Abstract
Objectives. To determine the association between poison center opioid exposure calls and National Vital Statistics System (NVSS) deaths.
Methods. We categorized Centers for Disease Control and Prevention NVSS mortality and the Researched Abuse, Diversion and Addiction-Related Surveillance System poison center program cases from 2006 to 2016 by International Classification of Diseases, Tenth Revision, codes (heroin [T40.1]; natural or semisynthetic opioids [T40.2]; methadone [T40.3]; synthetic opioids, other than methadone [T40.4]). We scaled rates by 100 000 population and calculated Pearson correlation coefficients. Sensitivity analysis excluded polysubstance cases involving either heroin or synthetic opioids as well as natural and semisynthetic opioids.
Results. The NVSS mortality and poison center program exposure rates showed similar trends from 2006 to 2012, and diverged after 2012 for all opioids combined, natural and semisynthetic opioids, and synthetic opioids (r = −0.37, −0.12, and 0.30, respectively). Sensitivity analysis with removal of heroin or synthetic opioid polysubstance deaths markedly improved correlations for all opioids combined and natural and semisynthetic opioids (r = 0.87 and 0.36, respectively).
Conclusions. The NVSS mortality and poison center exposure rates showed similar trends from 2006 to 2012 then diverged, with sensitivity analysis suggesting polysubstance cases also involving heroin or illicit fentanyl as the cause.
Public Health Implications. The NVSS and poison center program may provide complementary data when trends diverge. Public health interventions must include both licit and illicit opioids for maximal impact.
Over the past 25 years, increased prescribing of opioids has led to an epidemic of opioid abuse, diversion, and overdose throughout the United States.1 From 1999 to 2016, the Centers for Disease Control and Prevention (CDC) has estimated that more than 200 000 people died from overdoses related to prescription opioids.2 As both federal and state agencies work to develop strategies to address this epidemic, a more nuanced understanding of the drugs involved that lead to greater mortality will allow the development of focused and specific interventions.
On a national level, the National Vital Statistics System (NVSS) is the most widely cited and referenced data set used to identify nationwide trends in cause-specific mortality.3 The NVSS multiple cause-of-death mortality files originate from state and territorial health departments, are centralized and maintained by CDC (released annually), and provide data on demographic, geographic, and cause-of-death information across the United States.4 Because all deaths are legally required to be included, this data source is considered a complete case accounting of mortality in the United States. Literal causes of death from death certificates are assigned primarily by local medical examiners and coroners, and cause-of-death information in NVSS has been aggregated by using the International Classification of Disease, Tenth Revision (ICD-10), codes since 1999.5
Although these data are the most comprehensive mortality data available, some shortcomings include the lack of real-time data availability with a typical lag time of 1 to 2 years after the close of the calendar year, inability to obtain greater context for individual cases within the larger set of data, and lack of product specificity. As the US Food and Drug Administration seeks to provide more useful regulation and guidance regarding prescription opioids, product-specific information is crucial to guiding decisions. In addition, more detailed and specific data are needed to understand the root cause of prescription opioid deaths. Although less comprehensive in some regards, data from other sources may be more specific and more rapidly available. One example is the nationwide network of poison centers that gather data on spontaneous reports of exposures and acute medical events such as overdose and death.6
Poison center cases are classified into 2 major types: information cases and exposure cases. Information cases are those in which the caller is looking for information, but no substance has been consumed. Not surprisingly, in recent years, a good portion of information cases have gone silent, with traffic directed to the Internet instead leading to the observed decline in overall call volume to US poison centers.7 On the other hand, exposure cases are those in which actual or suspected contact with a substance that has been ingested, inhaled, absorbed, applied to, or injected into the body, regardless of toxicity or clinical manifestation. Exposure cases are further divided into human and animal exposures. Furthermore, human exposures can be classified into pharmaceutical and nonpharmaceutical exposures. Analgesics comprise one of the largest categories of pharmaceutical exposures. The analgesics category represents about 20% of all poison center cases within the pharmaceutical exposures category, including acetaminophen, aspirin, ibuprofen, and prescription opioids.8
Given the importance of gaining a better understanding of prescription opioid deaths, we compared the rates of prescription opioid exposures and deaths from US poison centers to the mortality rates reported by NVSS. A previous analysis showed a strong correlation between methadone overdose deaths and poison center intentional exposure cases in 2006 to 2007 in a subset of poison centers.9 To update and extend this analysis, we set out to determine the level of association between poison center calls and overdose deaths. We hypothesized that the poison center data would accurately correlate with CDC data while also containing a more nuanced report of the events and substances used surrounding the death.
METHODS
We included 2 data sources in this analysis, the NVSS multiple cause-of-death mortality files and the Researched Abuse, Diversion and Addiction-Related Surveillance (RADARS) System poison center program.
Data Collection
We extracted the NVSS multiple cause-of-death mortality files by using the Wide-ranging Online Data for Epidemiologic Research (WONDER) apparatus for 2006 to 2016.10 These files contain the official national statistics for deaths reported to vital registration systems across the United States and territories. Drug overdose deaths were classified according to the ICD-10 underlying cause-of-death codes: X40–44 (unintentional), X60–64 (suicide), X85 (homicide), or Y10–Y14 (undetermined intent).3 Among the deaths with drug overdose as the underlying cause, the type of opioid involved was defined by the following ICD-10 multiple cause-of-death codes: heroin (T40.1); natural and semisynthetic opioids (T40.2), which includes hydrocodone, oxycodone, morphine, and other commonly used analgesics; methadone (T40.3); and synthetic opioids, other than methadone (T40.4). The last category includes fentanyl and its analogs, but does not differentiate between pharmaceutical and illicitly manufactured sources (e.g., as an adulterant in heroin); this category also includes buprenorphine and tramadol (Table A, available as a supplement to the online version of this article at http://www.ajph.org). Deaths involving more than 1 type of opioid were included as a single case in the rates for each category.
The RADARS System is a real-time surveillance system that measures prescription drug abuse and diversion for specific products across the United States. The RADARS System poison center program studies acute health events as reported by the general population, caregivers, and health care providers regarding potentially toxic exposures.11 As of December 2016, the RADARS System poison center program collected data from 50 regional US poison centers in 48 states, including urban, suburban, and rural regions (providing coverage for more than 93% of the US population), and subjected the call data to extensive manual data quality review to reduce misclassification of exposure (e.g., instances where a reported substance was not reported, correcting product misclassification) and outcomes, as has been previously described.12 The poison center program is able to identify the specific product in 80.1% of natural and semisynthetic opioid case mentions.
Trained specialists (primarily nurses and pharmacists) at each center collect data by using a nationally standardized electronic health record. An exposure case is defined as any case in which a patient has been exposed to the substance of interest, whether the exposure was intentional or accidental; this is in contrast to mortality data where “intent” is used to describe the intent of death (e.g., suicide vs accidental). A direct death case is defined as a poison center case in which the patient died as a result of the exposure or a direct complication of the exposure, with a fatality verification performed as required by National Poison Data System guidelines.13 Both exposure and direct death cases from the poison center program were classified by the same ICD-10 categories used for the NVSS deaths from 2006 to 2016 (Table A, available as a supplement to the online version of this article at http://www.ajph.org). Any case in which more than 1 category of opioid was involved is counted as a single case in rates for each category.
Analysis
We performed all statistical procedures with SAS version 9.4 (SAS Institute Inc, Cary, NC). We utilized annual data from 2006 through 2016; we chose 2006 because of limited data availability within the poison center system before that time. We excluded poison center cases with confirmed nonexposures by manual review from the analysis. Numerators were case counts from poison center exposure rates and direct death rates, calculated separately. We based denominators for population adjustment on the population of the United States within the coverage area of participating poison centers, and it is an average of the population within each applicable year, with resulting rates scaled by 100 000 population. We based population estimates on the 3-digit zip code tabulation area population in 2000 and 2010. We used linear interpolation and extrapolation to estimate population between 2000 and 2010 and after 2010. We then calculated a Pearson correlation coefficient (r) comparing each respective poison center population rate with the NVSS rate per 100 000 population. Because deaths attributable to synthetic opioids and heroin had a large increase from 2014 to 2016, we conducted a posthoc sensitivity analysis excluding death cases that involved either heroin or a synthetic opioid in addition to another opioid.
RESULTS
There were 564 180 exposure cases reported to RADARS System poison centers for the opioids of interest from 2006 to 2016; 2275 were direct deaths. There were 198 274 opioid-associated deaths reported during the same time period nationally by NVSS. Approximately 1% of all opioid-associated deaths nationally were reported by RADARS System poison centers as direct deaths.
RADARS System poison center call rates were higher than NVSS mortality rates for all prescription opioids (ICD-10 T40.2, T40.3, and T40.4) combined, and for synthetic opioids (T40.4) and natural and semisynthetic opioids (T40.2) individually (Table B, available as a supplement to the online version of this article at http://www.ajph.org). Methadone poison center case rates were slightly lower than NVSS mortality rates.
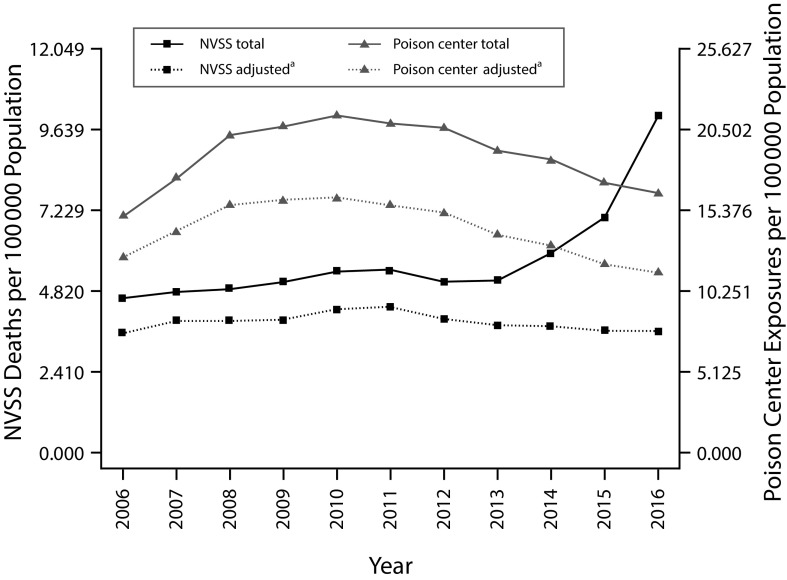
From 2006 through 2016, poison center exposures for all prescription opioids combined (ICD-10 T40.2, T40.3, and T40.4) increased until 2011 and then showed a gradual decline. Crude mortality rates for all prescription opioids combined reported by NVSS showed similar trends until 2013 and then abruptly increased (Figure 1). This divergence resulted in a negative correlation between poison center program exposures and NVSS mortality rates (Pearson correlation coefficient r = −0.37). Trends were similar for poison center direct deaths (Figure A, available as a supplement to the online version of this article at http://www.ajph.org), with a negative correlation (r = −0.41).
FIGURE 1—
Rates of Centers for Disease Control and Prevention National Vital Statistics System (NVSS) Deaths and Researched Abuse, Diversion and Addiction-Related Surveillance System Poison Center Program Exposures for All Prescription Opioids Combined: United States, 2006–2016
Note. All prescription opioids combined: International Classification of Diseases, Tenth Revision, codes T40.2, T40.3, and T40.4.5
aCases adjusted to exclude those also involving heroin or synthetic opioids.
Similarly, for synthetic opioids (ICD-10 T40.4) the rate of exposures reported to the poison center program correlated well with the crude mortality rates reported by NVSS from 2006 through 2012 (r = 0.83), but then diverged from 2013 to 2016, with r = 0.30 from 2006 to 2016 (Figure 2). The exposure rates peaked in 2010 in the poison center program and have remained flat to downtrending since that time, while the NVSS mortality rates increased markedly since 2012. We saw a similar trend with poison center direct deaths (2006–2012 r = 0.61; 2006–2016 r = 0.30; Figure B, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 2—
Rates of Centers for Disease Control and Prevention National Vital Statistics System (NVSS) Deaths and Researched Abuse, Diversion and Addiction-Related Surveillance System Poison Center Program Exposures for Synthetic Opioids: United States, 2006–2016
Note. Synthetic opioids: International Classification of Diseases, Tenth Revision, code T40.4.5
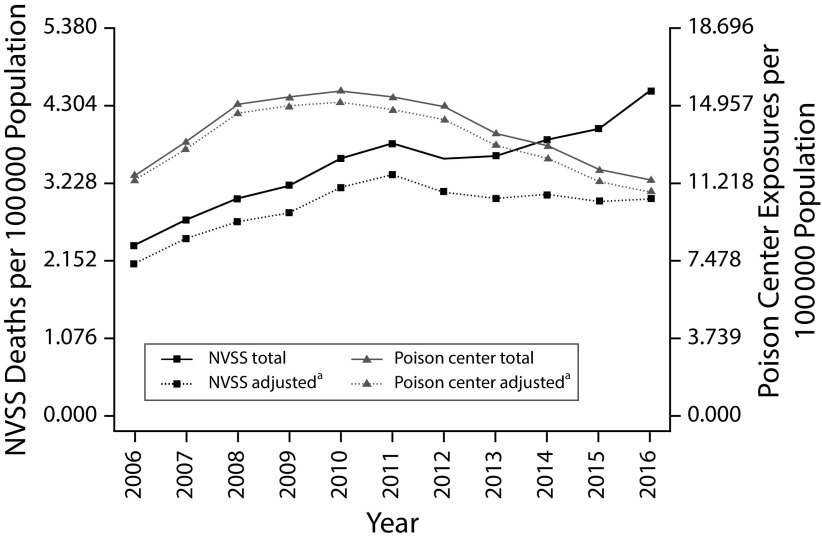
For natural and semisynthetic opioids (ICD-10 T40.2), poison center exposures increased until 2011 and then remained flat to downtrending since that time. Crude NVSS mortality rates, however, showed similar trends until 2012 when they again began to increase (Figure 3. Correlation between poison center program exposures and NVSS mortality rates was again negative (r = −0.12). Poison center direct death rates showed a similar pattern with r = 0.08 (Figure C, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 3—
Rates of Centers for Disease Control and Prevention National Vital Statistics System (NVSS) Deaths and Researched Abuse, Diversion and Addiction-Related Surveillance System Poison Center Program Exposures for Natural and Semisynthetic Opioids: United States, 2006–2016
Note. Natural and semisynthetic opioids: International Classification of Diseases, Tenth Revision, code T40.2.5
aCases adjusted to exclude those also involving heroin or synthetic opioids.
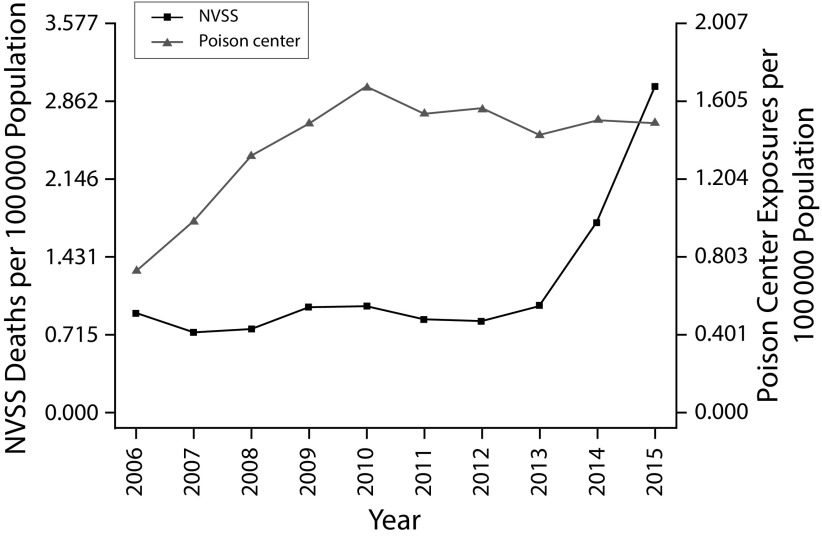
For methadone alone (ICD-10 T40.3), the rate of exposures reported to the poison center program correlated well with the crude mortality rates reported by NVSS (r = 0.87). Methadone exposure and mortality rates have been declining since 2007 in both the poison center program and NVSS data (Figure 4). Poison center direct death rates showed similar correlation with NVSS data, with r = 0.89 (Figure D, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 4—
Rates of Centers for Disease Control and Prevention National Vital Statistics System (NVSS) Deaths and Researched Abuse, Diversion and Addiction-Related Surveillance System Poison Center Program Exposures for Methadone: United States, 2006–2016
Note. Methadone: International Classification of Diseases, Tenth Revision, code T40.3.5
aCases adjusted to exclude those also involving heroin or synthetic opioids.
Given the dramatic rise in heroin use as well as the increase in illicit synthetic opioids such as fentanyl from 2012 on, we hypothesized that polysubstance cases involving either heroin or a synthetic opioid and a prescription opioid might account for the divergence seen between poison center and NVSS trends around this time. We performed a sensitivity analysis in which we adjusted the data to remove polysubstance cases also involving heroin or a synthetic opioid. When we removed these polysubstance cases, the correlation between poison center exposure and NVSS mortality rates for all prescription opioids combined (T40.2, T40.3, and T40.4) increased markedly (r = 0.87; Figure 1). Trends were similar for poison center direct deaths (Figure A, available as a supplement to the online version of this article at http://www.ajph.org), with r = 0.73 with the sensitivity analysis.
For natural and semisynthetic opioids (T40.2), removing polysubstance cases also involving heroin or a synthetic opioid again markedly increased the correlation for poison center exposure rates and NVSS mortality rates (r = 0.36; Figure 3). Poison center direct death rates showed a similar pattern with r = 0.44 when we excluded cases also involving heroin or synthetic opioids (Figure C, available as a supplement to the online version of this article at http://www.ajph.org).
For methadone (T40.3), removing polysubstance cases also involving heroin or a synthetic opioid had minimal impact on methadone poison center exposure rate and NVSS mortality rate correlations (r = 0.92). Trends for poison center direct death rates were similar, with r = 0.92 when we excluded cases also involving heroin or synthetic opioids (Figure 2).
DISCUSSION
The NVSS mortality rates and the poison center program exposure and direct death rates showed similar time trends from 2006 through 2012. Methadone data showed excellent correlation for the entire 11-year study period while all prescription opioids combined, natural and semisynthetic opioids, and synthetic opioids showed very similar time trends between poison center and NVSS data for 7 years and then diverged. After 2012, poison center data continued to show flat to declining exposure and death rates for all 3 groupings of ICD-10 toxicology codes, while NVSS data began to show rapidly rising crude mortality rates.
The timing of divergences between NVSS and the poison center program results may help identify potential causes. Dramatic increases in both heroin and illicit synthetic opioids were seen around 2012 to 2013.14 Within the ICD-10 T40.4 synthetic opioid group, fentanyl and other synthetic analogs are included. During this time, there was no significant increase seen in outpatient pharmaceutical fentanyl drug dispensing.15 However, reports of illicit fentanyl seizures by law enforcement as well as overdose presentations and deaths associated with fentanyl increased dramatically.16
One possible explanation for the difference between NVSS and poison center program rates after 2012 is the contrasting methods used for identifying substances involved in a death. Poison center program data often provide enhanced resolution compared with causes of death reported on death certificates. Individual calls and case notes for cases reported to the poison center program include specific details regarding the type, and often name brand, of the opioid used, how it was obtained, and details surrounding the time of use that may allow the poison specialist on the call to categorize the product and the associated exposure or death in a more specific way than allowed by the aggregate classifications of ICD-10 codes.
In contrast, NVSS data are limited by the level of detail submitted to NVSS by coroners and medical examiners.17 Typically, this information will include the active pharmaceutical ingredient involved in a case, but lacks specific product identification because postmortem sampling can establish the chemical identity, but not the specific formulation or product (e.g., oxycodone vs OxyContin). Furthermore, death certificates do not provide information regarding the context surrounding the drug’s use. Without additional information about a specific case, fentanyl obtained through a prescription and illicitly manufactured fentanyl are indistinguishable from one another in a postmortem laboratory analysis result. The CDC has noted this major limitation to NVSS data and has suggested removing synthetic opioids from estimates of prescription opioid deaths.18 Poison center program data for synthetic opioids may be more specific when the data include only prescription synthetic opioids, and therefore be lower than the nonspecific synthetic opioid rates reported in NVSS.
A second possible explanation for divergence between NVSS and poison center program rates noted after 2012 is the rising rate of heroin abuse.19 Many individuals who misuse and abuse opioids use more than 1 opioid at a time, and this includes rising rates of heroin coabuse.20 Natural and semisynthetic prescription opioids (T40.2) account for the majority of opioids prescribed in the United States.21 As a consequence, it is likely that these are also the opioids most often used simultaneously with heroin. When we removed cases in which both heroin or synthetic opioids and other prescription opioids were listed as causes of death, and examined cases in which only natural and semisynthetic opioids were listed, we found a higher correlation between NVSS mortality rates and rates of exposure reported to poison center programs. This suggests poison center program data may be better able to discriminate between cases in which heroin has played a role, whereas NVSS data may be confounded by polysubstance deaths that obscure the decrease in isolated prescription opioid deaths. The correlation also shows that broad trends seen in poison center program data reflect the mortality trends seen in NVSS data well when the data are appropriately matched.
Correlations were higher between NVSS mortality rates and rates of exposures reported to the poison center program than rates of direct deaths reported to the poison center program for all prescription opioids combined. One potential reason for the higher correlation with exposure rates than direct deaths may be the relatively small number of opioid-related deaths reported directly to poison centers.22 Many of these deaths occur outside of health care facilities, and the patient may have died before a bystander was able to contact a local poison center. Poison center exposure case rates, however, may be a much more useful measure of the amount of an opioid drug available in the community and, therefore, the overdose risk associated with that drug.
Limitations
Both NVSS mortality data and poison center program data have significant limitations. As mentioned, NVSS mortality data are limited to what is available on death certificates. The data included, as well as what testing is used to determine causes of death, are widely variable by state and even county.23 These data lack additional context. The NVSS data are also published on a delayed basis, and toxicological results of autopsy investigations occurring later in the calendar year may not be reported as thoroughly as earlier in the calendar year.
Poison center program data are limited by spontaneous reporting, and represent only a subset of all possible cases. In particular, death cases are reported to poison centers much less often than exposures, and pharmaceutical opioid exposures are reported to poison centers more often than heroin exposures.7 However, previous work has shown that poison center heroin exposures show remarkably similar patterns when compared with NVSS deaths.7 In addition, poison center program data have broad geographic coverage within the United States, are reported in real time, and are available in a more timely manner than NVSS data.11
Finally, mortality data are influenced by state-level practice variations in conducting and interpreting postmortem toxicology assays, giving rise to misclassification bias. During the study period, there were multiple efforts to improve reporting for overdose deaths, intending to increased overdose case detection and reporting.24 In contrast, poison centers had nationally standardized and consistent reporting guidance and trainings throughout the study period, and this form of bias is likely to be lower in poison center data.
In addition, many states first started assaying for fentanyl analogs in 2013 and later, after the recognition of the emerging phenomenon; these deaths would have been solely classified as heroin overdose deaths before these assays were being used consistently, as supported by our sensitivity analyses. This time variation in medical examiner practice represents a form of diagnostic suspicion bias (a type of confirmation bias) in mortality data whereby medical examiners may be more likely to assay for specific compounds if that substance is known to be popularly abused or of emerging concern, as has been previously suggested.25
The identification of similar trends by both NVSS and poison center program data may be useful in the future. Poison center program data may provide an early warning system to identify specific drugs and categories of drugs that are likely to cause harm, and allow for intervention before availability of NVSS mortality data. Detection of a new increase in exposure calls related to a specific product may be a useful signal detection tactic to allow rapid investigation of the cases reported, ways in which that product is being used, and associated complications. In addition, the increased specificity of poison center data may allow more targeted interventions toward specific opioids rather than inform concerns about broad categories of opioids. In particular, our data suggest that the greatest threat to public health stems from heroin and synthetic opioids.
Although a focus on safe opioid prescribing remains extremely important, redirection of resources toward interventions to have an impact on illicit opioids is also crucial. Increased availability of bystander naloxone, community training in its use and overdose recognition and prevention, use of harm reduction networks to increase awareness and safe use practices in communities of people who inject drugs, and increased street testing for synthetic opioids have much greater potential for immediate mortality reduction. However, NVSS data provide the most definitive population-based estimate of mortality prevalence. As a consequence, these 2 data sets may provide complementary data in cases in which they diverge from one another. Utilization of and comparison between both data sets may allow for more effective public health interventions. Future directions for research include standardizing demographic characteristics of decedents to match the 2 data sources to derive methods for improved surveillance.
Conclusions
The NVSS mortality rates and exposure rates reported to the poison center program show very similar trends from 2006 through 2012 for all categories of opioids. Divergences between the 2 after 2012 may be explained by rising rates of heroin abuse as well as illicit fentanyl abuse, which are discriminated by the poison center program but not by NVSS. When cases involving heroin and synthetic opioids such as fentanyl are excluded, NVSS mortality rates are highly correlated to both exposure and direct death rates reported to the poison center program. These adjusted trends also show that deaths attributable to prescription opioids alone are indeed decreasing despite contradictory CDC reports. Data from poison centers may provide more detail (including product specificity) and be available in a more timely fashion than national mortality rates, while still providing similar patterns of broad trends over time.
ACKNOWLEDGMENTS
The authors would like to gratefully acknowledge additional insight and input from John Schwarz, PhD, and Elise Bailey, MSPH.
HUMAN PARTICIPANT PROTECTION
Approval for the poison center program was obtained from the Colorado Multiple institutional review board. The public de-identified data from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System were considered exempt from institutional review board requirements.
REFERENCES
- 1.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The DAWN report: highlights of the 2011 Drug Abuse Warning Network (DAWN) findings on drug-related emergency department visits. Available at: https://www.samhsa.gov/data/report/dawn-report-highlights-2011-drug-abuse-warning-network-dawn-findings-drug-related-emergency. Accessed November 20, 2017.
- 2.Hedegaard H, Warner M, Miniño AM. Drug overdose deaths in the United States, 1999–2016. NCHS Data Brief, no. 294. Hyattsville, MD: National Center for Health Statistics; 2017.
- 3.Wide-ranging Online Data for Epidemiologic Research (WONDER) Atlanta, GA: Centers for Disease Control and Prevention, National Center for Health Statistics; 2016. Available at: http://wonder.cdc.gov. Accessed November 15, 2017.
- 4.Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378–1382. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System Training Manual. 2017. Available at: https://www.cdc.gov/nchs/data/dvs/2b_2017.pdf. Accessed November 14, 2017.
- 6.Gummin DD, Mowry JB, Spyker DA, Brooks DE, Fraser MO, Banner W. 2016 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clin Toxicol (Phila). 2017;55(10):1072–1252. doi: 10.1080/15563650.2017.1388087. [DOI] [PubMed] [Google Scholar]
- 7.Dasgupta N, Bailey JE, Dart RC. Implications of declining poison center case volume on drug abuse trend monitoring. RADARS System Technical Report, 2017-Q3. 2017. Available at: https://www.radars.org/system/publications/2017%203Q%20QTR.pdf. Accessed January 19, 2018.
- 8.Bucher Bartelson B, Le Lait MC, Green JL et al. Changes in misuse and abuse of prescription opioids following implementation of Extended-Release and Long-Acting Opioid Analgesic Risk Evaluation and Mitigation Strategy. Pharmacoepidemiol Drug Saf. 2017;26(9):1061–1070. doi: 10.1002/pds.4257. [DOI] [PubMed] [Google Scholar]
- 9.Dasgupta N, Davis J, Funk MJ, Dart R. Using poison center exposure calls to predict methadone poisoning deaths. PLoS One. 2012;7(7):e41181. doi: 10.1371/journal.pone.0041181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Multiple cause of death 1999–2016 on CDC WONDER online database. 2017. Available at: http://wonder.cdc.gov/ucd-icd10.html. Accessed January 12, 2018.
- 11.Dart RC, Surratt HL, Cicero TJ et al. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(3):241–248. doi: 10.1056/NEJMsa1406143. [DOI] [PubMed] [Google Scholar]
- 12.Davis JM, Severtson SG, Bucher-Bartelson B, Dart RC. Using poison center exposure calls to predict prescription opioid abuse and misuse-related emergency department visits. Pharmacoepidemiol Drug Saf. 2014;23(1):18–25. doi: 10.1002/pds.3533. [DOI] [PubMed] [Google Scholar]
- 13.Bronstein AC, Spyker DA, Cantilena LR, Jr, Green JL, Rumack BH, Giffin SL. 2008 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 26th Annual Report. Clin Toxicol (Phila) 2009;47(10):911–1084. doi: 10.3109/15563650903438566. [DOI] [PubMed] [Google Scholar]
- 14.O'Donnell JK, Gladden RM, Seth P. Trends in deaths involving heroin and synthetic opioids excluding methadone, and law enforcement drug product reports, by census region—United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(34):897–903. doi: 10.15585/mmwr.mm6634a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. QuintilesIMS. Transactional Data Warehouse. 2016.
- 16.Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increase in synthetic opioid-involved overdose deaths—27 states, 2013–2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837–843. doi: 10.15585/mmwr.mm6533a2. [DOI] [PubMed] [Google Scholar]
- 17.Warner M, Paulozzi LJ, Nolte KB, Davis GG, Nelson LS. State variation in certifying manner of death and drugs involved in drug-intoxication deaths. Acad Forensic Pathol. 2013;3(2):231–237. [Google Scholar]
- 18.Seth P, Rudd RA, Noonan RK, Haegerich TM. Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health. 2018;108(4):500–502. doi: 10.2105/AJPH.2017.304265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang X, Keyes KM, Li G. Increasing prescription opioid and heroin overdose mortality in the United States, 1999–2014: an age–period–cohort analysis. Am J Public Health. 2018;108(1):131–136. doi: 10.2105/AJPH.2017.304142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(2):154–163. doi: 10.1056/NEJMra1508490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iwanicki JL, Severtson SG, McDaniel H et al. Abuse and diversion of immediate release opioid analgesics as compared to extended release formulations in the United States. PLoS One. 2016;11(12):e0167499. doi: 10.1371/journal.pone.0167499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore PQ, Weber J, Cina S, Aks S. Syndrome surveillance of fentanyl-laced heroin outbreaks: utilization of EMS, medical examiner, and poison center databases. Am J Emerg Med. 2017;35(11):1706–1708. doi: 10.1016/j.ajem.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 23.Stone DM, Holland KM, Bartholow B et al. Deciphering suicide and other manners of death associated with drug intoxication: a Centers for Disease Control and Prevention consultation meeting summary. Am J Public Health. 2017;107(8):1233–1239. doi: 10.2105/AJPH.2017.303863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Council of State and Territorial Epidemiologists. Consensus recommendations for national and state poisoning surveillance: Report from the Injury Surveillance Workgroup (ISW7). 2012. Available at: http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/Injury/ISW7.pdf. Accessed February 20, 2018.
- 25.Dasgupta N, Mandl KD, Brownstein JS. Breaking the news or fueling the epidemic? Temporal association between news media report volume and opioid-related mortality. PLoS One. 2009;4(11):e7758. doi: 10.1371/journal.pone.0007758. [DOI] [PMC free article] [PubMed] [Google Scholar]