Abstract
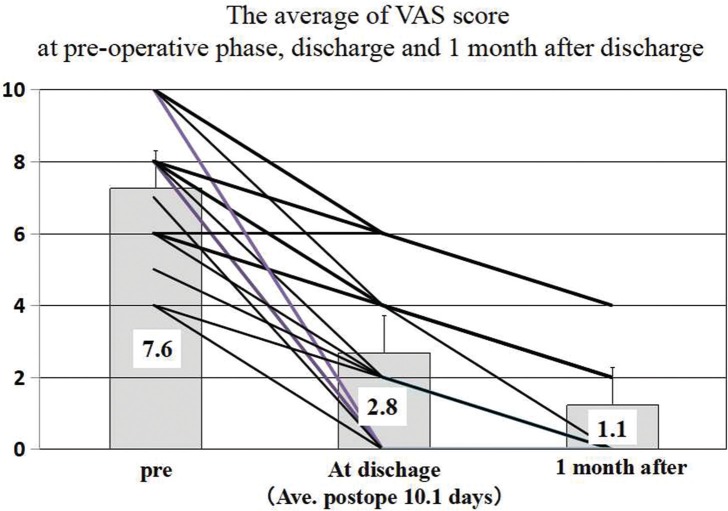
This study was to assess the efficacy of microdiscectomy, cage fixation, and right tranuncal foramintomy for the patients suffering from right radiulo-myelopathy. Anterior cervical foraminotomy was reported to be an effective option for the treatment of cervical degenerative radiculopathy but with the problem of recurrence. Since Hakuba reported the method of trans-unco-discal approach in 1976, it was designed as keyhole foraminotomy which was called transuncal approach, transpedicular approach or transvertebral approach. In the anterior approach, we usually use the right-sided approach because most of us are right-handed surgeons. We retrospectively investigated our patients who had the right foraminal stenosis causing radiculopathy and were treated with microdiscectomy, cage fixation, and right keyhole transuncal foraminotomy. Since 2011, 23 patients were treated with the manner. All of the 23 patients who had central canal stenosis and among the 23 patients, 8 patients showed only right radiculopathy and 15 patients showed radiculo-myelopathy. In all patients, the radiculopathy disappeared or significantly improved without any complications postoperatively. The average of VAS scores was 7.6 ± 2.2 in preoperative state, 2.8 ± 2.2 at discharge, and 1.1 ± 1.6 in 1 month after surgery. The average of follow-up time was 38.3 months and they had no recurrence of radiculopathy. We showed that this manner is effective and one option for the combined disease of right foraminal and canal stenosis and we believe that this manner is not complex and safe if we can understand the anatomy.
Keywords: cervical radiculopathy, transuncal foraminotomy, cage fixation, uncinate process, recurrence
Introduction
Since Hakuba1) reported the trans-unco-discal approach as a method of anterior foraminotomy of cervical spondylosis, some surgeons proposed the variant methods of anterior foraminotomy.2–4) In 2009, Matz et al. reviewed the indications for anterior cervical decompression for the treatment of cervical degenerative radiculopathy.5) With regard to anterior cervical discectomy with or without fusion and anterior cervical foraminotomy compared to physical therapy or conservative immobilization, more rapid relief (within 3–4 months) may be seen with anterior cervical discectomy with or without fusion with the maintenance of gains over the course of 12 months. Conflicting evidence exists as to the efficacy of anterior foraminotomy with reported success rates of 52–99% but recurrent symptom is as high as 30%.
We usually used the right-sided approach in the anterior approach, because the right-handed surgeons have easier access in using a drill in right-sided approach. We do not drill out end plate of upper and lower vertebrae to prevent subsidence of cylindrical titanium cages. But it is not easy to drill out the osteophytes and remove disc materials within the right foramen in right-sided approach while preserving the right lateral portion of end plate and uncinate process, because the upper part of the right uncinated process interfered within the operative view.
Therefore, we usually used the keyhole transuncal approach in right foraminal stenosis causing radiculopathy, as well as usual transdiscal approach.
From January 2011 to December 2016, 23 patients with the right foraminal stenosis were treated with right keyhole transuncal foraminotomy with cage fixation. In this report, the efficacy of this method was investigated to evaluate pre- and post-operative radiographic data, visual analog score (VAS) and Japanese orthopaedic association (JOA) score.
Patients and Methods
We reviewed our hospital records of all patients of cervical spondylosis with right foraminal stenosis treated with keyhole transuncal foraminotomy with cage fixation between January 2011 and December 2016. From their hospital records, we extracted clinical and radiographic data, computed tomographic (CT) scans, and magnetic resonance imaging (MRI). In our institution, among 175 cases of cervical spondylosis which was operated by one senior neurosurgeon, anterior microdiscectomy and fixation was done in 116 cases (66.6%). Among 116 patients, microdiscectomy and fixation with the right keyhole transuncal foraminotomy were performed in 23 cases (19.8%) and the right keyhole transuncal foraminotomy without cage fixation was done in 3 cases. All of the above 23 cases had not only right fomaminal stenosis but also central canal stenosis due to disc herniation and/or osteophytes at the same level. The VAS score of the 23 cases, preoperatively, at discharge, and 1 month after discharge, were researched with questionnaire postoperatively. The JOA score was assessed preoperatively and at discharge by physiotherapists. All of the 23 patients were followed up more than 1 year.
Radiological evaluation
For all patients, static and dynamic radiographs, CT scans, and MRI were obtained preoperatively and postoperatively. Follow-up static and dynamic radiographs of the cervical spine were subsequently taken to assess the following measurements through the outpatient clinic: the C2–7 sagittal Cobb angle (C2–7 CA) at neutral, anterior and posterior flexion, C2–7 sagittal vertical axis (C2–7 SVA), T1 slope, cranial tilting, cervical tilting, and vertebral and disc height of upper and lower adjacent segments to the treated level (Table 1).
Table 1.
The characteristics of the patients and pre- and postoperative radiographic results
| (a) Patient population (n = 23) | |
|---|---|
| Age (years) | 54 (36–74) |
| Sex (male:female) | 16:7 |
| Average follow up (months) | 39.3 (12–91) |
| Number of patients | |
| Responsible levels | |
| C4/5 | 3 |
| C5/6 | 15 |
| C6/7 | 5 |
| Factor of foraminal stenosis | |
| Disc herniation | 5 |
| Spur | 3 |
| Both | 15 |
| (b) Radiographic results | |||
|---|---|---|---|
|
| |||
| Preoperative (mean ± SD) | Final follow-up (mean ± SD) | P-value | |
| C2–7 Cobb angle (CA) (°) | |||
| Neutral | 11.6 ± 9.9 | 13.4 ± 8.8 | 0.42 |
| Anterior flexion | 18.5 ± 8.7 | 14.8 ± 11.6 | 0.17 |
| Posterior flexion | 25.2 ± 13.5 | 27.6 ± 15.6 | 0.53 |
| C2–7 SVA (mm) | 22.1 ± 10.3 | 19.8 ± 8.3 | 0.3 |
| T1 slope (°) | 22.9 ± 9.3 | 24.5 ± 8.4 | 0.47 |
| Cranial tilting (°) | 18.5 ± 5.6 | 18.2 ± 7.0 | 0.86 |
| Cervical tilting (°) | 13.8 ± 6.3 | 16.5 ± 7.6 | 0.12 |
| Vertebral body height (mm) | |||
| Upper | 13.2 ± 1.3 | 13.0 ± 1.2 | 0.48 |
| Lower | 13.6 ± 1.7 | 13.2 ± 1.7 | 0.3 |
| Disc height (mm) | |||
| Upper | 6.6 ± 0.8 | 6.5 ± 0.8 | 0.76 |
| Lower | 6.5 ± 1.0 | 6.4 ± 1.1 | 0.74 |
Cervical parameters, vertebral, and disc height
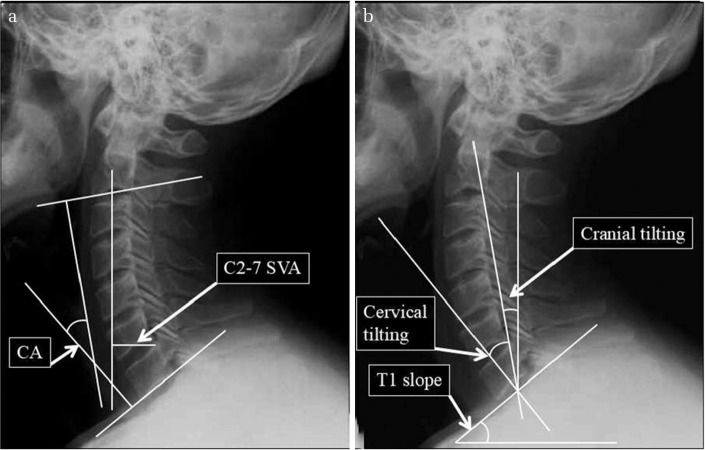
C2–7 sagittal Cobb angle (CA): the CA between the lower endplates of C2 and C7 (Fig. 1a).
Fig. 1.
Measurements of radiological parameters (a) C2–7 sagittal Cobb angle (CA), C2–7 sagittal vertical axis (C2–7 SVA). (b) T1 slope, cervical tilting, cranial tilting.
C2–7 sagittal vertical axis (C2–7 SVA): the distance from the posterosuperior corner of C7 to a vertical line from the center of the C2 vertebra (Fig. 1a).
T1 slope: the angle between the upper endplate of T1 (T1UEP) and the horizontal line (Fig. 1b).
Cervical tilting: an angle formed between the vertical line from the center of T1UEP and the line from the center of C2 vertebra (Fig. 1b).
Cranial tilting: an angle formed between the line from the center of the T1UEP to the dens and the SVA from the T1UEP (Fig. 1b).
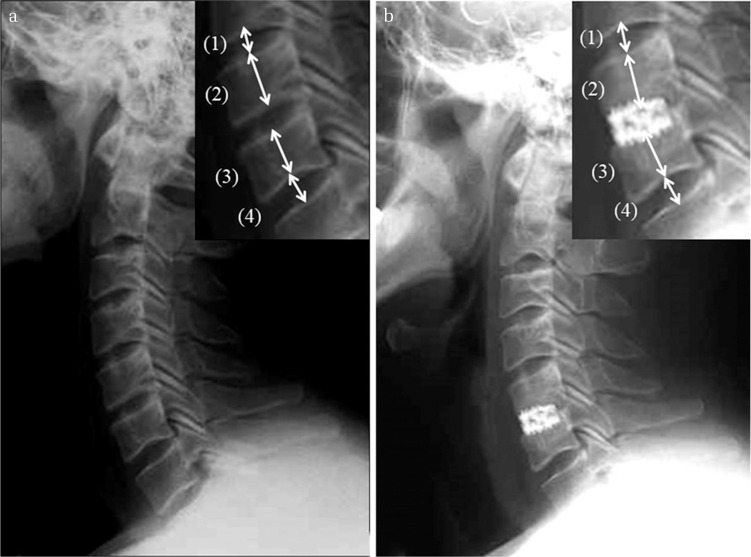
Disc heights were measured at the highest position and vertebral body heights were measured at the same position and postoperative heights were measured at the same position (Fig. 2).
Fig. 2.
Measurements of vertebral and disc heights. (a) preoperative image (b) postoperative image. (1) Disc height of upper adjacent segment to the treated level (2) Vertebral height of upper adjacent segment (3) Vertebral height of lower adjacent segment (4) Disc height of lower adjacent segment.
Statistical analysis
Statistical significance was calculated by the Stat-View 5.0 software (SAS Institute Inc., Cary, NC, USA). All data were presented as the mean ± SD. To compare the difference between two samples, we used Student’s t-tests; values of P < 0.05 were considered statistically significant.
Operative methods
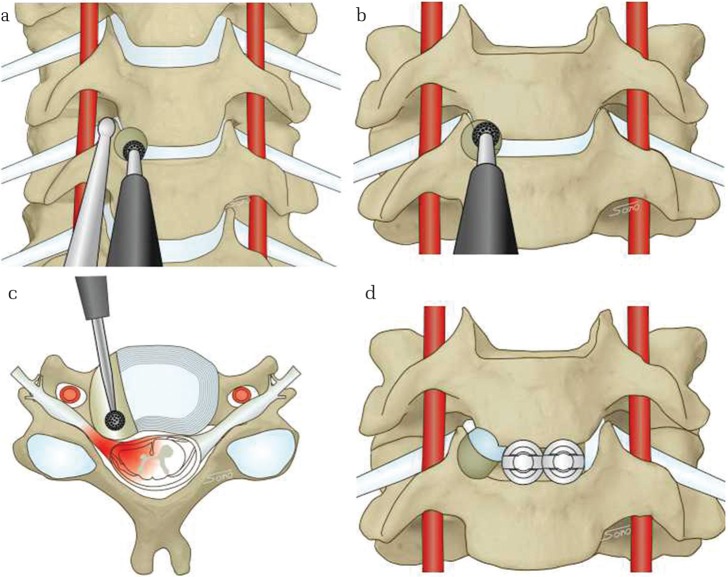
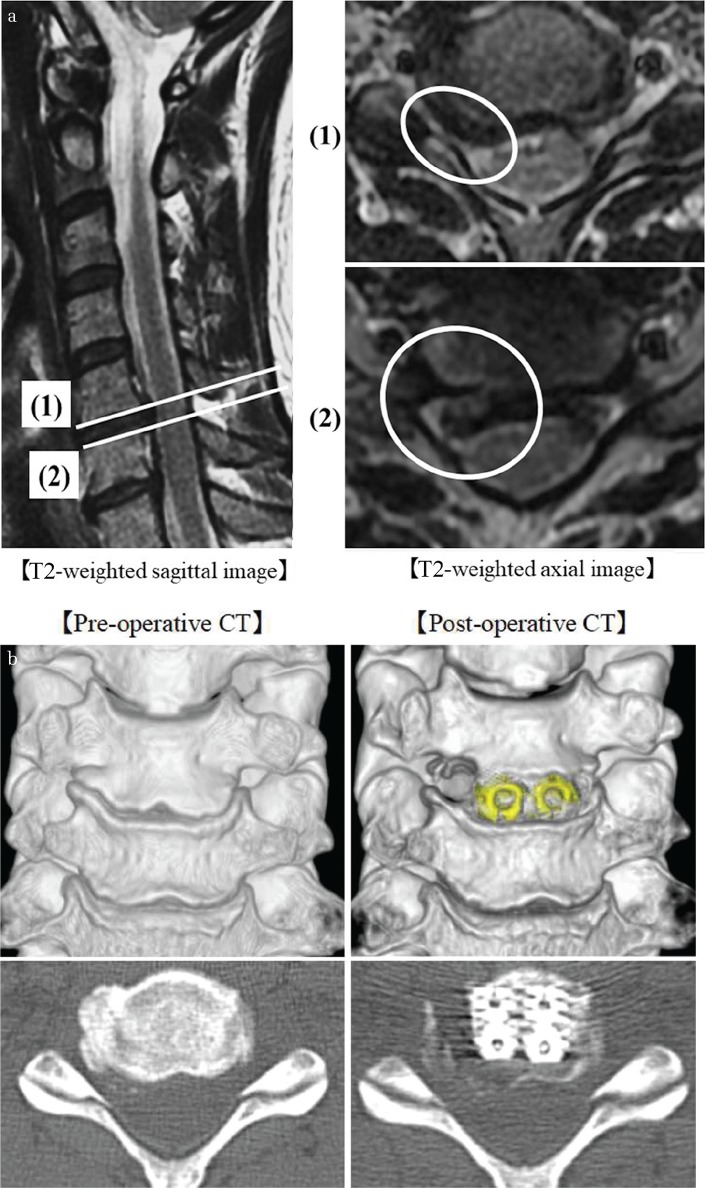
The approach was the same as the standard anterior microdiscectomy and fixation in all cases, and we approached from the right side. After a 3 cm transverse skin incision, the anterior aspect of responsible disc space and the upper and lower vertebral bodies were exposed and the level was confirmed with lateral fluoroscope. A small amount of dye was inserted into the disc space through a needle for further identification. The schema was shown in Fig. 3. At first, the medial portion of the longus colli muscle was slightly detached and the lateral corner of the right uncinate process was exposed with a curet inserted to the lateral portion of the uncinate process (Fig. 3a). The uncinate process was then carefully drilled out with a 3 mm diamond drill while preserving the lateral side of the process for the purpose of protecting the vertebral artery (VA) (Fig. 3b). The direction of the drill was slightly medial and the size of a keyhole was usually 7 mm in diameter and the lateral sides of uncinate process was preserved (Fig. 3c). The keyhole was formed as there was a dyed disc in the center. After the herniated disc materials and spurs nearby the foramen were carefully removed with a curet and dissector, the foramen became widened and the root was seen with no compression. Next, usual microdiscectomy and osteophytectomy were performed through transdiscal approach. The end plate of upper and lower vertebrae was not drilled out to prevent subsidence of cylindrical titanium cages (Ammtec, Tokyo, Japan) although posterior spurs were drilled out. The cylindrical titanium cages were inserted in the inter-locking fashion (Fig. 3d). A typical case was shown in Fig. 4. A 46-year-old woman presented with weakness and numbness in right arm and hand 2 months before. T2-weighted images disclosed severe foraminal stenosis due to osteophyte and disc herniation at C5/6 on right (Fig. 4a) and CT also showed foraminal stenosis at C5/6 on right and postoperative CT showed the drilled out foramen on right and cage fixation in the inter-locking fashion (Fig. 4b).
Fig. 3.
Schema of transuncal foraminotomy and cage fixation. (a) The lateral corner of right uncinate process was exposed with a curet inserted to the lateral portion of the uncinate process. (b) The uncinate process was then carefully drilled out with a 3 mm diamond drill while preserving the lateral side of the process for the purpose of protecting the VA. (c) The direction of the drill was slightly medial and the size of a keyhole was usually 7 mm in diameter and the lateral sides of uncinate process was preserved. (d) The cylindrical titanium cages were inserted in the inter-locking fashion.
Fig. 4.
Representative case images. (a) Pre-operative MR T2-weighted image. (1) Axial T2-weighted image at the inferior border of C5 body disclosed severe foraminal stenosis due to osteophyte and disc herniation on right. (2) Axial T2-weighted image at the superior border of C6 body disclosed disc herniation dominantly on right. (b) Pre- and postoperative 3D-CT and axial images.
Results
Microdiscectomy, cage fixation, and right keyhole transuncal foraminotomy were performed in 23 patients. The characteristics were shown in Table 1. The average age of patients was 54 years (range 36–75), 69.6% (16/23) were man. The average of interval from onset was 3.5 months (range 1–18).
All patients had central canal stenosis due to disc herniation and/or osteophytes and presented with radiculopathy and 65.2% (15/23) showed radiculo-myelopathy. All patients presented radicular pain, and 6 with arm pain, 13 with scapular pain, and 4 with arm and scapular pain. The responsible level was C4/5 in 3, C5/6 in 15, and C6/7 in 5. The factor of foraminal stenosis was disc alone in 5, spur alone in 3, and both in 15. The operative complications were not seen in all patients. As shown in Fig. 5, preoperative VAS score (average 7.6 ± 2.2) was significantly improved at discharge (average 2.8 ± 2.2) and at 1 month after discharge (average 1.1 ± 1.6). Radicular pain was completely disappeared in 34.8% (8/23) at discharge and in 60.9% (14/23) at 1 month after discharge. At 1 month after discharge, radicular pain was improved in all patients, but VAS score remained 2 in 21.7% (5/23) and 4 in 17.4% (4/23) at 1 month after discharge. Good recovery rate at 1 month after discharge was 82.6% (19/23, VAS score: 0–2).
Fig. 5.
The average of visual analog score (VAS) scores at preoperative phase, discharge and 1 month after surgery of the 23 cases. The error bars showed SD and lines showed the changes in each patient. In all cases, VAS score was improved and radicular pain was completely disappeared in 34.8% (8/23) at discharge and in 60.9% (14/23) at 1 month after discharge. At 1 month after discharge, VAS score remained 2 in 21.7% (5/23) and 4 in 17.4% (4/23).
Preoperative JOA score in patients with myelopathy (n = 15 cases, average 15.3 ± 1.1) was improved at discharge (average 16.6 ± 0.4) and 93.3% (14/15) showed the recovery of the score. All patients were followed up and presented with no recurrence of radiculopathy (average follow up period, 39.3 months, median period, 32 months respectively). The X-ray and CT scan were performed in all patients at 1 year after operation and bone fusion at the 1 year after operation was acquired in 91.3% (21/23).
As shown in Table 1, the C2–7 CA at neutral, anterior and posterior flexion changed from 11.6 ± 9.9°, 18.5 ± 8.7°, 25.2 ± 13.5° preoperatively to 13.4 ± 8.8°, 14.8 ± 11.6°, 27.6 ± 15.6° at final follow–up. The C2–7 SVA changed from 22.1 ± 10.3 mm preoperatively to 19.8 ± 8.3 mm at final follow-up. T1 slope changed from 22.9 ± 9.3° preoperatively to 24.5 ± 8.4°. Cranial tilting and cervical tilting changed at 18.5 ± 5.6°, 13.8 ± 6.3° preoperatively to 24.5 ± 8.4°, 16.5 ± 7.6° at final follow-up. There were no statistical differences in all data between preoperative and final follow-up period. Moreover, the vertebral height of the upper and lower adjacent segment decreased from 13.2 ± 1.3 mm, 13.6 ± 1.7 mm preoperatively to 13.0 ± 1.2 mm, 13.2 ± 1.7 mm at final follow-up. The disc height of the upper and lower adjacent segment decreased from 6.6 ± 0.8 mm, 6.5 ± 1.0 mm to 6.5 ± 0.8 mm, 6.4 ± 1.1 mm. There were also no significant differences in vertebral and disc height of the upper and lower adjacent segment.
Discussion
The surgery for cervical spondylosis and discogenic disease is generally divided into two approaches; the posterior and the anterior approach. While the various methods of the posterior approach were established since 1934,6) Robinson and Smith7) in 1955 and Cloward8) in 1958 pioneered the anterior cervical discectomy with bone fusion to accomplish direct decompression of the compressive spondylotic spur and disc fragment.
In 1976, Hakuba1) introduced the transuncodiscal approach, which is a combined anterior and lateral approach to cervical discs. In addition to resecting the uncovertebral joint, the entire disc was removed including the ipsilateral posterior osteophyte and the contralateral uncinated process. Snyder and Bernhardt,9) in 1989, reported an anterior cervical fractional interspace decompression for the treatment of cervical radiculopathy. Decompression was performed with a high-speed 5 mm burr in the lateral one-third of the intervertebral disc and limited to a 3 mm radius around the nerve root. Jho,3) in 1996, described the modified approach, which is completely exposing the vertebral artery when the entire uncinate process is removed. Lee,4) in 2006, described small keyhole transuncal foraminotomy for unilateral cervical radiculopathy with preservation of the intervertebral disc. The drilling was gently inclined medially about 10–20° and somewhat cranially parallel to the intervertebral space. Our method is greatly different from Jho’s and Lee’s method at the point of drilling and preserving the lateral side of the uncinate process and in addition, VA is not exposed. We slightly separate the longus colli muscle and start drilling at the center of the uncinate process and proceed to its base for complete foraminotomy through a keyhole usually 7 mm in diameter.
Several authors reported the efficacy of the various anterior foraminotomy, but Matz reviewed the indications and utility of anterior cervical nerve root decompression.5) The success rates were 52–99% but recurrent symptoms were as high as 30%. On the other hands, the efficacy of posterior cervical foraminotomy for cervical radiculopathy was reported and McAnany et al.10) reviewed that there was no significant difference in the pooled outcome between a traditional open or a minimally-invasive foraminotomy using a tubular retractor. The pooled clinical success rate was 92.7% for open foraminotomy and 94.9% for minimally-invasive foraminotomy.
In our cases, there were no significant differences between preoperative and postoperative radiographic data in all parameters (Table 1). Disc and vertebral height at upper and lower adjacent segment was tended to be slightly decreased, but there were no significant differences between preoperative and postoperative state (the average of follow up period; 18.8 ± 9.7 months). We could not assess the long-term follow up, but we think that deleting a part of uncinate process does not affect the change in alignment.
In our practice, right transuncal foraminotomy without cage fixation was performed in 3 cases. In all the 3 cases, the responsible level was C6/7 and the factor of foraminal stenosis was only disc. They showed the right foraminal stenosis but no central canal stenosis and no recurrence. We routinely use the right-sided anterior approach for cervical spondylosis and choice microdiscectomy, cage fixation and the right keyhole transuncal foraminotomy for the patients with right foraminal and central canal stenosis due to disc herniation and/or osteophytes with right radiculopathy. The reason why we perform cage fixation is that we try to avoid the recurrence of the symptom and decompression of the cord at the level. Although cage fixation will cause loss of a motion segment movement and disc degeneration and spondylotic changes at adjacent intervertebral levels,11) we believe that fixation will prevent the recurrence of the radiculopathy. In our series, this manner was performed in 8 patients without myelopathy because they had canal stenosis. Foraminotomy alone was performed in 3 patients because they had no canal stenosis. We could not prove whether microdiscectomy and fixation should be done in the patients with no canal stenosis because our cases were very small. All of the 3 patients treated with foraminotomy alone and the 23 patients treated with this manner had no recurrence of the radiculopathy at the treated level and no additional surgery at the other levels of cervical spine (follow up time; 76, 19, 12 months, average of follow up time; 38 months, respectively).
Various methods of anterior foraminotomy and transcorpereal anterior cervical foraminotomy were reported.2–4,12–21) More recently, anterior transcorporeal procedure using CT-based intraoperative spinal navigation and percutaneous endoscopy were reported.20,21) Transcorporeal approach has some advantage. The endplates are preserved and the degenerative changes at the adjacent segment are lower than microdiscectomy and fusion. Compared to our methods, uncinate process is completely preserved. Conversely, it has some problems. The complications reported spinal cord or nerve root injury and cerebrospinal fluid leakage, insufficient decompression, and instability, fracture and kyphotic changes.12–15) Anterior transcorporeal procedures seem to require high anatomical understanding and surgical skill and we believe that our method is simple and has a lower risk of vertebral artery injury. We also choose the right approach for the patients with left radiculopathy due to the left foraminal stenosis because we can easily drill out left side of osteophyte and remove disc materials for sufficient decompression of the left foramen. Therefore, usual microdisectomy and fixation was chosen for the patients with myelopathy and left radiculopathy due to the left foraminal stenosis. Usual microdisectomy and fixation through left-sided anterior approach might be an option for the patient with both of right radiculopathy and myelopathy, but we think that the manner has some problems. First, the operative view is unusual. Second, right-handed surgeons have not easy access in using a drill in left-sided approach although skillful operator may not mind. The reason is that a drill must be headed from the caudal side to the cranial side and it is difficult to look at the tip of a drill. Therefore, we believe that our approach is a reasonable and effective method and may be one option because we could get the same operative view as usual anterior microdiscectomy via right-sided anterior approach.
In our cases, there were no patients who showed left radiculopathy due to left foraminal stenosis with no canal stenosis. We think that it is debatable to choose whether left foraminotomy alone from right-or left-sided anterior approach with or without fixation, or posterior foraminotomy alone. As shown above, posterior foraminotomy may be less invasive than our method. It is controversial that whether posterior foraminotmy is superior to anterior foraminotomy as same as whether posterior approach is superior to anterior approach for cervical myelopathy and our method could be one option for right cervical radiculopathy.
Conclusions
We reported reasonable results in the patients treated with microdiscectomy, cage fixation and right keyhole transuncal foraminotomy for right foraminal and central canal stenosis via right anterior approach. This method is safe and useful for the patient who shows right foraminal and canal stenosis.
Footnotes
Conflicts of Interest Disclosure
No potential conflicts of interest were disclosed.
References
- 1).Hakuba A: Trans-unco-discal approach. A combined anterior and lateral approach to cervical discs. J Neurosurg 45: 284–291, 1976 [DOI] [PubMed] [Google Scholar]
- 2).Grundy PL, Germon TJ, Gill SS: Transpedicular approaches to cervical uncovertebral osteophytes causing radiculopathy. J Neurosurg 93: 21–27, 2000 [DOI] [PubMed] [Google Scholar]
- 3).Jho HD: Microsurgical anterior cervical foraminotomy for radiculopathy: a new approach to cervical disc herniation. J Neurosurg 84: 155–160, 1996 [DOI] [PubMed] [Google Scholar]
- 4).Lee JY, Löhr M, Impekoven P, et al. : Small keyhole transuncal foraminotomy for unilateral cervical radiculopathy. Acta Neurochir (Wien) 148: 951–958, 2006 [DOI] [PubMed] [Google Scholar]
- 5).Matz PG, Holly LT, Groff MW, et al. Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and Congress of Neurological Surgeons : Indications for anterior cervical decompression for the treatment of cervical degenerative radiculopathy. J Neurosurg Spine 11: 174–182, 2009 [DOI] [PubMed] [Google Scholar]
- 6).Mixter WJ, Barr JS: Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med 211: 210–215, 1934 [Google Scholar]
- 7).Robinson RA, Smith GW: Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp 96: 223–224, 1955 [Google Scholar]
- 8).Cloward RB: The anterior approach for removal of ruptured cervical disks. J Neurosurg 15: 602–617, 1958 [DOI] [PubMed] [Google Scholar]
- 9).Snyder GM, Bernhardt M: Anterior cervical fractional interspace decompression for treatment of cervical radiculopathy. A review of the first 66 cases. Clin Orthop Relat Res 246: 92–99, 1989 [PubMed] [Google Scholar]
- 10).McAnany SJ, Kim JS, Overley SC, Baird EO, Anderson PA, Qureshi SA: A meta-analysis of cervical foraminotomy: open versus minimally-invasive techniques. Spine J 15: 849–856, 2015 [DOI] [PubMed] [Google Scholar]
- 11).Pospiech J, Stolke D, Wilke HJ, Claes LE: Intradiscal pressure recordings in the cervical spine. Neurosurgery 44: 379–384; discussion 384–385, 1999 [DOI] [PubMed] [Google Scholar]
- 12).Choi G, Lee SH, Bhanot A, Chae YS, Jung B, Lee S: Modified transcorporeal anterior cervical microforaminotomy for cervical radiculopathy: a technical note and early results. Eur Spine J 16: 1387–1393, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Choi G, Arbatti NJ, Modi HN, et al. : Transcorporeal tunnel approach for unilateral cervical radiculopathy: a 2-year follow-up review and results. Minim Invasive Neurosurg 53: 127–131, 2010 [DOI] [PubMed] [Google Scholar]
- 14).Choi KC, Ahn Y, Lee CD, Lee SH: Combined anterior approach with transcorporeal herniotomy for a huge migrated cervical disc herniation. Korean J Spine 8: 292–294, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Hong WJ, Kim WK, Park CW, et al. : Comparison between transuncal approach and upper vertebral transcorporeal approach for unilateral cervical radiculopathy - a preliminary report. Minim Invasive Neurosurg 49: 296–301, 2006 [DOI] [PubMed] [Google Scholar]
- 16).Kim JS, Eun SS, Prada N, Choi G, Lee SH: Modified transcorporeal anterior cervical microforaminotomy assisted by O-arm-based navigation: a technical case report. Eur Spine J 20 (Suppl 2): S147–S152, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Kim MH: Clinical and radiological long-term outcomes of anterior microforaminotomy for cervical degenerative disease. Spine 38: 1812–1819, 2013 [DOI] [PubMed] [Google Scholar]
- 18).Sakai T, Katoh S, Sairyo K, et al. : Anterior transvertebral herniotomy for cervical disc herniation: a long-term follow-up study. J Spinal Disord Tech 22: 408–412, 2009 [DOI] [PubMed] [Google Scholar]
- 19).Yamamoto Y, Hara M, Nishimura Y, Haimoto S, Wakabayashi T: Hybrid method of transvertebral foraminotomy combined with anterior cervical decompression and fusion for multilevel cervical disease. Neurol Med Chir (Tokyo) 58: 124–131, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Quillo-Olvera J, Lin GX, Suen TK, Jo HJ, Kim JS: Anterior transcorporeal tunnel approach for cervical myelopathy guided by CT-based intraoperative spinal navigation: technical note. J Clin Neurosci 48: 218–223, 2018 [DOI] [PubMed] [Google Scholar]
- 21).Du Q, Wang X, Qin JP, et al. : Percutaneous full-endoscopic anterior transcorporeal procedure for cervical disc herniation: a novel procedure and early follow-up study. World Neurosurg 112: e23–e30, 2018 [DOI] [PubMed] [Google Scholar]