Abstract
AIM:
This study aimed to compare the effect of Dexmedetomidine and fentanyl as an adjuvant to lidocaine 5% in spinal anaesthesia to increase post-operative analgesia among women candidates for elective caesarean.
METHODS:
Eighty-four pregnant women candidates for caesarian were randomly divided into fentanyl and Dexmedetomidine groups. In the first group, 25 μg fentanyl was added to lidocaine 5% while in the second group, 0.5 μg per kilogram Dexmedetomidine was added to lidocaine 5%. After the operation, a pain score of the patients in recovery and within 4, 12 and 24 hours after the operation, the average length of analgesia and the average amount of the analgesics taken within 24 hours and after the operation were recorded.
RESULTS:
The average length of postoperative anaesthesia and the average amount of the drug taken within the first 24 hours after the operation in fentanyl group was more than the Dexmedetomidine group (P = 0.01). Shivering in Dexmedetomidine group was more common than what was observed in the fentanyl group (P = 0.001). Higher rates of nausea-vomiting were observed in the fentanyl group (P = 0.001).
CONCLUSIONS:
Fentanyl results in a longer period of postoperative analgesia and less consumption of drugs after the operation. Fentanyl is recommended in caesarian.
Keywords: Dexmedetomidine, Fentanyl, Pain, Spinal Anesthesia, Lidocaine
Introduction
The rate of caesarian operations has experienced a dramatic rise in developed and developing countries within the last 30 years [1]. Caesarian usually causes moderate to severe pain for 48 hours and requires favourable pain management after the operation that both enables the mother to move faster and plays a key role in post-caesarian rehabilitation [2]. Post-caesarian pain control enhances the mother’s satisfaction and milking capacity, because, insufficient analgesia increases the level of plasma catecholamine [3]. Proper analgesia after caesarian helps the mother feel more comfortable and enhances her movement and ability to take better care of her neonatal [4]. Spinal anaesthesia is one of the most stable methods of anaesthesia in lower abdominal surgeries [5] and reduces the volume of blood lost during the operation and prevents Thromboembolic events after operation [6].
It is widely used for caesarian operations as it is safer for the mother, more useful for the fetus and results in greater satisfaction [7]. In spinal anaesthesia, various adjutants are used with local anaesthetics that prevent somatic and visceral pain and providing lasting postoperative analgesia [8].
It has been proved that spinal Opioids and local anaesthetics operate synergistically in the spinal level in the studies conducted on animals [9]. Adding opioids may have unfavourable side effects such as respiratory depression, itching, nausea and vomiting [6]. Respiratory depression is the side effect of opioids which have the greatest fear for anaesthetists [10]. Fentanyl is structurally similar to local anaesthetics, and it has a local anaesthetic effect on primary C sensory afferents that facilitate analgesic effects. However, useful analgesia needs to be moderated based upon the maternal and fetal side effects like bradycardia, respiratory depression, hypotension, nausea, vomiting and itching [3] [8]. Dexmedetomidine is an elective alpha-two agonist that induces analgesia, tranquillity, and forgetfulness without depressing respiratory performance [11]. As it influences the locus ceruleus area which is associated with the frequency of sleeping and breathing, it has a minimal sedative respiratory depression effect [12]. Dexmedetomidine in the clinic was initially introduced as a short-term effect venous sedative. As the medicine represents the analgesic properties associated with connecting to a2-AR, various researches have studied it as a systematic analgesic adjutant particularly in the acute preoperative form. Considering the great lipophilic of Dexmedetomidine, the medicine will remain in the tissue of placenta and increase the frequency and range of vaginal contractions [13].
Considering the importance of trying to relieve the pain after the operation and wide utilization of opioids to reduce pain after operation and their major side effects and keeping in mind the fact that no comparison has ever been made between the analgesic effects of Dexmedetomidine and fentanyl in caesarian and due to the large prevalence of caesarian operation and the importance of reducing postoperative pain in the health and satisfaction of women candidates for caesarian, we decided to study the effects of adding Dexmedetomidine and fentanyl to lidocaine 5% in reducing the postoperative pain of caesarian among women candidate for it.
Material and Methods
A written letter of introduction was obtained from the authorities of the university for research centres, and the purpose of the research was described for all research centres, and their written consent was obtained. The information of the participants remained confidential with the research executive team. Throughout the research, all ethical statements stipulated in Helsinki Research and by the research committees of ethics of Arak Medical Sciences University were observed. This research was approved with the ethical code of IR.ARAKMU.REC.1395.138 on July 19th, 2016 (Table 1). This research is registered under the code IRCTz2017012320258N28.
Table 1.
The information of research variables
| Name | Definition (scientific and applied) | Type of variable | Scale of variable | Variable measurement unit | ||
|---|---|---|---|---|---|---|
| Based on research goals | Based on the type of variable | Qualitative | Quantitative | |||
| Being placed in fentanyl and Dexmedetomidine group | Fentanyl and Dexmedetomidine are the two medicines used in this research | * | * | * | Questionnaire Fentanyl or Dexmedetomidine | |
| The average length of analgesia after operation (average time to request the first painkiller) | The length of anaesthesia after an operation | * | * | * | * | MinutesQuestionnaire |
| Average pain score in recovery, 4, 12, and 24 hours after the operation | Average pain based upon VAS | * | * | * | VAS rulerNumber | |
| The average amount of the analgesics taken within the first 24 hours after the operation | The average amount of the painkillers taken within 24 hours following the operation | * | * | * | QuestionnaireMilligram | |
| Age | Years passed | * | * | * | QuestionnaireYears | |
This is a double-blinded, randomised clinical trial research conducted randomly on non-emergency patients resorting to Taleghani Hospital of Arak for caesarean. As many as 84 pregnant women candidates for elective non-emergency repetitive caesarean and had a single fetus signed the informed consent form and took part in the research and was randomly divided into fentanyl and Dexmedetomidine groups. All the qualified participants were randomly distributed into the above-said groups using blocked randomisation. (Method used to generate the random allocation sequence was blocked randomisation) Having signed the informed consent form, the patients entered the operation room and initially received 3 to 5 cc per kilogram crystalloid as compensatory volume expand (CVE). After conducting the necessary monitoring and checking the vital signals of the patient, the patient assumed a sitting position and cage 25 needles was sent through theL4-L5 or L5-S1 space, and they underwent spinal anaesthesia for caesarean. 25 μg fentanyl was added to lidocaine 5% in the first group, while 30 to 35 μg (0.5 μg per kilogram) Dexmedetomidine (equal 2 cc, each ml of a diluted vial of Dexmedetomidine was 15 mg) was added to lidocaine 5% in the second group.
The total volume of both solutions in each group reached 4 cc. After conducting spinal anaesthesia and entering the cerebrospinal fluid space, the above-said medicine was injected. After injecting the medicine, the patient was asked to assume a supine position, and after making sure about the spinal block, the operation started. Immediately after spinal anaesthesia, breathing, heart rate, blood pressure and percentage of oxygen saturation were recorded. To abide by the principles of a blind research, the solutions prepared for injection in spinal space were prepared by an anesthetist and given to the assistant resident. Considering the similar volume and appearance of both solutions and unawareness of the resident of the type of solutions used to inject the patients, the resident was blind to the medicines. The patients had no information of the injected material and were randomly divided between the two groups. Finally, after the operation, the pain scores of the patients in recovery, 4, 12, and 24 hours following the operation were measured using Visual analogue scale (VAS). Considering the first demand for analgesics and the average amount of the analgesics used within 24 hours after operation, the average length of analgesia was calculated. The resulting information was analysed using SPSS 19, and the data was shown using statistical tables and charts.
Inclusion criteria: 1) The patients must apply for elective caesarean. 2) The patients must apply for second-time repetition non-emergency caesarean. 3) All mothers must be pregnant with a single fetus. 4) The patients must have filled the informed consent form to take part in the research. 5) They must agree to undergo spinal anaesthesia. 6) They should not be banned from undergoing spinal anaesthesia. 7) They should never be sensitive to local anaesthesia. 8) They should not be sensitive to drugs. 9) They should not be sensitive to Dexmedetomidine. 10) The operation should maximally last 60 minutes. 11) All operations need to be conducted by a single surgeon. 12) All patients must undergo spinal anaesthesia by a single anaesthetist.
Exclusion criteria: 1) All those patients whose spinal anaesthesia has failed and they have applied for general anaesthesia. 2) All patients are suffering from drug abuse. 3) Operations that last longer than 60 minutes. 4) Sensitivity to the drugs used in the project. 5) Having a certain indication of general anaesthesia. 6) Having a BMI equal to or larger than 35. 7) Twine or more patients. 8) Multiparous patients.
Based on the type of research, a clinical trial was chosen as the best method to conduct this research. In line with the principles of simple probability sampling, 84 patients were divided into two groups (42 each) using the randomised numbers table.
The total number of samples is 84 people. And the period of study was 8 months.
Statistical calculations were conducted using SPSS 16 (Chicago, IL, USA). The parametric variables were presented as Mean ± SD and analysed by the analysis of variance (one-way ANOVA) post-hoc test; non-parametric variables were analyzed by Kruskal-Wallis test, and qualitative data were analyzed by chi-square test. A P value less than 0.05 was considered statistically significant.
Results
According to Table 2, no significant difference was observed between the pain score in Dexmedetomidine and fentanyl in recovery and 4, 12, and 24 hours following the operation (0.05 ≤ P). As a result, the two groups were similar regarding pain score.
Table 2.
Comparing the pain score of patients candidate for caesarean using spinal anaesthesia in recovery, 4, 12, and 24 hours after operation in both groups
| Time | Dexmedetomidine | Fentanyl | P-value |
|---|---|---|---|
| Recovery | 0 | 0 | 0.05 ≤ |
| 4 hours following the operation | 5.1 ± 80.8 | 6.02 ± 1.2 | 0.05 ≤ |
| 12 hours following the operation | 2.5 ± 1.03 | 2.1 ± 1.05 | 0.05 ≤ |
| 24 hours following the operation | 1.0 ± 7.88 | 1.09 ± 0.75 | 0.05 ≤ |
Significant: p ≤ 0.05, non-significant: p ≥ 0.05.
As p-value = 0.01, a significant difference was observed between the two groups regarding the average length of analgesia. The average length of postoperative analgesia in fentanyl group was longer than what was observed in Dexmedetomidine group (Table 3).
Table 3.
Comparing the average length of postoperative analgesia and the average amount of drug taken among patients candidate for caesarean with the spinal method in both groups
| Time | Dexmedetomidine | Fentanyl | P-value |
|---|---|---|---|
| Average length of analgesia (hours) | 1.2 ± 57.3 | 4.40 ± 1.4 | 0.01 |
| Groups | Dexmedetomidine | Fentanyl | P-value |
| The average amount of drug taken (in milligrams) | 148.26 ± 8.3 | 119.04 ± 23.3 | 0.01 |
Significant: p ≤ 0.05, non-significant: p ≥ 0.05
As p-value = 0.01, a significant difference was observed between the two groups regarding the average amount of drugs taken within 24 hours after the operation. The average amount of drug taken in fentanyl group was less than what was observed in Dexmedetomidine group (Table 3).
No significant difference was observed between the two groups regarding average blood pressure and heart rate before spinal anaesthesia (P ≥ 0.05) (Table 4).
Table 4.
Comparing the average blood pressure and heart rate of patients candidate for caesarean using spinal anaesthesia before anaesthesia and immediately after anaesthesia and in recovery in both groups
| Groups | Dexmedetomidine | Fentanyl | P-value |
|---|---|---|---|
| Average blood pressure | 74.27 ± 12.2 | 73.92 ± 11.8 | ≥ 0.05 |
| Average heart rate | 85.32 ± 13.8 | 73.83 ± 10.9 | ≥ 0.05 |
| Groups | Dexmedetomidine | Fentanyl | P-value |
| Average blood pressure | 66.80 ± 8.8 | 66.69 ± 7.9 | ≥ 0.05 |
| Average heart rate | 28.74 ± 7.7 | 75.4 ± 9.8 | ≥ 0.05 |
| Groups | Dexmedetomidine | Fentanyl | P-value |
| Average blood pressure | 72.2 ± 8.6 | 73.3 ± 7.9 | ≥ 0.05 |
| Average heart rate | 81.4 ± 6.7 | 82.9 ± 8.7 | ≥ 0.05 |
Significant: p ≤ 0.05, non-significant: p ≥ 0.05.
No significant difference was observed between the two groups regarding average blood pressure and heart rate after spinal anaesthesia (P ≥ 0.05) (Table 4). According to Table 4, no significant difference was observed between the two groups regarding average blood pressure and heart rate in recovery (P ≥ 0.05).
A significant difference was observed between the two groups regarding the frequency of shivering in recovery with the shivering being more common and frequent in Dexmedetomidine group (P = 0.001). According to Table 5, a significant difference was observed between the two groups regarding nausea-vomiting with a higher frequency of nausea-vomiting observed in the fentanyl group (P = 0.001).
Table 5.
Comparing the occurrence of shivering and nausea-vomiting among patients candidate for caesarean using spinal anaesthesia in recovery for both groups
| Groups | Dexmedetomidine | Fentanyl | P-value |
|---|---|---|---|
| The frequency of shivering in recovery | 4 | 2 | 0.001 |
| The frequency of nausea-vomiting in recovery | 1 | 4 | 0.001 |
Significant: p ≤ 0.05, non-significant: p ≥ 0.05.
No statistically significant difference was observed between the two groups regarding their average age (P ≥ 0.05) (Table 6). No statistically significant difference was observed between the two groups regarding the age of the pregnancy (P ≥ 0.05) (Table 6).
Table 6.
Comparing the average age of the patient’s candidate for caesarean in both groups
| Average age | Dexmedetomidine | Fentanyl | P-value |
|---|---|---|---|
| Average age of patients | 24.8 ± 8.7 | 25.1 ± 9.8 | P ≥ 0.05 |
| Average weeks of pregnancy | 39.1 ± 7.8 | 39.5 ± 9.9 | P ≥ 0.05 |
Significant: p ≤ 0.05, non-significant: p ≥ 0.05.
Figure 1 shows are comparing the average postoperative analgesic time and comparing the average amount of drug taken within 24 hours after an operation by patients candidate for caesarean using spinal anaesthesia in both groups.
Figure 1.
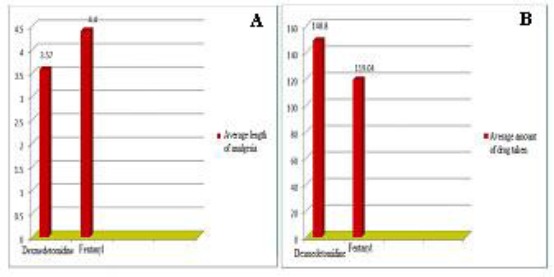
A) Comparing the average postoperative analgesic time; B) The average amount of drug taken within 24 hours after an operation by patients candidate for caesarean using spinal anaesthesia in both groups
Discussion
In this study, 84 pregnant women candidates for elective non-emergency repetitive caesarean were randomly divided into fentanyl and Dexmedetomidine groups. All the qualified participants were randomly distributed into the above-said groups using a randomised numbers table
Our data showed that there was no significant difference between the two groups regarding pain score in recovery, 4, 12 and 24 hours following the operation (P ≥ 0.05). In parallel, we have found between groups the terms of pain score similarly. Moreover, there is a significant difference between the two groups in terms of the average length of analgesia with a longer period of postoperative analgesia reported in fentanyl group (P = 0.01) as well as we have been indicated a significant difference among the two groups in terms of the number of drugs taken within the first 24 hours following the operation with less amount of drugs taken in fentanyl group (P = 0.01).
Furthermore, results demonstrate that there is no significant difference among the groups regarding the average blood pressure and heart rate of patient’s immediately after spinal anaesthesia and recovery (P ≥ 0.05). On the other hand, we have also been exhibited a significant difference between the groups regarding shivering in recovery with higher rates of shivering reported in Dexmedetomidine group (P = 0.001). Regarding nausea and vomiting, the difference between the two groups was significant with a higher rate of nausea and vomiting observed in the fentanyl group (P = 0.001). A study was conducted by Mahendru et al., 2013 to compare adding Dexmedetomidine, clonidine and fentanyl to bupivacaine in an intrathecal manner with the goal of investigating the sedative factors and sensory and motor block and cardiovascular effects and reduction of anaesthetics in spinal anaesthesia. They concluded that Dexmedetomidine has a greater postoperative analgesic effect and a longer period of sensory and motor block with minimum side effects [14]. In the present research, fentanyl resulted in greater postoperative analgesia. This observation can be attributed to the fact that Dexmedetomidine and Fentanyl were both added to lidocaine in our research, whereas in Mahendru et al., 2013, Dexmedetomidine and Fentanyl were added to Bupivacaine. Our research was conducted on pregnant women candidates for caesarean, while Mahendru’s study was conducted on lower limb operations.
Agrawal et al., 2016 researched to compare particulars of the block in spinal anaesthesia using intravenous Dexmedetomidine and clonidine. 5 cases of hypotension were observed in Dexmedetomidine group, while another 7 cases were observed in the clonidine group. The length of postoperative anaesthesia was longer in Dexmedetomidine group. They arrived at the conclusion that better conditions were achieved as a result of using Dexmedetomidine [15]. In the present research, Fentanyl yielded a longer period of anaesthesia with less drug needed after the operation. This difference is probably due to the difference in basic medicine used in our research (lidocaine) and Agrawal’s research (Bupivacaine).
Xiawei et al., 2017 studied the addition of Dexmedetomidine to a mixture of lidocaine and Ropivacaine in elongating the block. Sensory block was achieved earlier in Dexmedetomidine group, and a statistically significant difference was observed (P < 0.05). Motor block was also achieved faster in Dexmedetomidine with a statistically significant difference (P < 0.05). The length of sensory and motor blocks in Dexmedetomidine group was longer with a statistically significant difference (P < 0.05). They claimed that adding Dexmedetomidine to lidocaine and Ropivacaine helped elongate the length of sensory and motor block and sensory and motor blocks will be achieved faster [16]. In the present research, fentanyl elongated the postoperative analgesia.
In another research by Khezri et al., 2014 with the topic the effect of adding clonidine and fentanyl to bupivacaine has been indicated that there is a significant difference between the two groups regarding the length of anaesthesia and the length of the block. They have shown a statistically significant difference was observed between clonidine and fentanyl (P = 0.006). Anaesthesia and block were longer than placebo and clonidine in the fentanyl group, and a significant difference was observed between clonidine and fentanyl (P = 0.001) [17]. The amount of the drug taken up to 24 hours was less and postoperative analgesia was more in fentanyl group. Moreover, in a study else by Parmar et al., 2010 with the subject the effect of intravenous Dexmedetomidine in spinal anaesthesia using ropivacaine suggested that the blood pressure before and after this procedure was less in Dexmedetomidine group. The length of the block in Dexmedetomidine group was longer. A higher sedation score and more demand for Atropine was reported in Dexmedetomidine group. They pointed to the fact that Dexmedetomidine increased the length of the block with fewer side effects and gives the patient appropriate sedation. While using Dexmedetomidine, the anaesthetist must pay attention to bradycardia caused by Dexmedetomidine [18]. In the present research, Fentanyl was more effective than Dexmedetomidine. And also, Mahmoud et al., 2009 studied the effect of adding Dexmedetomidine to bupivacaine in spinal anaesthesia in Urology, they have found that sensory and motor block in 10 μg Dexmedetomidine group was longer, and it took much shorter to achieve block. They concluded that dose influences the effect on the block [19]. In the present research, Fentanyl had a greater influence than Dexmedetomidine.
In conclusion, considering the analysis conducted, the average length of postoperative analgesia in fentanyl group was longer than Dexmedetomidine group. The average amount of drugs taken after operation in fentanyl group was less than Dexmedetomidine group. The frequency of shivering in Dexmedetomidine group was less than the fentanyl group, and higher rates of nausea-vomiting were observed in the fentanyl group.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Martin TC, Bell P, Ogunbiyi O. Comparison of general anaesthesia and spinal anaesthesia for Carsarean Section in Antigua and Barbuda. West Indian Med. 2007;56:330–333. [PubMed] [Google Scholar]
- 2.Samina I. Postoperative analgesia following Caesarean Section intravenous patient-controlled analgesia versus conventional continuous infusion. Open Journal of Anesthesiology. 2012;2:120–126. https://doi.org/10.4236/ojanes.2012.24028. [Google Scholar]
- 3.Pazuki S, Kamali A, Shahrokhi N. Comparison of the Effects of Intrathecal Midazolam and Tramadol with the Conventional Method of Postoperative Pain and Shivering Control after Elective Cesarean Section. Biomedical & Pharmacology Journal. 2016;9:995–1003. https://doi.org/10.13005/bpj/1039. [Google Scholar]
- 4.Behdad S. Analgesic effect of intravenous Ketamine during spinal anesthesia in pregnant women undergone Caesarean Section. Anesth Pain Med. 2013;3:230–233. doi: 10.5812/aapm.7034. https://doi.org/10.5812/aapm.7034 PMid:24282773 PMCid: PMC3833040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta M. Comparision of intrathecal Dexmedetomidine with Buprenorphine as adjuvant to Bupivacaine in spinal anaesthesia. J Clin Diagn Res. 2014;8:114–117. doi: 10.7860/JCDR/2014/7883.4023. PMid:24701498 PMCid: PMC3972523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moraca RJ, Sheldon DG, Thirlby RC. The role of epidural anesthesia and analgesia in surgical practice. Ann Surg. 2003;238:663–673. doi: 10.1097/01.sla.0000094300.36689.ad. https://doi.org/10.1097/01.sla.0000094300.36689.ad PMid: 14578727 PMCid: PMC1356143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skarmas SK. Comparision of pre-mixed and sequentially intrathecal administration of Clonidine with hyperbaric Bupivaxaine in Caesarean Sections. International Multispecialty. Journal of Health. 2015;1:20–24. [Google Scholar]
- 8.Gupta R, Verma R, Bogra J, Kohli M, Raman R, Kushwaha JK. A comparative study of intrathecal Dexmedetomidine and Fentanyl as adjuvants to Bupivacaine. J Anaesthesiol Clin Pharmacol. 2011;27:339–343. doi: 10.4103/0970-9185.83678. https://doi.org/10.4103/0970-9185.83678 PMid:21897504 PMCid: PMC3161458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christiansson L. Update on adjuvants in regional anaesthesia. Periodicum Biologrum. 2009;111:161–170. [Google Scholar]
- 10.Bowdle T. Adverse effect of opioid agonists and agonist-antagonists in anaesthesia. Drug Saf. 1998;19:173–189. doi: 10.2165/00002018-199819030-00002. https://doi.org/10.2165/00002018-199819030-00002 PMid:9747665. [DOI] [PubMed] [Google Scholar]
- 11.Li C, Li Y, Wang K, Kong X. Comparative evaluation of Remifentanil and Dexmedetomidine in general anesthesia for cesarean delivary. Med Sci Monit. 2015;21:3806–3813. doi: 10.12659/MSM.895209. https://doi.org/10.12659/MSM.895209 PMid:26638888 PMCid: PMC4676355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee M, Ko JH, Kim EM, Cheung MH, Choi YR. The effect of intravenous Dexmedetomidine as spinal anaesthesia. Korean J Anaesthesiol. 2014;67:252–257. doi: 10.4097/kjae.2014.67.4.252. https://doi.org/10.4097/kjae.2014.67.4.252 PMid:25368783 PMCid: PMC4216787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdalla W, Ammar MA, Tharwat AI. Combination of dexmedetomidine and remifentanil for labor analgesia: A double-blinded, randomized, controlled study. Saudi J Anaesth. 2015;9:433–438. doi: 10.4103/1658-354X.159470. https://doi.org/10.4103/1658-354X.159470 PMid:26543463 PMCid: PMC4610090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahendru V, Tewari A, Katyal S. A comparison of intrathecal dexmedetomidine, clonidine, and fentanyl as adjuvants to hyperbaric bupivacaine for lower limb surgery: A double blind controlled study. J Anaesthesiol Clin Pharmacol. 2013;29:496–502. doi: 10.4103/0970-9185.119151. https://doi.org/10.4103/0970-9185.119151 PMid:24249987 PMCid: PMC3819844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agrawal A, Agrawal S, Payal Y. Comparison of block characteristics of spinal anesthesia following intravenous Dexmedetomidine and Clonidine. J Anaesthesiol Clin Pharmacol. 2016;32:339–343. doi: 10.4103/0970-9185.188830. https://doi.org/10.4103/0970-9185.188830 PMid:27625482 PMCid: PMC5009840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xiawei L, Jinlei Z, Riyong W, Fangfang X. Dexmedetomidine Added to Local Anesthetic Mixture of Lidocaine and Ropivacaine Enhances Onset and Prolongs Duration of a Popliteal Approach to Sciatic Nerve Blockade. Clinical Therapeutics Journal. 2017;39:89–97. doi: 10.1016/j.clinthera.2016.11.011. https://doi.org/10.1016/j.clinthera.2016.11.011 PMid:27955918. [DOI] [PubMed] [Google Scholar]
- 17.Khezri MB, Rezaei M, Delkhosh Reihany M, Haji Seid Javadi E. Comparison of postoperative analgesia effect of intrathecal Clonidine and Fentanyl added to Bupivacaine in patients undergoing Cesarean Section. Pain Res Treat. 2014;2014:513628. doi: 10.1155/2014/513628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parmar K. Effect of intrathecal Ropivacaine with Dexmedetomidine for operative and postoperative analgesia. Journal of Evaluation of Medical and Dental Sciences. 2014;3:2917–2925. https://doi.org/10.14260/jemds/2014/2225 PMid:25071006. [Google Scholar]
- 19.Mahmoud M, Sami A, Aloweidi A. Effect of dexmedetomidine added to spinal bupivacaine for urological procedures. Saudi J Anaesth. 2009;30:365–370. [PubMed] [Google Scholar]


