Abstract
Rapid advances and improved networking abilities have led to the widespread adoption of technology in healthcare, especially focused on diagnostics, documentation and evaluation, or mining of data to improve outcomes. Current technology allows for rapid and accurate decision-making in clinical care decisions for individual patients, collation and analysis at different levels for administrative and financial purposes, and the ability to visualise, analyse, and share data in real time for departmental needs. The adoption of technology may help to improve efficiency and efficacy of healthcare services. Obstetric anaesthesia is a specialised area that has to address the well-being of the pregnant woman and the unborn baby simultaneously. A shift toward caesarean sections as the major mode of childbirth has led to an increased involvement of anaesthesiologists with childbirth. Decisions are often made in high pressure, time intense situations to protect maternal and foetal health. Furthermore, labour analgesia using various neuraxial and non-neuraxial techniques is being demanded by parturients frequently, and for the materno-foetal safety, risk management is the core issue. Hence, it is essential that obstetric anaesthesia teams regularly audit their outcomes to improve services and to identify potential trouble spots earlier. It may be helpful to have audit parameters displayed as visual data, rather than complex tabular and numerical data, for ease of sharing, analysis, and redressal of problem areas. We describe the design and use of an obstetric anaesthesia dashboard that we have used in our department for the past 5 years.
Key words: Anaesthesia outcomes audit, dashboard, maternal and foetal safety
INTRODUCTION
Clinical practice units, teams, and hospitals are increasingly relying on electronic medical records to collect, store, retrieve, and analyse patient-related data.[1],[2],[3],[4],[5],[6] Electronic Health or Medical Records (EHMRs) are designed to improve efficacy and efficiency of care at every point of care, across disciplines, and are no longer restricted to static data. EHMR allows for the validation and analysis of data pertaining to patient safety, outcomes, adherence to protocols or evidence-based guidelines, assessment of risk, and analysis of processes and policies pertaining to clinical care quality.[7],[8],[9] EHMR can lead to the generation of extensive data, both quantitative and qualitative, and may lead to extremely large data files for each individual. However, the purpose of the EHMR is partially lost if clinicians are unable to visualise, retrieve, synchronise, and examine more closely relevant pieces of information in real time to help with optimal patient care. Technical advances in computing and networks have improved the capability to synchronise patient data and perform clinically meaningful problem-solving analysis in real time. The integration of patient information into a dashboard display may help to assess information more rapidly, streamline processes, reduce response times, and reduce errors of oversight in clinical care.[10],[11],[12],[13],[14]
Obstetric anaesthesia is a specialised practice within anaesthesia that has to simultaneously monitor the health of two or sometimes three individuals—the pregnant mother and the growing foetus or baby. The practice of obstetric anaesthesia involves the evaluation of the pregnant mother including risk assessment for both the mother and foetus, a multidisciplinary approach that involves close liaison with the obstetrician, internist, neonatologist, and other specialties of care. The obstetric anaesthesiologist has to simultaneously consider several parameters including physiological parameters for maternal and foetal well-being assessment, maternal morbidity and their potential impact on foetal well-being, interventions to deliver the baby, short-term and long-term impact on the new born babies, short-term and long-term impact on the well-being of the mother, and potential impact on reproductive health and subsequent pregnancy for the mother. These assume particular significance in a country like India that has a large number of childbirths by caesarean sections and significant maternal morbidity with a potential for maternal, foetal, neonatal, and infant mortality.[15]
In this narrative review, we discuss the development and use of an obstetric anaesthesia dashboard with particular focus on clinical risk assessment and management that not only provide optimal outcomes but also serves as a dynamic quality enhance tool for each anaesthetic rendered during pregnancy.
PERINATAL HEALTH AND OBSTETRIC ANAESTHESIA IN INDIA
Maternal mortality rates remain relatively high in India although there is a declining trend in recent years.[15] A significant proportion of pregnant women in India are affected by various maternal morbidities, especially undernourishment, anaemia, hypertensive disorders of pregnancy, and diabetes. These maternal morbidities affect maternal health, the potential for a normal, safe childbirth and the well-being of the growing foetus as well as new born babies. The shift toward institutionalised perinatal care has resulted in a larger proportion of women receiving specialised childbirth care including caesarean sections and assisted vaginal deliveries, options for painless or pain managed childbirth, and improved neonatal care, which has helped in better maternal, neonatal, and infant well-being. The National Family Health Survey-4 (NFHS-4) from India (2015-16) reported that infant mortality rates reduced from 57 (NFHS-3 done in 2005-06) to 41 per 1,000 live births.[15] The NFHS-4 also reported an increasing uptake of antenatal services compared to NFHS-3.[15] The proportion of women who had at least four antenatal care visits increased to 51.2% from the 37.0% reported in NFHS-3. Institutional births increased from 38.7% to 78.9% and childbirths by caesarean sections increased to 17.2% from the 8.5% during the same period.[15] The maternal mortality rates (per 100,000 live births) have also shown a decline from 254 in 2004-06 to 167 in 2011-13.[16]
The potential to involve obstetric anaesthesiologists earlier in the childbirth planning process is a benefit of institutional deliveries. Obstetric anaesthesiologists can be involved during antenatal care to develop an individualised childbirth plan that considers the maternal and foetal well-being. However, several challenges remain for the provision of optimal anaesthesia care, including late referrals for emergency childbirth, and incomplete documentation or lack of access to prior medical records.
Improvements in perinatal outcomes involve each discipline associated with pregnancy and childbirth auditing and evaluating processes, procedures, and outcomes pertaining to their disciplines. The audit can help to identify problem areas and to develop strategies to address specific problems. The audit has several other benefits including the ability to share information within the obstetric anaesthesia team and across other disciplines involved with childbirth, to monitor processes and outcomes in real time, and to evaluate trends in care indicators over a longer period of time.
THE USE OF DASHBOARDS TO AID INTERPRETATION OF DATA
There is an increasing recognition of quality metrics as indicators of care outcomes. Although a vast variety of data can be collected, quality metrics prioritise and focus on important indicators that can influence the process and outcomes of care. However, evaluation of these metrics may be time intensive and may require extensive chart reviews to collect pertinent information. Dashboards are increasingly used to provide data, even in real time, on quality metrics.[10],[11],[12],[13],[14] Dashboards provide a user interface that can be used to retrieve and analyse, in a single screen, information pertinent to the clinical care of a single patient.[10],[11],[12],[13],[14] Dashboards can also help to improve clinical decision-making by retrieving and presenting scattered medical information of patients in a single screen, in real time, enhancing the competency, efficacy, and efficiency of decision-making and reducing potential for errors by oversight or missed information.[10],[11],[12],[13],[14] Dashboards also provide an easily accessible and interpretable visual interface that optimises clinical decision-making.[10],[11],[12],[13],[14] These benefits of dashboards have led to the development and deployment of dashboards in several areas of patient care including intensive care units.[10],[11],[12],[13],[14]
Visual analytics are generally used in healthcare to interpret data related to clinical care, scientific research, and financial or administrative data.[17],[18],[19],[20],[21],[22] Visual analytics have been extensively used to understand data pertaining to clinical care including blood transfusion, medication alerts, and compliance to protocols, collation, and integration of data from multiple EHMRs, visualising outcomes data and enhancing healthcare education.[23],[24],[25],[26],[27],[28],[29],[30] Anaesthesia Information Management Systems with user interface usability are widely used to generate automated electronic anaesthesia records.[31],[32],[33]
The concept of a dashboard can also be applied to evaluate quality metrics for the performance of a particular clinical unit focused on metrics pertaining to quality of patient care. In this instance, the dashboard can be designed to provide information pertaining to workflow processes, bed occupancy, transition or change from one procedure to another (e.g., from a local or regional anaesthesia to general anaesthesia, or from a planned normal vaginal delivery to an emergency caesarean section), response times to specific emergencies, and even adherence to clinical management protocols. The dashboard for a unit can thus provide an overall or larger picture of the quality metrics for the efficacy and efficiency of a department beyond information on individual patients. These metrics can provide early warning systems for departments or unit to revisit and address any deficiencies or problems in clinical patient care.
The concept of departmental performance assessment or evaluation is not new. Most, if not all, departments perform regular reviews at different intervals. Some may review on a weekly basis and some on a monthly, quarterly, half yearly, or even on an annual basis. The inability to identify problems in real time is a disadvantage of reviews at later dates. This delay may impact on the quality of patient care in the interim. The advantage of a dashboard is the ability to audit in real time and to have the results accessible to all pertinent members in a visual interface and at a single central location. Additionally, the use of a departmental performance dashboard can help to highlight specific areas of concern. These areas can be further examined in detail by reviewing appropriate charts and process algorithms.
ADAPTING THE DASHBOARD CONCEPT TO AUDIT AN OBSTETRIC ANAESTHESIA UNIT
We designed and implemented a simple user-friendly dashboard to provide real-time information to audit the performance of a dedicated obstetric anaesthesia unit in an advanced tertiary care perinatal institute in South India. We focused on few areas pertinent to improved patient care for the development of quality metrics that included around 80 anaesthesia-related variables and subvariables [Tables 1–4]. These included information on labor analgesia, childbirth modes including caesarean sections and assisted vaginal delivery, anaesthesia-related complications and transition from one mode of anaesthesia to another, and use of general anaesthesia and administrative data pertinent to improved patient care. We developed three cutoff criteria for each quality metric—a normal range, mild abnormal range, and abnormal range warranting immediate redressal. The quality metrics and cutoff criteria were chosen by a literature review, review of the departmental statistics for the past 5 years and consensus after discussion with members of the unit and obstetricians at the study institute. The beauty of this unique dashboard is that it allows us to dynamically adjust the cutoffs in various color zones, depending on the performance consistency, hence the departmental standards can aim to perform better than the acceptable defined international standards.
Table 1.
Data pertaining to general statistics of the group
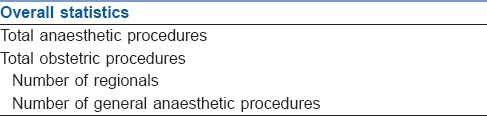
Table 4.
Administrative data collected as part of the dashboard
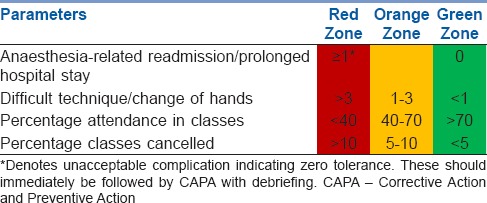
Table 2.
Parameters pertaining to childbirth and labor analgesia
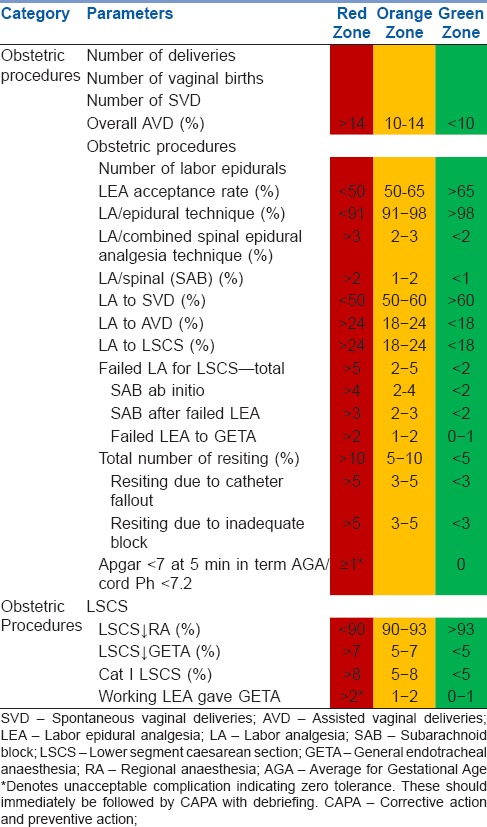
Table 3.
Parameters pertaining to anaesthesia problems
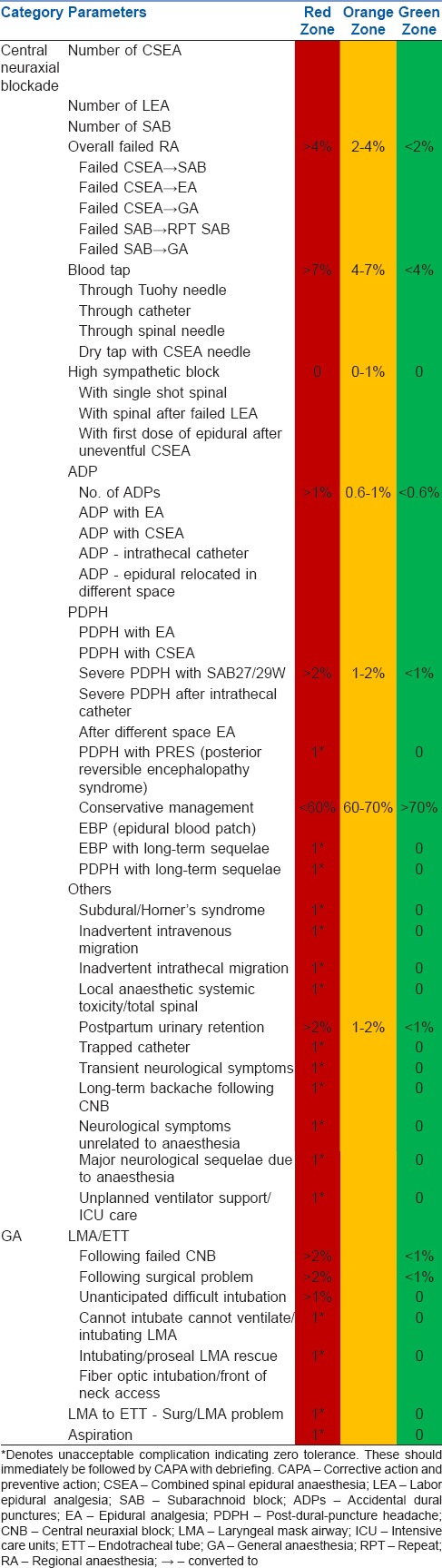
Each cutoff range was color coded for ease of visual interpretation—green for normal ranges, orange for mild abnormal ranges, and red for abnormal ranges warranting immediate action. Visual analytic computational tools help to integrate data analysis with active visual interfaces and ease navigation of large amounts of data. Visual analytics tools allow for a rapid visual interpretation of pertinent data, display of large amounts of filtered data in almost real time, and allow users to rapidly identify areas of concern that have to explore further in depth. An effective visual dashboard should display critical information on a single screen, have sparse graphical icons, display context in abbreviated forms, and use different colors and color intensities rather than different hues of the same color.[18],[19],[20],[34],[35],[36]
We created the visual dashboard in MS Excel and placed it in a central location easily accessible by all members of the obstetric anaesthesia team. All parameters are reviewed immediately after an adverse event. Otherwise, the data are reviewed when any parameter enters the amber zone. The excel sheet is entered on a daily basis. Monthly data presentation and discussion with team is mandatory. The dashboard presented information in real time and by month and allowed for comparisons across months and years.
We found several advantages or benefits with the use of the dashboard. The dashboard allowed us to interpret information in almost real time shortening the response time to issues. The visual interface and color codes allowed us to immediately focus on areas of high concern and work out strategies to address those. For example, the dashboard allowed all members to have a visual interpretation on the success or conversion rates from labor analgesia counseling, to have an almost real-time visual interpretation and discuss with the obstetrics team if the rates of caesarean sections were increasing, to identify in almost real times changes in rates of transition from one mode of anaesthesia to another, and overall complication rates across the department. The dashboard also allowed us to perform a focused chart review to identify, study, and troubleshoot problems. The dashboard allowed us to share information with all team members in almost real time and to solicit comments, suggestions, and strategies from all team members. Particularly, the dashboard dynamic review audit has helped the department to think innovatively and reduce common preventable causes of epidural catheter resiting for labor analgesia patients, reduced the incidence of wet taps—PDPH, lead to newer innovative methods to reduce bloody taps, reduced failed regionals for emergency caesarean sections, anticipate and minimise difficult intubations to name a few. The dashboard also made comparisons between months and previous years easier. We chose to use MS Excel over other traditional relational databases since it is widely available and relatively easier to use. We did not have to invest additional resources to train personnel or to obtain specialized software or statistical expertise for this purpose.
SUMMARY
There is increasing recognition that perinatal health outcomes in India can only be improved by a multidisciplinary approach and a paradigm shift from an approach focused only on an obstetrics-pediatrician care axis. Several clinical disciplines including intensivists, radiologists, nutritionists, and anaesthesiologists are actively involved in care for each pregnant woman. The role of the obstetric anaesthesiologist is gaining more importance as institutional deliveries and competence, acceptance, and use of caesarean sections is increasing. The expanding role also necessitates the development and deployment of appropriate quality checks and audit processes with an aim to improve patient care and safety, increase efficiency, optimize resource allocation and utilisation, and enhance clinical, departmental, and organisational decision-making. The use of a simple yet pertinent dashboard can help greatly to optimise performance of obstetric anaesthesia teams in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kheterpal S, Healy D, Aziz MF, Shanks AM, Freundlich RE, Linton F, et al. Incidence, predictors, and outcome of difficult mask ventilation combined with difficult laryngoscopy: A report from the multicenter perioperative outcomes group. Anesthesiology. 2013;119:1360–9. doi: 10.1097/ALN.0000435832.39353.20. [DOI] [PubMed] [Google Scholar]
- 2.Dutton RP. Registries of the anesthesia quality institute. Int Anesthesiol Clin. 2014;52:1–4. doi: 10.1097/AIA.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 3.Kheterpal S. In the land of the blind, the one-eyed man is king. Anesthesiology. 2014;120:523–5. doi: 10.1097/ALN.0000000000000123. [DOI] [PubMed] [Google Scholar]
- 4.Wolfe PJ. Making sense of big data. Proc Natl Acad Sci U S A. 2013;110:18031–2. doi: 10.1073/pnas.1317797110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costa FF. Big data in biomedicine. Drug Discov Today. 2014;19:433–40. doi: 10.1016/j.drudis.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 6.Jamoom E, Beatty P, Bercovitz A, Woodwell D, Palso K, Rechtsteiner E. Physician adoption of electronic health record systems: United States, 2011. NCHS Data Brief. 2012;98:1–8. [PubMed] [Google Scholar]
- 7.Kudyba S. Healthcare Informatics: Increasing Efficiency and Productivity. New York: Taylor Francis; 2010. [Google Scholar]
- 8.Stead WW, Searle JR, Fessler HE, Smith JW, Shortliffe EH. Biomedical informatics: Changing what physicians need to know and how they learn. Acad Med. 2011;86:429–34. doi: 10.1097/ACM.0b013e3181f41e8c. [DOI] [PubMed] [Google Scholar]
- 9.Murdoch TB, Detsky AS. The inevitable application of big data to health care. JAMA. 2013;309:1351–2. doi: 10.1001/jama.2013.393. [DOI] [PubMed] [Google Scholar]
- 10.Effken JA, Loeb RG, Kang Y, Lin ZC. Clinical information displays to improve ICU outcomes. Int J Med Inform. 2008;77:765–77. doi: 10.1016/j.ijmedinf.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Egan M. Clinical dashboards: Impact on workflow, care quality, and patient safety. Crit Care Nurs Q. 2006;29:354–61. doi: 10.1097/00002727-200610000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Effken J, McEwen M, Vincent D, Shea K, Garcia-Smith D, Youngmi K. Application and evaluation of the ecological psychology approach to instructional design (EPAID) J Asynchronous Learn Netw. 2009;13:41–56. [Google Scholar]
- 13.Khemani S, Patel P, Singh A, Kalan A, Cumberworth V. Clinical dashboards in otolaryngology. Clin Otolaryngol. 2010;35:251–3. doi: 10.1111/j.1749-4486.2010.02143.x. [DOI] [PubMed] [Google Scholar]
- 14.Wells B. Clinical dashboard: CEOs see quality data as critical part of reviewing personnel, hospital performance. Computerworld. 2009;43:28–31. [Google Scholar]
- 15.National Family Health Survey 4, India. [Last accessed on 2018 Mar 18]. Available from: http://www.rchiips.org/NFHS/pdf/NFHS4/India.pdf .
- 16.National Institution for Transforming India Aayog. National Institution for Transforming India. [Last accessed on 2018 Mar 18]. Available from: http://www.niti.gov.in/content/maternal-mortality-ratio-mmr-100000-live-births .
- 17.Ola O, Sedig K. The challenge of big data in public health: An opportunity for visual analytics. Online J Public Health Inform. 2014;5:223. doi: 10.5210/ojphi.v5i3.4933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barton D, Court D. Making advanced analytics work for you. Harv Bus Rev. 2012;90:78–83, 128. [PubMed] [Google Scholar]
- 19.Kang YA, Görg C, Stasko J. How can visual analytics assist investigative analysis? Design implications from an evaluation. IEEE Trans Vis Comput Graph. 2011;17:570–83. doi: 10.1109/TVCG.2010.84. [DOI] [PubMed] [Google Scholar]
- 20.Gillespie G. Getting a visual on health analytics. Health Data Manag. 2014;22:39–42. [PubMed] [Google Scholar]
- 21.Blount M, Ebling MR, Eklund JM, James AG, McGregor C, Percival N, et al. Real-time analysis for intensive care: Development and deployment of the artemis analytic system. IEEE Eng Med Biol Mag. 2010;29:110–8. doi: 10.1109/MEMB.2010.936454. [DOI] [PubMed] [Google Scholar]
- 22.Kohn MS, Sun J, Knoop S, Shabo A, Carmeli B, Sow D, et al. IBM's health analytics and clinical decision support. Yearb Med Inform. 2014;9:154–62. doi: 10.15265/IY-2014-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mane KK, Bizon C, Owen P, Gersing K, Mostafa J, Schmitt C, et al. Patient electronic health data-driven approach to clinical decision support. Clin Transl Sci. 2011;4:369–71. doi: 10.1111/j.1752-8062.2011.00324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mane KK, Bizon C, Schmitt C, Owen P, Burchett B, Pietrobon R, et al. VisualDecisionLinc: A visual analytics approach for comparative effectiveness-based clinical decision support in psychiatry. J Biomed Inform. 2012;45:101–6. doi: 10.1016/j.jbi.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Perer A, Sun J. MatrixFlow: Temporal network visual analytics to track symptom evolution during disease progression. AMIA Annu Symp Proc. 2012;2012:716–25. [PMC free article] [PubMed] [Google Scholar]
- 26.Goldsmith MR, Transue TR, Chang DT, Tornero-Velez R, Breen MS, Dary CC, et al. PAVA: Physiological and anatomical visual analytics for mapping of tissue-specific concentration and time-course data. J Pharmacokinet Pharmacodyn. 2010;37:277–87. doi: 10.1007/s10928-010-9160-6. [DOI] [PubMed] [Google Scholar]
- 27.Lo YS, Lee WS, Liu CT. Utilization of electronic medical records to build a detection model for surveillance of healthcare-associated urinary tract infections. J Med Syst. 2013;37:9923. doi: 10.1007/s10916-012-9923-2. [DOI] [PubMed] [Google Scholar]
- 28.Rajwan YG, Barclay PW, Lee T, Sun IF, Passaretti C, Lehmann H, et al. Visualizing central line – Associated blood stream infection (CLABSI) outcome data for decision making by health care consumers and practitioners-an evaluation study. Online J Public Health Inform. 2013;5:218. doi: 10.5210/ojphi.v5i2.4364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vaitsis C, Nilsson G, Zary N. Big data in medical informatics: Improving education through visual analytics. Stud Health Technol Inform. 2014;205:1163–7. [PubMed] [Google Scholar]
- 30.Stabile M, Cooper L. Review article: The evolving role of information technology in perioperative patient safety. Can J Anaesth. 2013;60:119–26. doi: 10.1007/s12630-012-9851-0. [DOI] [PubMed] [Google Scholar]
- 31.Wanderer JP, Rao AV, Rothwell SH, Ehrenfeld JM. Comparing two anesthesia information management system user interfaces: A usability evaluation. Can J Anaesth. 2012;59:1023–31. doi: 10.1007/s12630-012-9771-z. [DOI] [PubMed] [Google Scholar]
- 32.Nair BG, Horibe M, Newman SF, Wu WY, Peterson GN, Schwid HA, et al. Anesthesia information management system-based near real-time decision support to manage intraoperative hypotension and hypertension. Anesth Analg. 2014;118:206–14. doi: 10.1213/ANE.0000000000000027. [DOI] [PubMed] [Google Scholar]
- 33.Rose DK, Cohen MM, Wigglesworth DF, Yee DA. Development of a computerized database for the study of anaesthesia care. Can J Anaesth. 1992;39:716–23. doi: 10.1007/BF03008236. [DOI] [PubMed] [Google Scholar]
- 34.Kimball R, Ross M, Thornthwaite W, Mundy J, Becker B, editors. The Data Warehouse Lifecycle Toolkit. 2nd ed. Hoboken: Wiley; 2008. [Google Scholar]
- 35.Tufte ER. The Visual Display of Quantitative Information. 2nd ed. Cheshire: Graphics Press; 2001. [Google Scholar]
- 36.Few S. Dashboard design: Beyond meters, gauges and traffic lights. Bus Intell J. 2005;10:18–24. [Google Scholar]


