [Google Scholar]
- Gellad, W. F. , Thorpe J. M., Zhao X., Thorpe C. T., Sileanu F. E., Cashy J. P., Hale J. A., Mor M. K., Radomski T. R., Hausmann L. R. M., Donohue J. M., Gordon A. J., Suda K. J., Stroupe K. T., Hanlon J. T., Cunningham F. E., Good C. B., and Fine M. J.. 2018. “Impact of Dual Use of Department of Veterans Affairs and Medicare Part D Drug Benefits on Potentially Unsafe Opioid Use.” American Journal of Public Health 108 (2): 248–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goulet, J. L. , Kerns R. D., Bair M., Becker W. C., Brennan P., Burgess D., Carroll C. M., Dobscha S., Driscoll M. A., Fenton B. T., Fraenkel L., Haskell S. G., Heapy A. A., Higgins D. M., Hoff R. A., Hwang U., Justice A. C., Piette J. D., Sinnott P., Wandner L., Womack J. A., and Brandt C. A.. 2016. “The Musculoskeletal Diagnosis Cohort: Examining Pain and Pain Care among Veterans.” Pain 157 (8): 1696–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooten, W. M. , Shi Y., Gazelka H. M., and Warner D. O.. 2011. “The Effects of Depression and Smoking on Pain Severity and Opioid Use in Veterans with Chronic Pain.” Pain 152 (1): 223–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jena, A. B. , Goldman D., Weaver L., and Karaca‐Mandic P.. 2014. “Opioid Prescribing by Multiple Providers in Medicare: Retrospective Observational Study of Insurance Claims.” BMJ 348: g1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klabunde, C. N. , Potosky A. L., Legler J. M., and Warren J. L.. 2000. “Development of a Comorbidity Index Using Physician Claims Data.” Journal of Clinical Epidemiology 53 (12): 1258–67. [DOI] [PubMed] [Google Scholar]
- Morasco, B. J. , and Dobscha S. K.. 2008. “Prescription Medication Misuse and Substance use Disorder in VA Primary Care Veterans with Chronic Pain.” General Hospital Psychiatry 30 (2): 93–9. [DOI] [PubMed] [Google Scholar]
- Nahin, R. L. 2017. “Severe Pain in Veterans: The Effect of Age and Sex, and Comparisons with the General Population.” J Pain 18 (3): 247–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otis, J. D. , Keane T. M., and Kerns R. D.. 2003. “An Examination of the Relationship between Chronic Pain and Post‐Traumatic Stress Disorder.” Journal of Rehabilitation Research and Development 40 (5): 397–405. [DOI] [PubMed] [Google Scholar]
- Peterson, K. , Anderson J., Ferguson L., and Mackey K.. 2016. “Evidence Brief: The Comparative Effectiveness of Selected Complementary and Integrative Health (CIH) Interventions for Preventing or Reducing Opioid Use in Adults with Chronic Neck, Low Back, and Large Joint Pain.” VA Evidence‐based Synthesis Program Evidence Briefs. [PubMed]
- Phifer, J. , Skelton K., Weiss T., Schwartz A. C., Wingo A., Gillespie C. F., Sands L. A., Sayyar S., Bradley B., Jovanovic T., and Ressler K. J.. 2011. “Pain Symptomatology and Pain Medication Use in Civilian PTSD.” Pain 152 (10): 2233–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizer, S. D. , and Gardner J. A.. 2011. “Is Fragmented Financing Bad for Your Health?” Inquiry 48 (2): 109–22. [DOI] [PubMed] [Google Scholar]
- Reifler, L. M. , Droz D., Bailey J. E., Schnoll S. H., Fant R., Dart R. C., and Bartelson B. B.. 2012. “Do Prescription Monitoring Programs Impact State Trends in Opioid Abuse/Misuse?” Pain Med 13 (3): 434–42. [DOI] [PubMed] [Google Scholar]
- Saunders, K. W. , Dunn K. M., Merrill J. O., Sullivan M., Weisner C., Braden J. B., Psaty B. M., and Von Korff M.. 2010. “Relationship of Opioid Use and Dosage Levels to Fractures in Older Chronic Pain Veterans.” Journal of General Internal Medicine 25 (4): 310–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal, K. H. , Shi Y., Cohen G., Cohen B. E., Maguen S., Krebs E. E., and Neylan T. C.. 2012. “Association of Mental Health Disorders with Prescription Opioids An High‐Risk Opioids Use in US Veterans of Iraq and Afghanistan.” Journal of the American Medical Association 307 (9): 940–7. [DOI] [PubMed] [Google Scholar]
- Solomon, D. H. , Raassen J. A., Glynn R. J., Lee J., Levin R., and Schneeweiss S.. 2010. “The Comparative Safety of Analgesics in Older Adults with Arthritis.” Archives of Internal Medicine 170 (22): 1968–78. [DOI] [PubMed] [Google Scholar]
- Stewart, W. F. , Ricci J. A., Chee E., Morganstein D., and Lipton R.. 2003. “Lost Productive Time and Cost Due to Common Pain Conditions in the US Workforce.” Journal of the American Medical Association 290 (18): 2443–54. [DOI] [PubMed] [Google Scholar]
- Strong, J. , Ashton R., and Chant D.. 1991. “Pain Intensity Measurement in Chronic Low Back Pain.” Clinical Journal of Pain 7 (3): 209–18. [DOI] [PubMed] [Google Scholar]
- Stroupe, K. T. , Smith B. M., Hogan T. P., St Andre J. R., Gellad W. F., Weiner S., Lee T. A., Burk M., Cunningham F., Piette J. D., Rogers T. J., Huo Z., and Weaver F. M.. 2013. “Medication Acquisition across Systems of Care and Patient–Provider Communication among Older Veterans.” American Journal of Health System Pharmacy 70 (9): 804–13. [DOI] [PubMed] [Google Scholar]
- The White House: Office of the Press Secretary . 2017. “President Donald J. Trump is Taking Action on Drug Addiction and the Opioid Crisis.” Washington, DC: The White House; [accessed on November 28, 2017]. Available at https://www.whitehouse.gov/the-press-office/2017/10/26/president-donald-j-trump-taking-action-drug-addiction-and-opioid-crisis [Google Scholar]
- Toblin, R. L. , Quartana P. J., Riviere L. A., Walper K. C., and Hoge C. W.. 2014. “Chronic Pain and Opioid Use in US Soldiers after Combat Deployment.” JAMA Internal Medicine 174 (8): 1400–1. [DOI] [PubMed] [Google Scholar]
- “VA Information Resource Center, Record and Person Counts in the VA/CMS Medicare Data, CY 1997‐2013.” Hines, IL: U.S. Dept. of Veterans Affairs, Health Services Research and Development Service, VA Information Resource Center; 2015. [Google Scholar]
- VIReC Support for VA/CMS Data provided by the Department of Veterans Affairs, VA Health Services Research and Development Service, VA Information Resource Center (Project Numbers SDR 02‐237 and 98‐004), Hines, IL. 2016.
- Wilsey, B. L. , Fishman S. M., Gilson A. M., Casamalhuapa C., Baxi H., and Zhang H.. 2010. “Profiling Multiple Provider Prescribing of Opioids, Benzodiazepines, Stimulants, and Anorectics.” Drug and Alcohol Dependence 112: 99–106. [DOI] [PubMed] [Google Scholar]
- Wolinsky, F. D. , Miller T. R., An H., Brezinski P. R., Vaughn T. E., and Rosenthal G. E.. 2006. “Dual Use of Medicare and the Veterans Health Administration: Are There Adverse Health Outcomes?” BMC Health Serv Res 6: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf, A. D. , Vos T., and March L.. 2010. “How to Measure the Impact of Musculoskeletal Conditions.” Best Pract Res Clin Rheumol 24: 723–32. [DOI] [PubMed] [Google Scholar]
- Zale, E. L. , Maisto S. A., and Ditre J. W.. 2015. “Interrelations between Pain and Alcohol: An Integrative Review.” Clin Psychol Rev 37: 57–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


