The NaloxBox initiative is an innovative, community-access naloxone program that provides tools, training, and awareness to empower laypeople to rescue victims of opioid overdose. NaloxBox is to opioid overdose as an automated external defibrillator is to sudden cardiac arrest, furnishing simple-to-use, life-saving tools to members of the public so that they can accomplish rescues in advance of the arrival of emergency medical services personnel.
NEED FOR EXPANDED LAYPERSON RESCUE CAPACITY
Deaths from opioid overdose in the United States continue to escalate, exceeding 42 000 in 2016, and Rhode Island ranks 10th in the country in opioid overdose rate.1 Naloxone is a potent antidote to opioid overdose that restores consciousness and breathing, saves lives, and prevents permanent injury. Naloxone prescribing from medical providers and distribution from public health workers to individuals at risk are not sufficient. Because victims cannot help themselves when an opioid overdose renders them unresponsive, rescue depends on timely and effective intervention by others. First responders can be too late.
Layperson rescue with intranasal naloxone had a 98% success rate in a Massachusetts study, and in that same study implementation of overdose education and naloxone distribution (OEND) programs was associated with reduced opioid overdose mortality rates.2 Citing thousands of naloxone rescues from laypeople,3 the Centers for Disease Control and Prevention (CDC) calls for more comprehensive naloxone distribution and training with respect to layperson rescue. The Food and Drug Administration also calls for expanded access to naloxone, including pursuit of approval of over-the-counter naloxone on the part of manufacturers.4 Although some states’ regulations allow standing-order naloxone prescriptions from medical providers to pharmacies and allow OEND programs to expand access to naloxone, few programs exist that offer it as a freely accessible public safety asset.
The American Heart Association’s basic life support algorithm calls for administration of naloxone when a pulse is present but consciousness and breathing are depressed and opioid overdose is suspected. However, the lack of a system for providing community-access naloxone makes possible a tragic, preventable situation wherein the rescuer knows how to save the victim but is left powerless to intervene.
Naloxone intranasal formulations are designed for layperson use,5 and a majority of US states, including Rhode Island, have Good Samaritan laws protecting lay rescuers.6 Naloxone must be delivered as promptly as possible to avert death or permanent injury from hypoxia, and the broad contamination of the illicit drug supply with fentanyl has made prompt administration more urgent. In Rhode Island approximately one in 10 overdoses occur in public, and, similar to the situation in other states, the proportion of opioid deaths involving fentanyl is increasing yearly. In 2017, 63% of opioid overdose deaths in Rhode Island involved fentanyl.7 Fentanyl’s rapid onset of action and potency underscore the need for single-dose or multidose naloxone intervention at the earliest possible time point.
NALOXBOX DESIGN AND IMPLEMENTATION
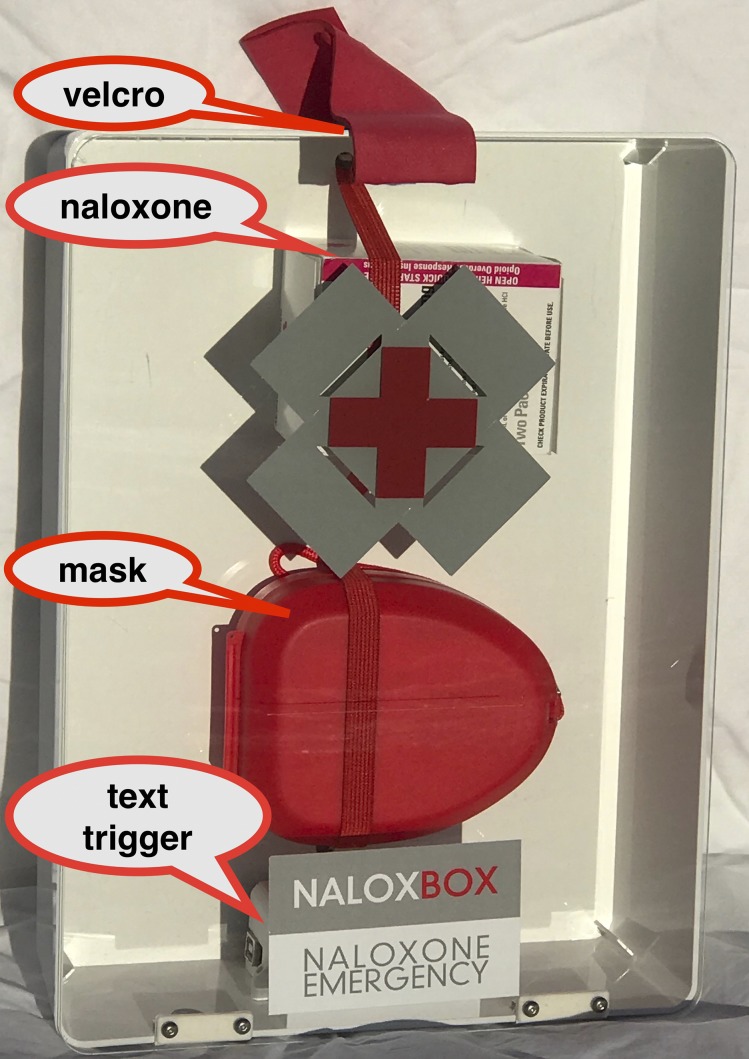
The NaloxBox pilot was supported by a pair of 2017 Rhode Island Department of Health (RIDOH) overdose prevention mini-grants supported by the CDC. The pilot involved a collaboration between an emergency medicine physician (G. A. C.) and an expert in industrial design (C. B. R.). The goal was to create an attractive and accessible unit (Figure 1) with graphics and instructions to facilitate rescue and information on how to secure personal naloxone and addiction services. The hinged, Plexiglas front panel is fastened only by Velcro for ease of access, and the latest-version NaloxBoxes can be equipped with electronics to notify facility staff of NaloxBox openings and the potential need to assist a victim and to inspect and restock the unit.
FIGURE 1—
NaloxBox With Labels Indicating Key Features
Each NaloxBox contains multiple doses of naloxone and a barrier mask to facilitate rescue breaths. Four doses of the 0.4-milligram intramuscular formulation were furnished in facilities where staff underwent training on intramuscular administration, and two doses of the 4- milligram intranasal formulation were furnished in settings where layperson rescue seemed more likely. Prescription labels indicating expiration dates are placed in units, and locations, contact information, and expiration dates are centrally inventoried.
Installation locations serving high-risk populations were identified through outreach to the Rhode Island Coalition for the Homeless, outreach to the Rhode Island governor’s naloxone working group, and e-mails to naloxboxproject@gmail.com resulting from media coverage. The installations targeted individuals seeking food in soup kitchens (Amos House, McAuley Ministries), the homeless (House of Hope, Crossroads, McKinney House), ex-prisoners in transition to permanent housing (9 Yards, OpenDoors RI), and individuals in recovery from addiction (House of Hope). Additional installations were established in public facilities including city halls (Providence, Central Falls), libraries (Providence, Central Falls, Woonsocket), public housing (Pawtucket), and the RIDOH building. Self-referrals and RIDOH “heat maps” of incident overdoses will inform upcoming site selection.
NaloxBox locations are mapped at http://preventoverdoseri.org/naloxboxes. This RIDOH-supported Web site informs the public about the program and how to locate the nearest NaloxBox. It is hoped that in the future, 911 dispatchers will employ such maps to direct callers to the nearest NaloxBox and that individuals will employ apps to locate NaloxBoxes and naloxone-carrying bystanders.
INITIAL NALOXBOX EXPERIENCE
Over the first five months of the program, we successfully engaged 18 collaborating agencies, installed 47 NaloxBoxes, and conducted on-site training sessions at all sites where training had not already been conducted. The 37 remaining RIDOH grant-supported NaloxBoxes have been spoken for, and additional requests have been received from 13 states along with Ottawa, Canada.
The NaloxBox pilots were not conducted as research initiatives; because we were the installers and worked with OEND partners that were providing naloxone, however, we were informed regarding NaloxBox issues and usage. To our knowledge, none of the installed units have been vandalized, two have required restocking, and to date we have confirmed one successful NaloxBox-involved rescue.
In this rescue a layperson reportedly administered multiple doses of naloxone to reverse a fentanyl overdose in a multi-unit dwelling, and the victim was later discharged from the hospital to home. The NaloxBox used in this rescue was stocked with intramuscular naloxone, so it came as some surprise that a layperson was able to administer this form of naloxone and that semipublic tools proved useful in a private dwelling.
No adverse effects have been reported. An insurer threatened to, but in the end did not, increase the insurance premium for one agency after the facility manager notified the insurer that it had installed NaloxBoxes.
OPPORTUNITIES TO SCALE THE SOLUTION
NaloxBoxes were designed to minimize costs. They are simple to install, and the NaloxBox approach to outreach and collaboration can be easily replicated by other state and province departments of health, municipalities, community agencies, and OEND experts.
Efforts are under way to scale the NaloxBox program inside and beyond Rhode Island. A grant has been secured to refine the user interface and deploy 36 units in Ohio, and an established nonprofit organization experienced in OEND work and community emergency preparedness soon will assume NaloxBox operations. To support individuals in recovery and to communicate the message that recovery is possible, NaloxBoxes will be assembled by individuals in jobs training at the first facility to install NaloxBoxes, Amos House. The price of the units has not been finalized but is anticipated to be about $200 not including naloxone. A grant proposal is being prepared for a multicenter trial of NaloxBox and enhanced OEND interventions.
PUBLIC HEALTH SIGNIFICANCE
Multipronged efforts are needed to address the escalating epidemic of opioid overdose deaths. Naloxone rescue is the prong aimed at immediately preventing death, but personal-use naloxone is insufficiently effective. Community-access naloxone represents an important supplemental method for accomplishing rescues.
The NaloxBox initiative could serve as a model for building a system of community-access naloxone. The worsening epidemic of opioid overdose deaths in the United States and the growing, devastating impact of fentanyl indicate a significant need to strengthen and broaden the rescue capacity of laypeople.
REFERENCES
- 1.Centers for Disease Control and Prevention. Opioid overdose: drug overdose death data. Available at: https://www.cdc.gov/drugoverdose/data/statedeaths.html. Accessed September 6, 2018.
- 2.Walley A, Xuan Z, Hackman HH et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174. doi: 10.1136/bmj.f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wheeler E, Jones TS, Gilbert MK et al. Opioid overdose prevention programs providing naloxone to laypersons. MMWR Morb Mortal Wkly Rep. 2015;64(23):631–635. [PMC free article] [PubMed] [Google Scholar]
- 4.Mahoney K. FDA supports greater access to naloxone to help reduce opioid overdose deaths. Available at: https://blogs.fda.gov/fdavoice/index.php/2016/08/fda-supports-greater-access-to-naloxone-to-help-reduce-opioid-overdose-deaths. Accessed September 6, 2018.
- 5.Lewis CR, Vo HT, Fishman M. Intranasal naloxone and related strategies for opioid overdose intervention by nonmedical personnel: a review. Subst Abuse Rehabil. 2017;8:79–95. doi: 10.2147/SAR.S101700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute on Drug Abuse. Medications to treat opioid addiction. Available at: https://www.drugabuse.gov/publications/research-reports/medications-to-treat-opioid-addiction/overview. Accessed September 6, 2018.
- 7.Prevent Overdose RI. Overdose deaths related to fentanyl). Available at: http://preventoverdoseri.org/overdose-deaths. Accessed September 6, 2018.