Abstract
Foreign bodies get into the bladder by self insertion, migration or as a component of iatrogenic and penetrating injuries. Diagnosis and treatment pose great challenges to the urologist especially if they are radiolucent. A common pattern of presentation is with lower urinary tract symptoms. High index of suspicion is required in patient with lower urinary symptoms. We hereby report 5 cases of foreign bodies in the urinary bladder, 2 (40%) self inflicted, 2(40%) iatrogenic and 1(20%) due to migration of the object; as well as their successful management.
Conclusion
Foreign bodies in the urinary bladder still remain a great challenge to the urologist; removal of the foreign body without injury to the urinary bladder or the urethra gives good outcome.
Keywords: Foreign body, Urinary bladder, Self insertion, Iatrogenic, Migration, Successful extraction
Introduction
Foreign bodies in the urinary bladder pose urological challenges in terms of diagnosis and treatment. Ingress of foreign bodies into the urinary bladder may be by self insertion, iatrogenic, migration from adjacent organs and penetrating ballistic trauma1-10. The major route of entry is by self insertion through the urethra mainly for sexual gratification, or associated conditions like dementia, psychiatric disorders, drug intoxication and to procure abortion 4, 5, 7, 8, 10, 11. There is a marked preponderance of male patients 1, 12, 13, 14. A great diversity of objects has been found in the bladder as foreign objects. These include electric wires, bullets, mobile phone charger cable, thermometer, eyelid pencils, pieces of foley catheter, intra uterine contraceptive devices (IUCD), light bulb, surgical gauzes (retained guaze pieces), chicken and fish bones, orthopaedic screws, household batteries, hair ball, and broken parts of endoscopic instruments 1- 12, 15, 16. Those that insert foreign bodies to have sexual gratification present late due to guilt-feelings and embarrassment. Diagnosis is by detail clinical examination and appropriate investigations. Most of these patients may present with both irritative and obstructive lower urinary tract symptoms (urinary frequency, urgency, urinary retention), hematuria, urinary incontinence, and chronic pelvic pain7, 12, 15. Radiopaque foreign bodies will be seen on plain radiographs while ultrasonography will identify others. Urethrocystoscopy will visualize the object and its position in the urinary bladder. Treatment in each case has to be individualized based on the nature, location, size of the foreign body and the age of the patient 7, 12. We hereby report our experience in successful management of five cases of foreign bodies in the urinary bladder over a period of six years at the Federal Teaching Hospital, Abakaliki, Nigeria.
Case 1
A 70-year old farmer had acute urinary retention and was relieved by passing a size 16F two-way Foley catheter into the bladder and left indwelling in a peripheral clinic. Eight days post catheterization; he had intractable urethral pain at night and forcibly pulled on the catheter. He presented to us with a history of suprapubic pain, urinary frequency, urgency, hematuria and urinary retention, twenty four hours after the incident holding the catheter he pulled on. A history of alcohol intoxication was divulged on the night of the incident. Inspection of the catheter showed the distal balloon end missing. The patient was catheterized to relieve him of the retention and the bladder irrigated with normal saline. Abdominal ultrasonography showed the tip of the catheter, solitary stone and enlarged prostate. Ultrasonography gave the volume of the prostate as 332 cm3. Urethrocystoscopy confirmed the above findings. The patient was worked up for open prostatectomy and retrieval of the catheter tip and the bladder stone (Fig. 1). Psychiatric examination was unremarkable.
Fig. 1: Retrieved catheter tip and stone (Case 1).

Case 2
A 15-year old female secondary school student presented with a two weeks history of lower abdominal pain, dysuria, urinary frequency, urgency and later total painful hematuria. She was masturbating with an eyelid pencil when it disappeared into her body. Physical examination showed suprapubic tenderness and a linear object was palpable anterior to the vaginal vault. Trans abdominal ultrasonography showed a thick long linear structure in the urinary bladder (Fig. 2). Urine cultured E. coli sensitive to levofloxacin which was given and made the urine sterile. Thereafter, under spinal anesthesia, suprapubic cystotomy was done and the lid pencil (11cm long) was retrieved from the urinary bladder (Fig. 3). A psychiatric evaluation was normal. The patient was discharged five day post surgery.
Fig. 2: Ultrasonography showing foreign body in the bladder (Case 2).
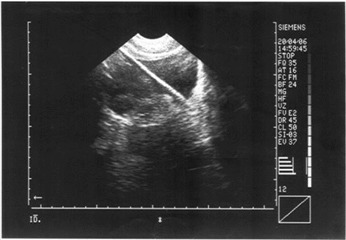
Fig. 3: Retrieved eyelid pencil from the urinary bladder (Case 2).

Case 3
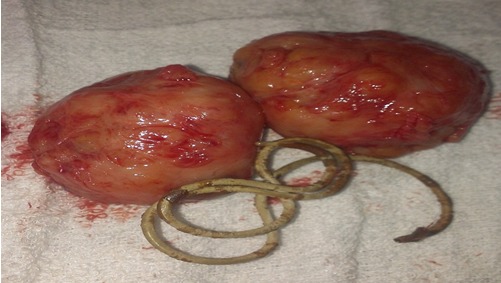
A 69-year old retired school principal presented with 14 day history of painful micturition, frequency of urine, nocturia, urgency, total hematuria. He had unfinished transurethral resection of the prostate due to transurethral resection syndrome 5 months prior to presentation. On examination, he was in acute urinary retention for which he was catheterized and had bladder irrigation with normal saline. Digital rectal examination revealed an enlarged prostate with benign features. Transrectal ultrasonography showed a coiled wire in the bladder and an enlarged prostate with benign features and a prostate volume of 131.1cm3. Cystoscopy showed the foreign body to be the wire loop of the resectoscope used for the previous endoscopic surgery. The patient was worked up and under spinal anesthesia, open prostatectomy was done during which the wire loop was removed (Fig. 4). The patient’s recovery was uneventful and was discharged 10 days post surgery.
Fig. 4: Retrieved wire loop of resectoscope plus prostate specimen (Case 3).
Case 4
A 47 years old female trader had a retained catheter after a laparotomy at a peripheral hospital. In an attempt to deflate the catheter at the hospital, the catheter was cut at the level of the urethral meatus but the distal balloon stump slipped into the urinary bladder She was referred two weeks later with urinary frequency, dysuria, painful total hematuria mixed with pus and suprapubic tenderness. Urine culture yielded heavy growth of Pseudomonas sensitive to ceftriaxon, which was appropriately treated. . Pelvic ultrasonography showed the catheter stump within the urinary bladder which was further confirmed on Cystoscopy. Attempt at removing the catheter piece endoscopically was unsuccessful. An open cystotomy was done and the catheter stump removed. The patient was discharged 5 days after surgery.
Case 5
A 68-year old female trader presented with a 14 day history of painful micturition, day time frequency, nocturia, intermittent total painful hematuria and suprapubic pain. She had a transabdominal hysterectomy 5 years earlier. On physical examination, she was pyrexic, had a midline abdominal scar and marked suprapubic tenderness. Urine examination showed numerous pus cells and red blood cells. Culture yielded heavy growth of Klebsiella and Pseudomonas species. Abdomino pelvic ultrasonography showed a mass within the lumen of the bladder posteriorly, measuring 6.7cm × 3.9cm casting posterior acoustic shadows in the urinary bladder. There was an associated fluid with multiple calculi embedded within. Urethrocystoscopy showed a mass of mixed echogenicity with calcifications. Antibiotics were administered according to sensitivity pattern. Via a suprapubic cystotomy, the urinary bladder was explored and the mass was gauze adherent to the posterior bladder wall. The gauze was dissected off the bladder wall and removed with the calculi, (Fig. 5). The bladder lumen was lavaged with saline. The bladder wall was thoroughly examined for any fistula but none found. The wound was closed and indwelling urethral catheter left in place. Post operative recovery was uneventful. The indwelling catheter was removed after ten days and the patient discharged home in good condition.
Fig. 5: Gauze and calculi retrieved from the urinary bladder (Case 5).

Discussion
The main findings in this study were that foreign bodies in the urinary bladder are rare as we encountered 5 cases over a period of 6 years. Irekpita et al in their study noted also the rare occurrence of foreign bodies in the urinary bladder 6. Furthermore, there were 3(60%) female patients and 2(40%) male patients in this series. This differs from other studies in which there is male preponderance 1, 12, 13, 14. Late presentation was the norm in all the patients due to ignorance and poverty thus worsening the morbidities encountered. In this series of foreign bodies in the urinary bladder, 2(40%) were self inflicted, 2(40%) iatrogenic and 1(20%) migration of retained gauze into the bladder following hysterectomy. Bansal et al in their study noted that iatrogenic and self inserted foreign bodies have become major contributors to the incidence of foreign bodies in the urinary bladder 5. The intractable urethral pain on a background of alcohol intoxication prompted the pulling on the indwelling catheter in case 1 while the sharp spikes of vesical stone were the platform for the shearing force that fragmented off the distal tip of the catheter. The second case of self insertion of eye lid pencil was for sexual gratification. The patient presented 13 days after the incident because of the shame and embarrassment associated with the condition 5, 12, 17. In the third case the wire loop of the monopolar resectoscope dislodged during the procedure of resecting the prostate. The prostate weighed 132 grams and was above the limit of 80 grams recommended for monopolar resection in one study 18. Hence the use of open surgery to remove the prostate and the wire loop Fig . The balloon of the urethral catheter retained in case 4 failed to deflate due to its poor quality and the method adopted to remove it was unprofessional hence the distal balloon end slipped into the urinary bladder. Use of high quality catheter will avert this type of incident. The surgical gauze in the urinary bladder in case 5 was found 5 years after hysterectomy. Any foreign body lying around the urinary bladder has the potential of migration into the bladder 2, 19. Gossypiboma denotes foreign material viz guaze sponges and towels inadvertently left in the body cavity after surgery 20. It derives from two sources Latin word “gossypium” meaning textile or cotton and the Swahili word “boma” meaning place of concealment 20, 21, 22, 23. Textiloma and gauzoma are other terminologies used 20, 23, 24. True incidence of gossypiboma is not known due to underreporting by physicians for medico legal reasons, humiliation, embarrassment and possible job loss. It has a reported incidence of 1 in 100 - 5000 of all surgical intervention and 1 in 1000 - 1500 for all intra abdominal operations 20, 23, 25. Furthermore 50% of gossypibomas are discovered as late as 5 years or more after surgery 26 and was first described by Wilson in 1884 27. Gossypiboma elicits two types of foreign body reactions: exudative leading to abscess formation and aseptic fibrinoid reaction leading to adhesions and encapsulation 28.In the index patient the gauze elicited chronic inflammation posterior to the bladder wall with eventual erosion into the bladder lumen. While in the lumen there was infective cystitis and calculi formation. Furthermore no fistula was seen on the bladder wall on close inspection. This phenomenon has been reported in other studies whereby the fistula healed up due to high vascularity of the bladder and dense fibrosis caused by the gauze 2, 19. Complications encountered before treatment in these series included urosepsis, stone formation, acute urinary retention. We used open cystotomy in all the patients to remove the foreign bodies and at the same time treat any coexisting pathology within the urinary bladder. No case of malignancy of the urinary bladder was encountered during follow up.
Conclusions
Foreign bodies in the urinary bladder still remain a great challenge to the urologist; removal of the foreign body without injury to the urinary bladder or the urethra gives good outcome.
Table 1. Summary of foreign bodies in the urinary bladder.
| No. of Patients | Age (Yrs) | Sex | Type of foreign Body | Circumstance of entry | Treatment |
| 1 | 70 | M | Catheter tip | Self Inflicted | Retrieved at open prostatectomy |
| 1 | 15 | F | Eye lid pencil | Self Insertion | Suprapubiccystotomy |
| 1 | 69 | M | Wire loop of resectoscope | Iatrogenic | Retrieved at open prostatectomy |
| 1 | 47 | F | Catheter tip | Iatrogenic | Suprapubiccystotomy |
| 1 | 68 | F | Surgical gauze | Migration | Suprapubic cystotomy |
References
- 1.Shimokihar K, Kawahara T, Hayashi Y, Tsutsumi S, Takamoto D, Mochizuki T, Uemura H. Foreign body in the bladder: A case report. Int. J. Surg. Case Rep. 2017;32:22–24. doi: 10.1016/j.ijscr.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Priyadarshi V, Sehgal N, Puri A, Singh JP, Bera MK, Pal DK. Migrated Intravesical Foreign Bodies: A Five Year Review. Med Sur Urol. 2016;5:2168–9857. [Google Scholar]
- 3.Ahmed ST, Alam A. An unusual foreign body in the urinary bladder: The art of management. . Helenic J Surg. 2016;88:234–237. [Google Scholar]
- 4.Zango B, Kabore FA, Kabore M, Kirakoya B, Ky BD, Yameogo C. Acute Generalized Peritonitis due to the migration of a ballpoint pen from bladder to great peritoneal cavity: A case report. Open J Urol. 2016;6:27–30. [Google Scholar]
- 5.Bansal A, Yadav P, Kumar M, Sankhwar S, Purkait B, Jhanwar A. Foreign bodies in the urinary bladder and their management: A single centre experience from north India. Int Neuro Urol J. 2016;20:260–269. doi: 10.5213/inj.1632524.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Irekpita E, Imomoh P, Kesieme E, Onuorah V. Intravesical foreign bodies: A case report and a review of the literature. Int Med Case Rep J. 2011;4:35–39. doi: 10.2147/IMCRJ.S18857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oguntayo OA, Zayyan M, Odogwu K, Koledade K, Mbibu H, Bello A. Foreign body (metallic flashlight cover) in the urinary bladder mimicking advanced cancer of the cervix: case report and review of the literature. Afr. J Urol. 2009;15:111–113. [Google Scholar]
- 8.Cyprien Z, Timothée K, Gustave S, Adama O, Alain T, Karim P. An Unusual Intravesical Foreign Body for Abortion Attempt. About a Case Report at Bobo Dioulasso University Teaching Hospital (Burkina Faso) and Literature Review. Open J Urol. 2014;4:33–36. [Google Scholar]
- 9.Ekenze SO, Ezomike UO, Offor I, Enyanwuma IE. Transperineal migration of a portion of a writing pen into the urinary bladder. Afr J Paed Surg. 2010;7:121–123. doi: 10.4103/0189-6725.62847. [DOI] [PubMed] [Google Scholar]
- 10.Hosseini SR, Rezaei H, Mohseni MG, Ganjali H, Behtash N, Arzani M. Screw as a bladder foreign body. Urol case rep. 2017;11:69–70. doi: 10.1016/j.eucr.2016.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kochakam W, Pummanagura W. Foreign bodies in the female urinary bladder. 20 year experience in Ramathibodi hospital. Asian J Surg . 2008;31:130–133. doi: 10.1016/S1015-9584(08)60073-1. [DOI] [PubMed] [Google Scholar]
- 12.Kesri G, Gupta P, Gupta HL, Sadasukhi TC, Dangayachi KK. An unusual self inflicted foreign body in the urinary bladder. IJMPCR. 2015;4:68–71. [Google Scholar]
- 13.Eckford SD, Persad RA, Brewster SF, Gingell JC. Intravesical foreign bodies; five year review. Br J Urol. . 1992;69:41–45. doi: 10.1111/j.1464-410x.1992.tb15456.x. [DOI] [PubMed] [Google Scholar]
- 14.Bakshi GK, Agarwal S, Shetty SV. An unusual foreign body in the bladder. J Postgrad Med. 2000;46:41–42. [PubMed] [Google Scholar]
- 15.Soomro H, Jalbani IK, Faruqui N. Intravesical foreign body: tertiary care center experience from Pakistan. J. Pak Med Asso. 2016;66:S131–S133. [PubMed] [Google Scholar]
- 16.Vezhaventhan G, Jeyaraman R. Unusual foreign body in the urinary bladder. A case report. The Internet J. Urol. 2006;4 [Google Scholar]
- 17.Mibang N, Faridi MS, Rahman J, Shantajit N, Lairammuana R, Somarendra K. Glass ampoule in urinary bladder as a foreign body. Asian J. Urol. 2016;3:96–98. doi: 10.1016/j.ajur.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Persu C, Geogescu D, Arabagui I, Cauni V, Moldoveanu C, Geavlete P. TURP for BPH. How large is too large? . J. Med. Life. 2010;3:376–380. [PMC free article] [PubMed] [Google Scholar]
- 19.Mylarappa P, Sirikantaiah HC. J Clin Diagn Res. Vol. 5. 2011; Calcified intravecical gossypiboma following abdominal hysterectomy. A case report. pp. 645–647. [Google Scholar]
- 20.Umunna JI. Gossypiboma and its complications. J West Afr Coll Surg. 2012;2:95–105. [PMC free article] [PubMed] [Google Scholar]
- 21.Patil KK, Patil SK, Gorad KP, Pandial AH, Arora SS, Gantum RP. Intraluminal migration of surgical sponge gossypiboma. Saudi J Gastroenterol. 2010;16:221–222. doi: 10.4103/1319-3767.65195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mungadi IA, Atahiru NA, Saidu SA. Vesical gossypiboma mimicking calculus: A report of two cases. Afric J Urol. 2007;13:136–138. [Google Scholar]
- 23.Samba A, Mumini K, Okpala AC. Gossypiboma: Retained surgical sponge after total abdominal hysterectomy with spontaneous transurethral partial extrusion. Gynecol obstet case rep. 2017;3:39. [Google Scholar]
- 24.Aghahowa ME, Achem FF, Umobong EO, Ojo BA. Gossypiboma or textiloma: A report of 2 cases and strategies for prevention. AJMCR. . 2014;2:123–125. [Google Scholar]
- 25.Chopra S, Suri V, Sikka P, Agganwal N. A case series on gossypiboma – varied clinical presantations and their management. J clin diagn Res. 2015;9:QR01–QR03. doi: 10.7860/JCDR/2015/15927.6978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang CC, Huang CJ, Hsieh JS. Paravesical gossypiboma following inguinal herniorraphy. Laparoscopic retrieval. J Minim Access Surg. 2015;11:216–217. doi: 10.4103/0972-9941.152099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Naeem M, Ahmad M, Samad A, Haq IW. Gossypiboma: A medical negligence. Pak J Surg. 2017;33:83–86. [Google Scholar]
- 28.Mohammad MA, Chukwuemeka AL, Aji SA, Tukur J, Diggoi GI, Ibrahim M. Intravesical migration of gossypiboma following vaginal hysterectomy: An unusual cause of acute urinary retention. Arch Int Surg. 2014;4:176–179. [Google Scholar]


