Abstract
Cervical cancer is a serious malignancy that affects the health of females. In the present study, the association between breast cancer type 1 susceptibility protein/breast cancer type 2 susceptibility protein-containing complex subunit 3 (BRCC3) and cervical cancer was investigated. Reverse transcription-quantitative polymerase chain reaction and western blotting were performed to determine BRCC3 mRNA and protein expression levels in cervical cancer tissues and cells, in addition to the expression levels of proteins associated with the epithelial-mesenchymal transition (EMT) process in HeLa and SiHa cells. Cell Counting Kit-8, Transwell and wound healing assays were performed to determine the cell viability, invasion and migration abilities of cervical cancer cells, respectively. The results of the present study revealed that BRCC3 expression was significantly increased in cervical cancer tissues, which was also revealed to be associated with the clinical stages and pathological grades of cervical cancer exhibited by patients, in addition to the survival time. Furthermore, BRCC3 expression levels were enhanced in HeLa, SiHa and C-33A cervical cancer cells. BRCC3 interference in HeLa and SiHa cells was revealed to suppress cell viability, invasion and migration abilities via upregulation of E-cadherin expression levels and downregulation of Vimentin, matrix metalloproteinase (MMP)-2, MMP-9, snail family transcriptional repressor (Snai)1 and Snai2 expression levels. In conclusion, the expression levels of BRCC3 were revealed to be increased in cervical cancer tissues, which were positively associated with clinical features of cervical cancer. Furthermore, BRCC3 interference inhibited the cell viability, invasion and migration abilities of HeLa and SiHa cells via regulation of EMT progression and expression levels of Snai family members. In addition, the results of the present study suggested that BRCC3 represents an oncogene associated with cervical cancer, and may also represent a novel therapeutic biomarker for the diagnosis, treatment and prognosis of patients with cervical cancer.
Keywords: breast cancer type 1 susceptibility protein/breast cancer type 2 susceptibility protein-containing complex subunit 3, cell invasion, migration, cervical cancer, epithelial-mesenchymal transition, snail family transcriptional repressor
Introduction
Cervical cancer is one of the most common malignant tumors diagnosed among females worldwide (1). Furthermore, cervical cancer has a high incidence rate and exhibits the second highest mortality rate associated with cancer in women (2,3). Thus, cervical cancer seriously affects the health of women (4,5). Furthermore, ~470,000 novel cases occur each year worldwide, resulting in 233,000 patients with cervical cancer succumbing to the disease annually (6). A previous study revealed that >85% of patients with cervical cancer live in developing countries (7).
Human papillomavirus (HPV) infection is one of the leading causes of cervical cancer and is associated with a majority of cervical cancer cases (8,9). The primary causes of mortality associated with cervical cancer are unsuccessful surgical treatment, tumor recurrence and metastasis (10). The first step in metastasis is localized invasion, which involves numerous phenotypic changes in the primary tumor (11,12). Malignant epithelial-mesenchymal transition (EMT) is an important factor leading to the development of distant tumor metastases (13,14). The multilayered cell structure of normal epithelial tissue does not contribute to the movement and invasion of malignant cells (15), and thus to develop the capability of movement and invasion, tumor cells lose epithelial phenotypes, leading to EMT progression (16). Cellular gene expression profiles are also altered in tumor cells: The expression levels of marker proteins, including E-cadherin, of epithelial cells are downregulated; whereas, the expression of markers, including vimentin, of mesenchymal cells are upregulated (17,18). Interactions among epithelial cells disappear. Cells exhibit a more mesenchymal phenotype, causing them to exhibit stronger motor abilities in order to induce local infiltration and invasion of tumor cells into the blood vessels and lymph vessels, in addition to subsequent transfer to distant target organs (19,20). The zinc-finger transcription Snai protein family regulates chromatin, which may induce the progression of EMT in cancer cells and promote cancer progression and metastasis (21).
Breast cancer type 1 susceptibility protein/breast cancer type 2 susceptibility protein-containing complex subunit 3 (BRCC3) is an E3 ubiquitin ligase (22). BRCC3 is associated with G2/M arrest in breast cancer cells and DNA damage (23). The expression of BRCC3 is associated with increased cell proliferation (24). Previous studies have also revealed that BRCC3 is associated with nasopharyngeal carcinoma and ovarian cancer (25,26). A further study demonstrated that suppression of BRCC3 may render glioma cells more sensitive to chemotherapy treatment (27). However, whether BRCC3 has an effect on cervical cancer remains unknown. The aim of the present study was to investigate the association between BRCC3 and clinical features of cervical cancer, in addition to determining the underlying molecular mechanism, particularly in association with EMT. The results of the present study revealed that BRCC3 represented a novel biomarker associated with cervical cancer, which may further develop therapeutic applications for the treatment of cervical cancer.
Materials and methods
Patients and tissues
Human cervical cancer tissue samples were obtained from 46 patients with cervical cancer between August 2016 and August 2017 in Jinhua Municipal Central Hospital, Jinhua Hospital of Zhejiang University (Jinhua, China). According to the International Federation of Gynecology and Obstetrics (FIGO) criteria (28,29), 17 patients were suffering from stage I/II cervical cancer, and the remaining 29 patients were suffering from stage III/IV cervical cancer. Normal control tissues were separated from corresponding adjacent cancerous tissues. No radiotherapy or chemotherapy was performed prior to sample collection. In addition, patients were divided into two groups relative to the median values of BRCC3 expression levels, according to previously published criteria (30). Obtained tissues were frozen and preserved in liquid nitrogen, and subsequently prepared for reverse transcription-quantitative polymerase chain reaction (RT-qPCR) and western blot analyses. Written informed consent was obtained from all patients, and the present study was approved by the ethics committee of Jinhua Municipal Central Hospital, Jinhua Hospital of Zhejiang University (Jinhua, China).
Cell culture
Human cervical cancer cells, including HeLa (HPV-18+ cells), SiHa (HPV-16+ cells) and C-33A cells (HPV− cells), were purchased from the American Type Culture Collection (Manassas, VA, USA). Human cervical epithelial cells (HcerEpic; cat. no. BNCC340374) were purchased from the BeNa Culture Collection (Kunshan, China). All cells were cultured in high glucose Dulbecco's modified Eagle's medium (DMEM; Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA) containing 10% fetal bovine serum (FBS; Gibco; Thermo Fisher Scientific, Inc.) and 100 ng/ml penicillin/streptomycin (Invitrogen; Thermo Fisher Scientific, Inc.) in humidified air with 5% CO2 at 37°C. Once cells reached the logarithmic phase, they were subjected to subsequent RT-qPCR and western blot analyses to determine the expression levels of BRCC3 in the aforementioned cell lines.
Cell transfection
HeLa and SiHa cells were plated in 6-well plates (1×105 cells/well) and incubated in complete DMEM in the absence of antibiotics at 37°C for 24 h. Following this, for the small interfering (si)BRCC group, cells were transfected with BRCC3 siRNA (200 nM; Shanghai GenePharma Co., Ltd., Shanghai, China) using Lipofectamine® 2000 (Invitrogen; Thermo Fisher Scientific, Inc.) in DMEM in the absence of FBS. The BRCC3 siRNA sequence was: 5′-GUACUGGGUUUGUUACAGAUU-3′. Cells transfected with a scrambled siRNA and untreated cells were considered to represent negative control (NC) and control groups, respectively. The scrambled siRNA sequence was: 5′-UCACUGCGCUCGAUGCAGUTT-3′. Following this, cells were cultured in complete DMEM with FBS and 100 ng/ml penicillin/streptomycin for 24 h for subsequent analysis. The efficiency of cell transfection was investigated via determination of BRCC3 expression levels using RT-qPCR and western blot analyses.
Cell Counting Kit-8 (CCK-8) assay
A CCK-8 assay (Beyotime Institute of Biotechnology, Haimen, China) was used to investigate the effect of BRCC3 on the viability of HeLa and SiHa cells. Cells were seeded in three independent 96-well plates (5×103 cells/well) and incubated for 12, 24 and 48 h time intervals at 37°C. Following this, CCK-8 reagent (20 µl) was added into each well and the plates were subsequently incubated for 1 h at 37°C. Optical density values at 450 nm were detected using a microplate reader (BioTek Instruments, Inc., Winooski, VT, USA).
Transwell assay
Transwell assays were performed to investigate the function of BRCC3 on the invasive abilities of HeLa and SiHa cells. Cells from the siBRCC3, NC and control groups were suspended in complete DMEM without FBS (1×106 cells/ml) and subsequently transferred into the upper chambers of 24-well plates coated with Matrigel (BD Biosciences, Franklin Lakes, NJ, USA). Lower chambers were filled with complete DMEM and 10% FBS. Following incubation for 48 h at 37°C, invaded cells were stained with 0.1% crystal violet for 30 min at 37°C and cell numbers were counted under a light microscope (Leica Microsystems GmbH, Wetzlar, Germany) in five randomly selected high-power fields, with 100× magnification.
Wound healing assay
Wound healing assays were performed to investigate the effect of BRCC3 on the migration abilities of HeLa and SiHa cells. Cells from the siBRCC3, NC and control groups were seeded in three independent 12-well plates (1×105 cells/well). Following being cultured overnight, the cell layer was scratched using a pipette tip. Cells were subsequently cultured in a humidified incubator at 37°C for 48 h. The width of the wounded area was measured using a light microscope (Leica Microsystems GmbH), at ×100 magnification.
RT-qPCR
RT-qPCR assays were performed to determine the mRNA expression levels of target genes and the 2−ΔΔCq method of quantification was employed (31). RT was performed using 1 µg RNA, which was extracted from different groups (Control, NC, siBRCC3) of HeLa and SiHa cells, using TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Inc.). An AMV reverse transcription system (Promega Corporation, Madison, WI, USA) was used to obtain cDNA templates, with 40°C for 60 min and 70°C for 5 min. The primers used for the determination of E-cadherin, Vimentin, matrix metalloproteinase (MMP)-2, MMP-9, snail family transcriptional repressor (Snai)1, Snai2, BRCC3 and β-actin expression levels were all purchased from Invitrogen (Thermo Fisher Scientific, Inc.), and the sequences of these primers are presented in Table I. β-actin was used as an internal control. qPCR amplification was performed using the following thermocycling conditions: Pre-denaturation at 95°C for 35 sec; followed by 40 cycles of denaturation at 95°C for 10 sec and annealing/extension at 60°C for 40 sec. A SYBR Green PCR Mix (Applied Biosystems; Thermo Fisher Scientific, Inc.) was used to perform qPCR, in addition to an ABI 7300 Thermocycler (Applied Biosystems; Thermo Fisher Scientific, Inc.). Relative mRNA levels were normalized against β-actin expression levels in each sample.
Table I.
Primer sequences used in the present study.
| Protein | Direction | Sequence (5′→3′) |
|---|---|---|
| β-actin | Forward | GTGGACATCCGCAAAGAC |
| Reverse | GAAAGGGTGTAACGCAACT | |
| E-cadherin | Forward | ACGCATTGCCACATACACTC |
| Reverse | GGTGTTCACATCATCGTCCG | |
| Vimentin | Forward | TGTTTCCAAGCCTGACCTCA |
| Reverse | CTCCGGTACTCAGTGGACTC | |
| MMP-2 | Forward | CAGCCCTGCAAGTTTCCATT |
| Reverse | GTTGCCCAGGAAAGTGAAGG | |
| MMP-9 | Forward | GAGACTCTACACCCAGGACG |
| Reverse | GAAAGTGAAGGGGAAGACGC | |
| Snai1 | Forward | TTACCTTCCAGCAGCCCTAC |
| Reverse | TCCCACTGTCCTCATCTGAC | |
| Snai2 | Forward | CTCCATCTGACACCTCCTCC |
| Reverse | TTTCTAGACTGGGCATCGCA | |
| BRCC3 | Forward | AACAGAGGCAGAGAGGTTGG |
| Reverse | AGCAAGTGTAGAGTACCCGG |
MMP, matrix metalloproteinase; BRCC3, BRCA1/BRCA2-containing complex subunit 3; Snai, snail family transcriptional repressor.
Western blotting
Western blotting was performed to determine the protein expression levels of RBCC3, EMT-associated proteins (E-cadherin, Vimentin, MMP-2 and MMP-9), as well as Snai1 and Snai2, in cervical cancer and normal tissues. Total protein was extracted using Total Proteins Extraction kit (Beijing Solarbio Science & Technology Co., Ltd., Beijing, China) and quantified using a bicinchoninic acid assay kit (Beyotime Institute of Biotechnology), according to the manufacturer's protocol. An ultra-microspectrophotometer (Nanodrop 2000; NanoDrop; Thermo Fisher Scientific, Inc., Wilmington, DE, USA) was used to further determine protein concentration. Following this, total protein (10 µg) was added to a 10% SDS-PAGE gel, separated and transferred onto polyvinylidene fluoride membranes. Following blocking with 5% skimmed dried milk for 1 h at room temperature, membranes were incubated with primary antibodies against the following proteins at 4°C overnight: BRCC36 (encoded by the BRCC3 gene in humans; cat. no. ab62075; 1:1,000; Abcam, Cambridge, UK), E-cadherin (cat. no. ab15148; 1:500; Abcam), Vimentin (cat. no. ab45939; 1:1,000; Abcam), MMP-2 (cat. no. ab92536; 1:1,000; Abcam), MMP-9 (cat. no. ab38898; 1:1,000; Abcam), Snai1 (cat. no. ab82846; 1:1,000; Abcam), Snai2 (cat. no. ab27568; 1:1,000; Abcam) and β-actin (cat. no. ab8227; 1:2,000; Abcam). Following this, membranes were incubated with goat anti-rabbit immunoglobulin G H&L HRP (1:5,000; ab205718 and ab6721; Abcam) at 37°C for 1 h. Following this, proteins were visualized using an enhanced chemiluminescence detection assay (GE Healthcare, Chicago, IL, USA). Relative protein quantities were normalized against β-actin expression levels in each sample. Densitometric analysis was performed using Quantity One software version 4.6.2 (Bio-Rad Laboratories).
Statistical analysis
Statistical analyses were performed using SPSS 22.0 (IBM Corp., Armonk, NY, USA). Each assay was independently replicated a minimum of three times. Data are presented as the mean ± standard deviation. A χ2 test was used to analyze non-continuous variables. To analyze continuous variables, the Student's t-test or one-way analysis of variance followed by Tukey's multiple comparisons test was performed to determine statistically significant differences. Kaplan-Meier assays were used to determine survival analysis. P<0.05 was considered to indicate a statistically significant difference.
Results
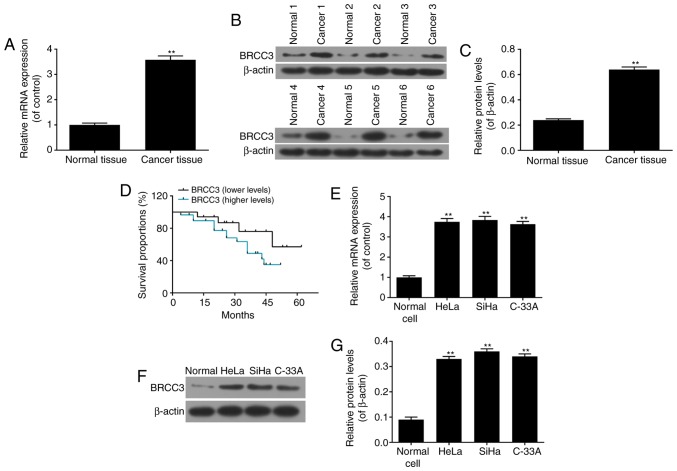
Expression levels of BRCC3 are upregulated in cervical cancer tissues and cells
To investigate the function of BRCC3 in cervical cancer, the mRNA and protein expression levels of BRCC3 in cervical cancer tissues were determined via RT-qPCR and western blot analyses, respectively. The results demonstrated that the mRNA and protein expression levels of BRCC3 significantly increased in cervical cancer tissues compared with normal cervical tissues (P<0.01; Fig. 1A-C). Representative western blotting images are presented in Fig. 1B. Presentations of clinical symptoms were analyzed, and the results revealed that increased levels of BRCC3 were significantly positively associated with advanced stages of cervical cancer as determined by the FIGO grading system, while the increased levels of BRCC3 were also related to the lower differentiated grades of cervical cancers, of highly malignant tumors (29,32; Table II). The results of survival analyses demonstrated that patients with cervical cancer and increased levels of BRCC3 exhibited a decreased survival time compared with patients with cervical cancer and decreased levels of BRCC3 (Fig. 1D). Continuous infection with HPV is the predominant factor resulting in the development of cervical cancer, particularly infection with HPV16 and HPV18. BRCC3 mRNA and protein expression levels were investigated in different cervical cancer cell lines, including HeLa (HPV-18+), SiHa (HPV-16+) and C-33A cells (HPV−). The results demonstrated that the mRNA and protein expression levels of BRCC3 were significantly increased in all cervical cancer cell lines compared with normal cervical cells; however, no statistically significant differences were observed between the cervical cancer cell lines (P<0.01; Fig. 1E-G).
Figure 1.
Expression levels of BRCC3 are significantly increased in cervical cancer tissues and cells. (A) mRNA expression levels of BRCC3 were investigated via RT-qPCR in cervical cancer tissues. Protein expression levels of BRCC3 were investigated via (B) western blotting and (C) quantification in cervical cancer tissues. (D) Survival analysis of patients with cervical cancer was performed via Kaplan-Meier analysis, and it was demonstrated that survival time was associated with BRCC3 expression levels. (E) mRNA expression levels of BRCC3 were investigated via RT-qPCR in HeLa, SiHa and C-33A cervical cancer cells in addition to HcerEpic normal cells. BRCC3 protein expression levels in HeLa, SiHa and C-33A cervical cancer cells in addition to HcerEpic normal cells were investigated by (F) western blotting and (G) quantification. **P<0.01 vs. respective normal control group. RT-qPCR, reverse transcription-quantitative polymerase chain reaction; BRCC3, breast cancer type 1 susceptibility protein/breast cancer type 2 susceptibility protein-containing complex subunit 3.
Table II.
Expression levels of BRCC3 are associated with clinical features of cervical carcinoma.
| BRCC3 expression levels, no. patients | |||
|---|---|---|---|
| Factors | Higher | Lower | P-value |
| Age, years | 0.978 | ||
| <50 | 13 | 7 | |
| ≥50 | 17 | 9 | |
| FIGO stages | 0.001a | ||
| I and II | 6 | 11 | |
| III and IV | 24 | 5 | |
| Histological grade | 0.005a | ||
| Well/moderately differentiated | 5 | 9 | |
| Poorly differentiated | 25 | 7 | |
P<0.05, as determined by the χ2 test. FIGO, International Federation of Gynecology and Obstetrics.
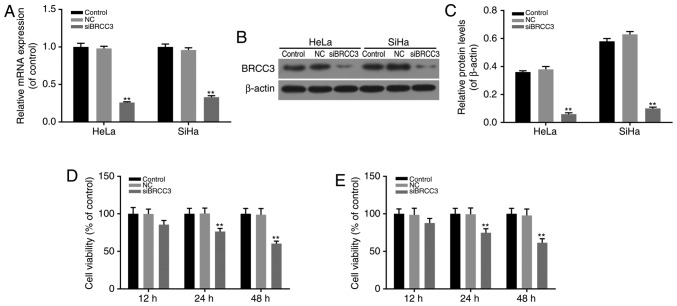
BRCC3 interference suppresses the viability of cervical cancer cells
HeLa and SiHa cells exhibiting high expression levels of BRCC3 and HPV-positive cells were chosen for the following study, for the high expression of BRCC3 and HPV 16 + or HPV 18 + infection. A BRCC3 interference model was established via transfection to investigate the function of BRCC3 in cervical cancer cells. The efficiency of transfection in HeLa and SiHa cells was investigated by determining the mRNA and protein expression levels of BRCC3, and it was revealed that the expression levels of BRCC3 were successfully suppressed in transfected cells compared with non-transfected NC cells (P<0.01; Fig. 2A-C). Following this, the viabilities of transfected cells were investigated using CCK-8 assays, and the results revealed that following transfection, the levels of cell viability exhibited by HeLa and SiHa cells were significantly suppressed in a time-dependent manner. Compared with NC cells, the cell viability of HeLa cells was markedly decreased to 85.7, 76.4 and 60.4% at 12, 24 and 48 h time intervals, respectively; whereas, the cell viability of SiHa cells was significantly decreased to 87.8, 74.8 and 61.5% at 12, 24 and 48 h time intervals, respectively (P<0.01; Fig. 2D and E).
Figure 2.
BRCC3 interference inhibits the cell viability of cervical cancer cells. (A) mRNA expression levels of BRCC3 were investigated via reverse transcription-quantitative polymerase chain reaction in HeLa and SiHa cervical cancer cells following BRCC3 interference. Protein expression levels of BRCC3 in HeLa and SiHa cervical cancer cells were investigated via (B) western blotting and (C) quantification. The cell viability of (D) HeLa and (E) SiHa cells following BRCC3 interference was investigated using a Cell Counting Kit-8 assay. **P<0.01 vs. respective NC group. BRCC3, breast cancer type 1 susceptibility protein/breast cancer type 2 susceptibility protein-containing complex subunit 3; si, small interfering; NC, negative control.
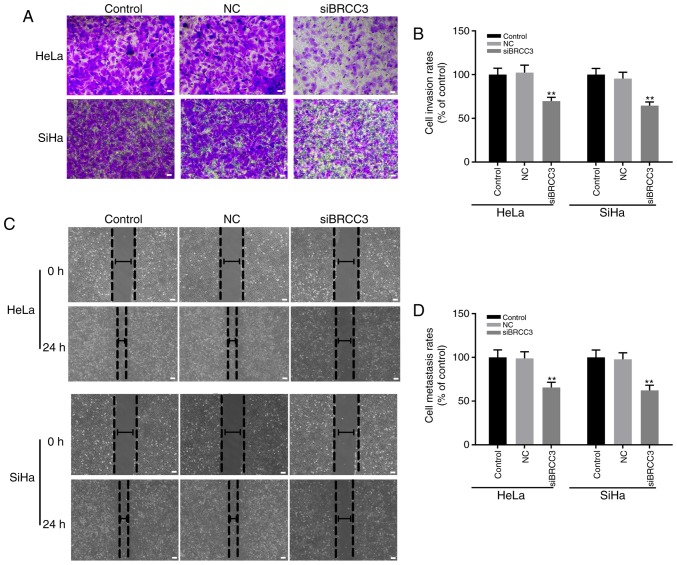
BRCC3 interference suppresses the invasion and migration abilities of cervical cancer cells
The effect of BRCC3 interference on the invasion and migration abilities of cervical cancer cells was investigated in the present study by performing wound healing and Transwell assays, respectively. The results demonstrated that compared with the NC group, the invasion rates exhibited by transfected HeLa and SiHa cells were significantly decreased compared with the NC group to 69.7 and 64.5%, respectively (Fig. 3A and B). Furthermore, the migration rates exhibited by transfected HeLa and SiHa cells were significantly decreased to 65.6 and 62.3% compared with the NC group, respectively (P<0.01; Fig. 3C and D). In addition, no statistically significant differences were exhibited between the invasion and migration rates of HeLa and SiHa cells (P>0.05; Fig. 3).
Figure 3.
BRCC3 interference suppresses the invasion and migration abilities of cervical cancer cells. The invasive abilities of HeLa and SiHa cells following BRCC3 interference were investigated via Transwell assays; (A) representative images and (B) quantification are presented. The migration abilities of HeLa and SiHa cells following BRCC3 interference were investigated via wound healing assays; (C) representative images and (D) quantification are presented. Scale bars, 50 µm. **P<0.01 vs. respective NC group. BRCC3, breast cancer type 1 susceptibility protein/breast cancer type 2 susceptibility protein-containing complex subunit 3; si, small interfering; NC, negative control.
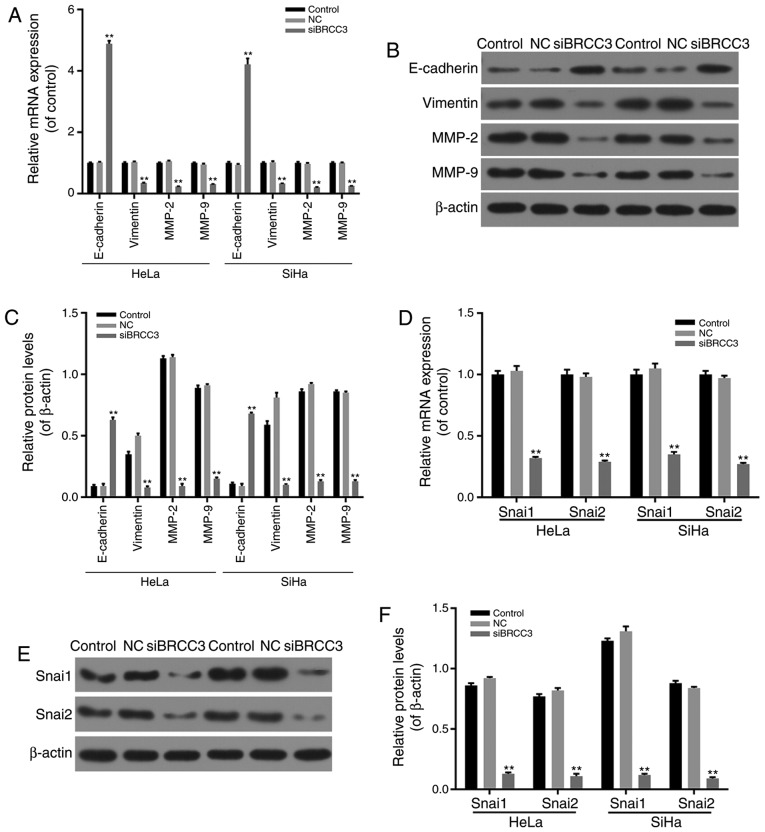
BRCC3 interference inhibits EMT progression and the Snai pathway in cervical cancer cells
To investigate the molecular mechanisms underlying the inhibitory effect of BRCC3 silencing on the invasion and migration abilities of cervical cancer cells, in addition to cell viability levels, the effect of siBRCC3 on the expression levels of EMT-associated factors was determined via RT-qPCR and western blotting. The results demonstrated that E-cadherin was significantly upregulated in transfected cells compared with the NC group, whereas the mRNA and protein expression levels of Vimentin, MMP-2 and MMP-9 were significantly downregulated in transfected HeLa and SiHa cells compared with the NC group (P<0.01; Fig. 4A-C). Therefore, the results suggested that BRCC3 interference inhibited cell migration and invasion abilities in cervical cancer cells via regulation of EMT-associated factors.
Figure 4.
BRCC3 interference suppresses EMT and the Snai pathway in cervical cancer cells. (A) mRNA expression levels of EMT-associated factors (E-cadherin, Vimentin, MMP-2 and MMP-9) were investigated via RT-qPCR in HeLa and SiHa cervical cancer cells following BRCC3 interference. Expression levels of proteins associated with EMT in HeLa and SiHa cervical cancer cells were investigated by (B) western blot analysis and (C) quantification. (D) mRNA expression levels of Snai1 and Snai2 were investigated by RT-qPCR in HeLa and SiHa cervical cancer cells following BRCC3 interference. Snai1 and Snai2 protein expression levels in HeLa and SiHa cervical cancer cells were investigated via (E) western blotting and (F) quantification. **P<0.01 vs. respective NC group. BRCC3, breast cancer type 1 susceptibility protein/breast cancer type 2 susceptibility protein-containing complex subunit 3; si, small interfering; RT-qPCR, reverse transcription-quantitative polymerase chain reaction; NC, negative control; EMT, epithelial-mesenchymal transition; Snai, snail family transcriptional repressor; MMP, matrix metalloproteinase.
In addition, the mRNA and protein expression levels of Snai1 and Snai2 in transfected HeLa and SiHa cells were investigated via RT-qPCR and western blotting analyses. The results revealed that mRNA and protein levels of Snai1 and Snai2 were significantly decreased in transfected cells compared with the NC group (P<0.01; Fig. 4D-F).
Discussion
Considering that cervical cancer represents a malignant tumor that has the second highest incidence rate among females, the disease has attracted much attention, and studies are continuously being performed to establish improved diagnosis and treatment strategies (33). Tumor recurrence and migration represent the principal factors associated with surgical failure (34). In the present study, a novel tumor oncogene, BRCC3, was investigated, in addition to its function and mechanism associated with the invasion and migration abilities of cervical cancer cells.
Clinical analyses of cervical cancer tissues and adjacent normal tissues, obtained from 46 patients with cervical cancer revealed that BRCC3 expression was significantly increased in cervical cancer tissues, and BRCC3 expression levels were positively correlated with increasing clinical stages and pathological grades. Patients with increased expression levels of BRCC3 exhibited shorter survival times. This suggested that BRCC3 has important oncogenic roles and may represent a target gene for the diagnosis and treatment of patients with cervical cancer. To further investigate the molecular mechanism underlying the association between BRCC3 and cervical cancer, the expression levels of BRCC3 in three cervical cancer cell lines (HeLa, SiHa and C-33A cells) were determined. The results revealed that the expression levels of BRCC3 were increased all three cell lines. Considering that HPV infection is the leading cause of cervical cancer, and that >70% of cervical cancer is caused by HPV-16 and HPV-18 infection, the molecular mechanism underlying the effect of BRCC3 on HPV-18+ HeLa cells and HPV-16+ SiHa cells was also investigated via BRCC3 interference. The results demonstrated that BRCC3 interference inhibited the cell viability, and the invasion and migration abilities, of HeLa and SiHa cells.
EMT has an important role in embryonic development, chronic inflammation, tissue remodeling, cancer metastasis and numerous fibrotic diseases (25). The principal characteristics of EMT include decreased levels of cell adhesion molecules (including E-cadherin), the transformation of the cytokeratin cytoskeleton to a Vimentin-based cytoskeleton, and the development of morphological characteristics associated with mesenchymal cells (35,36). E-cadherin can regulate the activity of tight junctions in cells and prevent cell invasion and migration. A previous study demonstrated that decreased expression of E-cadherin induces EMT (37). Expression of E-cadherin may be regulated at numerous levels of transcription, translation and post-translational protein degradation (38). Vimentin is a type III intermediate filament protein in mesenchymal cells and represents the principal component of the cytoskeleton. Dysregulation of vimentin has been previously demonstrated in metastatic cells (39). MMPs are zinc-dependent endopeptidases that contribute to extracellular matrix degradation and are associated with tumor invasion and metastasis (40). MMPs are predominantly composed of non-glycosylated MMP2 and glycosylated MMP9, which belong to the type IV collagen protein family. Collagen degradation affects levels of cell invasion and tumor metastasis (41). Expression levels of MMP2 and MMP9 are closely associated with cervical cancer metastasis (42,43). In the present study, the knockdown of BRCC3 significantly inhibited the expression of MMP2 and MMP9, which suppressed the invasion and migration of HeLa and SiHa cervical cancer cells. Therefore, the results suggested that knockdown of BRCC3 suppressed EMT progression in cervical cancer cells.
In different tumors affecting humans, aberrant expression levels of Snai1 and Snai2 may affect EMT progression, cell invasion and migration (44,45). Snai1 has been demonstrated to induce hepatocellular carcinoma via enhancement of cell growth (46), and to accelerate pancreatic tumor growth (47) and breast cancer development (48). The results of the present study revealed that the knockdown of BRCC3 inhibited the expression of Snai1 and Snai2. In addition, a previous study demonstrated that the knockdown of Snai1 may be associated with MMP9, which subsequently induces the EMT process (49). Therefore, knockdown of BRCC3 may inhibit the EMT progress via regulation of Snai1/2 and MMP2/9 expression levels, thereby decreasing the invasion and migration of cervical cancer cells.
In conclusion, the results of the present study revealed a novel oncogene in cervical carcinoma, which was highly expressed in the majority of cervical cancer tissues and was demonstrated to be positively associated with cervical cancer progression. Knockdown of BRCC3 in HeLa and SiHa cervical cancer cells revealed that BRCC3 interference inhibited the viability, in addition to the invasion and migration abilities, of cervical cancer cells via regulation of Snai family members and MMPs, which subsequently inhibit the progress of EMT. The results of the present study suggested that BRCC3 may represent an effective target gene for the diagnosis and treatment of cervical cancer.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Authors' contributions
QZ conceived the study and FZ performed the experiments.
Ethics approval and consent to participate
Written informed consent was obtained from all patients, and the present study was approved by the ethics committee of Jinhua Municipal Central Hospital, Jinhua Hospital of Zhejiang University (Jinhua, China).
Patient consent for publication
All patients provided written informed consent before the present study.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Furusawa Y, Yunoki T, Hirano T, Minagawa S, Izumi H, Mori H, Hayashi A, Tabuchi Y. Identification of genes and genetic networks associated with BAG3-dependent cell proliferation and cell survival in human cervical cancer HeLa cells. Mol Med Rep. 2018 Aug 10; doi: 10.3892/mmr.2018.9383. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 2.Kan Y, Dong D, Zhang Y, Jiang W, Zhao N, Han L, Fang M, Zang Y, Hu C, Tian J, et al. Radiomic signature as a predictive factor for lymph node metastasis in early-stage cervical cancer. J Magn Reson Imaging. 2018 Aug 13; doi: 10.1002/jmri.26209. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 3.Okuhara T, Ishikawa H, Goto E, Okada M, Kato M, Kiuchi T. Processing fluency effect of a leaflet for breast and cervical cancer screening: A randomized controlled study in Japan. Psychol Health Med. 2018;11:1–11. doi: 10.1080/13548506.2018.1492732. [DOI] [PubMed] [Google Scholar]
- 4.Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, Murray CJ, Naghavi M. Breast and cervical cancer in 187 countries between 1980 and 2010: A systematic analysis. Lancet. 2011;378:1461–1484. doi: 10.1016/S0140-6736(11)61351-2. [DOI] [PubMed] [Google Scholar]
- 5.Krieger N, Bassett MT, Gomez SL. Breast and cervical cancer in 187 countries between 1980 and 2010. Lancet. 2012;379:1391–1392. doi: 10.1016/S0140-6736(12)60596-0. [DOI] [PubMed] [Google Scholar]
- 6.Eifel PJ, Winter K, Morris M, Levenback C, Grigsby PW, Cooper J, Rotman M, Gershenson D, Mutch DG. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: An update of radiation therapy oncology group trial (RTOG) 90–90. J Clin Oncol. 2004;22:872–880. doi: 10.1200/JCO.2004.07.197. [DOI] [PubMed] [Google Scholar]
- 7.Smith JS, Lindsay L, Hoots B, Keys J, Franceschi S, Winer R, Clifford GM. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: A meta-analysis update. Int J Cancer. 2007;121:621–632. doi: 10.1002/ijc.22527. [DOI] [PubMed] [Google Scholar]
- 8.Borges BES, Brito EB, Fuzii HT, Baltazar CS, Sá AB, Silva CIMD, Santos GFS, Pinheiro MDCN. Human papillomavirus infection and cervical cancer precursor lesions in women living by Amazon rivers: Investigation of relations with markers of oxidative stress. Einstein (Sao Paulo) 2018;16:eAO4190. doi: 10.1590/s1679-45082018ao4190. (In English; Portuguese) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Budukh A, Palayekar V, Maheshwari A, Deodhar K, Purwar P, Bagal S, Vadigoppula A, Lokhande M, Panse N, Dikshit R, et al. Menstrual pad, a cervical cancer screening tool, a population-based study in rural India. Eur J Cancer Prev. 2017 Jul 12; doi: 10.1097/CEJ.0000000000000387. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 10.Qureshi R, Arora H, Rizvi MA. EMT in cervical cancer: Its role in tumour progression and response to therapy. Cancer Lett. 2015;356:321–331. doi: 10.1016/j.canlet.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 11.Okusha Y, Eguchi T, Sogawa C, Okui T, Nakano K, Okamoto K, Kozaki KI. The intranuclear PEX domain of MMP involves proliferation, migration, and metastasis of aggressive adenocarcinoma cells. J Cell Biochem. 2018 May 15; doi: 10.1002/jcb.27040. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 12.Vences-Catalán F, Levy S. Immune targeting of tetraspanins involved in cell invasion and metastasis. Front Immunol. 2018;9:1277. doi: 10.3389/fimmu.2018.01277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwickert G, Walenta S, Sundfør K, Rofstad EK, Mueller-Klieser W. Correlation of high lactate levels in human cervical cancer with incidence of metastasis. Cancer Res. 1995;55:4757–4759. [PubMed] [Google Scholar]
- 14.Kim HJ, Do IG, Jeon HK, Cho YJ, Park YA, Choi JJ, Sung CO, Lee YY, Choi CH, Kim TJ, et al. Galectin 1 expression is associated with tumor invasion and metastasis in stage IB to IIA cervical cancer. Hum Pathol. 2013;44:62–68. doi: 10.1016/j.humpath.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 15.Baquero Díaz A, Romero BR, Gomez-Izquierdo L, Polo RA, Martin-Juan J, Rodriguez-Panadero F. Epithelial-to-mesenchymal transition in malignant mesothelioma. Eur Res J. 2011;38:2950. [Google Scholar]
- 16.Kahlert UD, Nikkhah G, Maciaczyk J. Epithelial-to-mesenchymal(-like) transition as a relevant molecular event in malignant gliomas. Cancer Lett. 2013;331:131–138. doi: 10.1016/j.canlet.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 17.Chaw SY, Majeed Abdul A, Dalley AJ, Chan A, Stein S, Farah CS. Epithelial to mesenchymal transition (EMT) biomarkers-E-cadherin, beta-catenin, APC and Vimentin-in oral squamous cell carcinogenesis and transformation. Oral Oncol. 2012;48:997–1006. doi: 10.1016/j.oraloncology.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Hao L, Ha JR, Kuzel P, Garcia E, Persad S. Cadherin switch from E- to N-cadherin in melanoma progression is regulated by the PI3K/PTEN pathway through Twist and Snail. Br J Dermatol. 2012;166:1184–1197. doi: 10.1111/j.1365-2133.2012.10824.x. [DOI] [PubMed] [Google Scholar]
- 19.Luo D, Xu X, Li J, Chen C, Chen W, Wang F, Xie Y, Li F. The PDK1/cJun pathway activated by TGFβ induces EMT and promotes proliferation and invasion in human glioblastoma. Int J Oncol. 2018 Aug 14; doi: 10.3892/ijo.2018.4525. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 20.Zuo Q, Wang J, Chen C, Zhang Y, Feng DX, Zhao R, Chen T. ASCL2 expression contributes to gastric tumor migration and invasion by downregulating miR223 and inducing EMT. Mol Med Rep. 2018 Aug 8; doi: 10.3892/mmr.2018.9363. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li J, Yu H, Xi M, Ma D, Lu X. The SNAI1 3′UTR functions as a sponge for multiple migration-/invasion-related microRNAs. Tumor Biol. 2015;36:1067–1072. doi: 10.1007/s13277-014-2733-z. [DOI] [PubMed] [Google Scholar]
- 22.Dong Y, Hakimi MA, Chen X, Kumaraswamy E, Cooch NS, Godwin AK, Shiekhattar R. Regulation of BRCC, a holoenzyme complex containing BRCA1 and BRCA2, by a signalosome-like subunit and its role in DNA repair. Mol Cell. 2003;12:1087–1099. doi: 10.1016/S1097-2765(03)00424-6. [DOI] [PubMed] [Google Scholar]
- 23.Py BF, Kim MS, Vakifahmetoglu-Norberg H, Yuan J. Deubiquitination of NLRP3 by BRCC3 critically regulates inflammasome activity. Mol Cell. 2013;49:331–338. doi: 10.1016/j.molcel.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 24.Boudreau HE, Broustas CG, Gokhale PC, Kumar D, Mewani RR, Rone JD, Haddad BR, Kasid U. Expression of BRCC3, a novel cell cycle regulated molecule, is associated with increased phospho-ERK and cell proliferation. Int J Mol Med. 2007;19:29–39. [PubMed] [Google Scholar]
- 25.Tu Z, Xu B, Qu C, Tao Y, Chen C, Hua W, Feng G, Chang H, Liu Z, Li G, et al. BRCC3 acts as a prognostic marker in nasopharyngeal carcinoma patients treated with radiotherapy and mediates radiation resistance in vitro. Radiat Oncol. 2015;10:123. doi: 10.1186/s13014-015-0427-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rebbeck TR, Mitra N, Wan F, Sinilnikova OM, Healey S, McGuffog L, Mazoyer S, Chenevix-Trench G, Easton DF, Antoniou AC, et al. Association of type and location of BRCA1 and BRCA2 mutations with risk of breast and ovarian cancer. JAMA. 2015;313:1347–1361. doi: 10.1001/jama.2014.5985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chai KM, Wang CY, Liaw HJ, Fang KM, Yang CS, Tzeng SF. Downregulation of BRCA1-BRCA2-containing complex subunit 3 sensitizes glioma cells to temozolomide. Oncotarget. 2014;5:10901–10915. doi: 10.18632/oncotarget.2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Del Carmen MG, Pareja R, Melamed A, Rodriguez J, Greer A, Clark RM, Rice LW. Isolated para-aortic lymph node metastasis in FIGO stage IA2-IB2 carcinoma of the cervix: Revisiting the role of surgical assessment. Gynecol Oncol. 2018;150:406–411. doi: 10.1016/j.ygyno.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 29.Tomita N, Mizuno M, Makita C, Kondo S, Mori M, Sakata J, Tsubouchi H, Hirata K, Tachibana H, Kodaira T. Propensity score analysis of radical hysterectomy versus definitive chemoradiation for FIGO stage IIB cervical cancer. Int J Gynecol Cancer. 2018 Aug 7; doi: 10.1097/IGC.0000000000001336. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 30.Jiang C, Wang H, Zhou L, Jiang T, Xu Y, Xia L. MicroRNA-212 inhibits the metastasis of nasopharyngeal carcinoma by targeting SOX4. Oncol Rep. 2017;38:82–88. doi: 10.3892/or.2017.5641. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 32.Liu Y, Zhang Y, Cheng R, Liu S, Qu F, Yin X, Wang Q, Xiao B, Ye Z. Radiomics analysis of apparent diffusion coefficient in cervical cancer: A preliminary study on histological grade evaluation. J Magn Reson Imaging. 2018 May 14; doi: 10.1002/jmri.26192. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 33.Wipperman J, Neil T, Williams T. Cervical cancer: Evaluation and management. Am Fam Physician. 2018;97:449–454. [PubMed] [Google Scholar]
- 34.Kodama J, Shinyo Y, Hasengaowa, Kusumoto T, Seki N, Nakamura K, Hongo A, Hiramatsu Y. Loss of basement membrane heparan sulfate expression is associated with pelvic lymph node metastasis in invasive cervical cancer. Oncol Rep. 2005;14:89–92. [PubMed] [Google Scholar]
- 35.Rhim AD, Mirek ET, Aiello NM, Maitra A, Bailey JM, Mcallister F, Reichert M, Beatty GL, Rustgi AK, Vonderheide RH, et al. EMT and dissemination precede pancreatic tumor formation. Cell. 2012;148:349–361. doi: 10.1016/j.cell.2011.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.De Craene B, Berx G. Regulatory networks defining EMT during cancer initiation and progression. Nat Rev Cancer. 2013;13:97–110. doi: 10.1038/nrc3447. [DOI] [PubMed] [Google Scholar]
- 37.Frixen UH, Behrens J, Sachs M, Eberle G, Voss B, Warda A, Löchner D, Birchmeier W. E-cadherin-mediated cell-cell adhesion prevents invasiveness of human carcinoma cells. J Cell Biol. 1991;113:173–185. doi: 10.1083/jcb.113.1.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cano A, Pérez-Moreno MA, Rodrigo I, Locascio A, Blanco MJ, del Barrio MG, Portillo F, Nieto MA. The transcription factor snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nat Cell Biol. 2000;2:76–83. doi: 10.1038/35000025. [DOI] [PubMed] [Google Scholar]
- 39.Kokkinos MI, Wafai R, Wong MK, Newgreen DF, Thompson EW, Waltham M. Vimentin and epithelial-mesenchymal transition in human breast cancer - observations in vitro and in vivo. Cells Tissues Organs. 2007;185:191–203. doi: 10.1159/000101320. [DOI] [PubMed] [Google Scholar]
- 40.Sheu BC, Lien HC, Ho HN, Lin HH, Chow SN, Huang SC, Hsu SM. Increased expression and activation of gelatinolytic matrix metalloproteinases is associated with the progression and recurrence of human cervical cancer. Cancer Res. 2003;63:6537–6542. [PubMed] [Google Scholar]
- 41.Zhai Y, Hotary KB, Nan B, Bosch FX, Muñoz N, Weiss SJ, Cho KR. Expression of membrane type 1 matrix metalloproteinase is associated with cervical carcinoma progression and invasion. Cancer Res. 2005;65:6543–6550. doi: 10.1158/0008-5472.CAN-05-0231. [DOI] [PubMed] [Google Scholar]
- 42.Lizarraga F, Espinosa M, Ceballos-Cancino G, Vazquez-Santillan K, Bahena-Ocampo I, Schwarz-Cruz Y, Celis A, Vega-Gordillo M, Lopez Garcia P, Maldonado V, Melendez-Zajgla J. Tissue inhibitor of metalloproteinases-4 (TIMP-4) regulates stemness in cervical cancer cells. Mol Carcinog. 2016;55:1952–1961. doi: 10.1002/mc.22442. [DOI] [PubMed] [Google Scholar]
- 43.Li XW, Tuergan M, Abulizi G. Expression of MAPK1 in cervical cancer and effect of MAPK1 gene silencing on epithelial-mesenchymal transition, invasion and metastasis. Asian Pac J Trop Med. 2015;8:937–943. doi: 10.1016/j.apjtm.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 44.Kahlert UD, Joseph JV, Kruyt FAE. EMT- and MET-related processes in nonepithelial tumors: Importance for disease progression, prognosis, and therapeutic opportunities. Mol Oncol. 2017;11:860–877. doi: 10.1002/1878-0261.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thaper D, Vahid S, Nip KM, Moskalev I, Shan X, Frees S, Roberts ME, Ketola K, Harder KW, Gregory-Evans C, et al. Targeting Lyn regulates Snail family shuttling and inhibits metastasis. Oncogene. 2017;36:3964–3975. doi: 10.1038/onc.2017.5. [DOI] [PubMed] [Google Scholar]
- 46.Qi J, Li T, Bian H, Li F, Ju Y, Gao S, Su J, Ren W, Qin C. SNAI1 promotes the development of HCC through the enhancement of proliferation and inhibition of apoptosis. FEBS Open Bio. 2016;6:326–337. doi: 10.1002/2211-5463.12043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shields MA, Ebine K, Sahai V, Kumar K, Siddiqui K, Hwang RF, Grippo PJ, Munshi HG. Snail cooperates with KrasG12D to promote pancreatic fibrosis. Mol Cancer Res. 2013;11:1078–1087. doi: 10.1158/1541-7786.MCR-12-0637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kang AR, An HT, Ko J, Kang S. Ataxin-1 regulates epithelial-mesenchymal transition of cervical cancer cells. Oncotarget. 2017;8:18248–18259. doi: 10.18632/oncotarget.15319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lin CY, Tsai PH, Kandaswami CC, Lee PP, Huang CJ, Hwang JJ, Lee MT. Matrix metalloproteinase-9 cooperates with transcription factor Snail to induce epithelial-mesenchymal transition. Cancer Sci. 2011;102:815–827. doi: 10.1111/j.1349-7006.2011.01861.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.