Abstract
Objectives. To identify the 20 most important and most preventable health problems that should be addressed in the next 20 years in China.
Methods. In 2015, we applied a modified electronic Delphi technique to reach consensus from a panel of top Chinese health experts (n = 70), who were requested to identify 20 health problems that, in their judgment, were most important and preventable. We also compared the results with evidences from epidemiological studies on disease-specific mortalities and disability-adjusted life years.
Results. Consensus was reached after the second-round survey. The final agreed-upon 20 most important and most preventable health problems included 9 noncommunicable diseases, 4 communicable diseases, 2 unhealthy behaviors, and 2 forms of environmental pollution, plus depression, road injury, and contamination of food with pesticides, antibiotics, and hormone residues. The results are supported by relevant epidemiological studies in China.
Conclusions. The 20 most important and most preventable health problems in China for the next 20 years, agreed upon by a panel of top Chinese health experts, should be taken into consideration in national policymaking.
During the past 3 to 4 decades, China has experienced rapid economic development. Despite the obvious advantages of this development, for many people it has also resulted in unhealthy lifestyles and mental health problems, together with serious environmental problems including severe air pollution.1,2 Over the same period, the total fertility rate and child mortality have fallen sharply, and China has become the fastest-aging country in the world, putting enormous pressure on health care and social welfare.3 Because of these lifestyle changes, environmental deterioration, and population aging, China is facing a great challenge from noncommunicable diseases (NCDs), which now account for 87% of all deaths.4 The increased incidence of NCDs has had a major economic impact and has challenged the health care system and all of society; total mortality has leveled off after many years of falling.2,5 From 2004 to 2016, the government invested heavily in disease control and prevention, but the overall incidence of notifiable infectious diseases has increased rather than decreased.6 Emerging communicable diseases such as severe acute respiratory syndrome continue to threaten the country and occasionally result in public crises.7
As a consequence, improving health in China has become one of the top strategies for national development.8,9 Although the main focus for achieving this aim has been established, with “prevention first” as the priority, the operational plan in terms of which diseases to prevent and which causes to control remains unclear. To set specific goals and better allocate limited resources, China needs to identify and establish priorities.
To this end, we conducted the present study among top Chinese academics in health to identify and to rank the 20 most important and most preventable health problems for the next 20 years in China.
METHODS
The study used a modified Delphi method to reach consensus on the 20 most important and most preventable health problems.5,10 We established a working group of experts to design the study, to develop the Delphi survey instrument, and to analyze and report the results. We agreed that at least 2 rounds of the Delphi survey should be conducted to achieve a consensus among the panelists. The decision whether to undertake further rounds of the survey depended on whether the result from the completed rounds represented a consensus.
Participants
We invited all academicians (n = 116) in the Department of Medicine of the Chinese Academy of Engineering, 1 of the 2 foremost academic institutions in China, to take part in the study. We also invited all candidate academicians in the 2015 election for the field of medicine (n = 60). In addition, 29 nonacademician experts were recommended by the working group and were invited to take part in the study.
First-Round Survey
The first-round instrument comprised the informed consent form, the instructions, and the questionnaire. The questionnaire was composed of 3 sections. The first section included questions on the basic demographics and professional discipline of the participant. The second section was a list of 106 diseases and health-related issues to be selected by the panelist; these were classified into 9 groups:
communicable diseases (39 items),
NCDs (23 items),
mental and neurological disorders (8 items),
unhealthy behaviors (5 items),
diseases in women and children (8 items),
injuries (5 items),
nutrition and food safety (4 items),
environmental and occupational health issues (12 items), and
endemic diseases (2 items).
Participants were also presented with 5 blank areas in which they could suggest other possible health problems. The third section asked the panelists to score the importance and preventability of each of the health problems.
The instrument was Web based and captured data from the invited panelists; in some cases, we mailed panelists a hard copy of the instrument. To initiate the study, all eligible panelists were invited by an official e-mail from the Department of Medicine of the Chinese Academy of Engineering; in this e-mail, they were fully informed about the aims of the survey.
The first-round survey began on September 15, 2015, and was completed on November 30, 2015. All participants were asked to identify the 20 health problems that they thought would be the most important, as well as the 20 most likely to be preventable, in the next 20 years in China. To do this, they could choose from the list provided and could also add new items. The total number of health problems identified had to be exactly 20 for the questionnaire to be accepted. Panelists were asked to rate 2 aspects for each health problem: the degree of importance and the degree of preventability. Panelists were also asked to rate their familiarity with each health problem. We measured all degrees of importance, preventability, and familiarity by assigning a score from 0 (least important, preventable, or familiar) to 9 (most important, preventable, or familiar).
Second-Round Survey
The second-round survey took place between April 15, 2016, and July 31, 2016. We invited for the second round only those participants who had completed the first round. The same information about the participant was requested as in the first round, except for demography and professional discipline. Panelists were also provided with the results from the first round on the 20 most important and most preventable health problems. We cut the list of health problems by 74 to include only those chosen by at least 10% of panelists in the first round. As in the first round, panelists were asked to identify exactly 20 health problems that they thought were the most important and the most preventable. In both rounds, we sent up to 3 reminders in cases of nonresponse.
Data Analysis
We defined the selection rate for a specific health problem as the percentage of panelists who selected it. We calculated median scores and interquartile ranges for the degrees of importance and of preventability, respectively, as measures of central tendency and dispersion.
To assist in selecting the final top 20 health problems, we calculated a composite index for each health problem selected by the panelist according to the following formula:
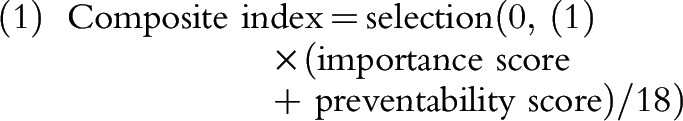 |
The formula took into consideration the panelists’ personal prioritization on each health problem, using the sum of the panelists’ importance and preventability scores. Because the possible highest total score of importance and preventability is 18 (i.e., 9+9), we divided the sum of importance score and preventability score by 18 so the results would be between 0 and 1.
We further weighted the selection rate, the degree of importance, the degree of preventability, and the composite index by the familiarity of the panelists with each selected health problem. To do this, we simply multiplied these measures by the score of familiarity divided by 9. Then, we prioritized the health problems by the weighted median composite index and selected the top 20 health problems.
We evaluated the stability of consensus on the basis of the consistency of response between 1 round and the next.10 In the present study, we considered the stability of consensus to be achieved if at least half of the panelists had selected the health problem in their list of the top 20 health problems identified, and there was minimal change in the selections from the previous round.11
In addition, we calculated Kendall’s coefficient of concordance (W) to measure the agreement among the panelists in terms of the health problems selected and their importance, preventability, and composite index.12,13 We performed all analyses with the statistical software package SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Out of the 205 invited experts, 95 agreed to participate and completed the first-round survey (a response rate of 46%). Respondents were mostly male (82%), and the mean age was 63.6 years. Respondents were working mainly in the fields of public health (21%), clinical medicine (42%), and medical research (35%). They had been engaged in their professional discipline for more than 15 years (Table 1). Nonrespondents were older (mean age = 69.1 years) and, hence, had been engaged in their professional disciplines for longer than respondents. Other characteristics such as gender, professional field, and membership in the Chinese Academy of Engineering were similar between respondents and nonrespondents (Table A, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 1—
Demographic Characteristics of Expert Panelists Participating in the 2 Rounds of the Survey: China, 2015–2016
| Panelist Characteristics | Round 1, % or Mean ±SD (n = 95) | Round 2, % or Mean ±SD (n = 70) |
| Male gender | 82 | 83 |
| Age, y | 63.6 ±11.9 | 64.0 ±12.2 |
| Invitation sources | ||
| Academicians from Chinese Academy of Engineering | 54 | 56 |
| Academician candidates, 2015 election to the field of medicine | 27 | 23 |
| Invited experts | 19 | 21 |
| Current professional field | ||
| Public health | 21 | 26 |
| Clinical medicine | 42 | 40 |
| Basic medical research | 35 | 33 |
| Others | 2 | 1 |
| Time engaged in field, y | ||
| 19–30 | 42 | 40 |
| 31–40 | 34 | 34 |
| > 40 | 24 | 26 |
Of the 95 respondents to the first round, 70 also responded to the second round. The demographic characteristics of the respondents were similar between the 2 rounds (Table 1). The final panel of experts was made up of participants who responded to both rounds.
Consensus on the Top 20 Health Problems
In the first round, the survey provided participants with a list of 106 health problems from which to select. Panelists selected 101 health problems from the list and added another 24. Thus, 125 health problems were identified in total (Table B, available as a supplement to the online version of this article at http://www.ajph.org).
In the second round, 19 health problems from the first-round top 20 remained in the top 20, with some differences in rankings. Only 1 item, stomach cancer, was removed from the top 20; it was replaced by obesity and overweight. All the final top 20 health problems had been identified by at least half of the panelists who completed both rounds. The final top 20 were the same health problems, whether judged by selection rate, degree of importance, degree of preventability, or composite index, although they did not have the same ranking in each perspective. On the basis of this result, we considered that consensus had been reached and discontinued the survey after round 2.
Table 2 lists the final 20 most important and most preventable health problems, in rank order by composite index. We categorized them into NCDs (9 items), communicable diseases (4 items), unhealthy behaviors (2 items), environmental and occupational health issues (2 items), mental and neurological disorders (1 item), nutrition and food safety (1 item), and injuries (1 item). Rankings by selection rate, importance, and preventability are also shown in Table 2.
TABLE 2—
Final 20 Most Important and Most Preventable Health Problems Identified: China, 2015–2016
| Selections Rate |
Importance Score |
Preventability Score |
Composite Index |
||||||
| Health Problem | Domain Class | % | Rank | Median (IQR) | Rank | Median (IQR) | Rank | Median (IQR) | Rank |
| Diabetes mellitus | NCD | 83.3 | 1 | 7.20 (2.50) | 1 | 6.35 (2.70) | 2 | 0.74 (0.27) | 1 |
| Hypertension | NCD | 82.7 | 2 | 7.20 (2.50) | 1 | 6.30 (2.40) | 3 | 0.72 (0.26) | 2 |
| CHD/MI | NCD | 81.6 | 3 | 7.20 (2.50) | 1 | 5.60 (3.20) | 5 | 0.69 (0.26) | 3 |
| Air pollution | EO | 74.3 | 6 | 6.80 (2.50) | 4 | 6.30 (2.40) | 3 | 0.64 (0.24) | 4 |
| Lung cancer | NCD | 75.9 | 4 | 6.40 (3.20) | 5 | 4.90 (3.10) | 11 | 0.58 (0.28) | 5 |
| Stroke | NCD | 75.4 | 5 | 6.40 (3.30) | 5 | 5.60 (3.40) | 5 | 0.57 (0.30) | 6 |
| Smoking | UB | 65.4 | 8 | 6.35 (8.10) | 8 | 7.20 (9.00) | 1 | 0.56 (0.67) | 7 |
| Hepatitis | CD | 66.0 | 7 | 6.30 (4.20) | 9 | 5.60 (4.20) | 5 | 0.53 (0.37) | 8 |
| Water pollution | EO | 63.1 | 11 | 6.40 (5.10) | 5 | 5.60 (4.40) | 5 | 0.52 (0.42) | 9 |
| HIV/AIDS | CD | 65.1 | 9 | 5.95 (4.40) | 10 | 5.50 (4.20) | 10 | 0.50 (0.30) | 10 |
| Emerging infectious diseases | CD | 63.9 | 10 | 5.60 (5.10) | 11 | 4.00 (4.30) | 17 | 0.47 (0.38) | 11 |
| Liver cancer | NCD | 60.3 | 12 | 5.60 (7.20) | 11 | 4.20 (5.60) | 14 | 0.41 (0.52) | 12 |
| Alzheimer’s disease | NCD | 57.3 | 13 | 5.60 (7.20) | 11 | 3.60 (5.40) | 18 | 0.36 (0.53) | 13 |
| Unhealthy dieta | UB | 52.0 | 15 | 5.25 (7.20) | 14 | 5.60 (7.20) | 5 | 0.36 (0.49) | 13 |
| Depression | MN | 54.9 | 14 | 4.80 (7.20) | 16 | 4.20 (6.00) | 14 | 0.35 (0.49) | 15 |
| Road injury | I | 47.7 | 18 | 4.85 (7.20) | 15 | 4.85 (7.20) | 12 | 0.33 (0.45) | 16 |
| Contamination of foodb | NF | 47.9 | 17 | 4.80 (6.40) | 16 | 4.35 (6.40) | 13 | 0.32 (0.44) | 17 |
| Obesity and overweight | NCD | 50.9 | 16 | 4.80 (7.20) | 16 | 4.20 (7.20) | 14 | 0.30 (0.49) | 18 |
| Breast cancer | NCD | 44.0 | 19 | 3.25 (6.40) | 19 | 2.45 (6.00) | 19 | 0.18 (0.38) | 19 |
| Tuberculosis | CD | 42.6 | 20 | 1.50 (6.40) | 20 | 1.50 (6.40) | 20 | 0.09 (0.34) | 20 |
Note. CD = communicable diseases; CHD/MI = coronary heart disease/myocardial infarction; EO = environmental and occupational health; I = injuries; IQR = interquartile range; MN = mental and neurological disorders; NCD = noncommunicable diseases; NF = nutrition and food safety; UB = unhealthy behaviors. All data in the table were weighted by the familiarity of the panelists with each selected health problem.
High dietary intakes of saturated fat, trans-fats, and salt, and low intake of fruits.
Contamination with pesticides, antibiotics, and hormone residues.
The Top 20 in Terms of Importance and Preventability
With regard to degree of importance, diabetes mellitus, hypertension, and coronary heart disease were tied for first; air pollution was fourth, and lung cancer, stroke, and water pollution were tied for fifth (Table 2).
In terms of preventability, smoking was ranked first, diabetes mellitus second, and hypertension and air pollution were tied for third. Coronary heart disease, stroke, hepatitis, water pollution, and unhealthy diet were tied for fifth (Table 2).
Although lung cancer was tied for fifth in importance, it was listed 11th in terms of preventability. By contrast, smoking was identified first in terms of preventability but eighth in importance.
Differences in Panelists’ Ratings by Professional Field
Comparison of the final top 20 list identified by panelists from different professional fields showed that the ranking of a particular health problem could vary by 1 to 12 places. Five health problems had differences in rankings of fewer than 5 points, 10 had differences ranging from 5 to 9 points, and the remaining 5 had differences in rankings of 10 points or more. In general, panelists from the field of public health were more likely to give unhealthy lifestyle (smoking and unhealthy diet) and road injury a higher priority; panelists from clinical medicine were more likely to prioritize NCDs such as lung cancer, breast cancer, and depression; and panelists from medical research were more likely to award emerging infectious diseases a higher rank (Table 3).
TABLE 3—
Final 20 Most Important and Most Preventable Health Problems Identified, Composite Index in Different Professional Fields: China, 2015–2016
| Public Health (n = 18) |
Clinical Medicine (n = 28) |
Medical Research (n = 23) |
||||||
| Health Problem | Domain Class | Median (IQR) | Rank | Median (IQR) | Rank | Median (IQR) | Rank | Difference in Rank Order Among Fields |
| Diabetes mellitus | NCD | 0.78 (0.22) | 2 | 0.71 (0.34) | 2 | 0.72 (0.23) | 1 | 1 |
| Hypertension | NCD | 0.80 (0.19) | 1 | 0.66 (0.26) | 3 | 0.72 (0.26) | 1 | 2 |
| CHD/MI | NCD | 0.64 (0.33) | 5 | 0.75 (0.22) | 1 | 0.64 (0.26) | 6 | 5 |
| Air pollution | EO | 0.74 (0.22) | 4 | 0.57 (0.31) | 5 | 0.68 (0.25) | 3 | 2 |
| Lung cancer | NCD | 0.58 (0.27) | 9 | 0.58 (0.27) | 4 | 0.58 (0.22) | 10 | 6 |
| Stroke | NCD | 0.59 (0.33) | 8 | 0.53 (0.31) | 6 | 0.64 (0.25) | 6 | 2 |
| Smoking | UB | 0.77 (0.24) | 3 | 0.53 (0.61) | 6 | 0.38 (0.53) | 13 | 10 |
| Hepatitis | CD | 0.49 (0.37) | 11 | 0.41 (0.56) | 10 | 0.65 (0.23) | 4 | 7 |
| Water pollution | EO | 0.63 (0.28) | 6 | 0.37 (0.51) | 12 | 0.61 (0.19) | 8 | 6 |
| HIV/AIDS | CD | 0.37 (0.51) | 14 | 0.48 (0.38) | 8 | 0.60 (0.22) | 9 | 6 |
| Emerging infectious diseases | CD | 0.39 (0.41) | 13 | 0.35 (0.49) | 14 | 0.65 (0.18) | 4 | 10 |
| Liver cancer | NCD | 0.22 (0.37) | 18 | 0.40 (0.41) | 11 | 0.58 (0.22) | 10 | 8 |
| Alzheimer’s disease | NCD | 0.20 (0.32) | 19 | 0.31 (0.52) | 15 | 0.51 (0.24) | 12 | 7 |
| Unhealthy dieta | UB | 0.61 (0.23) | 7 | 0.28 (0.43) | 17 | 0.00 (0.40) | 19 | 12 |
| Depression | MN | 0.16 (0.28) | 21 | 0.42 (0.38) | 9 | 0.37 (0.49) | 15 | 12 |
| Road injury | I | 0.54 (0.43) | 10 | 0.09 (0.37) | 21 | 0.13 (0.39) | 18 | 11 |
| Contamination of foodb | NF | 0.31 (0.43) | 16 | 0.29 (0.36) | 16 | 0.38 (0.43) | 13 | 3 |
| Obesity and overweight | NCD | 0.49 (0.64) | 11 | 0.21 (0.45) | 19 | 0.00 (0.41) | 19 | 8 |
| Breast cancer | NCD | 0.19 (0.39) | 20 | 0.36 (0.52) | 13 | 0.00 (0.23) | 19 | 7 |
| Tuberculosis | CD | 0.32 (0.43) | 15 | 0.00 (0.33) | 22 | 0.00 (0.32) | 19 | 7 |
Note. CD = communicable diseases; CHD/MI = coronary heart disease/myocardial infarction; EO = environmental and occupational health; I = injuries; IQR = interquartile range; MN = mental and neurologic disorders; NCD = noncommunicable diseases; NF = nutrition and food safety; UB = unhealthy behaviors. All data in the table were weighted by the familiarity of the panelists with each selected health problem.
High dietary intake of saturated fat, trans-fats, and salt, and low intake of fruit.
Contamination with pesticides, antibiotics, and hormone residues.
Differences Between Round 1 and Round 2
In the first round, Kendall’s coefficient of concordance (W) was 0.261, 0.269, 0.256, and 0.299 for the selection rate, degree of importance, degree of preventability, and composite index, respectively; in the second round, it was 0.460, 0.463, 0.430, and 0.608, respectively.
To understand whether the better centrality in the selection of health problems in round 2 than in round 1 was due to loss of panelists, Table 4 compares the selection rates of the top 20 health problems between round 1 and round 2 for the same panelists, and between panelists for the same round (i.e., the first round). It clearly shows that the selection rate for all top 20 health problems increased from round 1 to round 2, by a mean of 24%, and that these increases were entirely due to the methodology because the selection profiles of the 2 panels showed good agreement (Table 1). Furthermore, Table 4 shows that the final selection rate for each top 20 health problem was 50% or greater.
TABLE 4—
Top 20 Health Problems Selected by Panelists, and Proportions of Panelists Who Selected Them, by Panel and Round of Survey: China, 2015–2016
| Final Panel (n = 70) |
|||||
| Health Problem | Initial Panel (n = 95), % (Rank) | Round 1 % (Rank) | Round 2 % (Rank) | Difference Between 2 Panels, % | Difference Between 2 Rounds, % |
| Diabetes mellitus | 73 (1)a | 69 (2)a | 100 (1) | −4 | +31 |
| CHD/MI | 58 (7) | 56 (6) | 97 (2) | −2 | +41 |
| Hypertension | 60 (6) | 54 (8) | 96 (3) | −6 | +41 |
| Lung cancer | 73 (1) | 71 (1) | 93 (4) | −2 | +21 |
| Stroke | 56 (8) | 53 (10) | 91 (5) | −3 | +39 |
| Air pollution | 47 (12) | 49 (12) | 90 (6) | +2 | +41 |
| Emerging infectious diseases | 65 (4) | 69 (2) | 84 (7) | +4 | +16 |
| HIV/AIDS | 62 (5) | 64 (5) | 80 (8) | +2 | +16 |
| Hepatitis | 67 (3) | 67 (4) | 79 (9) | 0 | +11 |
| Water pollution | 37 (19) | 40 (18) | 77 (10) | +3 | +37 |
| Liver cancer | 56 (8) | 53 (10) | 73 (11) | −3 | +20 |
| Smoking | 54 (10) | 56 (6) | 71 (12) | +2 | +16 |
| Depression | 53 (11) | 54 (8) | 70 (13) | +1 | +16 |
| Alzheimer’s disease | 46 (13) | 41 (16) | 70 (13) | −5 | +29 |
| Contamination of fooda | 43 (15) | 44 (14) | 61 (15) | +1 | +17 |
| Road injury | 41 (17) | 41 (16) | 59 (16) | 0 | +17 |
| Unhealthy dietb | 37 (19) | 39 (19) | 59 (16) | +2 | +20 |
| Obesity and overweight | 33 (23) | 29 (26) | 59 (16) | −4 | +30 |
| Breast cancer | 42 (16) | 43 (15) | 54 (19) | +1 | +11 |
| Tuberculosis | 45 (14) | 46 (13) | 50 (20) | +1 | +4 |
| Mean | –0.5 | 23.7 | |||
Note. CHD/MI = coronary heart disease/myocardial infarction.
Contamination with pesticides, antibiotics, and hormone residues.
High dietary intake of saturated fat, trans-fats, and salt, and low intake of fruit.
To determine whether our results were affected by removal of the 74 health problems in round 1 that were chosen by fewer than 10% of panelists and, if so, by how much, we counted the total number of choices (1 health problem = 1 choice) made by the panelists in round 1, and the numbers of choices for each health problem that were reselected, not reselected, and not able to be reselected (having been removed from the list after round 1) in round 2. Among all 1390 choices that the final panel made in round 1, 56% (n = 776) were reselected, 31% (n = 431) were not reselected, and 13% (n = 183) were not able to be reselected in round 2.
DISCUSSION
This study identified the 20 most important and most preventable health problems for the next 20 years in China, using a modified Delphi method, after 2 rounds of consultation by a panel composed of distinguished academic experts in health in China.
Among the final top 20 health problems, 14 comprised NCDs and the major risk factors that contribute to NCDs, including unhealthy behaviors (smoking and unhealthy diet) and environmental pollution (air and water pollution). Four of the final top 20 health problems were communicable diseases, 1 was a food safety issue, and 1 was road injuries.
According to the National Health Statistics in 2015, the diseases identified in the top 20 health problems accounted for 61% of total deaths in China.14 Based on the Global Burden of Disease Study 2010, the diseases included in the top 20 health problems accounted for 36% of the total lost disability-adjusted life years (DALYs) in China, and were risk factors for 45% of lost DALYs.15 The results indicate that the experts’ choices show good agreement with the national statistics and are supported by objective evidences (Table C, available as a supplement to the online version of this article at http://www.ajph.org). Meanwhile, we still noticed an apparently large inconsistency between the experts’ rankings and the rankings on major causes of death or lost DALYs. The main reason is because the latter ranks only the importance of the problems by a certain objective standard (e.g., death), whereas the former ranks both importance and preventability. In addition, when the experts scored importance, they may also have considered other characteristics of the health problem, such as the number of people affected, its importance in the future, and their personal beliefs regarding its consequences. This inconsistency also highlights the need to include the opinions of experts in decision-making, rather than relying on health statistics alone.
The ranking of the top 20 health problems by composite index indicates that the panelists prioritized health problems where intervention could prevent disease worsening or the development of other serious conditions (e.g., diabetes mellitus and hypertension are listed as the top 2, above diseases such as coronary heart disease, stroke, and cancers), and focused more on NCDs than on infectious diseases. The upstream risk factors for NCDs—such as air and water pollution, smoking, unhealthy diet, and food contamination with pesticides, antibiotics, and hormone residues—were all among the top 20 health problems, along with major chronic diseases including coronary heart disease, stroke, and lung, liver, and breast cancer.
National surveys estimate that China has over 200 million adults with hypertension and more than 100 million with diabetes mellitus, giving China the greatest numbers of such patients in the world.16,17 It is thus not a surprise that diabetes mellitus and hypertension were listed as first and second among all health problems, but it is interesting that hypertension was not chosen as the top priority, given that the number of patients is more than twice that of diabetes mellitus. The same can be seen with stroke and coronary heart disease: the Chinese population experiences 3 to 5 times as many strokes as cases of acute coronary syndrome, but coronary heart disease was ranked as the third priority and stroke the sixth. The explanations for these differences are not clear, but they may be related to differences in participants’ perspectives on the consequences of these diseases.15,18–21 A similar explanation might account for why some diseases that cause significant loss of life or loss of DALYs (e.g., musculoskeletal disorders, chronic obstructive pulmonary disease, falls, stomach cancer, esophageal cancer, and sense organ diseases)15 were not included in the top 20 health problems. Comparison of the top 20 health problems with the major causes of death and of lost DALYs should inform future health communications and policy recommendations (Table C).
Although objective data such as major causes of death, major causes of loss of DALYs, incidence, prevalence, and mortality of diseases and risk factors are all important in health policymaking, it is still difficult to compare diseases and risk factors, upstream and downstream risk factors, or physical and mental conditions to decide which is more important. This is because their impacts on individuals’ health and on society are different and people’s values are different. Thus, collating the priorities of individuals with professional knowledge and expertise and forming a consensus by objective methods is a useful and important practice to inform decision-making in a modern society, and the Delphi technique has become a useful tool for decision-making in a range of disciplines.22–25
In our study, at least 30% of option choices were changed in round 2 by panelists after receiving the feedback of results from round 1, and concordance coefficients nearly doubled, indicating that the modified Delphi technique successfully focused the panelists’ choices.
In addition, the study showed that the ranking of the top 20 health problems was different among panelists with different professional backgrounds, although they identified the same top 20 health problems. For example, smoking was ranked third by panelists in public health but sixth by those in clinical medicine and 13th by those in medical research. Depression was ranked ninth by panelists in clinical medicine but 15th by those in medical research and 21st by those in public health. Emerging infectious diseases were ranked fourth by panelists in medical research but 13th by those in public health and 14th by those in clinical medicine. These results reemphasize the importance of panelist selection when using the Delphi technique.
There were some limitations in our study. First, the response rate to the first-round survey was low, leading to a low final response rate of 34%. This may be partly explained by a busy workload and, for some participants, inability to complete the Web-based survey because of limited Internet access. To minimize the problem, we mailed a printed copy of the questionnaire to those who requested it (19%). Our analysis (Table A) showed that the responders and nonresponders were similar in gender and professional background, but nonresponders were 5.5 years older than responders and their time engaged in the field was 4.4 years longer. Further analysis showed that between age groups, the 20 most important and most preventable health problems identified were exactly the same, and the rankings for each health problem differed slightly except for liver cancer (Table D, available as a supplement to the online version of this article at http://www.ajph.org). Thus, we believe that selection bias was small, if it existed, although the overall response rate was not high.
Second, to simplify the second survey we removed 74 potential options that fewer than 10% of the panelists had selected in the first-round survey, which might have forced panelists to make choices that they would not otherwise have made. However, our analyses showed that, at most, 13% of the choices could have been affected in this way. On the other hand, even if those options had not been removed from the list, there was no possibility of identifying them in the final top 20 because their selection rate in the first-round survey was so low (below 10%). Finally, as in any study using the Delphi technique, the results may vary because of changes in the panel. Our results reflected the opinions of a group of top Chinese medical and health experts and should not be interpreted as representative opinions of the field.
Conclusions
A panel of top Chinese health experts reached consensus on the 20 most important and most preventable health problems in China for the next 20 years. The results should be taken into consideration in national policymaking.
Public Health Implications
Results of the study provide useful information for prioritizing the operational tasks and help the health authorities in China to set specific goals for and allocate resources to implement a health action plan that will ultimately affect 1.3 billion people living in the most populous country in the world. Furthermore, the study offers a method and a practical case for setting health priorities for a nation or area that could be used by health policymakers from other countries.
ACKNOWLEDGMENTS
The study was sponsored by the Chinese Academy of Engineering, Beijing, China (grant 2014-ZD-09).
We thank all of the study participants for their great contribution to the study. We are also very grateful to Ruitai Shao (Department for Management of Noncommunicable Diseases, Disability, Violence and Injury Prevention, World Health Organization, Geneva, Switzerland) and Richard Smith (Ovations Chronic Disease Initiative, UnitedHealth Europe, London, UK) for their critical review and comments to on our article. We also thank Oxford PharmaGenesis Ltd, Oxford, UK, for providing editorial support free of charge.
HUMAN PARTICIPANT PROTECTION
The study protocol was reviewed and approved by the Ethics Committee of the National Institute for Communicable Diseases Control and Prevention, Chinese Center for Diseases Control and Prevention.
Footnotes
REFERENCES
- 1.Chen R, Kan H, Chen B et al. Association of particulate air pollution with daily mortality: The China Air Pollution and Health Effects Study. Am J Epidemiol. 2012;175(11):1173–1181. doi: 10.1093/aje/kwr425. [DOI] [PubMed] [Google Scholar]
- 2.Wu Y, Benjamin EJ, MacMahon S. Prevention and control of cardiovascular disease in the rapidly changing economy of China. Circulation. 2016;133(24):2545–2560. doi: 10.1161/CIRCULATIONAHA.115.008728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daar AS, Singer PA, Leah Persad D et al. Grand challenges in chronic non-communicable diseases. Nature. 2007;450(7169):494–496. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 4.Zhao Y, Smith JP, Strauss J. Can China age healthily? Lancet. 2014;384(9945):723–724. doi: 10.1016/S0140-6736(14)61292-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Health and Family Planning Commission of the People’s Republic of China. The 2015 Report of Disease Prevention and Control Progress in China. Available at: http://en.nhfpc.gov.cn/2015-06/03/c_46242_3.htm. Accessed August 4, 2017.
- 6.Yang S, Wu J, Ding C et al. Epidemiological features of and changes in incidence of infectious diseases in China in the first decade after the SARS outbreak: an observational trend study. Lancet Infect Dis. 2017;17(7):716–725. doi: 10.1016/S1473-3099(17)30227-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang L, Wang Y, Jin S et al. Emergence and control of infectious diseases in China. Lancet. 2008;372(9649):1598–1605. doi: 10.1016/S0140-6736(08)61365-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.China Copyright and Media. The Chinese Dream infuses socialism with Chinese characteristics with new energy. Available at: https://chinacopyrightandmedia.wordpress.com/2013/05/06/the-chinese-dream-infuses-socialism-with-chinese-characteristics-with-new-energy. Accessed August 4, 2017.
- 9.World Health Organization. Healthy China 2030 (from vision to action). Available at: http://www.who.int/healthpromotion/conferences/9gchp/healthy-china/en. Accessed August 4, 2017.
- 10.Rowe G, Wright G. The Delphi technique as a forecasting tool: issues and analysis. Int J Forecast. 1999;15(4):353–375. [Google Scholar]
- 11.Swanepoel E, Fox A, Hughes R. Practitioner consensus on the determinants of capacity building practice in high-income countries. Public Health Nutr. 2015;18(10):1898–1905. doi: 10.1017/S136898001400216X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sim J, Wright C. Research in Health Care: Concepts, Designs and Methods. Cheltenham, UK: Nelson Thornes; 2000. [Google Scholar]
- 13.Cross V. The same but different: a Delphi study of clinicians’ and academics’ perceptions of physiotherapy undergraduates. Physiotherapy. 1999;85(1):28–39. [Google Scholar]
- 14.National Health and Family Planning Commission of the People’s Republic of China. China’s Health and Family Planning Statistical Yearbook (2016) Beijing, China: Peking Union Medical College Press; 2017. [Google Scholar]
- 15.Yang G, Wang Y, Zeng Y et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381(9882):1987–2015. doi: 10.1016/S0140-6736(13)61097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu Y, Wang L, He J et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–959. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 17.National Health Commission of the People’s Republic of China. 2014 report on Chinese resident’s chronic disease and nutrition. Available at: http://en.nhfpc.gov.cn/2015-06/15/c_45788.htm. Accessed August 4, 2017. [DOI] [PMC free article] [PubMed]
- 18.Chen W-W, Gao R-L, Liu L-S China cardiovascular diseases report 2015: a summary. J Geriatr Cardiol. 2017;14(1):1–10. [DOI] [PMC free article] [PubMed]
- 19.He Q, Wu C, Luo H et al. Trends in in-hospital mortality among patients with stroke in China. PLoS One. 2014;9(3):e92763. doi: 10.1371/journal.pone.0092763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao D, Liu J, Wang W et al. Epidemiological transition of stroke in China. Stroke. 2008;39(6):1668–1674. doi: 10.1161/STROKEAHA.107.502807. [DOI] [PubMed] [Google Scholar]
- 21.Moran A, Zhao D, Gu D et al. The future impact of population growth and aging on coronary heart disease in China: projections from the Coronary Heart Disease Policy Model-China. BMC Public Health. 2008;8(1):394. doi: 10.1186/1471-2458-8-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spies LA, Gray J, Opollo J, Mbalinda S. Uganda nursing research agenda: a Delphi study. Int Nurs Rev. 2015;62(2):180–186. doi: 10.1111/inr.12167. [DOI] [PubMed] [Google Scholar]
- 23.Brenner M, Hilliard C, Regan G et al. Research priorities for children’s nursing in Ireland: a Delphi study. J Pediatr Nurs. 2014;29(4):301–308. doi: 10.1016/j.pedn.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Versteeg M, Du Toit L, Couper I. Building consensus on key priorities for rural health care in South Africa using the Delphi technique. Glob Health Action. 2013;6(1):19522. [DOI] [PMC free article] [PubMed]
- 25.Teeling-Smith G. Medicines in the 1990’s: experience with a Delphi forecast. Long Range Plann. 1971;3(4):69–74. [Google Scholar]


