Abstract
Purpose
The study was designed to provide programmatic recommendations for interventions to increase contraceptive prevalence in northern Nigeria. Family-planning use in North-East and North-West regions of Nigeria has remained very low, despite years of domestic and donor investments. We examine respondents’ perceptions of their own need for contraception and specifically focus on young women because of their higher risk for maternal mortality.
Methods
In this cross-sectional study, we interviewed 1,624 married women younger than 25 years and 1,627 men married to women younger than 25 years, in Kaduna and Katsina states in northern Nigeria. We classified respondents into five categories: 1) having no real need for contraception, 2) perceiving no need for contraception, despite physical or behavioral need, 3) having met need by using a modern contraceptive method, 4) perceiving met need by employing traditional practices, and 5) having unmet need for contraception.
Results
Half of female respondents had no need for contraception because they were either pregnant or desiring a pregnancy at the time of the survey. A quarter of female and male respondents were not using contraception because of their religious beliefs. Less than 2% of respondents had unmet need because of lack of availability or access, or due to poor quality of care. Men had more positive views of family planning than women.
Conclusion
Our findings suggest that young women in northern Nigeria would benefit from a programmatic approach that targets men, utilizes religious leaders, and addresses the prevalent religious and sociocultural norms that present barriers to contraceptive use. Such interventions have the potential to increase contraceptive prevalence more substantially, but the literature on these types of interventions in northern Nigeria is scarce. Therefore, more research is needed to identify and document what approaches work or do not work to increase contraceptive use in northern Nigeria.
Keywords: family planning, unmet need, adolescents, northern Nigeria, religious norms, social norms
Introduction
It is estimated that globally about 758 million women married or in union were using contraception in 2015. Of these, about 142 million women were in sub-Saharan Africa. Yet unmet need for family planning remains high, especially in sub-Saharan Africa where it is highest, at 24%.1 Unmet need for family planning translates into unwanted pregnancies, with associated health risks for mothers and children.2 The burden of these health risks is highest among young mothers, especially those younger than 20 years,3 who have a higher risk of eclampsia, puerperal sepsis, endometritis, systemic infections, low birthweight, preterm delivery, and several neonatal complications.4 There fore, reducing unmet need for contraception among young women has significant implications for reducing maternal and neonatal mortality and improving health outcomes.
This study unpacks unmet need for contraception of young women and men married to young women in northern Nigeria, which is characterized by some of the poorest health indicators in the world. The total fertility rate for North-West region Nigeria in 2013 was 6.7, compared to the national figure of 5.5.5 Similarly, maternal mortality ratio for North-East region of Nigeria was recently estimated at 1,549 per 100,000 live births, compared to the national figure of 560.6 Results from the 2013 Nigeria Demographic and Health Survey (DHS) show that early marriage remains a common practice in northern Nigeria. Among married women in the region aged 15–24 years, the median age of marriage was 15, and many girls married when they were 12 years old or younger.5
Contraceptive use in northern Nigeria is very low. In 2013, only 2.7% and 3.6% of married women aged 15–49 years in North-East and North-West regions of the country, respectively, were using a modern contraceptive method, with even lower use in rural areas.6 A multivariate analysis of national-level 2013 DHS data, which controlled for geographic region, found that older, better educated, and wealthier women were more likely to use a modern contraceptive method.7 A recent analysis of additional variables, using the same data, found that ideational characteristics, socioeconomic and demographic profiles, and Islamic religious culture explained the gap in contraceptive use between northern and southern Nigeria.8
Despite the very low rate of contraceptive use in the region, unmet need for family planning among married women of reproductive age was only 17.5% in the North-East and 12.0% in the North-West regions.5 Low contraceptive prevalence coexists in the region with relatively low unmet need rates, because married women in northern Nigeria appear to want many children and therefore do not wish to use contraception. A recent review of the literature found several religious and cultural norms that contribute to this phenomenon. Muslims, the religious majority in northern Nigeria, follow the religious injunction to procreate, and there is a prevailing belief that children are gifts from God, and as such should not be refused. Men want their lineage to continue through their many children, as more children mean higher prestige. Also, in polygamous marriages wives compete to have the most children, believing that the more children they have the more their husbands would love them, so that their children would get a larger share of his inheritance; in monogamous marriages, women want to have many children so that their husbands will not want to take a second wife.9
These figures have not significantly changed despite years of programming to increase availability and accessibility to family-planning services and improve quality of care. According to the 2013 DHS, contraceptives are available in most public primary health care facilities in Nigeria, free of charge. With the exception of condoms and oral contraceptives, which are most commonly bought from chemists (patent medicine stores), the most common source for contraceptives is public health facilities.5 Studies show that women are fairly satisfied with the quality of family-planning services in northern Nigeria.10
In this context, therefore, it is important to better understand the dynamics of unmet need for family planning in northern Nigeria, to help customize programs to improve family-planning utilization. Sinai et al proposed a model of unmet need for contraception, which considers women’s perceptions of their need, to allow for more targeted program design (Box 1).11 The model classifies unmet need into five categories: real no need, perceived no need, real met need, perceive met need, and unmet need.
Box 1. Unmet-need model proposed by Sinai et al as a practical approach for program design.
Real no need. These are women who currently have no need for contraception. This may be permanent if, for example, they have had a hysterectomy, or temporary if they are currently pregnant, or desire to have a child in the near future. As long as they are in this state, they would not be interested in family-planning information or services, because at the current time they would not use these, even if they will have a need in the future.
Perceived no need. These women think that they have no need for contraception, and therefore do not use family planning methods, but in fact they do have a need. Examples are women who think that they are protected from pregnancy because they only have sex infrequently, or because they are still in postpartum amenorrhea. As long as they perceive that they do not have a need, they too would not be interested in family-planning information or services. Women with perceived no need would benefit most from programs that would provide couples with information about their fertility, including, for example: 1) the days in the cycle in which women can become pregnant, 2) the fact that men are fertile all the time, 3) that infrequent sexual activity can still result in pregnancy, and 4) that breastfeeding women can conceive, including when they are still in postpartum amenorrhea.
Real met need. These are women who use a modern contraceptive method.
Perceived met need. These women use traditional practices, such as withdrawal, or the use of herbs and tinctures. They are not protected from pregnancy, but they think that they are, therefore they are not interested in modern contraceptives. These women would benefit most from informational programs about how ineffective traditional practices are and the benefits of modern contraceptive use.
Unmet need. These are women who are not pregnant, do not wish to become pregnant in the near future, consider themselves fertile, and do not belong to either of the other four categories. Depending on the reason they do not use a method, they would benefit from traditional supply-side programming (eg, increased availability, accessibility, and quality of family-planning services), or from community-level interventions that address gender norms.
The authors tested their model using data from Mali and Benin10 and found that sampled women in Mali would have benefited most from programs to improve availability, accessibility, and quality of services, while women in their Benin sample would have benefited from educational programs about their fertility and the fact that traditional family-planning practices are not effective in preventing pregnancy.
The Sinai et al model has an added advantage in that it can be used to examine unmet need not only for women but also men. This is significant in the northern Nigeria context, where many women are not empowered to attend family-planning services and men make most household decisions, including decisions about how many children to have, when to have them, and whether to use contraception.10,12 Moreover, there is very little covert use of family planning in northern Nigeria, because women are afraid of severe consequences if their husbands find out. A 2011 survey found that if men learned that their wife was using contraception covertly, 31% would scold her, 18% would beat her, 16% would divorce her, and 14% would tell other family members in order to shame her.13
The Sinai et al model requires only seven survey questions and is easy to include in broader surveys. This current study uses the model to better understand the drivers of unmet need for family planning of young married women, and of men married to young women, in northern Nigeria. It provides information that would be useful in designing programs to increase demand for, and utilization of, modern contraception in the region.
Methods
Using a structured questionnaire, we interviewed 1,624 married women younger than 25 years, and 1,627 married men, who had a wife younger than 25 years, as part of a cross-sectional study on knowledge, attitudes, and perceptions of various aspects of maternal and child health, including family planning. The study was undertaken in Kaduna and Katsina states, two of the states where the Maternal Newborn and Child Health 2 (MNCH2) Programme is active.
Sample selection
The women and men were surveyed in the same areas, and used similar sampling methodologies, but the two samples were selected independently. That is, we did not interview married couples or women and men from the same households. We began by randomly selecting one local government area from each of the three senatorial districts in each state. We listed all communities in the selected areas, and then removed from the list communities supported by other maternal and child health programs, so that our results would not be contaminated by their programmatic efforts. We then randomly selected two communities from each selected area, for a total of 12 study communities in the two states combined.
Our target sample size was 800 young women and 800 men in each state, so as to have sufficient power for statistical calculations that are beyond the scope of the current paper. To identify respondents, we listed all households residing in the 12 selected communities. For the women survey, we randomly selected a quarter of the households from the list using a random number generator on an Android phone. About two-thirds of the selected households included at least one married woman younger than 25 years, and one respondent from each of these households was interviewed. To survey men, we used a random number generator on an Android phone to select households from the list, and one eligible man was selected from each. For both samples, if there were two eligible individuals in the same household, one was randomly selected.
Data collection
Before data collection began, we obtained ethical approval for the protocol, study instruments, and all study procedures from the Health Research and Ethics Committees of Kaduna and Katsina states. Men were interviewed by male interviewers and women by female, to align with cultural and religious norms in the region. Since many married women in northern Nigeria are limited in their social interactions without their husbands’ permission,10 and may be in physical or emotional risk if they go against his wishes, we ensured that these norms were respected, in addition to following all international and Nigerian guidelines for protecting the privacy and confidentiality of study participants. All respondents provided informed consent in private. In some cases, women’s husbands or other relatives needed to agree to the woman’s participation. However, the woman was then consented privately also, to ensure that she was not coerced to participate, and it was explained to her husband that she must be interviewed in private, and that her responses cannot be shared with him, or the study results would not be valid. As approved by both ethics committees, consent was verbal, so as not to keep any record of respondents’ identities.
The Nigerian Constitution does not establish a minimum age for marriage, and by Nigerian law married women of any age are considered emancipated adults.14 Therefore, the few very young respondents did not need consent from a parent or guardian to participate in the study. Our youngest respondents were 12 years old, although we encountered younger married girls. We interviewed only young women that the interviewers judged to be sufficiently mature to understand the questions and respond coherently.
Fieldwork was undertaken in early 2017. The interviews were done in Hausa, the most commonly used local language in Kaduna and Katsina. The women and men questionnaires were parallel and asked the same questions, but with the appropriate gender terminology. Data were collected directly into Android phones, using the SurveyCTO application. Simple frequencies and cross-tabulations were calculated using SPSS version 23.15
Operationalizing the model
The seven survey questions needed to categorize respondents into the five contraceptive need categories were part of a structured questionnaire that included a variety of questions about respondents’ knowledge and attitudes related to family planning and maternal and child health. The questions, as presented in the manuscript that introduced the Sinai et al model, are:11
Are you pregnant now? (yes = real no need);
(if no to #1) Would you like to become pregnant within the next 12 months? (yes = no real need);
(if no to #2) Are you currently doing something to delay or avoid getting pregnant? (yes = met need, real or perceived);
(if yes to #3) Which method are you using? (modern = real met need; traditional = perceived met need);
(if no to #3) Is it possible for you to become pregnant?;
(if no to #5) Why do you say that? (real or perceived no need, depending on reason);
(if yes to #5) You said that you do not want to become pregnant this year, but you are not using any method to avoid pregnancy. Please tell me why (perceived unmet need or perceived no need, depending on reason).
Female respondents’ need status was determined as follows:
Real no need: respondents who were pregnant at the time of the survey, desired to have a child in the next year, or had a hysterectomy.
Perceived no need: respondents who said that they were not using a method because they were breastfeeding or have not yet menstruated following childbirth, because they had sex only infrequently (due, eg, to their husband’s frequent travel), or because they perceived that they were sub-fertile.
Real met need: respondents who said that at the time of the survey they were using one of the following modern contraceptive methods: female or male sterilization, oral contraceptives, injection, implant, intrauterine device, condom, diaphragm, Standard Days Method, or lactational amenorrhea method.
Perceived met need: respondents who said that at the time of the survey they were using a traditional family-planning practice. These included periodic abstinence, withdrawal, the use of a variety of potions or tinctures (drink or douche), and amulets.
Unmet need: any of the respondents who did not fit into any of the other categories were considered to have an unmet need. They were sexually active, were not pregnant, did not wish to become pregnant in the near future, yet were not using a method, for a reason that did not imply that they believed they had no need for contraception. Included in this category were respondents whose husbands did not allow them to use a method or would not discuss method use with them, those who were afraid of side effects or health consequences of method use, respondents who believed that contraceptive use is against their religion, and those who did not have access to available methods (eg, did not know where to get a method, method too expensive, etc).
Men’s need status was determined in the same manner as women’s, but with one crucial difference. Women could have one, and only one, need status. By definition, they could only fit in one of the five need categories. Men, however, could have more than one need status assigned to them. Since polygamy is prevalent in northern Nigeria, men were asked the seven questions needed to determine their need status for each of their wives separately, and therefore could have a different need status for each wife.
Results
We interviewed a total of 1,624 young women and 1,627 men respondents in Kaduna and Katsina states combined. Table 1 shows their characteristics. Because our target population for each sample was different – women were all younger than 25 years and men could be of any age, as long as they had a wife younger than 25 years – the two samples were quite different. By definition, men were much older (age range 18–80 years). The age range for women respondents was 12–25 years.
Table 1.
Respondent profile
| Characteristic | Women (n=1,624) | Men (n=1,627) |
|---|---|---|
|
| ||
| Mean age (years) | 19.9 | 40.1 |
| % Muslim | 97.5 | 90.1 |
| % in polygamous marriage | 31.2 | 27.0 |
| Mean age at first marriage (years) | 15.4 | |
| Mean number of living children | 1.4 | 4.7 |
| % literate | 32.0 | 64.0 |
| % work outside the home | 49.8 | 95.6 |
| % household connected to electricity | 49.7 | 58.2 |
| Mean ideal number of children | 8.5 | |
Most respondents were Muslim and over a quarter were in polygamous marriages (maximum four wives). The 63.9% of women who had at least one child had, on average, 2.1 children. Men had between 0 and 38 living children. Men were significantly better educated than women, and most worked outside the home, compared to only about half of women. We used electricity as proxy for household wealth and found that the households of about half of the respondents were not connected to electricity.
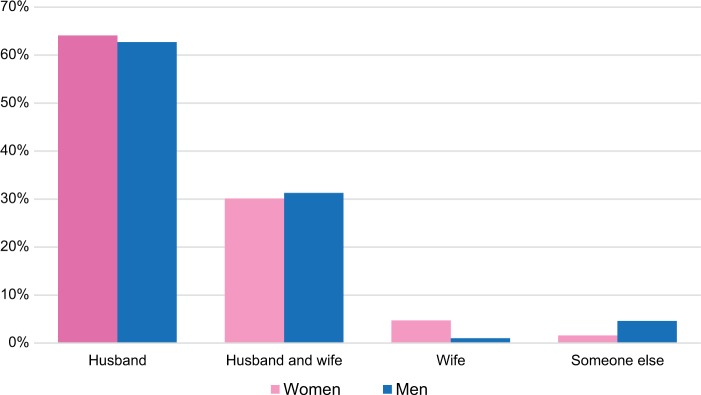
Women respondents in our sample married young. The mean age at first marriage was 15.4 years, and 8.7% of women were married at age 12 years or younger (as young as 8 years of age). They wanted to have large families, with an overall ideal number of children of eight in Kaduna and nine in Katsina. As Figure 1 shows, about two-thirds of both men and women believed that the husband alone should decide whether or not to use contraception. Table 2 shows knowledge and use of modern contraception overall, and for the four most used methods in the region: oral contraceptive, injection, implant, and condom. While current contraceptive prevalence is low, we see that significantly more men than women have heard of methods, have ever used them, and were using them at the time of the survey.
Figure 1.
Perceptions of who should decide to use contraception.
Table 2.
Knowledge and use of modern contraceptive methods (%)
| Knowledge and use by method | Women (n=1,624) | Men (n=1,627) |
|---|---|---|
|
| ||
| Heard of at least one modern contraceptive method | 46.0 | 57.5 |
| Heard of oral contraceptives | 38.3 | 32.9 |
| Heard of injection | 39.7 | 42.0 |
| Heard of implant | 18.8 | 16.3 |
| Heard of male condom | 11.1 | 31.8 |
| Ever used a modern contraceptive method | 9.2 | 23.0 |
| Ever used oral contraceptives | 5.1 | 6.8 |
| Ever used injection | 4.2 | 12.5 |
| Ever used implant | 1.4 | 5.0 |
| Ever used male condom | 1.7 | 6.3 |
| Currently using a modern contraceptive method | 5.2 | 12.7 |
| Currently using oral contraceptives | 2.2 | 3.6 |
| Currently using injection | 1.8 | 6.0 |
| Currently using implant | 0.9 | 3.3 |
| Currently using male condom | 0.8 | 2.5 |
Notes: Modern contraceptive methods include female and male sterilization, oral contraceptives, intrauterine device, injectables, implants, condoms, diaphragm, and Standard Days Method.
We next look at need for contraception. This is shown in Table 3. Half of women had no current need for contraception – almost all because they were currently pregnant or wished to become pregnant within a year. The next largest categories were women and men who had no fertility intensions because of their religion. When we asked them if they wanted to have more children they said that how many children they had was “up to God”. We cannot determine if they wanted to have a child now (real no need), or if they would have preferred to not become pregnant, had they felt empowered to make fertility decisions (unmet need). All men in this category and 98% of women were Muslim.
Table 3.
Need for contraceptiona (%)
| Need status | Women (n=1,611b) | Men (n=1,540b) |
|---|---|---|
|
| ||
| No real need Perceived no need Real met need (uses modern contraceptive method) Perceived met need (uses traditional method) Unmet need Fertility intentions not known because “It is up to God” |
50.2 12.9 5.2 0.6 10.8 20.4 |
60.0 6.0 13.4 2.5 5.0 23.2 |
|
| ||
| Reason for unmet needc Against religion Fear of side effects or health risk Spouse would not approve Supply-side reason Community perceptions |
5.8 2.1 2.0 1.2 0.3 |
3.8 1.6 0.5 1.2 0.6 |
Notes:
While women’s status is unique, men can have more than one status, if they have a different status with different wives. Therefore, figures add to more than 100% for men.
There was insufficient data to determine need status for 14 women and 87 men.
Both women and men could specify more than one reason for their unmet need. Therefore, totals add to more than the total unmet need figures.
Modern contraceptive use was low, but traditional method use was lower. About 11% of women and 5% of men had unmet need as defined by the Sinai et al model.9 They were not pregnant, did not want to become pregnant in the next year, were sexually active, realized that they were at risk for pregnancy, and yet were not using a method. Of interest is the reason they provided for not using a contraceptive method. As Table 3 shows, about 6% of women and 4% of men (more than half of women with unmet need and three-quarters of men with unmet need) said this was because of their religion. Few respondents were not using a method because of their perceptions of community and spousal disapproval, because of fear of side effects or health consequences, or because of supply-side factors such as availability and accessibility to methods or quality of care.
To gage overall attitudes toward contraceptive use, we asked respondents if they agreed or disagreed with statements about contraception, some positive and some negative. As Table 4 shows, men’s views of contraception were substantially more positive than women’s. A larger proportion of men agreed with the positive statements, and a larger proportion of men disagreed with the negative statements.
Table 4.
Opinions about contraception
| Statement | Women (n=1,624) | Men (n=1,627) |
|---|---|---|
|
| ||
| Positive statements (% agree) Women who use family planning look better than women who do not use family planning Couples who practice family planning and have fewer children are better able to provide for their family |
35.1 41.9 |
40.3 42.0 |
|
| ||
| Negative statements (% disagree) Women who use family planning are straying from the correct path or are immoral Family planning methods provided by the health programs in this community are difficult to use Using family planning is bad for a woman’s health |
46.8 31.7 31.2 |
50.9 37.0 51.3 |
Discussion
The study was designed to analyze the need for contraception among young married women, and of men married to young women, in two states in northern Nigeria, with a focus on programmatic implications. Overall, our results confirm the findings reported in literature about northern Nigeria. Women in the region marry early, and many are not educated. On the surface, it appears that couples want to have many children, and men are the ones who make decisions about how many children to have, when to have them, and whether or not to use contraception. When we look deeper, however, we see that both women and men do not feel empowered to decide how many children they want; therefore, we cannot really say that they want to have many children. We can speculate that the large number they provided in response to the question was more an expectation than a wish for many children.
Our men and women samples were quite different by definition. Men had many more children both because they were older and because more than a quarter had multiple wives. Polygamy and the age difference may explain, in part, some other observed differences between men and women, such as knowledge and use of modern contraceptive methods. Significantly more men than women had heard of at least one modern contraceptive method. We can speculate that this was because 1) men had more opportunities to be exposed to family-planning messages, as they were older, and they had more freedom to move about than women in the region; and 2) they may have heard about methods from more than one wife. And yet fewer than 60% of men had heard of a method, so that there is significant room for improvement. Similar proportions of women and men had heard about oral contraception, injections, and implants, but significantly more men than women had heard of condoms, which is not surprising.
Ever and current use of modern contraceptive methods show similar patterns. More than twice as many men than women had ever used a modern method or were using a method at the time of the survey, which was expected given polygamy (one wife using a method and another does not). While it is not surprising that more men than women had ever used condoms, it is interesting to note that more men than women had also ever used (or, rather, one of their wives had ever used) or were currently using, contraceptive injection. Still, only 5.2% of women were using a modern contraceptive method at the time of the survey, and 13.4% of men were using a method with at least one of their wives. These figures are higher than the 2013 DHS figures for Kaduna and Katsina states,5 but are still very low.
Programs to increase demand for and utilization of family-planning methods can take a variety of forms. Some programs, for example, are designed to increase the availability and accessibility of methods or improve quality of care, while others are aimed at demand creation. Our findings allow us to identify the type of programs that would be most beneficial in the northern Nigeria context.
Almost a quarter of female respondents were not using a contraceptive method because of their religious beliefs. They either did not feel empowered to decide whether or not they would want to have another child because this was “up to God” or they did not want to become pregnant, but felt that using a method would be against their religion. A half of female respondents were either pregnant at the time of the survey or desired a pregnancy in the near future. It is quite likely that many of these were pregnant or desiring a pregnancy because of their religious beliefs. Therefore, interventions that target these religious beliefs have a great potential in increasing family-planning use in the study areas.
The majority of the population in northern Nigeria are Muslim. There are several conflicting interpretations of Islamic scripture related to contraceptive use. Some Muslim scholars perceive the use of contraception to be un-Islamic, as seems to be the case in many parts of northern Nigeria. However, family planning in the context of child spacing was discussed in Muslim communities hundreds of years ago, right from the early days of Islam, and Islamic teachings clearly demonstrate under which conditions this is allowed and what methods are permissible.16 While some Islamic religious scholars believe that contraceptive use is forbidden, others view Islam as a religion of mercy, and argue that contraceptive use is permissible when excessive fertility leads to proven health risks to mother and child, or if it leads to economic hardship or the inability of parents to raise their children according to religious tradition.13 As a result, contraceptive prevalence is quite high in some majority Muslim countries, such as Indonesia, where 62.5% of married women of reproductive age were using contraception in 2013.17
The few pilot studies that attempted to harness religious leaders to the cause of increasing contraceptive use in northern Nigeria show promise. For example, the Center for Development and Population Activities implemented a program in northern Nigeria where Imams were trained to advocate for birth spacing and the use of modern contraception. The Chief Imam clarified Islam’s position on using modern contraception, affirming the critical message that birth spacing is desirable for the well-being of mother and child, and this helped to positively influence the network of Islamic leaders in northern Nigeria.18 Operations research is needed to test interventions that use religious leaders in northern Nigeria to advocate for birth spacing and contraceptive use. Such interventions could, for example, use Islamic scholars who approve of family-planning use to educate Imams and sensitize them, so that they later advocate for birth spacing in their sermons, emphasizing health benefits to mother and child, or through example in their own married life.
Another factor to consider when deliberating the effect of religion on family-planning method use is the specific method. Short-acting methods may be more permissible than long-acting ones, as they are useful for birth spacing and not for birth limiting which is forbidden. Contraceptive pills, injections, implants, and condoms all have potential for significant uptake in northern Nigeria. The Standard Days Method, a modern fertility awareness-based method of family planning, also shows promise.19
Previous studies in northern Nigeria suggest that communities are not in favor of contraceptive use. Women who use contraceptives are considered promiscuous, and men who allow their wives to use contraceptives are considered weak.20 And yet only four women and 12 men in our samples said this was the reason that they were not using contraception. This does not mean that community-level programs to address gender norms and overall community perceptions are not necessary. They simply take second place to targeting religious interpretations. We posit that programs involving religious leaders can target this aspect of community dynamics, in addition to individual perceptions.
We observed very little use of traditional methods. On the other hand, almost 13% of women had perceived no need for family planning because they only had sex infrequently, or because they believed that breastfeeding or postpartum amenorrhea protected them from pregnancy. A recent study found that about two-thirds of women who attended a tertiary hospital in Kano state in northern Nigeria resumed sexual relations within 8 weeks of giving birth.21 These women are at risk of pregnancy and would benefit from educational programs, perhaps at the community level, providing information about fertility awareness. Such programs can take many forms, such as the use of public media or providing information in health facilities. Further research is needed to test the impact of these programs on contraceptive prevalence in the region.
About 11% of women had what the model we used termed “unmet need”. Few said that the reason they were not using a method was lack of access. Some were not using contraception because of fear of side effects or health risks, or because their husbands would not approve, but half were not using a method because they felt it was against their religion. This finding implies that programs to increase availability of and access to contraception, as well as to improve quality of counseling about side effects and health risks may not be top priority. While such interventions are always important, couples in northern Nigeria seldom avail themselves of their benefits.
Given that our findings for men mirrored the findings for women and that both men and women respondents agreed that men should make fertility decisions, it is key for programs that are designed to increase contraceptive uptake to target men. Few programs in northern Nigeria have done this,9 but those show promise. For example, the Maternal and Child Health Integrated Program, funded by The United States Agency for International Development (USAID), trained 247 male motivators in Kano, Katsina, and Zamfara states to counsel men on the importance and benefits of healthy timing and spacing of pregnancies and the use of modern contraceptives. Their intervention demonstrated the potential usefulness of targeting men. The 19% contraceptive acceptance rate in the project, while still low, was significantly higher than the 3% known figure for the region at the time.22 This intervention should be replicated at a larger scale and tested, to see if this is the best model for involving men in promoting birth spacing in northern Nigeria. We also advocate the need for a social network analysis study of men in northern Nigeria, to assess information flow, and determine the best approach for educating men on the benefits of birth spacing and family-planning use on a large scale.
The Sinai et al model we followed uses five categories to classify need for family planning: 1) having no real need for contraception; 2) perceiving no need for contraception, despite physical or behavioral need; 3) having met need by using a modern contraceptive method; 4) perceiving met need by employing traditional practices; and 5) having unmet need for contraception. We posit that there is one more category – one in which many of our respondents belong – 6) not feeling empowered to make decisions about how many children to have, when to have them, or whether or not to use contraception, because this is completely “up to God”.
Conclusion
Family-planning programming has been ongoing in northern Nigeria for many years with significant domestic and donor investments. The focus has been on increasing availability and accessibility to methods, improving quality of care, advancing governance and supply-chain issues, with some demand-creation efforts. Yet modern contraceptive prevalence remains very low. Our results show that couples in northern Nigeria would benefit from a different approach, one that targets men, utilizes religious leaders, and works with the prevalent religious and social norms, rather than against them. Such interventions have the potential to increase contraceptive prevalence more substantially. However, the sheer size of the region may pose a challenge for interventions to achieve impact at the population level. To be successful in increasing contraceptive prevalence, programs must be undertaken on a very large (and expensive) scale. It is therefore crucial that interventions are well tested in the northern Nigeria context before they are scaled up, to improve their probability of success. The literature on past interventions that used a similar approach is scarce. Therefore, more research is needed so that relevant programs can be undertaken and scaled up in northern Nigeria, for improved health outcomes.
Acknowledgments
This study was funded by UK aid from the UK government through the Nigeria MNCH2 Programme (PO 6468); the views expressed are the authors’ and do not necessarily reflect the UK government’s official policies.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.United Nations, Department of Economic and Social Affairs, Population Division Trends in Contraceptive Use Worldwide 2015 (ST/ESA/SER.A/349) 2015 [Google Scholar]
- 2.Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev. 2010;32(1):152–174. doi: 10.1093/epirev/mxq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mouli-Chandra V, McCarraher DR, Phillips SJ, Williamson NE, Hain-sworth G. Contraception for adolescents in low and middle income countries: needs, barriers, and access. BMC Reproductive Health. 2014;11(1):1. doi: 10.1186/1742-4755-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ganchimeg T, Ota E, Morisaki N, et al. Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. BJOG. 2014;121(S1):40–48. doi: 10.1111/1471-0528.12630. [DOI] [PubMed] [Google Scholar]
- 5.National Population Commission (NPC) [Nigeria] and ICF International . Nigeria Demographic and Health Survey 2013. Abuja, Nigeria and Rockville, MA: NPC and ICF International; 2014. [Google Scholar]
- 6.African Population and Health Research Center [webpage on the Internet] Maternal Health in Nigeria: Facts and Figures. [Accessed March 23, 2018]. Available from: http://aphrc.org/post/publications/maternal-health-nigeria-facts-figures.
- 7.Ejembi CL, Dahiru T, Aliyu AA. Contextual factors influencing modern contraceptive use in Nigeria. DHS Working Paper No 120. Rockville, MA: ICF International; 2015. [Google Scholar]
- 8.Babalola S, Oyenubi O. Factors explaining the North–South differentials in contraceptive use in Nigeria: A nonlinear decomposition analysis. Demogr Res. 2018;38(12):287–308. [Google Scholar]
- 9.Sinai I, Anyanti J, Khan M, Daroda R, Oguntunde O. Demand for Women’s Health Services in Northern Nigeria: A Review of the Literature. Afr J Reprod Health. 2017;21(2):96–108. doi: 10.29063/ajrh2017/v21i2.11. [DOI] [PubMed] [Google Scholar]
- 10.Ual K, Sambo MN, Oche MO, Saad A, Raji MO, Isah A. Determinants of client satisfaction with family planning services in government health facilities in Sokoto, Northern Nigeria. Sahel Med Stud. 2017;8(1):20–26. [Google Scholar]
- 11.Sinai I, Igras S, Lundgren R. A practical alternative to calculating unmet need for family planning. Open Access J Contracept. 2017;8:53–59. doi: 10.2147/OAJC.S137705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolf M, Abubakar A, Tsui S, Williamson NE. Child Spacing Attitudes in Northern Nigeria. Washington, DC: FHI; 2008. [Google Scholar]
- 13.Ameh N, Shittu OS, Abdul MA. Role of men in contraceptive use in northern Nigeria: a cross sectional study. Trop J Obste Gynaecol. 2011;28(1):43–47. [Google Scholar]
- 14.Girls not Brides [webpage on the Internet] Nigeria. 2018. [Accessed April 24, 2018]. Available from: https://www.girlsnotbrides.org/child-marriage/nigeria/
- 15.IBM CR . IBM SPSS Statistics for Windows, Version 23. Armonk, NY: IBM Corp; 2015. [Google Scholar]
- 16.El Hamri N. Approaches to family planning in Muslim communities. J Fam Plann Reprod Health Care. 2010;36(1):27–31. doi: 10.1783/147118910790291019. [DOI] [PubMed] [Google Scholar]
- 17.The World Bank [webpage on the Internet] Data: Contraceptive Prevalence. [Accessed March 30, 2018]. Available from: https://data.worldbank.org/indicator/SP.DYNCONU.ZS?locations=ID.
- 18.CEDPA Engaging social networks in family planning programming: lessonsfrom research and interventions. A report for: Terikunda Jekulu: Using network analysis to address unmet need in Mali. 2012. [Accessed March 30, 2018]. Available from: http://irh.org/resource-library/terikunda-jekulu-using-network-analysis-for-social-change-breaking-through-the-barriers-of-unmet-need-for-fp-in-mali/
- 19.Ujuju C, Anyanti J, Adebayo SB, Muhammad F, Oluigbo O, Gofwan A. Religion, culture and male involvement in the use of the Standard Days Method: evidence from Enugu and Katsina states of Nigeria. Int Nurs Rev. 2011;58(4):484–490. doi: 10.1111/j.1466-7657.2011.00900.x. [DOI] [PubMed] [Google Scholar]
- 20.Ankomah A, Anyanti J, Abebayo S, Giwa A. Barriers to contraceptive use among married young adults in Nigeria: a qualitative study. Int J Trop Dis Health. 2013;3(3):267–282. [Google Scholar]
- 21.Iliyasu Z, Galadanci HS, Danlami KM, Salihu HM, Aliyu MH. Correlates of postpartum sexual activity and contraceptive use in Kano, northern Nigeria. Afr J Reprod Health. 2018;22(1):103–112. doi: 10.29063/ajrh2018/v22i1.10. [DOI] [PubMed] [Google Scholar]
- 22.Nyako Z, Usuf S, Segun T, Airede L, ishola G, Otolorin EO. Use of male birth spacing motivators to mobilize communities for family planning acceptance in northern Nigeria. Inernational Conference on Family planning; Dakar Senegal. 2011; [Accessed October 03, 2018]. Available from: http://fpcon-ference.org/2011/wp-content/uploads/FPConference2011-Agenda/default_1023.html. [Google Scholar]