Abstract
Public–private partnerships are an effective way to address the global double burden of malnutrition. While public–private partnerships operate in multiple forms, their leadership usually falls to governments, public health agencies, or nongovernmental organizations, with the private sector taking a subordinate role. The rapid ascent of social media and mass communications worldwide has provided a disruptive technology for new nutrition intervention programs. A new model, provisionally called private–public engagement, takes advantage of social media, mass media, and integrated social marketing to reach parents, families, and communities directly. These new private–public engagement initiatives need to be managed in ways suggested for public–private partnerships by the World Health Organization, especially if the private sector is in the lead. Once the rationale for engagement is defined, there is a need to mobilize resources, establish in-country partnerships and codes of conduct, and provide a plan for monitoring, evaluation, and accountability. Provided here is an example consistent with the private–public engagement approach, ie, the United for Healthier Kids program, which has been aimed at families with children aged less than 12 years. Materials to inspire behavioral change and promote healthier diets and lifestyle were disseminated in a number of countries through both digital and physical channels, often in partnership with local or regional governments. A description of this program, along with strategies to promote transparency and communication among stakeholders, serves to provide guidance for the development of future effective private–public engagements.
Keywords: child, codes of conduct, double burden of malnutrition, social media, principles, private–public engagement, public–private partnership
INTRODUCTION
The global double burden of childhood malnutrition manifests as both undernutrition and overweight.1–3 Low- and middle-income countries are most vulnerable; in some communities, stunting, wasting, and obesity can coexist.4–6 Given increasingly limited public resources, childhood malnutrition appears resistant to local or single-sector solutions.7
Transformative approaches are needed to ensure deeper engagement by multisector stakeholders.7,8 The United Nations has encouraged governments, health jurisdictions, and civil society to engage with the private sector through public–private partnerships (PPPs) to address malnutrition.5,6,9 The more-successful and -sustained nutrition initiatives have been those that brought together government agencies, nongovernmental organizations, policymakers, schools, civil society, the food industry, and the media.3,9–13 International agencies have repeatedly called for increased engagement with the private sector to address the double burden of malnutrition in low- and middle-income countries.14–16
The chief features of PPPs in public health nutrition have been described previously.17 Three types of functioning PPPs were identified. Philanthropic PPPs were characterized by charitable donations of money or food.17 Transactional PPPs required a higher level of interaction through shared principles and goals. Transformational PPPs, the highest level of engagement, involved multiple partners, large-scale programs, and social change.17 The common assumption underlying all PPPs has been that the public sector would take the lead, selecting and auditing potential industry partners in line with public health goals.17,18
The rapid advent of social media and mass communications worldwide has provided a disruptive new technology that complements the traditional communication channels. A new intervention framework, provisionally called private–public engagement (PPE), takes advantage of social media, mass media, and integrated social marketing to reach parents, families, and communities directly. Novel PPE initiatives should not escape scrutiny and need to be managed in ways suggested for PPPs by the World Health Organization, especially if the private sector is to be in the lead. The rationale for engagement needs to be defined. Once the rationale is established, there is a need to mobilize resources, establish in-country partnerships and codes of conduct, and provide a plan for monitoring, evaluation, and accountability. Describing how these goals should be achieved is the topic of this review.
There is a clear global need for a new intervention framework. The majority of social marketing programs to prevent childhood obesity have been developed and delivered in the United States,19–25 Europe,26–29 or Australia.30,31 Only a few have addressed the rising rates of overweight in low- and middle-income countries, and these have tended to be community interventions in relatively isolated locations such as the Marshall Islands32 or Micronesia.33 With the recent increase in the global reach of mass communication channels such as television, Internet, and mobile phones, there are new opportunities to use social marketing approaches to create demand for healthy behavior among wider and more diverse global populations.
PUBLIC–PRIVATE PARTNERSHIPS
The supporting role of the private sector in many PPPs has been to provide funding and other support for health programs initiated by governments and nongovernmental organizations.18,34 One well-known initiative with a global reach, Ensemble Prévenons l’Obésité des Enfants (EPODE),28,35 is a childhood obesity prevention program driven largely by public institutions and local governments. Local policymakers, such as mayors, have worked with schools and other public institutions to engage parents and children on issues related to childhood body weight. The role of the food industry (both multinational and smaller local enterprises) has been to provide financial support to the EPODE program and help fund local implementation of EPODE-affiliated programs.
Many of the existing programs (for examples, see Table 119–24,26–28,30,36–38,39) operate primarily through schools20,21,27,40 and have often been limited to one city or to a few school districts.19,20,22,30 However, some programs achieved a broader reach. Food Hero23 began with a smaller-scale pilot program before expanding to a wider audience, in this case, one US state. The Fuel Up to Play 60 program21 promoted physical activity and nutrition in school-aged children in partnership with the National Football League. The national-level programs Change4Life26 and UNICEF Kid Power24 were designed by public agencies to achieve public health goals through multistakeholder engagement. While EPODE now functions globally, another program, Pro Children,27 operates in 3 European countries.
Table 1.
Social marketing programs used to influence children’s nutrition and lifestyle
| Category | Program | Channels | Behaviors targeted | Audience | Behavioral outcome measures | Target and scale of program | Stakeholders | Initiator |
|---|---|---|---|---|---|---|---|---|
| Schools | Team Nutrition20,36 | Schools (lessons, displays, tastings). Parent newsletter and events. Media coverage | Dietary choices (variety and quality) | Children and parents | Process measures (eg, no. of hours); qualitative interviews; questionnaires; teacher and food service observations; observations of children’s food choices and behaviors | 7 school districts in different US states | Government (US Department of Agriculture) | Public |
| Pro Children27 | Schools (classroom activities, F&V availability); parent activities; web tool (F&V advice); local media | F&V intake | Children and parents | 24-h dietary recalls; FFQs | Schools in 3 European countries (Norway, the Netherlands, Spain) | Government (European Commission), academic institutions | Public | |
| Fuel Up to Play 6021 | Schools (provision of educational activities, access to nutritious foods, and sports equipment) | Physical activity, nutritional choices | Children and parents | School decides how to track behaviors. Suggestions include the use of surveys; informal feedback from teachers or parents; and tracking the following: no. of children participating, meal purchases, and student behavior. Some studies have explored longitudinal effects on diet, physical activity, and fitness21,39 | Nationwide in the USA | Private organizations (National Football League; National Dairy Council) | Private | |
| Community | Bike, Walk, and Wheel22,37 | Mass media, posters, promotions | Use of active transport | Community | Observations of pedestrians and cyclists | One US city (Columbia, MO) | Nonprofit organizations (PedNet Coalition; Robert Wood Johnson Foundation), local government | NGO |
| Community plus online component | EPODE28 | Messaging disseminated through communities; environmental changes in schools and public spaces; events in schools and in the broader community (eg, stores, parks) | Nutritional choices, physical activity | Children | Anthropometry; process measures and output measures (no. of events, materials developed) | Mostly higher-SES countries | Government, NGOs, private partners | Public–private |
| 5-4-3-2-1 Go!19 | Mass media, events, student ambassadors, website | Nutritional choices, physical activity | Community | Home observations; interviews; assessment of reach and awareness | One US city (Chicago, IL) | Consortium of local organizations (CLOCC) | Public | |
| Change4Life26 | Digital technology, school interventions, social media | Nutritional choices, physical activity | Children and parents | Parent interviews; assessment of claimed behavior adoption; basket analysis of shopping behavior; tracking of national obesity trends | Nationwide in the UK | National government (National Health Service) | Public | |
| InFANT Extend30 | Group lessons for parents, Facebook group, newsletters delivered by email | F&V intake, decreased intake of SSBs and energy-dense foods, more physical activity, less screen time | Parents | Anthropometry; FFQs; accelerometers; questionnaires | One Australian metro area (Melbourne, Victoria) | NGO-funded organizations (World Cancer Research Fund), academic partners | Public | |
| Online only | Food Hero23,38 | Social media, website (recipe focused), community kit for nutrition educators | Nutritional choices | Parents | Assessment of no. of active users, clicks on posts, and virality of posts | One US state (Oregon) | Academic institution (Oregon State University) | Public? |
| Social movement | UNICEF Kid Power24 | Activity monitor for children in the USA. School program exists, but children can participate independently, tooWith increased activity, corporate sponsors donate meals for malnourished children in developing countries | Physical activity | Children | Assessment of no. of children enrolled in school programs, no. of meals distributed to those in need | Nationwide in the USA | NGOs (UNICEF, Force for Change), industry partner (Target Corporation) | NGO |
Abbreviations: CLOCC, Consortium to Lower Obesity in Chicago Children; EPODE, Ensemble Prévenons l’Obésité des Enfants; F&V, fruits and vegetables; FFQ, food frequency questionnaire; NGO, nongovernmental organizations; SSB, sugar-sweetened beverage; UNICEF, United Nations Children’s Fund.
While schools remain the primary channel of communication, some programs have reached the general community through messaging and interventions in other public spaces (eg, parks, shops) and through mass media.19,22,28,40,41 Digital communications are one tool for behavioral change. Although a few online programs have targeted parents directly,30,38 most interventions built around social media have targeted adolescents and young adults.42–44
ROLE OF THE PRIVATE SECTOR
Private-sector engagement is increasingly viewed as indispensable to creating change in the food supply or the global food environment.9,15,45–47 While the role of the food industry in preventing childhood malnutrition continues to be a topic for spirited debate,48,49 government spending on public health has declined in recent years.17,50–52 In particular, governments of low- and middle-income countries are forced to devote their scarce resources to the prevention and treatment of the continuum of malnutrition, from wasting and stunting to overweight.53
Transnational food companies can leverage their research, expertise, consumer insight, and marketing power to address global nutrition challenges. Because they operate globally, large food companies are uniquely positioned to implement large-scale initiatives around the world. Their global reach stands in contrast to PPPs that may be driven and financed by committed local stakeholders such as local governments or nongovernmental organizations19,22,30 but may lack the necessary resources to network and develop programs on a larger scale.
The importance of balancing the benefits and risks of PPPs to address global malnutrition has been well described in influential works.17,54 Kraak et al17 noted that large food companies have contributed to PPPs to alleviate hunger, promote food security, and help develop microenterprises or small businesses. They highlighted the importance of so-called transformational PPPs that addressed complex global nutrition challenges such as food fortification and the creation of programs to promote a healthy diet and to prevent obesity. Among the leaders in this space were the Global Alliance for Improved Nutrition, described as an “alliance of governments, international organizations, the private sector and civil society” and the Healthy Weight Commitment Foundation.17
Private–public engagement differs from PPP in one important respect. In PPE, the private sector takes the leading role in bringing together multiple entities—families, schools, communities, policymakers, the media, and nongovernmental organizations, among others—to address health-related issues.
The principles for managing the benefits and risks remain the same. Transformational PPE programs need to be aligned with local and regional policies on nutrition and health. Their rules of engagement with stakeholders, both public and private, also need to follow standard principles. These include having a clearly defined set of achievable goals to benefit the public, a clear statement of work, and a statement of roles and responsibilities of partners. Accountability is essential to ensure that the objectives of PPEs meet both public and private needs. Also needed are guidelines for the use of industry brands, logos, icons, and color schemes and policies on where and how the names and logos of the partnering organizations should be used. All communications must follow country-specific policies related to marketing to children, which may forbid the use of specific products or brand names.
AN EXAMPLE OF PPE: THE UNITED FOR HEALTHIER KIDS PROGRAM
The United for Healthier Kids (U4HK) program, now launched in 11 countries by Nestlé, uses social media, mass media, and integrated social marketing to reach parents and caregivers directly. The main principles of the U4HK program are presented in Box 1. These rules of engagement highlight the importance of building evidence-based health interventions with committed partners that are adapted and fully responsive to local needs. Such principles could also guide future PPE initiatives by other companies that are equally committed to creating shared value for society.55,56
Box 1.
Six suggested principles for private–public engagement programs
1. Ensure a clear rationale for local engagement: Public health nutrition content should be culture specific, sensitive to local needs, and aligned with existing local programs and national guidelines.
2. Build programs on solid partnerships: A tripartite model is encouraged, one that brings together private industry, government agencies, NGOs, and consumers. Multiple stakeholders bring complementary resources to the table and must have clear roles and responsibilities.
3. Base programs on long-term commitment: Each country or region should commit to running the program for several years and creating a local coordination team.
4. Use a science-driven approach: Health messaging should be science driven and evidence based, guided by nutrition, behavioral, and social sciences.
5. Monitor and evaluate programs for impact: Outcome and process evaluations are needed to assess project performance. New metrics on the effectiveness of social media may need to be developed.
6. Ensure programs are transparent and accountable: Reports and other information about the program and its partners should be available to all stakeholders and partners, including the public.
The U4HK transformational PPE model is shown in Figure 1. The PPP approach to reaching families through multiple communication channels is shown on the left, while the complementary PPE approach, which makes greater use of direct access by social media, is shown on the right.
Figure 1.
The United for Healthier Kids (U4HK) transformational model of private–public engagement (PPE). The public–private partnership (PPP) approach to reaching families through multiple communication channels is shown on the left, while the complementary PPE approach, which makes greater use of direct access by social media, is shown on the right.
Six science-based behavioral goals
At the time it was launched, the U4HK program had public health nutrition goals that were clearly defined. The content, built around 6 goals for dietary or behavioral change (Figure 2), was science driven and evidence based. The 6 family-centered goals for dietary or behavioral change selected for inclusion in the U4HK program were based on an exhaustive review of the literature by internal and external experts. A global advisory board, convened by Nestlé, provided advice on the overall framework58 and scientific content of the program. This framework was used in each country as guidance for creating content. The board also established a framework for assessment to guide countries in measuring the reach of the program, change in knowledge and attitudes, and intended and effective change in behavior.
Figure 2.
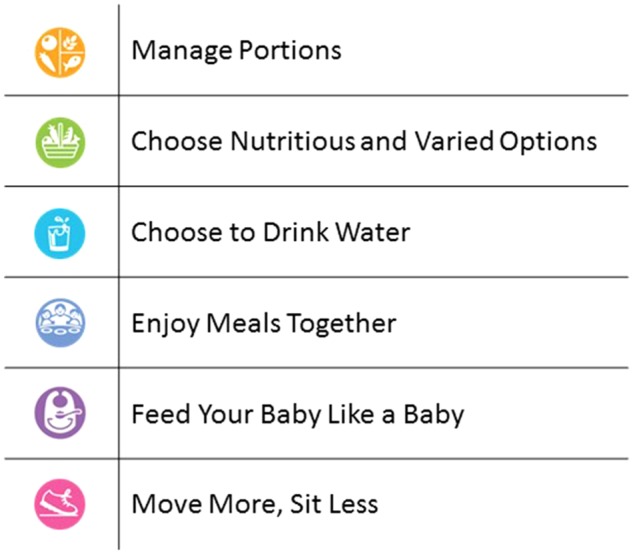
Six family-centered strategies for dietary or behavioral change used in the United for Healthier Kids (U4HK) program.
The focus on parents of children under 12 years of age was guided by a socioecological model57–59 that emphasizes the role of personal, social, and environmental factors and the role of the environment in health decision-making. Studies have shown that the time window of early to middle childhood represents a critical opportunity for promoting lifelong behavioral change.60
The 6 behavioral goals outlined in the following sections were developed to be understood by laypeople. In each country or region, program materials were translated into the local language, and wording was aligned with existing local health messaging, where appropriate.
Manage portions.
Portion sizes can influence the amount of food consumed at each eating occasion, with larger portions leading to higher energy intakes.61–65 Larger portions of energy-dense foods, which contain concentrated energy per unit of weight, can lead to overeating.66,67 Selecting ample portions of nutrient-rich vegetables and limiting portions of energy-dense foods are important parts of healthy eating habits.68–70 Serving larger portions of fruits and vegetables at dinner promotes intake of both of these types of foods among young children.68 Parents were taught specific strategies to use portion size positively to increase the intake of more nutritious foods.66,71 The goal was to convey the notion that foods need to be balanced within a meal and portion sizes matched to the child’s age. Practical guidance on how parents can become positive role models was provided through both the social media platform and on-the-ground implementation.72,73
Choose nutritious and varied options.
Introducing a broader variety of foods from within and across food groups into children’s diets has nutritional benefits, as does reducing sugars and fats that are eaten in excess. Variety in foods can be a driver of sensory enjoyment and can be shaped to increase consumption of healthier, nutrient-rich foods.74 Among the strategies found to be effective in increasing the consumption of healthy foods at home are the use of a variety of vegetables and fruits as snacks and side dishes and the incorporation of vegetables and fruits into main dishes.71,75,76 Providing children with balanced food choices while avoiding overt food restrictions was identified as a successful technique.77,78 The U4HK program provided practical ideas and tips for improving dietary variety, building on strategies such as repeated exposure, modeling eating healthy foods, and involving children in preparing nutritious meals.81–84
Choose to drink water.
Another goal was to make water the preferred choice over sugar-sweetened beverages.85–88 To achieve this, the water supply needs to be accessible, safe, reliable, and affordable. The U4HK program provided information about the role of water in hydration and why water should be the preferred beverage for hydration. Practical guidance included strategies to make drinking water fun and attractive.87
Enjoy meals together.
The behavioral structure of meals is a component of a healthy lifestyle.88–91 Where, how, and with whom children eat, as well as for how long they eat, can affect diet quality and body weight.92–96 In some studies, frequent family meals were linked to lower risk of childhood overweight.89,97 Family meals also provide time for interactions that can help children’s social and emotional development.98,99 The U4HK program gave practical guidance on how to provide structure and create a positive environment during mealtime while avoiding distractions at the table in order to increase children’s consumption of a variety of nutrient-rich foods.99 Toys, books, smartphones, and television may not be compatible with mindful eating.
Feed your baby like a baby.
Adequate nutrition during the first 1000 days of life, from conception, through pregnancy, and up to 2 years of age, is vital for infant growth and development.100–104 Dietary intake studies often show that infants consume foods and beverages that are not appropriate for their age105,106 and that nutrient requirements are not met. The U4HK program provided practical guidance to promote exclusive breastfeeding for 6 months and continued breastfeeding for up to 24 months and to encourage responsive feeding (ie, looking for cues of hunger and satiety) to benefit infants’ nutritional status. Dietary patterns are established by age 2 years. Early exposure to a greater variety of nutritious foods may lead to preferences for a diversity of foods throughout childhood and beyond.105,107
Move more, sit less.
Regular physical activity is an integral part of a healthy lifestyle for children.108 It helps develop motor skills and promotes decision-making, attention, and teamwork.108,109 Materials to encourage physical activity provided guidance for parents to motivate their children to spend more time being physically active and less time being sedentary (eg, using digital devices). That guidance took into consideration certain limitations such as dangerous living environments or financial constraints.
The overarching goal was to deliver consistent and positively framed messages and interventions rooted in nutritional and behavioral sciences.110,111 Each country or region selected which of these behavioral goals to implement, depending on local needs and the local context. The use of social media allowed the program content to be adapted to the specific nutritional needs, health priorities, and available resources in each country.
ROLE OF SOCIAL MEDIA AND MASS MEDIA
Capable of reaching large parts of populations in most countries, modern technologies such as social media are fast becoming an essential component of nutrition intervention programs at the population level. The new technologies are engaging and can promote networking and community building among parents and caregivers.112 Television, newspapers, and radio can raise awareness, influence attitudes and beliefs, and affect public opinion.111,113,114 In multiple studies, greater exposure to Internet-based intervention content has been consistently associated with greater effectiveness.111,115 Electronic health (e-health) and mobile health (m-health) methods, especially when paired with goal setting and self-monitoring, can have a larger impact on public health than the traditional face-to-face approaches to health education.116 Moreover, with the rapid growth of the Internet and the use of mobile devices in developing countries, such methods are increasingly being used among low- and middle-income populations to improve physical activity and eating behavior.116 However, not all populations use, or have equal access to, social media or mass media. In the U4HK program, therefore, it was important to choose the right mix of outreach approaches and channels to parents. For example, in the Philippines, short and memorable messages relevant to the local behaviors were aired through a radio station rather than on TV. Additional on-ground community activities became part of the program in order to permit access by parents across all socioeconomic classes.
SOCIAL MARKETING: BALANCING RISKS AND BENEFITS
Another strategy that uses mass communication channels to promote health behavior change is social marketing. Social marketing has been defined as the systematic application of marketing, alongside other concepts and techniques, to achieve specific behavioral goals for a social good.117 Social marketing programs focus on the application of 6 core concepts to increase the efficiency and impact of social programs: (1) explicit social goals; (2) citizen-focused planning and delivery; (3) citizen-perceived value as assessed via the social marketing mix; (5) data- and insight-informed audience segmentation, analysis of competition, barriers, assets, and action plan; and (6) development of systemic, strategic, and reflexive programs.
Interventions using a social marketing approach can encourage healthier lifestyles.40,118–120 Both the Change4Life26 and the EPODE28 programs have applied social marketing strategies to change lifestyles and environmental factors and to reduce the risk of childhood obesity. However, the application of social marketing differed between the 2 programs. While EPODE was inspired by social marketing theory, it was not designed solely on the basis of social marketing benchmarks.121 By contrast, Change4Life used social marketing principles together with the help of private marketing agencies to create a social movement within the United Kingdom. Social marketing can be used as part of a strategy to develop a social movement by engaging target audiences in the selection, design, implementation, and evaluation of social programs. Used in this way, social marketing is a powerful tool for engaging citizens and creating ownership and responsibility rather than a more top-down, expert-driven approach to social change.
Although the effects of EPODE’s predecessor, the Fleurbaix Laventie Ville Santé Study, were published in 2009122 and the effects of EPODE in France appeared promising in 2010,123 other studies of the effects of EPODE have not yet been published. Thus, the overall impact of EPODE is unclear. The EPODE for the Promotion of Health Equity studies conclude that effects of EPODE’s integrated community-based approach can be seen in differences in children’s lifestyle behaviors and parental practices; however, a 1-year follow-up assessment suggests that the long-term effects of the program may be limited.124,125
Although it can be challenging to specifically evaluate the role of social marketing in a comprehensive program like EPODE, several of the affiliated programs that used the EPODE approach have shown promising outcomes. For example, both the Belgian program VIASANO and the Dutch program Young People at a Healthy Weight showed decreases in weight status and improvements in behavior after using social marketing.87,126 For some of the EPODE and related programs, the publications lack details about the activities implemented and the social marketing strategies used, thereby limiting the ability to replicate successful methods elsewhere.
In contrast, the Change4Life program was based on social marketing principles using specialists from both public and private sectors to inform the program and was developed and described thoroughly.127,128 Emphasis was placed on evaluation to create and optimize a program that focused on targeted segments of families with young children. Multiple process and impact evaluations have been conducted of specific interventions or elements of the program.26,41,127,129,130 There appears to be substantial evidence that engagement in Change4Life positively influences change toward more-healthy eating.127 These results provide encouraging evidence that Change4Life made progress toward its aim to create a social movement to sustain the program over the long term.
MONITORING A SOCIAL MOVEMENT
Social movements critically depend on working collaborations to understand the local needs, social environment, and culture as well as the likely barriers and challenges. A social movement develops when multiple elements of society, such as families, nonprofit organizations, government, and private industry, take action to promote change for a specific societal benefit. Key to a successful social movement is insight into how messages are shared, how interaction is sustained over time, what motivates participants, and what barriers participants face.131 Interactions on social networks drive more people with the ambition of making a long-lasting, positive impact on society to become engaged, and a dynamic can be built that is cumulative and sustained in its effect. Like the Change4Life initiative in the United Kingdom, the U4HK program aims to inspire and mobilize people into collective action that results in the formation of a self-sustaining social movement to improve children’s health behaviors. Change4Life used social marketing principles to create a social movement by building partnerships with many sectors, using tactics such as community outreach to engage citizens in the program development, and establishing forums to allow private-sector partners to offer input on how to increase the impact of the program.
A social movement is not a controllable approach to change. Its success depends on whether the messages used are aligned with the needs, desires, values, and goals of the target population and whether leadership is present to define the goals of the movement, to establish the tactics to be used, and to mobilize and coordinate collective action.132,133 A social movement has the potential to influence public policy to promote change through the simultaneous actions of family, government, public and private organizations, and civil society. However, appeals to improve health and reduce body weight have not proved motivating enough for the general public.134 Stealth interventions have been considered a potentially important additive to the creation of a social movement,134 and a combination of approaches would likely be the most impactful.
IMPLEMENTATION AND MONITORING
Approaches to implementation of social marketing techniques need to be tailored to the local environment in order to address the primary needs of the target population and to address barriers to behavioral change in a way that is culturally appropriate. As an example of how the U4HK program was implemented in two countries that differ greatly in terms of both the culture and nutritional challenges, 2 pilot markets, Mexico and the Philippines, are described. Mexico currently has the higher prevalence of childhood obesity,135 while the major concerns in the Philippines are nutritional deficiencies and a high prevalence of stunting (30%).135
Mexico
The Mexican U4HK pilot program had 4 primary partners: the Ministry of Health, the Ministry of Public Education, the Kimberly-Clark Corporation, and Televisa. The Ministry of Health endorsed the program, which was launched on the Ministry’s premises. The behavioral content selected by in-country Mexican partners was chosen to align with an ongoing governmental campaign.136 The following goals were selected: manage portions; choose nutritious and varied options; choose to drink water; feed your baby like a baby; and move more, sit less. Focus groups were conducted with Mexican parents and other caregivers (eg, grandparents) to explore both motivating factors and barriers to achieving these goals.
Multiple communication channels created awareness and reached large segments of the population. The largest national TV network, Televisa, helped to create a new format of TV shows by combining elements of a reality show and a talk show and featuring interventions based on behaviors described in the U4HK program. The show was broadcast weekly for 26 weeks. Specialists with different fields of expertise (pediatrics, psychology, and nutrition) monitored and guided families through the interventions over the course of the 26 weeks. The 5 families that participated in the TV show underwent a detailed nutritional and health assessment before and after the show. There were promising changes in the dietary habits of the families, with the estimated consumption of fruits and vegetables increasing by 120% among adults and by 104% among children. In 2014, the TV show reached an estimated 5 million parents and caregivers weekly. Consumer research showed that viewers of the TV show were more familiar with the behavioral goals and placed a higher importance on children’s physical activity.
The television program was successful in building awareness but was resource intensive to produce. Once consumers were aware of the program, communications shifted toward digital resources, and new content was created specifically for dissemination through Facebook, YouTube, and Twitter. Overall, digital media generated a total of 13.5 million exposures to the audience in 2014 alone: 10.3 million views on Facebook, 2 million views on YouTube, and 1.2 million visits to websites. As the messaging became amplified by external press, the program snowballed to include more than the original partners. An additional 34 million exposures of the U4HK messages were generated in the form of published articles, mass media releases, and blogs. There is also some evidence that related groups, such as United for my Healthy Community, were created and linked on Facebook.
Historically, campaigns of this nature have focused almost exclusively on the number of people reached and how those people interact online with the content,137 with little emphasis on the effects of the program on behavioral change. To address this gap, a study was conducted to assess the impact of a Facebook campaign on consumers’ shopping habits.138 The research participants were families with school-aged children who were members of a Kantar consumer panel, a group that scans their grocery purchases into a database. The study tracked the families’ exposure to Facebook messages using embedded cookies and examined associations with the nutritional quality of the family food purchases. Results showed that families who were exposed to at least 4 messages bought significantly healthier groceries, with increases in fruit and vegetable purchases and decreases in pastry and fast food purchases. There was a trend for an association between increased exposure to the Facebook content and better nutritional quality. This promising demonstration of the potential impact of social media on health behaviors merits further exploration.
Two offline interventions featuring physical tools were developed. The first was a portioned plate designed to help families balance the intake of different food groups. The Mexican Ministry of Health distributed 40 000 of these plates and conducted 4 workshops for parents to provide information about portion size. Another intervention was developed through an industry partnership with the Kimberly-Clark Corporation, which printed fun characters, so-called grease monsters, on napkins and paper towels to encourage consumers to remove excessive grease from fried foods. In August of 2016 alone, over 20 million napkins were sold (corresponding to over 225 000 packages). This demonstrates how nudges for behavioral changes can be incorporated into existing commercial products at little cost to the industrial partner in order to benefit the local population.
The Philippines
In an intervention conducted in the Philippines, 4 behavioral goals were selected on the basis of local public health needs: manage portions; choose nutritious and varied options; choose to drink water; and enjoy meals together. The program initially targeted employees of Nestlé Philippines who had children aged 4 to 12 years. Partners from the public and private sectors included the Food and Nutrition Research Institute, the Department of Tourism, the Central Bank of the Philippines, and Facebook and other private companies. Multiple workshops and brainstorming sessions with partners were held. Once on board, employees of partner organizations were reached through the same employee engagement program.
The national TV broadcasting company helped both in organizing the formal nationwide launch of the program at prime time and in disseminating the content. A new concept called “food economics” addressed the main drivers of food choice, notably taste, affordability, availability, and cultural acceptance. Recipes were developed for school cafeterias and for parents to prepare nutrient-rich meals at home. The next steps were to provide practical tips for parents on how to prepare tasty meals with high nutritional value at an affordable cost. The U4HK program has partnered with a network of nongovernmental organizations to engage parents by providing nutritional education and practical culinary instruction that is being field tested by National Food and Nutrition Research Institute.
This content was communicated to parents via digital channels, reaching over 18 million mothers in the Philippines. The Facebook group now has more than 200 000 fans, and the U4HK website generated 30 000 unique visits and 150 000 page views within 2 weeks. When exposures from all communication channels such as digital media, broadcast TV, and the press are combined, more than 150 million exposures to the audience can be estimated. Responses to the U4HK program and the nutrition-related content overall were positive.
A Nestlé-sponsored initiative was launched in 2016 to raise public awareness of hunger and malnutrition and to encourage people to volunteer at and donate to local nongovernmental organizations. Several digital platforms, including a website, YouTube (messages from celebrity ambassadors), and Twitter (#HangryAboutHunger), were used to disseminate content. A launch event featured presentations by government partners and officials, including the vice president of the Philippines. Using a social listening model, which has been previously used by researchers to monitor the rate of mentions of medical conditions,139,140 mentions of malnutrition on social media in the Philippines were compared with mentions of other issues. In the first 4 months after the launch, mentions of malnutrition on social media doubled, making malnutrition the third most discussed issue on social media in the Philippines, after human rights and climate change. The likely impact of increased awareness on volunteering and donating to food-related nongovernmental organizations is being measured.
Table 2 provides a more complete overview of U4HK’s reach across several countries.
Table 2.
United for Healthier Kids (U4HK) results through March 2017
| Country/region | Launch date | Mass media and digital |
On-ground participation |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Reach of program |
Engagement |
|||||||||
| Unique visits to website | Unique consumers reached (FB, Instagram) | Views (YouTube) or impressions (Twitter) | Impressions (press, TV, radio, print, others)a | Active app downloadsa | Interactions with U4HK FB contentb | Parents/children participating in U4HK activationsa | Parents/children attending U4HK nutrition consultationsa | Parents/children at U4HK-sponsored eventsa | ||
| Brazil | May 2015 | 35 000 | 419 849 | NA | 4100 | NA | 95 000 | 6900 | NA | NA |
| Central Americac | September 2015 | 159 152 | 26 197 351 | NA | 550 000 | NA | ND | 320 | 7982 | 1500 |
| Ecuador | November 2016 | NA | 1 7494 09 | 132 124 | 8 359 300 | NA | ND | NA | NA | NA |
| Egypt | April 2016 | 30 000 | 15 000 000 | 238 604 | 3 451 740 | NA | 37 000 | NA | NA | NA |
| Mexico | August 2014 | 1 275 427 | 67 314 119 | 11 022 199 | 274 000 000 | 17 078 | 2 242 418 | 140 000 | NA | NA |
| Middle Eastd | October 2015 | 261 565 | 29 201 146 | 13 302 739 | 3 000 000 | 92 000 | 45 011 | ND | NA | NA |
| Pakistan | August 2016 | 115 249 | 10 100 000 | 3 420 000 | 14 400 000 | NA | ND | ND | NA | NA |
| The Philippines | September 2014 | 133 544 | 8 492 483 | NA | 38 000 000 | NA | ND | ND | NA | NA |
| Switzerland | November 2016 | 1538 | NA | 1 200 000 | 1 200 000 | NA | ND | 150 | NA | NA |
| Thailand | June 2016 | NA | 14 811 702 | NA | 27 418 872 | NA | ND | 1261 | NA | NA |
Abbreviations: FB, Facebook; NA, not applicable; ND, no data.
Figure extracted from December 2016 report.
Facebook clicks, likes, views.
Panama and Guatemala.
United Arab Emirates, Lebanon, Kuwait, Jordan, Kingdom of Saudi Arabia.
A PLAN FOR EVALUATION
The U4HK program is a complex multisector intervention with a population-wide reach. It has now been launched in 11 countries, and there are plans for subsequent expansion to other countries and regions. Each of the 11 countries performed a local assessment of the nutritional situation, developed a plan for local engagement with public and private partners, and selected relevant behavioral goals. Table 3135,141 summarizes the U4HK program in place in these 11 countries.
Table 3.
Overview of the use of social media, digital assets, and offline activities in the multicountry program United for Healthier Kids (U4HK)
| Country/region | Stunting/overweight (year of survey)a | Behaviors targetedb | U4HK digital assets |
No. of partners | Government partners | Other partners | Nondigital activities | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Website | Twitter/Instagram | YouTube | Mobile | ||||||||
| Brazil | 7.1%/7.3% (2007) | 2, 4, 6 | ✓ | ✓ | ✓ | 22 | Municipal secretaries of education | NGOs, industry, media | Gamified activities at school and home | ||
| Ecuador | 25.2%/7.5% (2012–2013) | 1, 2, 4, 5, 6 | ✓ | 4 | Ministry of Education, Municipality of Quito | Media, chefs association | TV series | ||||
| Egypt | 22.3%/15.7% (2014) | 1, 2, 4, 5, 6 | ✓ | ✓ | ✓ | 6 | Ministry of Social Solidarity | Academia, industry, media | Distribution of breastfeeding covers; pilot intervention in village | ||
| Guatemala | 46.5%/4.7% (2014–2015) | 1, 2 | ✓ | ✓ | 4 | Secretary of Food Security and Nutrition | NGOs, university, media | TV and radio spots, mobile nutritional consultations | |||
| Mexico | 9.0%/13.6% (2011–2012) | 1, 2, 4, 5, 6 | ✓ | ✓ | ✓c | ✓ | app | 20 | Ministry of Health, Ministry of Education | Academia, industry, media | TV program; portion plates/guides; grease monster napkins |
| Middle East | 15.4%/10.7% (2016) | 1, 2, 4, 6 | ✓ | ✓ | ✓ | ✓ | app | 11 | Dubai Health Authority | Academia, industry, media | Book; supermarket campaign |
| Pakistan | 45.0%/4.8% (2012–2013) | 2, 4, 6 | ✓ | ✓ | ✓ | ✓ | SMS | 5 | Ministry of Planning and Development | Industry, media | Activities in local stores and schools |
| Panama | 19.1%/NA (2008) | 1, 2, 4, 6 | ✓ | ✓ | Consultation via app | 5 | Ministry of Health, Ministry of Education | Nutritionist association, media | TV clips; sponsored sports events; school activities | ||
| Philippines | 30.3%/5.0% (2013–2014) | 1, 2, 4 | ✓ | ✓ | ✓ | ✓ | 14 | Academia, NGOs, media | Pilot nutritional intervention; volunteerism platform | ||
| Switzerland | NA/11% (2017)d | 1, 2, 3, 4 | ✓ | ✓ | 2 | Chefs association | Cooking classes | ||||
| Thailand | 16.3%/10.8% (2012) | 2, 4, 6 | ✓ | 5 | Ministry of Education | Academia, media | School program with portion plates | ||||
Abbreviations: app, application; NGO, nongovernmental organization; SMS, short message service (ie, text message).
Data extracted from UNICEF/World Health Organization/World Bank Group—Joint Child Malnutrition Estimates, 2017.135
1, Manage portions; 2, choose nutritious and varied options; 3, enjoy meals together; 4, choose to drink water; 5, feed your baby like a baby; 6, move more, sit less.
These assets were launched but are no longer active.
Data extracted from Stamm et al (2017).141
From its inception to the end of 2016, the U4HK program reached over 3.8 million parents through websites, social media pages, and on-ground activities, with many more messages communicated through social media (YouTube, Twitter) and traditional media (eg, TV, radio, print). Attesting to its multisector engagement, U4HK is currently collaborating with some 50 diverse partners and stakeholder groups.
Metrics to assess the success of complex approaches, community engagement, and social movements are themselves complex. The design, sampling, and data collection methods used with PPE initiatives, the influence of the physical, social, or economic environment, the secular trends, and the duration or intensity of interventions do not lend themselves to easy statistical analysis.142–147 Interventions driven by social media cannot be tested using classic randomized controlled trials.116,148
Despite these challenges, it is essential to monitor the various PPE programs and evaluate their outcomes in order to enable large-scale reach and behavior change. Evaluating the impact of such programs is challenging: it is difficult to attribute specific effects to particular components of an intervention, since social marketing campaigns can work through both direct and indirect pathways.111 Factors external to PPE interventions may also add or subtract from their impact.
To evaluate a complex program, evaluators will need to go beyond the traditional notions of evaluation research and experimental design.145,148–150 To increase the impact and sustainability of the program, it will be helpful to involve target groups and stakeholders in the design, implementation, and evaluation.151,152 However, this more participatory evaluation approach often means that the intervention will change during the implementation process, and this cannot be foreseen in the planning stage.153 Interventions will also evolve depending on available resources (eg, budget, human resources), the needs of stakeholders, and the environment.145,154 Of note, previous studies using social media as a means of behavior change have often reported very high attrition rates,155 likely reflecting the nature of how people use these tools in real life. Studies that can capture how many people drop out of a study in the absence of laboratory or field visits and incentives will give better estimates of the potential impact of the intervention on the general population.
The first goal of evaluation is to demonstrate the progress achieved against the set of public health nutrition goals and objectives. To be successful, interventions driven by PPE need to be subject to rigorous, locally sensitive, continuous evaluation. Annual targets are set by each country on the basis of local priorities and activation plans. The evaluation of the program is comprised of process measures, measures of reach (eg, number of parents and children reached), and measures of the level of engagement achieved, as well as measures of behavior change intent, claimed behavior change, and objectively measured behavior change. Independent researchers and research agencies are part of this process at both the global and the local levels.
The second goal of evaluation is to promote transparency and communication: progress reports relative to a defined goal need to be shared with governmental as well as nongovernmental partners, including the scientific community and the general public. The third goal of evaluation is to optimize accountability by strengthening and amplifying those aspects of the program that work and by refining or removing those aspects that were not successful.
ACCOUNTABILITY AND GLOBAL REACH
The ability of for-profit organizations to act as leaders or facilitators of initiatives in public health nutrition needs to be constantly evaluated and open to public scrutiny. The proposed evaluations of U4HK will track the impact of interventions on health outcomes, the relative efficiency of the U4HK program, and the return on investment. Additional process measures should assess the effect of PPE on future broad-reaching, sustained collaborations between the private sector, public agencies, and civil society. Outcome and process evaluations are needed to assess whether PPE strategies can make a measurable impact on global public health. Those efforts are spelled out in the World Health Organization position on protecting public health goals and programs from industry-related conflicts of interest. Consistent with these rules of conduct, the U4HK program has been and will be continuously monitored and evaluated to ensure the projected milestones and success criteria are met. Given the need for health interventions that extend beyond local political cycles, the global goals were set for a time horizon of 10 years and beyond.
CONCLUSION
Public–private partnerships have proven to be effective in addressing the double burden of malnutrition. Reaching parents directly through social marketing strategies built around social and mass media is a relatively new approach, identified here as PPE. It is imperative that PPE programs follow the principles and rules of engagement previously formulated for PPPs. The U4HK program is an example of how such programs can be introduced and implemented in multiple countries.
Acknowledgments
The authors would like to thank the U4HK project manager, Inti Pérez, as well as the teams in each U4HK country for their support in providing local data about the program.
Author contributions.
A.D., B.J.R., B.C., A.M.P., J.K.D., and P.K.-W. conceived the idea for the current review. T.M.v.K. drafted the original manuscript, and A.D., P.K.-W., L.R.F., and J.F. drafted additional sections. All authors provided intellectual contributions to the revisions of the manuscript. A.D. and L.R.F. were responsible for reorganizing and finalizing the manuscript. All authors critically reviewed and approved the final manuscript.
Funding/support.
No external funds supported this work.
Declaration of interest.
A.D., A.M.P., B.C., B.J.R., J.K.D., and J.F. are members of the Scientific Advisory Board for U4HK and receive a compensation for their services. M.v.K. was compensated for literature search and editorial work as a consultant to Nestlé. L.R.F. and P.K. are Nestlé employees. A.D. is a member of the Nestlé Scientific Advisory Board and has received grants, contracts, and honoraria from private industry, foundations, and public agencies for projects on nutrient profiling, diet quality, and health. The authors have no other relevant interests to declare.
References
- 1. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–451. [DOI] [PubMed] [Google Scholar]
- 2. Tzioumis E, Adair LS.. Childhood dual burden of under- and over-nutrition in low- and middle-income countries: a critical review. Food Nutr Bull. 2014;35:230–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Abdullah A. The double burden of undernutrition and overnutrition in developing countries: an update. Curr Obes Rep. 2015;4:337–349. [DOI] [PubMed] [Google Scholar]
- 4. Caballero B. A nutrition paradox—underweight and obesity in developing countries. N Engl J Med. 2005;352:1514–1516. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization. Global Nutrition Targets 2025: Policy Brief Series .Geneva, Switzerland: World Health Organization; 2014. WHO reference no. WHO/NMH/NHD/14.2. [Google Scholar]
- 6. Commission on Ending Childhood Obesity. Report of the Commission on Ending Childhood Obesity. Geneva, Switzerland: World Health Organization; 2016. [Google Scholar]
- 7. Dobbs R, Sawers C, Thompson F, et al. How the World Could Better Fight Obesity.www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/how-the-world-could-better-fight-obesity. Published November 2014. Accessed July 12, 2018.
- 8. Popkin BM, Adair LS, Ng SW.. Now and then: the Global Nutrition Transition: the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Freire WB, Silva-Jaramillo KM, Ramirez-Luzuriaga MJ, et al. The double burden of undernutrition and excess body weight in Ecuador. Am J Clin Nutr. 2014;100:1636S–1643S. [DOI] [PubMed] [Google Scholar]
- 10. Oddo VM, Rah JH, Semba RD, et al. Predictors of maternal and child double burden of malnutrition in rural Indonesia and Bangladesh. Am J Clin Nutr. 2012;95:951–958. [DOI] [PubMed] [Google Scholar]
- 11. Rivera JA, Pedraza LS, Martorell R, et al. Introduction to the double burden of undernutrition and excess weight in Latin America. Am J Clin Nutr. 2014;100:1613S–1616S. [DOI] [PubMed] [Google Scholar]
- 12. Hoddinott JF, Gillespie S, Yosef S.. Public-Private Partnerships and the Reduction of Undernutrition in Developing Countries http://ebrary.ifpri.org/cdm/ref/collection/p15738coll2/id/129857. Discussion paper 1487. Washington, DC: International Food Policy Research Institute; 2015. Accessed November 20, 2016.
- 13. United Nations System Standing Committee on Nutrition. Nutrition and business, how to engage? SCN News. 2011;39:1–107. Available at: http://www.unscn.org/files/Publications/SCN_News/SCNNEWS39_10.01_high_def.pdf. Accessed July 16, 2018 [Google Scholar]
- 14. Food and Agriculture Organization of the United Nations, International Fund for Agricultural Development, World Food Programme. The State of Food Insecurity in the World 2014. Strengthening the Enabling Environment for Food Security and Nutrition. Rome, Italy: Food and Agriculture Organization of the United Nations; 2014. [Google Scholar]
- 15.We can end poverty; millennium development goals and beyond 2015. United Nations website. http://www.un.org/millenniumgoals/. Accessed May 26, 2015.
- 16. World Health Organization. Global Nutrition Policy Review: What Does It Take to Scale up Nutrition Action? http://www.who.int/nutrition/publications/policies/global_nut_policyreview/en/. Published 2013. Accessed July 16, 2018. [Google Scholar]
- 17. Kraak VI, Harrigan PB, Lawrence M, et al. Balancing the benefits and risks of public–private partnerships to address the global double burden of malnutrition. Public Health Nutr. 2012;15:503–517. [DOI] [PubMed] [Google Scholar]
- 18. Eggersdorfer M, Bird JK.. How to achieve transparency in public-private partnerships engaged in hunger and malnutrition reduction. World Rev Nutr Diet. 2016;115:224–232. [DOI] [PubMed] [Google Scholar]
- 19. Evans WD, Necheles J, Longjohn M, et al. The 5-4-3-2-1 Go! intervention: social marketing strategies for nutrition. J Nutr Educ Behav. 2007;39:S55–S59. [DOI] [PubMed] [Google Scholar]
- 20. Lefebvre RC, Olander C, Levine E.. The impact of multiple channel delivery of nutrition messages on student knowledge, motivation and behavior: results from the Team Nutrition pilot study. Soc Mar Q. 1999;5:90–98. [Google Scholar]
- 21. Hoelscher DM, Moag-Stahlberg A, Ellis K, et al. Evaluation of a student participatory, low-intensity program to improve school wellness environment and students’ eating and activity behaviors. Int J Behav Nutr Phys Act. 2016;13:59. doi:10.1186/s12966-016-0379-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Thomas IM, Sayers SP, Godon JL, et al. Bike, walk, and wheel: a way of life in Columbia, Missouri. Am J Prev Med. 2009;37:S322–S328. [DOI] [PubMed] [Google Scholar]
- 23. Tobey LN, Manore MM.. Social media and nutrition education: the Food Hero experience. J Nutr Educ Behav. 2014;46:128–133. [DOI] [PubMed] [Google Scholar]
- 24. UNICEF Kid Power. UNICEF Kid Power website. http://unicefkidpower.org. Accessed July 18, 2018.
- 25. Hoffman JA, Morris V, Cook J.. The Boston Middle School-Corner Store Initiative: development, implementation, and initial evaluation of a program designed to improve adolescents’ beverage-purchasing behaviors. Psychol Sch. 2009;46:756–766. [Google Scholar]
- 26. HM Government. Change4Life One Year On. In Support of Healthy Weight, Healthy Lives. London, UK: HM Government; 2010. Available at: http://webarchive.nationalarchives.gov.uk/20130124053508/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_115511.pdf [Google Scholar]
- 27. Te Velde S, Brug J, Wind M, et al. Effects of a comprehensive fruit- and vegetable-promoting school-based intervention in three European countries: the Pro Children study. Br J Nutr. 2008;99:893–903. [DOI] [PubMed] [Google Scholar]
- 28. Borys JM, Le Bodo Y, Jebb SA, et al. EPODE approach for childhood obesity prevention: methods, progress and international development. Obes Rev. 2012;13:299–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Marcus C, Nyberg G, Nordenfelt A, et al. A 4-year, cluster-randomized, controlled childhood obesity prevention study: STOPP. Int J Obes. 2009;33:408. doi:10.1038/ijo.2009.38 [DOI] [PubMed] [Google Scholar]
- 30. Campbell KJ, Hesketh KD, McNaughton SA, et al. The extended Infant Feeding, Activity and Nutrition Trial (InFANT Extend) Program: a cluster-randomized controlled trial of an early intervention to prevent childhood obesity. BMC Pub Health. 2016;16:166. doi:10.1186/s12889-016-2836-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sanigorski AM, Bell A, Kremer PJ, et al. Reducing unhealthy weight gain in children through community capacity-building: results of a quasi-experimental intervention program, Be Active Eat Well. Int J Obes. 2008;32:1060. doi:10.1038/ijo.2008.79 [DOI] [PubMed] [Google Scholar]
- 32. Gittelsohn J, Dyckman W, Tan ML, et al. Development and implementation of a food store–based intervention to improve diet in the Republic of the Marshall Islands. Health Promot Pract. 2006;7:396–405. [DOI] [PubMed] [Google Scholar]
- 33. Kaufer L, Englberger L, Cue R, et al. Evaluation of a “traditional food for health” intervention in Pohnpei, Federated States of Micronesia. Pac Health Dialog. 2010;16:61–73. [PubMed] [Google Scholar]
- 34. Dangour AD, Diaz Z, Sullivan LM.. Building global advocacy for nutrition: a review of the European and U.S. landscapes. Food Nutr Bull. 2012;33:92–98. [DOI] [PubMed] [Google Scholar]
- 35. Van Koperen TM, Jebb SA, Summerbell CD, et al. Characterizing the EPODE logic model: unravelling the past and informing the future. Obes Rev. 2013;14:162–170. [DOI] [PubMed] [Google Scholar]
- 36. Levine E, Olander C, Lefebvre C, et al. The Team Nutrition pilot study: lessons learned from implementing a comprehensive school-based intervention. J Nutr Educ Behav. 2002;34:109–116. [DOI] [PubMed] [Google Scholar]
- 37. Sayers SP, LeMaster JW, Thomas IM, et al. Bike, walk, and wheel: a way of life in Columbia, Missouri, revisited. Am J Prev Med. 2012;43:S379–S383. [DOI] [PubMed] [Google Scholar]
- 38. Tobey L, Koenig H, Brown N, et al. Reaching low-income mothers to improve family fruit and vegetable intake: Food Hero social marketing campaign—research steps, development and testing. Nutrients. 2016;8:562. doi:10.3390/nu8090562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bai Y, Saint-Maurice PF, Welk GJ, et al. The longitudinal impact of NFL PLAY 60 programming on youth aerobic capacity and BMI. Am J Prev Med. 2017;52:311–323. [DOI] [PubMed] [Google Scholar]
- 40. Aceves-Martins M, Llauradó E, Tarro L, et al. Effectiveness of social marketing strategies to reduce youth obesity in European school-based interventions: a systematic review and meta-analysis. Nutr Rev. 2016;74:337–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Adams J, Halligan J, Burges Watson D, et al. The Change4Life convenience store programme to increase retail access to fresh fruit and vegetables: a mixed methods process evaluation. PLoS One. 2012;7:e39431. doi:10.1371/journal.pone.0039431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Williams G, Hamm MP, Shulhan J, et al. Social media interventions for diet and exercise behaviours: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2014;4:e003926. doi:10.1136/bmjopen-2013-003926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Chang T, Chopra V, Zhang C, et al. The role of social media in online weight management: systematic review. J Med Internet Res. 2013;15:e262. doi:10.2196/jmir.2852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hamm MP, Shulhan J, Williams G, et al. A systematic review of the use and effectiveness of social media in child health. BMC Pediatr. 2014;14:138. doi:10.1186/1471-2431-14-138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Katan MB. Weight-loss diets for the prevention and treatment of obesity. N Engl J Med. 2009;360:923–925. [DOI] [PubMed] [Google Scholar]
- 46. Kraak VI, Kumanyika SK, Story M.. The commercial marketing of healthy lifestyles to address the global child and adolescent obesity pandemic: prospects, pitfalls and priorities. Public Health Nutr. 2009;12:2027–2036. [DOI] [PubMed] [Google Scholar]
- 47. World Health Organization. Global Strategy on Diet, Physical Activity and Health: A framework to monitor and evaluate implementation,. http://www.who.int/dietphysicalactivity/Indicators%20English.pdf. Published 2006. Accessed July 18, 2018. [Google Scholar]
- 48. The Lancet. Change4Life brought to you by PepsiCo (and others). Lancet. 2009;373:96. [DOI] [PubMed] [Google Scholar]
- 49. Nestle M. Food industry and health: mostly promises, little action. Lancet. 2006;368:564–565. [DOI] [PubMed] [Google Scholar]
- 50. Kinner K, Pellegrini C.. Expenditures for public health: assessing historical and prospective trends. Am J Public Health. 2009;99:1780–1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Himmelstein DU, Woolhandler S.. Public health’s falling share of US health spending. Am J Public Health. 2016;106:56–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gottret P, Schieber G. In: Health Financing Revisited: A Practioner’s Guide. Washington, DC: World Bank; 2006. [Google Scholar]
- 53. Gottret P, Schieber G.. Health transitions, disease burdens, and health expenditure patterns In: Health Financing Revisited: A Practitioner’s Guide. World Bank: Washington, DC, USA: 2006:23–39. [Google Scholar]
- 54. Rowe S, Alexander N, Kretser A, et al. Principles for building public-private partnerships to benefit food safety, nutrition, and health research. Nutr Rev. 2013;71:682–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Creating shared value. Nestlé website. https://www.nestle.com/csv/what-is-csv. Accessed July 18, 2018.
- 56.Our commitments. Nestlé website. http://www.nestle.com/csv/what-is-csv/commitments. Accessed July 18, 2018.
- 57. Dahlgren G, Whitehead M.. Policies and Strategies to Promote Social Equality in Health. Stockholm, Sweden: Institute of Future Studies; 1991. [Google Scholar]
- 58. Lobstein T, Baur L, Uauy R.. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5:4–85. [DOI] [PubMed] [Google Scholar]
- 59. Sallis JF, Owen N, Fisher E.. Ecological models of health behavior In: Health Behavior: Theory, Research, and Practice. 5th ed.San Francisco, CA: Jossey-Bass; 2015: 43–64. [Google Scholar]
- 60. Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371:340–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kral TVE, Rolls BJ.. Portion size and the obesity epidemic In: Cawley J, ed. The Oxford Handbook of the Social Science of Obesity. Oxford, England: Oxford University Press; 2011: 367–384. [Google Scholar]
- 62. Rolls BJ, Roe LS, Kral TVE, et al. Increasing the portion size of a packaged snack increases energy intake in men and women. Appetite. 2004;42:63–69. [DOI] [PubMed] [Google Scholar]
- 63. Rolls BJ, Engell D, Birch LL.. Serving portion size influences 5-year-old but not 3-year-old children’s food intakes. J Am Diet Assoc. 2000;100:232–234. [DOI] [PubMed] [Google Scholar]
- 64. Rolls BJ, Roe LS, Meengs JS.. The effect of large portion sizes on energy intake is sustained for 11 days. Obesity (Silver Spring.). 2007;15:1535–1543. [DOI] [PubMed] [Google Scholar]
- 65. Fisher JO, Arreola A, Birch LL, et al. Portion size effects on daily energy intake in low-income Hispanic and African American children and their mothers. Am J Clin Nutr. 2007;86:1709–1716. [DOI] [PubMed] [Google Scholar]
- 66. Leahy KE, Birch LL, Fisher JO, et al. Reductions in entree energy density increase children’s vegetable intake and reduce energy intake. Obesity (Silver Spring.). 2008;16:1559–1565. [DOI] [PubMed] [Google Scholar]
- 67. Kling SMR, Roe LS, Keller KL, et al. Double trouble: portion size and energy density combine to increase preschool children’s lunch intake. Physiol Behav. 2016;162:18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Mathias KC, Rolls BJ, Birch LL, et al. Serving larger portions of fruits and vegetables together at dinner promotes intake of both foods among young children. J Acad Nutr Diet. 2012;112:266–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. van Kleef E, Bruggers I, de Vet E.. Encouraging vegetable intake as a snack among children: the influence of portion and unit size. Public Health Nutr. 2015;18:2736–2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Kral TV, Kabay AC, Roe LS, et al. Effects of doubling the portion size of fruit and vegetable side dishes on children’s intake at a meal. Obesity (Silver Spring.). 2010;18:521–527. [DOI] [PubMed] [Google Scholar]
- 71. Spill MK, Birch LL, Roe LS, et al. Hiding vegetables to reduce energy density: an effective strategy to increase children’s vegetable intake and reduce energy intake. Am J Clin Nutr. 2011;94:735–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Johnson SL, Hughes SO, Cui X, et al. Portion sizes for children are predicted by parental characteristics and the amounts parents serve themselves. Am J Clin Nutr 2014;99:763–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Pearson N, Biddle SJ, Gorely T.. Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutr. 2009;12:267–283. [DOI] [PubMed] [Google Scholar]
- 74. Roe LS, Meengs JS, Birch LL, et al. Serving a variety of vegetables and fruit as a snack increased intake in preschool children. Am J Clin Nutr. 2013;98:693–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. de Wild VW, de Graaf C, Boshuizen HC, et al. Influence of choice on vegetable intake in children: an in-home study. Appetite. 2015;91:1–6. [DOI] [PubMed] [Google Scholar]
- 76. Royo-Bordonada MA, Gorgojo L, Ortega H, et al. Greater dietary variety is associated with better biochemical nutritional status in Spanish children: the Four Provinces Study. Nutrit Metab Cardiovasc Dis. 2003;13:357–364. [DOI] [PubMed] [Google Scholar]
- 77. Entin A, Kaufman-Shriqui V, Naggan L, et al. Parental feeding practices in relation to low diet quality and obesity among LSES children. J Am Coll Nutr. 2014;33:306–314. [DOI] [PubMed] [Google Scholar]
- 78. Russell CG, Worsley A, Campbell KJ.. Strategies used by parents to influence their children’s food preferences. Appetite. 2015;90:123–130. [DOI] [PubMed] [Google Scholar]
- 79. Van der Horst K, Ferrage A, Rytz A.. Involving children in meal preparation. Effects on food intake. Appetite. 2014;79:18–24. [DOI] [PubMed] [Google Scholar]
- 80. Rohlfs Domínguez P, Gámiz F, Gil M, et al. Providing choice increases children’s vegetable intake. Food Qual Pref. 2013;30:108–113. [Google Scholar]
- 81. Edelson LR, Mokdad C, Martin N.. Prompts to eat novel and familiar fruits and vegetables in families with 1–3 year-old children: relationships with food acceptance and intake. Appetite. 2016;99:138–148. [DOI] [PubMed] [Google Scholar]
- 82. Anzman-Frasca S, Savage JS, Marini ME, et al. Repeated exposure and associative conditioning promote preschool children’s liking of vegetables. Appetite. 2012;58:543–553. [DOI] [PubMed] [Google Scholar]
- 83. Drewnowski A, Rehm CD, Constant F.. Water and beverage consumption among adults in the United States: cross-sectional study using data from NHANES 2005–2010. BMC Public Health. 2013;13:1068. doi:10.1186/1471-2458-13-1068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Popkin BM, D’Anci KE, Rosenberg IH.. Water, hydration, and health. Nutr Rev. 2010;68:439–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Drewnowski A, Rehm CD, Constant F.. Water and beverage consumption among children age 4-13y in the United States: analyses of 2005–2010 NHANES data. Nutr J. 2013;12:85. doi:10.1186/1475-2891-12-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Vieux F, Maillot M, Constant F, et al. Water and beverage consumption among children aged 4–13 years in France: analyses of INCA 2 (Étude Individuelle Nationale des Consommations Alimentaires 2006–2007) data. Public Health Nutr. 2016;19:2305–2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Van de Gaar VM, Jansen W, Van Grieken A, et al. Effects of an intervention aimed at reducing the intake of sugar-sweetened beverages in primary school children: a controlled trial. Int J Behav Nutr Phys Act. 2014;11:98. doi:10.1186/s12966-014-0098-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Christian MS, Evans CE, Hancock N, et al. Family meals can help children reach their 5 a Day: a cross-sectional survey of children’s dietary intake from London primary schools. J Epidemiol Commun Health. 2013;67:332–338. [DOI] [PubMed] [Google Scholar]
- 89. Taveras EM, Rifas-Shiman SL, Berkey CS, et al. Family dinner and adolescent overweight. Obes Res. 2005;13:900–906. [DOI] [PubMed] [Google Scholar]
- 90. Larsen JK, Hermans RC, Sleddens EF, et al. How parental dietary behavior and food parenting practices affect children’s dietary behavior. Interacting sources of influence? Appetite. 2015;89:246–257. [DOI] [PubMed] [Google Scholar]
- 91. Hughes SO, Patrick H, Power TG, et al. The impact of child care providers’ feeding on children’s food consumption. J Dev Behav Pediatr. 2007;28:100–107. [DOI] [PubMed] [Google Scholar]
- 92. Birch LL, Davison KK.. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin North Am. 2001;48:893–907. [DOI] [PubMed] [Google Scholar]
- 93. Tabbakh T, Freeland-Graves JH.. The home environment: a mediator of nutrition knowledge and diet quality in adolescents. Appetite. 2016;105:46–52. [DOI] [PubMed] [Google Scholar]
- 94. Schrempft S, van Jaarsveld CH, Fisher A, et al. The obesogenic quality of the home environment: associations with diet, physical activity, TV viewing, and BMI in preschool children. PLoS One. 2015;10. doi:10.1371/journal.pone.0134490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Crawford DA, Ball K, Cleland VJ, et al. Home and neighbourhood correlates of BMI among children living in socioeconomically disadvantaged neighbourhoods. Br J Nutr. 2012;107:1028–1036. [DOI] [PubMed] [Google Scholar]
- 96. Veldhuis L, van Grieken A, Renders CM, et al. Parenting style, the home environment, and screen time of 5-year-old children; the ‘be active, eat right’ study. PLoS One. 2014;9:e88486. doi:10.1371/journal.pone.0088486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Nuvoli G. Family meal frequency, weight status and healthy management in children, young adults and seniors. A study in Sardinia, Italy. Appetite. 2015;89:160–166. [DOI] [PubMed] [Google Scholar]
- 98. Pan BA, Perlmann RY, Snow CE.. Food for thought: dinner table as a context for observing parent–child discourse In: Menn L, Ratner NB, eds. Methods for Studying Language Production. Mahwah, NJ: Lawrence Erlbaum Associates; 2000:205–224. [Google Scholar]
- 99. Spagnola M, Fiese BH.. Family routines and rituals: a context for development in the lives of young children. Infants Young Child. 2007;20:284–299. [Google Scholar]
- 100. Emmett PM, Jones LR.. Diet, growth, and obesity development throughout childhood in the Avon Longitudinal Study of Parents and Children. Nutr Rev. 2015;73(suppl 3):175–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Brands B, Demmelmair H, Koletzko B.. How growth due to infant nutrition influences obesity and later disease risk. Acta Paediatr. 2014;103:578–585. [DOI] [PubMed] [Google Scholar]
- 102. Langley-Evans SC. Nutrition in early life and the programming of adult disease: a review. J Hum Nutr Diet. 2015;28(suppl 1):1–14. [DOI] [PubMed] [Google Scholar]
- 103. Woo Baidal JA, Locks LM, Cheng ER, et al. Risk factors for childhood obesity in the first 1,000 days. A systematic review. Am J Prev Med. 2016;50:761–779. [DOI] [PubMed] [Google Scholar]
- 104. Binns C, Lee M, Low WY.. The long-term public health benefits of breastfeeding. Asia Pac J Public Health. 2016;28:7–14. [DOI] [PubMed] [Google Scholar]
- 105. Birch L, Savage JS, Ventura A.. Influences on the development of children’s eating behaviours: from infancy to adolescence. Can J Diet Pract Res. 2007;68:S1–S56. [PMC free article] [PubMed] [Google Scholar]
- 106. Fox MK, Pac S, Devaney B, et al. Feeding infants and toddlers study: what foods are infants and toddlers eating? J Am Diet Assoc. 2004;104(1 suppl 1):S22–S30. [DOI] [PubMed] [Google Scholar]
- 107. Lytle LA, Seifert S, Greenstein J, et al. How do children’s eating patterns and food choices change over time? Results from a cohort study. Am J Health Promot. 2000;14:222–228. [DOI] [PubMed] [Google Scholar]
- 108. Janssen I, LeBlanc AG.. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Kontra C, Albert N, Beilock SL.. Embodied cognition: from the playing field to the classroom In: Hodges NJ, Williams AM, eds. Skill Acquisition in Sport: Research, Theory and Practice. 2nd ed.Oxford, UK: Routledge; 2012:325–336. [Google Scholar]
- 110. Gill TP, Boylan S.. Public health messages: why are they ineffective and what can be done? Curr Obes Rep. 2012;1:50–58. [Google Scholar]
- 111. Wakefield MA, Loken B, Hornik RC.. Use of mass media campaigns to change health behaviour. Lancet. 2010;376:1261–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Dahl S. Social Media Marketing: Theories and Applications. London, UK: Sage Publishing; 2015. [Google Scholar]
- 113. Economos CD, Brownson RC, DeAngelis MA, et al. What lessons have been learned from other attempts to guide social change? Nutr Rev. 2001;59:S40–S56. [DOI] [PubMed] [Google Scholar]
- 114. Beaudoin CE, Fernandez C, Wall JL, et al. Promoting healthy eating and physical activity: short-term effects of a mass media campaign. Am J Prev Med. 2007;32:217–223. [DOI] [PubMed] [Google Scholar]
- 115. Randolph W, Viswanath K.. Lessons learned from public health mass media campaigns: marketing health in a crowded media world. Annu Rev Public Health. 2004;25:419–437. [DOI] [PubMed] [Google Scholar]
- 116. Vandelanotte C, Muller AM, Short CE, et al. Past, present, and future of eHealth and mHealth research to improve physical activity and dietary behaviors. J Nutr Educ Behav. 2016;48:219–228.e1. [DOI] [PubMed] [Google Scholar]
- 117. French J, Blair-Stevens C.. Social Marketing National Benchmark Criteria. London, UK: National Social Marketing Centre; 2006. http://www.thensmc.com/sites/default/files/benchmark-criteria-090910.pdf. Accessed August 7, 2018. [Google Scholar]
- 118. Carins JE, Rundle-Thiele SR.. Eating for the better: a social marketing review (2000–2012). Public Health Nutr. 2014;17:1628–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Gracia-Marco L, Vicente-Rodriguez G, Borys JM, et al. Contribution of social marketing strategies to community-based obesity prevention programmes in children. Int J Obes. 2011;35:472–479. [DOI] [PubMed] [Google Scholar]
- 120. Kubacki K, Rundle-Thiele S, Lahtinen V, et al. A systematic review assessing the extent of social marketing principle use in interventions targeting children (2000-2014). Young Consumers. 2015;16:141–158. [Google Scholar]
- 121. Gracia-Marco L, Mayer J, Vicente-Rodriguez G, et al. Methods and social marketing In: Borys JM, Le Bodo Y, De Henauw S, Moreno LA, Romon M, Seidell JC, Visscher TLS, eds. Preventing Childhood Obesity. EPODE European Network Recommendations. 1st ed.Cachan Cedex, France: Lavoisier; 2011:85–119. [Google Scholar]
- 122. Romon M, Lommez A, Tafflet M, et al. Downward trends in the prevalence of childhood overweight in the setting of 12-year school- and community-based programmes. Public Health Nutr. 2009;12:1735–1742. [DOI] [PubMed] [Google Scholar]
- 123. Romon M, Duhamel A, Salleron J, et al. Évolution de la prévalence du surpoids et de l’obésité chez les enfants de 4 à 11 ans entre 2005 et 2010 dans les villes « EPODE » [in French]. Nutr Clin Et Métabol 2010;24:58. doi:NUCLI-12-2010-24-S1-0985-0562-101019-201005516 [Google Scholar]
- 124. Mantziki K, Renders CM, Vassilopoulos A, et al. Inequalities in energy-balance related behaviours and family environmental determinants in European children: changes and sustainability within the EPHE evaluation study. Int J Equity Health. 2016;15:160. doi:10.1186/s12939-016-0438-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Mantziki K. Integrated Community-Based Approaches to Prevent Childhood Overweight and Obesity [doctoral thesis]. Amsterdam, the Netherlands: Vrije Universiteit Amsterdam; 2017. [Google Scholar]
- 126. Vinck J, Brohet C, Roillet M, et al. Downward trends in the prevalence of childhood overweight in two pilot towns taking part in the VIASANO community-based programme in Belgium: data from a national school health monitoring system. Pediatr Obes. 2016;11:61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Public Health England. Social Marketing Strategy 2014 to 2017 .London, UK: Public Health England; 2015:182. [Google Scholar]
- 128. Mitchell S, Clifford A, Hardy A, et al. Change4Life, Three Year Social Marketing Strategy. London, UK: Department of Health; 2011. [Google Scholar]
- 129. Wrieden WL, Levy LB.. ‘Change4Life Smart Swaps’: quasi-experimental evaluation of a natural experiment. Public Health Nutr. 2016;19:2388–2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Croker H, Lucas R, Wardle J.. Cluster-randomised trial to evaluate the ‘Change for Life’ mass media/social marketing campaign in the UK. BMC Public Health. 2012;12:404. doi:10.1186/1471-2458-12-404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. French J, Gordon R.. Strategic Social Marketing. London, UK: Sage Publications; 2015. [Google Scholar]
- 132. Bate P, Bevan H, Robert G.. Towards a Million Change Agents. A Review of the Social Movements Literature: Implications for Large Scale Change in the NHS. London, UK: NHS Modernisation Agency; 2004. [Google Scholar]
- 133. Morris A. Reflections on social movement theory: criticisms and proposals. Contemp Sociol. 2000;29:445–454. [Google Scholar]
- 134. Robinson TN. Save the world, prevent obesity: piggybacking on existing social and ideological movements. Obesity (Silver Spring). 2010;18(suppl 1):S17–S22. [DOI] [PubMed] [Google Scholar]
- 135. UNICEF, World Health Organization, World Bank Group. Levels and Trends in Childhood Malnutrition. UNICEF/WHO/World Bank Group Joint Child Malnutrition Estimates http://www.who.int/nutgrowthdb/estimates/en/. Published 2018. Accessed July 18, 2018.
- 136. National Ministry of Health. Estrategia Nacional Para La Prevención y El Control Del Sobrepeso, La Obesidad y La Diabetes. Mexico City, Mexico: IEPSA; 2013. [Google Scholar]
- 137. Blair MK. Using digital and social media platforms for social marketing In: French J, ed. Social Marketing and Public Health: Theory and Practice. 2nd ed.Oxford, UK: Oxford University Press; 2017:203–216. [Google Scholar]
- 138. Monroy Gómez J. Impact of a digital Facebook campaign on the purchase and consumption of food in Mexican families with children under 12 years: a social marketing strategy. Oral presentation at: World Social Marketing Conference; May 15–18, 2017; Washington, DC.
- 139. Sinnenberg L, Buttenheim AM, Padrez K, et al. Twitter as a tool for health research: a systematic review. Am J Public Health. 2017;107:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Weeg C, Schwartz HA, Hill S, et al. Using Twitter to measure public discussion of diseases: a case study. JMIR Public Health Surveill. 2015;1:e6. doi:10.2196/publichealth.3953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Stamm H, Fischer A, Lamprecht M.. Vergleichendes Monitoring der Gewichtsdaten von Kindern und Jugendlichen in der Schweiz. Analyse von Daten aus den Kantonen Basel-Stadt, Bern, Graubünden, Jura, Luzern, Obwalden, St. Gallen und Uri sowie den Städten Bern, Freiburg und Zürich Gesundheitsforderung. Schweiz Arbeitspapier 41 [in German]. Bern, Switzerland: Gesundheitsförderung Schweiz; 2017.
- 142. Merzel C, D’Afflitti J.. Reconsidering community-based health promotion: promise, performance, and potential. Am J Public Health. 2003;93:557–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Nastasi BK, Hitchcock J.. Challenges of evaluating multilevel interventions. Am J Community Psychol. 2009;43:360–376. [DOI] [PubMed] [Google Scholar]
- 144. Koepsell TD, Wagner EH, Cheadle AC, et al. Selected methodological issues in evaluating community-based health promotion and disease prevention programs. Annu Rev Public Health. 1992;13:31–57. [DOI] [PubMed] [Google Scholar]
- 145. Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi:https://doi.org/10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Atienza AA, King AC.. Community-based health intervention trials: an overview of methodological issues. Epidemiol Rev. 2002;24:72–79. [DOI] [PubMed] [Google Scholar]
- 147. Komro KA, Flay BR, Biglan A, et al. Research design issues for evaluating complex multicomponent interventions in neighborhoods and communities. Transl Behav Med. 2016;6:153–159. doi: 10.1007/s13142-015-0358-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Sanson-Fisher RW, Bonevski B, Green LW, et al. Limitations of the randomized controlled trial in evaluating population-based health interventions. Am J Prev Med. 2007;33:155–161. [DOI] [PubMed] [Google Scholar]
- 149. Whitehead TL. Traditional approaches to the evaluation of community based interventions: strengths and limitations. College Park, Maryland: University of Maryland; 2002:11. The Cultural Ecology of Health and Change (CEHC) Working Papers Series. [Google Scholar]
- 150. Campbell M, Fitzpatrick R, Haines A, et al. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321:694–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Guijt I. Participatory Approaches, Methodological Briefs: Impact Evaluation No. 5. Florence, Italy: UNICEF Office of Research; 2014. [Google Scholar]
- 152. King JA, Cousins JB, Whitmore E.. Making sense of participatory evaluation: framing participatory evaluation. New Dir Eval. 2007;2007:83–105. [Google Scholar]
- 153. Koelen MA, Vaandrager L, Colomér C.. Health promotion research: dilemmas and challenges. J Epidemiol Community Health. 2001;55:257–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Van Koperen TM, De Kruif A, Van Antwerpen L, et al. Barriers to and facilitators of the evaluation of integrated community-wide overweight intervention approaches: a qualitative case study in two Dutch municipalities. Int J Environ Res Public Health. 2016;13:390. doi:10.3390/ijerph13040390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Maher CA, Lewis LK, Ferrar K, et al. Are health behavior change interventions that use online social networks effective? A systematic review. J Med Internet Res. 2014;16:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]



