ABSTRACT
Objectives: The perceived relative safety of thoracic thrust joint manipulation (TTJM) has contributed to evidence supporting its use. Yet, TTJM is not without risk, where transient side effects (SE) and severe adverse events (AE) have been documented. With evidence supporting the importance of prethrust examination in reducing AE in other spinal regions this study investigated TTJM knowledge and pre-TTJM examination.
Method: An e-survey, informed by existing evidence and expertise was designed and piloted. Eligibility criteria: UK-trained physiotherapists who use TTJM. Recruitment via professional networks and social media from December 2016 to February 2017. Data analysis included descriptive analyses (means, standard deviation and frequencies/central tendencies), and content analysis (themes and frequencies) for free text data.
Results: From 306 responses, the sample comprised 146 (53%) males, mean (SD) age 36.37(8.68) years, with 12.88(8.67) years in practice, 11.07(8.14) years specialization, working in National Health Service/private practice (81%) and performing 0–5 TTJM/week (86%). Examination: 40% (n = 83) utilized pre-TTJM examination with 45% (n = 139) adapting the examination for different regions. Technique selection and effect: preferred technique was prone rotational TTJM (67%). Perception of the primary underlying effect was neurophysiological (54%), biomechanical (45%) or placebo (1%). Knowledge: Levels of agreement were found for contraindications (85%), precautions (75%), and red flags (86%) with more variability for risks including AE and SE (61%).
Discussion: UK physiotherapists demonstrated good knowledge and agreement of contraindications, precautions, and red flags to TTJM. With <50% respondents utilizing pre-TTJM examination, variable knowledge of TTJM risks, and therapeutic effects of TTJM further research is required.
KEYWORDS: Examination, survey, thoracic, thrust manipulation, clinical knowledge, current practice
Introduction
Despite a relative paucity of research, the thoracic spine is the most commonly manipulated spinal region [1,2]. Also termed thrust joint manipulation (TJM) the technique involves high-velocity, low-amplitude forces directed at spinal joints [3]. With a relative high incidence of temporary side effects (SE) (80% after first treatment and 70% following the second treatment) including neck pain, fatigue, headache and upper back pain, compared to the cervical spine [4], and reports of adverse events (AE) including spinal cord injury, pneumothorax, and hemothorax [3,5], concerns have been raised that the current pre-TJM examination may not be adequate to determine the level of risk when using thoracic thrust joint manipulation (TTJM) [3]. This problem is further compounded given the known risks of cervical TJM and our understanding of the regional interdependence theory [6] resulting in a proliferation of research investigating the use of TTJM for shoulder and neck complaints [7–9] including recently published clinical practice guidelines recommending TTJM for neck pain [10].
Within this emerging body of research there is little consideration of, or differentiation between SE and AE, where SEs are reversible, often transient in nature [4] and are a recognized sequelae of TJM [11–13] as opposed to more concerning AEs where there is the potential for life changing consequences such as spinal cord injury [3]. In the absence of data specific to the thoracic spine, a systematic review of AE and manual therapy reported that 41% of patients can expect SE after treatment (e.g. muscle tenderness, headache), especially after the first treatment, with the relative incidence of AE small [13,14]. Notwithstanding this AE such as stroke and in some cases death following manual therapy in the biomechanically linked cervical spine cannot be ignored [15–17]. A survey investigating cervical spine manipulation and clinical use of examination pre-TJM found that 77% of International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT) member organizations utilized premanipulative screening guidelines, although only 50% recommended the use of standardized information regarding AE [12]. These findings contributed to the development of evidence informed and IFOMPT-endorsed clinical reasoning framework to assist clinicians’ examination of cervical spine prior to orthopedic manual therapy intervention that may include TJM [18].
Despite the reported poor accuracy of TTJM [19] and positioning for some TTJM techniques placing stress on adjacent spinal regions, for example upper thoracic spine (T1-4) TJM techniques, the perception that TTJM are safe persists in practice. A survey of US physical therapists reported that 91.1% respondents were less likely to perform pre-TTJM examination compared to the cervical spine [2]. This is a concern given the exponential growth in empirical studies supporting use of TTJM [8,20], recommendation in guidelines [10], evidence of AE [3,5] and critically that appropriate pre-TJM examination may reduce the risk of AE [2]. A review of 134 case reports of AE following cervical TJM concluded that 44.8% of AE could have been prevented by pre-TJM examination of contraindications and red flags [21], supporting the need for further research and establishing a comparable clinical reasoning framework for the thoracic spine.
The objectives of the study were to investigate amongst UK physiotherapists: (a) the use of TTJM and premanipulative examination; and (b) the knowledge of the contraindications, precautions, red flags, and risk associated with TTJM; and (c) to inform future research
Design and methods
An online survey was designed based on current evidence to capture UK physiotherapists’ practice and knowledge of TTJM, and is reported in line with the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) [22].
Survey
The survey structure and content was informed by current evidence to enhance the validity and reliability of the tool and author expertise. Content validity was strengthened with the inclusion of known symptoms relating to TTJM based on current evidence [3,5,20]. The differentiation of items within categories for red flags (general medical concern) and contraindications (specific effects of a particular treatment) was informed by current literature [3]. Construct validity was enhanced with the design being based on existing surveys [2,12]. The survey comprised open and closed questions, with no option of a review step, and could be completed on any electronic device with Internet access.
The survey was developed to capture demographic data, including age, gender, years in clinical practice, years of specialization in musculoskeletal practice, thoracic spine specific continuing professional development, practice setting, professional grade, with the prime foci being clinical examination prior to TTJM and respondent knowledge of SE and AE in the use of TTJM. Ten UK musculoskeletal physiotherapists who undertook TTJM piloted the survey prior to the main study in November 2016. Following the pilot revisions included clarification of instructions, including completion time (10–15 min), ranking question for choice of technique, order of questions, specifying ‘spine’ for some of the choices, for example spine surgery, and options for free text data to be added. The main survey was hosted on Qualtrics, a secure online data collection platform, for a 9-week period from 19.12.16 until 20.02.17. Frequent prompts and publicity for participation in the survey were done throughout the period the survey was live and the survey accessible via any electronic device with access to the Internet.
Sample and recruitment
Inclusion criteria: UK-trained physiotherapists who perform TTJM as part of their regular/routine clinical practice. Individuals were invited to participate online via professional networks, e-mail and social media (Twitter, LinkedIn, and Facebook). The sample size (Ns) needed for the aspired level of precision was determined (n = 276) based on:
Where Ns = sample size, Np = size of target population, p = proportion of population predicted to choose one of two response categories, B = sampling error (0.05 = ± 5% of the true population value), C = Z statistic associated with the confidence level [23]. The total UK physiotherapy population (Np) is ~ 53,000. The proportion of the population (p) expected to choose one of the two response categories (to participate or not) was set as 0.50. The acceptable sampling error (B) was set as 0.03, and the confidence level (C) at 95%, giving a corresponding Z statistic of 1.645. The required sample size was therefore n = 276.
Data analysis
Following removal of duplicate IP addresses, the data were transferred to statistical analysis software (SPSS Version 24: SPSS Inc., Chicago, IL). Descriptive data analyses (frequencies, mean, and standard deviation) were used to characterize the sample. For closed questions frequencies were calculated and findings tabulated or presented graphically. Free text responses were analyzed using content analysis to enable themes/categories to be derived and quantified with calculation of frequencies for each category [24].
Within the literature there is indistinct differentiation between AE and SE [12,13]. In an attempt to address this ambiguity, a framework for categorization of AE from manual therapy was developed, and symptoms graded into Major, Moderate, or Mild/Not Adverse AE [25]. The framework has evolved with the term AE encompassing serious symptoms as outlined by the Major categorization mentioned earlier, and SE being the more transient symptoms akin to the Mild/Not adverse definition [4]. In line with this and with author consensus the ‘risks’ for the levels of agreement questions in the survey were split into AE and SE (see Table 1).
Table 1.
Knowledge of contraindications, precautions, red flags, and risks of TTJM.
| N = 169 | Completely Disagree (%) |
Somewhat Disagree (%) |
Neutral (%) | Somewhat Agree (%) |
Completely Agree (%) |
|
|---|---|---|---|---|---|---|
| Contraindications | Metastatic disease* | 1.1 | 0.0 | 1.7 | 8.4 | 88.8 |
| Metabolic bone disease* | 0.6 | 0.6 | 1.7 | 9.0 | 88.2 | |
| Osteomyelitis* | 2.2 | 0.0 | 2.2 | 13.5 | 82.0 | |
| Neurological pathology* | 1.7 | 3.4 | 3.9 | 14.0 | 77.0 | |
| Traumatic pathology* | 1.7 | 2.8 | 5.1 | 14.6 | 75.8 | |
| Long-term steroid use* | 0.0 | 4.5 | 6.2 | 27.0 | 62.4 | |
| Aortic aneurysm* | 0.6 | 3.9 | 6.7 | 14.6 | 74.2 | |
| Congenital fusions or dysplasia’s | 1.7 | 2.8 | 8.4 | 29.2 | 57.9 | |
| Surgical fusion* | 1.7 | 2.2 | 9.0 | 23.6 | 63.5 | |
| Tuberculosis* | 0.6 | 2.8 | 10.1 | 12.9 | 73.6 | |
| Untreated cardiac insufficiency* | 0.6 | 6.2 | 11.8 | 23.6 | 57.9 | |
| Acute abdominal pain* | 1.1 | 2.8 | 15.2 | 22.5 | 58.4 | |
| Bleeding disorder* | 1.1 | 5.6 | 12.9 | 24.7 | 55.6 | |
| Inflammatory disease | 0.6 | 9.0 | 11.2 | 32.6 | 46.6 | |
| Recent spine surgery | 1.1 | 4.5 | 16.9 | 33.7 | 43.8 | |
| Vertebrobasilar ischemia or cervical artery dysfunction | 4.5 | 9.6 | 12.9 | 17.4 | 55.6 | |
| Angina pectoris | 2.2 | 12.4 | 15.7 | 27.5 | 42.1 | |
| Precautions | No change or worsening symptoms after multiple manipulations* | 1.2 | 0.0 | 2.9 | 14 | 82.0 |
| Previous adverse reaction to TJM* | 0.6 | 0.6 | 5.8 | 33.7 | 59.3 | |
| Osteopenia* | 1.2 | 2.3 | 4.7 | 24.4 | 67.4 | |
| Inflammatory process* | 0.6 | 2.3 | 7.6 | 33.1 | 56.4 | |
| Psychological dependence on manipulations* | 1.2 | 5.2 | 7.0 | 29.7 | 57.0 | |
| Systemic infections* | 0.0 | 5.8 | 13.4 | 33.7 | 47.1 | |
| Children * | 3.5 | 3.5 | 14.0 | 18.6 | 60.5 | |
| Spondylolisthesis | 4.1 | 4.1 | 14.0 | 23.8 | 54.1 | |
| Pain with psychological overlay | 2.3 | 11.0 | 10.5 | 32.6 | 43.6 | |
| Hypermobility or ligamentous laxity | 1.7 | 11.6 | 11.6 | 31.4 | 43.6 | |
| Serious degenerative joint disease | 2.9 | 15.1 | 8.7 | 31.4 | 41.9 | |
| Arterial calcification¥ | 0.6 | 6.4 | 23.8 | 32.6 | 36.6 | |
| Herpes zoster on the thoracic spine¥ | 1.2 | 2.9 | 26.7 | 23.8 | 45.3 | |
| Arterial hypertension¥ | 1.7 | 7.6 | 25.0 | 33.7 | 32.0 | |
| Disc herniation/protrusion | 4.1 | 13.4 | 18.6 | 26.2 | 37.8 | |
| Significant kyphosis and/or scoliosis | 4.1 | 18.0 | 14.5 | 28.5 | 34.9 | |
| Vertigo¥ | 4.7 | 15.7 | 30.2 | 25.6 | 23.8 | |
| Red flag | Pain of a nonmechanical nature* | 0.6 | 1.2 | 3.6 | 18.9 | 75.7 |
| Altered coordination in upper or lower limbs* | 0.0 | 1.2 | 4.7 | 22.5 | 71.6 | |
| Unremitting pain* | 0.0 | 2.4 | 3.6 | 18.9 | 75.1 | |
| Night pain* | 0.6 | 7.1 | 11.8 | 27.2 | 53.3 | |
| Weakness in upper or lower limbs or torso* | 0.0 | 7.1 | 12.4 | 36.7 | 43.8 | |
| Changes in bladder function* | 0.6 | 1.8 | 4.7 | 17.8 | 75.1 | |
| Changes in bowel function* | 0.0 | 1.8 | 5.9 | 16.6 | 75.7 | |
| Previous personal history of cancer* | 0.0 | 3.6 | 6.5 | 23.7 | 66.3 | |
| Sexual dysfunction* | 0.6 | 2.4 | 10.1 | 22.5 | 64.5 | |
| Night sweats* | 1.2 | 2.4 | 10.1 | 28.4 | 58.0 | |
| Pain worsening with cough, sneeze or going to the toilet | 0.6 | 7.1 | 16.0 | 34.9 | 41.4 | |
| Numbness in upper or lower limbs or torso | 1.2 | 10.1 | 13.6 | 36.1 | 39.1 | |
| Pins and needles in upper or lower limbs or torso | 1.2 | 14.2 | 16.0 | 37.3 | 31.4 | |
| Risks | Adverse events | |||||
| Increase in pain local to the targeted region following TJM* | 0.6 | 5.5 | 8.0 | 38.7 | 47.2 | |
| Thoracic spine fracture | 3.1 | 9.2 | 11.7 | 28.2 | 47.9 | |
| Pneumothorax ¥ | 3.1 | 11.0 | 15.3 | 23.9 | 46.6 | |
| Spinal cord injury¥ | 6.7 | 10.4 | 12.9 | 29.4 | 40.5 | |
| Hemothorax¥ | 3.1 | 9.8 | 18.4 | 20.9 | 47.9 | |
| Epidural hematoma¥ | 2.5 | 9.2 | 22.7 | 25.8 | 39.9 | |
| Herniated thoracic disc¥ | 3.7 | 16.0 | 18.4 | 33.7 | 28.2 | |
| Dural sleeve tear¥ | 4.9 | 10.4 | 23.3 | 31.9 | 29.4 | |
| CVA/stroke¥ | 6.7 | 14.1 | 22.1 | 23.3 | 33.7 | |
| Thoracic sphinx¥ | 1.8 | 12.3 | 36.8 | 23.9 | 25.2 | |
| Cervical artery dissection§ | 9.8 | 20.9 | 15.3 | 18.4 | 35.6 | |
| Vertebral artery dissection§ | 9.2 | 21.5 | 16.6 | 17.2 | 35.6 | |
| Side Effects | ||||||
| Local discomfort/soreness§ | 6.7 | 17.8 | 19.0 | 25.8 | 30.7 | |
| Headache§ | 6.1 | 24.5 | 22.1 | 33.1 | 14.1 | |
| Fatigue§ | 7.4 | 25.2 | 32.5 | 25.8 | 9.2 |
Note: Ranking based on total score for ‘ completely’ and ‘somewhat agree’; * > 80% agreement; ¥lack of agreement and high levels of neutral scores;§disagreement
Ethics
This study was approved by the School of Sport, Exercise and Rehabilitation Sciences, University of Birmingham and participation in the survey was entirely voluntary.
Results
With 343 different IP addresses recorded and 306 completed surveys satisfying the a priori sample size calculation, an 89.2% view rate was recorded (306/343). Furthermore of the 306 completed surveys, 160 were completed in full (answered all questions) resulting in a 46.6% (160/343) participation rate; this is discussed later. All surveys were included in the analysis from the outset, with the number of responses per questions reported accordingly.
Demographics and respondent characteristic are included in Table 2. The majority of respondents worked in either private practice (n = 157) or National Health Service (NHS) (n = 127) setting, with the former being the environment where respondents were most likely to perform TTJM (n = 132, 50.4% of the 262 responses for this question).
Table 2.
Respondent characteristics and use of TTJM.
| Age % (n) years | 36.37 (8.68) |
| Gender % (n) male | 52.9 (146) |
| Clinical experience mean (SD) years | 12.88 (8.67) |
|
Musculoskeletal specialization mean (SD) years |
11.07 (8.14) |
| Practice setting | % (n)* |
| • NHS | 41.5 (127) |
| • Private practice | 51.3 (157) |
| • Sport | 13.1 (40) |
| • Military | 3.3 (10) |
| • Lecturer | 7.8 (24) |
| • Researcher | 2.6 (8) |
| • Other | 4.2 (13) |
|
Work setting/environment |
Number of TTJM/ week |
Number of physiotherapists |
Percentage (%) |
| National Health Service (NHS) | 0–5 | 70 | 98.6 |
| 16–20 | 1 | 1.4 | |
| Private Practice | 0–5 | 80 | 79.2 |
| 6–10 | 13 | 12.9 | |
| 11–15 | 5 | 5 | |
| 16–20 | 1 | 1 | |
| 21 + | 2 | 2 | |
| Sport | 0–5 | 16 | 80 |
| 6–10 | 4 | 20 | |
| Military | 0–5 | 8 | 80 |
| 6–10 | 1 | 10 | |
| 11–15 | 1 | 10 | |
| Academic (lecturer/researcher) | 0–5 | 2 | 100 |
| Other | 0–5 | 6 | 85.7 |
| 6–10 | 1 | 14.3 |
Note: *Total percentage/sum exceeds reported sample to reflect multiple work settings for some participants
The majority of respondents (n = 105, 49.8% of n = 211 responses) reported managing two to five patients a week with thoracic spine dysfunction, and 86.3% (n = 182 of n = 211 responses) performing 0–5 TTJM a week. Slightly greater use of TTJM in was observed in those working in a private practice settings (Table 2).
Current practice
Pre-thrust examination
Of the 209 respondents that responded to the question, 39.7% (n = 83) used prethrust examination, with 27 using a tool of their own design, 25 a workplace standardized proforma, 23 their own clinical reasoning as a means of examination with a specific subset of questions, 5 respondents gave minimal detail as to the format of pre-TTJM examination, and 3 used a combination of both their own clinical reasoning and workplace standardized proforma. The profile of those using a screening proforma according to grade of practice and work setting is provided in Table 3.
Table 3.
Use of a screening proforma prior to application of TTJM against grade work setting.
| Yes n (%) | No n (%) | ||
|---|---|---|---|
|
Grade of job N = 210 |
Band 5/Junior | 5 (6) | 1 (0.8) |
| Band 6/Senior | 14 (16.9) | 32 (25.4) | |
| Band 7/Senior | 19 (22.9) | 39 (31) | |
| Band 8/Specialist | 10 (12) | 12 (9.5) | |
| Extended Scope Practitioner | 10 (12) | 19 (15.1) | |
| Clinical Specialist | 10 (12) | 10 (7.9) | |
| Consultant | 3 (3.6) | 5 (4.0) | |
| Lecturer | 2 (2.4) | 1 (0.8) | |
| Researcher | 0 (0) | 1 (0.8) | |
| Other | 10 (12) | 6 (4.8) | |
|
Work setting N = 209 |
NHS | 43 (51.8) | 61 (48.4) |
| Private Practice | 42 50.6 | 79 (62.7) | |
| Sport | 13 (15.7 | 20 (15.9) | |
| Military | 1 (1.2) | 9 (13.3) | |
| Lecturer | 11 (13.3) | 8 (6.3) | |
| Researcher | 3 (3.6) | (2.4) | |
| Other | 6 (7.2) | 2 (1.6) |
Upper and lower thoracic spine
Less than half the respondents (n = 76 from n = 139 responses, 45%) would differentiate between the upper and lower thoracic spine during examination prior to performing TTJM. These respondents associated the upper thoracic region with the cervical spine, including specific questioning for vertebrobasiliar insufficiency/cervical artery dissection, and the lower thoracic region with the lumbar spine, including special questions to examine for cauda equina involvement.
Technique selection and clinical use
The primary technique of choice for TTJM was the prone lying ‘butterfly’/ ’rotational’/’screw’ in 67.1% (n = 108 of n = 161 responses) of respondents, with supine PA/AP thrust second at 30.4% (n = 49) and seated traction last with 2.5% (n = 4). From content analysis, respondents reported technique selection was based on ‘ease of application’ (n = 49), ‘comfort for therapist and patient’ (n = 35), ‘previous results’ (n = 24), ‘confidence or competence’ (n = 23), perceived ‘accuracy’ (n = 10), ‘clinical reasoning’ (n = 10), ‘previous success in performing the technique’ (n = 11) ‘only technique taught/known’ (n = 6), and ‘perceived safest’ (n = 3).
Respondents reported using TTJM for complaints in a number of regions other than the thoracic spine, including the cervical spine, rib, lumbar spine, shoulder, temporomandibular joint, pelvis, elbow, wrist, and lower limb joints (Figure 1). The majority, however, utilized TTJM when treating thoracic spine (n = 155), followed by the shoulder (n = 144), then the cervical spine (n = 134), rib (n = 124), and lumbar spine (n = 107).
Figure 1.
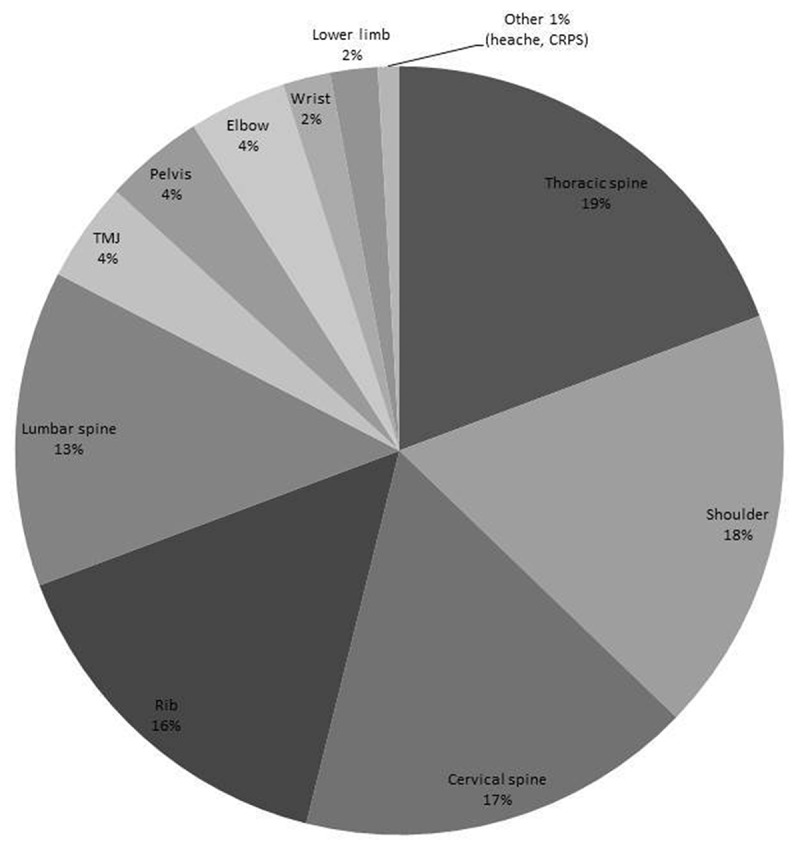
Clinical use of TTJM for managing musculoskeletal complaints.
Knowledge
Clinical reasoning in the use of TTJM
In terms of information and/or clinical reasoning that would inform respondents’ decision-making to utilize TTJM, data were provided by 63.1% (n = 193) of the sample.
Clinical presentation – movement dysfunction (n = 59), pain location, and behavior (n = 23), pain mechanism specifically nociceptive (n = 17), low severity and irritability (n = 13), mechanical presentation (n = 10), clinical reasoning (n = 8), postural component (n = 4), onset (n = 4), and no progress with lower grade mobilizations (n = 1)
Patient centered factors – no yellow flags (n = 8), previous positive response (n = 8), age (n = 6), and acceptability to patient (n = 5).
TTJM specific factors – no contraindications (n = 36)
Thoracic spine education and professional development
The majority of respondents (n = 113) first received teaching of the thoracic spine at a postgraduate level with 83.7% reporting this occurring within specific course modules, short courses or in-service training. Of 196 respondents, 20% (n = 39) had never undertaken a thoracic spine professional development course. Of the other respondents, 56% (n = 110) had completed one or two courses, 15% (n = 30) three courses and 9% (n = 17) completed between four and six courses, although from free text responses few were specific to TTJM.
Therapeutic use of TTJM
The primary reasoning for choosing TTJM as a treatment option was reported by 161 respondents, with 54% primarily reasoning use for neurophysiological effects, followed by 44.7% for biomechanical effects, and 1.2% for placebo. Fifty-five respondents (18%) of the sample provided data for ‘other’ effects which as well as elaborating on justification for earlier choices included factors related to patient expectations/behavior (n = 23), perhaps perceived to have not been captured in the ‘placebo’ category.
Knowledge of potential AE
Overall, there were high levels of agreement (> 80%, inclusive of ‘completely’ and ‘somewhat agree’ responses) for many stated contraindications with the exception of ‘inflammatory disease’, ‘recent surgery‘, ‘vertebrobasilar ischemia or cervical artery dysfunction’, and ‘angina pectoris‘. For precautions less than half achieved this threshold of agreement, including ‘no change or worsening symptoms after multiple manipulations’, ‘previous adverse reaction to TJM’, ‘osteopenia’, ‘inflammatory process’, ‘psychological dependence on manipulations’, ‘systemic infections’, and ‘children’. Neutral responses were recorded by around a quarter of respondents for ‘arterial calcification’, ‘herpes zoster on the thoracic spine’, ‘arterial hypertension’, and ‘vertigo’. For red flags the majority achieved high levels agreement with the exception of ‘pain worsening with cough, sneeze or going to the toilet’, ‘numbness in upper or lower limbs or torso’, and ‘pins and needles in upper or lower limbs or torso’ with around 15% of these receiving a neutral response. In terms of risks only increase in pain local to the targeted region following TJM achieved > 80% agreement, with contrasting or neutral responses reported for the majority of those listed, notably ‘local discomfort/soreness’, ‘headache’, ‘fatigue’, ‘cervical, or vertebral artery dissection’. See Table 1.
Additional contraindications included ‘unexplained or unremitting pain’ (n = 9), ‘no consent’ (n = 7), ‘anxious/fearful patient’ (n = 6), ‘pregnancy’ (n = 4), ‘< 18 years’, ‘worsening or bilateral neurological symptoms’ (n = 2), others (n = 17) which included ‘discitis’, ‘systemically unwell’, ‘hypermobility’, ‘shingles’, ‘acute spasm’, ‘rib fracture’, ‘night pain’, ‘spinal infection’, ‘previous spontaneous pneumothorax’, evidencing some overlap between those perceived contradictions and precautions; and for red flags these included context specify factors (n = 4) and single responses for ‘unexplained weight loss’, ‘immunosuppressed’, ‘intravenous drug use’, ‘bilateral neurological symptoms’, ‘confirmed medical diagnosis, for example tuberculosis, cancer’, and ‘context specify factors’.
In line with current research guidance and author consensus, the risks were split into AE (more serious) and SE (temporary/transient) with findings suggesting marginally higher levels of agreement of AE (62.5%) compared to SE (56.1%) (Figure 2).
Figure 2.
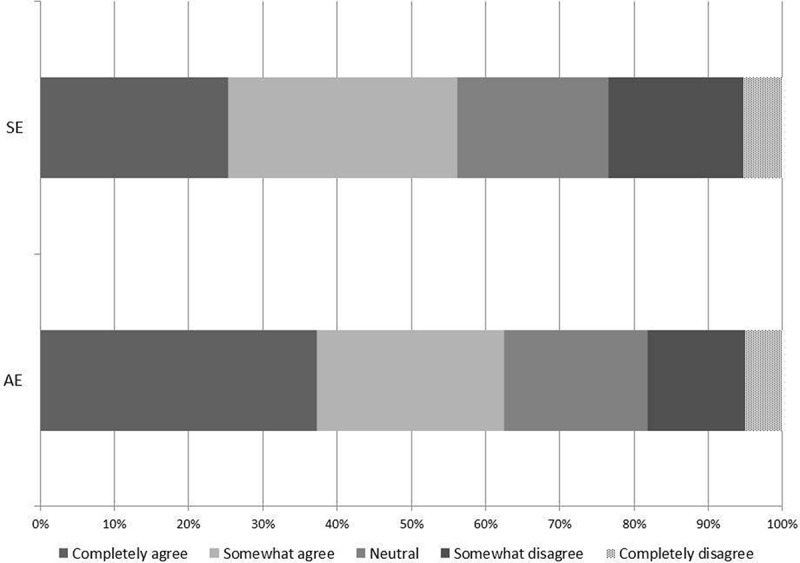
Level of agreement for SE and AE of TTJM.
Discussion
This is the first survey to investigate clinical practice of TTJM, providing valuable insights to inform future research and practice. Findings suggest that UK physiotherapists have some good knowledge of AE and SE associated with TTJM, yet a significant percentage do not utilize any form of pre-thrust examination. Moreover with almost half reasoning a biomechanical effect to support use of TTJM, something that is largely unproven, further attention is needed to reduce the evidence-practice gap to support safe and best practice.
Pre thrust examination
Only 40% of the sample utilized prethrust examination prior to TTJM, with considerable differences in practice from limited use of workplace standardized forms, to the majority utilizing either their own clinical reasoning or independently developed form for practice. This variability in practice and the documented under reporting of SE and AE [3,14,17] and potential for serious AE, highlights a need for further guidance to support clinical reasoning in practice. Our findings along with existing evidence offer a starting point from which this framework could be developed. Findings do indicate a level of reasoning around TTJM with evidence that pre-TTJM examination would be tailored according to thrust location, incorporating questions from the cervical spine prethrust examination for upper-TTJM and lumbar spine for lower-TTJM. This is an encouraging and important consideration given the poor accuracy of TJM [19] and positioning for some TTJM techniques placing stress on adjacent spinal regions, for example upper-TTJM techniques and cervical spine position.
Clinical use of TTJM
The survey highlighted the wide range of joints/complaints for which respondents utilize TTJM as part of management, where there is somewhat limited empirical support [7,20]. This widespread use of TTJM highlights the perceived contribution of the thoracic spine to a range of clinical complaints [9] and support for the model of regional interdependence [6]. With current clinical guidelines recommending thoracic mobilization/manipulation for neck pain [10], and a likely increase in the use of TTJM there is an urgent need to develop international best practice guidelines to minimize the risk of AE; as has been shown in the cervical spine [2,21].
Contraindications, precautions, red flags, and risks
Whilst the majority of the stated contraindications and red flags demonstrated high levels of agreement, some presentations yielded relatively high number of neutral response and in a few cases such as ‘pins and needles in upper or lower limbs or torso’ some disagreement. For many presentations more information would likely be required to precisely inform respondent decision-making prior TTJM, including TTJM location and patient specific factors such as coexisting symptoms, symptom behavior, age, general health, etc. Notwithstanding this it is a concern that almost a third of respondents did not agree that there is a risk of cervical and vertebral artery dissection with TTJM, although this is perhaps attributable to the preferred techniques being prone rotational TTJM or supine PA/AP TTJM which primarily target the mid-thoracic region and do not, unlike upper-TTJM place as much stress on the cervical spine. The lack of consistency across the majority of AE and all SE highlights a need for more clinical knowledge and research in this relatively underresearched spine region [9]. With seven case studies (age 17–71 years) citing injury to the spinal cord following TTJM [3] a system by which instances of AE can be recorded
in detail would usefully inform this relatively limited evidence base, a recommendation which has been made for both clinical practice and during training of TJM [14,17].
Therapeutic effect
Findings that TTJM is primarily for a biomechanical effect, something which is largely unproven [26], contrasts with evidence supporting a stronger case for the neurophysiological effects including pain relief via descending inhibition [27,28], increases in pain-pressure thresholds [29] and decreases in muscle inhibition [30]. Whilst this highlights a knowledge-practice gap the findings perhaps reflect the relatively small number of physiotherapists (15.4%) receiving preregistration TTJM education and a fifth not completing related post registration education.
Implications for future research
Findings highlight that the majority of UK physiotherapists do not regularly perform pre-TTJM examination, although the use of a survey does not allow for examining of clinical reasoning, which may be better captured with focus groups or semistructured interviews. A priority is now to establish whether important findings from this survey notably, the lack of prethrust examination and observed knowledge-practice gaps are reflected internationally. With the UK being a member organization of IFOMPT, an international survey is now required to inform the future development of best practice guidelines. Findings will also inform revisions and refinement of future e-survey design to incorporate, where appropriate findings from our analysis and strategies to optimize response rate [31].
Implications for future practice
Current research suggests that TTJM SE and AE are under-reported, and arguably a clearer distinction between SE and AE is needed for clinicians. This, alongside a centralized reporting system, would allow clinicians to confidently document the type and frequency of symptoms following TTJM. Further consideration of how to reduce the evidence-practice gap is needed alongside a greater awareness of the potential risks associated with TTJM, although ironically it is only in very recent years that a body of empirical evidence base supporting the use of TTJM for shoulder and neck complaints has emerged.
Strengths and limitations
This survey was informed by current evidence, experts, and designed to capture current UK practice. Whilst the overall sample size met an a priori sample size calculation, and response rate compares favorably to other e-surveys [31] some respondents did not complete all questions impacting on the participation rate and some findings then being based on results which fell short of the desired sample size for precision. However the sample characteristics suggest overall response representativeness was not impacted [32]. Where limited to UK-trained physiotherapists this may not be fully representative of practice in the United Kingdom, with a number of non-UK-trained practicing clinicians being ineligible. The use of multiple closed questions limits depth of analysis although as with other surveys this preliminary data gathering is vital to inform the development of methodologically robust research going forward.
Conclusion
UK-trained physiotherapists’ demonstrated good knowledge and agreement of TTJM contraindications, precautions, and red flags although more variability was seen for risks and therapeutic effects of TTJM. These knowledge gaps and variable use of pre-TTJM examination supports the need for further work. From this preliminary research, knowledge of international practices is now needed to inform development of a clinical reasoning framework for pre-TTJM examination.
Funding Statement
The authors would like to thank Arthritis Research Council and Musculoskeletal Association of Chartered Physiotherapists for funding to support completion of this project.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Adams G, Sim J.. A survey of UK manual therapists’ practice of and attitudes towards manipulation and its complications. Physiother Res Int. 1998;3(3):206–227. [DOI] [PubMed] [Google Scholar]
- [2].Puentedura E, Slaughter R, Reilly S, et al. Thrust joint manipulation utilized by U.S. physical therapists. J Man Manip Ther. 2016;25(2):74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Puentedura EJ, O’Grady WH. Safety of thrust joint manipulation in the thoracic spine: a systematic review. J Man Manip Ther. 2015;23(3):154–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Puentedura E, Landers M, Cleland J, et al. Thoracic spine thrust manipulation versus cervical spine thrust manipulation inpatients with acute neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2011;41(4):208–220. [DOI] [PubMed] [Google Scholar]
- [5].Struewer J, Frangen T, Ziring E, et al. Massive haemothorax after thoracic spinal manipulation for acute thoracolumbar pain. Orthopedic Reviews. 2013. 5 (3): e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Sueki DG, Cleland JA, Wainner RS. A regional interdependence model of musculoskeletal dysfunction: research, mechanisms, and clinical implications. J Man Manip Ther. 2013;21(2):90–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Cleland JA, Childs JD, Fritz JM, et al. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise and patient education. Phys Ther. 2007;87(1):9–23. [DOI] [PubMed] [Google Scholar]
- [8].Ganer N, Kulandaivelan S, Malik M, et al. Thoracic spinal manual therapy and regional interdependence: a review. Int J Health Sci Res. 2016;6(5):337–344. [Google Scholar]
- [9].Heneghan NR, Rushton A. Understanding why the thoracic region is the ‘Cinderella’ region of the spine. Man Ther. 2016;21:274–276. [DOI] [PubMed] [Google Scholar]
- [10].Blanpied PR, Gross AR, Elliott JM, et al. Clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American physical therapy association. JOSPT. 2017;47(7):A1–A83. [DOI] [PubMed] [Google Scholar]
- [11].Cagnie B, Vinck E, Beernaert A, et al. How common are side effects of spinal manipulation and can these side effects be predicted. Man Ther. 2004;9(3):151–156. [DOI] [PubMed] [Google Scholar]
- [12].Carlesso L, Rivett D. Manipulative practice in the cervical spine: a survey of IFOMPT member countries. J Man Manip Ther. 2011;19(2):66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Carnes D, Mars TS, Mullinger B, et al. Adverse events and manual therapy: a systematic review. Man Ther. 2010a;15(4):355–363. [DOI] [PubMed] [Google Scholar]
- [14].Thoomes-de Graaf M, Thoomes E, Carlesso L, et al. Adverse effects as a consequence of being the subject of orthopaedic manual therapy training, a worldwide retrospective survey. Musculoskelet Sci Pract. 2017;29:20–27. [DOI] [PubMed] [Google Scholar]
- [15].Haldeman S, Kohlbeck FJ, McGregor M. Unpredictability of cerebrovascular ischemia associated with cervical spine manipulation- a review of sixty-four cases after cervical spine manipulation. Spine. 2002;27(1):49–55. [DOI] [PubMed] [Google Scholar]
- [16].Kerry R, Taylor AJ, Mitchell J, et al. Manual therapy and cervical artery dysfunction, directions for the future: a clinical perspective. J Man Manipulative Ther. 2008;16(1):39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kranenburg HA, Schmitt MA, Puentedura EJ, et al. Adverse events associated with the use of cervical spine manipulation or mobilization and patient characteristics: A systematic review. Musculoskelet Sci Pract. 2017;28:32–38. [DOI] [PubMed] [Google Scholar]
- [18].Rushton A, Rivett D, Carlesso L, et al. International framework for examination of the cervical region for potential of cervical arterial dysfunction prior to orthopaedic manual therapy intervention. Man Ther. 2014;19(3):222–228. [DOI] [PubMed] [Google Scholar]
- [19].Ross JK, Bereznick DE, McGill SM. Determining cavitation location during lumbar and thoracic spinal manipulation: is spinal manipulation accurate and specific? Spine. 2004;29(13):1452–1457. [DOI] [PubMed] [Google Scholar]
- [20].Walser RF, Meserve BB, Boucher TR. The effectiveness of thoracic spine manipulation for the management of musculoskeletal conditions: a systematic review and meta-analysis of randomized clinical trials. J Man Manipulative Ther. 2009;17(4):237–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Puentedura E, March J, Anders J, et al. Safety of cervical spine manipulation: are adverse events preventable and are manipulations being performed appropriately? A review of 134 case reports. J Man Manip Ther. 2012;20(2):66–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of Internet e-surveys (CHERRIES). J Med Int Res. 2004;6(3e34):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Dillman DA. Mail and internet surveys: the tailored design method. 2nd ed Hoboken (NJ): John Wiley; 2007. [Google Scholar]
- [24].Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405. [DOI] [PubMed] [Google Scholar]
- [25].Carnes D, Mullinger B, Underwood M. Defining adverse events in manual therapies: a modified Delphi consensus study. Man Ther. 2010b;15(1):2–6. [DOI] [PubMed] [Google Scholar]
- [26].McCarthy C, Bialosky J, Rivett D. Section 3.1: principles of modern management. Chapter 29: spinal manipulation In:Jull G, Moore A, Falla D, et al editors. Grieve’s modern musculoskeletal physiotherapy. 4th ed Elsevier, London, UK;2015. [Google Scholar]
- [27].Skyba DA, Radhakrishnan R, Fohlwing JJ, et al. Joint manipulation reduces joint hyperalgesia by activation of monamine receptors but not opioid or GABA receptors in the spinal cord. Pain. 2003;106(1):159–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Bialosky JE, Bishop MD, Price DD, et al. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Fernandez-de-Las Penas C, Perez-de-Heredia M, Brea-Rivero M, et al. Immediate effects on pressure pain threshold following a single cervical spine manipulation in healthy subjects. JOSPT. 2007;37(6):325–329. [DOI] [PubMed] [Google Scholar]
- [30].DeVocht JW, Pickar G, Wilder DG. Spinal manipulation alters electromyographic activity of parsapinal muscles: a descriptive study. J Manipulative Physiol Ther. 2005;28(7):465–471. [DOI] [PubMed] [Google Scholar]
- [31].Nulty DD. The adequency of response rates to online and paper surveys: what can be done? Assess Eval Higher Educ. 2008;33(3):301–314. [Google Scholar]
- [32].Cook C, Heath F, Thompson RL. A meta-analysis of response rates in web- or internet-based surveys. Educ and Psychol Meas. 2000;60(6):821–836. [Google Scholar]


