Introduction:
Mixed states have been described as a combination of or transition between mania and depression and are experienced by an estimated 20% of individuals with bipolar disorder.1–3 Bipolar disorder is associated with a 20–30 times higher suicide risk than that of the general population4 and mixed states are considered to be a particularly high-risk state for suicide, regardless of the specific constellation of symptoms or predominant polarity;2 however, estimations of risk have been inferred from cross-sectional studies demonstrating increased suicidal behavior among those with a history of mixed symptoms.5–10 Few prospective studies have investigated suicidal behavior across mood states. A prospective study that followed 120 persons with bipolar I disorder for up to 10 years found that those with a history of mixed states (37% of the sample prospectively) had a more chronic course of illness, with approximately 10 episodes per patient compared to the 5 episodes per patient without a history of mixed states. Individuals with a history of mixed states also had more suicide attempts (30% vs. 13%), a difference that was significant in univariate analysis, but not after adjustment for age of onset.11 A two-year prospective study followed 91 individuals with bipolar I disorder, looking at the month in which participants scored highest on the suicide item from a modified Hamilton Rating Scale for depression, and found higher suicidality to be more strongly correlated with depression and hopelessness, but less robustly with mixed state.12
To date, suicidal behavior within mixed states has not been quantified in any time-varying manner prospectively or assessed in relation to the component depressive or manic states. For these reasons, it is critically important to understand and address the excess burden of risk in mixed states to inform clinical risk assessment. To address this question, the present study assessed whether suicidal behavior during mixed states is increased beyond what would be expected from the manic and depressive components alone. We hypothesized that the risk of suicidal behavior during a mixed state is greater than can be explained by the additive effects of the individual risk conveyed by mania and depression.
Methods:
Study Sample
This study used data from the National Institute of Mental Health Collaborative Depression Study (CDS). The CDS was a prospective observational study of 909 Caucasian, English-speaking patients with bipolar and unipolar disorders, recruited between 1978 and 1981 from academic centers in Illinois, Iowa, Massachusetts, Missouri, and New York. For the purposes of this analysis, the study cohort was restricted to participants with prospectively defined bipolar disorder with at least one year of follow-up. These 429 participants were followed for a mean follow-up time of 18 years up to a maximum follow-up time of 31 years, for a total of 7,693 person-years of follow-up.
Mood State
To facilitate comparison with the existing body of literature, we first classified exposure as any history of mixed states – history of mixed states was defined as a report of current mixed episode at the intake interview or at least one mood interval with symptoms of both mania/hypomania and depression during follow-up.
To address the primary question of whether suicidal behavior during mixed state is increased beyond what would be expected from the individual manic and depressed components, the exposures of interest were time-varying mania/hypomania, depression, and mixed state, which was defined as the concurrent presence of both mania/hypomania and depression within a time interval. Weekly symptom severity and onset of manic/hypomanic and depressive symptoms were captured using the Longitudinal Interval Follow-up Evaluation (LIFE), which was administered semiannually for five years and then annually for the remainder of the study duration. From this, weekly mood ratings were estimated using the LIFE Psychiatric Status Rating (PSR) scale), using a threshold of ≥3 to identify clinically significant manic/hypomanic or depressive symptoms as done in prior analyses.13–19 For major depression and mania, which use a 6-point rating scale, a PSR of 3 requires at least ‘considerably less psychopathology than full criteria with no more than moderate impairment of functioning, but still has obvious evidence of the disorder; i.e., experiences either one to two symptoms severely or two to three symptoms moderately’ or higher. For hypomania and chronic minor/intermittent depression, which use a 3-point rating scale, a score of 3 requires meeting RDC criteria for Definite – Severe. Normal mood/euthymia was defined as the absence of clinically significant mania/hypomania and depression as previously defined.
Suicidal Behavior
Suicidal behavior was broadly defined as a suicide completion or a suicide attempt of any degree of intent or medical lethality, in keeping with previous CDS analyses.16,20–23 A history of suicide attempts at intake into the study was captured using the Schedule of Affective Disorders and Schizophrenia (SADS)24,25 and suicide attempts and completions were ascertained over follow-up using the LIFE, which characterizes suicide attempt based on both intent and medical lethality.
Statistical Analysis
Descriptive statistics were analyzed using the Wilcoxon Rank-Sum test for continuous variables and the Pearson Chi-square test for categorical variables to contrast participants with and without a history of mixed states. A Cox proportional hazards regression model was used to assess time-to-onset of suicidal behavior through the calculation of a hazard ratio and 95% confidence interval. For all time-to-event analyses, frailty models were used to account for intra-subject correlation, in an approach similar to that of Holma et al.26 Frailty models are an appropriate choice for modeling recurrent events – such as suicidal behavior – for which there may be heterogeneity between individuals that at the same time confers excess risk and cannot be accounted for by the available data.27 Cox regression models rely on the assumption of proportional hazards – the assumption of proportional hazards was tested through inspection of log-log survival plots stratified by history of mixed states and through testing for significance of an interaction between history of mixed states and time on outcome.
Suicidal behavior was modeled as a repeatable event and censored cases were defined as those for which a report of suicidal behavior did not occur during the follow-up period. Mania/hypomania and depression were modeled as non-mutually exclusive dichotomous variables. Both mania/hypomania and depression were modeled as time-varying exposures, changing from 0 to 1 and vice versa, with 1 indicating the onset of clinically relevant symptoms. The time scale was measured in weeks from study enrollment; to most efficiently capture shifts in affect and to account for the potential for multiple occurrences of suicidal behavior within a single affective state, intervals were determined based on mania/hypomania, depression, and suicidal behavior, with any change in mood/outcome status signaling the start of a new measurement interval. To model mixed states, a mania × depression interaction term was entered into the models as a covariate. A significant interaction suggests that there is a multiplicative effect of concurrent manic and depressive symptoms, or in other words that the presence of a mixed state conveys an excess burden of risk of suicidal behavior greater than would be expected additively by the components attributable to manic or depressive symptoms alone.
All analyses were conducted using SAS 9.3. Unless otherwise noted, all models were adjusted for age (time-varying) and sex and the referent state for all analyses was normal mood/euthymia. Moderation by bipolar subtype was assessed; given important differences by subtype and more optimal modeling, analyses are presented separately for bipolar I and bipolar II disorder. Additional models adjusted for the potentially confounding clinical variables of number of past suicide attempts, neuroticism, the presence/absence of anxiety disorder, and the presence/absence of substance use disorder. The number of prior suicide attempts was modeled as a time-varying covariate set initially to the number of past suicide attempts as of study enrollment, increasing by one following each attempt that occurred over the course of follow-up. Presence of an anxiety disorder was chosen due to the known increased suicide risk associated with comorbid bipolar disorder and anxiety28–30 and was defined as RDC diagnosis of panic disorder, generalized anxiety disorder, obsessive-compulsive disorder, and/or phobic disorder. Presence of a substance use disorder was selected due to its known association with both mixed episodes and suicide risk10,31 and defined as a history of any alcohol or substance use disorder. Neuroticism was captured using the Maudsley Personality Inventory (MPI), scored on a scale ranging from 0 to 48, with higher scores indicating higher neuroticism.
Medication use was not modeled due to the number of time-varying covariates already modeled and prior publication of analyses designed specifically to look at the effects of medication and suicide in this sample;21–23 previous analyses of this cohort reveal that the majority of depressive episodes were medically managed with a mood stabilizer (approximately half) or a mood stabilizer plus an antidepressant (approximately one quarter).32
Results
Sociodemographic and clinical variables for those with and without a history of mixed states can be seen in Table 1. The mean participant age at baseline was 36 years. Participants were predominantly female (58%) and the majority had a diagnosis of bipolar I disorder (66.2%). Over one third of participants (38.0%) had a history of mixed states. Participants with a history of mixed states were more likely than those without a history of mixed states to be female and to have a diagnosis of bipolar I disorder. Those with a history of mixed states were also more likely to have a comorbid diagnosis of generalized anxiety disorder or panic disorder.
Table 1.
Descriptive Analysis
| Total (n=429) | Mixed States (n=163) | No Mixed States (n=266) | ||
|---|---|---|---|---|
| N(%) | N(%) | N(%) | p-value | |
| Diagnosis | 0.020 | |||
| Bipolar I Disorder | 284 (66.2%) | 119 (73.0%) | 165 (62.0%) | |
| Bipolar II Disorder | 145 (33.8%) | 44 (27.0%) | 101 (38.0%) | |
| Generalized Anxiety Disorder | 20 (4.7%) | 12 (7.4%) | 8 (3.0%) | 0.038 |
| Obsessive-Compulsive Disorder | 10 (2.3%) | 3 (1.8%) | 7 (2.6%) | 0.60 |
| Panic Disorder | 15 (3.5%) | 10 (6.1%) | 5 (1.9%) | 0.020 |
| Phobic Disorder | 23 (5.4%) | 11 (6.8%) | 12 (4.5%) | 0.32 |
| Substance Abuse Disorder | 157 (36.6%) | 57 (35.0%) | 100 (37.6%) | 0.58 |
| Sex | 0.022 | |||
| Female | 249 (58.0%) | 106 (65.0%) | 143 (53.8%) | |
| Male | 180 (42.0%) | 57 (35.0%) | 123 (46.2%) | |
| Married | 145 (33.8%) | 57 (35.0%) | 88 (33.1%) | 0.69 |
| Education Level | 0.68 | |||
| No Diploma | 51 (11.9%) | 17 (10.4%) | 34 (12.8%) | |
| High School Diploma | 112 (26.1%) | 45 (27.6%) | 67 (25.2%) | |
| Some College | 146 (34.0%) | 59 (36.2%) | 87 (32.7%) | |
| College Graduate | 120 (28.0%) | 42 (25.8%) | 78 (29.3%) | |
| Mean (sd) | Mean (sd) | |||
| Age | 36.28 (13.14) | 34.55 (10.96) | 37.33 (14.22) | 0.22 |
| Neuroticism | 30.55 (12.55) | 31.78 (11.98) | 29.78 (12.86) | 0.14 |
History of Mixed States
Number of Suicide Attempts and Completions
A total of 160 participants had at least one suicide attempt or completion; there were a total of 430 suicide attempts and 20 completions that occurred over the course of follow-up, for a total of 450 occurrences of suicidal behavior. Of these, 77 (17.1%) were from 6 participants with ≥10 repeat attempts, and 205 (45.6%) were from 26 participants with ≥5 repeat attempts.
Crude event rates for suicidal behavior are summarized in Figure 1. Over the course of follow-up, there were a total of 450 occurrences of suicidal behavior that occurred over 7,693 person-years of data (5.8 per 100 person-years), including 443 person-years of mania/hypomania, 2,518 person-years of depression, 113 person-years of mixed state, and 4,618 person-years of normal mood/euthymia. The rate of suicidal behavior was highest during depression (13.2 per 100 person-years). Rate of suicidal behavior were higher for individuals with a history of mixed states than for those without a history of mixed states overall (7.4 vs. 4.6 per 100 person-years; rate ratio 1.61).
Figure 1.
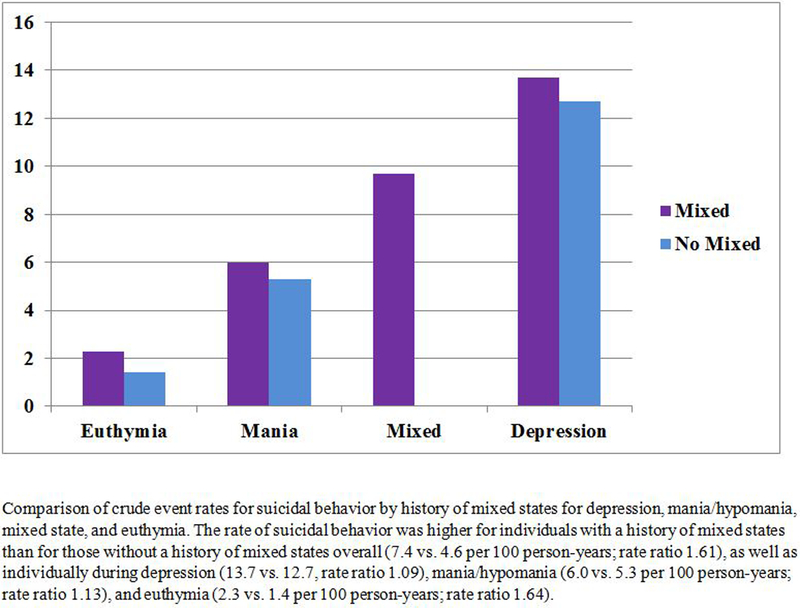
Crude Event Rates for Suicidal Behavior (per 100 person-years)
Course of Illness
We next assessed the amount of time spent in each mood state for those with and without a history of mixed states. The mean proportion of time spent depressed was 46.3% for individuals with a history of mixed states and 28.2% for those without (Figure 2; Wilcoxon rank sum p<0.0001).
Figure 2.
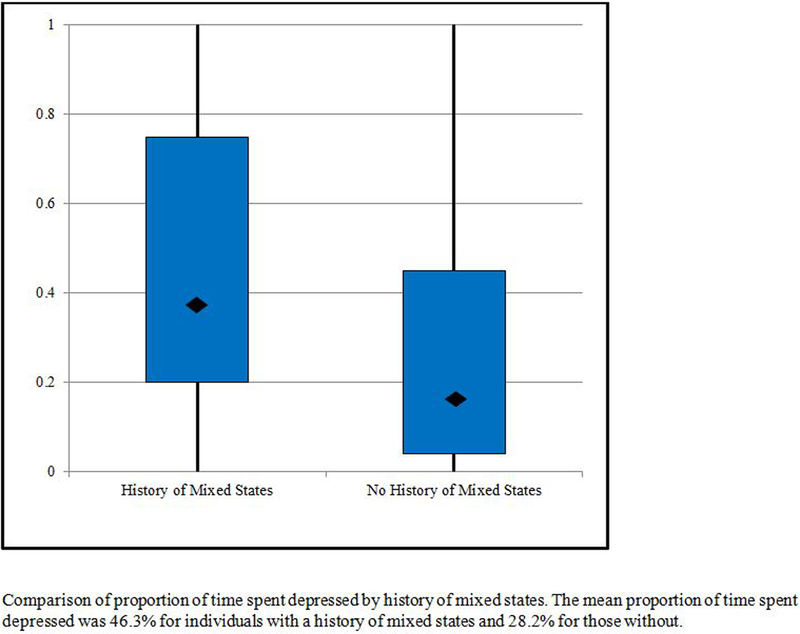
Proportion of Time Spent Depressed by History of Mixed states
Survival Analysis
Assessment of a mood-by-bipolar subtype interaction revealed a significant influence of bipolar subtype on the risk of suicidal behavior during depression (p=0.03), such that risk for suicidal behavior during depression was greater for those with bipolar I subtype. For this reason, all time-to-event analyses are reported separately for bipolar I disorder and bipolar II disorder.
Bipolar I Disorder
In frailty models adjusted for age and sex, there was an increased risk of suicidal behavior conveyed by mania/hypomania (HR: 1.96, 95% CI: 1.28–2.99, p=0.0019) and by depression (HR: 5.49, 95% CI: 4.01–7.51, p<0.0001). There was a significantly less than additive effect of mixed state on suicidal behavior beyond the risk attributable to mania/hypomania and depression (p=0.0001).
As a sensitivity analysis, we assessed whether mixed states increase risk during the mood transition following a mixed state rather than immediately during the mixed state itself. Extending each interval of mixed through the addition of a 2-week lag period did not reveal an effect of mixed state on suicidal behavior beyond the additive contributions of depression and mania/hypomania, nor did a lag period of 4 or 8 weeks. Adjusting for the number of prior suicide attempts did not appreciably alter the age- and sex-adjusted effect estimates for hypomania or depression, nor did adjusting for anxiety; however, comorbid substance use (p=0.004) and neuroticism (p=0.01) were significant independent predictors of risk.
To investigate whether those with a history of mixed states are at higher risk of suicidal behavior in a given mood state, Cox models were run with the inclusion of an interaction between history of mixed states and depression and mania/hypomania, which failed to reveal any significant interactions between history of mixed states and risk of suicidal behavior within an episode of mania/hypomania (p=0.09), but did reveal a differential effect of a history of mixed states on risk of suicidal behavior within an episode of depression (p=0.02), such that those with a history of mixed states had a higher risk of suicidal behavior while depressed.
Bipolar II Disorder
For individuals with bipolar II disorder, there was no evidence of an increased risk of suicidal behavior conveyed by hypomania (HR: 1.86, 95% CI: 0.73–4.76, p=0.19); however, there was an increased risk of suicidal behavior during depression (HR: 3.66, 95% CI: 2.51–5.35, p<0.0001). There was no increased risk of suicidal behavior during mixed state beyond the risk attributable to hypomania and depression. Adding a lag period of 2, 4, or 8 weeks did not reveal an effect of mixed state on suicidal behavior beyond the additive contributions of depression and mania/hypomania. Similarly, adjusting for the number of prior suicide attempts did not appreciably alter the age- and sex-adjusted effect estimates for hypomania or depression, nor did adjusting separately for anxiety, neuroticism, or substance use.
Cox models run with the inclusion of an interaction between history of mixed states and mood state failed to reveal any significant interaction between history of mixed states and depression (p=0.59) or hypomania (p=0.89). Thus, those with a history of mixed states were not significantly more likely to experience suicidal behavior when depressed or hypomanic.
Relative Contribution to Risk
Using the crude event rates, the causes for excess suicidal behavior in those with a history of mixed states were explored using direct standardization. The majority of excess suicidal behavior in those with a history of mixed states (71.1%) was related to a depressive-predominant course of illness, while 15.5% could be explained by the higher event rate while euthymic, 11.6% due to the higher rate while depressed, and 1.8% due to the higher event rate with mania.
Discussion
This study demonstrates that depression is a high-risk mood state for suicidal behavior and there is no increased risk during mixed state beyond the risk contributable to the depressed component. The lack of an increased risk of suicidal behavior during mixed state necessitates a revised understanding of the clearly elevated risk in those with a history of mixed states that has been noted across the literature.
Consistent with the existing literature, which focuses largely on comparisons between those with and without a history of mixed states, we found that individuals with a history of mixed states experience more suicidal behavior and spend a greater proportion of time depressed than individuals with no history of mixed states. Through survival analysis systematically assessing risk with mood state as a time-varying variable, we were able to identify that the elevated risk of suicidal behavior among those who experience mixed states is largely (71.1%) due to the combined effects of this greater proportion of time spent depressed with some additional risk of suicidal behavior when depressed in those with bipolar I disorder.
In this current study, the prevalence of mixed states was 38% – notably higher than the estimated prevalence of 20% reported in previous studies.1–3 This higher estimate is almost identical to the 37% prevalence observed by Gonzalez-Pinto et al. in their 10 year prospective study,11 which likely reflects the greater ascertainment enabled by long-term follow-up. Gonzalez-Pinto et al. also noted that those with mixed states had more depressive symptoms; however, these findings were confounded by age of onset, which may be a proxy for a more chronic course.33 Rather than adjust for age of onset, we were able to directly address course of illness by assessing risk by mood state as a time-varying covariate.
The Collaborative Depression Study, which applied RDC criteria, does not allow a direct assessment of DSM-5 mixed states. As a point of comparison, the DSM-5 defines mixed state as experiencing any one of the following: 1. meeting full criteria for a manic/hypomanic episode (elevated or expansive mood and at least three other symptoms, or irritable mood and at least four other symptoms) and at least 3 depressive symptoms (Mania/hypomania with mixed features), or 2. meeting full criteria for a major depressive episode (depressed mood or loss of interest and at least five other symptoms) and at least 3 manic/hypomanic symptoms (Major Depression with mixed features).
Our RDC-based operationalization of mixed state approximates that of the DSM-5, although it should be noted that the criteria used for our study are likely slightly broader. The DSM-5 accounts only for the total number of symptoms, but not for the severity of individual symptoms; therefore, a patient who does not meet full diagnostic criteria for major depression or mania but is experiencing mood symptoms to a moderate degree of impairment (e.g., experiencing two to three symptoms moderately) would be captured as experiencing mixed states under our definition, but not under the DSM-5. On the other hand, a patient who meets full diagnostic criteria for one syndrome and is experiencing 3 or more symptoms of the other syndrome, but only to a mild degree, would not be captured as experiencing mixed states under our criteria, but would under the DSM-5. In this current study, accepting RDC criteria as a proxy for DSM-5 major depression, mania and hypomania, 93% of intervals with clinically significant depressive symptoms at some point during the interval also met DSM-5 criteria for a major depressive episode, 86% of intervals of clinically significant mania/hypomania symptoms met DSM-5 criteria for mania or hypomania and 91% of mixed intervals met full diagnostic criteria for one syndrome (major depression, mania, or hypomania) as required by DSM-5.
The strengths of this study are the sample size, the long duration of follow-up, and the use of structured clinical interview to ascertain diagnoses. The risk associated with mood states, including risk episodes, was modeled in state-of-the-art survival analytical models that allowed for repeated events within subjects and fully utilized the prospective data. This study is limited in the use of a racially homogeneous sample, which may restrict the generalizability of our findings. It should be noted in addition that, although the outcome of suicidal behavior included both suicide attempts and completions, this measure predominantly captured suicide attempts; as such, the conclusions drawn from this analysis may be more relevant to the risk of suicide attempt than to the risk of completed suicide.
Overall, the takeaway message from this research is that much of the suicide risk related to having a history of mixed states is not a product of the mixed state itself, but rather can be attributed to a depression-predominant course of illness. Clinicians should pay close attention to depressive mood states in bipolar disorder in the assessment of suicide risk and aggressively treat this modifiable risk factor to mitigate risk for those with or without a history of mixed episodes.
References
- 1.Rihmer A, Gonda X, Balazs J, et al. The importance of depressive mixed states in suicidal behaviour. Neuropsychopharmacologia Hungarica : a Magyar Pszichofarmakologiai Egyesulet lapja = official journal of the Hungarian Association of Psychopharmacology 2008;10(1):45–9. [PubMed] [Google Scholar]
- 2.Swann AC, Lafer B, Perugi G, et al. Bipolar mixed states: an international society for bipolar disorders task force report of symptom structure, course of illness, and diagnosis. The American journal of psychiatry 2013;170(1):31–42. [DOI] [PubMed] [Google Scholar]
- 3.Shim IH, Woo YS, Bahk WM. Prevalence rates and clinical implications of bipolar disorder “with mixed features” as defined by DSM-5. Journal of affective disorders 2015;173:120–5. [DOI] [PubMed] [Google Scholar]
- 4.Pompili M, Gonda X, Serafini G, et al. Epidemiology of suicide in bipolar disorders: a systematic review of the literature. Bipolar disorders 2013;15(5):457–90. [DOI] [PubMed] [Google Scholar]
- 5.Swann AC, Steinberg JL, Lijffijt M, et al. Continuum of depressive and manic mixed states in patients with bipolar disorder: quantitative measurement and clinical features. World Psychiatry 2009;8(3):166–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cassidy F, Murry E, Forest K, et al. Signs and symptoms of mania in pure and mixed episodes. Journal of affective disorders 1998;50(2–3):187–201. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg JF, Perlis RH, Bowden CL, et al. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. The American journal of psychiatry 2009;166(2):173–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pacchiarotti I, Mazzarini L, Kotzalidis GD, et al. Mania and depression. Mixed, not stirred. Journal of affective disorders 2011;133(1–2):105–13. [DOI] [PubMed] [Google Scholar]
- 9.Strakowski SM, McElroy SL, Keck PE Jr., et al. Suicidality among patients with mixed and manic bipolar disorder. The American journal of psychiatry 1996;153(5):674–6. [DOI] [PubMed] [Google Scholar]
- 10.Balazs J, Benazzi F, Rihmer Z, et al. The close link between suicide attempts and mixed (bipolar) depression: implications for suicide prevention. Journal of affective disorders 2006;91(2–3):133–8. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez-Pinto A, Barbeito S, Alonso M, et al. Poor long-term prognosis in mixed bipolar patients: 10-year outcomes in the Vitoria prospective naturalistic study in Spain. The Journal of clinical psychiatry 2011;72(5):671–6. [DOI] [PubMed] [Google Scholar]
- 12.Johnson SL, McMurrich SL, Yates M. Suicidality in bipolar I disorder. Suicide Life Threat Behav 2005;35(6):681–9. [DOI] [PubMed] [Google Scholar]
- 13.Fiedorowicz JG, Solomon DA, Endicott J, et al. Manic/hypomanic symptom burden and cardiovascular mortality in bipolar disorder. Psychosom Med 2009;71(6):598–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akhter A, Fiedorowicz JG, Zhang T, et al. Seasonal variation of manic and depressive symptoms in bipolar disorder. Bipolar disorders 2013;15(4):377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fiedorowicz JG, Coryell WH, Rice JP, et al. Vasculopathy related to manic/hypomanic symptom burden and first-generation antipsychotics in a sub-sample from the collaborative depression study. Psychother Psychosom 2012;81(4):235–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fiedorowicz JG, Leon AC, Keller MB, et al. Do risk factors for suicidal behavior differ by affective disorder polarity? Psychological medicine 2009;39(5):763–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fiedorowicz JG, Endicott J, Solomon DA, et al. Course of illness following prospectively observed mania or hypomania in individuals presenting with unipolar depression. Bipolar disorders 2012;14(6):664–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fiedorowicz JG, Endicott J, Leon AC, et al. Subthreshold hypomanic symptoms in progression from unipolar major depression to bipolar disorder. The American journal of psychiatry 2011;168(1):40–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fiedorowicz JG, Palagummi NM, Behrendtsen O, et al. Cholesterol and affective morbidity. Psychiatry research 2010;175(1–2):78–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fiedorowicz JG, Coryell WH. Cholesterol and suicide attempts: a prospective study of depressed inpatients. Psychiatry research 2007;152(1):11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leon AC, Fiedorowicz JG, Solomon DA, et al. Risk of suicidal behavior with antidepressants in bipolar and unipolar disorders. The Journal of clinical psychiatry 2014;75(7):720–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leon AC, Solomon DA, Li C, et al. Antidepressants and risks of suicide and suicide attempts: a 27-year observational study. The Journal of clinical psychiatry 2011;72(5):580–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leon AC, Solomon DA, Li C, et al. Antiepileptic drugs for bipolar disorder and the risk of suicidal behavior: a 30-year observational study. The American journal of psychiatry 2012;169(3):285–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Archives of general psychiatry 1978;35(7):837–44. [DOI] [PubMed] [Google Scholar]
- 25.Endicott J, Spitzer RL. Use of the Research Diagnostic Criteria and the Schedule for Affective Disorders and Schizophrenia to study affective disorders. The American journal of psychiatry 1979;136(1):52–6. [DOI] [PubMed] [Google Scholar]
- 26.Holma KM, Melartin TK, Haukka J, et al. Incidence and predictors of suicide attempts in DSM-IV major depressive disorder: a five-year prospective study. The American journal of psychiatry 2010;167(7):801–8. [DOI] [PubMed] [Google Scholar]
- 27.Amorim LD, Cai J. Modelling recurrent events: a tutorial for analysis in epidemiology. Int J Epidemiol 2015;44(1):324–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sala R, Goldstein BI, Morcillo C, et al. Course of comorbid anxiety disorders among adults with bipolar disorder in the U.S. population. Journal of psychiatric research 2012;46(7):865–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goes FS. The importance of anxiety states in bipolar disorder. Current psychiatry reports 2015;17(2):3. [DOI] [PubMed] [Google Scholar]
- 30.Schaffer A, Isometsa ET, Tondo L, et al. International Society for Bipolar Disorders Task Force on Suicide: meta-analyses and meta-regression of correlates of suicide attempts and suicide deaths in bipolar disorder. Bipolar disorders 2015;17(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Swann AC, Moeller FG, Steinberg JL, et al. Manic symptoms and impulsivity during bipolar depressive episodes. Bipolar disorders 2007;9(3):206–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Solomon DA, Fiedorowicz JG, Leon AC, et al. Recovery from multiple episodes of bipolar I depression. The Journal of clinical psychiatry 2013;74(3):e205–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Perlis RH, Dennehy EB, Miklowitz DJ, et al. Retrospective age at onset of bipolar disorder and outcome during two-year follow-up: results from the STEP-BD study. Bipolar disorders 2009;11(4):391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]


