Abstract
A comprehensive review of pharmacological and medical aspects of the muscarinic class of acetylcholine agonists and antagonists is presented. The therapeutic benefits of achieving receptor subtype selectivity are outlined and applications in the treatment of Alzheimer’s disease are discussed. A selection of chemical routes are described, which illustrate contemporary methodology for the synthesis of chiral medicinal compounds (asymmetric synthesis, chiral pool, enzymes). Routes to bicyclic intrannular amines and intramolecular Diels-Alder reactions are highlighted.
Keywords: Alzheimer’s disease, nicotine, acetylcholine, arecoline, himbacine, tacrine, cyclostelletamines, intramolecular Diels-Alder reaction, indole alkaloids
| Contents | |
| 1 | The Pharmacology of Muscarinic Receptors |
| 1.1 | Introduction |
| 1.2 | Muscarinic receptor subtypes |
| 2 | Pharmacological Effects of Agonists and Therapeutic Applications |
| 2.1 | Cardiovascular system |
| 2.2 | Gastointestinal tract |
| 2.3 | Other smooth muscle |
| 2.4 | Glandular secretions |
| 2.5 | The eye |
| 2.6 | Central nervous system |
| 3 | Pharmacological Effects of Antagonists and Therapeutic Applications |
| 3.1 | Introduction |
| 3.2 | Cardiovascular system |
| 3.3 | Gastrointestinal tract |
| 3.4 | Urinary bladder |
| 3.5 | Airways |
| 3.6 | The eye |
| 3.7 | Prostate gland |
| 4 | The Medicinal Chemistry of Muscarinic Receptor Agonists and Antagonists |
| 4.1 | Scope |
| 5 | Muscarinic Agonists |
| 5.1 | Arecoline |
| 5.2 | Heterocyclic and other derivatives of arecoline |
| 5.3 | The synthesis of 1-aza-bicyclo[2.2.1]heptanes (1-azanorbornanes) and 1-azabicyclo[2.2.2]octanes (quinuclidines) |
| 5.3.1 | Intramolecular nucleophilic displacement by amines |
| 5.3.2 | Dieckmann condensation |
| 5.3.3 | Ester surrogates |
| 6 | Muscarinic Antagonists |
| 6.1 | Enantioselective synthesis of tertiary centres; tolterodine, rociverine, IQNP |
| 6.2 | Diels-Alder reactions |
| 6.2.1 | Indole alkaloids; allosteric activators of muscarinic binding |
| 6.2.2 | Himbacine; a muscarinic antagonist with allosteric properties |
| 6.2.3 | Cyclostellettamines; macrocyclic muscarinic antagonists |
| 7 | Conclusions and Future Prospects |
| 8 | References |
1 The Pharmacology of Muscarinic Receptors
1.1 Introduction
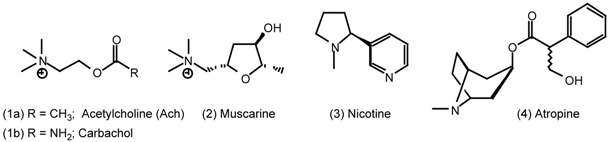
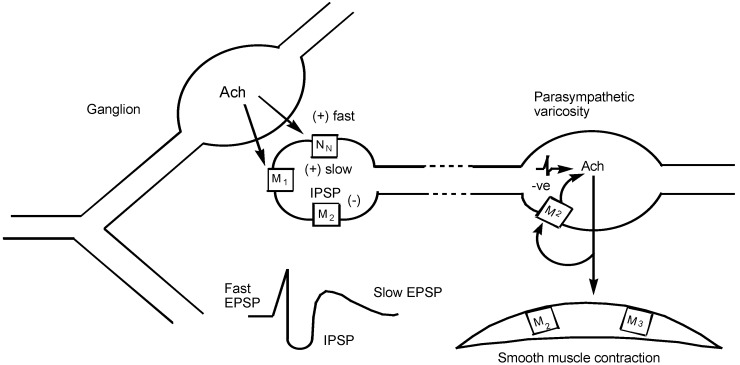
Muscarinic receptors are the receptor sites for the neurotransmitter of the parasympathetic autonomic nervous system, acetylcholine (Ach, 1a). Their primary location is on the post-synaptic cell membranes of smooth muscle, cardiac muscle and glandular tissue at the ends of parasympathetic nerve pathways. Muscarinic receptors are therefore responsible for mediating the physiological effects of parasympathetic nerve activity (Fig 1). These responses include; cardiac slowing, contraction of a wide range of smooth muscles (gastro-intestinal tract, detrusor muscle of the bladder, bronchioles, urethra, gall bladder and ducts, iris circular muscle, seminal vesicles and vas deferens), vasodilatation and increased secretion from exocrine glands (salivary glands, mucosal glands of the airways, gastric acid secretion and lachrymal secretion). The secretion of sweat is anatomically and physiologically a sympathetic response, but is mediated via the release of Ach onto muscarinic receptors. Acetylcholine interacts with two receptor types; termed muscarinic and nicotinic because the responses can be selectively mimicked by the alkaloids muscarine (2) and nicotine (3). The effects of stimulating these receptors can be distinguished by atropine (4) which is a competitive antagonist of muscarinic receptors and not nicotinic receptors. The main locations of nicotinic receptors are autonomic ganglia, the adrenal medulla, causing release of adrenaline, and the neuromuscular junctions in skeletal muscle [1].
Figure 1.
Muscarinic receptors at different locations along the autonomic parasympathetic efferent pathway. Acetylcholine (Ach) released from the preganglionic varicosity can interact with nicotinic NN, muscarinic M1 and muscarinic M2 receptors to produce a fast depolarisation (fast EPSP), a slow depolarization (slow EPSP) and hyperpolarization (IPSP), respectively. Nicotinic receptor stimulation sets up the action potential in the postganglionic neurone to release Ach from parasympathetic nerve terminal varicosities. This can interact with M2 or M3 receptors in smooth muscle.
As well as post-synaptically at parasympathetic nerve endings, muscarinic receptors have other locations. They are present on the ends of peripheral parasympathetic neurones (i.e. pre-synaptically) where they are responsible for auto-inhibition of transmitter release [2]. A further location is on the autonomic ganglia where the main process of neurotransmission is through Ach interacting with nicotinic receptors. However, muscarinic receptors are also present and are responsible for a secondary inhibitory component of transmission and a final slow depolarisation of the ganglionic cell body [3]. Muscarinic receptors are also widely distributed in the brain where they have both pre- and post- synaptic locations.
Drugs may interact with muscarinic receptors acting as agonists, stimulating and therefore mimicking the effects of endogenous Ach, or they may be antagonists, preventing the normal parasympathetic functions of the body and allowing sympathetic activity to predominate. Because of the wide range of locations of muscarinic receptors and responses to their stimulation or blockade, a variety of therapeutic applications have been known for many years.
A vast number of naturally occurring and synthetic agents have been available for some time but in general these show no tissue selectivity and therefore if aimed at a specific target will tend to produce undesirable side effects at other sites. More recently, the search has been for selective compounds and this has been primarily based on the fact that muscarinic receptors are now known to exist as at least five subtypes. The distribution of these receptor subtypes differs and tissue responses are mediated by the different subtypes. This review will deal with the muscarinic receptors involved in the various tissue responses, the current and potential therapeutic applications of stimulating or blocking these receptors, the medicinal chemistry of agents that interact with muscarinic receptors and the attempts to achieve selectivity among agonists and antagonists. Compounds with these muscarinic properties have a diverse range of structures and generalisations are readily confounded. Nevertheless the majority of the compounds have a basic nitrogen and a surrogate for the acetate group of acetylcholine (1a) and/or an aromatic moiety. Accordingly throughout this review, the chemical structures are drawn with the most basic nitrogen on the left and the acetate surrogate on the right whenever practically possible, to match the structures for acetylcholine (1a) and muscarine (2). Some amines are shown as the free base and others as the salt. The structure depicted is consistent with that assigned to the name of the compound, which may be for the salt or the free base. Anionic counterions are not shown unless they are relevant.
1.2 Muscarinic Receptor Subtypes
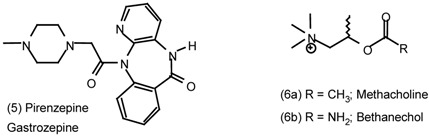
The possibility of more than one muscarinic receptor was first suggested by the preferential binding of the antagonist pirenzepine (5) to certain areas of brain tissue and autonomic ganglia rather than to smooth and cardiac muscle [4]. By the use of functional tissue responses and radioligand binding to tissue homogenates it is now clear that there are three firmly identified muscarinic receptors, M1, M2 and M3, with a fourth M4 now gaining acceptance (Table 1) [5]. Molecular biological techniques have resulted in the cloning of five muscarinic receptor cDNAs, designated m1 to m5, which encode the corresponding muscarinic receptor. When expressed in mammalian cell lines, these cloned receptors (identified by the lower case m) have the pharmacological characteristics of the M1 to M4 natural receptors. An M5 receptor has yet to be identified for a functional response, although recently m5 receptor binding sites have been proposed in certain brain regions after all other muscarinic receptor types have been occluded [6]. The amino acid sequences of the m1 to m5 receptors have been identified for several species including humans. There are a number of similarities in the amino acid residues of the m1 and m3 receptor compared with the m2 and m4 sequences. Muscarinic receptors belong to the super-family of G protein-linked receptors in which the amino acid chain spans the cell membrane seven times, with each hydrophobic trans-membrane domain formed into an α-helix. These α-helixes are arranged around a central pocket that serves as the point of entry of the agonist or antagonist and specific amino acid residues provide the groups for the drug receptor interactions.
Table 1.
Muscarinic receptors, second messengers and tissue responses
| Receptor subtype | Second messenger | Organ/tissue | Response |
| M1 | IP3/DAG↑ | autonomic ganglion including myenteric plexus | depolarization, slow EPSP increased gastric acid secretion via vagus nerve |
| M2 | cAMP↓ and direct coupling to K+ channel | vas deferens (rabbit) brain (cerebral cortex) canine saphenous vein heart - | reduced twitch height and NA release binding sites contraction |
| atrium | reduced rate (negative chronotropy) | ||
| sinu-atrial node prejunctional at autonomic nerve endings | reduced rate (negative chronotropy) reduced NA or Ach release | ||
| ileum smooth muscle | predominant binding sites - uncertain function | ||
| M3 | IP3/DAG↑ | smooth muscle -gut urinary bladder trachea iris circular muscle blood vessels- | contraction minor binding sites |
| endothelium smooth muscle glands - | release of NO and vasodilatation contraction | ||
| oxyntic cells (gastric acid) salivary glands pancreatic β cells | increased acid secretion salivation insulin release | ||
| M4 | cAMP↓ | guinea-pig uterus | contraction |
| rabbit anococcygeus muscle | NO-dependent relaxation | ||
| rabbit lung | binding sites | ||
| M5 | IP3/DAG↑ | brain regions | binding sites after all others occluded |
| Abbreviations: Ach, acetylcholine; cAMP, cyclic adenosine 3',5'-monophosphate; DAG, 1,2-diacylglycerol; EPSP, slow depolarization; IP3, inositol 1,4,5-triphosphate; NA, noradrenaline; NO, nitric oxide. | |||
The coupling of muscarinic receptors to the pharmacological response is through the G protein primarily at the third intracellular loop. Agonist activation of the receptor causes replacement of GDP with GTP binding to the α-subunit of the G protein which is then cleaved from the β- and γ-subunits. The GTP-bound α-subunit is thereby activated and stimulates or inhibits the activity of intracellular enzymes involved in the production of second messengers linked to the tissue response. M1, M3 and m5 receptors are linked through G protein of the Gq family to stimulation of phosphoinosidase C (PIC)[also known as phospholipase C, PLC]. PIC hydrolyses phosphoinositides including phosphatidylinositol 4,5-bisphosphate (PIP2), which forms inositol 1,4,5-triphosphate (IP3) and 1,2- diacylglycerol (DAG). IP3 and possibly DAG are second messengers for responses mediated via M1, M3 and m5 receptors. IP3 binds to receptor sites on the intracellular sarcoplasmic reticulum stores for Ca2+ and causes release of Ca2+ to initiate smooth muscle contraction and glandular secretion (M3 responses). DAG stimulates protein kinase C which initiates phosphorylation of key proteins involved in muscle contraction and Ca2+ influx.
In contrast, M2 and M4 receptors are coupled through Gi to the enzyme adenylyl cyclase. Cleavage of the GTP-bound α-subunit of the G protein results in inhibition of adenylyl cyclase and a fall in the levels of cyclic adenosine 3’,5’-monophosphate (cAMP) production from ATP. cAMP is a second messenger for a number of receptor types including β-adrenoceptors and histamine H2 receptors, its formation resulting in the activation of cAMP-dependent protein kinase (PKA) which produces tissue responses by phosphorylating a number of substrates. Thus, M2 and M4 receptor-mediated responses are brought about by inhibition of cAMP levels and inhibition of cAMP-dependent intracellular events. M2 receptors may also be linked through G proteins directly to ion channels without an intermediate second messenger, for example, in the heart [5, 7, 8, 9]. The muscarinic receptor subtypes, their second messengers and the pharmacological responses are summarised in Table 1.
2 Pharmacological Effects of Agonists and Therapeutic Applications
2.1 Cardiovascular System
The heart is slowed by parasympathetic activity of the vagus nerve on the sinu-atrial node pacemaker tissue, while ventricular contractility is only reduced when it is raised by sympathetic tone (i.e. an antiadrenergic effect). These effects are due to M2 receptor stimulation. The direct effect on nodal tissue is mainly due to direct coupling to K+ channels which are opened to allow K+ efflux, hyperpolarization and a reduction of the action potential duration. This results in cardiac slowing (bradycardia). The antiadrenergic activity is due to M2 receptor-mediated inhibition of cAMP production [10].
Blood vessels do not normally receive a parasympathetic innervation, but they respond to muscarinic agonists with a generalised vasodilatation and a fall in blood pressure. The vasodilator action is due to the presence of M3 muscarinic receptors on the endothelial lining of the vessel. Stimulation of these causes the release of nitric oxide (NO) by the action of nitric oxide synthase (NOS) on L-arginine, the nitric oxide causing relaxation of the underlying smooth muscle through accumulation of cGMP [11]. When the endothelium is removed or damaged, Ach (1a) can cause a contraction or local spasm of the smooth muscle. The receptor type mediating this response is poorly characterised and appears to be either of the M1 or M3 type depending on the vascular bed [12]. These cardiovascular effects of muscarinic agonists are no longer made use of therapeutically. The use of the vasodilator action of methacholine (6a) to treat vascular insufficiency, such as Raynaud’s syndrome, has ceased because of its unreliability. However, the possibility of M2 receptor-mediated bradycardia and circulatory collapse as a side effect of muscarinic agonists should not be overlooked.
2.2 Gastrointestinal Tract
The response of the gut to muscarinic agonists is an increase in motility and smooth muscle contraction (M3), increased secretions of gastric acid from the parietal (oxyntic) cells of the stomach and of digestive enzymes throughout the gut. The effect of vagal stimulation is blocked by the M1 receptor-selective antagonist, pirenzepine (5), and attributed to antagonism of M1 receptors in the parasympathetic ganglia of the gastric intramural plexus. The effects of agonists, however, are weakly antagonised by pirenzepine and due to a direct action at M3 receptors on the oxyntic cell [13]. The increase in intestinal motility by the non-selective agonist, bethanechol (6b), is utilised in cases of postoperative gastric distension and atony and in non-obstructive adynamic (paralytic) ileus [14].
2.3 Other Smooth Muscle
Smooth muscle in the airways and other organs such as the urinary bladder (detrusor muscle), gall bladder, vas deferens and urethra contracts in response to parasympathetic activation and muscarinic agonists; the effects being mediated via M3 receptors. The only current use of these actions is in the relief of postoperative and postpartum non-obstructive urinary retention. Although M3 receptors exclusively mediate the contractions of smooth muscle from these organs and the gastrointestinal tract, radioligand binding data has shown the presence of a mixed population of M2 and M3 receptors in most of these tissues. Indeed, the M2 receptors outnumber the M3 receptors by about 4:1. This has been confirmed by Northern blotting to determine the mRNA for the receptors and by immuno-precipitation experiments to estimate the receptor protein species expressed. What then is the role of these more abundant M2 receptors? It is proposed that they may provide an indirect component to the contractile responses under certain conditions since they are negatively linked to adenylyl cyclase and stimulation causes a decrease in cAMP levels. The reduction in cAMP would oppose the raised levels that accompany the relaxation of smooth muscle induced by sympathetic nerve activity or sympathomimetic amines. Thus, a contraction could ensue as result of this antagonism of relaxant tone. It has been suggested therefore that selective M3 antagonists are not necessarily the ideal for treatment of smooth muscle disorders, since they could expose an M2 receptor-mediated contraction [9].
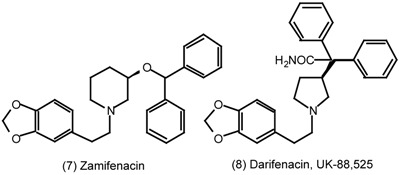
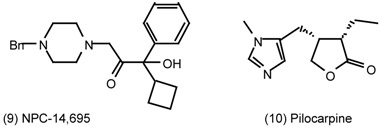
2.4 Glandular Secretions
Secretions from exocrine glands are uniformly stimulated by muscarinic agonists through M3 receptors. While these effects are probably mediated via the same receptor type as smooth muscle contraction, there is some evidence for differences in the activities of antagonists. For example, zamifenacin (7) and darifenacin (8) are M3 selective antagonists which show selectivity towards the smooth muscle M3 receptors of the ileum compared with M3 receptors controlling salivary secretion [15]. Furthermore, the M3 selective antagonist NPC-14,695 (9) showed selectivity for bronchial smooth muscle compared with salivary secretion [16]. The reasons for this tissue selectivity are unclear since the involvement of identical receptors should result in the same degree of antagonism. One possibility is that receptor configuration or antagonist binding are affected by tissue-dependent factors such as the signal transduction pathways (receptor coupling) or the presence of other receptor subtypes which exert a modulating function [15].
2.5 The Eye
Parasympathetic nerves control of the circular (sphincter pupillae) muscle of the iris and the ciliary muscle which alters the curvature of the lens. The iris circular muscle contracts via M3 receptors in response to bright light, constricting the pupil. Contraction of the ciliary muscle accommodates the lens for near vision and is also M3 receptor-mediated. The contraction of the iris away from the drainage canal for the aqueous humour (canal of Schlemm) opens the drainage angle which facilitates its drainage. This property of muscarinic agonists reduces the raised intraocular pressure that occurs in glaucoma. Topical pilocarpine (10) has been widely used for many years in the treatment of wide-angle and narrow-angle glaucoma [17]. Visual discomfort through M3 receptor stimulation remains a problem with systemically administered muscarinic agonists.
2.6 Central Nervous System
Muscarinic receptors in the brain offer a major therapeutic target for muscarinic agonists in the treatment of Alzheimer’s disease [18, 19, 20]. This is based on two aspects of the pathophysiology of Alzheimer’s disease (AD) and memory dysfunction; the cholinergic hypothesis of memory dysfunction and the muscarinic receptor regulation of amyloid metabolism. The loss of memory in AD is associated with a cholinergic deficit, which takes the form of a selective decrease of cholinergic neurones in the ventral forebrain whose axons project into the cortex and hippocampus. These cholinergic projections form vital components of the ascending reticular activating system which is involved in memory function and attention. There is an associated reduction in the activity of choline acetyltransferase (CAT), the enzyme responsible for synthesis of Ach. The postsynaptic muscarinic receptors upon which these neurones impinge and therefore involved in cognitive function are of the M1 subtype. Although the neurones are damaged in AD, the M1 receptors are not significantly reduced. Further support for a role of central muscarinic receptors in memory is the observation that antagonists, such as hyoscine (scopolamine, 11), impair memory [21].
The second major histopathological change observed in AD is the presence of amyloid plaques, together with neurofibrillary tangles in dead and dying neurones in the brain. Amyloid deposits consist of aggregates of peptides having 40-43 amino acid residues and known as β-amyloid peptide (Aβ). Aβ is derived from the cleavage of a family of glycoproteins termed amyloid precursor protein (APP) and is neurotoxic [22]. In cultured cell lines transfected with m1 and m3 receptors, it has been shown that the muscarinic agonist carbachol (1b) can reduce the secretion of Aβ [23]. In cells transfected with m2 and m4 receptors, APP processing was not affected by muscarinic agonists. The site of action of the M1 receptor agonist appears to be an increase in the activity of a protease, α-secretase, through phosphoinositide turnover and stimulation of protein kinase C. α-Secretase cleaves the APP in the Aβ domain so that Aβ cannot be produced from APP; muscarinic agonists therefore reduce the levels of Aβ produced [24]. Thus, it appears that Ach acting on M1 receptors may prevent the deposition of neurotoxic amyloid in the brain and thus influence the pathogenic process itself. Muscarinic agonists selective for M1 receptors therefore have potentially a two-fold action in the treatment of AD; stimulation of the postsynaptic receptors involved in memory and inhibition of amyloid deposition [25].
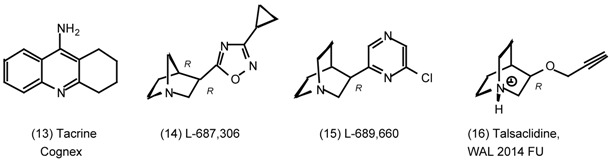
Currently, treatment of AD by this approach is limited to the use of anticholinesterases which non- selectively enhance the reduced levels of Ach [26,27]. Physostigmine (12a) has been reported to induce small transient improvements in cognitive function in Alzheimer’s patients. Tacrine (13) [28] is a reversible non-competitive inhibitor of cholinesterase with three-fold selectivity for butyrylcholinesterase which has also shown improvements in these patients [29]. The clinical use of tacrine (13) has however been restricted by its hepatotoxicity [30]. Another disadvantage of anticholinesterases is that their activity may be self-limiting. The raised Ach levels could activate autoinhibitory pre-synaptic M2 receptors which would reduce the levels of Ach released. Indeed, blockade of these pre-synaptic receptors offers an alternative approach to the treatment of AD, their blockade would presumably enhance the release of Ach from the central neurones. Thus, an optimal combination would be M1 agonism together with M2 antagonism [31]. L-687,306 (14) [32] and the related chloropyrazine, L-689,660 (15) [33,34], display this type of property. The former has M1 partial agonist activity and M2/M3 antagonistic activity, while L-689,660 is an M1 agonist, M3 partial agonist and M2 antagonist based on functional tissue responses [35]. By radioligand binding analysis, however, they show no selectivity of binding affinity [36](cf. ester surrogates). Talsaclidine (16) is also an M1 selective full agonist but M2 and M3 partial agonist [37] which is effective and well tolerated in Phase I safety trials [38]. Thus, selectivity for M1 receptors through differential binding has been difficult to achieve. The selectivity of the compounds described above has been attained by utilising differences in receptor reserve for the various muscarinic receptor subtypes and their functional responses.
3. Pharmacological Effects of Antagonists and Therapeutic Applications
3.1 Introduction
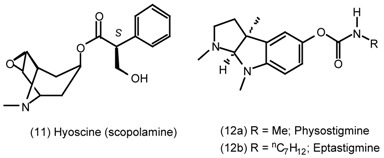
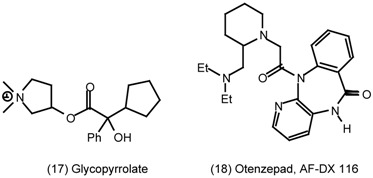
The prototype muscarinic antagonist is atropine, which is the racemate, (±)-hyoscyamine (4), of the naturally occurring alkaloid from the Deadly Nightshade (Atropa belladonna). (-)-Hyoscyamine occurs naturally, but racemisation takes place on heating and extraction. In spite of the synthesis of a wide range of new antagonists, atropine remains one of the most potent antagonists available. (-)- Hyoscyamine (or atropine) is a competitive antagonist without selectivity for any of the subtypes of muscarinic receptor. It antagonises the effects of muscarinic agonists and of the parasympathetic nervous system allowing sympathetic tone to dominate. In vivo, however, atropine (4) has differential effects on the various organs of the body with the salivary and bronchial secretions being depressed by low doses. As the dose is increased, so progressively more organs are affected, the order being pupil, heart, bladder and gastrointestinal tract. Finally, large doses are required to inhibit gastric acid secretion and motility. The reason for this is firstly the presence of pre-synaptic autoinhibitory M2 receptors, blockade of which by atropine allows the release of more Ach from parasympathetic neurones to overcome the post-synaptic blockade. The second reason is that parasympathetic nerve pathways in many organs contain non-adrenergic non-cholinergic components which release not Ach but alternative or co-transmitters, including ATP. These contribute to the tissue response but are not blocked by muscarinic antagonists. The degree of resistance to blockade varies between organs depending on the involvement of NANC pathways; in the bladder and gastrointestinal tract they are particularly evident [1]. The therapeutic usefulness of non-selective antagonists like atropine is restricted by their wide-spread effects. This may be an advantage, however, for example in the use of hyoscine (11) and glycopyrrolate (17) in premedication for surgical procedures. The blockade of salivary and mucus secretions, cardioprotection, block of smooth muscle spasm and a degree of amnesia and sedation are desirable properties, although with modern anaesthetics the use of antimuscarinic premedicants is less common these days.
3.2 Cardiovascular System
The heart rate is under parasympathetic tone via M2 receptors on the SA node, which are blocked by atropine to cause tachycardia. There may be a paradoxical transient slowing of heart rate after slow intravenous administration, probably because of initial blockade of the pre-synaptic M2 autoreceptors. The tachycardia, however, predominates together with an increase in conduction velocity which facilitates transmission of excitation to the ventricles via the AV node. This property of atropine (4) is used in the emergency treatment of acute myocardial infarction when the dominant autonomic influence on the heart is via the vagus nerve, causing sinus or nodal bradycardia. Selective M2 receptor antagonists are therefore of potential value for this indication and AF-DX 116 (otenzepad) (18) is in the latter stages of development for bradycardia [39].
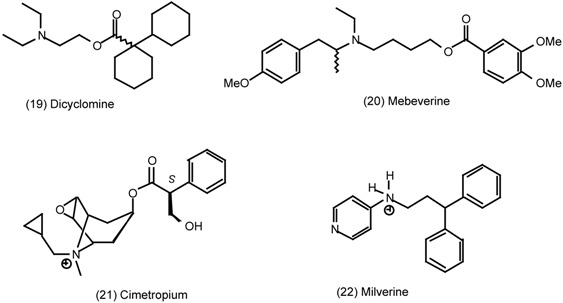
3.3 Gastrointestinal Tract
Muscarinic antagonists inhibit the contractions of the gastrointestinal tract induced by Ach and other muscarinic agonists mediated via M3 receptors. They are, however, generally less effective against the increases in contractility and motility due to parasympathetic nerve stimulation. The reason for this is the contribution of atropine-resistant NANC pathways to the contraction. The partial inhibition of gastrointestinal motility by atropinic drugs has led to their widespread use as antispasmodics in the treatment of disorders associated with intestinal hypermotility. The belladonna alkaloids have long been used for the treatment of gastrointestinal upset, Tincture of Belladonna having formerly been a common component of several widely used mixtures. Established non-selective antimuscarinics, including dicyclomine (19), are used for the relief of intestinal colic due to muscle spasm, particularly in children. An expanding market is also for the symptomatic treatment of diarrhoea associated with irritation of the lower bowel, such as mild dysenteries and diverticulitis, known as irritable bowel syndrome (IBS). Existing drugs for the treatment of IBS, such as mebeverine (20), cimetropium (21) and milverine (22), have additional properties including Ca2+ channel blockade which contributes to their antispasmodic activity [40]. There is therefore a need for selective M3 receptor antagonists for the treatment of gastrointestinal tract disorders. Zamifenacin (7) and darifenacin (8) show selectivity for M3 over M2 and M1 receptors and the latter has been in Phase II clinical evaluation with encouraging results [15]. Since M3 receptors are also involved in the secretory and miotic (pupil constriction) responses of muscarinic agonists, side effects of dry mouth and visual discomfort are still likely with such antagonists. Darifenacin (8), however, shows selectivity towards the ileum compared with salivary glands and other smooth muscle. The reasons for this are unclear at present, but it has been suggested that this might indicate a difference in the M3 receptors in different tissues. It would be advantageous to exploit these differences in developing newer more selective compounds for use in gastrointestinal disorders [40].
A different application for muscarinic antagonists in the gastrointestinal tract has been in the treatment of peptic ulcers. Gastric acid secretion induced by parasympathetic nerve activity is due to a direct action of Ach on the acid secreting parietal cells and an indirect effect through the release of gastrin from the antrum of the stomach. The secretory responses of muscarinic agonists are blocked predictably for an M3 receptor-mediated effect, so that the selective M1 receptor antagonist, pirenzepine (5), is weakly effective. However, pirenzepine is more potent as an antagonist of secretion induced by nerve stimulation. The site of action is probably inhibition of M1 receptors located on the post-ganglionic nerves of the myenteric plexus. As a result of the inhibition of gastric acid secretion and reduced gastric motility, antimuscarinic agents aid the healing of peptic ulcers. Widespread side- effects arising from their non-selective blockade of muscarinic receptors and improved efficacy of histamine H2 antagonists, cimetidine and ranitidine, have resulted in a decline in their use. The M1 selective antagonist pirenzepine (5), however, has a lower incidence of muscarinic side effects and is as effective as cimetidine at promoting ulcer healing in patients with duodenal ulcer.
3.4 Urinary Bladder
The contraction of the detrusor muscle of the body of the bladder in response to filling to a critical level resulting in micturition is mediated via the action of Ach released from parasympathetic nerves on M3 receptors. This response is inhibited by muscarinic antagonists and the ensuing urinary retention is of value in the management of urinary incontinence (UI) [41]. They have widespread application in urge incontinence in the elderly, in children suffering from nocturnal enuresis, and to reduce urinary frequency in spastic paralysis. Urge incontinence occurs when there is an involuntary passing of urine associated with a strong desire to void the bladder. Motor urge incontinence occurs where there is increased contractile activity of the bladder brought on by outflow obstruction, inflammation or irritation, such as that due to infection associated with cystitis. Stress incontinence is due to weakness of the skeletal muscle associated with the external sphincter of the bladder and is therefore not susceptible to antimuscarinic drugs. The muscarinic antagonists in current use include propantheline (23) and emepronium (24). Being quaternary ammonium compounds, they are not transported into the brain and therefore only have peripheral side effects, including dry mouth, blurred vision and tachycardia, due to their non-selective blockade of muscarinic receptors.
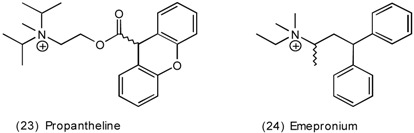
The drug of choice for UI is oxybutynin (25), which is a non-selective muscarinic antagonist with additional direct smooth muscle relaxant properties through Ca2+ channel blockade and local anaesthesia. Terodiline (26) is a muscarinic antagonist with additional Ca2+ channel blocking activity that gained a valuable place in the management of UI [42]. It was, however, withdrawn after reports of serious heart rhythm disturbances attributed to depression of the SA node, which is probably unrelated to muscarinic receptor blockade and therefore not likely to occur with other drugs in this class. Tolterodine (27) is a new non-selective muscarinic antagonist that has bladder selectivity over salivary secretions and has been shown to be well tolerated and effective in patients with UI with minimal propensity to cause dry mouth [43].
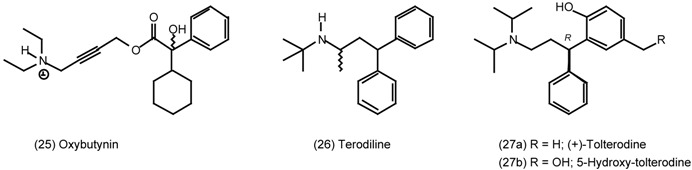
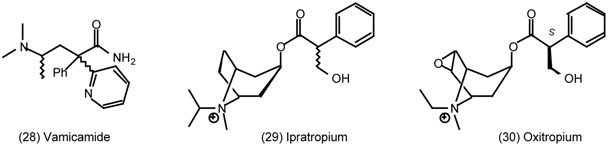
As with gastrointestinal applications, there is an advantage from M3 receptor selective antagonists and several of these are in development. The limitations are again that M3 receptors are also involved in salivary secretion and eye functions, leading to potential for appropriate side effects. M3 selective compounds displaying tissue selectivity for the bladder have been identified, including zarifenacin (7) and vamicamide (28). The latter compound is more selective in vivo probably because of favourable pharmacokinetics which allows it to be concentrated in the bladder, thereby exerting a localised spasmolytic action [44].
3.5 Airways
Parasympathetic innervation of the airways releases Ach onto M3 receptors which causes bronchoconstriction and increased volume of mucous secretion (without altered viscosity). Blockade of these effects by muscarinic antagonists is of limited use in the treatment of asthma but may be beneficial during acute exacerbations of asthma. They are particularly useful in chronic obstructive pulmonary disease (COPD) associated with emphysema and chronic bronchitis, which are regarded as having non-reversible obstruction of the airways. Presumably the parasympathetic vagal tone to the lungs is reversible [45]. A possible disadvantage of atropinic drugs is inhibition of ciliary beating and therefore impaired mucociliary clearance.
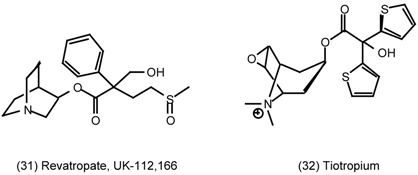
Muscarinic antagonists currently in use, including ipratropium (29) and oxitropium (30), are non- selective between receptor subtypes. Administered by inhalation they are virtually devoid of systemic effects on the eye, bladder and heart, and the charged quaternary nitrogen atom prevents CNS effects. An unexplained advantage of ipratropium (29) over atropine (4) is that it does not appear to impair mucociliary clearance [46]. It would be an advantage to selectively block the M3 receptors mediating bronchoconstriction and bronchial secretions, together with the M1 receptors involved in ganglionic transmission of the vagal reflex pathways. Blockade of autoinhibitory presynaptic M2 receptors on the parasympathetic nerve terminals would counteract these inhibitory actions by facilitating Ach release. Thus agents selective for M3 and M1 receptors are currently being sought for use in the treatment of COPD. Revatropate (31) is one such compound which has shown benefit in early clinical trials [15]. Tiotropium (32) has non-selective binding properties but achieves M3 selectivity because of a preferential off-rate from M3 compared with M2 receptors [47].
3.6 The Eye
Muscarinic antagonists prevent the parasympathetic nerve-mediated contraction of the circular muscle of the iris in response to bright light and the accompanying pupillary constriction. The contraction of the ciliary body allowing the lens to accommodate for near vision is also blocked (cycloplegia). Both of these effects are due to blockade of M3 receptors. The dilation of the pupil (mydriasis) and relaxation of the iris into the drainage angle of the anterior chamber of the eye, impedes drainage of aqueous humour into the canal of Schlemm. There is therefore a risk of raising intraocular pressure and precipitating glaucoma of the narrow-angle type in susceptible individuals. While muscarinic receptor antagonists have ophthalmic uses, mainly for dilating the pupil to make eye examinations of the retina, the point of major importance is the risk of glaucoma and the contraindication of their uses in patients at risk.
3.7 Prostate Gland
The human prostate gland is sparsely innervated by cholinergic nerves [48] and muscarinic receptors of the M1 type have been found localised to the glandular epithelium, where they are therefore primarily involved in secretory responses [49]. An involvement in cell proliferation is also suggested and therefore a role in the hyperplasia of benign prostatic hypertrophy (BPH) [50]. This is a common disorder affecting over 70% of men in their seventies which leads to difficulty in initiating and completing the voiding of urine. Muscarinic agonists also cause contraction of isolated smooth muscle strips from the prostatic stroma [51] and enhance contractions to field stimulation of guinea-pig prostatic stroma, possibly through activation of presynaptic receptors facilitating noradrenergic transmitter release. Muscarinic antagonists are generally regarded as being contraindicated in patients with BPH because they interfere with the normal parasympathetic control of the bladder reflex. However, in view of the involvement of muscarinic receptors in the prostate gland itself, there is an argument for the use of M1 selective muscarinic antagonists in the treatment of BPH. We are not aware of any clinical evidence for their effectiveness.
4. The Medicinal Chemistry of Muscarinic Receptor Agonists and Antagonists
4.1 Scope
As noted in the introduction, muscarinic receptor agonists and particularly antagonists have a diverse range of chemical structures. It is not feasible or perhaps even desirable within a review of this length to make a broad survey of the field. Even a review of currently prescribed medicines or research tools would be beyond the space allocated. Therefore this section will concentrate on some recent trends and highlight generic synthetic methods. Emphasis will also be given to anti-Alzheimer drugs in view of the pressing need for effective treatments, albeit the efficacy of a muscarinic treatment rationale for this area has yet to be established unequivocally. Towards the end of this section, emphasis will also be given to natural products which have muscarinic activity, with the intention that they may provide a spur to endeavours for the creation of new medicinal entities.
5 Muscarinic Agonists
It is a good general rule that muscarinic agonists are small molecules, whereas antagonists are large molecules which frequently contain an aromatic moiety. This enforces an inherent conservatism in the design of agonists. The designers of agonists must perforce be incrementalists, making modest but significant structural modifications to obtain receptor sub-type selectivity, whereas the antagonist designer works on a broader canvas and has the freedom to employ bold strokes of synthetic virtuosity.
5.1 Arecoline
Arecoline (33b) has been an important lead compound in this area. The free acid, arecaidine (33a) (or acrecaine) and arecoline (33b) are obtained from betel or areca nuts (Areca catechu)[52,53]. These have been chewed in many parts of Asia to induce salivation (a muscarinic property) and euphoria (a nicotinic receptor stimulant property) [54]. Habitual chewing of these nuts is strongly correlated with the incidence of oral cancer [55,56]. Arecoline has about 80% of the muscarinic activity of Ach (1a) at physiological pH, and has been used to treat Alzheimer's' disease. Verbal memory was improved at low doses [57,58], whereas attention and visuospatial abilities were improved at higher doses [59]. Low doses were tolerated well [60], but high doses produced nausea and vomiting [61]. The optimum dose varied fourfold from 4-16mg day [62] and about 20% of patients had no response whatsoever. Unfortunately arecoline (33b) is orally ineffective, due to first-pass metabolism and all of these studies were performed with intravenous perfusion of the drug. Attempts to develop a transdermal device were confounded by skin inflammation [63], although this could be mitigated by modifying the vehicle [64] and intranasal absorption is efficient [65]. The first step in the metabolism of arecoline by mice liver homogenates is hydrolysis of the ester group by a carboxylesterase [66].
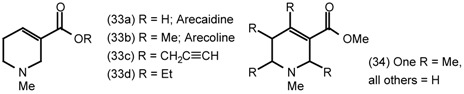
There have been two main strategies to improve the efficacy and selectivity of arecoline (33b). Derivatives have been prepared in which the ester is replaced by a less or non-hydrolysable equivalent. Alternatively the piperidine ring has been bridged to give rigid derivatives following the common pharmacological dictum that rigidity confers selectivity. Consequently there are innumerable muscarinic agonists based on the 1-aza-bicyclo[2.2.1]heptane (azanorbornane) and 1-aza- bicyclo[2.2.2]octane (quinuclidine) skeletons bearing an ersatz ester group. The novelty in this area derives from the choice of ester surrogate and, more rarely the means by which the ring system is constructed. The exquisite sensitivity to substitution may be judged from the monomethyl-derivatives (34) which were all antagonists-partial agonists. Even the ethyl derivative (33d) is only a partial agonist [67] and N-desmethylarecoline (guvacoline) has a lower affinity for muscarinic receptors. The propargyl ester (33c) is as potent as the methyl ester (33b), and is frequently used as a research tool because it has slight M2 selectivity, however it is too easily hydrolysed to be a viable medicine [68].
5.2 Heterocyclic and Other Derivatives of Arecoline
Arecoline (33b) is commercially available and has served as the starting material for many derivatives. Alternatively sodium borohydride reduction of pyridinium salts is an excellent way to prepare 1,2,5,6-tetrahydropyridine derivatives, particularly if a substituent is present at the 3-position.
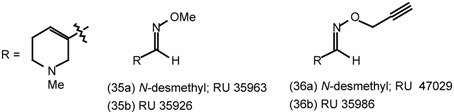
The O-methyl (35) and O-propargyl (36) oxime derivatives of arecoline carboxaldehyde had potent agonist properties in a battery of assays, with M1 selectivity over all other muscarinic receptor subtypes. They also relieved scopolamine induced memory deficit in rats and mice at doses 2-3 orders of magnitude lower than arecoline (33b) and had a longer duration of action [69,70]. 1,2,4-oxadiazoles can be regarded as "cyclised" oxime derivatives. The methyl derivative (37) was more potent than arecoline (33b), but had marginally lower efficacy [71]. The ethyl-triazole (38a) and the tetrazole (38b) are both M1 agonists and M2 antagonists such that cholinergic side effects were only found at high doses. Increasing the chain length at the 2-position decreases the efficacy and increases antagonistic profiles [72].
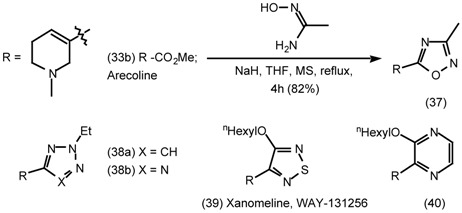
Xanomeline (39) has emerged as one of the most potent unbridged arecoline derivatives. It has higher potency and efficacy for m1 and m4 than for m2, m3 and m5 receptor subtypes [73], binds to the m1 receptor subtype uniquely tightly [74,75] and stimulates phosphoinositide hydrolysis in the brain. In cells containing human m1 receptors which are stably expressing amyloid precursor protein (APP), xanomeline (39) stimulates APP release with a potency 1000 greater than carbachol and reduces the secretion of Aβ by 46% [76] (cf 2.6 Central nervous system). In patients with Alzheimer's disease, it halted cognitive decline and reduced behavioural symptoms such as hallucinations, delusions and vocal outbursts [77,78]. As might be expected there have been numerous attempts to prepare analogues with comparable potency and efficacy. Transplanting the thiadiazole ring of xanomeline to a range of bicyclic amines reduced selectivity [79,80] as did the use of pyrazine analogues (40) [81].
5.3 The Synthesis of 1-Aza-bicyclo[2.2.1]heptanes (1-Azanorbornanes) and 1-Aza-bicyclo- [2.2.2]-octanes (Quinuclidines)
Methods for the synthesis of muscarinics based on the 1-aza-norbornane and quinuclidine skeletons almost invariably commence with the ketones (41) or the hydroxymethyl-derivatives (42) or derivatives at a higher oxidation state. Of these four compounds only quinuclidinone (41b) and quinuclidinol (52) are commercially available and the latter costs circa £1.50/grm. Quinuclidinol (52) is an intermediate in the synthesis of [3H]-quinuclidinyl benzilate (QNB) and the N-methyl derivative which are frequently used as non-selective muscarinic antagonists in pharmacological experiments. There are surprisingly few syntheses of quinuclidine derivatives and fewer of 1-aza-norbornanes and many are low yielding. In short, the synthesis of these compounds is comparatively undeveloped and the brief review of synthetic methods presented here is intended to spur further developments in this area.

5.3.1 Intramolecular Nucleophilic Displacement by Amines
The first reported synthesis of 1-aza-norbornan-3-one (41a) commences with the condensation of 2-pyrrolidinone (44) with diethyl oxalate (43) to give the diketoester (45). This reaction proceeds via N-acylation of 2,3-pyrrolidinone, ring opening of the imide and a Dieckmann cyclisation to give the diketoester (45) which exists predominantly as the enol (46) [82]. Catalytic hydrogenation gives the cis-hydroxy-ester which is reduced to the diol (48a). Thermolysis in the gas phase in a flow reactor over basic alumina gave the alcohol (49) which was oxidised to 1-aza-norbornan-3-one (41a) with Jones’ reagent (62% yield) [83].
This synthesis has been re-examined recently. The ring expansion and reduction steps were repeated in virtually identical yields to the original work. Ring closure using Mitsunobu reagents gave a poor yield, however protection of the amine as the carbobenzyloxy derivative (48b) and selective primary tosylation proceeded in virtually quantitative yield. Hydrogenolysis of the carbobenzyloxy group and treatment with mild base effected cyclisation in excellent yield [84].
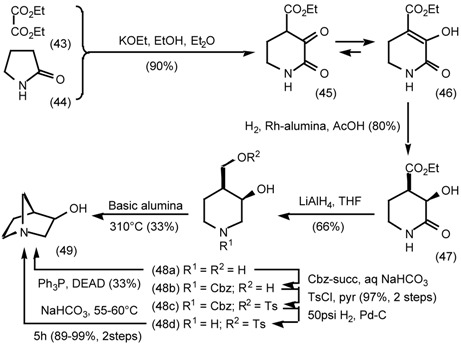
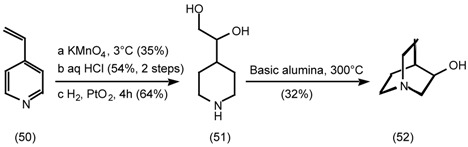
“Cyclodehydration” by thermolysis was also used in the synthesis of quinuclidinol (52). Dihydroxylation of 4-vinylstyrene (50), pyridinium salt formation and catalytic hydrogenation gave the 4-(dihydroxyethyl)-piperidine (51) which was cyclised as before [85]. Although this sequence is brief it suffers from two poor steps. The 35% yield for permanganate oxidation is adjusted for recovered starting material and the apparently poor yield for hydrochloride formation is due to the use of crude material from the prior permanganate oxidation.
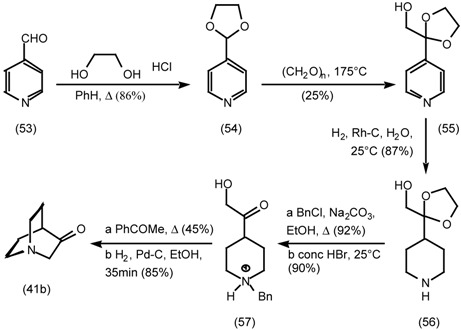
Thermal cyclodehydration was also used to prepare quinuclidinone (41b). 4-Pyridinecarboxaldehyde ketal (54) was alkylated by formaldehyde via the quaternary aminol and the enamine [86]. Catalytic hydrogenation gives the piperidine ketal (56), which was benzylated on nitrogen and the ketal removed. Cyclodehydration was achieved under comparatively mild conditions by refluxing in acetophenone (bp 202°C) [87].
All of the syntheses described thus far (with one exception) have used an archaic thermolytic cyclodehydration to create the bicyclic ring system. In the following three contemporary examples, displacement of a bromide or a sulfonate ester by the ring nitrogen is the key cyclisation step. Nevertheless in the next synthesis the carbon skeleton is assembled in a similar way to the older work.
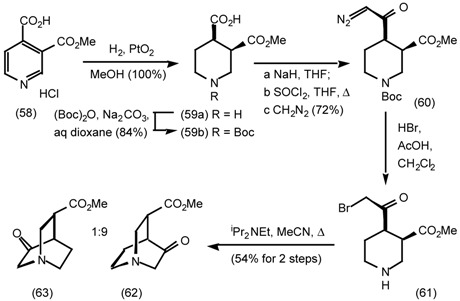
Catalytic hydrogenation of the pyridine monoester (58) gave the cis-product (59a) which was protected as the t-butoxycarbonyl derivative (59b). Reaction of the acid chloride with diazomethane gave the diazoketone (60) which was displaced to give the α-bromoketone (61).
The final cyclisation could be only be achieved in fair yield under high dilution conditions using Hunig's base. The ratio of the products (62):(63) implies that cyclisation occurs predominantly with retention of stereochemistry at the ring carbons bearing the carbonyl substituents, although clearly there are other explanations for the stereoselectivity observed [88].
There are few enantioselective routes to 1-azanorbornanes and quinuclidines because they are comparatively easy to resolve as diastereomeric salts or by chiral HPLC. Moreover medicinal chemists usually require both enantiomers for testing. The following synthesis illustrates the enantioselective transacylation of a prochiral diol in organic solvent catalysed by a lipase. The prochiral diol (66c) was assembled by aldol condensation of Meldrum's acid (64) with 4-N-benzylpiperidone (65), reduction of the alkene, cleavage of the benzyl and acetal protecting groups (with esterification), reprotection of the amine and reduction of the diester. Acetylation yielded the prochiral diacetate (66b) which was hydrolysed by porcine pancreatic lipase (PPL) or a variety of other lipases to give the (S)-hydroxyacetate (66a) with low enantioselectivity (best result, 39% yield, 74%ee). The converse reaction; irreversible acetylation of the diol (66c) with vinyl acetate (as solvent) gave the (R)-hydroxy-acetate (66d), hence in both cases the enzyme is selective for reaction at the (pro-R)-group [89]. After routine functional group manipulations, the mesylate underwent intramolecular nucleophilic displacement to give (R)-3-hydroxymethylquinuclidine (R)-(42b) without erosion of enantiomeric excess [90].
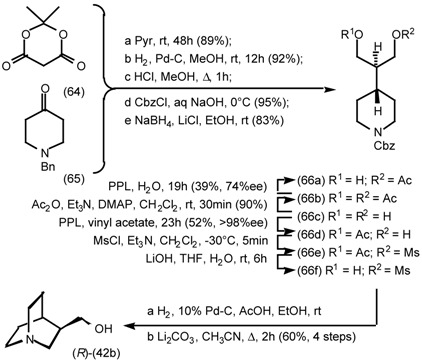
Despite spectacular advances in asymmetric synthesis, sugars continue to be important starting materials for the synthesis of enantiomerically pure natural products [91, 92, 93] such as marine toxins [94] and pheromones [95]. Two syntheses of (3S,5S)-quinuclidin-3,5-diol (73) demonstrate the use of carbohydrates in the synthesis and demonstrate the pitfalls of extrapolating well known chemistry. The first synthesis which proceeded as expected, commenced with d-arabinose dithioacetal (67a), which was selectively protected at the 6-hydroxy group, the thioacetal cleaved and the furanose protected as the 1,2-O-isopropylidene derivative (68). Oxidation yielded a ketone which reacted unusually rapidly with a stable phosphorane, presumably due to the adjacent electron withdrawing groups. Manipulation of the two carbon appendage gave an azido-furanoside (70c), which was hydrolysed to the azidopyranoside (71).
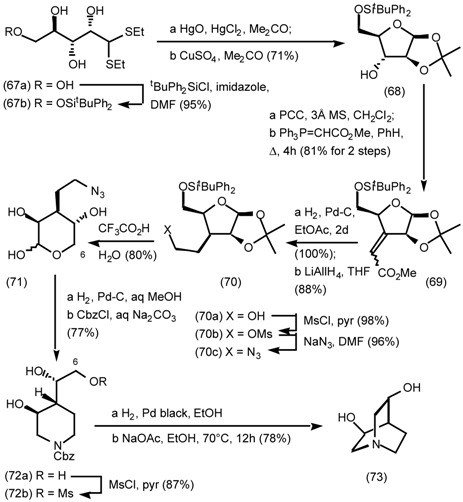
Hydrogenation gave an amine which underwent reductive amination with the aldehydic form of the lactol to give the piperidine which was protected as the carbobenzyloxy-derivative (72a). Selective mesylation of the primary hydroxyl group (72b) and hydrogenolysis, followed by intramolecular nucleophilic displacement gave (3S,5S)-quinuclidin-3,5-diol (73).
Functional analysis of this synthesis reveals that the strategy amounts to the appendage of a twocarbon side chain to a pair of electrophiles (74). C-1 is engaged in the first ring forming step at the aldehyde oxidation state and C-5 as the mesylate in the second ring forming step. A logistical alternative would be to form the first ring by displacement at C-5 and then form the second ring by displacement at C-1. This seemingly trivial modification resulted in unexpected results.
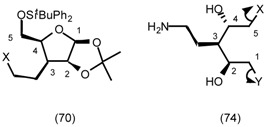
The C-5 hydroxyl group was unmasked by cleavage of the silyl ether and converted to the mesylate. Reduction of the azide, intramolecular nucleophilic displacement and protection yielded the tricycle (75). Cleavage of the sugar ring yielded the triol (76a), which was selectively mesylated at the primary hydroxyl group which was formerly C-1 of the sugar. Hydrogenolysis of the carbobenzyloxy group gave the tetrahydrofuran (77) as the major product in an inseparable mixture with the desired quinuclidine (73). This result is in stark contrast to the cyclisation of the epimeric alcohol (72b) which exclusively gave the quinuclidine (73). Direct protection of the diol (76b) as the bis(benzyl ether) (79) was not possible and an alternative more circuitous route via the dithioacetal (78) had to be employed [96,97].
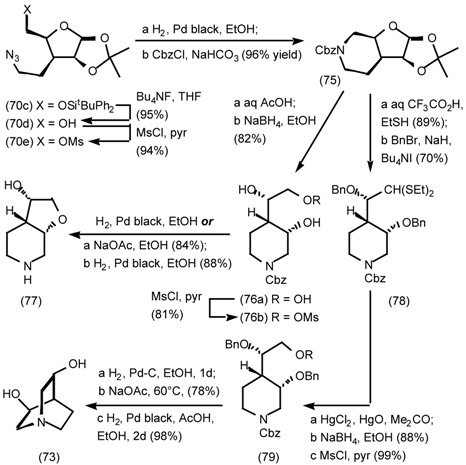
Similar methodology was also employed in the synthesis of (S)-quinuclidinol [98,99] and the meso-compound, (3R*,5S*)-quinuclidin-3,5-diol [100]. In each case in the second ring closure where a hydroxy group was orientated cis to the side-chain bearing a terminal mesylate [cf (70b)], tetrahydrofuran formation was faster than quinuclidine formation, whereas when they were orientated trans [cf (72)] quinuclidines were formed exclusively.
In most syntheses of 1-aza-norbornanes a piperidine ring is constructed first and the ring system is completed by cyclising the “one carbon bridge”. This approach benefits from the rich chemistry of pyridines and the ease by which they can be reduced to piperidines. The following two syntheses utilise the alternative approach in which a two carbon bridge is constructed between positions 1 and 3 of a pyrrolidine.
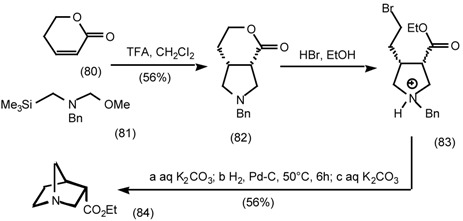
Treatment of N-benzyl-N-(methoxymethyl)-N-[(trimethylsilyl)methyl]amine (81) with trifluoroacetic acid generates an iminium ylide [101] which undergoes 1,3-dipolar cycloaddition to the unsaturated pyrone (80). Cleavage of the lactone ring with hydrogen bromide in ethanol, gives the bromoester (83) which upon treatment with base cyclises and benzyl group hydrogenolysis gives the endo-ester (84) [102,103]. The same cycloaddition to 3-exo-methylene-butyrolactone provides access to 4-substituted 1-aza-norbornanes [104,105].
1,2,4-oxadiazoles have long been used as metabolically stable analogues of carboxylic acids, esters [106] and amides [107], but it is less widely appreciated that an alkyl group at C-5 has acidic properties which are comparable to an ester. The trimethylammonium salt (87b) was conceived as a minimalist analogue of the muscarinic receptor “super agonist”, L-690,548 (91) [108]. The heterocycle (87a) was constructed by conventional means and methylated to give the trimethylammonium salt (87b). At pH 7.4 in water this had a half life of only 45 minutes and treatment with mild base enabled the alkene (88) to be isolated. This suggested that the trimethylammonium compound (87b) might be usable as an electrophilic synthon for substituted 5-ethyl-1,2,4-oxadiazoles. Treatment with a range of nucleophiles under basic conditions enabled the preparation of sundry amines, the benzyl thioether (87c) and the ether (87d). Substitution with 3-hydroxypyrrolidine (89), mesylation, treatment with potassium tamyloxide to give the α-1,2,4-oxadiazole anion and intramolecular nucleophilic substitution expeditiously yielded L-670,548 (91) in 21% yield for the entire sequence [109]. The exo:endo ratio (86:14) is probably not a function of the orientation of the mesylate group, because in another synthesis of this target a 90:10 ratio was observed also under basic conditions [110]. Hence the ratio reflects a thermodynamic mixture formed by equilibration of the α-1,2,4-oxadiazole anion.
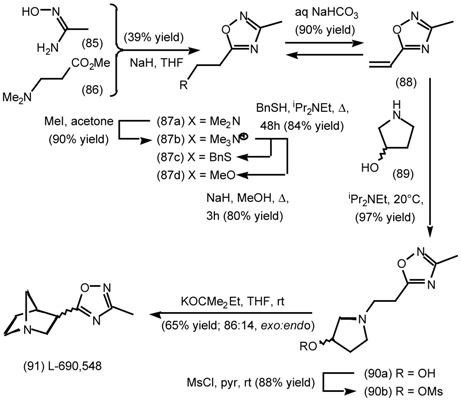
5.3.2 Dieckmann Condensation
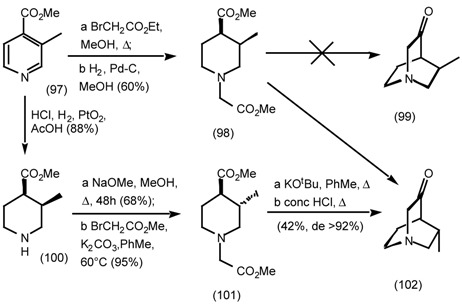
In work described as the synthesis of “spasmolytically active esters” quinuclidone (41b) was prepared by a Dieckmann condensation (intramolecular Claisen condensation). The carbon skeleton was assembled by alkylation of methyl isonicotinate (92) with ethyl bromoacetate, which facilitated reduction to the piperidine (93). The cyclisation was achieved using molten potassium in toluene which was reported to give superior yields to sodium [111]. This sequence was repeated using potassium ethoxide as the base for the Dieckmann cyclisation [112] and extended to the ester (96), by formation of the cyanohydrin (94), methanolysis to the α-hydroxyester and elimination to the alkene which was hydrogenated [113].
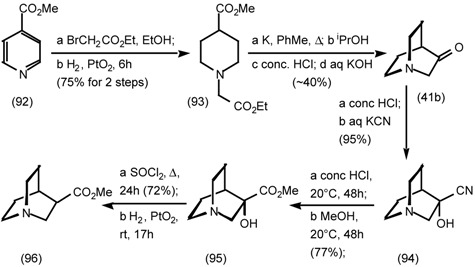
The methyl derivatives (98) (101) gave an unexpected result. The cis-isomer (98) was prepared as above and the trans-isomer (101) by base catalysed epimerisation. The structure (101) depicted in the scheme is the enantiomer of the epimer produced by epimerisation of the cis-methyl ester (100). This enables the products (99) (102) to be compared more easily. Treatment of both the cis- and trans-isomers (98) (101) with base gave almost exclusively the anti-methyl-quinuclidinone (102) (>96%). This presumably indicates that cyclisation syn to the methyl group is disfavoured, although this does not preclude a rationalisation in which deprotonation adjacent to the 4-ester group is faster for both stereoisomers than cyclisation [114].
The hydrogenation of pyrroles is much more difficult than that of pyridines, consequently a different approach must be used for the synthesis of 1-aza-norbornan-3-one (41a). Methyl glycinate (104) presumably undergoes sequential Michael addition and acylation with dimethyl itaconate (103) to give the 2-pyrrolidinone (105). The alternative sequence consisting of acylation followed by cyclisation would require a disfavoured 5-endo-trig Michael addition. Interestingly the diester (105) did not undergo Dieckmann cyclisation presumably because of the rigidity imparted by amide resonance. Selective reduction of the amide in the presence of a pair of esters gave the pyrrolidine analogue (106) of the piperidine (93) which underwent Dieckmann cyclisation in slightly better yield. The ketone (41a) was homologated to the corresponding exo-ester (109) by Peterson olefination with the anion derived from 2-trimethylsilyl-1,3-dithiane (107) and methanolysis [115,116].
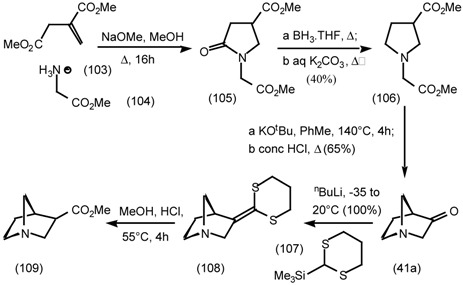
The use of a directed elimination is essential for this homologation as the following sequence illustrates. Formation of the cyanohydrin (110), hydrolysis and esterification gave the hydroxy-ester (111) in a sequence [(94)(95)] identical to that employed for quinuclidinone (41b). However treatment of the exo-alcohol (111) with diethylaminosulfur trifluoride (DAST) gave the nortricyclene (112) in 76% yield via the norbornyl cation The endo-alcohol (111) gave the same product in 40% yield. This of course results from the better overlap of the 4,5 carbon-carbon bond with the anti-bonding orbital of the departing sulfur trifluoride derivative when it is in the exo-position.
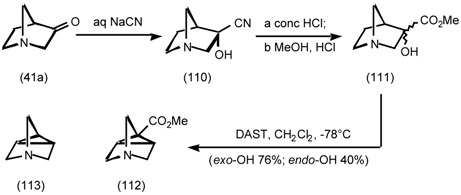
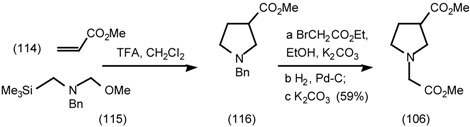
The pKa’s for quinuclidine, 1-azanorbornane and 4-azatricyclo[2.2.1.02,6]heptane (113) are 10.8, 10.5 and 9.0, respectively. Ring strain increases the p-orbital composition of the intra-annular bonds, which increases the propensity to accept electron density from the lone pair [117]. These comparatively small differences in pKa’s have a big impact on penetration of the blood-brain barrier, which rejects quarternary ammonium salts. The diester (106) has also been prepared by 1,3-dipolar cycloaddition to methyl acrylate (114), alkylation by ethyl bromoacetate and benzylic hydrogenolysis [118].
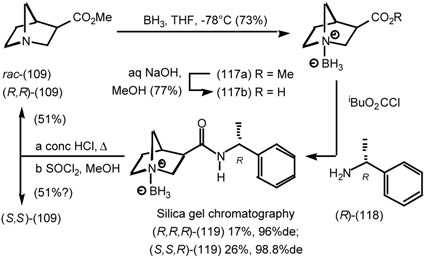
Enantiomerically pure ketone (41a) and ester (109) have been prepared in two ways. Racemic 1- aza-norbornan-3-ol (49) was resolved by crystallisation of the tartaric acid salts and Swern oxidation gave the ketones (41a) which were homologated to the esters (109) by the Peterson dithiane sequence described above. The absolute configurations were determined from circular dichroism spectra and measurements of X-ray crystallographic anomalous dispersion [119]. The ester (109) has also been resolved by column chromatography of the diastereomeric carboxamides (119) and the absolute configuration determined by X-ray crystallography. Protection of the tertiary amine as a borane complex was required to prevent decomposition during purification and remarkably this survived alkaline hydrolysis and mixed anhydride formation. It was ultimately cleaved by refluxing in concentrated hydrochloric acid [120]!
5.3.3 Ester Surrogates
Work at the Merck Neuroscience centre in the UK directed towards developing 1,2,4-oxadiazole derivatives of 1-aza-norbornanes (120) and quinuclidines (121) resulted in some extremely potent compounds. Some of these compounds have been reported earlier in this review (cf. Central nervous system). Their structures are repeated here for convenience.
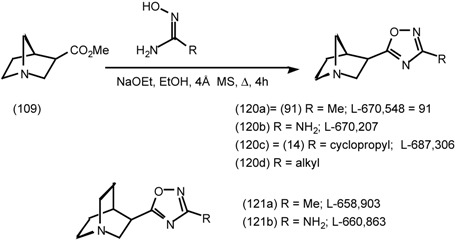
All four stereoisomers of the 3-methyl-1,2,4-oxadiazole (91 = 120a) were prepared individually using the borane carboxamide resolution described above, plus base catalysed epimerisation to access the endo-diastereoisomers. Both of the exo-diastereoisomers had identical predicted cortical efficacy and were full agonists at the muscarinic receptor based on the displacement of [3H]-oxotremorine-M and [3H]-scopolamine. Moreover the (3R,4R)-exo-stereoisomer (91 = 120a, actual structure depicted) had a ten fold higher affinity. The exo-stereoisomers were full agonists at M1, M2 and M3 receptors in three tissue preparations and the (3R,4R)-exo-stereoisomer (91 = 120a) had some potency selectivity for the M2/M3 receptors over M1 [121]. It also had excellent brain penetration; 3.8 % of the administered dose entered the CNS, which is comparable to the percentage of the weight of the mouse brain relative to body weight (2-5%) Increasing the hydrogen bonding capability of the 1,2,4- oxadiazole by replacing methyl with amino (120b) improved the efficacy by increased binding to the agonist state of the receptor, but this was offset by a reduction in CNS penetration (0.24%). The 1-azanorbornanes (120a,b) and the quinuclidines (121a,b) had up to a 1000 fold higher affinity than arecoline (33b). They also produced peripherally mediated salivation and centrally mediated hypothermia at doses 50-50,00 fold lower than arecoline (33b). The methyl derivative (91 = 120a) is particularly noteworthy, it produced hypothermia at does of 0.0016mg/Kg making it one of the most potent CNS active muscarinic agonists known [121,122]. These properties make these compounds useful research tools, but are the exact opposite of those required for treating conditions such as Alzheimer’s disease.
In general for these compounds as the size of the 3-substituent on the 1,2,4-oxadiazole ring (120d) increases, the efficacy decreases and 3-alkyl chains which are longer than n-propyl confer antagonist properties. The cyclopropyl derivative (14 = 120c) only has limited selectivity in binding assays, but is a partial agonist in M1 and an antagonist in M2 and M3 tissue assays [123,124]. In tissues with a large receptor reserve a partial agonist is sufficient to elicit maximal effects and is more likely to be show receptor selectivity and hence minimise side effects. This prompted a search for compounds with lower efficacy.
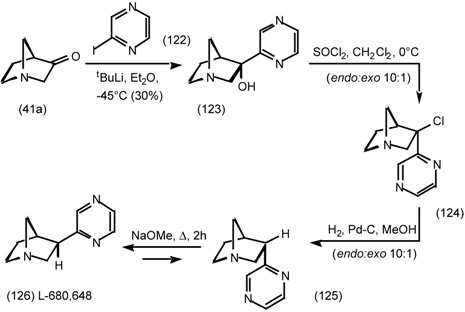
The pyrazine, L-680,648 (126) was assembled by fairly standard methodology. In this case substitution of the hydroxyl group does not result in elimination or non-classical norbornyl cation type rearrangements, because the hydroxyl group is in the endo-position and carbonium character is stabilised by the pyrazine ring. The endo-adduct (125) was easily epimerised to the exo-adduct (126) by base treatment, due to stabilisation of the carbanion by the pyrazine ring. The pyrazine (126) had an affinity and predicted cortical muscarinic efficacy comparable to that of the extremely potent 3-amino- 1,2,4-oxadiazole (120b). In general quinuclidines have lower muscarinic activity than the corresponding 1-azanorbornanes. Amongst a huge range of compounds the chloropyrazine emerged as a ligand with useful properties and was prepared via two routes.
The enolate of the ester (96) was alkylated by 2,6-dichloropyrazine (127) and decarboxylated by treatment with conc hydrochloric acid. Presumably the proximal nitrogen acts in the same way as a ketone in a β-ketoacid and the reaction goes via an enamine [125,126]. This procedure was deemed impractical on a large scale due to the high costs of the quinuclidine derivative (96) and the low temperature for the alkylation.
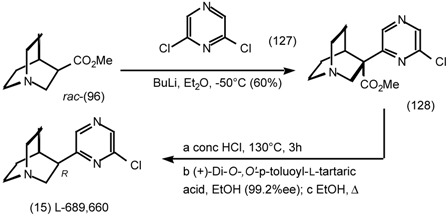
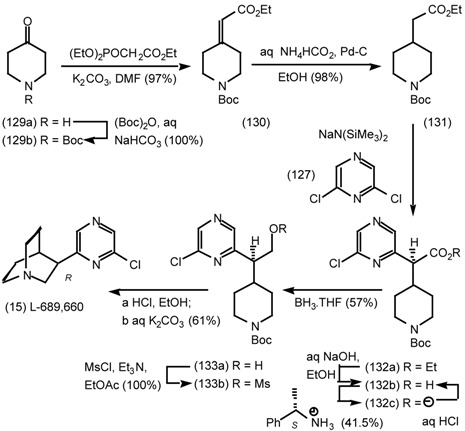
In the second, more practical synthesis, 4-piperidone (129a) was protected and converted to the α,β-unsaturated ester (130) by reaction with a Horner-Wittig reagent. Alkylation of the ester enolate with 2,6-dichloropyrazine (127) completed the carbon skeleton and the ester was hydrolysed to the acid to enable resolution with α-methylbenzylamine. Reduction of the enantiomerically pure acid (132b) to the alcohol (133a) with borane-tetrahydrofuran complex, mesylation and cleavage of the tbutoxycarbonyl group revealed the amine, which displaced the mesylate to give the chloropyrazine, L- 689,660 (15) [127].
L-689,660 showed no muscarinic receptor subtype selectivity in binding assays, but in pharmacological tissue assays it was a potent M1 and M3 agonist and a M2 antagonist [128]. This selectivity is presumably due to the low intrinsic activity that confers the ability to exploit differences in effective receptor reserve. It was capable of crossing the brain-blood barrier and was active in several rat behavioural studies. For example it reversed a scopolamine (11) induced performance deficit [129].
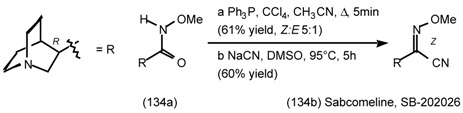
As noted above oxime derivatives of arecoline (35) (36) are potent agonists. Similarly the imidoyl nitrile, sabcomeline, SB 202026 (134b) is a highly potent muscarinic partial agonist that exhibits functional selectivity for effects mediated by M1 receptors [130].
The preparation was very simple. The N-methoxycarboxamide (134a) was converted to the imidoyl chloride which was substituted by cyanide to give a 5:1 mixture of E:Z geometric isomers which were separated by column chromatography. The (Z)-stereoisomer was resolved by sequential salt formation with (R)-(-)- and (S)-(+)-1,1'-binaphthyl-2,2'-diyl hydrogen phosphate and the absolute configuration determined using X-ray crystallographic anomalous dispersion measurements [131,132]. Sabcomeline (134b) caused a significant improvement in a visual object discrimination task in non-cognitively impaired marmosets without side effects [133] and improved performance in a maze task by rats [134]. It is currently in phase III clinical trials
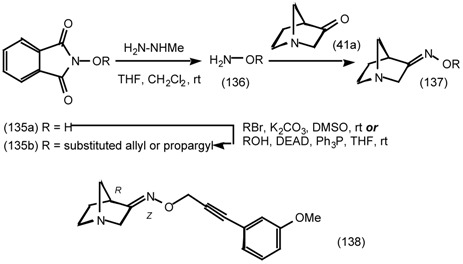
The propargyl oximes (137b) provide a neat solution to the problem of maintaining agonist activity whilst adding functionality to obtain selectivity The functional group is placed at the end of a long alkyne boom so that it does not interfere with critical receptor binding, but can interact selectively with other portions of the receptor. O-Substituted hydroxylamines were prepared by conventional alkylation of N-hydroxyphthalimide (135a) with allyl and propargyl bromides or by a Mitsunobu type displacement of the corresponding alcohols [135], followed by N-methylhydrazine cleavage of the imide.
The oximes were formed as a mixture of (Z) and (E)-stereoisomers, which were separated by HPLC [136,137,138]. The (E)-isomers had weak or no muscarinic activity compared to the (Z)-isomers and the most selective compound was the (R)-enantiomer of the 3'-methoxyphenylpropargyl derivative (138) (CI-1017), which had good selectivity for m1 receptors over m2 [139].
6 Muscarinic Antagonists
Muscarinic antagonists are generally bulkier molecules than agonists and they embrace a much wider range of chemical structures. A tertiary amine is more or less obligatory and most contain an aromatic moiety, but classification within these broad boundaries is difficult. Consequently within this section methods of synthesis and metabolism are exemplified rather than SARs.
6.1 Enantioselective Synthesis of Tertiary Centres; Tolterodine, Rociverine, IQNP
Tolterodine (27a) is a fast acting treatment for urge incontinence(UI, see Urinary bladder) [140]. It inhibits urinary bladder contraction, without inhibiting salivation, a phenomena which cannot be explained in terms of selectivity for a single muscarinic receptor subtype [141] (cf. Urinary Bladder). In mice, dogs and humans the predominant metabolic pathway for tolterodine is hydroxylation of the 5- methyl group by CYP2D6 (cytochrome P450 2D6)[142], followed by oxidation to the aldehyde and carboxylic acid. N-dealkylation by CYP3A was a minor pathway [143].
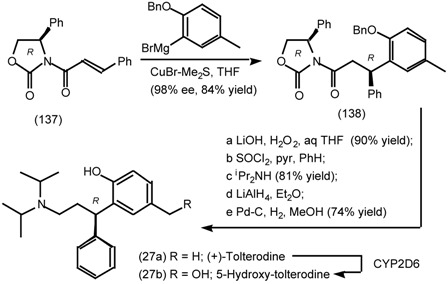
5-Hydroxy-tolterodine (27b) has a similar pharmacological activity to that of the parent compound [144,145] and hence CYP2D6 polymorphism has little effect on the anti-muscarinic activity [146]. Tolterodine (27a) and 5-hydroxy-tolterodine (27b) were detected at the pM to nM level in plasma by capillary LC-MS with a sheathless electrospray source [147,148].
An asymmetric synthesis of Tolterodine (27a) utilises conjugate addition [149] of an aryl cuprate to an Evans' [150] N-cinnamoyl oxazolidinone (137). A range of stereodirecting groups were surveyed and although some gave marginally better stereoselectivity and yields (eg cis-4,5-diisopropyl and cis- 4,5-diphenyl), the commercial (4S)-oxazolidonine derived from (R)-phenylglycine (137) proved to be the most practical alternative [151].
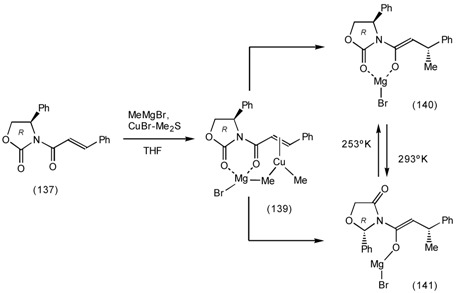
A NMR investigation of this mechanism of the conjugate addition has revealed three intermediates. The first is a π-complex of the cuprate reagent with the alkene (139) in which the two methyl groups can be distinguished. After methyl transfer two rotomers are present. The coordinated enolate (140) is more stable at lower temperatures, whereas the non-coordinated enolate (141) is formed at higher temperatures, which has a substantial effect on the stereoselectivity of reactions with electrophiles [152].
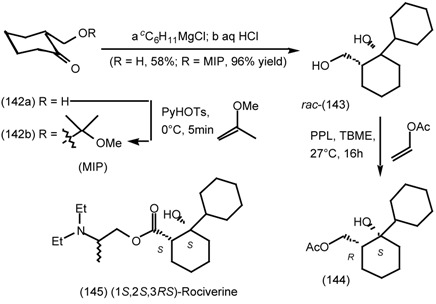
Rociverine (RilatenTM) (145) is a useful antispasmodic with neurotropic and myotropic properties used to treat urge incontinence and nocturia in the elderly. Commercial rociverine is a mixture of four diastereoisomers with a cis-relationship between the hydroxy and carboxylic substituents on the cyclohexane ring. The cis-(1S,2S)-diastereoisomers have high selectivity for binding to m1 receptors, whilst the cis-(1R,2R)-diastereoisomers are the most potent for all receptor (m1-m5) sub-types [153]. A dicyclohexyl carboxylic acid synthon was assembled by Grignard addition and resolved using a lipase. Addition of cyclohexylmagnesium chloride to 2-hydroxymethylcyclohexanone (142a) gave a mixture of cis- and trans-diols (ratio 55:45) in poor yield. In contrast the methoxy-isopropyl acetal (142b) gave exclusively the cis-isomer in excellent yield, with the protecting group being removed during work-up. The hydrophobic diol rac-(143) was resolved by pig pancreatic lipase (PPL) catalysed trans-acylation with vinyl acetate in t-butyl methyl ether [154]. This reaction is irreversible because the vinyl alcohol readily isomerises to acetaldehyde, however it slowly deactivates enzymes by reaction with basic amino acids such as lysine. At 72% conversion the enantiomeric excess of the residual diol was maximised (1R,2S-143, 85%ee), whereas at 28% conversion the enantiomeric excess of the monoacetate was maximised (144, 78%ee) [155] at the expense of poor yields in both cases. Consequently in subsequent work, the rociverine (145) was resolved by diastereomeric salt formation with tartaric or di-O-benzoyl-tartaric acid [156].
The imaging of the location of muscarinic receptors is a rapidly developing field [157]. Older techniques such as autoradiography are in many cases being supplanted by positron emission tomography (PET) [158,159] and single photon emission computed tomography (SPECT) [160,161,162]. These techniques rely on ligands [163] which bear radiolabels with a short half-life (eg 11C, 18F [164], 76Br, 99mTc or 123I). Consequently not only must the ligand be able to bind to the receptor selectively, but it must have a precursor which can be used to attach the radiolabel quickly, in high radiochemical yield and with minimum purification. For example, the substitution of vinylstannanes by iodine-123 (or 125I) has emerged as a standard technique, because it can be accomplished in just 5 minutes [165].
The iodoalkene IQNP (151b) has been developed as a SPECT imaging agent modelled on quinuclidinyl benzilate. It localises in the brain at the sites of Ach receptors and has some selectivity for the muscarinic receptor subtypes.
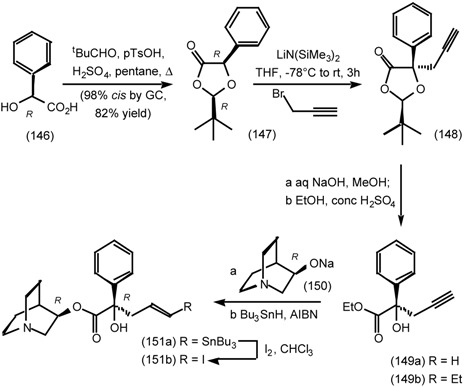
An enantioselective synthesis has been developed using Seebach's 1,3-dioxolanone method for the α-alkylation of α-hydroxyl-carboxylic acids [166]. Condensation of pivaldehyde and (S)-mandelic acid, remarkably gives predominantly the cis-diastereoisomer (147). Deprotonation destroys the original stereocentre of the mandelic acid, but the t-butyl group attached to the acetal directs alkylation of the enolate to the other face to give the propargyl derivative (148). Overall this amounts to alkylation with retention of configuration [167]. The carboxylic acid (149b) has also been resolved via the α-methylbenzylamine salt [168]. The (E,3R,1'R)-stereoisomer (151b) binds selectively to the m1 receptor subtype, whereas the (Z,3R,1'R)-stereoisomer binds to both m1 and m2 receptor subtypes [169].
6.2 Diels-Alder Reactions
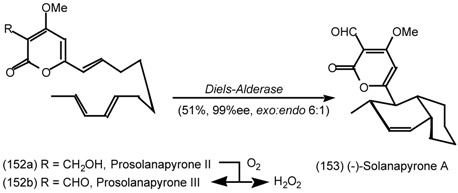
One of the holy grails of enzymology is the determination of the structure of an enzyme capable of catalysing Diels-Alder reactions [170]. Recently two cell free fractions from Alternaria solani have been purified [171], which are capable of converting prosolanapyrone II (152a) to solanapyrones A (153) and D [172], which can be rationalised as an oxidation followed by an intramolecular Diels- Alder reaction [173,174]. In this section the application of Diels-Alder reactions in the synthesis of muscarinics will be discussed, with particular emphasis on biomimetic Diels-Alder reactions.
6.2.1 Indole Alkaloids; Allosteric Activators of Muscarinic Binding
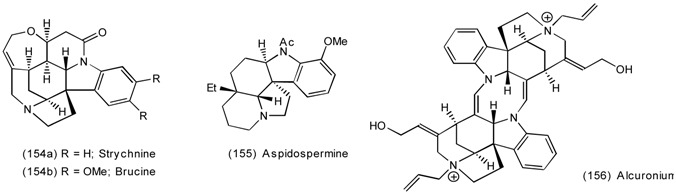
Several naturally occuring indole alkaloids eg (154a) [175], (154b), (155), (156) [176] bind to the five muscarinic receptor subtypes at allosteric sites. The binding of ligands at these sites increases or decreases the binding of other ligands to the receptor. For example, brucine (154b) increases the affinity of Ach (1a) about two fold at m1 receptors, N-chloromethyl-brucine three fold at m3 receptors and brucine N-oxide 1.5 fold at m4 receptors [177]. Compounds with this activity would be valuable in conditions such as Alzheimer's disease where Ach levels are decreased. Clearly strychnine (154a) is an unlikely candidate as a medicinal entity! Lead compounds have the ring system of aspidospermine (155) minus the bis(methylene)-bridge, plus the δ-lactam ring of strychnine (154a) and brucine (154b). The Diels-Alder precursor (157) was prepared by condensation of N-benzylpiperidone with indole, followed by acylation and conversion to the salt with hydrochloric acid.
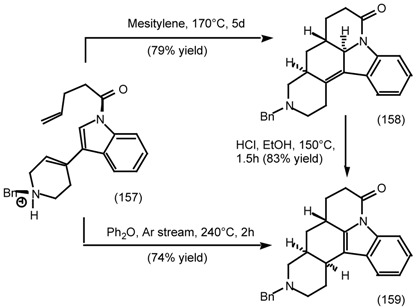
The diene component (157) is slightly electron rich, whereas the dienophile is unactivated, consequently high temperatures were required to effect cycloaddition. The initial adduct (158) with a trans, trans-relationship between the bridgehead hydrogens was isolated after heating at 170°C for 5 days. Treatment with acid caused an overall [1,3]-hydrogen shift to give the indole (159), which could also be accessed directly by cycloaddition-rearrangement at 240°C for 2 hours in a flow of argon. These cycloadditions were run in open vessels or in a gas flow as indicated, so that the initial hydrochloride salts were converted to the free amine substrate and/or product during the course of the reaction.
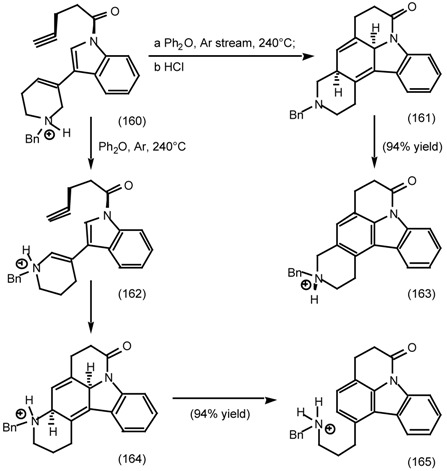
The crucial role of these conditions was demonstrated in the cycloaddition of the acetylenic diene (160). When this was performed under a stream of argon the expected adduct (161) underwent 1,4- elimination of hydrogen to give the piperidyl carbazole (163). Whereas under a static atmosphere of argon, acid catalysed shift of the alkene bond gave the thermodynamically more stable enamine, which underwent cycloaddition to give the 1,4-dihydrobenzene (164) and aromatisation by 1,4-elimination of the protonated amine to give the 3-aminopropyl carbazole (165) [178,179].
6.2.2 Himbacine; A Muscarinic Antagonist with Allosteric Properties
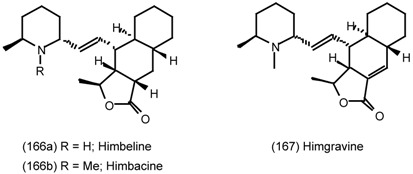
Himbacine (166b) was first isolated from the bark of the Australian pine tree, Galbulimima (Himantandra) baccata FM Bail in 1956. It has low toxicity and was initially used as an anti-spasmodic agent. It is a selective antagonist for the M2 and M4 muscarinic receptor sites [180] with allosteric properties [181,182], which has led to proposals for its use in the treatment of Alzheimer's disease [183] (cf. 2.6 Central nervous system for the mechanism). Analogue studies have shown that removal of the carbonyl group reduces the selectivity for M2 receptor types 20-fold [184], whereas replacement of the tricyclic moiety by dihydroanthracene increases the affinity for both M1 and M2 receptor types [185].
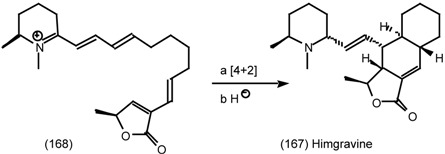
Baldwin has proposed that the dehydrodecalin rings of himgravine (167) are assembled biosynthetically by an endo-selective intramolecular Diels-Alder cycloaddition of the tetraene imminium salt (168) followed by reduction. A second reduction would then yield himbacine (166b).
Making a more pragmatic analysis; most synthetic routes to himbacine have utilised an intramolecular Diels-Alder reaction which yields a progenitor of the exocyclic alkene bond. This approach has the potential to correctly install five contiguous chiral centres directed solely by the C-11 methyl group. However contrary to this favourable prognostication, the cycloaddition of (E,E,E)-1,3,9- decatrienes frequently occurs with low stereoselectivity, although this problem can be mitigated by an electron withdrawing group attached to the dienophile.
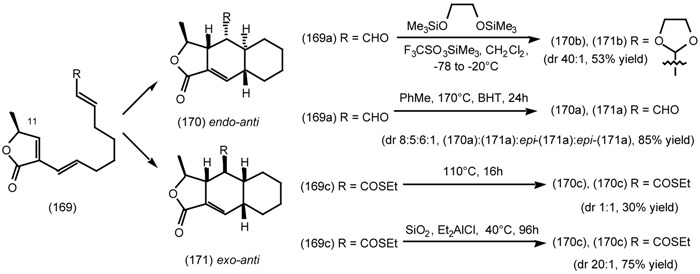
Treatment of the aldehyde (169a) with bis(O-trimethylsilyl)ethane diol and trimethylsilyl triflate gave the corresponding acetal which under the acidic conditions gave the corresponding oxonium ion analogous to the iminium ion postulated in the biosynthetic sequence. In situ Diels-Alder cycloaddition then gave the desired product (170b) with excellent stereoselectivity. Evidence for the intermediacy of the oxonium ion was provided by experiments in which treatment of the isolated acetal with trimethylsilyl triflate gave the same product, whilst treatment of the aldehyde (169a) with trimethylsilyl triflate gave a mixture of three isomers [186]. In contrast thermal Diels-Alder cycloaddition of the aldehyde (169a) required heating at 170°C and a mixture of four diastereoisomers were produced [187,188]. Similarly thermal cycloaddition of the triene (169c) gave an equal mixture of the two diastereoisomers (170c,171c) in low yield whereas the acid catalysed reaction gave predominantly the desired endo-anti-stereoisomer (170c) [189,190].
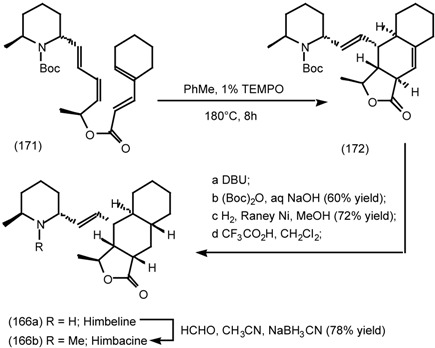
In a bold strategy, the tetraene (171) underwent an exo-selective Diels-Alder reaction to generate the "central" cyclohexane. The stereochemistry adjacent to the carbonyl group was corrected by treatment with base which also caused partial cleavage of the t-butoxycarbonyl protecting group. Reprotection and hydrogenation effected reduction of the endocyclic alkene bond without affecting the sterically encumbered exocyclic alkene bond. Acidic deprotection yielded himbeline (166a) and reductive methylation himbacine (166b) in 11 steps and a remarkable overall yield of 9.7% from (S)-2- methylpiperidine L-tartrate [191].
6.2.3 Cyclostellettamines; Macrocyclic Muscarinic Antagonists
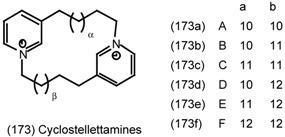
Some thirty 3-alkylated-polypyridines have been isolated from marine sponges (order Haplosclerida) [192,193]. Many of these are potent anti-bacterials and cytotoxins. The cyclostellettamines (173a-f) are bispyridinium macrocycles isolated from the marine sponge Stelletta maxima, which block the binding of [3H]-methyl quinuclidinyl benzilate to M1 (rat brain), M2 (rat heart) and M3 (rat salivary gland) receptors [194]. It has been postulated that manzamines A and B are formed biosynthetically by intramolecular Diels-Alder reaction of compounds related to the cyclostellettamines which have a 2,3-dihydropyridinium ring (acting as the diene component) and alkene groups in the linking carbon chains [195]. This proposal was validated in vitro by the biomimetic synthesis of kermaphidin B, albeit the Diels-Alder reaction only gave a minuscule yield (0.2-0.3%) [196]. The work described below may be regarded as a prelude to a thorough testing of the biosynthetic Diels-Alder proposal.
The synthesis of 32-36-membered rings can at the very least be described as demanding! Base treatment of the hydrochloride salt (174a, n = 7) resulted in nucleophilic addition to the pyridinium ring to give a bis-Zincke salt which upon thermolysis yielded the 20-membered bis-pyridinium macrocycle (177). However application of this methodology to the homologue (174b, n = 13) resulted in exclusive formation of the product of intramolecular attack (176) and larger rings could only be prepared by sequential alkylation [197].
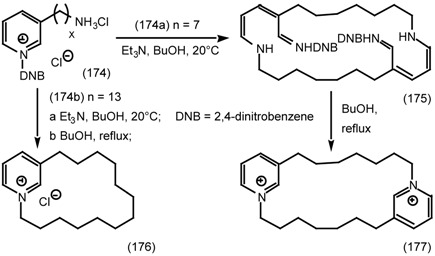
The complete set of natural cyclostellettamines (173a-f) were prepared by stepwise pyridine alkylation using a pyridinium N-oxide (178) and a hydroxyl group (179) as "protective groups". They were converted to the pyridine and an alkyl bromide (181) in a single step by treatment with phosphorus tribromide [198]. A comparable approach was used by Wanner and Koomen except that the pyridine was protected by a p-methoxy-benzyl group [199].
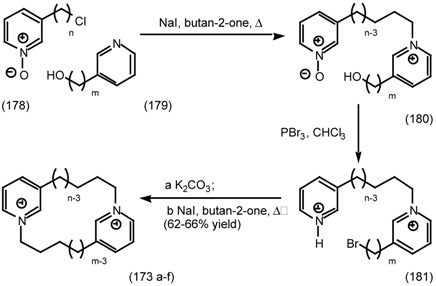
In the final synthesis of cyclostellettamines, Wittig reactions were used to append the hydrocarbon side chains, which resulted in an exercise in selective reduction and benzyl ether cleavage. The alkene bonds were reduced by catalytic hydrogenation without reduction of the pyridine (cf. 183) or pyridinium rings or cleavage of the benzylic ether (cf. 185). Cleavage of the benzyl ether (185) by catalytic hydrogenation was precluded by the pyridinium ring, however treatment with trifluoromethanesulfonic acid and trimethylsilyl iodide furnished the desired alcohol in 48% yield. Sulfonate ester formation and cyclisation under high dilution conditions (0.5mM) furnished cyclostellettamine C in good yield [200].
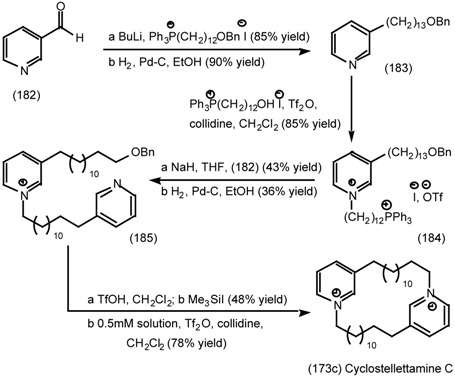
7 Conclusions and Future Prospects
The identification and cloning of the muscarinic receptor subtypes was celebrated as the great advance that would transform the study of muscarinics. However, thus far it has not proved possible to prepare small ligands with sufficient selectivity to distinguish between them and achieve therapeutic benefits. The paradigm of seeking partial agonists and exploiting effective receptor reserve has proved to be more effective for producing therapeutically useful compounds. Albeit significant advances are still required to effectively treat conditions such as Alzheimer's disease. Whereas a whole family of peptide muscarinic (MTs) and other toxins have been isolated from the venom of the African green mamba, Dendroapsis augusticeps [201,202] which have extra-ordinary selectivity. The five to six fold selectivity of pirenzepine (5) for m1 and tripitramine for m2 receptor subtypes is dwarfed by the 214 fold higher affinity of MT3 for m4 receptors over m1 and it has no significant binding to m2, m3 or m5 receptor subtypes [203]. Similarly M1-toxin is capable of blocking m1 receptors without affecting m2- m5 [204] and 125I- labelled M1-toxin has been used to visualise the distribution of M1 sites in the brain [205].
Millions of years of evolution constitutes the ultimate combinatorial laboratory. Nature continues to provide novel muscarinics such as martinelline (used as an eye medication in South America) [206], distantly related to the guanidino-derivatives (187) and novel polycyclic amines such as the TAN1251's (188) [207]. No doubt these will provide leads for new classes of muscarinics.
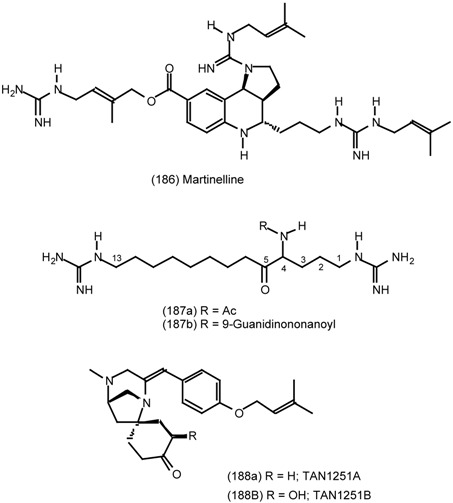
Postscript added in proof, Developments in Drugs for Alzheimer’s Disease (23rd January 2001):
The National Institute for Clinical Excellence (NICE) in the United Kingdom announced on the 19th January 2001 that three drugs: donepezil (Aricept), rivastigmine (Exelon) and galantamine (Reminyl), should be prescribed for patients with mild and moderate forms of Alzheimer’s disease. However, NICE has ruled that these drugs should not be made available by the National Health Service to patients with more advanced symptoms because of a lack of proven clinical benefits (http://news.bbc.co.uk/hi/english/health/newsid_1124000/1124794.stm). All three drugs are cholinesterase inhibitors. Tacrine (13) which is also a cholinesterase inhibitor was the first drug approved by the FDA (1993) for treating Alzheimer’s disease, but its use is decreasing in favour of donepezil (approved 1996), which has a similar but more selective mode of action and hence has fewer side effects. Moreover tacrine has a half life in the body of only 1.4 to 3.6 hours and hence has to be given four times a day. In contrast, donepezil has a half life of 70 hours and a single daily dose is sufficient.
Muscarinic agonists have fared less well. Sabcomeline (134b), milameline or RU 35926 (35b) and physostigmine (12a) are all no longer in development. The oral formulation of xanomeline (34) has also been withdrawn, but the skin patch continues in development. In most cases drugs these have been withdrawn during phase III trials due to poor efficacy or side effects. It remains to be seen if sufficient selective M1 agonist activity can be achieved without unacceptable side effects, whereas selectivity for neuronal Ach esterase as opposed to peripheral non-neuronal butyrylcholinesterase appears to be more easily attainable.
Footnotes
Sample Availability: Not applicable.
8 References
- 1.Broadley K. J. Autonomic Pharmacology. Taylor & Francis; London: 1996. [Google Scholar]
- 2.Starke K., Gothert M., Kilbinger H. Physiol. Rev. 1989;69:864–989. doi: 10.1152/physrev.1989.69.3.864. [DOI] [PubMed] [Google Scholar]
- 3.Newberry N. R., Priestley T. Br. J. Pharmacol. 1987;92:817–826. doi: 10.1111/j.1476-5381.1987.tb11386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hammer R., Berrie C. P., Birdsall N. J. M., Burgen A. S. V., Hulme E. C. Nature. 1980;283:90–92. doi: 10.1038/283090a0. [DOI] [PubMed] [Google Scholar]
- 5.International Union of Pharmacology XVIII classification of muscarinic acetylcholine receptors, Caulfield M. P., Birdsall N. J. M. Pharmacol. Rev. 1998;50:279–290.
- 6.Reever C. M., Ferrari-DiLeo G., Flynn D. D. Life Sci. 1997;60:1105–1112. doi: 10.1016/S0024-3205(97)00054-4. [DOI] [PubMed] [Google Scholar]
- 7.Hulme E. C., Birdsall N. J. M., Buckley N. J. Annu. Rev. Pharmacol. Toxicol. 1990;30:633–673. doi: 10.1146/annurev.pa.30.040190.003221. [DOI] [PubMed] [Google Scholar]
- 8.Caulfield M. P. Pharmacol. Ther. 1993;58:319–379. doi: 10.1016/0163-7258(93)90027-b. [DOI] [PubMed] [Google Scholar]
- 9.Eglen R. M., Hegde S. S., Watson N. Pharmacol. Rev. 1996;48:531–565. [PubMed] [Google Scholar]
- 10.Urquhart R. A., Broadley K. J. Gen. Pharmacol. 1992;23:619–626. doi: 10.1016/0306-3623(92)90137-9. [DOI] [PubMed] [Google Scholar]
- 11.Sneddon P., Graham A. J. Auton. Pharmacol. 1992;12:445–456. doi: 10.1111/j.1474-8673.1992.tb00393.x. [DOI] [PubMed] [Google Scholar]
- 12.Eglen R. M., Whiting R. L. J. Auton. Pharmacol. 1990;10:233–245. doi: 10.1111/j.1474-8673.1990.tb00023.x. [DOI] [PubMed] [Google Scholar]
- 13.Kromer W., Eltze M. J. Auton. Pharmacol. 1991;11:337–342. doi: 10.1111/j.1474-8673.1991.tb00257.x. [DOI] [PubMed] [Google Scholar]
- 14.Goyal R. K. N. Engl. J. Med. 1989;321:1022–1029. doi: 10.1056/NEJM198910123211506. [DOI] [PubMed] [Google Scholar]
- 15.Alabaster V. A. Life Sci. 1997;60:1053–1060. doi: 10.1016/s0024-3205(97)00047-7. [DOI] [PubMed] [Google Scholar]
- 16.Howell R. E., Laemont K. D., Kovalsky M. P., Lowe V. C., Waid P. P., Kinnier W. J., Noronha-Blob L. J. Pharmacol. Exp. Ther. 1994;270:546–553. [PubMed] [Google Scholar]
- 17.Kaufman P. L., Weidman T., Robinson J. R. In: Pharmacology of the Eye. Handbook of Experimental Pharmacology. Sears M. L., editor. Spriger-Verlag; Berlin: 1984. pp. 149–191. [Google Scholar]
- 18.Growdon J. H. Life Sci. 1997;60:993–998. doi: 10.1016/s0024-3205(97)00039-8. [DOI] [PubMed] [Google Scholar]
- 19.Babic T., Smith R. J., Petravic D. Neurologia Croatica. 1997;46:55–72. [Google Scholar]
- 20.Wen G. Y. J. Food Drug. Anal. 1998;6:465–476. [Google Scholar]
- 21.Huff F. J., Mickel S. F., Corkin S., Growdon J. H. Drug Devel. Res. 1988;12:271–278. [Google Scholar]
- 22.Yankner B. A., Duffy K. L., Kirschner D. A. Science. 1990;250:279–282. doi: 10.1126/science.2218531. [DOI] [PubMed] [Google Scholar]
- 23.Hung A. Y., Haass C., Nitsch R. M., Qiu W. Q., Citron M., Wurtman R. J., Growdon J. H., Selkoe D.J. J. Biol. Chem. 1993;268:22959–22962. [PubMed] [Google Scholar]
- 24.Muller D. M., Mendla K., Farber S. A., Nitsch R. M. Life Sci. 1997;60:985–991. doi: 10.1016/s0024-3205(97)00038-6. [DOI] [PubMed] [Google Scholar]
- 25.Avery E. E., Baker L. D., Asthana S. Drugs & Aging. 1997;11:450–459. doi: 10.2165/00002512-199711060-00004. [DOI] [PubMed] [Google Scholar]
- 26.Unni L. K. CNS Drugs. 1998;10:447–460. [Google Scholar]
- 27.Weinstock M. Neurodegeneration. 1995;4:349–356. doi: 10.1006/neur.1995.0042. [DOI] [PubMed] [Google Scholar]
- 28.Giacobini E. Neurochem. Int. 1998;32:413–419. doi: 10.1016/s0197-0186(97)00124-1. [DOI] [PubMed] [Google Scholar]
- 29.Hunter A. J., Murray T. K., Jones J. A., Cross A. J., Green A. R. Br. J. Pharmacol. 1989;98:79–86. doi: 10.1111/j.1476-5381.1989.tb16865.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nordberg A., Svensson A. L. Drug Safety. 1998;19:465–480. doi: 10.2165/00002018-199819060-00004. [DOI] [PubMed] [Google Scholar]
- 31.Doods H. N., Quirion R., Mihm G., Engel W., Rudolf K., Entzeroth M., Schiavi G. B., Ladinsky H., Bechtel W. D., Ensinger H. A., Mendla K. D., Eberlein W. Life Sci. 1993;52:497–503. doi: 10.1016/0024-3205(93)90307-O. [DOI] [PubMed] [Google Scholar]
- 32.Baker R., Showell G. A., Street L. J., Saunders J., Hoogsteen K., Freedman S. B., Hargreaves J. J. Chem. Soc., Chem. Commun. 1992:817–819. doi: 10.1039/c39920000817. [DOI] [Google Scholar]
- 33.Street L. J., Baker R., Book T., Reeve A. J., Saunders J., Willson T., Marwood R. S., Patel S., Freedman S. B. J. Med. Chem. 1992;35:295–305. doi: 10.1021/jm00080a014. [DOI] [PubMed] [Google Scholar]
- 34.Baker R., Street L. J., Reeve A. J., Saunders J. J. Chem. Soc., Chem. Commun. 1991:760–762. doi: 10.1039/c39910000760. [DOI] [Google Scholar]
- 35.Hargreaves R. J., McKnight A. T., Scholey K., Newberry N. R., Street L. J., Hutson P. H., Semark J. E., Harley E. A., Patel S., Freedman S. B. Br. J. Pharmacol. 1992;107:494–501. doi: 10.1111/j.1476-5381.1992.tb12773.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Freedman S. B., Dawson G. R., Iversen L. L., Baker R., Hargreaves R. J. Life Sci. 1993;52:489–495. doi: 10.1016/0024-3205(93)90306-N. [DOI] [PubMed] [Google Scholar]
- 37.Ensinger H. A., Bechtel W. D., Birke F. W., Mendla K. D., Mierau J., Speck G., Troger W. Drug Devel. Res. 1997;40:144–157. doi: 10.1002/(SICI)1098-2299(199702)40:2<144::AID-DDR5>3.0.CO;2-L. [DOI] [Google Scholar]
- 38.Adamus W. S., Leonard J. P., Troger W. Life Sci. 1995;56:883–890. doi: 10.1016/0024-3205(95)00024-Z. [DOI] [PubMed] [Google Scholar]
- 39.Schulte B., Volz-Zang C., Mutschler E., Horne C., Palm D., Wellstein A., Pitschner H.F. Clin. Pharmacol. Ther. 1991;50:372–378. doi: 10.1038/clpt.1991.153. [DOI] [PubMed] [Google Scholar]
- 40.Eglen R. M., Watson N. Pharmacol. Toxicol. 1996;78:59–68. doi: 10.1111/j.1600-0773.1996.tb00181.x. [DOI] [PubMed] [Google Scholar]
- 41.Anerson K.-E. Drugs. 1988;35:477–494. [Google Scholar]
- 42.Langtry H. D., McTavish D. Drugs. 1990;40:748–761. doi: 10.2165/00003495-199040050-00008. [DOI] [PubMed] [Google Scholar]
- 43.Nilvebrannt L., Hallen B., Larsson G. Life Sci. 1997;60:1129–1136. doi: 10.1016/s0024-3205(97)00057-x. [DOI] [PubMed] [Google Scholar]
- 44.Oyasu H., Yamamoto T., Sato N., Ozaki R., Mukai T., Ozaki T., Nishii T., Sato H., Fujisawa T., Tozuka Z., Koibuchi Y., Honbo T., Esumi K., Ohtsuka M., Shimomura K. Arzneimittelforsch./Drug Res. 1994;44:1242–1249. [Google Scholar]
- 45.Barnes P. J. Life Sci. 1993;52:521–527. doi: 10.1016/0024-3205(93)90310-y. [DOI] [PubMed] [Google Scholar]
- 46.Gross N.J. In: Asthma: Basic Mechanisms and Clinical Management. 2nd Edn. Barnes P. J., Rodger I. W., Thomson N. C., editors. Academic Press; London: 1992. pp. 555–566. [Google Scholar]
- 47.Maesen F. P. V., Smeets J. J., Costongs M. A. L., Cornelissen P. J. G., Wald F. D. M. Eur. Resp. J. 1993;6:1031–1036. [PubMed] [Google Scholar]
- 48.Dail W.G. Nervous Control of the Urogenital System. In: Maggi C.A., editor. The Autonomic Nervous System. vol. 3. Harwood; Switzerland: 1993. pp. 69–101. [Google Scholar]
- 49.Ruggieri M. R., Colton M. D., Wang P., Wang J., Smyth R. J., Pontari M. A., Luthin G. R. J. Pharmacol. Exp. Ther. 1995;274:976–982. [PMC free article] [PubMed] [Google Scholar]
- 50.Caine M., Raz S., Zeigler M. Br. J. Urol. 1975;47:193–202. doi: 10.1111/j.1464-410X.1975.tb03947.x. [DOI] [PubMed] [Google Scholar]
- 51.Lau W. A. K., Pennefather J. N., Mitchelson F. Proc. Aust. Soc. Clin. Exp. Pharmacol. Toxicol. 1996;110 [Google Scholar]
- 52.Holdsworth D. K., Jones R. A., Self R. Phytochemistry. 1998;48:581–582. doi: 10.1016/S0031-9422(98)00016-8. [DOI] [Google Scholar]
- 53.Wang C. K., Lee W. H., Peng C. H. Agric. Biol. Chem. 1997;45:1185–1188. doi: 10.1021/jf960547q. [DOI] [Google Scholar]
- 54.Ref 1, p341.
- 55.Jeng J. H., Hahn L. J., Lin B. R., Hsieh C. C., Chan C. P., Chang M. C. J. Oral. Pathol. Med. 1999;28:64–71. doi: 10.1111/j.1600-0714.1999.tb01998.x. [DOI] [PubMed] [Google Scholar]
- 56.Sharan R. N. Cancer J. 1996;9:13–19. [Google Scholar]
- 57.Raffaele K. C., Berardi A., Morris P. P., Asthana S., Haxby J. V., Schapiro M. B., Rapoport S. I., Soncrant T. T. Prog. Neuro-Psychopharmacol. & Biol. Psychiatry. 1991;15:643–648. doi: 10.1016/0278-5846(91)90054-5. [DOI] [PubMed] [Google Scholar]
- 58.Raffaele K. C., Berardi A., Asthana S., Morris P., Haxby J. V., Soncrant T. T. Psychopharmacology Bull. 1991;27:315–319. [PubMed] [Google Scholar]
- 59.Raffaele K. C., Asthana S., Berardi A., Haxby J. V., Morris P. P., Schapiro M. B., Soncrant T. T. Neuropsychopharmacology. 1996;15:163–170. doi: 10.1016/0893-133X(95)00179-H. [DOI] [PubMed] [Google Scholar]
- 60.Soncrant T. T., Raffaele K. C., Asthana S., Berardi A., Morris P. P., Haxby J. V. Psychopharmacology. 1993;112:421–427. doi: 10.1007/BF02244889. [DOI] [PubMed] [Google Scholar]
- 61.Asthana S., Raffaele K. C., Greig N. H., Berardi A., Morris P. P., Schapiro M. B., Rapoport S. I., Blackman M. R., Soncrant T. T. Psychoneuroendocrinology. 1995;20:623–636. doi: 10.1016/0306-4530(94)00084-N. [DOI] [PubMed] [Google Scholar]
- 62.Asthana S., Greig N. H., Holloway H. W., Raffaele K. C., Berardi A., Schapiro M. B., Rapoport S. I., Soncrant T. T. Clin. Pharmacol. & Therap. 1996;60:276–282. doi: 10.1016/S0009-9236(96)90054-5. [DOI] [PubMed] [Google Scholar]
- 63.Law M. Y. L., Pershing L. K., Roberts L. K. Int. J. Pharmaceutics. 1992;88:251–260. doi: 10.1016/0378-5173(92)90323-T. [DOI] [Google Scholar]
- 64.Kurihara-Bergstrom T., Good W. R., Feisullin S., Signor C. J. Control. Release. 1991;15:271–278. doi: 10.1016/0168-3659(91)90119-X. [DOI] [Google Scholar]
- 65.Hussain M. A., Mollica J. A. J. Pharm. Sci. 1991;80:750751. doi: 10.1002/jps.2600800808. [DOI] [PubMed] [Google Scholar]
- 66.Patterson T. A., Kosh J. W. Gen. Pharmacol. 1993;24:641–647. doi: 10.1016/0306-3623(93)90224-L. [DOI] [PubMed] [Google Scholar]
- 67.Moos W. H., Bergmeier S. G., Coughenour L. L., Davis R. E., Hershenson F. M., Kester J. A., McKee J. S., Marriott J. G., Schwarz R. D., Tecle H., Thomas A. J. J. Pharm. Sci. 1992;81:1015–1019. doi: 10.1002/jps.2600811012. [DOI] [PubMed] [Google Scholar]
- 68.Moser U., Gubitz C., Galvan M., Immelsehr A., Lambrecht G., Mutschler E. Drug Res. 1995;45-1:449–455. [PubMed] [Google Scholar]
- 69.Toja E., Bonett C., Butti A., Hunt P., Fortin M., Barzaghi F., Formento M. L., Maggioni A., Nencioni A., Galliani G. Eur. J. Med. Chem. 1991;26:853–868. doi: 10.1016/0223-5234(91)90128-A. [DOI] [Google Scholar]
- 70.Toja E., Bonett C., Butti A., Hunt P., Fortin M., Barzaghi F., Formento M. L., Maggioni A., Nencioni A., Galliani G. Eur. J. Med. Chem. 1992;27:519–526. doi: 10.1016/0223-5234(92)90186-5. [DOI] [Google Scholar]
- 71.Showell G. A., Gibbons T. L., Kneen C. O., MacLeod A. M., Merchant K., Saunders J., Freedman S. B., Patel S., Baker R. J. Med. Chem. 1991;34:1086–1094. doi: 10.1021/jm00107a032. [DOI] [PubMed] [Google Scholar]
- 72.Moltzen E. K., Pedersen H., Bogeso K. P., Meier E., Frederiksen K., Sanchez C., Lembol H.L. J. Med. Chem. 1997;37:4085–4099. doi: 10.1021/jm00050a006. [DOI] [PubMed] [Google Scholar]
- 73.Bymaster F. P., Whitesitt C. A., Shannon H. E., DeLapp N., Ward J. S., Calligaro D. O., Shipley L. A., BuelkeSam J. L., Bodick N. C., Farde L., Sheardown M. J., Olesen P. H., Hansen K. T., Suzdak P. D., Swedberg M. D. B., Sauerberg P., Mitch C. H. Drug Dev. Res. 1997;40:158–170. doi: 10.1002/(SICI)1098-2299(199702)40:2<158::AID-DDR6>3.0.CO;2-K. [DOI] [Google Scholar]
- 74.Christopoulos A., Pierce T. L., Sorman J. L., El Fakahany E. E. Mol. Pharmacol. 1998;53:1120–1130. [PubMed] [Google Scholar]
- 75.Christopoulos A., El Fakahany E. E. Eur. J. Pharmacol. 1997;334:R3–R4. doi: 10.1016/S0014-2999(97)01162-X. [DOI] [PubMed] [Google Scholar]
- 76.DeLapp N., Wu S., Belagaje R., Johnstone E., Little S., Shannon H., Bymaster F., Calligaro D., Mitch C., Whitesitt C., Ward J., Sheardown M., Fink-Jensen A., Jeppesen L., Thomsen C., Sauerberg P. Biochem. Biophys. Res. Commun. 1998;244:156–160. doi: 10.1006/bbrc.1998.8235. [DOI] [PubMed] [Google Scholar]
- 77.Bodick N. C., Offen W. W., Levey A. I., Cutler N. R., Gauthier S. G., Satlin A., Shannon H. E., Tollefson G. D., Rasmussen K., Bymaster F. P., Hurley D. J., Potter W. Z., Paul S. M. Archiv. Neurol. 1997;54:465–473. doi: 10.1001/archneur.1997.00550160091022. [DOI] [PubMed] [Google Scholar]
- 78.Bodick N. C., Offen W. W., Shannon H. E., Satterwhite J., Lucas R., Van Lier R., Paul S. M. Alzheimer Disease Assoc. Disorders. 1997;11:S16–S22. [PubMed] [Google Scholar]
- 79.Ward J. S., Merritt L., Stratford R., Brown T. J., Wijayaratne R., Szewczyk S. P., Calligaro D. O., Bymaster F. P., Shannon H. E., Mitch C. H., Johnson D.W., Wikel J. H., Olesen M. J., Sheardown M. J., Swedberg M. D. B., Sauerberg P. Life Sci. 1997;60:6. [Google Scholar]
- 80.Ward J. S., Merritt L., Calligaro D. O., Bymaster F. P., Shannon H. E., Sawyer B. D., Mitch C. H., Deeter J. B., Peters S. C., Sheardown M. J., Olesen P.H., Swedberg M. D. B., Sauerberg P. J. Med. Chem. 1995;38:2469–3481. doi: 10.1021/jm00018a007. [DOI] [PubMed] [Google Scholar]
- 81.Ward J. S., Merritt L., Klimkowski V. J., Lamb M. L., Mitch C. H., Bymaster F. P., Sawyer B., Shannon H. E., Olesen P. H., Honore T., Sheardown M. J., Sauerberg P. J. Med. Chem. 1992;35:4011–4019. doi: 10.1021/jm00100a005. [DOI] [PubMed] [Google Scholar]
- 82.Hass K., Wieland A. Chem. Ber. 1960;93:1686–1692. [Google Scholar]
- 83.Spry D. O., Aaron H. S. J. Org. Chem. 1969;34:3674–3676. doi: 10.1021/jo01263a118. [DOI] [Google Scholar]
- 84.Barrett S. D., Jaen J. C., Caprathe B. W., Thomas A. J., Tecle H. Org. Prep. Proc. Int. 1997;29:330–335. doi: 10.1080/00304949709355206. [DOI] [Google Scholar]
- 85.Aaron H. S., Owens O. O., Rosenstock P. D., Leonard S., Elkin S., Miller J. I. J. Org. Chem. 1965;30:1331–1333. doi: 10.1021/jo01015a561. [DOI] [Google Scholar]
- 86.Nielson A. T., Platt E. N. J. Heteocyclic Chem. 1969;6:891–900. [Google Scholar]
- 87.Nielson A. T. J. Heterocyclic Chem. 1970;7:231–234. [Google Scholar]
- 88.Snow R. J., Baker R., Herbert R. H., Hunt I. J., Merchant K. J., Saunders J. J. Chem. Soc., Perkin Trans. 1. 1991:409–420. doi: 10.1039/p19910000409. [DOI] [Google Scholar]
- 89.Review; Kazlauskas R., Bornscheuer U. In: Biotransformations. Kelly D. R., editor. Wiley-VCH; Weinheim: 1998. pp. 37–192. Volume 8a in the series Biotechnology.
- 90.Guanti G., Banfi L., Brusco S., Narisano E. Tetrahedron: Asym. 1994;5:537–540. doi: 10.1016/0957-4166(94)80012-X. [DOI] [Google Scholar]
- 91.Hanessian S. Total Synthesis of Natural Products: The Chiron Approach. Pergamon; Oxford: 1983. 291 [Google Scholar]
- 92.Bols M. Carbohydrate Building Blocks. Wiley; New York: 1996. [Google Scholar]
- 93.Fraser-Reid B. O. Acc. Chem. Res. 1996;29:57–66. doi: 10.1021/ar950104s. [DOI] [Google Scholar]
- 94.Nicolaou K. C., Veale C. A., Hwang C. K., Hutchinson J., Prasad C. V. C., Ogilvie W. W. Angew. Chem. Int. Ed. Engl. 1991;30:299–303. doi: 10.1002/anie.199102991. [DOI] [Google Scholar]
- 95.Mori K. Tetrahedron. 1989;45:3233–3298. [Google Scholar]
- 96.Vazqueztato M. P., Seijas J. A., Fleet G. W. J., Mathews C. J., Hemmings P. R., Brown D. Tetrahedron. 1995;51:959–974. [Google Scholar]
- 97.Fleet G. W. J., Mathews C. J., Seijas J. A., Tato M. P. V., Brown D. J. J. Chem. Soc., Perkin Trans I. 1989:1065–1066. [Google Scholar]
- 98.Fleet G. W. J., James K., Lunn R. J. Tetrahedron Lett. 1986;27:3053–3056. doi: 10.1016/S0040-4039(00)84714-0. [DOI] [Google Scholar]
- 99.Fleet G. W. J., James K., Lunn R. J., C. J., Matthews C. J. Tetrahedron Lett. 1986;27:3057–3058. doi: 10.1016/S0040-4039(00)84715-2. [DOI] [Google Scholar]
- 100.Fleet G. W. J., Mathews C. J., Seijas J. A., Tato M. P. V., Brown D. J. J. Chem. Soc., Perkin Trans I. 1989:1067–1068. [Google Scholar]
- 101.Terao Y., Kotake H., Imai N., Achiwa K. Chem. Pharm. Bull. 1985;33:2762–2766. doi: 10.1248/cpb.33.2762. [DOI] [Google Scholar]
- 102.Orlek B. S., Wadsworth H., Wyman P., Hadley M. S. Tetrahedron Lett. 1991;32:1241–1244. doi: 10.1016/S0040-4039(00)92055-0. [DOI] [Google Scholar]
- 103.Cotterell I. F., Hands D., Kennedy D. J., Kerensa J. P., Wright S. H. B., Hoogsteen K. J. Chem. Soc., Perkin Trans I. 1990:1091–1097. [Google Scholar]
- 104.Orlek B. S., Wadsworth H., Wyman P., Hadley M. S. Tetrahedron Lett. 1991;32:1245–1246. doi: 10.1016/S0040-4039(00)92056-2. [DOI] [Google Scholar]
- 105.Jenkins S. M., Wadsworth H. J., Bromidge S., Orlek B. S., Wyman P. A., Riley G. J., Hawkins J. J. Med. Chem. 1992;35:2392–2406. doi: 10.1021/jm00091a007. [DOI] [PubMed] [Google Scholar]
- 106.Diana G. D., Volkots D. L., Nitz T. J., Bailey T. R., Long M. A., Vescio N., Aldous S., Pevear D. C., Dutko F. J. J. Med. Chem. 1994;37:2421–2436. doi: 10.1021/jm00041a022. [DOI] [PubMed] [Google Scholar]
- 107.Andersen K. E., Lundt B. F., Jorgensen A. S., Braestrup C. Eur. J. Med. Chem. 1996;31:417–425. doi: 10.1016/0223-5234(96)89169-0. [DOI] [Google Scholar]
- 108.Street L. J., Baker R., Book T., Kneen C. O., Macleod A. M., Merchant K. J., Showell G. A., Saunders J., Herbert R. H., Freedman S. B., Harley E. A. J. Med. Chem. 1990;33:2690–2697. doi: 10.1021/jm00172a003. [DOI] [PubMed] [Google Scholar]
- 109.Macor J. E., Ordway T., Smith R. L., Verhoest P. R., Mack R. A. J. Org. Chem. 1996;61:3228–3229. doi: 10.1021/jo9603340. [DOI] [Google Scholar]
- 110.Saunders J., MacLeod A. M., Merchant K., Showell G. A., Snow R. J., Street L. J., Baker R. J. Chem. Soc., Chem. Commun. 1988:1618–1619. doi: 10.1039/c39880001618. [DOI] [Google Scholar]
- 111.Sternbach L. H., Kaiser S. J. Am. Chem. Soc. 1952;74:2215-18 & 2219-2221. [Google Scholar]
- 112.Daeniker H. U., Grob C. A. Org. Syn. Coll. V. 1973:989–993. [Google Scholar]
- 113.Grob C.A., Renk E. Helv. Chim. Acta. 1954;37:1672-1680 & 1681-1688 & 1689-1698. [Google Scholar]
- 114.Snow R. J., Baker R., Herbert R. H., Hunt I. J., Merchant K. J., Saunders J. J. Chem. Soc., Perkin Trans. 1. 1991:409–420. doi: 10.1039/p19910000409. [DOI] [Google Scholar]
- 115.Saunders J., MacLeod A. M., Merchant K., Showell G. A., Snow R. J., Street L. J., Baker R. J. Chem. Soc., Chem. Commun. 1988:1618–1619. doi: 10.1039/c39880001618. [DOI] [Google Scholar]
- 116.Street L. J., Baker R., Book T., Kneen C. O., Macleod A. M., Merchant K. J., Showell G. A., Saunders J., Herbert R. H., Freedman S. B., Harley E. A. J. Med. Chem. 1990;33:2690–2697. doi: 10.1021/jm00172a003. [DOI] [PubMed] [Google Scholar]
- 117.MacLeod A. M., Herbert R., Hoogsteen K. J. Chem. Soc., Chem. Commun. 1990:100–102. doi: 10.1039/c39900000100. [DOI] [Google Scholar]
- 118.Jenkins S. M., Wadsworth H. J., Bromidge S., Orlek B. S., Wyman P. A., Riley G. J., Hawkins J. J. Med. Chem. 1992;35:2392–2406. doi: 10.1021/jm00091a007. [DOI] [PubMed] [Google Scholar]
- 119.Boelsterli J., Eggnauer U., Pombo-Villar E., Weber H.-P., Walkinshaw M. Helv. Chim. Acta. 1992;75:507–512. doi: 10.1002/hlca.19920750210. [DOI] [Google Scholar]
- 120.Showell G. A., Baker R., Davis J., Hargreaves R., Freedman S. B., Hoogsteen K., Patel S., Snow R. J. J. Med. Chem. 1992;35:911–916. doi: 10.1021/jm00083a016. [DOI] [PubMed] [Google Scholar]
- 121.Freedman S. B., Harley E. A., Marwood R. S., Patel S. Eur. J. Pharmacol. 1990;187:193–199. doi: 10.1016/0014-2999(90)90006-R. [DOI] [PubMed] [Google Scholar]
- 122.Freedman S. B., Harley E. A., Patel S., Newberry N., Gilbert A. T., McKnight A., Tang J. K., Macquire J. J., Mudunkotuwa N. T., Baker R., Street L. J., MacLeod A. M., Saunders J., Iversen L. L. Br. J. Pharamacol. 1990;101:575–580. doi: 10.1111/j.1476-5381.1990.tb14123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Baker R., Showell G. A., Street L. J., Saunders J., Hoogsteen K., Freedman S. B., Hargreaves R. J. J. Chem. Soc., Chem. Commun. 1992:817–819. doi: 10.1039/c39920000817. [DOI] [Google Scholar]
- 124.Freedman S. B., Patel S., Harley E. A., Iversen L. L., Baker R., Showell G. A., Saunders J., McKnight A., Newberry N., Scholey K., Hargreaves R. Eur. J. Pharamacol. 1992;215:135–136. doi: 10.1016/0014-2999(92)90618-E. [DOI] [PubMed] [Google Scholar]
- 125.Baker R., Street L. J., Reeves A. J., Saunders J. Chem. Soc., Chem. Commun. 1991:760–762. doi: 10.1039/c39910000760. [DOI] [Google Scholar]
- 126.Street L. J., Baker R., Book T., Reeve A. J., Saunders J., Willson T., Marwood R. S., Patel S., Freedman S. B. J. Med. Chem. 1992;35:295–305. doi: 10.1021/jm00080a014. [DOI] [PubMed] [Google Scholar]
- 127.Ashwood M. S., Gibson A. W., Houghton P. G., Humphrey G. R., Roberts D. G., Wright S. H. B. J. Chem. Soc., Perk. Trans. I. 1995:641–644. doi: 10.1039/p19950000641. [DOI] [Google Scholar]
- 128.Hargreaves R. J., McKnight A. T., Scholey K., Newberry N. R., Street L. J., Hutson P. H., Semark J. E., Harley E. A., Patel S., Freedman S. B. Br. J. Pharmacol. 1992;107:494–501. doi: 10.1111/j.1476-5381.1992.tb12773.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Freedman S. B., Dawson G. R., Iverson L. L., Baker R., Hargreaves R. J. Life Sci. 1993;52:489–495. doi: 10.1016/0024-3205(93)90306-N. [DOI] [PubMed] [Google Scholar]
- 130.Loudon J. M., Bromidge S. M., Brown F., Clark M. S. G., Hatcher J. P., Hawkins J., Riley G. J., Noy G., Orlek B. S. J. Pharmacol. Exper. Therap. 1997;283:1059–1068. [PubMed] [Google Scholar]
- 131.Bromidge S. M., Cassidy F., Clark M. S. G., Eggleston D. S., Oriek B. S. J. Chem. Soc., Chem. Commun. 1994:2189–2190. doi: 10.1039/C39940002189. [DOI] [Google Scholar]
- 132.Bromidge S. M., Brown F., Cassidy F., Clark M. S. G., Dabbs S., Hadley M. S., Hawkins J., Loudon J. M., Naylor C. B., Orlek B. S., Riley G. J. J. Med. Chem. 1997;40:4265–4280. doi: 10.1021/jm9702903. [DOI] [PubMed] [Google Scholar]
- 133.Harries M. H., Samson N. A., Cilia J., Hunter A. J. Br. J. Pharmacol. 1998;124:409–415. doi: 10.1038/sj.bjp.0701844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hatcher J. P., Loudon J. M., Hagan J. J., Clark M. S. G. Psychopharmacology. 1998;138:275–282. doi: 10.1007/s002130050672. [DOI] [PubMed] [Google Scholar]
- 135.Grochowski E., Jurczak J. Synthesis. 1976:682–684. for recent examples see Maier L., Sporri H. Phosph. Sulfur & Related Element. 1992;70:39-48 & 49-57.
- 136.Tecle H., Jaen J. C., Augelli-Szafran C., Barrett S. D., Caprathe B. W., Lauffer D. J., Mirzadegan T., Moos W. H., Moreland D. W., Pavia M. R., Schwarz R. D., Thomas A. J., Davis R. E. Bioorg. Med. Chem. Lett. 1995;5:631–636. doi: 10.1016/0960-894X(95)00086-9. [DOI] [Google Scholar]
- 137.Tecle H., Lauffer D. J., Davis R. E., Mirzadegan T., Moreland D. W., Schwarz R. D., Thomas A. J., Raby C., Eubanks D., Brann M. R., Jaen J. C. Bioorg. Med. Chem. Lett. 1995;5:637–642. doi: 10.1016/0960-894X(95)00087-A. [DOI] [Google Scholar]
- 138.Jaen J. C., Barrett S., Brann M., Callahan M. J., Davis R., Doyle P., Eubanks D., Lauffer D., Lauffer L., Lipiniski W., Moreland D. W., Nelson C. B., Raby C., Schwarz R., Spencer C., Tecle H. Life Sci. 1995;56:845–852. doi: 10.1016/0024-3205(95)00019-3. [DOI] [PubMed] [Google Scholar]
- 139.Tecle H., Barrett S.D., Lauffer D. J., Augelli-Szafran C., Brann M. R., Callahan M. J., Caprathe B. W., Davis R. E., Doyle P. D., Eubanks D., Lipiniski W., Mirzadegan T., Moos W. H., Moreland D. W., Nelson C. B., Pavia M. R., Raby C., Schwarz R. D., Spencer C. J., Thomas A. J., Jaen J. C. J. Med. Chem. 1998;41:2524–2536. doi: 10.1021/jm960683m. [DOI] [PubMed] [Google Scholar]
- 140.Hills C. J., Winter S. A., Balfour J. A. Drugs. 1998;55:813–820. doi: 10.2165/00003495-199855060-00008. [DOI] [PubMed] [Google Scholar]
- 141.Gillberg P.G., Sundquist S., Nilvebrant L. Eur. J. Pharmacol. 1998;349:285–292. doi: 10.1016/S0014-2999(98)00214-3. [DOI] [PubMed] [Google Scholar]
- 142.Postlind H., Danielson A., Lindgren A., Andersson S. H. G. Drug Metab. Disp. 1998;26:289–293. [PubMed] [Google Scholar]
- 143.Andersson S. H. G., Lindgren A., Postlind H. Drug Metab. Disp. 1998;26:528–535. [PubMed] [Google Scholar]
- 144.Nilvebrant L., Gillberg P. G., Sparf B. Pharmacol. & Toxicol. 1997;81:169–172. doi: 10.1111/j.1600-0773.1997.tb02064.x. [DOI] [PubMed] [Google Scholar]
- 145.Nilvebrant L., Hallen B., Larsson G. Life Sci. 1997;60:1129–1136. doi: 10.1016/S0024-3205(97)00057-X. [DOI] [PubMed] [Google Scholar]
- 146.Brynne N., Dalen P., Alvan G., Bertilsson L., Gabrielsson J. Clin. Pharmacol. Therap. 1998;63:529–539. doi: 10.1016/S0009-9236(98)90104-7. [DOI] [PubMed] [Google Scholar]
- 147.Swart R., Koivisto P., Markides K. E. J. Chromatog. A. 1998;828:209–218. doi: 10.1016/S0021-9673(98)00788-2. [DOI] [PubMed] [Google Scholar]
- 148.Palmer L., Andersson L., Andersson T., Stenberg U. J. Pharm. Biomed. Anal. 1997;16:155–165. doi: 10.1016/s0731-7085(97)00023-x. [DOI] [PubMed] [Google Scholar]
- 149.For a review of asymmetric conjugate additions see Rossiter B.E., Swingle N. M. Chem. Rev. 1992;92:771–806.
- 150.For a review of the use of chiral oxazolidinones in asymmetric synthesis see Ager D. J., Prakash I., Schaad D. R. Aldrichimica Acta. 1997;30:3–12.
- 151.Andersson P. G., Schink H. E., Osterlund K. J. Org. Chem. 1998;63:8067–8070. doi: 10.1021/jo981259r. [DOI] [Google Scholar]
- 152.Leu B. S., Li G. G., Lung F. D., Hruby V. J. J. Org. Chem. 1995;60:5509–5514. [Google Scholar]
- 153.Barbier P., Renzetti A. R., Turbanti L., Di Bugno C., Fornai F., Vaglini F., Maggio R., Corsini G. U. Eur J. Pharm. 1995;290:125–132. doi: 10.1016/0922-4106(95)90024-1. [DOI] [PubMed] [Google Scholar]
- 154.Review; Kazlauskas R., Bornscheuer U. In: Biotransformations. Kelly D. R., editor. Wiley-VCH; Weinheim: 1998. pp. 37–192. Volume 8a in the series Biotechnology.
- 155.Di Bussolo V., Catelani G., Mastrorilli E., Di Bugno C., Giorgi R. Tetrahedron: Asym. 1996;7:3585–3592. doi: 10.1016/S0957-4166(96)00467-3. [DOI] [Google Scholar]
- 156.Di Bugno C., Colombani S.M., Dapporto P., Garzelli G., Paoli P., Subissi A. Turbanti Chirality. 1997;9:713–721. [Google Scholar]
- 157.Frey K. A., Minoshima S., Kuhl D. E. Quart. J. Nucl. Med. 1998;42:166–178. [PubMed] [Google Scholar]
- 158.Morgan A. E., Brodie J. D., Dewey S. L. Quart. J. Nucl. Med. 1998;42:151–157. [PubMed] [Google Scholar]
- 159.Maziere M. Pharmacol. Therap. 1995;66:83–101. doi: 10.1016/0163-7258(95)00003-Y. [DOI] [PubMed] [Google Scholar]
- 160.Mullan B. P., O'Connor M. K., Hung J. C. Neurosurgery Clinics of North Am. 1996;7:617–652. [PubMed] [Google Scholar]
- 161.Devous M. D. J. Neuroimaging. 1995;5:S2–S13. doi: 10.1111/jon19955s1s2. [DOI] [PubMed] [Google Scholar]
- 162.Waldemar G. Cerebrovascular Brain Metab. Rev. 1995;7:89–130. [PubMed] [Google Scholar]
- 163.Knapp F. F., McPherson D. W., Luo H., Zeeburg B. Anticancer Res. 1997;17:1559–1572. [PubMed] [Google Scholar]
- 164.Kiesewetter D. O., Carson R. E., Jagoda E. M., Herscovitch P., Eckelman W. C. Life Sci. 1998;64:511–518. doi: 10.1016/S0024-3205(98)00595-5. [DOI] [PubMed] [Google Scholar]
- 165.Lee. K. S., He X. S., Jones D. W., Coppola R., Gorey J. G., Knable M. B., de Costa B. R., Rice K. C., Weinberger D. R. J. Nucl. Med. 1996;37:2021–2024. [PubMed] [Google Scholar]
- 166.Seebach D., Naef R., Calderari G. Tetrahedron. 1984;40:1313–1324. doi: 10.1016/S0040-4020(01)82417-0. [DOI] [Google Scholar]
- 167.McPherson D. W., Knapp F. F., Jr. J. Org. Chem. 1996;61:8335–8336. doi: 10.1021/jo961033t. [DOI] [PubMed] [Google Scholar]
- 168.McPherson D. W., Lambert C. R., Jahn K., Sood V., McRee R. C., Zeeberg B., Reba R. C., Knapp F. F., Jr. J. Med. Chem. 1995;38:3908–3917. doi: 10.1021/jm00020a004. [DOI] [PubMed] [Google Scholar]
- 169.Cohen V. I., Zeeberg B. R., Boulay S. F., Sood V. K., Rayeq M. R., Danesh R. A., McPherson D. W., Reba R. C. J. Mol. Neuroscience. 1998;11:1–9. doi: 10.1385/JMN:11:1:1. [DOI] [PubMed] [Google Scholar]
- 170.Ichihara A., Oikawa H. Curr. Org. Chem. 1998;2:365–394. [Google Scholar]
- 171.Katayama K., Kobayashi T., Oikawa, Honma M. H., Ichihara A. Biochim. Biophys. Acta. 1998;1384:387–395. doi: 10.1016/S0167-4838(98)00040-5. [DOI] [PubMed] [Google Scholar]
- 172.Oikawa H., Kobayashi T., Katayama K., Suzuki Y., Ichihara A. J. Org. Chem. 1998;63:8748–8756. doi: 10.1021/jo980743r. [DOI] [Google Scholar]
- 173.Oikawa H., Yagi K., Watanabe K., Honma M., Ichihara A. J. Chem. Soc., Chem. Commun. 1997:97–98. doi: 10.1039/a607412j. [DOI] [Google Scholar]
- 174.Ichihara A., Oikawa H. Biosci. Biotech. Bioch. 1997;61:12–18. [Google Scholar]
- 175.Jakubik J., Bacakova L., El Fakahany E. E., Tucek S. Mol. Pharmacol. 1997;52:172–179. doi: 10.1124/mol.52.1.172. [DOI] [PubMed] [Google Scholar]
- 176.Dolezal V., Tucek S. Br. J. Pharmacol. 1998;124:1213–1218. doi: 10.1038/sj.bjp.0701966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Lazareno S., Gharagozloo P., Kuonen D., Popham A., Birdsall N. J. M. Mol. Pharmacol. 1998;53:573–589. doi: 10.1124/mol.53.3.573. correction 1999, 55, 194. [DOI] [PubMed] [Google Scholar]
- 178.Gharagozloo P., Miyauchi M., Birdsall B., Birdsall N. J. M. J. Org. Chem. 1998;63:1974–1980. doi: 10.1021/jo971981+. [DOI] [Google Scholar]
- 179.Lazareno S., Birdsall B., Fukazawa T., Gharagozloo p., Hashimoto T., Kuwano H., Popham A., Sugimoto M., Birdsall N. J. M. Life Sci. 1999;64:519–526. doi: 10.1016/s0024-3205(98)00596-7. [DOI] [PubMed] [Google Scholar]
- 180.Dorje F., Wess J., Lambrecht G., Tacke R., Mutschler E., Brann M. R. J. Pharmacol. & Exper. Therap. 1991;256:727–733. [PubMed] [Google Scholar]
- 181.Kilbinger H., Von Bardeleben R. S., Siefken H., Wolf D. Life Sci. 1995;56:981–987. doi: 10.1016/0024-3205(95)00037-7. [DOI] [PubMed] [Google Scholar]
- 182.Matsui H., Lazareno S., Birdsall N. J. M. Mol. Pharmacol. 1995;47:88–98. [PubMed] [Google Scholar]
- 183.Kozikowski A. P., Fauq A. H., Miller J. H., McKinney M. Bioorg. Med. Chem. Lett. 1992;2:797–802. doi: 10.1016/S0960-894X(00)80534-X. [DOI] [Google Scholar]
- 184.Malaska M. J., Fauq A. H., Kozikowski A. P., Aagaard P. J., McKinney M. Bioorg. Med. Chem. Lett. 1995;5:61–66. doi: 10.1016/0960-894X(94)00459-S. [DOI] [Google Scholar]
- 185.Malaska M. J., Fauq A. H., Kozikowski A. P., Aagaard P. J., McKinney M. Bioorg. Med. Chem. Lett. 1993;3:1247–1252. doi: 10.1016/S0960-894X(00)80325-X. [DOI] [Google Scholar]
- 186.Baldwin J. E., Chesworth R., Parker J. S., Russell A. T. Tetrahedron Lett. 1995;36:9551–9554. doi: 10.1016/0040-4039(95)02045-4. [DOI] [Google Scholar]
- 187.Debaecke G., Declercq P. J. Tetrahedron Lett. 1995;36:7515–7518. [Google Scholar]
- 188.Hofman S., DeBaecke G., Kenda B., DeClerg P. J. Synthesis. 1998:479–489. doi: 10.1055/s-1998-5928. [DOI] [Google Scholar]
- 189.Hart D. J., Wu W. L., Kozikowski A. P. J. Am. Chem. Soc. 1995;117:9369–9370. doi: 10.1021/ja00141a036. [DOI] [Google Scholar]
- 190.Hart D. J., Li J., Wu W. L., Kozikowski A. P. J. Org. Chem. 1997;62:5023–5033. doi: 10.1021/jo970612a. [DOI] [Google Scholar]
- 191.Chackalamannil S., Davies R. J., Asberom T., Doller D., Leone D. J. Am. Chem. Soc. 1996;118:9812–9813. doi: 10.1021/ja962542f. [DOI] [Google Scholar]
- 192.Andersen R. J., Van Soest R. W. M., Kong F. In: Alkaloids; Chemical and Biological Perspectives. Pelletier S. W., editor. Pergamon Press/Elsevier Science; Oxford, UK: 1996. pp. 301–355. [Google Scholar]
- 193.Tsuda M., Kobayashi J. Heterocycles. 1997;46:765–794. [Google Scholar]
- 194.Fusetani N., Asai N., Matsunaga S., Honda K., Yasumuro K. Tetrahedron Lett. 1994;35:3967–3970. doi: 10.1016/S0040-4039(00)76715-3. [DOI] [Google Scholar]
- 195.Baldwin J. E., Whitehead R. C. Tetrahedron Lett. 1992;33:2059–2062. doi: 10.1016/0040-4039(92)88141-Q. [DOI] [Google Scholar]
- 196.Baldwin J. E., Claridge T. D. W., Culshaw A. J., Heupel F. A., Lee V., Spring D. R., Whitehead R. C., Broughtflower R. J., Mutton I. M., Upton R. J. Angew. Chem. Int. Ed. Engl. 1998;37:2661–2663. doi: 10.1002/(SICI)1521-3773(19981016)37:19<2661::AID-ANIE2661>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 197.Kaiser A., Billot X., Gateau-Olesker A., Marazano C., Das B. C. J. Am. Chem. Soc. 1998;120:8026–8034. doi: 10.1021/ja9805369. [DOI] [Google Scholar]
- 198.Baldwin J. E., Spring D. R., Atkinson C. E., Lee V. Tetrahedron. 1998;54:13655–13680. doi: 10.1016/S0040-4020(98)00842-4. [DOI] [Google Scholar]
- 199.Wanner M. J., Koomen G. J. Eur. J. Org. Chem. 1998:889–895. doi: 10.1002/(SICI)1099-0690(199805)1998:5<889::AID-EJOC889>3.0.CO;2-G. [DOI] [Google Scholar]
- 200.Anan H., Seki N., Noshiro O., Honda K., Yasumuro K., Ozasa T., Fusetani N. Tetrahedron. 1996;52:10849–10860. doi: 10.1016/0040-4020(96)00628-X. [DOI] [Google Scholar]
- 201.Adem A., Karlsson E. Life Sci. 1997;60:1069–1076. doi: 10.1016/S0024-3205(97)00049-0. [DOI] [PubMed] [Google Scholar]
- 202.Liang J. S., Carsi-Gabrenas J., Krajewski J. L., McCaffrey J. M., Purkerson S. L., Santiago M.P., Strauss W. L., Valentine H. H., Potter L. T. Toxicon. 1996;34:1257–1267. doi: 10.1016/S0041-0101(96)00109-2. [DOI] [PubMed] [Google Scholar]
- 203.Jerusalinsky D., Kornisiuk E., Alfaro P., Quillfeldt J., Alonso M., Verde E. R., Cervenansky C., Harvey A. Neuroreport. 1998;9:1407–1411. doi: 10.1097/00001756-199805110-00029. [DOI] [PubMed] [Google Scholar]
- 204.Potter L. T., Hanchett-Valentine H., Liang J.-S., Max S. I., Purkerson S. L., Silberberg H. A., Strauss W. L. Life Sci. 1993;52:433–440. doi: 10.1016/0024-3205(93)90299-I. [DOI] [PubMed] [Google Scholar]
- 205.Adem A., Jolkkonen M., Bogdanovic N., Islam A., Karlsson E. Brain. Res. Bull. 1997;44:597–601. doi: 10.1016/S0361-9230(97)00281-5. [DOI] [PubMed] [Google Scholar]
- 206.Witherup K. M., Ransom R. W., Graham A. C., Bernard A. M., Salvatore M. J., Lumma W.C., Anderson P. S., Pitzenberger S. M., Varga S. L. J. Am. Chem. Soc. 1995;117:6682–6685. doi: 10.1021/ja00130a005. [DOI] [Google Scholar]
- 207.Nagumo S., Nishida A., Yamazaki C., Murashige K., Kawahara N. Tetrahedron Lett. 1998;39:4493–4496. doi: 10.1016/S0040-4039(98)00797-7. [DOI] [Google Scholar]