Abstract
Objectives: This scoping review (a) describes programs to improve mobility in hospitalized adults and (b) determines the methods used to measure mobility. Method: The Joanna Briggs Institute Methodology for Scoping Reviews was used to conduct this review. Results: Our findings suggest that using a multidisciplinary approach may be the most effective way to promote mobility in hospitalized older adults. Most studies did not articulate how physical activity was measured, indicating that more research is needed. Discussion: The literature shows that implementation of protocols designed to improve the early and regular implementation of physical mobility activities improves the health outcomes of hospitalized older people. Costs associated with healthcare utilization are also reduced, including hospital length of stay. Mobility programs that quantified mobility through validated measurement tools or accelerometers are the most promising as they provide feedback that reinforces progress of the patient and the expected benefits of early mobility.
Keywords: prevention, rehabilitation, early mobility, hospitalized older adults, scoping review, mobility programs
Background
The number of older adults in the United States is predicted to increase from 43.1 million in 2012 to well over 70 million by 2030, and older adults over the age of 85 years will triple from 5.9 million in 2012 to 14.1 million in 2040 (Administration on Aging, 2012). One third of all hospitalized patients in the United States are over 65, and as the number of older adults grows, increased hospital utilization can be expected (Weiss & Elixhauser, 2014; Weiss, Elixhauser, & Andrews, 2006). Insufficient physical mobility such as ambulation during hospitalization is commonly reported. Promoting physical mobility has been defined as getting patients out of bed, including sitting in a chair, toileting at bedside or bathroom, standing, and ambulating (Hoyer, Brotman, Chan, & Needham, 2015). While the promotion of physical mobility is important for all adult patients, people who are already frail, and older people are at greatest risk for sustaining muscle loss and weakness that could be long-lasting. Insufficient physical mobility during hospitalization is known to lead to a series of cascading, functional, decline-related problems including frailty, falls, complex hospital-to-home transitions, and death, even after controlling for illness severity and comorbidity (Brown, Friedkin, & Inouye, 2004; Brown, Redden, Flood, & Allman, 2009; Brown, Roth et al., 2009; Cruz-Jentoft et al., 2010; Greysen, 2016; Pedersen et al., 2013; Theou et al., 2016; Zisberg & Syn-Hershko, 2016).
Hospitalized older adults with low physical mobility, such as ambulation, are 34 times more likely to die, and 6 times more likely to be institutionalized compared with those who ambulate two or more times per day (Brown et al., 2004). These statistics are alarming considering that many hospitalized people are, in fact, older adults. Hospitalized older patients spend greater than 80% of their time lying in bed and less than 43 min per day walking, despite being ambulatory upon admission (Brown, Redden et al., 2009). Insufficient physical mobility in hospitalized older patients increases the risk for frailty and functional decline (Theou et al., 2016), further contributing to disability, morbidity, and mortality (Afilalo, 2011). Recovering from functional decline is challenging and can adversely impact older adults’ quality of life and transitions of care (Boltz, Capezuti, Shabbat, & Hall, 2010; Brown, Roth et al., 2009).
Regular physical mobility during hospitalization is critical to prevent functional decline and frailty (Zisberg, Shadmi, Gur-yaish, Tonkikh, & Sinoff, 2015; Zisberg & Syn-Hershko, 2016). Furthermore, there is consistent evidence that interventions to increase physical mobility are effective in reducing functional decline. Little is known about the feasibility of integrating these interventions into the hospital workflow to improve the physical mobility in adult patients (Ash et al., 2016; Engel, Tatebe, Alonzo, Mustille, & Rivera, 2013; Hastings, Sloane, Morey, Pavon, & Hoenig, 2014; King, Steege, Winsor, VanDenbergh, & Brown, 2016; Kosse, Dutmer, Dasenbrock, Bauer, & Lamoth, 2013; Wood et al., 2014).
Promoting physical mobility in hospitalized older patients is considered routine nursing care (Doenges, Moorhouse, & Murr, 2014). However, studies confirm that insufficient physical mobility is common (Zisberg & Syn-Hershko, 2016) and that patients are not adequately involved in decisions about their hospital care specific to promote physical mobility including ambulation (Fisher, Graham, Ottenbacher, Deer, & Ostir, 2016; Greysen, 2016). Recent literature about the effectiveness of mobility programs shows promise; yet, there is a lack of synthesized information that describes hospital-based programs to improve mobility in hospitalized adults, and the best-practice methods to measure mobility remain unknown. Thus, this gap in knowledge is addressed by conducting a scoping review to address and inform current practice. The purpose of this scoping review is to (a) describe hospital-based programs to improve mobility in hospitalized adults and (b) determine the methods to measure mobility.
Method
Design
In the spirit of evidence-based clinical practice, clinicians are interested in the selection of optimal interventions/treatments for their patients to overcome the apparent gaps in care (Guyatt, Rennie, Meade, & Cook, 2015). Accordingly, we conducted a scoping review to examine hospital-based programs to improve physical mobility in hospitalized adults; and explored what methods are used to measure physical mobility when programs to improve physical mobility have been implemented in the acute-care hospital setting for adults/older adults. This scoping review synthesis method will allow us to explore the broad topic of physical activity/mobility programs and enable knowledge transfer from all study types and gray literature to clinicians of all disciplines working in the acute care hospital setting seeking to promote the physical mobility of hospitalized adult/older adult patients. Akin to the systematic review methodology, the scoping review methodology is considered a rigorous and systematic approach to knowledge synthesis. Scoping reviews differ from systematic reviews in several ways (Arksey & O’Malley, 2005).
In scoping reviews, the research question is usually more broadly defined, and the inclusion/exclusion criteria are developed post hoc at the study selection stage, in contrast with systematic reviews, where the question is highly specific and the inclusion/exclusion criteria are developed a priori or at the protocol stage. Scoping reviews include all study types and “chart” the data based on themes and key issues (The Joanna Briggs Institute, 2015). However, scoping reviews do not include a quality assessment of the studies. Systematic reviews traditionally include specific study types with the goal to synthesize and aggregate quantitative study findings. To conduct the scoping review, we used the 6-step framework developed by Arksey and O’Malley and advanced by Levac, Colquhoun, and O’Brien (2010). The framework includes (a) identifying the research question; (b) identifying relevant literature; (c) study selection; (d) charting the data; (e) collating, summarizing, and reporting the articles; and (f) consulting and translating knowledge (Arksey & O’Malley, 2005).
Search Strategy
A university librarian assisted the search of databases CINHAL, JBIMSR, Cochrane, PsychInfo, Web of Science, and PubMed (Morris, Boruff, & Gore, 2016). The researchers and librarian jointly decided the search terms: Early ambulation and nurs*, and adults, and hospitalization, physical mobility AND hospitalized older adults. Reference lists of articles were reviewed to identify additional references (snowball method), resulting in a total of 1,128 studies, plus 5 conference proceedings and 20 dissertations. All conference proceedings were abstracts with full manuscripts published and, thus, were duplicates of articles previously reviewed by authors. The following criteria were utilized for this scoping review: types of studies, population and setting, and outcome measures. Of the dissertations reviewed, none met inclusion criteria for this scoping review.
Types of studies
In recognizing the complexities and human factors inherent in the hospital setting and, in particular, in conducting research in this space (Catchpole, 2013; Ebright, Patterson, Chalko, & Render, 2003; Lehman, 2009), we included all study types including quality improvement (QI) projects, pilot studies, randomized control trials, and quantitative descriptive studies, and gray literature. We did not limit the geographic area and included studies if they met our inclusion/exclusion criteria. We excluded literature reviews because, while they provided a summary of the state of knowledge and science on this subject, we sought to examine primary studies and not secondary sources.
Population and setting
Adult patients (ages 60 and over) admitted to an acute care hospital, and in intensive care and non-intensive care settings, were included. If studies included younger adults, we examined the sample to ensure that at least 40% of the population were 60 and older. This approach was described in one study as a feasible means of including studies when a subsample of the population meets inclusion criteria. Other authors used 95% as their age group inclusion criteria for systematic reviews (de Morton, Keating, & Jeffs, 2007). Some investigators studied “adults” but the majority of the sample was, in fact, older adults. Our target population is older adults. The studies that implemented programs to promote physical mobility (even if older people are the target) are usually implemented on hospital units that have both “adults” and “older adult” patients. The physiological age of a person can be higher or lower than their chronological age, because aging is not only limited to time, but is, in fact, a complex process with multiple causes.
Classification of adult status can be variable. We found one source that classified 18 to 35 as young adults, 36 to 55 as middle-aged adults, and 55+ as older adults (Petry, 2002). Orkaby et al. (2018) examined frailty and arterial stiffness in community-dwelling older adults that targeted ⩾60 years of age. The Centers for Disease Control and Prevention (CDC, 2015) classifies people aged 65+ as older adults based on Medicare eligibility. Yet, the United Nations and the World Health Organization (WHO) accept older adults as 60+ (WHO, 2002; United Nations, 2015). Advanced age and even a more recent term, oldest old, are found in the literature referring to those over 80+ in other countries (WHO, 1999; Rodondi, Chevallet, & Rizzoli, 2012). We chose to limit our search to adults aged 60 and older based on the physiological impact of physical immobility on the hospitalized individual such as decubiti, decreased musculoskeletal function, falls, functional decline, and so on and to capture a broader array of studies. Malhotra, Chan, Alay, Ma, and Saito (2016) compared studies from 1995 to 2015 of life expectancy estimates based on inactive health states for age 60 and age 65 groups. While the focus of their study was gender gaps in life expectancy based on activity/inactivity, the 60 and 65 age groups both experienced negative results of decline in their summary of the literature.
Outcome measures
We included only those studies (in English) that identified outcome measures or variables related to the utilization of a program, tool, or mechanism for measuring physical mobility or activity. For example, we included nurse-led, physical therapy-led, and multidisciplinary-led programs to improve physical mobility in this population. Because researchers are interested in a variety of outcome measures, we included all the outcome measures captured by the studies that matched our review criteria.
Studies conducted in rehabilitation hospitals were excluded because (a) such settings focus much of the patient’s time on activities designed to return function, physical mobility, and independence using rehabilitation teams; and (b) barriers to promoting physical mobility are uniquely different. Setting the age group to 65 or older would have resulted in only 9 studies included in this review, and limiting our review to studies that targeted 95 to 100% of our selected age group of ⩾60 years of age would have resulted in 24 studies. As the value of early mobilization has been extensively reported in the literature, and care of patients needs to be consistent across the age continuum, we defined our targeted population of older adults as age 60 and older.
Selection Process
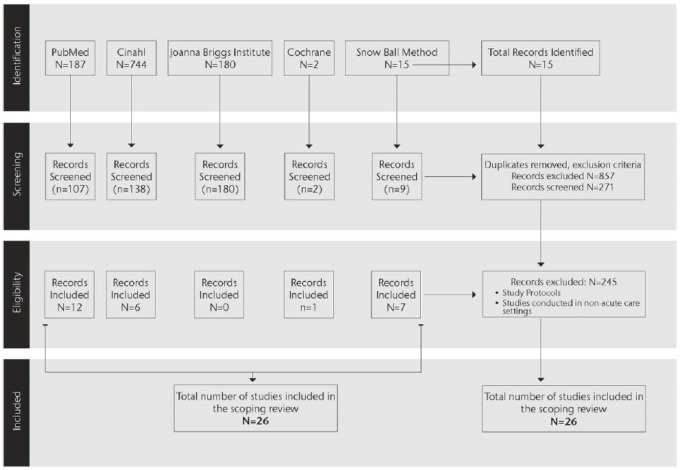
Reviewers (n = 4) independently began the process of identification and selection of relevant papers. The first reviewer used 5 databases (PubMed, CINAHL, Cochrane Review, Web of Science, and Google Scholar) and the second reviewer searched PubMed and CINAHL databases. Two other independent reviewers searched additional databases once terms were identified and agreed upon: JBIMSR, Cochrane, and PsychInfo. Web of Science and PubMed identified the same number of articles (N = 187). We also searched gray literature such as conference proceedings, and ProQuest Dissertations and Theses (N = 6,170). Conference proceedings were summaries of published research that were already included in this article. The ProQuest Dissertations and Theses using the search terms “physical mobility and hospitalized older adults” provided 5 articles relevant to this review. Titles and abstracts were screened by all reviewers for relevance and duplicates removed, resulting in the exclusion of 245 articles. To be included, research articles had to be published in the last 20 years, written in English, and retrievable in full text (see Figure 1). If there was a question or disagreement in the inclusion search, the reviewers ask the questions: (a) Did the papers include only adults? (b) If adults were the target population, were at least 40% of the adults 60 years or older? (c) Did the papers identify a physical mobility program? (d) Were outcomes identified? and (e) Was there an identifiable measurement for physical mobility or physical activity? Given that, in the last 10 years, a variety of technology has been used in research (e.g., actigraphy devices, Fitbit, and smartphones) to measure physical activity, our rationale for including articles within the 10-year framework is in line with standard literature searches. However, we expanded the search to 20 years to ensure we captured relevant older studies. Only articles that examined the outcomes of programs to improve physical activity in hospitalized adults (age 60 and older) were included, resulting in 26 articles that were examined for this scoping review.
Figure 1.
Prisma diagram.
Results
Different Meanings for Mobility
During the review of the literature, it became evident that the term mobility was frequently utilized in a variety of ways, making synthesis of the literature difficult. For example, “mobility” has been used to describe the physical activities necessary to maintain the functional ability of a patient, including ambulation, range-of-motion, and strengthening exercises (Zisberg et al., 2011). Second, mobility has been used to describe the physical functional ability, meaning what the patient is actually able to do (Brown et al., 2004; Brown, Redden, et al., 2009). Furthermore, mobility has been described in terms of levels of mobility, which is an attempt to quantify the mobility. A low level of mobility has been described as inactivity such as bed rest, and sitting in the chair with purposeful physical exercises such as ambulation either decreased, or absent (Brown et al., 2004; Pashikanti & Von Ah, 2012). A concept analysis found that the promotion of physical mobility is an “. . . interdisciplinary, goal-directed therapy to facilitate movement and improve patient outcomes” (Amidei, 2012, p. 80, emphasis added). The further clarification of conceptual discrepancies and dissonance could give directions for further inquiry and perhaps positively influence interdisciplinary efforts to improve the mobility of hospitalized older adults. For the purpose of this review, we will define the promotion of physical mobility as a process of getting patients out of bed, including sitting in a chair, toileting at bedside or bathroom, standing, and ambulating (Hoyer et al., 2015), with the purpose of preventing functional decline. However, as we write the results of the study findings, we will use the terms that the authors of the studies have used.
Programs to improve physical mobility (physical activity) in the hospital setting were either implemented in intensive care units, or general inpatient units. We included one Cochrane systematic review (n = 1), which described exercise programs provided to older medical inpatients as their secondary objective. The following themes were noted in the included studies: nurse led/driven (n = 6), physical therapy-led (n = 5), and interdisciplinary or multidisciplinary-driven (n = 14) mobility programs.
Nurse-Driven Mobility Programs
The Association of Rehabilitation Nurses (ARN) advocates for specialty nurses to take the lead in delivering evidence-based practice (EBP) and supportive technology to deliver optimal patient care (Vaughn et al., 2016). All nurse-led studies incorporated a quantitative measurement using pedometers, specific instruments for evaluation of outcomes, measures of milestones such as distance ambulated, or a novel protocol for measuring outcomes selected for their studies. The physical therapy-led studies also used distance in feet, accelerometry, mobility scales, and measured muscle strength. The multidisciplinary teams utilized a variety of mobility scales, hospital mobility protocols, Activities of Daily Living (ADL), or a defined program (walking program for older hospitalized veterans [STRIDE]; Resource-efficient mobility program [REMP]). Two studies incorporated Katz’s ADL as their measurement tool, and general Physical Therapy/Occupational Therapy (PT/OT) activities for patients. Table 1 summarizes key features of nurse-led studies.
Table 1.
Nurse-Led Mobility Studies (N = 6).
| Author(s), Year | Design | Sample size/setting (SD) | Aim/research question | Mobility Measurement | Outcome variables |
|---|---|---|---|---|---|
| Dickinson, Tschannen, and Shever (2013) | Pre-/Post-Mobility Protocol Implementation |
N = 1,112 Mean age: 58.6 (SD 16.3) |
Does early standardized process for mobility reduce or eliminate development of PU in a surgical ICU? | Early Mobility protocol: “Moving & Grooving” 3 phases with 5 categories in each. |
PU development-Braden assessment LOS Mobility categories |
| Drolet et al. (2013) | Quasi-experimental-QI | 3 months pre-implementation: ICU = 193 IMCU = 349 6 months post-implementation: 426 ICU 358 IMCU Mean age 65-67 (SD 17) |
Does a nurse-driven mobility protocol increase the percentage of patients ambulating during the first 72 hr of their hospital stay? | Mobility algorithm with gait belt-ambulation measured in feet | Distance measured Activity readiness assessments—multiple times/day by RN |
| King, Steege, Winsor, VanDenbergh, and Brown (2016) | 13-week Pilot study (Pre-/Post-training) with chart audit Qualitative study |
Registered nurses and certified nursing assistants participated in focus
groups. EMR of “Older adults” |
Developing a system-based intervention targeting barriers to nurse-initiated patient ambulation. | MOVIN: Frequency and distance (in feet) of ambulation |
Quantitative: Ambulation frequency/distance, numeric documentation, % patients
ambulating/day Qualitative: 3 themes identified |
| Klein, Mulkey, Bena, and Albert (2015) | Prospective, 2-group, Pre-/Post-intervention, comparative design |
N = 637 Age mean (SD): 62.7 (16.1) |
Does early mobilization protocol increase mobility and improve clinical/psychological outcomes? | Progressive mobility program with 4 measured milestones and 16 mobility levels | LOS 30d mortality—no significance DVT results—borderline significance |
| Padula, Hughes, and Baumhover (2009) | Nonequivalent, control group | N = 50; ⩾60+ | What is the impact of a nurse-driven mobility protocol on functional decline? | GENESIS: Geriatric Friendly Environment through Nursing Evaluation &
Specific Interventions for Successful Healing. Instruments used: (a) Functional status-Barthel Index, (b) Get Up & Go test |
LOS—treatment group had shorter LOS (4.96 days treatment vs. 8.72 days
control) Functional status—declined for both groups from preadmission to admission; treatment group scores were significantly higher at discharge than control group |
| Teodoro et al. (2016) | Pretest/posttest RCT: 1. Usual care Experimental |
N = 48 Mean age: 63.3 (+/–15.9) |
Determined if a formalized patient-focused program could improve ambulation in hospitalized medical-surgical patients. | STEP-UP: Studied the effectiveness of a Patient Ambulation Protocol | Primary outcome: Patient ambulation on 2 sequential days measured via
pedometer Ambulation in experimental group increased while usual care group decreased from baseline |
Note. PU = Pressure Ulcers; ICU = Intensive Care Unit; LOS = length of stay; QI = Quality Improvement; IMCU = Intensive Medical Care Unit; EMR = electronic medical record; RN = Registered Nurse; DVT = Deep vein thrombosis; RCT = Randomized Clinical Trials.
Randomized clinical trial
Teodoro et al. (2016) utilized a pre/posttest randomized clinical trial (RCT) design with 48 adults (mean age 63.3 +/–15.9 years). Ambulation was recorded using a pedometer measuring distance traveled in steps. There were 3 components to the ambulation program: (a) An educational video for patients and family on the importance of walking, (b) Daily goals for walking were posted inside patient rooms, and (c) A walking reminder card was placed on patients’ overhead tables with reminders to STEP-UP. Comparing pretest number of steps, the ambulation group (experimental group) increased in number of steps/hr counted for both posttest days compared with the control group.
Quasi-experimental
Drolet et al. (2013) developed a nurse-driven physical mobility protocol (Move to Improve) to increase the percentage of patients ambulating during their first 72 hr of hospitalization. While nurses took the lead, a team-based protocol (consisting of Registered Nurses [RN], advanced practice nurses, physical therapists, critical care pharmacists, respiratory therapists, and a critical care physician) used a physical mobility algorithm and gait belts. In addition, physical and respiratory therapists provided education regarding the mobilization of vented patients. Outcome measures included frequency and rates of ambulation before and after the intervention with distance measured for each patient’s ambulation efforts. Three months prior to implementation, only 6.2% of intensive care unit (ICU) patients and 15.5% of medical patients ambulated in the first 72 hr. Following implementation of the program, 20.2% of ICU patients and 71.8% of medical patients ambulated within the first 72 hr. Study findings suggest that nurses may increase patient mobility when specific guidelines and support is present. Study limitation includes a small sample size (N = 42), and pre-post study design.
Padula, Hughes, and Baumhover (2009) conducted a nonequivalent control-group study to examine the outcomes of a nurse-driven physical mobility protocol: The Geriatric Friendly Environment through Nursing Evaluation and Specific Interventions for Successful Healing (GENESIS) to improve functional status in 50 hospitalized older adults age ⩾60. The physical mobility program consisted of nurse’s questioning any bed-rest orders and directing a certified nurse assistant (CAN) to ambulate patients 3-to-4 times daily. The treatment group ambulated in the hall 2.7 days earlier and 3.12 times per day compared with the control group with 4.9 days (p = .007) and 2.44 times/day (p = NS). The treatment group had significantly shorter lengths of stay (LOS) of 4.96 days compared with 8.72 days for the control group (p < .001).
Prospective studies
Klein, Mulkey, Bena, and Albert (2015) conducted a two-group comparative design study in a neurologic ICU to determine if a structured, early mobilization protocol increased physical mobility and improved clinical and psychological outcomes. Data were collected 4 months pre- and post-intervention. The physical mobility protocol included (a) progressive mobility, (b) written physical mobility orders, and (c) a clinical nurse specialist to advocate for and assist with patient physical mobility. Noticeable outcomes from the program included an increased number of patients who could bear weight and pivot to a chair, with ambulation increasing from 21% in the pre-intervention group compared with 41% in the post-intervention group. ICU length of stay decreased from 7.4 to 4.7 days (p < .001), and hospital LOS decreased from 15.2 to 10.2 days (p < .001). The pre/post study design at a single center was a limitation, however, a moderate sample size was considered a strength (Klein et al., 2015).
Pilot and QI studies
King et al. (2016) used a system-based intervention (MOVIN) that consisted of five components including (a) psychomotor skills training for nurses, (b) communication tools such as dry-erase boards for information sharing between nursing staff, (c) ambulation pathways with clearly defined distance markers, (d) ambulation resources, and (e) a positive ambulation culture. Chart audits were used to note the frequency and distance of patient ambulation. The results showed a statistically significant increase in ambulation occurrences (t = 4.18, p = .001) and total distance measured in feet that patients ambulated on their units (t = 2.75, p = .01). Clinically, this equated to a threefold increase in the distance ambulated (from 12,175 feet per week to 30,218 feet during the intervention phase of the study).
Dickinson, Tschannen, and Shever (2013) implemented an early mobility protocol (“Moving and Grooving”) that used three principles: (a) evaluate patients for early mobilization at specific intervals within a day, (b) value even the smallest of efforts made by patients, and (c) recognize that poor tolerance for an activity is not a prediction for the rest of the patient care days. Pre- and post-implementation data were collected with significant improvements noted in four areas post-implementation for intervention group versus controls: LOS, hospital days to ICU, ICU-LOS, and Braden Scale for Pressure Ulcer scores. The authors acknowledge that the outcome of interest (decreased incidence of pressure ulcers) was not achieved by early mobility. There was a noticeable increase (71%) in compliance rates for using the mobility protocol.
PT-Driven Mobility Programs
For PT-driven mobility programs, we identified 6 articles (see Table 2). PT-led studies were defined as those studies where one or more authors were physical therapists; the articles described themselves as PT-driven; or the program being evaluated was developed, monitored, and evaluated by physical therapists.
Table 2.
PT-Led Mobility Studies (N = 5).
| Author(s), year | Design | Sample size/setting (SD) | Aim/research question | Mobility measurement | Outcome variables |
|---|---|---|---|---|---|
| Engel, Tatebe, Alonzo, Mustille, and Rivera (2013) | QI project (retrospective) | Adult medical-surgical ICU patients admitted 2009-2010 to California medical
center N = 473 Mean age = 64.4 (SD 15.4) |
Does increasing early PT improve function and discharge status and reduce length of stay? | Average distance in feet ambulated (measurement not validated) | LOS, days to PT evaluation, % discharged home |
| Engel, Needham, Morris, and Gropper (2013) | QI (Plan-Do-Study-Act) (retrospective) | Three U.S. ICUs (681 adults) | Does a structured ICU early mobility program improve outcomes and reduce costs? | Not measured | Number of PT sessions, length of stay, inpatient costs, |
| Fisher, Graham, Ottenbacher, Deer, and Ostir (2016) | Prospective, observational clinical cohort study | 164 older adults ⩾65 with acute medical illness admitted to hospital | Compare predictive power of accelerometry-derived walking activity and ADL functional measures on 30-day readmission. | Accelerometry (Orthocare Innovations Step Watch Activity Monitor—records steps per day & provides no feedback) | Readmission within 30 days of discharge |
| Raymond et al. (2017) | RCT |
N = 468 ⩾65 |
Does a HIFE group improve outcomes & therapist efficiency more than individual physiotherapy in older inpatient adults? | HIFE | Elderly Mobility Scale Berg Balance Scale Gait speed Timed Up and Go test Falls, LOS |
| The TEAM Study Investigators (2015) | Prospective, multicenter cohort study | 192 adults (58.0 +/–15.8 years) from 12 ICUs in Australia/New Zealand | What is the observed early mobilization while on mechanical
ventilation? What is the relationship between occurrence of ICU-acquired weakness and recovery? |
ICU mobility scale, early mobilization—any active exercise where patients used their muscle strength | PT interactions, duration, type, and barriers to mobilization. Medical Research Council Manual Muscle Test Sum Score, survival status, health-related quality of life |
Note. PT = Physical Therapy; QI = Quality Improvement; ICU = Intensive Care Unit; LOS = length of stay; ADL = Activities of Daily Living; RCT = Randomized Clinical Trials; HIFE = High-intensity functional exercise.
Randomized-controlled trial
Raymond et al. (2017) studied the effects of a high-intensity functional exercise (HIFE) group using an interdisciplinary mobility approach with participants 65 years and older (n = 468). The HIFE group consisted of group PT. Participants received a standing HIFE group three times weekly and individualized PT twice weekly. The control group was offered daily PT sessions with no group sessions. The outcome measures include the Elderly Mobility Scale, the Berg Balance Scale, gait speed, Timed Up and Go test, falls, and length of stay. Participants improved on all primary outcome measurements regardless of their group assignment. A significant difference between groups was only found for the Berg Balance Scale. Results show that group therapy combined with individual PT could be as effective as individualized PT alone. The economic impact of physical therapist efficiency was not measured.
Prospective, observational studies
Fisher et al. (2016) measured walking activity as the number of consecutive steps taken in a 24-hr period during a hospital stay measured by a dual-axis worn accelerometer. Their goal was to identify the number of steps walked as a threshold for readmission risk factors. They found a significant association between mean daily steps and 30-day hospital readmission and identified 475 steps as a possible threshold of minimal walking activity for a hospital admission. While this study did not develop, measure, or evaluate a new or existing program, the authors did focus on measuring walking with an accelerometer and determined sensitivity and specificity of number of consecutive steps as a predictor for hospital readmission.
The TEAM Study Investigators (2015) researched a current mobilization practice in an ICU setting and compared functional recovery at 6 months post-discharge by measuring muscle strength. The authors did not introduce or evaluate a new program; instead, they recruited patients (n = 192) who were independently mobile prior to ICU admission, had been in the ICU <72 hr, had been on ventilation for >24 hr with anticipation of at least an additional 48 hr more on ventilation. Early mobilization was defined as any active exercise where the patient could assist using their own muscle strength. Only 12% (n = 26) of patients actually walked during their hospitalization. The ICU mobility scale was used to rank patients. Investigators noted barriers to early mobilization and correlated mobility with survival at 90-day post-discharge. The TEAM investigators study focused on invasively ventilated patients in several ICU settings where PT is the standard of care and a multidisciplinary approach has been in place for several decades. While this study was included in the review, it was impossible to ascertain what percentage of patients were actually 60+ years of age. Patients ages ranged from 42.2 to 73.8 years. Because the setting was ICU, it may be ethically challenging to offer a program to only one age group when all patients may be at risk for similar complications that may result from inactivity or delayed physical mobility.
QI studies
The two QI studies varied in approach, design, measurement of mobility, and outcomes measured with a central focus on adults in the ICU setting. Using a 9-month retrospective analysis of a QI project at one site, Engel, Tatebe, et al. (2013) noted an increase in the number of patients receiving PT in the ICU. With an emphasis on early mobility, the research team established a collaborative early mobilization team of professionals (interprofessional/multidisciplinary: respiratory therapist, RNs, physicians, physical therapist). Physical therapists created guidelines based on individualized patient assessments, and the early mobilization team was tasked with adhering to collaborative practices, communication, and identification of barriers during the patients’ ICU stay. The results of this program showed statistical significance in the days for visit by a physical therapist—a decrease from 3 days for initial evaluation to 1 day (z = −5.97, p < .001); functional improvement increased from 40 feet (pre-intervention) to 140 feet walked (post-intervention; z = −3.132, p = .002); and overall hospital LOS decreased from 24.5 days to 16 days (z = −2.45, p = .014). Percentage of patients reporting satisfaction with their care increased along with significant increase in the number of ambulatory patients overall, from 43% the previous year to 50% during the intervention period (χ2 = 8.23, df = 1, p = .004).
Engel, Needham, Morris, and Gropper (2013) chose the Plan-Do-Study-Act framework for their three-site ICU early mobilization QI project. Their project investigated whether early PT in the ICU patient was practical and safe, and if a protocol-driven mobility plan would have an impact on practice patterns. Results revealed that not only did the number of patients receiving PT or OT increase from 70% to 93%, the mean number of treatments increased from 1 to 7 during the QI project period. Direct patient total costs were reduced by US$504,789 compared with the usual care group. An interprofessional (multidisciplinary) mobility team was directed and led by the lead physical therapist. A full-time mobility technician position was developed as part of the ongoing progression of their program.
Multidisciplinary-Driven Mobility Programs
Multidisciplinary studies were defined as those that included 3 or more professionals of the healthcare team (nurses, physicians, PT, and CNAs). These studies could be “led” by any one person on the team, but the overall focus was a team approach to assessing, supporting, and evaluating patient mobility. A total of 14 studies are included in this section of the scoping review (see Table 3).
Table 3.
Multidisciplinary-Led Mobility Studies (N = 14).
| Author(s) | Design | Sample size/setting (SD) | Aim/research question | Mobility measurement | Outcome variables |
|---|---|---|---|---|---|
| Azuh et al. (2016) | QI pilot project Descriptive correlation design | 1-year time frame; MICU (N = 3,233) 43.5-47.6% of patients 65+ 50.6-53.2% of patients = 26-64 years of age |
What are the benefits of early, active mobility in the MICU? | 5-point mobility scale to determine highest level of activity achievable | - Type of mobility interventions - Mobility/skin assessment - Hospital acquired pressure ulcer - Mobility level - Braden score - Rate of ventilator-associated pneumonia - ICU LOS - Hospital readmission - Staff attitudes toward mobilization and barriers |
| Brown et al. (2016) | Single blind RCT |
N = 100 Ages ⩾65 |
What is the effect of an in-hospital mobility program on posthospitalization function and community mobility? | Utilized a standard hospital mobility protocol | Functional outcome assessment Community mobility assessment Hospital mobility assessment Cognitive assessments Daily 24-hr fall reporting |
| Bummel et al. (2014) | RCT: 1:1:2 Usual care Early PT only Early cognitive therapy plus PT |
N = 87 Ages 48-69 |
What is the feasibility of early cognitive and PT/OT (combined) in hospitalized ICU adults? | Katz activities of ADL | ICU LOS Functional status: ADL Intervention safety |
| Darragh, Shiyko, Margulis, and Campo (2014) | Retrospective cohort design | Electronic health records N = 1,315 Mean age 80-82 |
What is the effect of a SPHM program on patient self-care outcomes? | - Self-care performance (FIM): Eating, grooming, dressing, upper body,
dressing lower body, bathing, and toileting. - Mobility was assessed using the mobility subscale of the motor FIM. |
- Self-care FIM at admission - LOS - Mobility score at admission - Self-care FIM at discharge |
| Hastings, Sloane, Morey, Pavon, and Hoenig (2014) | Clinical demonstration program |
N = 92 Older Veterans: Ages ⩾65 |
Describes the STRIDE program. Compared outcomes of STRIDE enrollees with those of a prospectively identified comparison group. |
STRIDE program: Early assessment Supervised ambulation Education to veterans & family |
LOS Falls 30-day ED visits Readmission rates |
| Hoyer et al. (2016) | QI with descriptive correlation design | 2 general medical units with 3,352 patients admitted during QI project time
period. Age 53.3+ (SD 17.8) |
Does a multidisciplinary mobility promotion QI project increase patient mobility and reduce hospital length of stay? | 8-point ordinal Johns Hopkins Highest Level of Mobility
scale. Ambulation in feet |
Changes in scores during and post-QI project. LOS Falls |
| Inouye et al. (1999) | Quasi-experimental design (nonrandom) | General medicine unit N = 852 Mean intervention group age: N = 426; 79.6 +/–6.1 years Mean usual care group age: N = 426; 79.8 +/–6.2 years |
Compared the effectiveness of a multicomponent strategy for reducing the risk
of delirium with that of a usual plan of care for hospitalized
patients. Determined adherence and effect of the intervention protocol. |
- Katz Activities of Daily Living. - Instrumental activities of daily living. |
- Delirium (CAM) rating - Total number of delirium - Level of adherence to intervention - Reasons for nonadherence to intervention. |
| Kram, DiBartolo, Hinderer, and Jones (2015) | EBP Project with descriptive design | 6-bed rural community adult ICU N = 83 Prebundle = 47 Postbundle = 36 Age not reported, but delirium was measured variable |
Does the implementation of the ABCDE bundle care, versus the usual care, reduce incidence of delirium, patient LOS and length of mechanical ventilation, thus decreasing ICU costs? | SAT safety screen Spontaneous breathing trial safety screen 2-min tolerance test Intensive care delirium checklist Early mobility safety screen Mobility exercises |
- Mean ICU LOS - Mean hospital LOS - Mean ventilator days - Average daily census |
| Mah, Staff, Fichandler, and Butler (2013) | Prospective descriptive study: comparing study patients with historical controls |
N = 59 Intervention group + control group Age 66 +/–17 Intervention 62.3 +/–17 Control |
To describe the effects of a team-based, resource-efficient mobility program. | REMP | Functional assessment: 1-7 level (1 = total assistance; 7 = completely independent) |
| Messer, Comer, and Forst (2015) | QI project with correlational descriptive design | 14-bed medical surgical ICU unit. Convenience sample of 41 nurses. Patients: N = 160 Pre-ED = 75 Post-ED = 85 Mean age: 64 |
Evaluated the effect of education for a progressive mobilization program for ICU nurses on knowledge and performance. | Frequency of mobility events (dangling, ambulating,
up-to-chair) Knowledge test scores. |
Pre- and post-educational knowledge and mobilization |
| Schaller et al. (2016) | Multi-center, parallel RCT | 5 university hospital SICU: Austria, Germany, United States
(3) Control: N = 96 (Mean age: 64) Intervention: N = 104 (Mean age: 66) |
Does early, goal-directed mobilization using a strict mobilization algorithm combined with facilitated inter-professional communication, in critically ill SICU patients, lead to improved mobility, decreased LOS and increased functional independence at hospital discharge? | - Patient mobilization capacity measured with the SOMS - mmFIM |
- Mean SOMS level - LOS in the SICU - mmFIM |
| Schweickert et al. (2009) | Multisite RCT | 2 medical centers; Hospitalized mechanically ventilated patients for less than 2 hr. N = 104; Age 57.7 (36-69) Intervention; 54.4 years (46.5-66.4) Control group |
What is the efficacy of combining daily interruption of sedation with physical and occupational therapy on functional outcomes in patients receiving mechanical ventilation? | - Functional status at hospital discharge (6 activities of daily
living) - Walking - # of days of delirium - V# of days alive and breathing without assistance during the first 28 days of hospital stay |
|
| Tousignant-Laflamme et al. (2015) | Descriptive design with qualitative and quantitative data | 20 eligible adults > 65 years treated in emergency department in Canada and assessed to have 1 or more clinical signs of immobilization syndrome | Does implementation of PT services in the ED for the selected population
reduce development of immobilization syndrome? Are interventions feasible and acceptable? |
None measured. | Development of immobilization syndrome, acceptability of the intervention |
| Wood et al. (2014) | QI—Before and after study |
N = 521 Adults on a 32-bed acute care general medical unit (described chronic conditions that fit targeted age group) |
Determined whether an early mobility program would improve patient outcomes. | Mobility Tiers: 1. Tier 1—Nonambulatory 2. Tier 2—Ambulatory Frequency of patient completion of activity session |
LOS Hospital readmission rates Incidence of unit falls Pressure ulcers Utilized a “mobility aide” to assist with patients |
Note. QI = Quality Improvement; MICU = Medical Intensive Care Unit; RCT = Randomized Clinical Trials; ICU = Intensive Care Unit; LOS = length of stay; PT = Physical Therapy; OT = occupational therapy; ADL = Activities of Daily Living; SPHM = safe patient handling and mobility; FIM = functional independent measurement; ED = emergency department; EBP = Evidence-Based Practice; ABCDE = awakening, breathing, coordination, delirium monitoring, and early mobility; CAM = Confusion Assessment Method; SAT = Sedation awakening trial; REMP = Resource-efficient mobility program; SICU = Surgical Intensive Care Unit; SOMS = SICU optimal mobilization score; mmFIM = Mini-modified functional independence measure score.
RCT
Four RCT articles were examined. Bummel et al. (2014) chose a 3 group RCT to examine the feasibility of integrating cognitive therapy with early PT as part of a mobility program. Patients were recruited from both Medical and Surgical ICUs and divided into three groups: usual care (n = 22), PT/OT only (n = 22), cognitive therapy with early PT/OT (n = 43). Their demonstration study established feasibility and safety of combining cognitive therapy with early PT/OT mobility. Limited sample size revealed insufficient power to detect any clinically meaningful changes in 3-month follow-up evaluations or to be able to draw generalizable conclusions.
Brown, Foley, and Lowman (2016) used a single blind randomized control approach to examine the outcomes of an interdisciplinary mobility program with a behavioral approach on post-hospitalization function and community mobility. In this study, 100 patients aged 65 and older were randomly assigned to the control group or the study group. Mobility program participants were ambulated up to twice daily, and a behavioral strategy was implemented to encourage activity. Control group participants were ambulated twice daily with no behavioral encouragement. Changes in ADLs were self-reported using the University of Alabama at Birmingham Study of Aging Life-Space Assessment (LSA). At 1-month post-hospitalization, LSA scores were significantly higher in the treatment group, indicating higher levels of ADLs. Study findings show that mobility programs with a behavioral component may increase ADL levels post-hospitalization. A predominantly male, veteran population was a limitation.
Schaller et al. (2016) incorporated a three country, five university hospital, assessor-blinded, randomized control trial (two groups stratified by Glasgow Coma Scale [GCS] scores ⩽8 or >8) to test if early mobilization contributes to improved mobility, decreased ICU LOS, and increased functional status at time of hospital discharge. This double-blinded study included measurements for GCS; Acute Physiology and Chronic Health Evaluation (APACHE II); sedation and awakening trials; spontaneous breathing trials; screening for arousal, delirium, and pain; and early enteral feedings. In addition, patient physiologic data, LOS on SICU, hospital LOS, in-hospital mortality, 3-month mortality, and discharge disposition were also measured. The control group received standard of care practice for mobilization and PT. The two-part intervention included a mobilization goal (as identified on early morning rounds) and goal implementation for all shifts by interprofessional closed-loop communication. A facilitator worked with the interprofessional clinical team each day to determine mobility goals. Complete mobility independence was reported in 59% of the intervention group, compared with 35% of the control group at the time of hospital discharge. The overall findings noted a statistically significant improvement in functional status in patients enrolled in the intervention group (p = .009), with shorter time in the SICU, 5 days compared with 7 days for control group, 95% confidence interval (CI) = [–4, –1], p = .0006, and a more desirable discharge position to home (p = .0007). Mortality before hospital discharge and 3 months after hospital discharge did not differ significantly between the two groups (p = .09 and .35, respectively). Limitations include the physicians not being blinded to patient group assignment, inability to generalize to other non-ICU settings, and differing standard of care protocols for the control group based on the hospital site.
Schweickert et al. (2009) focused on critically ill ICU patients who were sedated to ask if PT/OT after sedation interruption would improve functional outcomes. Functional status was defined as the ability to perform six activities of daily living and to be able to walk independently. Using an RCT design, the intervention group was more likely to return to functional status compared with the control group, p = .02; odds ratio (OR) = 2.7; 95% CI = [1.2, 6.1], had shorter duration of sedation (mean 2.0 days vs. 4.0 days, p = .02), and more ventilator-free days (23.5 days vs. 21.1 days, p = .05).
Quasi-experimental (Nonrandomized)
Inouye et al. (1999) determined that a prospective, controlled clinical trial using one intervention and two usual-care (control) units at a hospital without random assignment of participants was the best design given clinical limitations of available beds for the chosen units. As an alternative to randomization, they chose an individual matching strategy for baseline comparability of relevant risk factors for delirium: cognitive impairment, sleep deprivation, immobility, visual impairment, hearing impairment, and dehydration. The aim of their study was to compare the effectiveness of a multicomponent strategy, the Elder Life Program, for reducing the risk of delirium, which includes early mobilization three times a day. This program trained an interdisciplinary team comprised of a geriatric-specialist nurse, 2 specially trained Elder Life specialists, a certified therapeutic-recreation specialist, a PT consultant, a geriatrician, and trained volunteers (not specified). The control group received usual care by physicians, nurses, and support staff (e.g., PT, pharmacists, and nutritionists). Outcome measures for reassessment were change in orientation score, change in rate of sedative drug use for sleep, change in ADL score, early correction of vision, change in Whisper test, and change in ratio of blood urea nitrogen to creatinine. The results of the study indicated that the intervention group experienced less episodes of delirium, had higher ADL scores, and trended higher on the Whisper test. Costs per patient for this program were US$327 per intervention-group patient versus US$6,341 per case of delirium (control, usual care group). The binary outcome of interest was delirium, with mobility as one of six measured variables. Limitations of the study were nonrandomization of patients, possible contamination effect between the two groups, Hawthorne effect, and cross-over between providers caring for patients in both groups.
Prospective, observational cohort studies
Mah, Staff, Fichandler, and Butler (2013) conducted a prospective descriptive study with a sample of 59 participants, with 28 in the intervention and 31 in the historical control group to determine the effectiveness of a team-based, resource-efficient mobility program (REMP) to improve the mobility of hospitalized patients. In addition, the effectiveness of the REMP program to improve the unit-based processes to promote mobility was examined. Prospective and retrospective chart audits were done. This program consisted of regular functional assessments, and safe physical activity. The REMP team members include the bedside nurse, respiratory and physical therapists, and a PT aide. A functional assessment was performed by the REMP physical therapist within 48 hr of admission. Daily rounds were conducted with the REMP team, and mobility recommendations were discussed during multidisciplinary team meetings. Both intervention and control group improved in function. However, more REMP patients had significantly improved sitting balance at discharge compared with the control group (75% vs. 36.7%, p < .008). Study limitations included a small sample size (n = 59), and the use of medications not quantified for comparison in the control group.
Retrospective cohort study
Darragh, Shiyko, Margulis, and Campo (2014) examined 1,292 patients’ electronic medical records (EMR) to compare those receiving the intervention (safe patient handling and mobility [SPHM]) to those who did not (no-SPHM group). It was determined that patients who received inpatient rehabilitation services achieved modified independence in self-care compared with those without safe patient handling and mobility program services. Outcome measures were analyzed for age, LOS, diagnostic codes, and mobility. Using the Functional Independent Measurement (FIM) with interrater and test-retest reliability = .95 and internal consistency = .88-.97 categories, a mobility subscale was used that defined mobility as the total of two locomotion (walk/wheelchair and stairs) and three transfer items (bed/chair/wheelchair, toilet, and tub/shower). Comparing both groups, there was a statistically significant difference in self-care FIM at admission, No-SPHM = 23.95 (6.55); SPHM = 25.76 (6.19), p < .001, and LOS was nearly 2 days shorter for the intervention (SPHM) group (p < .007). There was no difference in mobility scores at admission or self-care FIM at discharge, which the authors recognize has both statistical implications as well as study limitations in the use of the FIM as their main outcome measure. The FIM is sensitive to inconsistent or inaccurate scoring and may not represent a patient’s true performance ability.
Descriptive, mixed methods
Tousignant-Laflamme et al. (2015) explored the feasibility (qualitative component) of adding PT services to an Emergency Department (ED). Their research question evaluates the potential clinical value of using PT services along with nursing staff as a mechanism of preventing immobilization syndrome (IS) in older adults with at least one sign of impaired mobility. Nurses identified eligible patients and PT made rounds in the ED 2 to 3 times a day during normal business hours to develop individualized intervention plans as the patient was being treated for primary visit. Between 30 and 40 min was provided for each eligible patient. If the patient was admitted to the hospital, they received an additional 1 to 2 visits depending on the length of their stay. Chart reviews were analyzed for barriers and facilitators using content analysis. Feasibility of the program was measured by access to patients, percentage of patients who met eligibility criteria, and acceptability of the interventions. ED personnel (nurses, physicians, and PT staff) were further interviewed to determine facilitators and barriers. With the small sample size (n = 20), of those who received the ED intervention and were admitted to the hospital, none of the patients developed IS. Two patients developed IS during their hospital stay but had not received the ED intervention. The authors determined that there is feasibility for an ED intervention to prevent IS, but only 11% of the ED eligibility patients would qualify for those services.
QI/EBP/clinical demonstration projects
Using a prospective consecutive case series design, Azuh et al. (2016) developed a 5-point mobility scale and created a mobility team that focused on skin-care prevention, and mobility. The team was comprised of nurses, rehabilitation specialists (PT/OT), and a patient mobility assistant. Data compared with 2 years earlier of 3,233 patients enrolled from the MICU noted a significant decrease from 9.2% to 6.2% in hospital-acquired pressure ulcers (p = .0405), hospital readmissions were significantly decreased from 17.1% to 11.5% (p = .0010), mean MICU LOS decreased from 11.7 to 10.7 days (not statistically significant, but has clinical implications in costs to patient and hospital) while ventilator-associated pneumonia rates did not decrease. Hospital readmissions also decreased by 33% for those who participated in the mobility program. From a qualitative perspective, 97% of the patients were satisfied with the mobility program and their interactions with the mobility team. The authors demonstrated that their mobility program was more cost-effective than the standard hospital PT model. While mobility levels were recorded and interventions designed for each level, mobility was not quantified by the number of steps, distance covered, or amount of time walking independently.
Hoyer et al. (2016) used SQUIRE guidelines for their prospective QI project to promote early mobility in the ICU setting. Their goal was to mobilize patients 3 times a day, quantify and document patient’s mobility, increase mobility through daily goal-setting, and standardize descriptions of patient mobility. Their multidisciplinary approach involved stakeholders comprised of nurses, physicians, rehabilitation therapists, and administrators. Results of their study revealed shorter LOS during the intervention period compared with the time period before implementation (3 vs. 4 days, p ≤ .001). The percent of patients who were ambulated increased from 60% to 78% (p = .001), and the percent of patients who improved in their mobility scores also increased significantly from 26% to 48% (p < .001).
Using formative and summative program evaluation, Kram, DiBartolo, Hinderer, and Jones (2015) described the ABCDE (awakening, breathing, coordination, delirium monitoring, and early mobility) bundle as an evidence-based, multidisciplinary method for decreasing hospital LOS, decreasing duration of mechanical ventilation, decreasing delirium prevalence, and decreasing healthcare costs. The authors examined the feasibility of implementing the ABCDE bundle in three rural hospital, general adult ICU settings. RNs performed an early mobility safety screening on all patients daily after multiple educational sessions were conducted for nursing, respiratory therapy, and rehabilitation staff. Post-bundle ICU and hospital LOS were decreased overall. Costs to the hospital were quantified based on a decrease in 1.8 days with a potential savings of US$2,156 per patient and US$700 per patient per ventilator-free days. Statistical significance was not noted in the ventilator-free days, but clinical significance has broader implications for patients, acuity levels, and daily costs to patient and hospital. Early mobility measurement was not described.
Messer, Comer, and Forst (2015) explored the introduction of an educational intervention for nurses where the ABCDE bundle mobility protocol was to be implemented in a medical-surgical unit that did not have a culture of early mobilization of patients. While the targeted population under study was nurses (n = 41), chart reviews were conducted 3 weeks before and 3 weeks after the educational intervention to note behavioral practice changes. Before the educational intervention, few patients (n = 75) were ambulated (8%), none were dangled with the majority documented as assisted up to a chair (36%). Post-educational intervention, there was an increase in overall mobility (p = .04) with more documented dangling (13%, p = .01), less ambulating (6%, p = .34), and more up to chair (45%, p = .20) events recorded. While nurses’ knowledge was significantly increased based on pre- and posttest scores, this did not translate to a change in the culture of the unit due to perceptions of time constraints and lack of experience in mobilization. A year after the study, additional staff were hired and trained to fill the role of mobility technicians.
Wood et al. (2014) evaluated a mobility program using a QI process that used a certified nurse assistant (CNA) as a mobility aide to promote mobility in hospitalized older adults. The primary role of the mobility aide included reviewing mobility orders, assisting and supervising 3 activity sessions daily, and meeting with physical therapists to discuss patient progress and needs. A total of 521 patients participated in the program. On average, patients participated in 1.74 (SD 0.34) activity sessions daily. Of all patients that participated, 87.7% participated in 2 daily sessions. Outcomes of this program included a decrease in the number of patient falls, pressure ulcers, and 30-day readmissions. After initiation of the mobility protocol, the average unit fall rate was reduced from 4.33 to 3.33. Mean readmission rates decreased from 19.7% to 17.3%. The large heterogeneous sample was a strength of this study. Limitations included the study design as a QI project, and compromised intervention fidelity related to lack of consistent, daily mobility aide presence.
Hastings et al. (2014) implemented a supervised walking program for older hospitalized veterans (STRIDE) to optimize physical function (Hastings et al., 2014). This QI project compared the STRIDE program with usual care. The STRIDE program consists of (a) physical therapist assessment within 24 hr of admission, (b) supervised ambulation for safety and completion of program activities, (c) patient education regarding the importance of ambulation, and (d) verbal motivation and encouragement. A total of 92 participants was included in the study, with 35 in the control group. The goal for participants was to engage in at least 20 min of supervised walking daily. STRIDE therapists followed established mobility protocols, offered rest breaks, monitored vital signs of the participants, and worked closely with the primary nurse to determine the best time for ambulation. Overall, 92% of STRIDE participants were able to be discharged home rather than to a skilled nursing facility compared with 74% of patients in the control group. Median length of stay of the participants was 4.7 days versus 5.7 days for the control group. Readmission rates and 30-day emergency room visits were not significantly different between the two groups (Hastings et al., 2014)
Discussion
The aim of this scoping review was to summarize hospital-based programs to improve mobility in hospitalized adults, and determine the methods used to measure physical mobility. These themes were deemed as relevant for this article and as noted by Crane (2017), one barrier noted by nurses in implementing physical mobility protocols or programs is the unavailability of PT staff once an initial assessment was performed.
The findings of this scoping review indicated that nurses, physicians, and therapists have all been engaged in programs designed to improve mobility (Fisher et al., 2016; King et al., 2016; Pashikanti & Von Ah, 2012; Pedersen et al., 2013; Zisberg & Syn-Hershko, 2016). Key findings from the mobility studies conclude that multidisciplinary team-based mobility programs/protocols and algorithms with behavioral change approaches were effective in improving the occurrence and distance ambulated (Drolet et al., 2013; King et al., 2016; Klein et al., 2015; Padula et al., 2009). Inherent in the many mobility programs is the involvement of bedside nurses. For example, bedside nurses were able to question bed-rest orders as part of a mobility program (King et al., 2016). Klein et al. (2015) found that a Clinical Nurse Specialist advocated for the mobility needs of patients and that bedside nurses are in a key position to coordinate team-based patient care so that mobility is promoted.
A weak study design is one of the major shortcomings of many of the studies. In the nurse-driven mobility and PT-driven studies, there was only one randomized controlled trial found through the literature search for each discipline (Raymond et al., 2017; Teodoro et al., 2016). There were 4 RCTs within the multidisciplinary-driven studies. One could argue that with so many programs all pointing to a similar end, having a randomized controlled design to study the improvement of mobility in hospitalized older adults is challenging and may not be essential to demonstrating that early mobility is effective, but that mobility programs need to be integrated into all patient aspects of care with consistent measurements established for quantity and quality of mobility efforts.
Another weakness is the limited use of more accurate ways of measuring ambulation. Only one nurse-driven study used pedometers and step counts (Teodoro et al., 2016), in contrast with the other nurse-driven studies that used chart audits to measure the timeliness, frequency, and distance of mobility (Dickinson et al., 2013; Drolet et al., 2013; King et al., 2016; Klein et al., 2015; Padula et al., 2009). Using accelerometer technology could provide a more robust measurement of the distance, frequency, and timeliness of ambulation, which may also aid in comparative analysis across studies to determine the effectiveness of mobility programs and their components. Underutilization of objective methods to measure physical activity could be due to high costs of accelerometers, differing reliability and validity, challenges with placing accelerometers on the older patient, and loss of devices. Surprisingly, only one of the PT-driven mobility program studies used accelerometer technology to measure step counts in the study participants. None of the multidisciplinary-driven studies utilized or measured mobility using accelerometers, but, instead, focused on a variety of scales or measured activities and outcome measures. Reliable and objective measurement tools should be included in future study protocols.
With the rise in the number of older adults who will be hospitalized in the future, increasing PT/OT frequency per patient may not be sustainable, or cost-effective. Another concern in PT-driven mobility programs is that nurses may willingly or by necessity relinquish ownership of the promotion of mobility, instead of collaborating with PT/OT who can provide expert guidance. In the nurse-driven mobility study by King et al. (2016), nursing staff behaviors and their perceptions shifted during the nurse-driven mobility program giving nurses a feeling of ownership for the promotion of mobility and feeling supported to promote mobility, which in turn improved the ambulation and a variety of other patient outcomes (King et al., 2016). A strength of the PT-led mobility studies was that findings corroborated the promotion of mobility as a priority that requires time and care coordination.
The relationship between mobility programs and increased mobility, and the improvement of functional outcomes of patients was a key focus of the multidisciplinary-driven mobility program studies (Azuh et al., 2016; Brown et al., 2016; Darragh et al., 2014; Inouye et al., 1999; Mah et al., 2013; Messer et al., 2015; Schaller et al., 2016; Schweickert et al., 2009). Furthermore, the effect of increased mobility on falls and other adverse health outcomes was a secondary focus (Brown et al., 2016; Hoyer et al., 2016; Leditschke et al., 2012; Tousignant-Laflamme et al., 2015; Wood et al., 2014). Similarly, several nurse-led, PT-led, and multidisciplinary-led studies all considered the impact of mobilization on healthcare utilization (Azuh et al., 2016; Darragh et al., 2014; Kram et al., 2015; Schaller et al., 2016; Wood et al., 2014). Multidisciplinary collaboration necessary to promote mobility was also examined across disciplines, including staff knowledge and attitudes toward mobilization, and potential staff barriers (Azuh et al., 2016; Messer et al., 2015).
One important theme throughout the literature is that effectively promoting regular mobility in hospitalized older adults is a team effort that requires collaboration among disciplines, and a structured, organized, and purposeful approach. Multidisciplinary mobility programs used various processes and algorithms as a way to promote early and regular mobility by delineating the specific roles of nurses, physical therapists, and physicians in the promotion of mobility. Notably, a standard geriatric-specific guideline for promoting mobility was not utilized in the reviewed literature, which could explain the wide variations across studies making synthesis of the findings challenging. However, the literature does show that the implementation of protocols designed to improve the early and regular implementation of physical mobility activities were shown to improve the health outcomes of hospitalized older people, and to have a positive impact on reducing costs associated with healthcare utilization, including hospital LOS. Yet, less is known about which specific multidisciplinary components are responsible for the achievement of these positive patient outcomes. While more inquiry is needed, mobility protocols may provide clear guidance to nurses on the type, frequency, and amount of mobility patients should receive during hospitalization (de Morton et al., 2007). Also, the presence of a mobility program may foster interdisciplinary communication and bring role clarification to the interacting disciplines (King et al., 2016). Mobility programs with a specific role-delineated protocol may give nurses “permission” to question bed-rest orders and take steps to provide mobility activities to the patient (Drolet et al., 2013; Padula et al., 2009; Pashikanti & Von Ah, 2012).
Conclusion
Maintaining physical function during hospitalization is known to prevent functional decline and frailty. A standardized mobility program using multiple disciplines and accurate monitoring and documentation of patient activity could be one way for hospitals to combat the adverse effects that can be present with decreased mobility in the older adult population. There is a paucity of research in the area of mobility programs that use objective methods to measure physical activity, with notable concerns in limited use of accurate and objective measurement tools including accelerometers, the presence of discrepancies in distance measurements, and inaccurate patient self-assessments. For future research, nurses have a unique opportunity to impact this phenomenon by conducting randomized controlled trials with robust sample sizes to demonstrate the impact of nurse-led multidisciplinary programs to improve mobility. Last, the use of hospital-based sustainable interventions to improve physical activity that incorporate accelerometer technology is a significant next step for future research.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Denise A Smart  https://orcid.org/0000-0003-4644-2982
https://orcid.org/0000-0003-4644-2982
References
- Administration on Aging. (2012). Bureau report, 2012. Available from http://www.aoa.gov
- Afilalo J. (2011). Frailty in patients with cardiovascular disease: Why, when, and how to measure. Current Cardiovascular Risk Reports, 5, 467-472. doi: 10.1007/s12170-011-0186-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amidei C. (2012). Mobilisation in critical care: A concept analysis. Intensive and Critical Care Nursing, 28, 73-81. doi: 10.1016/j.iccn.2011.12.006 [DOI] [PubMed] [Google Scholar]
- Arksey H., O’Malley L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8, 19-32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Ash M., Kelly E., Mercier T., Davis G., Renault M.-H., Daley P., . . . Webb-Anderson K. (2016). I.C.U. M.O.V.E.S: Intensive care unit mobility, optimizing a very early start…dynamics of critical care 2016 in Charlottetown, PE, September 25-27, 2016. Canadian Journal of Critical Care Nursing, 27(2), 14-14. [Google Scholar]
- Azuh O., Gammon H., Burmeister C., Frega D., Nerenz D., DiGiovine B., Siddiqui A. (2016). Benefits of early active mobility in the medical intensive care unit: A pilot study. The American Journal of Medicine, 129, 866-871.e1. doi: 10.1016/j.amjmed.2016.03.032 [DOI] [PubMed] [Google Scholar]
- Boltz M., Capezuti E., Shabbat N., Hall K. (2010). Going home better not worse: Older adults’ views on physical function during hospitalization. International Journal of Nursing Practice, 16, 381-388. doi: 10.1111/j.1440-172X.2010.01855.x [DOI] [PubMed] [Google Scholar]
- Brown C. J., Foley K. T., Lowman J. D., Jr., MacLennan P. A., Razjouyan J., Najafi B., . . . Allman R. M. (2016). Comparison of posthospitalization function and community mobility in hospital mobility program and usual care patients: A randomized clinical trial. JAMA Internal Medicine, 176, 921-927. doi: 10.1001/jamainternmed.2016.1870 [DOI] [PubMed] [Google Scholar]
- Brown C. J., Friedkin R. J., Inouye S. K. (2004). Prevalence and outcomes of low mobility in hospitalized older patients. Journal of the American Geriatrics Society, 52, 1263-1270. doi: 10.1111/j.1532-5415.2004.52354.x [DOI] [PubMed] [Google Scholar]
- Brown C. J., Redden D. T., Flood K. L., Allman R. M. (2009). The underrecognized epidemic of low mobility during hospitalization of older adults. Journal of the American Geriatrics Society, 57, 1660-1665. doi: 10.1111/j.1532-5415.2009.02393.x [DOI] [PubMed] [Google Scholar]
- Brown C. J., Roth D. L., Allman R. M. (2008). Validation of use of wireless monitors to measure levels of mobility during hospitalization. Journal of Rehabilitation Research & Development, 45, 551-558. doi: 10.1682/jjrd.2007.06.0086 [DOI] [PubMed] [Google Scholar]
- Brown C. J., Roth D. L., Allman R. M., Sawyer P., Ritchie C. S., Roseman J. M. (2009). Trajectories of life-space mobility after hospitalization. Annals of Internal Medicine, 150, 372-378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bummel N. E., Girard T. D., Ely E. W., Pahdharipande P. P., Morandi A., Hughes C. G., . . . Jackson J. C. (2014). Feasibility and safety of early combined cognitive and physical therapy for critically ill medical and surgical patients: The Activity and Cognitive Therapy in ICU (ACT-ICU) trial. Intensive Care Medicine, 40, 370-379. doi: 10.1007/s00134-013-3136-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catchpole K. (2013). Spreading human factors expertise in healthcare: Untangling the knots in people and systems. BMJ Quality & Safety, 22, 793-797. doi: 10.1136/bmjqs-2013-002036 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2015) Retrieved october 11, 2018 from: https://www.cdc.gov/cdi/definitions/older-adults.html
- Crane A. (2017). Implementing an early mobility protocol for patients in the intensive care unit (Doctoral dissertation, Brandman University, Irvine, CA). Available from ProQuest. (1025544) [Google Scholar]
- Cruz-Jentoft A. J., Baeyens J. P., Bauer J. M., Boirie Y., Cederholm T., Landi F., . . . Zamboni M. (2010). Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age and Ageing, 39, 412-423. doi: 10.1093/ageing/afq034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darragh A. R., Shiyko M., Margulis H., Campo M. (2014). Effects of a safe patient handling and mobility program on patient self-care outcomes. The American Journal of Occupational Therapy, 68, 589-596. doi: 10.5014/ajot.2014.011205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Morton N. A., Keating J. L., Jeffs K. (2007). Exercise for acutely hospitalised older medical patients. Cochrane Database of Systematic Reviews, 1, CD005955. doi: 10.1002/14651858.CD005955.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickinson S., Tschannen D., Shever L. L. (2013). Can the use of an early mobility program reduce the incidence of pressure ulcers in a surgical critical care unit? Critical Care Nursing Quarterly, 36, 127-140. doi: 10.1097/CNQ.0b013e31827538a1 [DOI] [PubMed] [Google Scholar]
- Doenges M. E., Moorhouse M. F., Murr A. C. (2014). Nursing care plans: Guidelines for individualizing client care across the life span (9th ed.). Philadelphia, PA: F.A. Davis. [Google Scholar]
- Drolet A., DeJuilio P., Harkless S., Henricks S., Kamin E., Leddy E. A., . . . Williams S. (2013). Move to improve: The feasibility of using an early mobility protocol to increase ambulation in the intensive and intermediate care settings. Physical Therapy, 93, 197-207. doi: 10.2522/ptj.20110400 [DOI] [PubMed] [Google Scholar]
- Ebright P. R., Patterson E. S., Chalko B. A., Render M. L. (2003). Understanding the complexity of registered nurse work in acute care settings. Journal of Nursing Administration, 33, 630-638. [DOI] [PubMed] [Google Scholar]
- Engel H. J., Needham D. M., Morris P. E., Gropper M. A. (2013). ICU early mobilization: From recommendation to implementation at three medical centers. Critical Care Medicine, 41, S69-S80. doi: 10.1097/CCM.0b013e3182a240d5 [DOI] [PubMed] [Google Scholar]
- Engel H. J., Tatebe S., Alonzo P. B., Mustille R. L., Rivera M. J. (2013). Physical therapist–established intensive care unit early mobilization program: Quality improvement project for critical care at the University of California San Francisco Medical Center. Physical Therapy, 93, 975-985. [DOI] [PubMed] [Google Scholar]
- Fisher S. R., Graham J. E., Ottenbacher K. J., Deer R., Ostir G. V. (2016). Inpatient walking activity to predict readmission in older adults. Archives of Physical Medicine and Rehabilitation, 97(9 Suppl), S226-S231. doi: 10.1016/j.apmr.2015.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greysen S. R. (2016). Activating hospitalized older patients to confront the epidemic of low mobility. JAMA Internal Medicine, 176, 928-929. doi: 10.1001/jamainternmed.2016.1874 [DOI] [PubMed] [Google Scholar]
- Guyatt G., Rennie D., Meade M. O., Cook D. J. (2015). Users’ guide to the medical literature: A manual for evidence-based clinical practice (3rd ed.). Quincy, IL: McGraw-Hill Education. [Google Scholar]
- Hastings S. N., Sloane R., Morey M. C., Pavon J. M., Hoenig H. (2014). Assisted early mobility for hospitalized older veterans: Preliminary data from the STRIDE program. Journal of the American Geriatrics Society, 62, 2180-2184. doi: 10.1111/jgs.13095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyer E. H., Brotman D. J., Chan K. S., Needham D. M. (2015). Barriers to early mobility of hospitalized general medicine patients: Survey development and results. American Journal of Physical Medicine & Rehabilitation, 94, 304-312. doi: 10.1097/phm.0000000000000185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyer E. H., Friedman M., Lavezza A., Wagner-Kosmakos K., Lewis-Cherry R., Skolnik J. L., . . . Needham D. M. (2016). Promoting mobility and reducing length of stay in hospitalized general medicine patients: A quality-improvement project. Journal of Hospital Medicine, 11, 341-347. doi: 10.1002/jhm.2546 [DOI] [PubMed] [Google Scholar]
- Inouye S. K., Bogardus S. T., Jr., Charpentier P. A., Leo-Summers L., Acampora D., . . . Cooney L. M., Jr. (1999). A multicomponent intervention to prevent delirium in hospitalized older patients. The New England Journal of Medicine, 340, 669-676. doi: 10.1056/nejm199903043400901 [DOI] [PubMed] [Google Scholar]
- King B. J., Steege L. M., Winsor K., VanDenbergh S., Brown C. J. (2016). Getting patients walking: A pilot study of mobilizing older adult patients via a nurse-driven intervention. Journal of the American Geriatrics Society, 64, 2088-2094. doi: 10.1111/jgs.14364 [DOI] [PubMed] [Google Scholar]
- Klein K., Mulkey M., Bena J. F., Albert N. M. (2015). Clinical and psychological effects of early mobilization in patients treated in a neurologic ICU: A comparative study. Critical Care Medicine, 43, 865-873. doi: 10.1097/ccm.0000000000000787 [DOI] [PubMed] [Google Scholar]
- Kosse N. M., Dutmer A. L., Dasenbrock L., Bauer J. M., Lamoth C. J. (2013). Effectiveness and feasibility of early physical rehabilitation programs for geriatric hospitalized patients: A systematic review. BMC Geriatrics, 13, Article 107. doi: 10.1186/1471-2318-13-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kram S. L., DiBartolo M. C., Hinderer K., Jones R. A. (2015). Implementation of the ABCDE bundle to improve patient outcomes in the intensive care unit in a rural community hospital. Dimensions of Critical Care Nursing, 34, 250-258. doi: 10.1097/dcc.0000000000000129 [DOI] [PubMed] [Google Scholar]
- Leditschke I. A., Green M., Irvine J., Bissett B., Mitchell I. A. (2012). What are the barriers to mobilizing intensive care patients? Cardiopulmonary Physical Therapy Journal, 23(1), 26-9. [PMC free article] [PubMed] [Google Scholar]
- Lehman C. A. (2009). Practical issues in conducting hospital-based research. Perioperative Nursing Clinics, 4, 269-276. [Google Scholar]
- Levac D., Colquhoun H., O’Brien K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5, Article 69. doi: 10.1186/1748-5908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mah J. W., Staff I., Fichandler D., Butler K. L. (2013). Resource-efficient mobilization programs in the intensive care unit: Who stands to win? The American Journal of Surgery, 206, 488-493. doi: 10.1016/j.amjsurg.2013.03.001 [DOI] [PubMed] [Google Scholar]
- Malhotra R., Chan A., Alay S., Ma S., Saito Y. (2016). Variation in the gender gap in inactive and active life expectancy by the definition of inactivity among older adults. Journal of Aging & Health, 28(7), 1279-98. [DOI] [PubMed] [Google Scholar]
- Messer A., Comer L., Forst S. (2015). Implementation of a progressive mobilization program in a medical-surgical intensive care unit. Critical Care Nurse, 35(5), 28-42. doi: 10.4037/ccn2015469 [DOI] [PubMed] [Google Scholar]
- Morris M., Boruff J., Gore G. (2016). Scoping reviews: Establishing the role of the librarian. Journal of the Medical Library Association, 104, 346-354. doi: 10.3163/1536-5050.104.4.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orkaby A. R., Lunetta K. L., Sun F. J., Driver J. A., Benjamin E. J., Hamburg N. M., … Murabito J. M. (2018). Cross-sectional association of frailty and arterial stiffness in community-dwelling older adults: The Framingham Heart Study. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. Advance online publication. doi: 10.1093/Gerona/gly134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padula C. A., Hughes C., Baumhover L. (2009). Impact of a nurse-driven mobility protocol on functional decline in hospitalized older adults. Journal of Nursing Care Quality, 24, 325-331. doi: 10.1097/NCQ.0b013e3181a4f79b [DOI] [PubMed] [Google Scholar]
- Pashikanti L., Von Ah D. (2012). Impact of early mobilization protocol on the medical-surgical inpatient population: An integrated review of literature. Clinical Nurse Specialist, 26, 87-94. doi: 10.1097/NUR.0b013e31824590e6 [DOI] [PubMed] [Google Scholar]
- Pedersen M. M., Bodilsen A. C., Petersen J., Beyer N., Andersen O., Lawson-Smith L., . . . Bandholm T. (2013). Twenty-four-hour mobility during acute hospitalization in older medical patients. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 68, 331-337. doi: 10.1093/gerona/gls165 [DOI] [PubMed] [Google Scholar]
- Petry N. M. (2002). A comparison of young, middle-aged, and older adult treatment-seeking pathological gamblers. The Gerontologist, 42, 92-99. [DOI] [PubMed] [Google Scholar]
- Raymond M. J., Jeffs K. J., Winter A., Soh S. E., Hunter P., Holland A. E. (2017). The effects of a high-intensity functional exercise group on clinical outcomes in hospitalised older adults: An assessor-blinded, randomised-controlled trial. Age and Ageing, 46, 208-213. doi: 10.1093/ageing/afw215 [DOI] [PubMed] [Google Scholar]
- Rodondi A., Chevallet T., Rizzoli R. (2012). Prevalence of vertebral fracture in oldest old nursing home residents. Osteoporosis International, 23(11), 2601-2606. doi: 10.1007/s00198-102-1900-6 [DOI] [PubMed] [Google Scholar]
- Schaller S. J., Anstey M., Blobner M., Edrich T., Grabitz S. D., Gradwohl-Matis I., . . . Eikermann M. (2016). Early, goal-directed mobilisation in the surgical intensive care unit: A randomised controlled trial. The Lancet, 388, 1377-1388. doi: 10.1016/s0140-6736(16)31637-3 [DOI] [PubMed] [Google Scholar]
- Schweickert W. D., Pohlman M. C., Pohlman A. S., Nigos C., Pawlik A. J., Esbrook C. L., . . . Kress J. P. (2009). Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. The Lancet, 373, 1874-1882. doi: 10.1016/s0140-6736(09)60658-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- TEAM Study Investigators. (2015). Early mobilization and recovery in mechanically ventilated patients in the ICU: A bi-national, multi-centre, prospective cohort study. Critical Care, 19(1), Article 81. doi: 10.1186/s13054-015-0765-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teodoro C. R., Breault K., Garvey C., Klick C., O’Brien J., Purdue T., . . . Matney L. (2016). STEP-UP: Study of the effectiveness of a patient ambulation protocol. MEDSURG Nursing, 25, 111-116. [PubMed] [Google Scholar]
- The Joanna Briggs Institute (2015). The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. Retrieved October 19, 2017 from: http://joannabriggs.org/assets/docs/sumari/Reviewers-Manual_Methodology-for-JBI-Scoping-Reviews_2015_v2.pdf
- Theou O., Tan E. C., Bell J. S., Emery T., Robson L., Morley J. E., . . . Visvanathan R. (2016). Frailty levels in residential aged care facilities measured using the frailty index and FRAIL-NH Scale. Journal of the American Geriatrics Society, 64, e207-e212. doi: 10.1111/jgs.14490 [DOI] [PubMed] [Google Scholar]
- Tousignant-Laflamme Y., Beaudoin A.-M., Renaud A.-M., Lauzon S., Charest-Bossé M.-C., Leblanc L., Grégoire M. (2015). Adding physical therapy services in the emergency department to prevent immobilization syndrome—A feasibility study in a university hospital. BMC Emergency Medicine, 15, Article 35. doi: 10.1186/s12873-015-0062-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations (2015). World Population Aging. Retrieved October 11, 2018 from: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf
- Vaughn S., Mauk K. L., Jacelon C. S., Larsen P. D., Rye J., Wintersquill W., … Dufresne D. (2016). The competency model for professional rehabilitation nursing. Rehabilitation Nursing, 41(1), 33-44. doi: 10.1002/rnj.225 [DOI] [PubMed] [Google Scholar]
- Weiss A. J., Elixhauser A. (2014, October). Overview of hospital stays in the United States, 2012 (Healthcare Cost and Utilization Project [HCUP] Statistical Briefs, Statistical Brief #180). Rockville, MD: Agency for Healthcare Research and Quality; Retrieved from http://www.hcup-us.ahrq.gov/reports/statbriefs/sb180-Hospitalizations-United-States-2012.pdf [Google Scholar]
- Weiss A. J., Elixhauser A., Andrews R. M. (2006). Characteristics of operating room procedures in U.S. hospitals, 2011 (Healthcare Cost and Utilization Project [HCUP] Statistical Briefs, Statistical Brief #170). Rockville, MD: Agency for Healthcare Research and Quality. [PubMed] [Google Scholar]
- Wood W., Tschannen D., Trotsky A., Grunawalt J., Adams D., Chang R., . . . Diccion-MacDonald S. (2014). A mobility program for an inpatient acute care medical unit. American Journal of Nursing, 114(10), 34-40; quiz 41-42. doi: 10.1097/01.NAJ.0000454850.14395.eb [DOI] [PubMed] [Google Scholar]
- World Health Organization report [WHO] (1999). Men Ageing and Health: Achieving health across the lifespan. 01WHO/NMH/NPH01.2. Retrieved October 11, 2018 from: http://apps.who.int/iris/bitstream/handle/10665/66941/WHO_NMH_NPH_01.2.pdf;jsessionid=13F96CBEED23EF1A1DF3BD2686BD06AB?sequence=1
- World Health Organization [WHO] (2002). Health Statistics & Information Systems: Proposed working definition of an older person in Africa for the MDS project. Retrieved October 11, 2018 from: http://www.who.int/healthinfo/survey/ageingdefnolder/en/
- Zisberg A., Shadmi E., Gur-yaish N., Tonkikh O., Sinoff G. (2015). Hospital-associated functional decline: The role of hospitalization processes beyond individual risk factors. Journal of the American Geriatrics Society, 63, 55-62. doi: 10.1111/jgs.13193 [DOI] [PubMed] [Google Scholar]
- Zisberg A., Shadmi E., Sinoff G., Gur-yaish N., Srulovici E., Admi H. (2011). Low mobility during hospitalization and functional decline in older adults. Journal of the American Geriatrics Society, 59, 266-273. doi: 10.1111/j.1532-5415.2010.03276.x [DOI] [PubMed] [Google Scholar]
- Zisberg A., Syn-Hershko A. (2016). Factors related to the mobility of hospitalized older adults: A prospective cohort study. Geriatric Nursing, 37, 96-100. doi: 10.1016/j.gerinurse.2015.1012 [DOI] [PubMed] [Google Scholar]