Abstract
Abnormal angiogenesis plays a major role in the development of early stage diabetic nephropathy. Vascular endothelial growth factor (VEGF) is a classical proangiogenic factor that regulates abnormal glomerular angiogenesis linked to glomerular hypertrophy in the early stage of diabetic nephropathy. Leucine-rich α-2-glycoprotein-1 (LRG1) was recently reported as a novel proangiogenic factor that is expressed in endothelial cells and promotes angiogenesis by modulating the transforming growth factor-β signaling pathway. However, the pathophysiology of LRG1 in diabetic nephropathy remains largely unknown. In the present study, we investigated intrarenal expression of the novel proangiogenic factor LRG1 in diabetic db/db mice by immunohistochemistry and a laser capture microdissection method during the development of diabetic nephropathy. We hypothesized that glomerular LRG1 expression is increased earlier than VEGF expression under conditions of pathological angiogenesis in the early stage of diabetic nephropathy. Thus, we compared glomerular expression of VEGF and LRG1 in diabetic db/db mice at 16 and 24 weeks of age. At 16 weeks, diabetic db/db mice exhibited glomerular hypertrophy with abnormal angiogenesis characterized by endothelial cell proliferation, which was concomitant with an increase in LRG1 expression of glomerular endothelial cells. However, glomerular VEGF expression was not increased at this early stage. At 24 weeks, the features of early diabetic nephropathy in db/db mice had developed further, along with further enhanced glomerular LRG1 expression. At this late stage, glomerular VEGF and fibrosis-related-gene expression was also significantly increased compared with nondiabetic db/m mice. These results suggest that LRG1 plays a pivotal role in the initial development of diabetic nephropathy by promoting abnormal angiogenesis, thereby suggesting that LRG1 is a potential preemptive therapeutic target of diabetic nephropathy.
1. Introduction
Diabetic nephropathy has become a leading cause of end stage renal disease (ESRD) worldwide [1, 2]. Despite treatment by inhibition of the renin angiotensin system and tight glycemic control, the risk of ESRD remains high. Diabetic nephropathy is diagnosed at the early stage by detection of microalbuminuria. However, early prevention of diabetic nephropathy progression remains challenging. Therefore, understanding the pathogenesis of early stage diabetic nephropathy and developing methods to control its progression are important issues.
Abnormal angiogenesis plays a major role in the development of early stage diabetic nephropathy [3, 4]. It is associated with glomerular hypertrophy and urinary albumin excretion [5–7]. Morphological changes in capillaries, such as elongation and an increased number, contribute to glomerular hypertrophy [3, 4]. In these aberrant vessels, the endothelial cells are swollen and immature, leading to increased vascular permeability [5, 8, 9].
Vascular endothelial growth factor (VEGF) is a critical regulator of abnormal angiogenesis, and its glomerular expression is involved in the pathogenesis of early stage diabetic nephropathy [10–12]. VEGF is mainly expressed in podocytes, and its receptor, vascular endothelial growth factor receptor-2 (VEGFR-2), is expressed in glomerular endothelial cells [13]. VEGF-VEGFR-2 signaling is upregulated in the diabetic glomerulus, which leads to abnormal angiogenesis and endothelial cell proliferation [14].
Very recently, Leucine-rich α-2-glycoprotein-1 (LRG1), a novel proangiogenic factor expressed in endothelial cells [15], has been reported to be involved in the development of diabetic nephropathy. Transcriptomic and in vitro analyses revealed that LRG1 in glomerular endothelial cells is one of the key regulators in the development of abnormal angiogenesis at the early stage of diabetic nephropathy [16]. However, the pathophysiology of LRG1 in diabetic nephropathy is still largely unknown.
The aim of this study was to compare glomerular expression of the classical proangiogenic factor VEGF and novel proangiogenic factor LRG1 in the early stage of diabetic nephropathy. We investigated glomerular expression of VEGF and LRG1 in a mouse model of diabetes (C57BL/KsJ-db/dbJcl; db/db mouse) and compared the changes in expression at 16 and 24 weeks of age to evaluate their association with diabetic nephropathy development.
2. Materials and Methods
2.1. Animals
This study was performed in accordance with the National Institutes of Health guidelines for the use of experimental animals. All animal experiments were reviewed and approved by the Animal Studies Committee of Yokohama City University. Male db/db mice and their age-matched nondiabetic db/m (C57BL/KsJ) littermates were purchased from CLEA Japan. The mice were housed in a controlled environment with a 12-hour light-dark cycle at 25°C. The mice were allowed free access to food and water. Mice were fed a standard diet (0.3% NaCl, 3.6 kcal/g, and 13.3% energy as fat; Oriental MF, Oriental Yeast Co, Ltd.). The mice were sacrificed at 16 and 24 weeks of age.
2.2. Biochemical Assays
Blood glucose was measured in blood obtained by tail vein puncture. Blood samples were also collected by cardiac puncture when mice were sacrificed in a fed state as described previously [17, 18]. Whole blood was centrifuged at 800 × g for 10 minutes at 4°C to separate the plasma. The resulting plasma was stored at -80°C until use. Plasma creatinine and urinary creatinine were measured using an autoanalyzer (Hitachi 7180; Hitachi, Tokyo, Japan). Urinary albumin was measured by an ELISA kit (Fujifilm Wako Shibayagi, Gunma, Japan).
2.3. Metabolic Cage Analysis
To collect urine, metabolic cage analysis was performed as described previously [19, 20]. Mice were provided with free access to tap water and fed a standard diet.
2.4. Histological and Immunohistochemical Analyses
Kidneys were fixed with 4% paraformaldehyde and embedded in paraffin. Sections of 4 μm in thickness were stained with periodic acid Schiff (PAS). Immunohistochemistry was performed as described previously [17, 18, 21]. Briefly, the paraffin-embedded sections were dewaxed and rehydrated. Antigen retrieval was performed by microwave heating. The sections were treated for 60 minutes with 10% normal goat serum in phosphate-buffered saline and blocked for endogenous biotin activity using an AVIDIN/BIOTIN Blocking kit (Vector Laboratories, CA, USA). The sections were then incubated with one of the following antibodies: (1) anti-LRG1 antibody (TAKARA, Japan) diluted at 1:100 or (2) anti-CD34 antibody (BD Pharmingen, Japan) diluted at 1:100. The sections were incubated for 60 minutes with biotinylated goat anti-rabbit IgG (Nichirei Corporation, Tokyo, Japan), blocked for endogenous peroxidase activity by incubation with 0.3% H2O2 for 20 minutes, treated for 30 minutes with streptavidin and biotinylated peroxidase (DAKO, Heidelberg, Germany), and then exposed to hematoxylin, dehydrated, and mounted. To evaluate the glomerular area, 25 glomeruli per mice were measured and averaged. All images were acquired using a BZ-9000 microscope (Keyence).
2.5. Real-Time Quantitative PCR Analysis
Total RNA was extracted from the kidney with ISOGEN (Nippon Gene, Tokyo, Japan), and cDNA was synthesized using the SuperScript III First-Strand System (Invitrogen, Carlsbad, CA, USA). Real-time quantitative PCR (RT-qPCR) was performed by incubating the reverse transcription product with TaqMan Universal PCR Master Mix and TaqMan probes (Applied Biosystems, Foster City, CA, USA), as described previously [22, 23]. mRNA levels were normalized to 18S rRNA as a control.
2.6. Laser Capture Microdissection and Subsequent RT-qPCR Analysis
Laser capture microdissection (LMD) was performed using a Leica LMD System (LMD 6000), as described previously [24, 25]. Briefly, formalin-fixed, paraffin-embedded tissues were cut into 10 μm-thick sections, mounted on polyethylene terephthalate membrane slides, and stained with hematoxylin-eosin. Next, renal glomeruli were microdissected using the LMD 6000 laser microdissection microscope. In total, 350 glomeruli were microdissected from the renal cortex per mouse. Total RNA was extracted from microdissected tissue using the RNeasy FFPE Kit (Qiagen, Hilden, Germany). cDNA was synthesized using the SuperScript III First-Strand System and applied to TaqMan RT-qPCR analysis.
2.7. Statistical Analysis
Statistical analysis was performed using GraphPad Prism software (GraphPad Software, La Jolla, CA, USA). All quantitative data are expressed as the mean ± SEM. Differences were analyzed using the unpaired Student's t-test. Values of P < 0.05 were considered as statistically significant.
3. Results
3.1. Characteristics of 16- and 24-Week-Old db/db Mice
Body weight, blood glucose, kidney weight, and the albuminuria level were significantly higher in db/db mice compared with db/m mice at 16 weeks of age (Table 1). At 24 weeks of age, body weight, blood glucose, kidney weight, and the albuminuria level were significantly increased in db/db mice compared with db/m mice. However, serum creatinine levels were identical in db/db and db/m mice at both 16 and 24 weeks of age (Table 1).
Table 1.
Body weight, blood glucose, kidney weight, plasma creatinine, and albuminuria of db/db and db/m mice.
| Variable | 16W | 24W | ||
|---|---|---|---|---|
| db/m | db/db | db/m | db/db | |
| (n=6) | (n=6) | (n=4) | (n=4) | |
| Body weight (g) | 29.2 ± 1.3 | 48.2 ± 0.7∗∗ | 37.0 ± 0.5 | 52.2 ± 4.8∗ |
| Blood glucose (mg/dl) | 134.8 ± 5.8 | >600∗∗ | 130 ± 6.7 | 574 ± 26∗∗ |
| Kidney weight (mg) | 182.3 ± 6.7 | 217.3 ± 8.5∗∗ | 225.0 ± 6.7 | 263.3 ± 5.8∗∗ |
| Plasma creatinine (mg/dl) | 0.12 ± 0.22 | 0.11 ± 0.1 | 0.08 ± 0.01 | 0.09 ± 0.02 |
| Albuminuria (mg/mg·Cr) | 0.25 ± 0.02 | 0.67 ± 0.16∗∗ | 0.04 ± 0.01 | 1.05 ± 0.53∗ |
All values are means ± SEM.
∗ P < 0.05, ∗∗P <0.01, vs db/m mice at the same age, unpaired t-test.
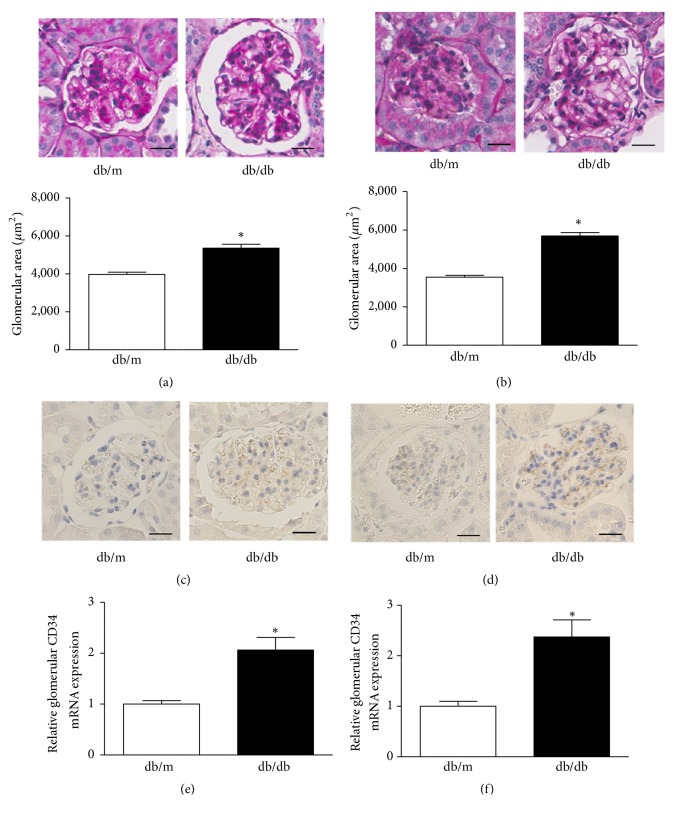
3.2. Glomerular Hypertrophy with Endothelial Cell Proliferation in db/db Mice
At 16 weeks of age, db/db mice exhibited a significantly larger glomerular area compared with db/m mice (3974.0 ± 117.6 μm2 versus 5359.0 ± 202.3 μm2, P < 0.001) (Figure 1(a)). At 24 weeks of age, the glomerular area had increased further in db/db mice compared with db/m mice (3542.2 ± 95.2 μm2 versus 5689.2 ± 182.5 μm2, P < 0.0001) (Figure 1(b)). We next examined CD34 immunostaining, as an endothelial cell marker, in the glomeruli of db/db and db/m mice. The immunostaining analysis showed enhancement of glomerular CD34 expression in db/db mice compared with db/m mice at 16 weeks of age (Figure 1(c)), and this trend became robust at 24 weeks of age (Figure 1(d)). These increases in glomerular endothelial cells indicated that abnormal angiogenesis had occurred in the kidneys of diabetic db/db mice [3, 26]. To confirm the increase of glomerular CD34 expression in db/db mice, we next examined CD34 mRNA expression in glomeruli of db/db and db/m mice using an LMD method. Glomerular CD34 mRNA expression was significantly increased in db/db mice compared with db/m mice at 16 and 24 weeks of age (Figures 1(e) and 1(f)). These results indicate that diabetic db/db mice exhibit glomerular hypertrophy with endothelial cell proliferation from the early stage of their lives, and these features are exacerbated along with aging.
Figure 1.
Glomerular hypertrophy with endothelial cell proliferation in db/db mice. Representative image of PAS staining in glomeruli of db/m and db/db mice at (a) 16 weeks and (b) 24 weeks of age. The glomerular area was increased in db/db mice at both ages (25 glomeruli per mice were measured and averaged). Values are expressed as the mean ± SEM (n = 4–6 in each group). ∗P < 0.05 versus db/m, unpaired t-test. Original magnification: ×200, bars = 20 μm. Representative image of CD34 immunostaining at (c) 16 weeks and (d) 24 weeks of age. Quantitative analysis of CD34 in 350 glomeruli identified by an LMD method at (e) 16 weeks and (f) 24 weeks of age. Values are expressed as the mean ± SEM (n = 4–6 in each group). ∗P < 0.05 versus db/m, unpaired t-test.
3.3. Enhanced LRG1 Immunostaining in Glomerular Endothelial Cells of db/db Mice at 16 Weeks of Age
We next examined LRG1 expression and distribution in the renal cortex of db/db and db/m mice at 16 weeks of age by immunohistochemical analysis. The results showed that db/db mice exhibited an increase in LRG1 expression of glomerular endothelial cells, whereas LRG1 was weakly expressed in glomerular endothelial cells of db/m mice (Figures 2(a) and 2(b)). LRG1 was also weakly expressed in tubular epithelial cells of renal tubules in db/db and db/m mice. However, LRG1 expression was not found in podocytes of db/db and db/m mice. These results indicate that an increase in LRG1 expression of glomerular endothelial cells might be associated with the development of diabetic nephropathy in db/db mice.
Figure 2.
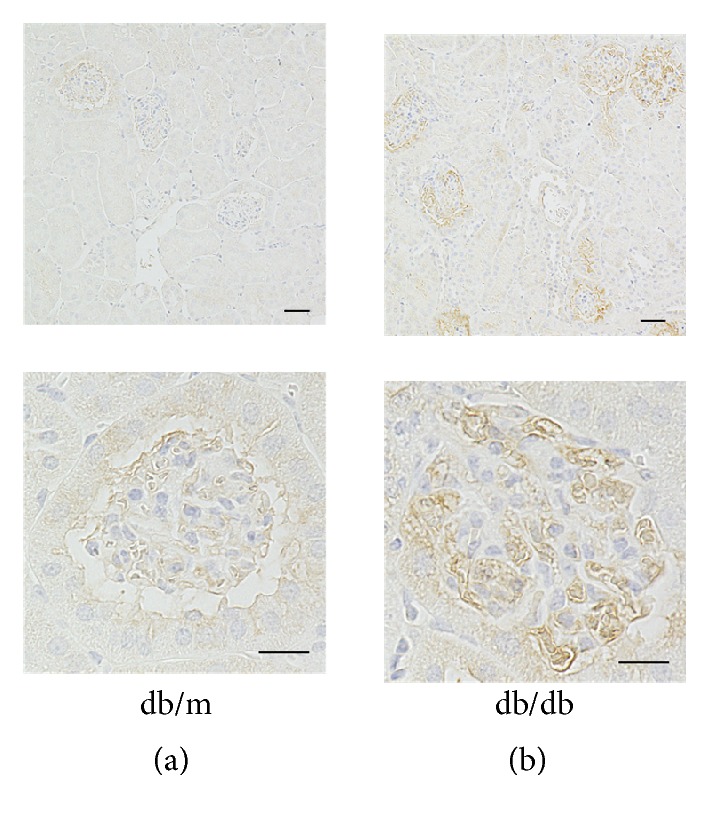
Enhanced LRG1 immunostaining in glomerular endothelial cells of db/db mice at 16 weeks of age. Representative image of LRG1 immunostaining at 16 weeks of age in (a) db/m and (b) db/db mice. Lower panels are higher magnifications of immunohistochemical staining for LRG1 in glomerular endothelial cells. Upper panels: original magnification: ×40, bars = 20 μm. Lower panels: original magnification: ×400, bars = 40 μm.
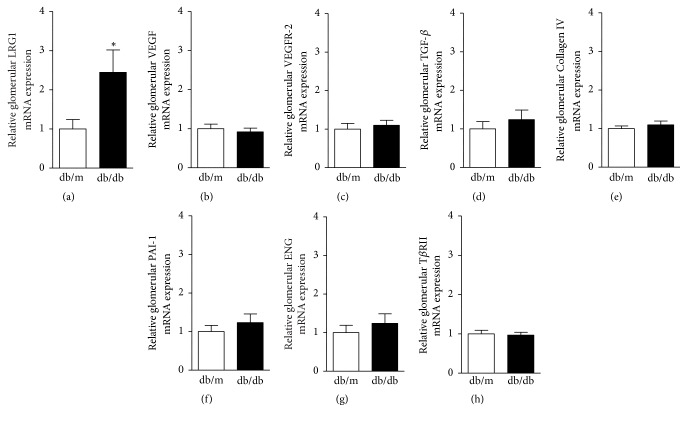
3.4. Enhanced Glomerular LRG1 mRNA Expression in db/db Mice at 16 Weeks of Age
We next examined gene expression in glomeruli of db/db and db/m mice at 16 weeks of age using the LMD method. Glomerular LRG1 mRNA expression was significantly increased by approximately 2.5-fold in db/db mice compared with db/m mice (1.0 ± 0.24 versus 2.4 ± 0.57, P < 0.05) (Figure 3(a)). Intriguingly, glomerular mRNA expression levels of VEGF and its main receptor, VEGFR-2, which are key mediators of abnormal angiogenesis and glomerular hypertrophy, were not increased in db/db mice compared with db/m mice (Figures 3(b) and 3(c)). Furthermore, glomerular mRNA expression levels of fibrosis-related genes, such as transforming growth factor-β (TGF-β), Collagen type IV (Collagen IV), and plasminogen activator inhibitor-1 (PAI-1), were identical in db/db and db/m mice (Figures 3(d)–3(f)). Since LRG1 directly binds to the TGF-β accessory receptor endoglin (ENG), and then the complex binds to TGF-β receptor-II (TβRII), we also examined glomerular mRNA expression of ENG and TβRII in db/db and db/m mice. However, there was no significant difference in glomerular mRNA expression levels of ENG and TβRII between db/db and db/m mice (Figures 3(g) and 3(h)). These results showed that the increase in LRG1 expression preceded the increase in expression of other angiogenesis- and fibrosis-related genes in the glomerulus of diabetic db/db mice.
Figure 3.
Enhanced glomerular LRG1 mRNA expression in db/db mice at 16 weeks of age. Quantitative analysis of angiogenesis- and fibrosis-related gene expression in glomeruli identified by the LMD method in db/m and db/db mice at 16 weeks of age. (a) LRG1, (b) VEGF, (c) VEGFR-2, (d) TFG-β, (e) Collagen IV, (f) PAI-1, (g) ENG, and (h) TβRII. Values are expressed as the mean ± SEM (n = 4–6 in each group). ∗P < 0.05, versus db/m mice, unpaired t-test.
3.5. Enhanced LRG1 Immunostaining in Glomerular Endothelial Cells of db/db Mice at 24 Weeks of Age
We next examined LRG1 expression in the renal cortex of db/db and db/m mice at 24 weeks of age by immunohistochemical analysis. The results showed that LRG1 expression was further enhanced in glomerular endothelial cells of db/db mice compared with db/m mice at 24 weeks of age (Figures 4(a) and 4(b)).
Figure 4.
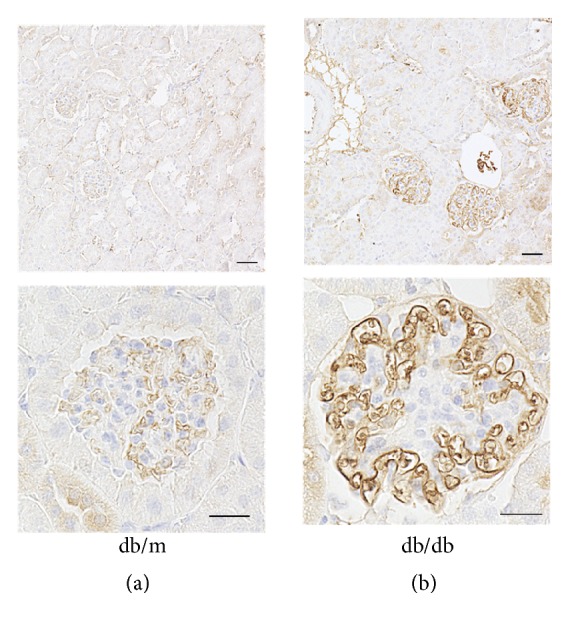
Enhanced LRG1 immunostaining in glomerular endothelial cells of db/db mice at 24 weeks of age. Representative image of LRG1 immunostaining at 24 weeks of age in (a) db/m and (b) db/db mice. Lower panels represent higher magnifications of immunohistochemical staining for LRG1 in glomerular endothelial cells. Upper panels: original magnification: ×40, bars = 20 μm. Lower panels: original magnification: ×400, bars = 40 μm.
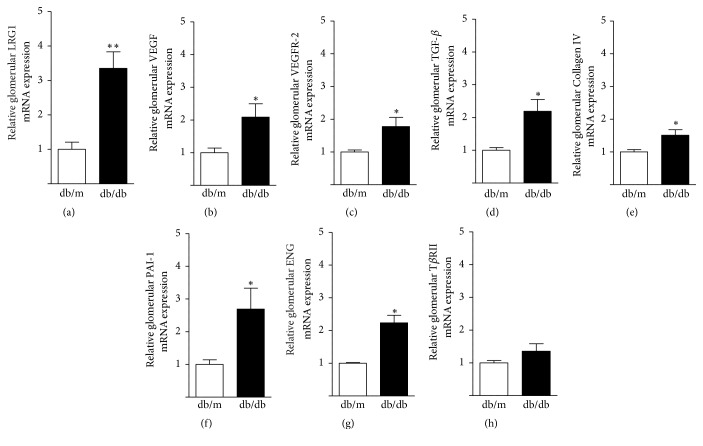
3.6. Increases in Glomerular LRG1, VEGF, and Fibrosis-Related Gene Expression of db/db Mice at 24 Weeks of Age
Finally, we examined gene expression in glomeruli of db/db and db/m mice at 24 weeks of age. Glomerular LRG1 mRNA expression was further increased by approximately 3.5-fold in db/db mice compared with db/m mice (1.0 ± 0.21 versus 3.40 ± 0.48, P < 0.01) (Figure 5(a)). Glomerular VEGF and VEGFR-2 mRNA expression was also significantly increased in db/db mice compared with db/m mice (Figures 5(b) and 5(c)). In addition, the glomerular expression levels of fibrosis-related genes, such as TGF-β, Collagen IV, and PAI-1, were significantly increased in db/db mice compared with db/m mice (Figures 5(d)–5(f)). Similarly, glomerular mRNA expression levels of ENG and TβRII were significantly increased in db/db mice compared with db/m mice (Figures 5(g) and 5(h)). These results indicated that diabetic nephropathy had developed further after the preceding increase in glomerular LRG1 expression of db/db mice.
Figure 5.
Enhanced glomerular LRG1, VEGF, and fibrosis-related gene expression in db/db mice at 24 weeks of age. Quantitative analysis of angiogenesis- and fibrosis-related gene expression in glomeruli identified by the LMD method in db/m and db/db mice at 24 weeks of age. (a) LRG1, (b) VEGF, (c) VEGFR-2, (d) TGF-β, (e) Collagen IV, (f) PAI-1, (g) ENG, and (h) TβRII. Values are expressed as the mean ± SEM (n = 4–6 in each group). ∗P < 0.05, ∗∗P < 0.01 versus db/m mice, unpaired t-test.
4. Discussion
In the present study, we investigated the intrarenal expression and distribution of a novel proangiogenic factor, LRG1, along with the development of early stage diabetic nephropathy. Our most important finding is that the increase in LRG1 expression of glomerular endothelial cells precedes the increase in VEGF expression, which is another proangiogenic factor involved in the development of diabetic nephropathy. This finding suggests that LRG1 plays a major role in the initial development of diabetic nephropathy by promoting abnormal angiogenesis and glomerular hypertrophy.
In diabetic db/db mice at 16 and 24 weeks of age, they exhibited moderate increases in albuminuria levels and glomerular hypertrophy without nodular glomerulosclerosis. These data indicate that our diabetic mice represented the features of early stage diabetic nephropathy, as reported previously [27]. Notably, at 16 weeks of age, glomerular LRG1 expression in diabetic mice was elevated despite glomerular VEGF expression being not increased yet. Considering the results indicating that the glomerular volume and endothelial cells were significantly increased in diabetic mice at this early age, abnormal angiogenesis would already exist in the glomerulus. Thus, there is the possibility that the abnormal angiogenesis observed in the very early stage of diabetic nephropathy in db/db mice was attributed to LRG1.
The interaction between LRG1 and VEGF is still unclear, but some studies have shown a possible link between these two factors. In the retina of LRG1 knockout mice, VEGF expression is significantly decreased compared with wild-type mice [15]. In colorectal cancer cells, LRG1 directly induces VEGF expression and promotes tumor angiogenesis [28]. However, LRG1 also exerts proangiogenic effects independently of the VEGF signaling pathway. Double blockade of LRG1 and VEGF suppresses angiogenesis more efficiently than single blockade in the mouse model of choroidal neovascularization [15]. In this study, we demonstrated for the first time that glomerular LRG1 expression was increased earlier than VEGF and VEGFR-2 expression under the conditions of pathological angiogenesis in the early stage of diabetic nephropathy. This finding suggests that glomerular LRG1 is involved in the pathogenesis of abnormal angiogenesis independently of the VEGF signaling pathway, at least in the very early stage of diabetic nephropathy.
Although LRG1 binds directly to ENG and activates the ALK1-Smad1/5/8 pathway for angiogenesis, the TGF-β-mediated Smad2/3 pathway is subsequently activated as a counterbalance against angiogenesis to induce quiescence in the endothelium [29, 30]. This vicious pathological cycle of angiogenesis and quiescence finally leads to glomerular fibrosis in diabetic nephropathy [31–34]. In our study, 24-week-old db/db mice exhibited upregulation of glomerular fibrosis-related genes, which was concomitant with glomerular hypertrophy and endothelial cell proliferation. It is assumed that the LRG1-induced abnormal angiogenesis observed in 16-week-old db/db mice resultantly led to glomerular fibrosis at the later stage.
Our study did not demonstrate whether the increased glomerular LRG1 expression actually caused the abnormal angiogenesis in diabetic db/db mice. Therefore, the functional role of LRG1 in abnormal angiogenesis in the early stage of diabetic nephropathy must be investigated further using LRG1 transgenic and knockout mice. Nevertheless, the findings of the present study provide important information regarding the pathogenesis of abnormal angiogenesis in early stage diabetic nephropathy, suggesting that LRG1 is a novel preemptive therapeutic target in diabetic nephropathy.
5. Conclusions
Diabetic db/db mice exhibited glomerular hypertrophy with abnormal angiogenesis characterized by endothelial cell proliferation at 16 weeks of age, concomitant with an increase in LRG1 expression of glomerular endothelial cells. However, glomerular VEGF expression was not increased at this early stage. The features of early diabetic nephropathy in db/db mice had developed further, along with further enhanced glomerular LRG1 expression at 24 weeks of age. Glomerular VEGF and fibrosis-related-gene expression was also significantly increased at this late stage compared with nondiabetic db/m mice. These data demonstrate that LRG1 might be pivotal for the initial development of diabetic nephropathy by promoting abnormal angiogenesis.
Acknowledgments
This work was supported by grants from the Yokohama Foundation for Advancement of Medical Science, a Uehara Memorial Foundation grant, Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science, grants from SENSHIN Medical Research, the Banyu Life Science Foundation International, and Salt Science Research Foundation (18C4), and a grant-in-aid from the Cardiovascular Research Fund, Tokyo, Japan. This research was also supported by the grant of Strategic Research Project of Yokohama City University, Japan Agency for Medical Research and Development (AMED), and by The Translational Research program; Strategic PRomotion for practical application of INnovative medical Technology (TR-SPRINT) from AMED. The authors thank Emi Maeda for technical assistance.
Contributor Information
Hiromichi Wakui, Email: hiro1234@yokohama-cu.ac.jp.
Kengo Azushima, Email: azushima@yokohama-cu.ac.jp.
Data Availability
The data used to support the findings of this study are included within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Authors' Contributions
Sona haku and Hiromichi Wakui designed and conducted the study. Sona haku, Hiromichi Wakui, and Kengo Azushima wrote the manuscript. Sona haku, Hiromichi Wakui, Kengo Azushima, Kotaro Haruhara, Sho Kinguchi, Kohji Ohki, Kazushi Uneda, Ryu Kobayashi, Miyuki Matsuda, Takahiro Yamaji, Takayuki Yamada, Shintaro Minegishi, Tomoaki Ishigami, Akio Yamashita, and Kenichi Ohashi performed the experiments. Sona haku, Hiromichi Wakui, and Kotaro Haruhara analyzed the data. Akio Yamashita, Kenichi Ohashi, and Kouichi Tamura supervised the study. All authors approved the final manuscript.
References
- 1.Gheith O., Othman N., Nampoory N., et al. Diabetic kidney disease: world wide difference of prevalence and risk factors. Journal of Nephropharmacology. 2016;5(1):49–56. doi: 10.4103/1110-9165.197379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnson S. A., Spurney R. F. Twenty years after ACEIs and ARBs: emerging treatment strategies for diabetic nephropathy. American Journal of Physiology-Renal Physiology. 2015;309(10):F807–F820. doi: 10.1152/ajprenal.00266.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo M., Ricardo S. D., Deane J. A., Shi M., Cullen-McEwen L., Bertram J. F. A stereological study of the renal glomerular vasculature in the db/db mouse model of diabetic nephropathy. Journal of Anatomy. 2005;207(6):813–821. doi: 10.1111/j.1469-7580.2005.00492.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ichinose K., Maeshima Y., Yamamoto Y., et al. 2-(8-Hydroxy-6-methoxy-1-oxo-1H-2-benzopyran-3-yl) propionic acid, an inhibitor of angiogenesis, ameliorates renal alterations in obese type 2 diabetic mice. Diabetes. 2006;55(5):1232–1242. doi: 10.2337/diabetes.. [DOI] [PubMed] [Google Scholar]
- 5.Østerby R., Nyberg G. New vessel formation in the renal corpuscles in advanced diabetic glomerulopathy. Journal of Diabetic Complications. 1987;1(4):122–127. doi: 10.1016/S0891-6632(87)80069-7. [DOI] [PubMed] [Google Scholar]
- 6.Nakagawa T., Kosugi T., Haneda M., Rivard C. J., Long D. A. Abnormal angiogenesis in diabetic nephropathy. Diabetes. 2009;58(7):1471–1478. doi: 10.2337/db09-0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dei Cas A., Gnudi L. VEGF and angiopoietins in diabetic glomerulopathy: how far for a new treatment? Metabolism - Clinical and Experimental. 2012;61(12):1666–1673. doi: 10.1016/j.metabol.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Østerby R., Hartmann A., Bangstad H.-J. Structural changes in renal arterioles in type I diabetic patients. Diabetologia. 2002;45(4):542–549. doi: 10.1007/s00125-002-0780-2. [DOI] [PubMed] [Google Scholar]
- 9.Østerby R. Glomerular structural changes in Type 1 (insulin-dependent) diabetes mellitus: causes, consequences, and prevention. Diabetologia. 1992;35(9):803–812. doi: 10.1007/BF00399925. [DOI] [PubMed] [Google Scholar]
- 10.Kang D. H., Hughes J., Mazzali M., et al. Impaired angiogenesis in the remnant kidney model: II. Vascular endothelial growth factor administration reduces renal fibrosis and stabilizes renal function. Biomed Research International. 2001;12(7):1448–1457. doi: 10.1681/ASN.V1271448. [DOI] [PubMed] [Google Scholar]
- 11.Kang D., Kim Y., Andoh T. F., et al. Post-cyclosporine-mediated hypertension and nephropathy: amelioration by vascular endothelial growth factor. American Journal of Physiology-Renal Physiology. 2001;280(4):F727–F736. doi: 10.1152/ajprenal.2001.280.4.F727. [DOI] [PubMed] [Google Scholar]
- 12.Ostendorf T., Kunter U., Eitner F., et al. VEGf165 mediates glomerular endothelial repair. The Journal of Clinical Investigation. 1999;104(7):913–923. doi: 10.1172/JCI6740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanabe Katsuyuk, I, Maeshima Yohe, I, Sato Yasufum, I, Wada Jun. Antiangiogenic therapy for diabetic nephropathy. BioMed Research International. 2017;2017:12. doi: 10.1155/2017/5724069.5724069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kowluru R. A., Zhong Q., Santos J. M. Matrix metalloproteinases in diabetic retinopathy: potential role of MMP-9. Expert Opinion on Investigational Drugs. 2012;21(6):797–805. doi: 10.1517/13543784.2012.681043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang X., Abraham S., McKenzie J. A., et al. LRG1 promotes angiogenesis by modulating endothelial TGF-β signalling. Nature. 2013;499(7458):306–311. doi: 10.1038/nature12345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fu J., Wei C., Zhang W., et al. Gene expression profiles of glomerular endothelial cells support their role in the glomerulopathy of diabetic mice. Kidney International. 2018;94(2):326–345. doi: 10.1016/j.kint.2018.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maeda A., Tamura K., Wakui H., et al. Angiotensin receptor-binding protein ATRAP/Agtrap inhibits metabolic dysfunction with visceral obesity. Journal of the American Heart Association. 2013;2(4) doi: 10.1161/JAHA.113.000312.e000312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Azushima K., Ohki K., Wakui H., et al. Adipocyte‐Specific Enhancement of Angiotensin II Type 1 Receptor‐Associated Protein Ameliorates Diet‐Induced Visceral Obesity and Insulin Resistance. Journal of the American Heart Association. 2017;6(3) doi: 10.1161/JAHA.116.004488.e004488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uneda K., Wakui H., Maeda A., et al. Angiotensin II Type 1 Receptor‐Associated Protein Regulates Kidney Aging and Lifespan Independent of Angiotensin. Journal of the American Heart Association. 2017;6(8) doi: 10.1161/JAHA.117.006120.e006120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ohsawa M., Tamura K., Wakui H., et al. Deletion of the angiotensin II type 1 receptor-associated protein enhances renal sodium reabsorption and exacerbates angiotensin II-mediated hypertension. Kidney International. 2014;86(3):570–581. doi: 10.1038/ki.2014.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wakui H., Dejima T., Tamura K. Activation of angiotensin II type 1 receptor-associated protein exerts an inhibitory effect on vascular hypertrophy and oxidative stress in angiotensin II-mediated hypertension. Cardiovascular Research. 2013;100(3):511–519. doi: 10.1093/cvr/cvt225. [DOI] [PubMed] [Google Scholar]
- 22.Haruhara K., Wakui H., Azushima K., et al. Angiotensin receptor-binding molecule in leukocytes in association with the systemic and leukocyte inflammatory profile. Atherosclerosis. 2018;269:236–244. doi: 10.1016/j.atherosclerosis.2018.01.013. [DOI] [PubMed] [Google Scholar]
- 23.Kobayashi R., Wakui H., Azushima K., et al. An angiotensin II type 1 receptor binding molecule has a critical role in hypertension in a chronic kidney disease model. Kidney International. 2017;91(5):1115–1125. doi: 10.1016/j.kint.2016.10.035. [DOI] [PubMed] [Google Scholar]
- 24.Minegishi S., Ishigami T., Kino T., et al. An isoform of Nedd4-2 is critically involved in the renal adaptation to high salt intake in mice. Scientific Reports. 2016;6(1) doi: 10.1038/srep27137.27137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wakui H., Tamura K., Masuda S.-I., et al. Enhanced angiotensin receptor-associated protein in renal tubule suppresses angiotensin-dependent hypertension. Hypertension. 2013;61(6):1203–1210. doi: 10.1161/HYPERTENSIONAHA.111.00572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nyengaard J. R., Flyvbjerg A., Rasch R. The impact of renal growth, regression and regrowth in experimental diabetes mellitus on number and size of proximal and distal tubular cells in the rat kidney. Diabetologia. 1993;36(11):1126–1131. doi: 10.1007/BF00401056. [DOI] [PubMed] [Google Scholar]
- 27.Azushima K., Gurley S. B., Coffman T. M. Modelling diabetic nephropathy in mice. Nature Reviews Nephrology. 2017;14(1):48–56. doi: 10.1038/nrneph.2017.142. [DOI] [PubMed] [Google Scholar]
- 28.Zhang J., Zhu L., Fang J., Ge Z., Li X. LRG1 modulates epithelial-mesenchymal transition and angiogenesis in colorectal cancer via HIF-1α activation. Journal of Experimental & Clinical Cancer Research. 2016;35(1):29. doi: 10.1186/s13046-016-0306-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pardali E., Goumans M.-J., ten Dijke P. Signaling by members of the TGF-β family in vascular morphogenesis and disease. Trends in Cell Biology. 2010;20(9):556–567. doi: 10.1016/j.tcb.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Goumans M.-J., Valdimarsdottir G., Itoh S., Rosendahl A., Sideras P., Ten Dijke P. Balancing the activation state of the endothelium via two distinct TGF-β type I receptors. EMBO Journal. 2002;21(7):1743–1753. doi: 10.1093/emboj/21.7.1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ziyadeh F. N., Hoffman B. B., Han D. C., et al. Long-term prevention of renal insufficiency, excess matrix gene expression, and glomerular mesangial matrix expansion by treatment with monoclonal antitransforming growth factor-beta antibody in db/db diabetic mice. Proceedings of the National Acadamy of Sciences of the United States of America. 2000;97(14):7667–7669. doi: 10.1073/pnas.120055097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Won Hong S., Isono M., Chen S., Iglesias-de la Cruz M. C., Han D. C., Ziyadeh F. N. Increased Glomerular and Tubular Expression of Transforming Growth Factor-β1, Its Type II Receptor, and Activation of the Smad Signaling Pathway in the db/db Mouse. The American Journal of Pathology. 2001;158(5):1653–1663. doi: 10.1016/S0002-9440(10)64121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen S., Iglesias-de la Cruz M. C., Jim B., Hong S. W., Isono M., Ziyadeh F. N. Reversibility of established diabetic glomerulopathy by anti-TGF-β antibodies in db/db mice. Biochemical and Biophysical Research Communications. 2003;300(1):16–22. doi: 10.1016/S0006-291X(02)02708-0. [DOI] [PubMed] [Google Scholar]
- 34.Cheng Xiaoyun, Gao Wenke, Dang Yongyan, et al. Both ERK/MAPK and TGF-Beta/Smad Signaling Pathways Play a Role in the Kidney Fibrosis of Diabetic Mice Accelerated by Blood Glucose Fluctuation. Journal of Diabetes Research. 2013;2013:8. doi: 10.1155/2013/463740.463740 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article.