Abstract
Objectives. To demonstrate the severity of undercounting opioid-involved deaths in a local jurisdiction with a high proportion of unspecified accidental poisoning deaths.
Methods. We matched toxicology data to vital records for all accidental poisoning deaths (n = 1238) in Marion County, Indiana, from January 2011 to December 2016. From vital records, we coded cases as opioid involved, specified other substance, or unspecified. We extracted toxicology data on opioid substances for unspecified cases, and we have reported corrected estimates of opioid-involved deaths after accounting for toxicology findings.
Results. Over a 6-year period, 57.7% of accidental overdose deaths were unspecified and 34.2% involved opioids. Toxicology data showed that 86.8% of unspecified cases tested positive for an opioid. Inclusion of toxicology results more than doubled the proportion of opioid-involved deaths, from 34.2% to 86.0%.
Conclusions. Local jurisdictions may be undercounting opioid-involved overdose deaths to a considerable degree. Toxicology data can improve accuracy in identifying opioid-involved overdose deaths.
Public Health Implications. Mandatory toxicology testing and enhanced training for local coroners on standards for death certificate reporting are needed to improve the accuracy of local monitoring of opioid-involved accidental overdose deaths.
The United States has experienced a dramatic increase in drug overdose deaths in the most recent reporting period (2015–2016), which is attributable to a rise in opioid-involved deaths.1 Despite these trends, a considerable number of drug overdose deaths remain unspecified (i.e., have no substance indicated as a primary or contributing cause of death), which is thought to lead to undercounting of opioid-involved deaths nationally.2 In 14 states, at least one fifth of accidental drug overdose deaths are unspecified.3 Although a considerable amount of federal, state, and local resources has been mobilized to address the opioid epidemic, the inability to accurately measure fatal opioid-involved overdoses remains a barrier to evaluating the effectiveness of policies and programs aimed at addressing this public health crisis.
Having a system that relies on local coroners and medical examiners to accurately record opioid substances on death certificates contributes to high rates of unspecified overdose deaths. The Centers for Disease Control and Prevention’s wide-ranging online surveillance data for epidemiological research are commonly used in national reports. These data employ International Classification of Disease, Tenth Revision (ICD-10)4 codes to standardize the classification of causes of death. The National Center for Health Statistics (NCHS) collects these data and uses software to classify information from death certificates and to determine underlying causes of death.5
However, this process is not ideal for detecting when opioids may have contributed to an overdose, even considering the availability of toxicology results. For example, if a coroner or medical examiner does not write the specific name of an opioid analgesic, or writes no name at all, the drug poisoning will be coded with an “unspecified” substance as a contributing factor. This practice is especially problematic when polysubstance use is indicated as a contributing cause of death, resulting in undercounting of accidental overdose deaths for 2 or more substances. Current best practices recommend that all substances implicated in a polysubstance overdose be listed individually on the death certificate,6 enabling the NCHS to classify and count them appropriately.
Reliance on local jurisdictions to accurately record death certificate data has resulted in extreme state-level variability in the proportion of drug overdose deaths classified as unspecified. For example, more than one third of accidental overdose deaths are coded as unspecified in Louisiana, Pennsylvania, Alabama, Montana, Indiana, and Delaware, whereas less than 1% are coded as unspecified in Washington, DC, Connecticut, and Rhode Island.3 This variation is largely the result of state policies on the death certificate system; specifically, states with a centralized medical examiner have a lower rate of unspecified drug-poisoning deaths than do those with a decentralized coroner system.7 The difference is that states with a decentralized coroner system do not require medical training, and there is little oversight in how deaths are investigated, including whether a toxicology analysis is conducted or reported.7–9
To date, previous approaches aimed at correcting the undercounting of opioid-involved deaths have relied on predictive modeling of national population-level surveillance data to impute the proportion of opioid-involved unspecified overdose deaths.2,10,11 These investigations have yielded corrected rates of opioid-involved deaths that are 20.9% to 40.8% higher than published national estimates in any particular year (i.e., 2011–2015).2,10,11 Despite the importance of such investigations in national opioid surveillance efforts, they are not without limitations. Primarily, predicted probabilities are subject to a margin of error, as evidenced by variability in corrected estimates. Further, reliance on population-level data to infer individual trends has come under recent criticism as contributing to ecological fallacies (i.e., inferences about individual-level trends from group-level data).12
In the context of opioid surveillance, the use of national population data carries several assumptions, including that individual specified poisoning deaths are accurately coded as non–opioid involved and that specific drug classes are accurately captured in existing data sources. Finally, because these analyses are conducted at the national and state levels, they have limited utility for local surveillance efforts. This is particularly true in a decentralized coroner system in which the impetus for improving opioid surveillance will need to be driven by local coroners. Accurate monitoring of local opioid trends is essential for informing the allocation of resources for interventions aimed at addressing the opioid epidemic (e.g., naloxone distribution, syringe exchange, treatment options).
We addressed these limitations by conducting a county-level case study of substances detected in unspecified accidental poisoning deaths using toxicology data as a criterion. The state of Indiana relies on a decentralized coroner system and is frequently ranked among the top 5 states with high proportions of unspecified overdose deaths.3,11 Marion County (Indianapolis) is the state’s largest county and accounts for a considerable 22% of all accidental drug overdose deaths. Through a collaboration with the local Marion County Coroner’s Office (MCCO), we collected toxicology data on all accidental drug overdose cases from 2011 to 2016. By matching toxicology data to vital records to determine substances detected in unspecified drug overdose cases, we have provided an accurate correction for opioid-involved deaths in a large local jurisdiction that could be easily replicated in other localities and that illustrates the need for improved local surveillance efforts.
METHODS
The toxicology data in this study come from the MCCO, which has jurisdiction over all drug-related overdoses and associated death certificates. Once a death is suspected to be a coroner’s case (e.g., deaths from accidental injuries, homicides, suicides, work-related deaths, deaths owing to therapeutic complications, or deaths about which there are doubts), the coroner initiates a case report for that individual, documenting demographic information, autopsy results, personal history gathered from interviews with close relatives or friends, and information contained in medical records. A preliminary cause of death is marked at this time pending toxicology results, which are routinely completed and available 4 to 6 weeks after the sample is submitted. The medical examiner reviews the toxicology results and combines them with the autopsy report. The coroner reviews these results to determine the cause of death. This information is recorded in the cause of death section on the death certificate and sent to the Indiana State Department of Health, which submits vital records to NCHS to assign ICD-10 codes.
Through an ongoing collaboration with the MCCO, we collected data from death certificates and toxicology screening reports for all fatal overdoses in Marion County. For each fatal overdose, 2 researchers independently coded the information from these 2 sources, and a senior reviewer conducted ongoing random accuracy checks. The toxicology reports that the MCCO provides rely on a detection threshold established by the testing agency that registers as positive when a substance exceeds the threshold. For cases before March 9, 2016, the Indiana State Department of Toxicology outsourced toxicology testing for opioids to AXIS Forensic Toxicology (formerly AIT Laboratories).13 Testing thresholds in place during this period were 0.5 nanograms per milliliter and 0.5 to 5.0 nanograms per milliliter for fentanyl and opioid compounds, respectively. For cases processed during the remainder of the study period (i.e., March 10, 2016, to December 31, 2016), toxicology testing was outsourced to NMS Labs. Specific detection thresholds varied by compound, but detection thresholds were generally more sensitive than were screening tests conducted by AXIS Forensic Toxicology.14
We used positive toxicology results, which were determined by detection thresholds set by the testing agency, as the criterion for an opioid-involved accidental drug overdose. We extracted data on several opioid substances from the toxicology reports: 6-monoacetylmorphine ([6-MAM] a heroin metabolite), fentanyl (and synthetic analogs), morphine, codeine, oxycodone, hydrocodone, oxymorphone, and hydromorphone. One limitation of toxicology data is the inability to determine the presence of 6-MAM in a heroin-related overdose because heroin undergoes rapid transformation into natural opioids (mainly morphine). However, codeine has been found in trace amounts in heroin-involved deaths, but unlike morphine, codeine is not a metabolite of heroin. In the absence of 6-MAM, morphine to codeine ratios in excess of 1 can be used to provide evidence of heroin use.15,16 However, in this study, all cases containing morphine and codeine additionally contained 6-MAM and thus were counted as heroin cases.17 We coded cases into 3 categories: prescription opiates, heroin, and fentanyl. Importantly, these categories are not mutually exclusive, as cases can contain all 3 substances.
We linked toxicology data from January 1, 2011, through December 31, 2016, to vital records data from the Indiana Death Registration System containing ICD-10 codes for both underlying causes of death and contributing codes (n = 1313). When an accidental drug overdose death is not assigned any contributing factors, it is considered unspecified in terms of cause of death (as inferred from toxicology findings). In other cases, there may be several substances detected in a toxicology report (i.e., a polydrug overdose), and for these cases no single substance is listed as the contributing cause, also resulting in an unspecified code (i.e., T50.9). Following the National Vital Statistics System guidelines, we determined which cases were coded as an accidental drug poisoning (X40-X-44) and, of these cases, which had additional contributing opioid-related ICD-10 codes (e.g., T40.0, T40.1, T40.2, T40.3, T40.4, or T40.6) or an unspecified code (T50.9). We identified accidental drug-poisoning ICD-10 codes for 94.3% (n = 1238) of the toxicology cases collected during this 6-year study. The remaining cases were either transferred out of county or determined to be nonaccidental drug-poisoning deaths.
On the basis of vital records, we classified all accidental drug-poisoning deaths as either unspecified, opioid involved, or specified other. Unspecified cases were cases in which no single substance was indicated by ICD-10 codes. That is, unspecified cases were coded as accidental drug poisoning (X40-X44) but contained only an unspecified contributing cause code (T50.9). Opioid-involved cases included cases for which at least 1 opioid was indicated as a primary or contributing case of death, regardless of whether other, nonopioid substances were indicated by ICD-10 codes. Specified other cases included all cases for which a specific substance was indicated by ICD-10 codes but no opioid analgesics were coded. Following classification, we conducted frequencies by category and year. Next, we examined the frequency of opioids detected in toxicology reports among unspecified and specified other cases. Finally, following linkage of toxicology data and vital records, we recoded unspecified and specified other cases as opioid involved on the basis of whether an opioid was detected at threshold levels in toxicology reports, consistent with recommended guidelines from the National Association of Medical Examiners regarding polysubstance deaths.6 From these data, we produced generated corrected frequencies by category and year.
RESULTS
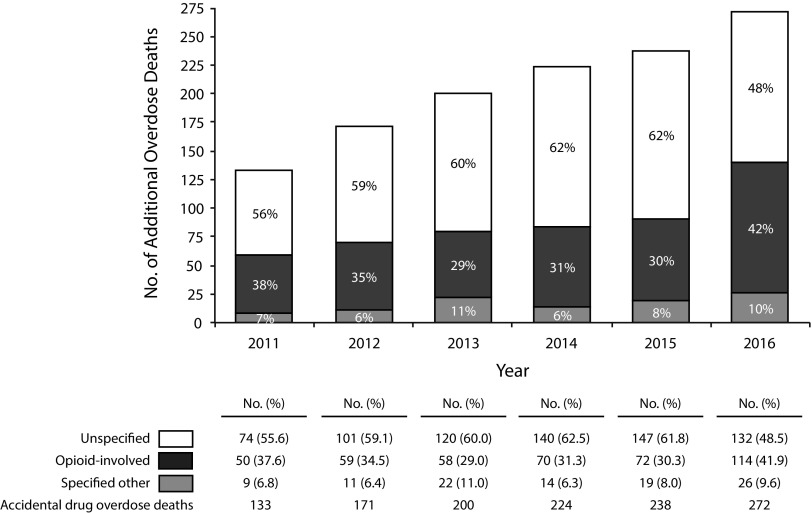
As illustrated in Figure 1, the number of accidental drug overdose deaths in Marion County more than doubled during the study period, from 133 in 2011 to 272 in 2016. For all annual estimates, accidental overdose deaths in Marion County were more likely to be coded as unspecified (range: 48.5%–62.5%) than as opioid involved (range: 29.0%–41.9%). On average, over the 6-year study period, 57.7% of accidental drug overdose cases were unspecified whereas 34.2% were coded as opioid involved. The proportion of cases classified as opioid involved was relatively consistent over the 6-year period, apart from 2016, when there was a 38.3% increase in the rate of opioid-involved deaths relative to 2015.
FIGURE 1—
Accidental Drug Overdose Deaths on the Basis of Coroner Death Certificate Records: Marion County, IN, 2011–2016
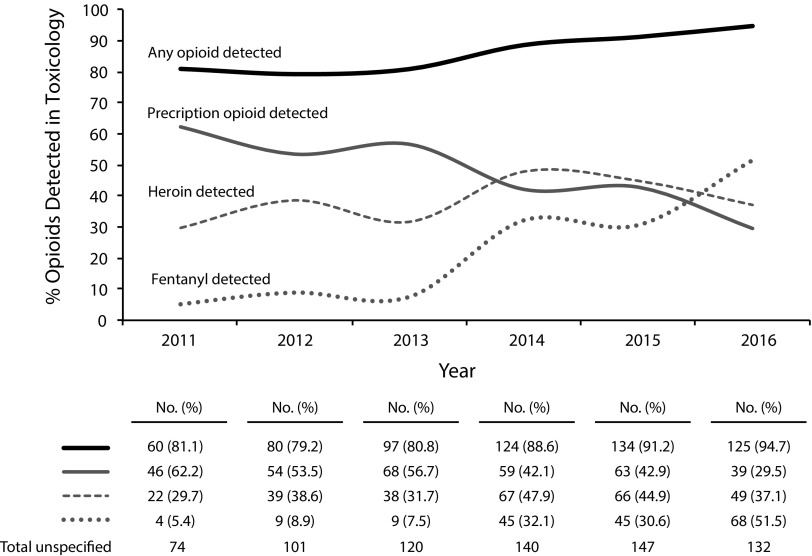
Next, we examined toxicology results to determine the threshold level of substances detected in unspecified cases. As shown in Figure 2, 86.8% (n = 620) of cases coded as unspecified during the study period tested positive for an opioid in the toxicology report. We found a steady decline in the presence of prescription opiates—in both total counts and percentage detected—in unspecified cases, from 62.2% (n = 46) in 2011 to 29.5% (n = 39) in 2016. The proportion of heroin detections varied over time, with a growth in detections from 2011 (29.7%; n = 22) to 2014 (47.9%; n = 67) and fewer detections in 2015 and 2016 (41.2%; n = 115 for both years). However, there were dramatic changes in the detection of fentanyl in unspecified cases from 5.4% (n = 4) in 2011 to 51.5% (n = 68) in 2016, representing an 853.7% increase over the study period. Critically, despite increases in accidental drug overdose deaths and changes in the types of opioid substances detected, the proportion of unspecified cases with detected opioids was less variable over time (range: 79.2%–94.7%) relative to individual substance trends.
FIGURE 2—
Opioids Detected in Toxicology Reports Among Unspecified Accidental Drug Overdose Cases: Marion County, IN, 2011–2016
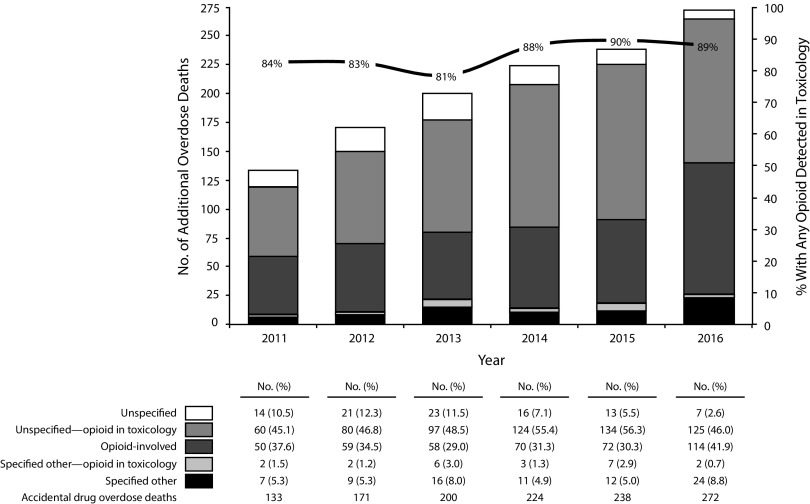
Finally, Figure 3 replicates Figure 1 and additionally indicates the number of unspecified cases or specified other cases that were opioid involved according to toxicology data. As shown, across all years, consideration of toxicology data alone generated a greater number of opioid-involved cases than originally indicated by ICD-10 codes (51.9% vs 34.2%, respectively). Excluding specified other accidental poisoning deaths that were opioid involved, there were still more opioid-involved cases in unspecified cases (50.1%) than in those reported by ICD-10 codes alone. Including toxicology results more than doubled the total proportion of opioid-involved deaths across the study period, from 34.2% to 86.0%, representing a 151.5% increase in the rate of opioid-involved accidental overdose deaths over the 6-year period, or 642 additional cases. Moreover, adjusted rates of opioid-involved deaths were comparable across the 6-year period, ranging from 80.5% (2013) to 89.5% (2015), despite the previously referenced 38.3% increase in the proportion of reported opioid-involved deaths from 2015 to 2016.
FIGURE 3—
Accidental Overdose Deaths on the Basis of Coroner Death Certificate Records and Toxicology Reports: Marion County, IN, 2011–2016
DISCUSSION
Through toxicology and vital record linkage, we have demonstrated the severity of undercounting opioid-involved accidental overdose deaths over a 6-year period in Marion County, Indiana. Inclusion of toxicology data more than doubled the proportion of opioid-involved deaths over the study period. Our results may be particularly meaningful for statewide opioid surveillance in Indiana, where comparable proportions of accidental drug overdose deaths are coded as unspecified. Our findings suggest that up to 9 in 10 accidental drug overdose deaths may be opioid involved and raise the possibility that researchers could produce more accurate counts of opioid-involved deaths by treating all unspecified accidental poisoning deaths as opioid involved rather than relying solely on cases coded as opioid involved.
Few published adjusted estimates of opioid-involved deaths have produced a correction as disparate from reported deaths as our study. To illustrate, corrected national rates of opioid-involved deaths are 20% to 30% higher than are reported rates in any specific year.2 On a state level, Louisiana has been given the most disparate corrected rate of opioid-involved deaths (125% higher than reported rates), following by Pennsylvania (108.2%), Mississippi (107.9%), and Alabama (107.1). Indiana, by comparison, has a corrected rate that is 104.3% higher (i.e., slightly more than double) than the reported rate.11 By contrast, in this study, the corrected rate produced by toxicology records was 151% higher—or 2.5 times greater—than the reported rate for Marion County. There are at least 2 possible explanations for our findings. First, there may be considerable variability in the proportion of opioid-involved deaths in local jurisdictions, as evidenced by comparably large jurisdictions reporting high rates of opioid-involved deaths (e.g., Allegheny County).18 Second, our findings may underscore the limitations of national data sets in accurately counting opioid deaths—even when few unspecified accidental overdose deaths are noted because of differences in local reporting.19
Of relevance to current surveillance efforts, our results suggest that recent increases in opioid-involved deaths may indicate improved tracking of opioid-involved deaths rather than being true increases. After accounting for toxicology data, our analysis showed a fairly stable proportion of opioid-involved deaths across the 6-year period. Importantly, although the county reported a more than one third increase in the proportion of opioid-involved deaths in the most recent reporting period (2015–2016), the true proportion of opioid-involved deaths according to toxicology results was nearly identical in 2015 and 2016 (89.5% and 88.6%, respectively). Examination of toxicology results by substance points to improved fentanyl detection and monitoring as a potential explanation for these trends. In particular, we observed a massive increase in fentanyl-related deaths over the study period, with a large jump between 2015 and 2016, commensurate with a substantial increase in the proportion of reported opioid-involved deaths. Nationally, fentanyl-related opioid overdose deaths have doubled during this period1; recent research suggests that this growth is largely attributable to the increasing availability of illicit fentanyl, which is often consumed unknowingly by users.20
More broadly, these trends suggest the need for improved local monitoring of opioid-involved deaths. In decentralized county-based coroner systems especially, coroners are less likely to use toxicology services and often lack a standardized structure for death investigations, which increases variability in reporting across jurisdictions and contributes to high proportions of reported unspecified overdose deaths.7,9 One way to address this issue in a decentralized system is to require the use of toxicology results to test for the presence of controlled substances. Kentucky passed this type of legislation in 2012, and Indiana passed similar legislation in 2018. However, Kentucky’s legislation has not resulted in reductions in the number of unspecified drug overdose cases,21 but it has given rise to an injury research prevention center that examines trends in the reported toxicology data to increase the accuracy of reporting.
Reducing the number of unspecified drug overdose deaths requires efforts beyond simply conducting toxicology testing. Rather, how toxicology findings are incorporated into cause of death determinations is paramount. Current evidence-based guidelines recommend that toxicology findings be used to specify all substances involved in polysubstance overdose deaths on the death certificate.6 As our findings suggest, adherence to this recommendation is likely to drastically increase the proportion of opioid-involved deaths in jurisdictions with high proportions of unspecified drug overdose deaths. However, determining threshold levels of drug concentrations responsible for cause of death is complicated by postmortem redistribution of substances,22,23 tolerance levels of decedents, drug interactions, and drug metabolism.6 Although we relied on positive drug identification to determine opioid-involved deaths, drug concentrations as causal factors in suspected overdose deaths should be investigated in consultation with a decedent’s medical history, circumstances of death, and autopsy findings.6
PUBLIC HEALTH IMPLICATIONS
Overall, local efforts to appropriately prioritize and allocate resources for the opioid epidemic remain stymied by inaccurate counting of opioid-involved deaths. Jurisdictions with decentralized county coroner systems may need to engage efforts beyond legislation to improve local opioid surveillance. Training protocols and standards for death certificate reporting have been developed for use by county coroners, who are on the front lines of opioid surveillance and who are increasingly overwhelmed by the sheer volume of overdose-related deaths.24,25 These approaches, however, require local and regional resources to ensure proper implementation. Improved local surveillance is a necessary precursor to the development and implementation of targeted strategies aimed at curbing the opioid epidemic.
The increasing prevalence of illicit fentanyl in local drug markets necessitates community-based solutions to this epidemic, which may include additional penalties for the distribution of illicit fentanyl, increased availability of high-dosage naloxone, and more community treatment options for opioid addiction (e.g., medication-assisted treatment).26,27 Despite diversion of resources at the national level to curtail the opioid epidemic, such broad-reaching strategies are unlikely to reach full effectiveness without accurate, timely, and responsive monitoring and intervention by those on the frontlines of this epidemic.
ACKNOWLEDGMENTS
This study was supported by the Centers for Disease Control and Prevention (CDC; grant 5 NU17CE002721-02).
At the time of this study, A. Ballew was employed by the Marion County Coroner’s Office. Her contributions to this article were limited to assisting in interpreting the findings. She had no role in data collection or analysis. All other authors have no conflicts of interest to report.
Note. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the CDC or the Department of Health and Human Services.
HUMAN PARTICIPANT PROTECTION
This study did not require institutional review because it involved only decedents.
Footnotes
See also Warner and Hedegaard, p. 1587.
REFERENCES
- 1.Hedegaard H, Warner M, Miniño AM. Drug Overdose Deaths in the United States, 1999–2016. Hyattsville, MD: National Center for Health Statistics; 2017. [Google Scholar]
- 2.Ruhm CJ. Corrected US opioid-involved drug poisoning deaths and mortality rates, 1999–2015. Addiction. 2018;113(7):1339–1344. doi: 10.1111/add.14144. [DOI] [PubMed] [Google Scholar]
- 3.Casteel K. There is more than one opioid crisis. 2018. Available at: https://fivethirtyeight.com/features/there-is-more-than-one-opioid-crisis. Accessed February 2, 2018.
- 4.ICD-10: International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 5.Centers for Disease Control and Prevention. Instruction manuals. 2017. Available at: https://www.cdc.gov/nchs/nvss/instruction_manuals.htm. Accessed May 15, 2018.
- 6.Davis GG. National Association of Medical Examiners and American College of Medical Toxicology Expert Panel on Evaluating and Reporting Opioid Deaths. Complete republication: National Association of Medical Examiners position paper: recommendations for the investigation, diagnosis, and certification of deaths related to opioid drugs. J Med Toxicol. 2014;10(1):100–106. doi: 10.1007/s13181-013-0323-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Warner M, Paulozzi LJ, Nolte KB, Davis GG, Nelson LS. State variation in certifying manner of death and drugs involved in drug intoxication deaths. Acad Forensic Pathol. 2013;3(2):231–237. [Google Scholar]
- 8.Centers for Disease Control and Prevention. Indiana—coroner/medical examiner laws. 2014. Available at: https://www.cdc.gov/phlp/publications/coroner/indiana.html. Accessed February 2, 2018.
- 9.Hickman MJ, Hughes KA, Strom KJ, Ropero-Miller JD. Medical Examiners and Coroners’ Offices, 2004. Washington, DC: Bureau of Justice Statistics; 2007. [Google Scholar]
- 10.Ruhm CJ. Drug poisoning deaths in the United States, 1999–2012: a statistical adjustment analysis. Popul Health Metr. 2016;14(1):2. doi: 10.1186/s12963-016-0071-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruhm CJ. Geographic variation in opioid and heroin involved drug poisoning mortality rates. Am J Prev Med. 2017;53(6):745–753. doi: 10.1016/j.amepre.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 12.Caputi TL, Sabet KA. Population-level analyses cannot tell us anything about individual-level marijuana–opioid substitution. Am J Public Health. 2018;108(3):e12. doi: 10.2105/AJPH.2017.304253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. AIT Laboratories. DetectiMed panel blood. 2014. Available at: http://portal.axisfortox.com/uploadedFiles/Test_Catalog/DetectiMed%20Panel%20Blood%2070630(1).pdf. Accessed May 11, 2018.
- 14.NMS Labs. Postmortem, expanded with NPS, blood (forensic) test. 2018. Available at: http://www.nmslabs.com/tests/Postmortem–Expanded-with-NPS–Blood–Forensic-/8054B. Accessed May 11, 2018.
- 15.Ellis AD, McGwin G, Davis GG, Dye DW. Identifying cases of heroin toxicity where 6-acetylmorphine (6-AM) is not detected by toxicological analyses. Forensic Sci Med Pathol. 2016;12(3):243–247. doi: 10.1007/s12024-016-9780-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Konstantinova SV, Normann PT, Arnestad M, Karinen R, Christophersen AS, Mørland J. Morphine to codeine concentration ratio in blood and urine as a marker of illicit heroin use in forensic autopsy samples. Forensic Sci Int. 2012;217(1–3):216–221. doi: 10.1016/j.forsciint.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 17.Harruff RC, Couper FJ, Banta-Green CJ. Tracking the opioid drug overdose epidemic in King County, Washington: using an improved methodology for certifying heroin related deaths. Acad Forensic Pathol. 2015;5(3):499–506. [Google Scholar]
- 18.Allegheny County Department of Human Services; Allegheny County Health Department. Opioid-related overdose deaths in Allegheny county, 2015–2016 update. 2018. Available at: http://www.achd.net/overdoseprevention/ACDHS-Opioid-Overdose-Deaths-Update-Report-0218.pdf. Accessed March 1, 2018.
- 19.Slavova S, O’Brien DB, Creppage K et al. Drug overdose deaths: let’s get specific. Public Health Rep. 2015;130(4):339–342. doi: 10.1177/003335491513000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cicero TJ, Ellis MS, Kasper ZA. Increases in self-reported fentanyl use among a population entering drug treatment: the need for systematic surveillance of illicitly manufactured opioids. Drug Alcohol Depend. 2017;177:101–103. doi: 10.1016/j.drugalcdep.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Akers D, Rock P, Slavova S, Bunn TL. Drug Overdose Deaths in Kentucky, 2000–2015. Lexington, KY: Kentucky Injury Prevention and Research Center; 2016. [Google Scholar]
- 22.Brockbals L, Staeheli SN, Gascho D, Ebert LC, Kraemer T, Steuer AE. Time-dependent postmortem redistribution of opioids in blood and alternative matrices. J Anal Toxicol. 2018;42(6):365–374. doi: 10.1093/jat/bky017. [DOI] [PubMed] [Google Scholar]
- 23.Yarema MC, Becker CE. Key concepts in postmortem drug redistribution. Clin Toxicol (Phila) 2005;43(4):235–241. [PubMed] [Google Scholar]
- 24.Webster LR, Dasgupta N. Obtaining adequate data to determine causes of opioid-related overdose deaths. Pain Med. 2011;12(suppl 2):S86–S92. doi: 10.1111/j.1526-4637.2011.01132.x. [DOI] [PubMed] [Google Scholar]
- 25.Robinson R. County coroners and their role in the heart of the opioid epidemic. Acad Forensic Pathol. 2017;7(1):80–86. doi: 10.23907/2017.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frank RG, Pollack HA. Addressing the fentanyl threat to public health. N Engl J Med. 2017;376(7):605–607. doi: 10.1056/NEJMp1615145. [DOI] [PubMed] [Google Scholar]
- 27.Stogner JM. The potential threat of acetyl fentanyl: legal issues, contaminated heroin, and acetyl fentanyl “disguised” as other opioids. Ann Emerg Med. 2014;64(6):637–639. doi: 10.1016/j.annemergmed.2014.07.017. [DOI] [PubMed] [Google Scholar]