Abstract
Avulsion fractures compromise function and movement at the affected joint. If left untreated, it can lead to deformity, nonunion, malunion, pain, and disability. The purpose of this review was to identify and describe the epidemiology and available treatment options for common avulsion fractures of the upper and lower extremities. Current evidence suggests that optimal treatment is dependent on the severity of the fracture. Conservative efforts generally include casting or splinting with a period of immobilization. Surgery is typically indicated for more severe cases or if nonoperative treatments fail; patient demographics or preferences and surgeon experience may also play a role in decision making. Some avulsion fractures can be surgically managed with any one of various techniques, each with their own pros and cons, and often there is no clear consensus on choosing one technique over another; however, there is some research suggesting that screw fixation, when possible, may offer the best stability and compression at the fracture site and earlier mobilization and return to function. Physicians should be mindful of the potential complications associated with each intervention.
Keywords: Review, avulsion fracture, upper extremity, lower extremity
Introduction
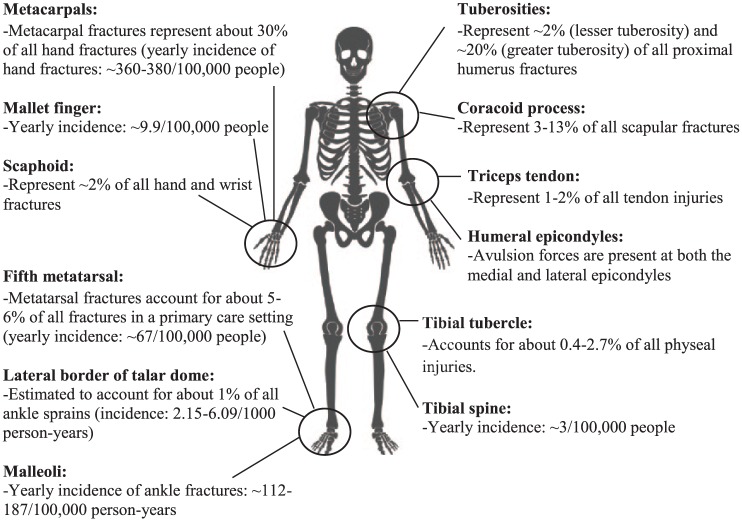
Avulsion fractures compromise function and movement at the affected joint.1,2 They are more prevalent in younger individuals who are generally more active.3 The injury occurs when a muscle tendon unit attached to a bony area produces enough force to tear a fragment of the bone while avulsing the tendon.1,4,5 If left untreated, this injury can lead to deformity, nonunion, malunion, pain, and disability.1,2,6,7 The purpose of this review was to identify and describe the epidemiology and available treatment options for common avulsion fractures of the upper and lower limbs (Figure 1).
Figure 1.
Avulsion fractures of the upper and lower limbs.
Background on avulsion fractures of the upper limb
Hand and wrist
Fractures of the metacarpals represent approximately 30% of all hand fractures.8 In 2 population studies conducted in Canada and the United Kingdom, yearly incidence rates of hand fractures were 360 and 380 per 100 000 people, respectively.9,10 The extensor carpi radialis longus and brevis muscles insert at the base of the second and third metacarpal bones, which place these areas at risk of an avulsion injury.2,11 The proposed mechanism of injury (MOI) is a force occurring at the dorsal aspect of the hand while the wrist is hyperextended. The contracting muscle can then displace the metacarpal fragment.2,11,12 Patients with pain and restricted movement at the wrist following trauma should be suspected of having such an injury.11 Radiographs and/or computed tomography (CT) should be used to confirm the diagnosis.11 Complications included posttraumatic arthritis, joint weakness and reduced grip strength, and deformity.11
Sports injuries are common at the distal phalanx.13 Mallet finger injuries affect the extensor mechanism at the distal interphalangeal (DIP) joint.1,13 The yearly incidence of this injury is estimated at 9.9 of 100 000 patients and is common in younger men (average age of diagnosis: 34 years).1,14,15 About three-fourths of mallet finger avulsions happen in the dominant hand and more than 90% are seen in the ulnar digits.1,15 Some authors have proposed that certain patients are genetically predisposed to the injury.15 Patients typically present with flexion deformity, with or without pain, and the inability to fully extend the DIP joint; a lateral x-ray can confirm the diagnosis.13,15 The most common MOI is sudden flexion at the DIP joint and accounts for about 2% of all sports injuries.1,13,16 Mallet finger injuries are generally classified using the Wehbe and Schneider system, which divides such injuries into 3 types (I, II, or III) and each is further divided into 3 subtypes (A, B, or C) depending on the amount of articular involvement (Table 1).1,17 An untreated or incorrectly treated injury can lead to deformity or eventual osteoarthritis in the finger.1,13,15
Table 1.
Wehbe and Schneider classification of mallet finger injuries.
| Type | 1 | No DIP joint subluxation |
| 2 | DIP joint subluxation | |
| 3 | Epiphyseal and physeal injuries | |
| Subtypes | A | <1/3 of articular surface involvement |
| B | 1/3 to 2/3 articular surface involvement | |
| C | >2/3 articular surface involvement |
Abbreviation: DIP, distal interphalangeal.
Avulsion fractures of the scaphoid comprise about 2% of all hand and wrist fractures.18 Forces produced during dorsiflexion-ulnar deviation is the mechanism of this injury.18,19 The fracture can occur after falling on an outstretched hand and the patient will present with swelling, pain, and paresthesias.19,20 The most common location of such an injury is at the tuberosity in the distal region of the scaphoid, but it can also occur at the proximal pole.21–24
Elbow
Triceps tendon ruptures are rare, making up approximately 1% to 2% of all tendon injuries and the tendon may avulse from the posterior olecranon, which is the most common site of triceps tendon rupture.25–29 Although the fracture may initially be missed on imaging (bone flake on the lateral radiograph), especially in the presence of concomitant injuries,25–27 the injury often occurs after falling onto an outstretched hand.25–27,30 Clinical signs include a gap in tendon continuity, swelling, tenderness, and the inability to extend the affected joint.25,27,31
The medial and lateral epicondyles of the humerus may also fracture due to avulsion forces.32–34 A common MOI for medial epicondyle fractures is an increase in flexor-pronator muscle tension, producing valgus stress at the elbow, such as during arm wrestling or collapsing on an outstretched hand.34,35 On the lateral side, an avulsion fracture can occur at the anconeus muscle, which assists in elbow extension and forearm pronation, the latter being the contributing MOI (eg, during weightlifting).33 The patient might feel a sudden sharp pain with tenderness and swelling at the joint, with weakness and pain on flexion of the wrist or elbow; the patient’s ability to fully extend the elbow may also be compromised.33,34
Shoulder
An avulsion fracture can occur at the greater or lesser tuberosity of the proximal humerus due to attachment of the rotator cuff musculature.36–38 Fractures at the lesser tuberosity are uncommon, occurring in 0.46 people per 100 000 and represent about 2% of proximal humerus fractures, whereas greater tuberosity fractures occur more often, accounting for ~20% of these injuries.36,37,39 Examination will show swelling and tenderness at the shoulder.36,38 Computed tomography will be helpful for a more accurate assessment of the fracture.36,38,40,41
Injuries to the coracoid process represent 3% to 13% of all scapular fractures, a proportion of which are due to avulsion.42,43 This injury will limit shoulder abduction and flexion.42 Com-puted tomography may be needed for diagnosis.42
Background on avulsion fractures of the lower limb
Knee
An avulsion fracture at the tibial tubercle most commonly occurs after sudden flexion of the quadriceps, typically at the beginning of a jump or during landing.3,44 It accounts for approximately 0.4% to 2.7% of all physeal injuries.45,46 The patient will have severe pain on the anterior aspect of the knee and, likely, be unable to walk and actively move the knee joint.44 Swelling and deformity may be present in the area surrounding the tibial tubercle and plain radiographs should be taken to confirm the diagnosis.44,46 The Watson-Jones classification divides this injury into 3 types, depending on the amount of involvement of the proximal epiphysis and degree of displacement (Table 2).3,44 Treatment should restore the anatomy of the displaced fragment, extensor mechanism alignment, and joint congruency.47
Table 2.
Watson-Jones classification of tibial tubercle avulsion fractures.
| Type | 1 | Avulsion of the apophysis without injury to the tibial epiphysis |
| 2 | Epiphysis is lifted cephalad and incompletely fractured | |
| 3 | Displacement of the proximal base of the epiphysis with the fracture line extending in the joint |
Tibial spine, or eminence, avulsion injuries are typically associated with the anterior cruciate ligament and have an estimated incidence of 3 in 100 000.48–50 This type of injury is more common in children or adolescents but has become increasingly more prevalent in the young adult.5,51 The MOI is hyperextension of the knee with rotation on the tibia occurring simultaneously, which may happen during auto accidents, falls, or sports.49,52 Patients will present with an inability to bear weight with pain and swelling at the knee.49 Chronic cases may also have impingement in the intercondylar notch, resulting in the loss of extension and continued pain.48 Clinical examination should be confirmed with x-rays or other diagnostic imaging.49 The injury can be classified into 4 types (I, II, III, or IV), which described the amount of comminution and displacement (Table 3).51–53
Table 3.
Meyers and McKeever classification of tibial spine avulsion fractures.
| Type | I | Nondisplaced or minimally displaced |
| II | Anterior 1/3 to 1/2 of the avulsed bone displaced proximally (beak-like deformity on lateral radiograph) | |
| III | Bone completely displaced from its bed | |
| IV | Displaced and comminuted |
Foot and ankle
In a primary care setting, metatarsal fractures account for about 5% to 6% of all fractures, with a yearly incidence estimated to be approximately 67 of 100 000 people.54,55 A fifth metatarsal avulsion injury is the most frequent type of metatarsal fracture.4,54–57 The injury typically results from inversion of the foot, generating tension along the plantar aponeurosis insertion.4,57,58 The most commonly used classification system for fifth metatarsal fractures is the Lawrence and Botte description and avulsion fractures are classified as Zone 1 injuries (Table 4).59,60 Recovery may require prolonged immobilization, high rates of nonunion and delayed union and refracture after union have been reported.4,59
Table 4.
Lawrence and Botte classification of fifth metatarsal fractures.
| Zone | 1 | Avulsion fracture of the tuberosity with or without involvement of the tarsometatarsal articulation |
| 2 | Fracture at the metaphysis-diaphysis junction, which extends into the fourth-fifth intermetatarsal facet | |
| 3 | Fracture at the proximal diaphysis, distal to the fourth and fifth metatarsal base articulation |
Avulsion fractures can also occur at the talus.61,62 The talar dome articulates with both the tibia and fibula and is important in ankle motion and weightbearing.61 The fracture may be missed on initial examination, being diagnosed as a ligamentous ankle sprain only.61,63 It has been reported that talar avulsion injuries represent about 1% of all sprains.62,64 The incidence of ankle sprains has ranged from 2.15 to 3.29 per 1000 person-years across 2 studies in the United States and 5.27 to 6.09 per 1000 person-years in 1 UK study.65–67 Magnetic resonance imaging (MRI) or CT scans may also be required for an accurate diagnosis.61,63 For lateral talar dome fractures, the injury occurs after inversion with dorsiflexion.61 Patients will have a swollen, bruised, and painful foot and compromised weightbearing.62 These fractures may be classified from stages I to IV using the Berndt and Harty system (Table 5).61,68
Table 5.
Berndt and Harty classification of avulsion fractures at the lateral border of the talar dome.
| Stage | I | Compression fracture subchondral bone |
| II | Partial osteochondral fragment fracture | |
| III | Completely detached fragment without displacement | |
| IV | Completely detached fragment with displacement |
At the ankle joint, both lateral and medial malleoli fractures may be due to avulsion.69–72 Early incidence estimates on ankle fractures range from 112 to 187 per 100 000 person-years and most of them occur at the malleoli.73,74 The patient will likely present with pain and instability, especially in those who are active.69 In addition to radiography, ultrasonography, CT, or MRI may be needed for diagnosis.71
Treatment of avulsion fractures
Metacarpal
The literature on metacarpal avulsion fractures is limited.2 A few cases of nonoperative management with plaster cast immobilization have been reported, but more often than not, complications such as fracture displacement and mal angulation occur that eventually require surgical intervention.2 Such complications can lead to persistent pain, limited range of motion (ROM), reduced wrist power, and metacarpal boss (a firm bump or swelling on the back of the hand where the metacarpals articulate with the carpal bones).
Surgical intervention stabilizes the joint, avoids tendon rupture, and restores joint integrity.11 Open reduction and internal fixation (ORIF) with Kirchner wires (K-wires) and lag screw fixation with tendon reattachment using a suture anchor have been reported.11,75 Najefi et al2 performed a similar procedure with a headless screw with similar success. Surgical fixation with a miniplate and screws can result in adequate reduction and restore grip strength and wrist extension.11 The ORIF is also reported to allow for faster recovery relative to conservative management.2 Internal fixation with screws is more stable than K-wires only and offers compression with less tissue irritation (Figure 2).2
Figure 2.
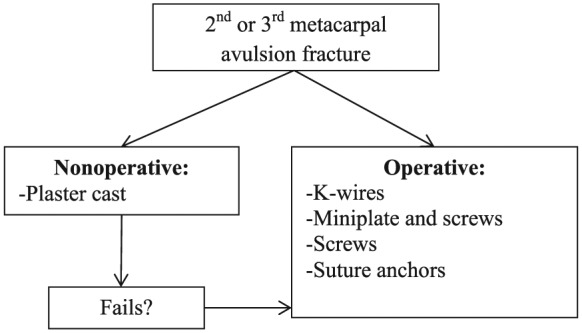
Treatment of metacarpal avulsion fracture.
Mallet finger
Nonoperative treatment of mallet finger injuries involves splinting the DIP joint to immobilize it and allow the injury to heal.1 There are numerous splint options available, which are used to help keep the finger in full extension or slight hyperextension.1,13,15 It is recommended that splinting be done 24 hours a day for 6 to 8 weeks, possibly followed by another 2 to 6 weeks of splinting at night only.1,13,15 Splinting may result in high patient satisfaction for up to 5 years, and even delayed splinting has demonstrated favorable results.1,76,77 The various splint options are made of different materials and may result in temporary benign complications (up to 45% has been reported; mainly skin-related and deformity) and patient satisfaction.1,13,15,78 The most commonly used splint is known as the Stack splint, but other options include a custom thermoplastic, aluminum foam, and Abouna splint.16 Patients have reported that the Stack splint is both comfortable and easy to clean.16 Abouna splints are more dynamic but its metal wires are known to rust and elastic tensor bands may wear out quickly.15
When splinting cannot correct acute deformities, patients become intolerable to splints, or when the fracture is deemed unstable and involves a substantial proportion of the articular surface, surgery may be required; some individuals may even seek treatment for aesthetic reasons.1,13,16 Several surgical interventions have been investigated: K-wires, extension block wiring, small screws, hook plate, pull-through wires, figure of 8 wiring, tension band wiring, umbrella handle K-wire, pull-through sutures, and external fixation.1,13 Percutaneous pinning of the DIP joint in extension could be attempted if the fracture is amenable to closed reduction.13 Open reduction can be performed and may even improve ROM and cosmetic appearance.13 A biomechanical study by Damron et al comparing K-wires, figure of 8 wiring, pull-through wires, and pull-through sutures found that pull-through sutures were most stable with no loss of reduction; loss of reduction with the other treatments ranged from 50% to 100%.1,16,79 In a retrospective study comparing K-wires versus ORIF with screws, although ORIF requires more surgical time, Lucchina et al80 found that screws fixation resulted in earlier mobilization and return to work, without the need for managing the pin tracts left with K-wire insertion. Early results with the umbrella handle technique (dorsal to volar percutaneous pinning with bending of the dorsal end of the K-wire into an “umbrella handle” shape and passing it through subcutaneously from the palmar side of the finger) and hook plate fixation are encouraging, although they may be more complex and involve a bulky implant that may eventually need to be removed.16 Surgery may result in favorable cosmetic appearance of the finger.1,81 Rates of postsurgical complications have ranged from 38% to 52% and include infection, nail deformity, device failure, joint incongruity, skin breakdown, fracture displacement, necrosis, and tendon rupture.1,78,82 These adverse outcomes are reduced with a percutaneous approach, but this method may not result in proper bone reduction (Figure 3).15
Figure 3.
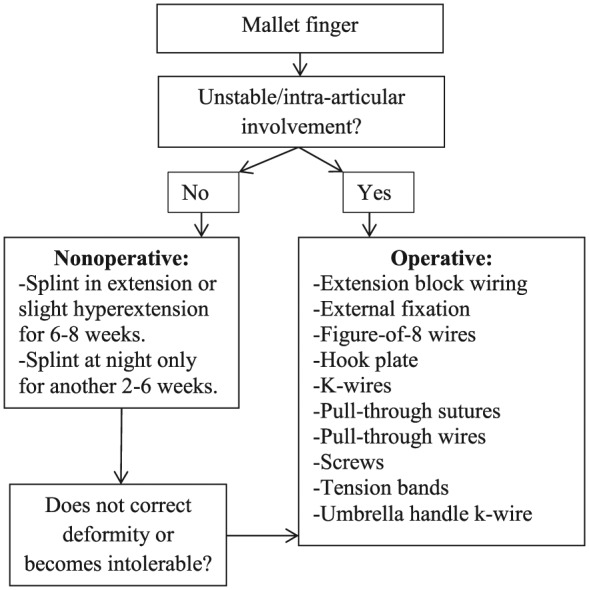
Treatment of mallet finger injury.
Scaphoid
Plaster casting for 6 weeks may offer full ROM and reduced pain, with adequate radiographic healing and proper stability at later follow-up.19
Scaphoid avulsion fractures fixed surgically are treated with a compression screw; stabilization of the fracture may be supplemented with K-wires, which can be removed once x-rays show evidence of bridging callus and there is a lack of tenderness.20 Immobilization may last for up to 8 weeks postoperatively.20 Other procedures may also be considered, such as carpectomy, fusion, or removal of the avulsed fragment, but these are salvage therapies reserved for more chronic cases (Figure 4).20
Figure 4.
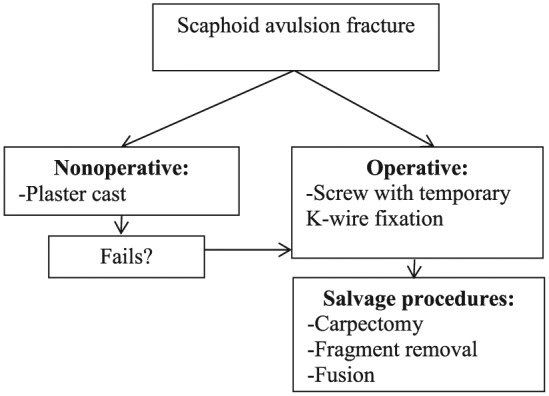
Treatment of scaphoid avulsion fracture.
Triceps tendon
The literature on treatment options for triceps tendon avulsions is limited to case reports and small case series.26 Managing these patients can be challenging as a triceps tendon avulsion is associated with the presence of concomitant injuries.26 It has been recommended to perform surgery in all cases, except for older, medically compromised patients or those with low functional demand.26,83 The most common surgical approach is to fix the avulsed fragment with sutures.25,84–87 K-wires, cerclage wires, anchors, or tension bands may also be used.25,29,31,85 If the fragment is too small to be repaired with an implant or severely comminuted, it may be excised prior to suturing tendon to bone.25,27,88,89 Postoperatively, the elbow is splinted, with active extension starting around 3 to 6 weeks and strength training at 3 months (Figure 5).29,84,88
Figure 5.
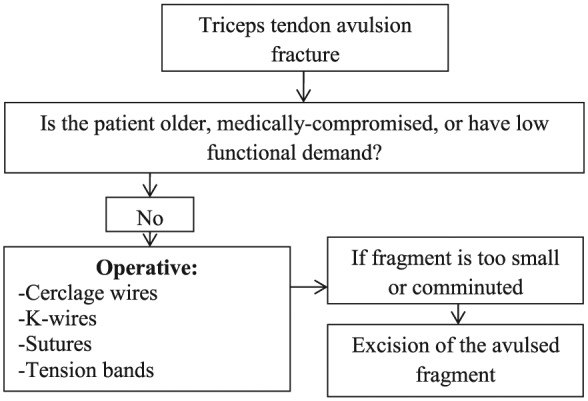
Treatment of triceps tendon avulsion fracture.
Medial and lateral epicondyles of the distal humerus
A conservative approach to treating this injury when the fracture is deemed undisplaced is via a plaster splint for approximately 2 to 6 weeks and then gradual mobilization of the elbow thereafter as soon as possible.32,34,35 Early mobilization is important to avoid subsequent stiffness and limitation.33
For displaced fractures, surgical options include K-wires, screws, staples, sutures, and tension bands.32,35 Although there is limited high-quality evidence on the topic, the use of operative fixation for epicondylar fractures has increased, with the advantage that it offers earlier mobilization and full ROM than conservative therapy, specifically following compression screw insertion.90 K-wire fixation stabilizes the injury but does not always compress the fracture fragments (Figure 6).90
Figure 6.
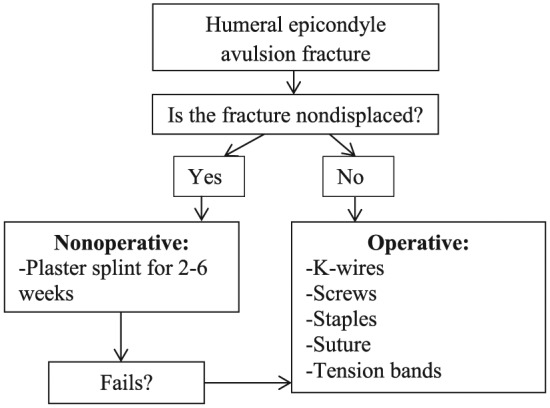
Treatment of humeral epicondyle avulsion fracture.
Tuberosities of the proximal humerus
Conservative treatment involves immobilization, for example, forearm straps for 6 to 8 weeks, for minimally displaced or nondisplaced fractures; functional training via physiotherapy should follow.36,41
Displaced fractures are best managed with screws or sutures and anchors; the former is preferred if the fragment is large enough, including headless screws.37,38,40,41,91 Cerclage wiring has also been used for lesser tuberosity injuries.36 Nonsurgical therapy can lead to chronic shoulder pain, particularly if not well reduced.37,40,92 In a recent systematic review by Vavken et al,91 the authors found that 17% (n = 60) of patients with lesser tuberosity avulsion fractures underwent successful nonoperative treatment. Surgery is recommended to prevent instability of the joint and weakness.38,40,41 Excision can be done if the fractured fragment is too small or comminuted, but this is not routine as bone-to-bone healing is preferred over tendon-to-bone healing.36,91 The arm should then be placed in a sling and after 2 to 3 weeks, light exercise can be initiated.36,38,40 Resistive exercises can begin after 6 weeks (Figure 7).40
Figure 7.
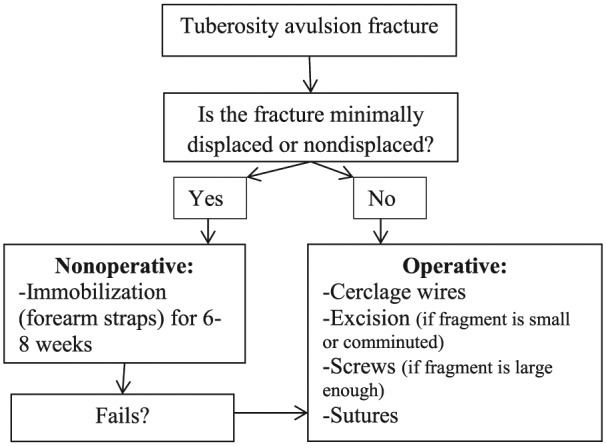
Treatment of tuberosity avulsion fracture.
Coracoid process
Avulsion fractures of the coracoid process are generally treated with screw fixation.42,43,93 A K-wire may also be used temporarily.42 Immobilization of the shoulder in a sling for 2 to 3 weeks and physiotherapy for 6 weeks are recommended (Figure 8).42,43
Figure 8.
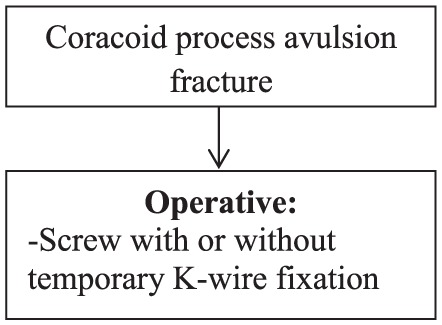
Treatment of coracoid process avulsion fracture.
Tibial tubercle
Watson-Jones type I tibial tubercle avulsion injuries (minimally displaced) may be treated conservatively by cast immobilization with the knee in extension.44,47 Some may even attempt closed reduction for more severely displaced fractures prior to surgery.47
Successful surgical management can be done with screws with early rehabilitation following a temporary nonweightbearing period.44,46 Compartment syndrome is a potential complication.46 The ORIF is recommended when severe displacement or comminution is present at the physis.46 Surgery should restore the extensor mechanism and joint congruency.46 Use of preoperative CT scans and intraoperative arthroscopy are also recommended to better visualize the fracture pattern (Figure 9).46
Figure 9.
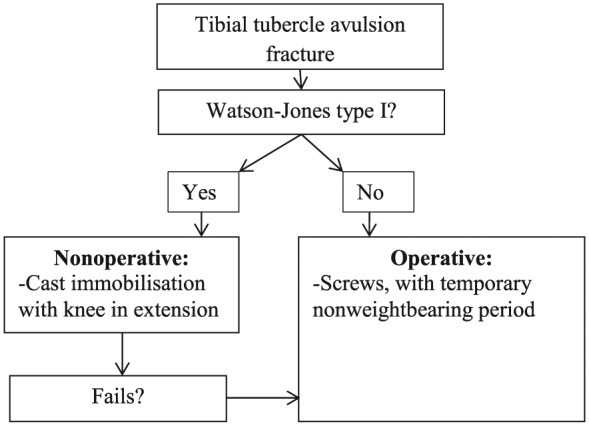
Treatment of tibial tubercle avulsion fracture.
Tibial spine
Closed reduction with casting or splinting in extension or slight flexion (20°-30°) can be done for less severe tibial spine avulsions.52,94 This is commonly done for type I undisplaced fractures for 6 to 12 weeks.94 High rates of nonunion and instability have been reported with conservative treatment, especially in higher grade fractures.95
Type III or greater tibial spine avulsions should be managed operatively; there is controversy surrounding the surgical fixation of type II injuries, but those with greater than 2 mm of displacement or where conservative treatment has failed are often treated surgically.5,51,52 Other indications include a mechanical block with reduced ROM and patients having a locked knee.51 There is controversy surrounding the surgical management of these injuries, but options include arthroscopy-assisted fixation or ORIF.48 Prompt operative fixation will minimize the probability of nonunion, laxity, and decreased ROM and should be done in the presence of a disrupted articular surface.49,52 Internal fixation can be done using a variety of options, with screws and sutures being the primary methods, exhibiting good clinical and radiographic outcomes.5,48,49,51 The issue of screw fixation versus sutures requires further investigation as the current evidence is limited and inconsistent.5 In a systematic review of different surgical treatments, Osti et al determined that suturing can avoid the second visit for screw removal, but it is also associated with a longer immobilization period and only partial weightbearing can be initiated postoperatively, which can cause joint stiffness and arthrofibrosis.6,7,94 Screw fixation is simple, reproducible, and allows for early mobilization and weightbearing but may not be possible with a small or comminuted bony fragment.5,51,94 Surgical intervention should result in stability, compression of the fragment, and no loss of reduction.51,52 There is still no consensus on optimal therapy, and classification type/injury pattern, surgeon preference, and patient characteristics are factors in this decision.5,94 Verdano et al50 outlined the pros and cons of each technique. Postoperative rehabilitation is also important for recovery in this patient population, but recommendations for this are also inconsistent (Figure 10).5
Figure 10.
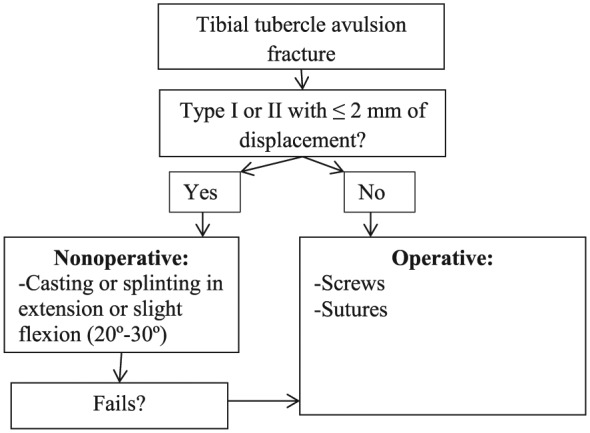
Treatment of tibial spine avulsion fracture.
Fifth metatarsal
Conservative treatment of fifth metatarsal avulsion fracture is promising as the area has good blood supply and healing potential.57 Nonoperative methods of treating fifth metatarsal fractures include foot orthotics or cast immobilization.57,58,96 In a 1-year retrospective study of 42 patients comparing a controlled ankle motion boot, hard-soled shoe, short leg cast, and a carbon fiber insert, Dineen et al58 found no significant differences in outcomes measuring pain, function, quality of life, and patient satisfaction. Occasionally, nonoperative management can lead to delayed union, malunion, nonunion, refracture, pain, and compromised function.96
When such fractures are intra-articular and displaced in younger, more active patients or the patient requires an early return to activity (eg, athletes), surgery should be performed, with options including tension bands or internal screw fixation.4,56,57 In a biomechanical study, cancellous screws demonstrated a significant improvement in fixation strength relative to tension bands. The screws withstood more than 3 times the load of the tension bands.4 Japjec et al57 (33 patients) showed that intramedullary screw fixation can result in healing within 8 weeks in most patients; however, 3 of these cases had a refracture after resuming training and were subsequently treated with a stronger and larger headless screw (Acutrak), which all healed uneventfully. Larger diameter screws are recommended for patients with high body mass or require an earlier return to activity.57 In a small cohort of patients managed conservatively, 4 of 9 patients had a healed fracture, whereas the rest did not heal by 6 months; 4 of the unhealed cases eventually underwent osteosynthesis and healed within an average of 10 weeks.57 In a randomized trial of 46 patients comparing conservative treatment with percutaneous cannulated screw fixation, all cases achieved union except for 3 who had a malunion and 2 with mild to moderate pain in the nonoperative group. Those in the operative group also had significantly better functional scores at 6 months, but not at 12 months; they also had significantly shorter time to full weightbearing and return to work.96 Screws offer more direct and consistent compression ideal for fracture union and early rehabilitation, and tension band fixation may result in subcutaneous irritation, causing patients to want them removed; however, the latter can be an option in patients with underlying bone disease or the fracture is highly comminuted.4,96 Recent evidence shows that a hook plate may also be a viable option (Figure 11).97
Figure 11.
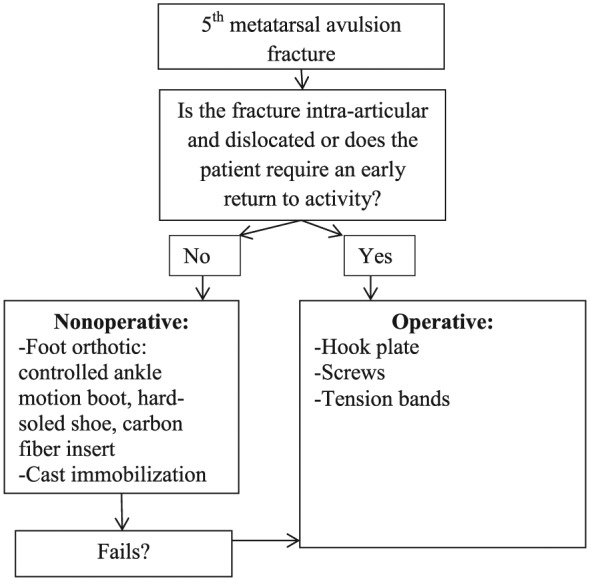
Treatment of fifth metatarsal avulsion fracture.
Lateral border of talar dome
Nonsurgical treatment of talus avulsion fractures includes a short leg cast or brace with a nonweightbearing status for about 4 to 6 weeks, followed by progressive weightbearing and physical therapy.61,63,98 Nonsteroidal anti-inflammatory drugs or analgesics may also be prescribed for pain management, but there is controversy surrounding their effects on bone healing.98
Patients with more severe injuries (stages III or IV) or persistent symptoms following nonoperative therapy are typically treated surgically, with options ranging from arthroscopy-assisted fixation (with or without subchondral bone drilling) to ORIF.61,63,98 The rationale for drilling is that it is proposed to increase vascularization and healing of the fragment.63 Implant fixation with screws, K-wires, or absorbable pins can be performed.63,98 Screws provide the desirable compression but will eventually require removal.63 K-wires do not require an arthrotomy, like screw insertion, but they must also be subsequently removed and do not provide compression.63 Absorbable pins do not need to be removed but may not provide adequate compression and increase the risk of a local reaction or bone resorption with degradation of the implant (Figure 12).63
Figure 12.
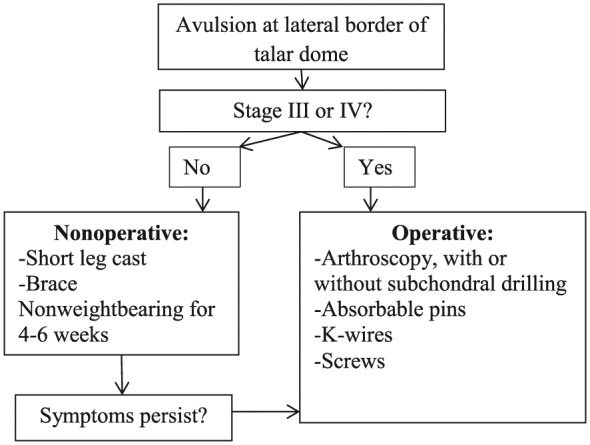
Treatment of avulsion fracture at the lateral border of talar dome.
Medial and lateral malleoli
Avulsion fractures of either malleolus are typically managed with tension bands or screws; however, a plate with screws may also be used.71,72,99,100 Tension band fixation may be preferred for smaller avulsed fragments.99,101–103 Screw fixation may also be contraindicated if the patient has osteoporosis or diabetes; such patients can be treated with a plate and screw system.72,99 Postoperatively, the patient may be nonweightbearing for 4 to 6 weeks, with ROM exercises initiated at 2 weeks (Figure 13).71,100
Figure 13.
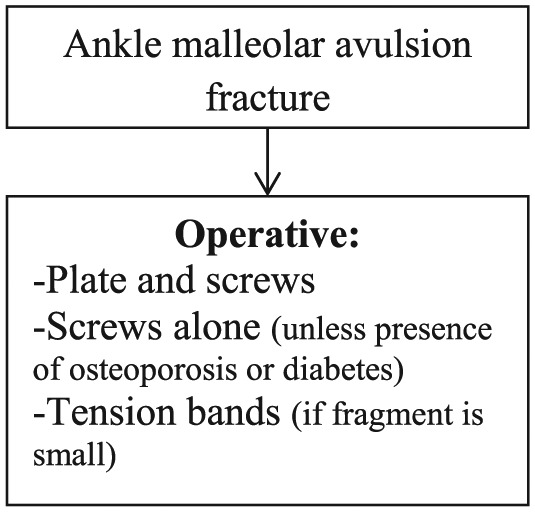
Treatment of ankle malleolar avulsion fracture.
Conclusions
An avulsion fracture can occur at numerous locations in the upper and lower limb. The literature on these injuries is limited to mainly case reports and case series, but current evidence suggests that optimal treatment is dependent on fracture severity. Conservative efforts generally include casting or splinting with a period of immobilization, with the appropriate pain management medication as needed followed by rehabilitation. Surgery is typically indicated for severe cases or if nonoperative treatment fails; patient demographics or preferences and surgeon experience may also play a role in this decision. The goals of surgery are realignment, earlier return to function, and, specifically in the case of mallet finger, to improve cosmetic appearance. Some avulsion fractures can be surgically fixed with various techniques, such as compression screws or K-wires, each with their own pros and cons, and there is no clear consensus on choosing one over the other; however, there is some research suggesting that screw fixation may offer the best stability and compression at the fracture site and earlier mobilization and return to function. Physicians should be mindful of the potential complications associated with each therapy, including surgery.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The preparation of the manuscript was funded, in part, by a research grant from Acumed.
Declaration of Conflicting Interests:The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: C.V. is an employee of OrthoEvidence Inc. O.R.A has received speaking fees from ConMed and research support from the Arthroscopy Association of North America. M.B. reports no other conflicts of interest.
Author Contributions: CV and MB contributed to the design of the study, and acquisition and interpretation of data; CV drafted the manuscript; MB and ORA reviewed and revised the manuscript prior to submission; All authors approved the final version of the manuscript.
ORCID iD: Christopher Vannabouathong  https://orcid.org/0000-0002-9694-6364
https://orcid.org/0000-0002-9694-6364
References
- 1. Alla SR, Deal ND, Dempsey IJ. Current concepts: mallet finger. Hand (N Y). 2014;9:138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Najefi A, Jeyaseelan L, Patel A, Kapoor A, Auplish S. Avulsion fractures at the base of the 2(nd) metacarpal due to the extensor carpi radialis longus tendon: a case report and review of the literature. Arch Trauma Res. 2016;5:e32872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stevens MA, El-Khoury GY, Kathol MH, Brandser EA, Chow S. Imaging features of avulsion injuries. Radiographics. 1999;19:655–672. [DOI] [PubMed] [Google Scholar]
- 4. Husain ZS, DeFronzo DJ. Relative stability of tension band versus two-cortex screw fixation for treating fifth metatarsal base avulsion fractures. J Foot Ankle Surg. 2000;39:89–95. [DOI] [PubMed] [Google Scholar]
- 5. May JH, Levy BA, Guse D, Shah J, Stuart MJ, Dahm DL. ACL tibial spine avulsion: mid-term outcomes and rehabilitation. Orthopedics. 2011;34:89. [DOI] [PubMed] [Google Scholar]
- 6. Pandey V, Cps S, Acharya K, Rao SK. Arthroscopic suture pull-out fixation of displaced tibial spine avulsion fracture. J Knee Surg. 2017;30:28–35. [DOI] [PubMed] [Google Scholar]
- 7. Pandey V, Mathai N, Varshini A, Acharya K. Management of comminuted tibial end bony avulsion of posterior cruciate ligament by open posterior approach using suture bridge technique: a case series. J Clin Orthop Trauma. 2017;8:S36–S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Diaz-Garcia R, Waljee JF. Current management of metacarpal fractures. Hand Clin. 2013;29:507–518. [DOI] [PubMed] [Google Scholar]
- 9. Downing ND. Fractures of the hand. Surgery. 2003;21:256–258. [Google Scholar]
- 10. Feehan LM, Sheps SB. Incidence and demographics of hand fractures in British Columbia, Canada: a population-based study. J Hand Surg Am. 2006;31:1068–1074. [DOI] [PubMed] [Google Scholar]
- 11. Kim KC, Shin HD, Rhee KJ. Treatment of avulsion fractures of the second metacarpal base with a miniplate and screws. Orthopedics. 2008;31:285. [DOI] [PubMed] [Google Scholar]
- 12. DeLee JC. Avulsion fracture of the base of the second metacarpal by the extensor carpi radialis longus. A case report. J Bone Joint Surg Am. 1979;61:445–446. [PubMed] [Google Scholar]
- 13. Bachoura A, Ferikes AJ, Lubahn JD. A review of mallet finger and jersey finger injuries in the athlete. Curr Rev Musculoskelet Med. 2017;10:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39:1338–1344. [DOI] [PubMed] [Google Scholar]
- 15. Salazar Botero S, Hidalgo Diaz JJ, Benaida A, Collon S, Facca S, Liverneaux PA. Review of acute traumatic closed mallet finger injuries in adults. Arch Plast Surg. 2016;43:134–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cheung JP, Fung B, Ip WY. Review on mallet finger treatment. Hand Surg. 2012;17:439–447. [DOI] [PubMed] [Google Scholar]
- 17. Wehbe MA, Schneider LH. Mallet fractures. J Bone Joint Surg Am. 1984;66:658–669. [PubMed] [Google Scholar]
- 18. Cockshott WP. Distal avulsion fractures of the scaphoid. Br J Radiol. 1980;53:1037–1040. [DOI] [PubMed] [Google Scholar]
- 19. Compson JP, Waterman JK, Spencer JD. Dorsal avulsion fractures of the scaphoid: diagnostic implications and applied anatomy. J Hand Surg Br. 1993;18:58–61. [DOI] [PubMed] [Google Scholar]
- 20. Moody L, Zhang AY. Treatment of an unusual trans-scaphoid perilunate avulsion fracture dislocation: a case report. Hand (N Y). 2015;10:328–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cheung JP, Tang CY, Fung BK. Current management of acute scaphoid fractures: a review. Hong Kong Med J. 2014;20:52–58. [DOI] [PubMed] [Google Scholar]
- 22. Kaewlai R, Avery LL, Asrani AV, Abujudeh HH, Sacknoff R, Novelline RA. Multidetector CT of carpal injuries: anatomy, fractures, and fracture-dislocations. Radiographics. 2008;28:1771–1784. [DOI] [PubMed] [Google Scholar]
- 23. Ten Berg PW, Drijkoningen T, Strackee SD, Buijze GA. Classifications of acute scaphoid fractures: a systematic literature review. J Wrist Surg. 2016;5:152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Toker S, Kilincoglu V. An abnormally displaced scaphoid fracture: a case report. Cases J. 2009;2:9309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Canbora K, Ozyurek S, Gumussuyu G, Kose O. Triceps tendon avulsion and associated injuries of the elbow [published online ahead of print May 9, 2013]. BMJ Case Rep. doi: 10.1136/bcr-2013-009460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gajendran VK, Bishop JA. Terrible triad elbow fracture-dislocation with triceps and flexor-pronator mass avulsion. Orthopedics. 2015;38:e143–e146. [DOI] [PubMed] [Google Scholar]
- 27. Kim JY, Lee JS, Kim MK. Fractures of the capitellum concomitant with avulsion fractures of the triceps tendon. J Hand Surg Am. 2013;38:495–497. [DOI] [PubMed] [Google Scholar]
- 28. Naito K, Homma Y, Morita M, Mogami A, Obayashi O. Triceps tendon avulsion: a case report and discussion about the olecranon ossification nucleus. Eur J Orthop Surg Traumatol. 2013;23:193–196. [DOI] [PubMed] [Google Scholar]
- 29. Weng PW, Wang SJ, Wu SS. Misdiagnosed avulsion fracture of the triceps tendon from the olecranon insertion: case report. Clin J Sport Med. 2006;16:364–365. [DOI] [PubMed] [Google Scholar]
- 30. Lambers K, Ring D. Elbow fracture-dislocation with triceps avulsion: report of 2 cases. J Hand Surg Am. 2011;36:625–627. [DOI] [PubMed] [Google Scholar]
- 31. Yoon MY, Koris MJ, Ortiz JA, Papandrea RF. Triceps avulsion, radial head fracture, and medial collateral ligament rupture about the elbow: a report of 4 cases. J Shoulder Elbow Surg. 2012;21:e12–e17. [DOI] [PubMed] [Google Scholar]
- 32. Kobayashi Y, Oka Y, Ikeda M, Munesada S. Avulsion fracture of the medial and lateral epicondyles of the humerus. J Shoulder Elbow Surg. 2000;9:59–64. [DOI] [PubMed] [Google Scholar]
- 33. Al-Kashmiri A, Sun K, Delaney JS. Lateral humeral epicondyle fracture secondary to avulsion of the anconeus muscle. Clin J Sport Med. 2007;17:408–409. [DOI] [PubMed] [Google Scholar]
- 34. Lokiec F, Velkes S, Engel J. Avulsion of the medial epicondyle of the humerus in arm wrestlers: a report of five cases and a review of the literature. Injury. 1991;22:69–70. [DOI] [PubMed] [Google Scholar]
- 35. Ghawabi MH. Fracture of the medial condyle of the humerus. J Bone Joint Surg Am. 1975;57:677–680. [PubMed] [Google Scholar]
- 36. Gruson KI, Ruchelsman DE, Tejwani NC. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008;39:284–298. [DOI] [PubMed] [Google Scholar]
- 37. LaMont LE, Green DW, Altchek DW, Warren RF, Wickiewicz TL. Subscapularis tears and lesser tuberosity avulsion fractures in the pediatric patient. Sports Health. 2015;7:110–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kuroda T, Go G, Ojima S, Nishi S, Mizuno K. Isolated avulsion fracture of the lesser tuberosity of the humerus: a case report. J Shoulder Elbow Surg. 1993;2:221–224. [DOI] [PubMed] [Google Scholar]
- 39. Neogi DS, Bejjanki N, Ahrens PM. The consequences of delayed presentation of lesser tuberosity avulsion fractures in adolescents after repetitive injury. J Shoulder Elbow Surg. 2013;22:e1–e5. [DOI] [PubMed] [Google Scholar]
- 40. Tosun B, Kesemenli CC. Isolated avulsion fracture of lesser tuberosity of the humerus: review of the literature and report of two cases. Int J Shoulder Surg. 2011;5:50–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wu GB, Wang SQ, Wen SW, Yu GR. Isolated avulsion fractures of lesser tuberosity humerus: a case report and review of the literature. Int J Clin Exp Med. 2014;7:780–784. [PMC free article] [PubMed] [Google Scholar]
- 42. Naik M, Tripathy SK, Goyal S, Rao SK. Combined acromioclavicular joint dislocation and coracoid avulsion in an adult [published online ahead of print May 20, 2015]. BMJ Case Rep. 2015. doi: 10.1136/bcr-2014-208563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Schneider MM, Balke M, Koenen P, Bouillon B, Banerjee M. Avulsion fracture of the coracoid process in a patient with chronic anterior shoulder instability treated with the Latarjet procedure: a case report. J Med Case Rep. 2014;8:394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Khoriati AA, Guo S, Thakrar R, Deol RS, Shah KY. Bilateral atraumatic tibial tubercle avulsion fractures: case report and review of the literature. Injury. 2015;46:767–769. [DOI] [PubMed] [Google Scholar]
- 45. Shelton WR, Canale ST. Fractures of the tibia through the proximal tibial epiphyseal cartilage. J Bone Joint Surg Am. 1979;61:167–173. [PubMed] [Google Scholar]
- 46. Subbu R, Nandra R, Jordan R, Krikler S. Lessons learnt from managing an avulsion fracture of the tibial tubercle extending into the tibial physis [published online ahead of print September 20, 2013]. BMJ Case Rep. doi: 10.1136/bcr-2013-200551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Abalo A, Akakpo-numado KG, Dossim A, Walla A, Gnassingbe K, Tekou AH. Avulsion fractures of the tibial tubercle. J Orthop Surg. 2008;16:308–311. [DOI] [PubMed] [Google Scholar]
- 48. Chouhan DK, Dhillon MS, John R, Khurana A. Management of neglected ACL avulsion fractures: a case series and systematic review. Injury. 2017;48:S54–S60. [DOI] [PubMed] [Google Scholar]
- 49. Gamboa JT, Durrant BA, Pathare NP, Shin EC, Chen JL. Arthroscopic reduction of tibial spine avulsion: suture lever reduction technique. Arthrosc Tech. 2017;6:e121–e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Verdano MA, Pellegrini A, Lunini E, Tonino P, Ceccarelli F. Arthroscopic absorbable suture fixation for tibial spine fractures. Arthrosc Tech. 2014;3:e45–e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mann MA, Desy NM, Martineau PA. A new procedure for tibial spine avulsion fracture fixation. Knee Surg Sports Traumatol Arthrosc. 2012;20:2395–2398. [DOI] [PubMed] [Google Scholar]
- 52. Hunter RE, Willis JA. Arthroscopic fixation of avulsion fractures of the tibial eminence: technique and outcome. Arthroscopy. 2004;20:113–121. [DOI] [PubMed] [Google Scholar]
- 53. Meyers MH, McKeever F. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1959;41-A:209–220; discussion 220-222. [PubMed] [Google Scholar]
- 54. Bowes J, Buckley R. Fifth metatarsal fractures and current treatment. World J Orthop. 2016;7:793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Petrisor BA, Ekrol I, Court-Brown C. The epidemiology of metatarsal fractures. Foot Ankle Int. 2006;27:172–174. [DOI] [PubMed] [Google Scholar]
- 56. Heineck J, Wolz M, Haupt C, Rammelt S, Schneiders W. Fifth metatarsal avulsion fracture: a rational basis for postoperative treatment. Arch Orthop Trauma Surg. 2009;129:1089–1092. [DOI] [PubMed] [Google Scholar]
- 57. Japjec M, Staresinic M, Starjacki M, Zgaljardic I, Stivicic J, Sebecic B. Treatment of proximal fifth metatarsal bone fractures in athletes. Injury. 2015;46:S134–S136. [DOI] [PubMed] [Google Scholar]
- 58. Dineen HA, Murphy TD, Mangat S, et al. Functional outcomes for nonoperatively treated proximal fifth metatarsal fractures. Orthopedics. 2017;40:e1030–e1035. [DOI] [PubMed] [Google Scholar]
- 59. Cheung CN, Lui TH. Proximal fifth metatarsal fractures: anatomy, classification, treatment and complications. Arch Trauma Res. 2016;5:e33298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lawrence SJ, Botte MJ. Jones’ fractures and related fractures of the proximal fifth metatarsal. Foot Ankle. 1993;14:358–365. [DOI] [PubMed] [Google Scholar]
- 61. Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002;66:785–794. [PubMed] [Google Scholar]
- 62. Robinson KP, Davies MB. Talus avulsion fractures: are they accurately diagnosed? Injury. 2015;46:2016–2018. [DOI] [PubMed] [Google Scholar]
- 63. Trousdale RDD, Manzanares J. Osteochondral lesions of the talar dome. Orthop Surg. 2001;7:1–12. [Google Scholar]
- 64. Schepers T, van Schie-van der Weert EM, de Vries MR, van der Elst M. Foot and ankle fractures at the supination line. Foot (Edinb). 2011;21:124–128. [DOI] [PubMed] [Google Scholar]
- 65. Bridgman SA, Clement D, Downing A, Walley G, Phair I, Maffulli N. Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England, and a survey of UK practice for severe ankle sprains. Emerg Med J. 2003;20:508–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Shah S, Thomas AC, Noone JM, Blanchette CM, Wikstrom EA. Incidence and cost of ankle sprains in United States Emergency Departments. Sports Health. 2016;8:547–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92:2279–2284. [DOI] [PubMed] [Google Scholar]
- 68. Berndt AL, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959;41-A:988–1020. [PubMed] [Google Scholar]
- 69. Haraguchi N, Kato F, Hayashi H. New radiographic projections for avulsion fractures of the lateral malleolus. J Bone Joint Surg Br. 1998;80:684–688. [DOI] [PubMed] [Google Scholar]
- 70. Nanfelt M, Zekas LJ, Palmer RH. What is your diagnosis? oblique fracture of the talus with subluxation of the talocalcaneal joint and avulsion fracture of the lateral malleolus. J Am Vet Med Assoc. 2006;229:357–358. [DOI] [PubMed] [Google Scholar]
- 71. Oakley J, Yewlett A, Makwana N. Avulsion fracture of the medial malleolus following posterior tibialis tendon dislocation: a case report. Foot Ankle Surg. 2011;17:94–97. [DOI] [PubMed] [Google Scholar]
- 72. Chung KJ, Huang B, Choi CH, Park YW, Kim HN. Utility of 3D printing for complex distal tibial fractures and malleolar avulsion fractures: technical tip. Foot Ankle Int. 2015;36:1504–1510. [DOI] [PubMed] [Google Scholar]
- 73. Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures—an increasing problem? Acta Orthop Scand. 1998;69:43–47. [DOI] [PubMed] [Google Scholar]
- 74. Daly PJ, Fitzgerald RH, Jr, Melton LJ, Ilstrup DM. Epidemiology of ankle fractures in Rochester, Minnesota. Acta Orthop Scand. 1987;58:539–544. [DOI] [PubMed] [Google Scholar]
- 75. Tsiridis E, Kohls-Gatzoulis J, Schizas C. Avulsion fracture of the extensor carpi radialis brevis insertion. J Hand Surg Br. 2001;26:596–598. [DOI] [PubMed] [Google Scholar]
- 76. Garberman SF, Diao E, Peimer CA. Mallet finger: results of early versus delayed closed treatment. J Hand Surg Am. 1994;19:850–852. [DOI] [PubMed] [Google Scholar]
- 77. Okafor B, Mbubaegbu C, Munshi I, Williams DJ. Mallet deformity of the finger. Five-year follow-up of conservative treatment. J Bone Joint Surg Br. 1997;79:544–547. [DOI] [PubMed] [Google Scholar]
- 78. Stern PJ, Kastrup JJ. Complications and prognosis of treatment of mallet finger. J Hand Surg Am. 1988;13:329–334. [DOI] [PubMed] [Google Scholar]
- 79. Damron TA, Engber WD, Lange RH, et al. Biomechanical analysis of mallet finger fracture fixation techniques. J Hand Surg Am. 1993;18:600–607; discussion 608. [DOI] [PubMed] [Google Scholar]
- 80. Lucchina S, Badia A, Dornean V, Fusetti C. Unstable mallet fractures: a comparison between three different techniques in a multicenter study. Chin J Traumatol. 2010;13:195–200. [PubMed] [Google Scholar]
- 81. Lubahn JD. Mallet finger fractures: a comparison of open and closed technique. J Hand Surg Am. 1989;14:394–396. [DOI] [PubMed] [Google Scholar]
- 82. Bischoff R, Buechler U, De Roche R, Jupiter J. Clinical results of tension band fixation of avulsion fractures of the hand. J Hand Surg Am. 1994;19:1019–1026. [DOI] [PubMed] [Google Scholar]
- 83. van Riet RP, Morrey BF, Ho E, O’Driscoll SW. Surgical treatment of distal triceps ruptures. J Bone Joint Surg Am. 2003;85-A:1961–1967. [DOI] [PubMed] [Google Scholar]
- 84. Athwal GS, McGill RJ, Rispoli DM. Isolated avulsion of the medial head of the triceps tendon: an anatomic study and arthroscopic repair in 2 cases. Arthroscopy. 2009;25:983–988. [DOI] [PubMed] [Google Scholar]
- 85. Dunn JC, Kusnezov N, Fares A, et al. Triceps tendon ruptures: a systematic review. Hand (N Y). 2017;12:431–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Gharanizadeh K, Mazhar FN, Molavy N, Bagherifard A, Shariatzadeh H. Avulsions of Triceps Brachii: associated injuries and surgical treatment; a case series. Acta Orthop Belg. 2016;82:197–202. [PubMed] [Google Scholar]
- 87. Ma JT, Mao YJ, Yu M, Yu GF, Zhu CQ, Zhang MC. Clinical characteristics of triceps brachii tendon rupture at olecranon ending. Zhongguo Gu Shang. 2014;27:957–960. [PubMed] [Google Scholar]
- 88. Louis DS, Peck D. Triceps avulsion fracture in a weightlifter. Orthopedics. 1992;15:207–208. [DOI] [PubMed] [Google Scholar]
- 89. Sharma P, Vijayargiya M, Tandon S, Gaur S. Triceps tendon avulsion: a rare injury. Ethiop J Health Sci. 2014;24:97–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Kamath AF, Cody SR, Hosalkar HS. Open reduction of medial epicondyle fractures: operative tips for technical ease. J Child Orthop. 2009;3:331–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Vavken P, Bae DS, Waters PM, Flutie B, Kramer DE. Treating subscapularis and lesser tuberosity avulsion injuries in skeletally immature patients: a systematic review. Arthroscopy. 2016;32:919–928. [DOI] [PubMed] [Google Scholar]
- 92. Goeminne S, Debeer P. The natural evolution of neglected lesser tuberosity fractures in skeletally immature patients. J Shoulder Elbow Surg. 2012;21:e6–e11. [DOI] [PubMed] [Google Scholar]
- 93. Gazzotti G, Patrizio L, Bondioli S, Scaravella E, Sabetta E. Successful surgical treatment of a four part fracture dislocations of the proximal humerus and coracoid avulsion. Acta Biomed. 2015;86:106–110. [PubMed] [Google Scholar]
- 94. Osti L, Buda M, Soldati F, Del Buono A, Osti R, Maffulli N. Arthroscopic treatment of tibial eminence fracture: a systematic review of different fixation methods. Br Med Bull. 2016;118:73–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Osti L, Merlo F, Liu SH, Bocchi L. A simple modified arthroscopic procedure for fixation of displaced tibial eminence fractures. Arthroscopy. 2000;16:379–382. [DOI] [PubMed] [Google Scholar]
- 96. Wu GB, Li B, Yang YF. Comparative study of surgical and conservative treatments for fifth metatarsal base avulsion fractures (type I) in young adults or athletes. J Orthop Surg (Hong Kong). 2018;26. doi: 10.1177/2309499017747128. [DOI] [PubMed] [Google Scholar]
- 97. Xie L, Guo X, Zhang SJ, Fang ZH. Locking compression plate distal ulna hook plate fixation versus intramedullary screw fixation for displaced avulsion fifth Metatarsal Base fractures: a comparative retrospective cohort study. BMC Musculoskelet Disord. 2017;18:405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Badekas T, Takvorian M, Souras N. Treatment principles for osteochondral lesions in foot and ankle. Int Orthop. 2013;37:1697–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Fowler TT, Pugh KJ, Litsky AS, Taylor BC, French BG. Medial malleolar fractures: a biomechanical study of fixation techniques. Orthopedics. 2011;34:e349–e355. [DOI] [PubMed] [Google Scholar]
- 100. Park JW, Kim SK, Hong JS, Park JH. Anterior tibiofibular ligament avulsion fracture in weber type B lateral malleolar fracture. J Trauma. 2002;52:655–659. [DOI] [PubMed] [Google Scholar]
- 101. Cleak DK, Dawson MH, Phoenix OF. Tension band wiring of avulsion fractures of the medial malleolus: a modified technique minimizing soft tissue injury. Injury. 1982;13:519–520. [DOI] [PubMed] [Google Scholar]
- 102. Downey MW, Duncan K, Kosmopoulos V, et al. Comparing the knotless tension band and the traditional stainless steel wire tension band fixation for medial malleolus fractures: a retrospective clinical study. Scientifica. 2016;2016:3201678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Wong-Chung J, Tucker A, Lynch-Wong M, Gibson D, O’Longain DS. The lateral malleolar bony fleck classified by size and pathoanatomy: the IOFAS classification. Foot Ankle Surg. 2017;24:300–308. [DOI] [PubMed] [Google Scholar]