Abstract
Background:
Situational awareness errors may play an important role in the genesis of patient harm. The authors examined closed anesthesia malpractice claims for death or brain damage to determine the frequency and type of situational awareness errors.
Methods:
Surgical and procedural anesthesia death and brain damage claims in the Anesthesia Closed Claims Project database were analyzed. Situational awareness error was defined as failure to perceive relevant clinical information, failure to comprehend the meaning of available information, or failure to project, anticipate or plan. Patient and case characteristics, primary damaging events and anesthesia payments in claims with situational awareness errors were compared to other death and brain damage claims from 2002–2013.
Results:
Anesthesiologist situational awareness errors contributed to death or brain damage in 198 of 266 claims (74%). Respiratory system damaging events were more common in claims with situational awareness errors (56%) than other claims (21%, p<0.001). The most common specific respiratory events in error claims were inadequate oxygenation or ventilation (24%), difficult intubation (11%), and aspiration (10%). Payments were made in 85% of situational awareness error claims compared to 46% in other claims (p = 0.001), with no significant difference in payment size. Among 198 claims with anesthesia situational awareness error, perception errors were most common (42%), while comprehension errors (29%) and projection errors (29%) were relatively less common.
Conclusions:
Situational awareness error definitions were operationalized for reliable application to real-world anesthesia cases. Situational awareness errors may have contributed to catastrophic outcomes in three quarters of recent anesthesia malpractice claims.
Introduction
Accurate situational awareness is considered to be a core element for the non-technical skills of decision-making, team work, and task management.1–5 Situational awareness can be described as a hierarchical model where the basic level of perception (i.e., detection) describes the degree to which relevant information (e.g. patient history, information provided by monitors such as blood pressure or oxygen saturation) is perceived by the anesthesiologist. Once the information is perceived, the anesthesiologist integrates this information with long-term memory content in order to comprehend (i.e., diagnose) the patient´s medical condition (e.g., hypovolemia, pneumothorax). At the highest level, projection, the anesthesiologist projects (i.e., predicts) the patient’s state into the near future allowing for planning ahead and thus, for managing resources relevant for optimal treatment.1,4
Situational awareness errors in medical care can lead to patient harm. In 2009, the World Health Organization recognized that situational awareness plays an important role in clinical decision-making by physicians.6 Situational awareness errors may occur in surgery and anesthesia.5,7–10 Studies in surgery using observational techniques and review of operative notes suggested that complications of laparoscopic cholecystectomy (e.g., bile duct injuries) and carotid endarterectomy were associated with situational awareness errors, especially involving perception.5,7,8 In anesthesia, investigators in Australia9 and Germany10 reviewed voluntary critical incidents not resulting in patient injury and found a significant number of situational awareness errors (40 and 82%, respectively). In primary care11 and nursing12,13 situational awareness errors were studied qualitatively, but without quantitative data. The role of situational awareness errors in major injury associated with anesthesia has not been previously investigated.
This study investigated the role of situational awareness errors by an individual anesthesiologist in major patient injury (severe brain damage and death) using anesthesia malpractice claims. Due to the lack of validated classification of situational awareness in clinical anesthesia, our first study aim was to develop detailed protocol to operationalize definitions of perception, comprehension, and projection errors based upon the scientific literature.11,14 To assess the role of cognitive skills involving situational awareness, we focused on claims involving a single anesthesiologist (rather than anesthesia care team) to avoid misclassification with complex interactions with communication, team work, and different type of training among members of an anesthesia team. We used the Anesthesia Closed Claims Project database to examine trends in permanent brain damage and death. We then studied the frequency and type of situational awareness errors in these malpractice claims where patients died or suffered severe brain damage between 2002 and 2013. For those cases judged as having situational awareness errors, data are provided with respect to the patient and case characteristics, the cause of injury, and associated anesthesia payments.
Methods
Closed Claims Project Methodology
The Anesthesia Closed Claims Project database is a structured collection of closed anesthesia malpractice claims described in detail elsewhere.15,16 Briefly, on-site anesthesiologist-reviewers abstracted data from closed anesthesia malpractice claims onto detailed data collection instruments at participating professional liability companies across the United States. The panel of 16 companies (at the time of this study) insured approximately one third of practicing anesthesiologists in the United States. Information was collected from medical records, consultant evaluations, expert witness reports, claims manager summaries, and legal summaries. Data collected included patient demographics, type of surgery, details regarding anesthesia care, patient outcomes, and legal outcomes. The on-site reviewer evaluated the outcome, severity of injury, and cause of injury (i.e. damaging event), and summarized the claim in a brief narrative, including the sequence of events and causes of injury. The Closed Claims Project Investigator Committee reviewed the claims, and any disagreements in assessments were resolved by Committee members.
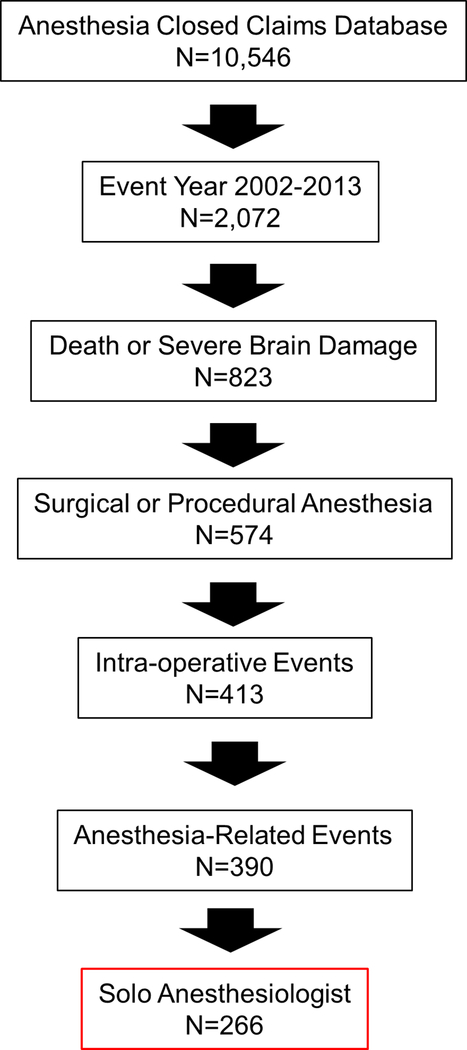
For this study, we used the Anesthesia Closed Claims Project database of 10,546 claims. Inclusion criteria were claims associated with surgical or procedural anesthesia care. Claims associated with obstetric anesthesia (including cesarean section) and pain medicine (acute or chronic) were not included. Additional inclusion criteria were based on the nature and phase of anesthesia care and the type of damaging event leading to injury. Claims with anesthesia-related damaging events that occurred intra-operatively were included; claims with injuries attributed to patient underlying condition, purely surgical events, or ambiguous events that could not be classified as to clinical cause were not included. Claims with damaging events occurring during other phases of anesthesia care (not intraoperative care) or outside the operating room were not included. As the study focused on situational awareness errors in individuals, only claims with care by a single physician anesthesiologist (rather than an anesthesia care team) were included. Analysis of trends in severe injury over time utilized all claims meeting inclusion criteria. In-depth analysis of the role of situational awareness error in severe injury was restricted to claims for death or severe brain damage that occurred in the years 2002–2013 that otherwise met inclusion criteria (Figure 1).
Figure 1:
Study inclusion criteria. The number of cases that met inclusion criteria are shown as each was applied to the Anesthesia Closed Claims Project database.
Definition of Variables
The damaging event in each claim was classified according to the primary mechanism that resulted in injury. Damaging events were grouped into the following categories: respiratory, cardiovascular, medication, equipment, regional block-related, or other. Examples of respiratory system events include difficult intubation, inadequate ventilation or oxygenation, and pulmonary aspiration. Examples of cardiovascular events include hemorrhage, electrolyte or fluid derangement, stroke, myocardial infarction, and pulmonary embolism. Medication events include wrong drug, wrong dose, and adverse drug reactions including malignant hyperthermia. Equipment events include cautery fires, central line insertion or management issues, anesthesia gas delivery equipment problems, and airway device injuries. Regional block related events include intravascular injection or absorption of local anesthetics and high blocks.
A situational awareness error in this study was defined as lack of situational awareness that contributed to patient death or brain damage. Two authors (CS, AB) assessed each claim for whether a situational awareness error occurred and whether it contributed to death or brain damage. Assessments were collected using REDCap (Research Electronic Data Capture)17 electronic data capture tools through a standardized questionnaire. An acceptable level of reliability κ (0.69) was achieved on a single round of assessment of a random sample of 100 cases. Disagreements were resolved by correspondence and/or discussion between these two authors, with resolution of remaining disagreements (n=8) by a third author (KBD).
If a situational awareness error contributed to death or brain damage, the team members involved in the error (anesthesia vs. surgical or other) were identified. Levels of situational awareness error were assessed for claims with errors by an anesthesiologist. The levels of situational awareness error were defined as perception (failure to perceive or misperception of information), comprehension (improper integration or comprehension of information), or projection (incorrect projection of foreseeable future trends). Given a lack of published operationalized definitions and examples of situation awareness levels in surgical or procedural anesthesia, we extended Singh’s adaptation of Endsley’s model to medical diagnosis to construct definitions and examples of levels of situation awareness in the clinical context of surgical and procedural anesthesia.11,14 We pretested our protocol (Table 1) on a subset of situational awareness error claims from the initial random sample of 100 cases, refining the definitions and examples on additional subsets of claims with situational awareness error until an acceptable level of inter-rater reliability was achieved. Acceptable reliability (κ = 0.40) for levels of situational awareness error was achieved on round three. While this met our a priori study measurement criterion, we decided to further refine the protocol to achieve a better level of reliability (κ = 0.53) with one additional round of coding using another subset of 25 claims.
Table 1:
Operationalized Definitions of Situational Awareness (SA) Error Levels
| If there were SA errors at multiple levels, code the lowest level of anesthesia SA error. |
| Level 1: Perception: What is the information? |
| Key issue: failure to gather information via history, physical exam, diagnostic tests, imaging or monitors, including absence of monitor(s) |
| • inadequate preoperative work-up (e.g. failure to question PO status or perform a more extensive cardiac evaluation) |
| • limited monitoring (e.g. equipment defect / missing, failure to place an arterial line); missing information was deleterious (e.g., missing arterial line) |
| • failure to monitor (missing ETCO2; no SpO2 reading, no arterial line; if there was no documentation that the patient was monitored, then assume the patient was not monitored (which is a level 1 error that not necessarily has to result in a level 2 or 3 error and that not necessarily has to contribute to death or brain damage) |
| • failure to check (perceive) a specific detail of the patient history / chart / test results that normally prompts a specific procedure or action (e.g. failure to consider patient name, low hemoglobin) |
| • Information was wrong (e.g. a documented value was wrong), regardless of the cause of wrong information (e.g. due to human error or other reason) |
| • non-awareness of the actions of other team members (such as the surgeon and nurses) |
| • non-awareness of equipment function (including potential problems) |
| • failure to communicate relevant information |
| • hidden information (visual barrier, e.g. drapes) |
| Level 2: Comprehension: What does the information mean? |
| Key issue: Failure to understand the significance of information obtained from history, physical exam, diagnostic tests, imaging findings, or monitors. The information was available, but it was not understood or misunderstood. If a decision (or no-decision, as illustrated by missing re-actions / non-actions) turns out wrong in face of a deteriorating event that occurred (just) in the past. |
| • failure to make the correct diagnosis |
| • failure to comprehend the cause and meaning of information (e.g. heart rate that is not within normal limits, 300–400 cc filling drains in few minutes – empty, drains continue to fill – reasonable physician would conclude patient is bleeding, likely need to draw labs, give blood, possibly return to OR) |
| • If there is information that patient is deteriorating and reasonable clinician would make diagnosis and act/react– if the physician(s) in case do not react in such a manner, conclude that this diagnosis not made/failed to comprehend |
| Level 3: Projection: What is likely to occur? |
| Key issue: Failure to forecast future events or scenarios based on a high-level understanding of the situation; failure to forecast potential outcomes based upon a chosen plan; poor planning for future events or poor/absence back-up plan. |
| If a decision turns out wrong in face of unanticipated events (e.g. well-known complications) that occur in the future: Level III.” |
| • Poor anesthetic plan (e.g. routine anesthesia plan for patient with known complex medical history or known significant comorbidities; office based anesthesia for patient with significant comorbidities; failure to plan for possible difficult airway in patient with obvious risk |
| • Proactive measures were not taken adequately although the deterioration was likely to occur or not surprising, retrospectively |
| • Failure to call for help to manage likely future complication / problems |
We defined an error of perception as failure to gather information via history, patient chart, physical exam, diagnostic tests, imaging or monitors, including absence of monitor(s) (Table 1 provides the protocol with clinical examples). Following the Endsley model of situational awareness as a dynamic process, we defined perception as encompassing both the active seeking of information as well as the passive receiving of information.18,19 Therefore, failure to seek information and failure to receive information were both defined as perception errors. Comprehension errors were defined as failure to understand the significance of information obtained from history, physical exam, diagnostic tests, imaging findings, or monitors, that is, the information was available but it was not understood or was misunderstood, which led to an incorrect diagnosis. The definition of comprehension errors relied heavily on the model put forth by Singh with its emphasis on diagnosis.11 Projection errors were failure to forecast future events or scenarios based on a high-level understanding of the situation.18 This included failure to forecast potential outcomes based upon a chosen plan, poor contingency planning, or poor/absent back-up plan. Because an error of perception nearly always leads to errors of comprehension and projection, if there were situational awareness errors at multiple levels, the lowest level of anesthesia situational awareness error was coded.20 The same two authors (CS, AB) assessed the level of situational awareness error and disagreements (n= 3) were resolved by discussion or the third author (KBD).
The severity of injury in each claim was assigned using the National Association of Insurance Commissioners’ 10-point scale which ranges from 0 (no apparent injury) to 9 (death).21 In this study brain damage was defined as brain damage with permanent disabling injury (score 6–8). The severity of injury represents the assessment at the time the claim was closed. A claim with severe brain damage resulting in death before claim closure was classified as death.
Statistical Analysis
Inter-rater reliability for the assessment of situational awareness error vs. no error (binary assessment) and inter-rater reliability for levels of situational awareness error (classification into one of three response categories) was measured by independent assessment of random samples from the study dataset using κ scores calculated on the initial two author judgments before discussion or tie-breaking by the third author. Κ values are calculated based on expected vs. observed probabilities across response categories. These values may be biased by a large number of response choices (resulting in low expected probabilities and rendering high κ values more likely) or highly uneven use of response choices (resulting in high expected probabilities, rendering high κ values difficult to achieve). With two and three response categories and fairly even distribution of responses in our data, κ scores above 0.4 were considered acceptable.22 All payments made to the plaintiff were extracted from the database and adjusted to 2015 dollar amounts with the Consumer Price Index.23 Median and interquartile range were reported for payments because they were not normally distributed. Claims with no payment were excluded from calculation of median and interquartile range. Trends in death and brain damage over time were reported as percentage of all claims per year meeting inclusion criteria. Years prior to 1980 with <50 total claims were combined sequentially to form groups with ≥ 50 claims. All claims from these years have closed and been entered into the database. The database is incomplete for events that occurred since 2004, as many of those claims are still open and some that have closed have not yet been collected and incorporated into the database; the rate of death and brain damage in 2009–2013 were calculated but may change considerably as additional claims from those years are added to the database. The years 2012–2013 have been combined due to very small denominators in those years. Characteristics of anesthesia situational awareness error claims were compared to all other claims meeting study inclusion criteria (“other claims”: no situational awareness error, surgical situational awareness error, or insufficient information) using chi square test, Fisher’s exact test, t-test for equality of means (age), or Mann-Whitney U-test (payment amount). All statistical analysis employed SPSS 22 for Windows (IBM Corporation, Armonk, New York, USA) with p<0.05 as the criterion for statistical significance and two-tailed tests. No a priori power calculation was conducted; the analyses were based on the available data.
Results
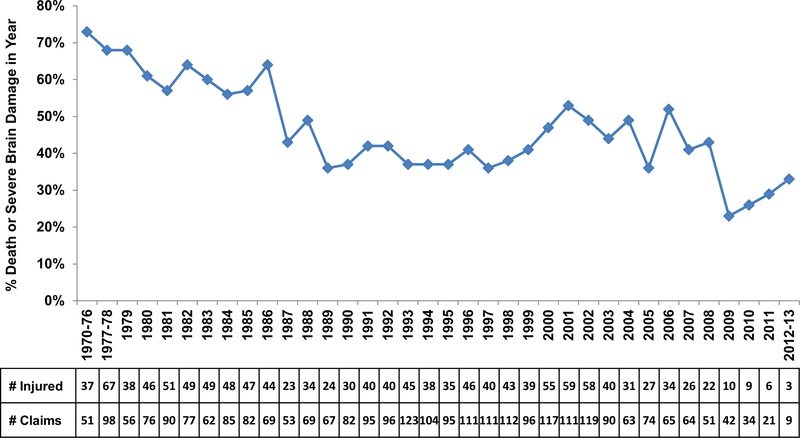
The proportion of claims for death or severe brain damage declined from 73% (n=37) of 51 claims in 1970–76 to 36% (24/67) in 1989, remaining in the 36–38% range through 1998. From 1999–2008, the proportion of death and severe brain damage varied from 41% to 52% (391/850, averaging 46%, Figure 2). In the years 2002–2013, 198 (74%) out of 266 claims had a situational awareness error by an anesthesiologist (e.g. “errors”) that contributed to patient death or brain damage (κ = 0.69). The remaining 68 (26%) claims in 2002–2013 included claims with no anesthesia error contributing to death or brain damage (n=50), surgical errors (n=10), and claims with insufficient information (n=8). Among 198 claims with anesthesia errors, errors of perception were most common (n=83, 42%), while errors of comprehension (n=58, 29%) and projection (n=57, 29%) were relatively less common (κ= 0.53). There was no difference by year of event in the relative frequency of error claims compared to other claims (p=0.71).
Figure 2:
Trends in death and brain damage in the Anesthesia Closed Claims Project database by year of event. The x-axis is year of event. Years prior to 1980 with <50 total claims were combined sequentially by year to form time periods with at least 50 claims. All claims from these years have closed and been entered into the database. The database is incomplete for events that occurred in 2009–2013, as many of those claims are still open and some that have closed have not yet been collected and incorporated into the database; the rate of death and brain damage in 2009–2013 may change as additional claims from those years are added to the database. The years 2012–2013 have been combined due to very small denominators in those years. The data table shows the number of claims for death or brain damage (# injured) each year and the total number of claims in the database meeting inclusion criteria (# claims).
Characteristics of situational awareness error claims vs. other claims
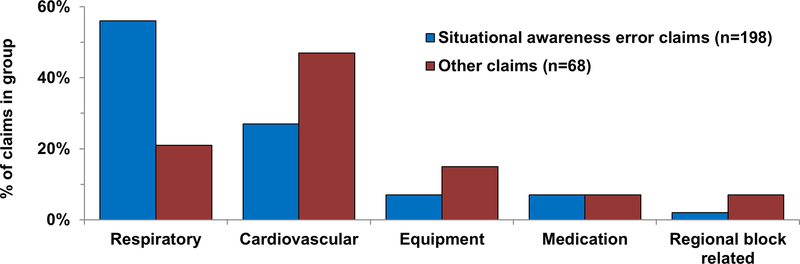
Patients in claims with errors tended to be younger than patients in other claims by an average of 6 years, but most were middle-aged (mean 50 vs. 56 years, p=0.023, Table 2). There were no other associations between patient characteristics and errors. Errors were not more common in emergency vs. routine cases (Table 2). The primary damaging event differed between error claims and others (p<0.001, Figure 3). In claims with errors, respiratory events were dominant (56%), whereas the most frequent primary damaging events in claims without errors were cardiovascular (47%, Figure 3). The most common specific respiratory events in claims with errors were inadequate oxygenation or ventilation (24% of errors), difficult intubation (11%), and pulmonary aspiration (10%, Table 2). The most common respiratory events in claims without anesthesia errors were pulmonary aspiration (9%) and difficult intubation (6%). Hemorrhage was the predominant cardiovascular system event in claims with errors (10%). In claims without errors, the most common cardiovascular events were hemorrhage (12%), myocardial infarction (6%), and pulmonary embolus (6%, Table 2).
Table 2:
Patient and Case Characteristics
| SA Error Claims N (% of 198) | Other Claims N (% of 68) | P | ||
|---|---|---|---|---|
| Male | 108 (55%) | 42 (62%) | 0.300 | |
| Adult | 189 (95%) | 66 (97%) | 0.735 | |
| Age in yrs: mean [SD] | 50 [18] | 56 [17] | 0.023 | |
| Obese (n=214) | 89 (54%) | 23 (47%) | 0.389 | |
| ASA Physical Status 3–5 (n=264) | 125 (64%) | 50 (74%) | 0.143 | |
| Emergency (n=263) | 45 (23%) | 14 (21%) | 0.783 | |
| Outpatient (n=260) | 59 (31%) | 12 (18%) | 0.045 | |
| Primary Anesthetic | 0.053 | |||
| General Anesthesia | 143 (72%) | 57 (84%) | ||
| Monitored Anesthesia Care | 46 (23%) | 7 (10%) | ||
| Regional Anesthesia | 9 (5%) | 4 (6%) | ||
| Most Common Damaging Events* | <0.01 | |||
| Respiratory Events | 111 (56%) | 14 (21%) | ||
| Inadequate oxygenation/ventilation | 48 (24%) | 2 (3%) | ||
| Difficult intubation | 21 (11%) | 4 (6%) | ||
| Pulmonary aspiration | 20 (10%) | 6 (9%) | ||
| Cardiovascular events | 53 (27%) | 32 (47%) | ||
| Hemorrhage | 19 (10%) | 8 (12%) | ||
| Myocardial infarction | 0 (0%) | 4 (3%) | ||
| Pulmonary embolus | 0 (0%) | 4 (6%) | ||
| Payment made (n=265) | 169 (85%) | 31 (46%) | <0.001 | |
| Median payment | $567,450 | $387,000 | 0.163 | |
| Interquartile range | $263,250-$1,096,500 | $191,400-$937,500 | ||
Payments made on behalf of the anesthesiologist and/or anesthesia corporation or group adjusted to 2015 dollar amounts. Claims with missing information were excluded. Claims with no anesthesia or anesthesia corporation payment excluded from median/interquartile range. p-values by chi square test, Fisher’s exact test (adult, primary anesthetic), t-test (age), and Mann Whitney U-test (payment amount) with Monte Carlo estimates are based on 10,000 randomly sampled tables. SA =situational awareness; SD = standard deviation; ASA = American Society of Anesthesiologists
Other primary damaging events shown in Figure 3.
Figure 3:
Most common damaging events by anesthesia situational awareness error vs. other claims. Miscellaneous other events not shown. P<0.001 between distribution of events by error/other by chi square test. P<0.01 by post hoc chi square test for respiratory events and cardiovascular events by error/other.
Payments made on behalf of the anesthesiologist and/or anesthesia corporation group were significantly more frequent in claims with errors (85%) than in other claims (46%, p<0.001, Table 2). When a payment was made, the size of payment did not differ between claims with errors and other claims (Table 2).
Most common events by level of situational awareness error: perception, comprehension, projection
Greater than half (60%) of the 83 perception errors involved respiratory system events, while 20% were cardiovascular system events. Respiratory events resulting from errors of perception were characterized by absence of respiratory monitoring resulting in inadequate oxygenation and/or ventilation (n=37, Table 3). Lack of ETCO2 and/or SpO2 monitoring, and absent alarms, lead to missing information and consequently failure to perceive the patient’s declining respiratory status, often until after cardiac arrest occurred. Perception errors also included inadequate preoperative evaluation and missing preoperative information that lead to inappropriate anesthesia plans and management (Table 3).
Table 3:
Examples of Errors of Perception, Comprehension and Projection
| Level 1: Perception - What is the information? Key issue: failure to gather information via history, physical exam, diagnostic tests, imaging or monitors, including absence of monitor(s) | ||
| Case Type | Case Description | Error Description |
| Cardiac arrest | 35–39 y.o. ASA 3–5 male with history of mental retardation, obesity, hypertension and NIDDM admitted for a urology procedure under GA. Cardiology work-up for difficulty breathing revealed dilated cardiomyopathy, EKG changes, and ejection fraction of 15%. The echo results were not in the records preoperatively. The patient’s family did not relate any cardiac history to the anesthesiologist preoperatively. The patient arrested during surgery, was resuscitated, but arrested again in the ICU and died. | Failure to gather information: preoperative test results not in the records; family did not relay information to anesthesiologist. |
| Pulmonary aspiration | 70–74 y.o. ASA 4 male inpatient with aortic stenosis and regurgitation, post aortic valve replacement, and CHF scheduled for cardiac defibrillator battery replacement. Preoperative evaluation also revealed morbid obesity and a bull neck. On the morning of surgery, the anesthesiologist asked the patient if he had eaten and the patient provided an unclear answer. The anesthesiologist did not query the nurses regarding NPO status. During induction of anesthesia, the patient had emesis consisting of food. The patient’s airway was suctioned and he was intubated, but developed ARDS and eventually died. It was later discovered that the patient had been served breakfast on the day of surgery. | Failure to gather information: Anesthesiologist failed to ascertain NPO status preoperatively. |
| Inadequate ventilation/oxygenation | 50–55 y.o. ASA 3 woman with comorbidities including coronary stents, congestive heart failure, pacemaker, and pulmonary edema 1 month prior for cataract extraction under monitored anesthesia care. The anesthesiologist administered midazolam and fentanyl in the holding area. The patient was then transported unmonitored to the operating room. Upon arrival 2–4 minutes later, she was unresponsive and apneic. She was resuscitated but arrested again two days later and died. | Failure to gather information – absence of monitors: Failure to monitor patient during transport after administering pre-induction drugs. |
| Inadequate ventilation/oxygenation | 70–75 y.o. ASA 3 man for colonoscopy under MAC. Monitors included EKG, FiO2 and ETCO2. The patient was given propofol and O2 delivered by nasal prongs. The anesthesiologist was chatting with the GI physician and not paying attention to the monitors. It was noted that the patient was not breathing. A code was called, LMA inserted, and 100% O2 administered. Saturations could not be obtained as the patient was in asystole. The patient was resuscitated but eventually died. The severity of the encephalopathy suggested a prolonged period of desaturation. | Non-awareness of equipment function: Anesthesiologist was not attentive to the monitors. |
| Inadequate oxygenation/ventilation | 60–65 y.o. morbidly obese ASA 3 man for elective screening colonoscopy under MAC. Numerous comorbidities included COPD requiring O2 at night. The patient was given a small dose of propofol for the procedure and received 3 L/min O2 via nasal cannula. The room was small and the anesthesiologist could not see the monitoring equipment. Severe bradycardia occurred and then the patient arrested. The procedure was aborted, and resuscitation attempts resulted in return of spontaneous circulation after 15 minutes. The patient was admitted to the ICU after he was resuscitated, but his condition continued to decline. Life support was withdrawn twelve days later, and he died shortly thereafter. | Failure to gather information – hidden information: Anesthesiologist could not observe monitoring equipment in small room. |
| Level 2: Comprehension: What was the diagnosis? Key issue: Failure to understand the significance of information obtained from history, physical exam, diagnostic tests, imaging findings, or monitors. The information was available, but it was not understood or misunderstood. | ||
| Case Type | Case Description | Error Description |
| Hemorrhage | 40–44 y.o. ASA 2 woman underwent an elective laparoscopic-assisted vaginal hysterectomy for endometrial cancer under general anesthesia. About an hour into the procedure, the surgeons encountered severe uterine bleeding. The anesthesiologist was aware of this event and treated hypotension with doses of ephedrine 10mg, phenylephrine 100 mcg. The blood pressure fell, the patient developed pulseless electrical activity, and resuscitation was begun. Fluid resuscitation by the anesthesiologist was inadequate and the patient became hypovolemic and acidotic, progressing to ventricular fibrillation. The patient was resuscitated and taken to ICU where she remained hemodynamically unstable and died the following morning. Cause of death on autopsy was hypovolemic shock. | Failure to comprehend the meaning and significance of information: The anesthesiologist perceived hypotension and bleeding but did not correctly comprehend the severity of bleeding resulting in inadequate treatment. |
| Esophageal intubation | 60–65 y.o. ASA 2 woman with history of a difficult intubation was scheduled for partial thyroidectomy under GA. After preoxygenation, GA was induced and the ETT placed. The anesthesiologist documented equal breath sounds bilaterally and negative gastric sounds; ETCO2 was zero, interpreted as monitor malfunction. Over 10 minutes, BP and SpO2 dropped; then the patient became bradycardic progressing to asystole, treated with CPR and atropine/ epinephrine. Twenty minutes after intubation, the patient was extubated and re-intubated, CPR continued, and ETCO2 increased to 38–40. The case was cancelled, and the patient taken to ICU. She was found to have hypoxic brain damage and did not regain consciousness. Review of the vital signs in the monitor after the event showed no ETCO2 and falling SpO2 during the 20 min episode. | Failure to understand monitoring information: Information was available (no ETCO2 on monitor) but was misinterpreted as machine malfunction, leading to failure to diagnosis esophageal intubation. |
| Tension pneumothorax | 45–50 y.o. female for arthroscopic shoulder repair under GA in a free standing ambulatory surgery center. The 3 hour surgery proceeded uneventfully. The patient was not ventilating well at the end of the surgery, so she was taken to the PACU intubated; SPO2 was 99% on admission. The patient’s SPO2 decreased over 15–20 minutes to the low 90’s, and finally to 64% when she arrested. CPR was performed and paramedics were called for transfer to the hospital ER. The patient was noted to have severe subcutaneous air. Bilateral thoracotomies were performed and an x-ray showed her lungs had expanded with significant pneumomediastinum and subcutaneous air. The ETT that was placed was in good position. The patient sustained significant permanent brain damage. | Failure to diagnose: Anesthesiologist did not diagnose patient’s oxygen desaturation postoperatively. |
| Level 3: Projection: What is likely to occur? Key issue: Failure to forecast future events or scenarios based on a high-level understanding of the situation; failure to forecast potential outcomes based upon a chosen plan; poor planning for future events or poor/absence back-up plan. | ||
| Case Type | Case Description | Error Description |
| Difficult re-intubation | A 40–50 y.o. ASA 2 obese woman underwent septoplasty and endoscopic sinus surgery. The anesthesiologist expected a difficult intubation. When he could not place an ETT via direct laryngoscopy, the anesthesiologist placed a LMA and eventually an ETT. Upon completing the procedure, the patient was extubated, but began to “flail and bite her tongue” and desaturated. The anesthesiologist placed another LMA and the saturation improved. A fiberoptic intubation was performed, but was unsuccessful. The LMA was replaced and a tracheostomy was performed as the patient became hypoxic and bradycardic. The patient transiently responded to atropine and epinephrine, but she eventually became asystolic. Resuscitation efforts were terminated after one hour. | Failure to plan for future events: The anesthesiologist anticipated and managed difficult intubation, but did not have an adequate extubation plan for a patient with a known difficult airway. |
| Inadequate anesthesia plan | 50–55 y.o. ASA 3–5 morbidly obese male suffering from severe aortic stenosis was admitted to the hospital with a-fib and pulmonary congestion. He also had cardiomegaly and elevated ventricular rate above 100. A transthoracic echo showed ventricular dysfunction and moderate aortic insufficiency. Cardiologists wanted to proceed with transesophageal echo with TEE-guided electrical conversion in the hope of converting him to sinus rhythm. The anesthesiologist administered a high dose (100mg) of propofol for sedation. The patient became hypoxic and bradycardic. The anesthesiologist attempted to ventilate with Ambu® bag but was not successful. The patient was intubated, and BP and heart rate returned to normal. The patient suffered anoxic brain injury and was left with permanent neurologic injury. | Poor anesthetic plan for patient with known significant comorbidities including morbid obesity: Anesthesiologist plan for heavy sedation in patient with severe cardiac disease including sedative agent with known BP effects, high sedative dose and failure to anticipate difficult mask ventilation indicates poor planning. |
| Difficult intubation | 25–30 y.o. ASA 3 female with stage IV colon cancer and submental salivary gland abscess which caused difficulty swallowing. A CT scan showed fluid collection at the floor of the mouth. She was taken to the OR for surgery under GA. The patient was induced with 140mg propofol, 220mg succinylcholine, 100mg lidocaine, and 250mcg fentanyl. The anesthesiologist was unable to see the cords with direct laryngoscopy and called for a Glidescope®, which was in another OR. The anesthesiologist was unable to ventilate; SPO2 was 85% and falling. Code was called and CPR begun. The anesthesiologist asked the nurse to bring a cricothyrotomy kit, but it was not readily available. The anesthesiologist proceeded to search for a difficult airway cart; the patient was not being ventilated during this time. Eventually the cricothyrotomy kit was provided and the surgeon performed a tracheostomy. The patient sustained severe brain damage and remained in a persistent vegetative state with need for total custodial care. | Poor plan – absence of backup plan: Anesthesiologist failed to have appropriate difficult airway equipment and plan for induction of GA in patient with airway pathology and potential obstruction. |
a-fib = atrial fibrillation; ARDS = acute respiratory distress syndrome; ASA = American Society of Anesthesiologists; BP = blood pressure; COPD = chronic obstructive pulmonary disease; CPR = cardio-pulmonary resuscitation; CT = computed tomography; EKG = electrocardiogram; ER = emergency room; ETCO2 = end-tidal carbon dioxide; ETT = endotracheal tube; FiO2 = fraction of inspired oxygen; GA = general anesthesia; GI = gastrointestinal; ICU = intensive care unit; L = liter; LMA = laryngeal mask airway; MAC = monitored anesthesia care; mcg = micrograms; mg = milligrams; min = minute; NIDDM = non-insulin dependent diabetes mellitus; O2 = oxygen; OR = operating room; PACU = post-anesthesia care unit; SpO2 = peripheral capillary oxygen saturation; TEE = transesophageal echo; y.o. = year old
Errors of comprehension (n=58) were equally divided between respiratory and cardiovascular events (n=23 each). Respiratory system events that were not comprehended appropriately included inadequate oxygenation or ventilation, difficult intubation, bronchospasm, and pulmonary aspiration. In multiple cases of difficult intubation, the anesthesiologists clearly perceived the difficulty as multiple attempts at intubation were described, but the extent of ongoing difficulty was not adequately comprehended as intubation attempts continued without changes in technique while the patient deteriorated. In these elective cases, the patient could have been awakened or an LMA used as a bridge for airway management, but the full difficulty of the airway management was not comprehended and these steps not taken. Errors of comprehension of inadequate oxygenation or ventilation was characterized by a similar lack of understanding of the ongoing seriousness of the clinical situation and continued deterioration of the patient. Half (n=11) of the cardiovascular system events with comprehension errors involved hemorrhage, with a typical example presented in Table 3.
Errors of projection (n=57) most commonly involved failure to anticipate or plan for difficult airway management (n=15) and pulmonary aspiration (n=11), which together accounted for approximately half of the projection errors. Difficult airway management projection errors included both lack of plans for intubation on induction and lack of plans for extubation of patients who had been difficult to intubate on induction (Table 3). Planning routine anesthetics that did not take into account severe patient comorbidities, often in ambulatory surgery centers or office locations, were also common errors of projection. Other projection errors involved lack of planning for fire prevention in high risk cases (cautery + open oxygen + procedure above the chest).
Discussion
Our study suggests that situational awareness errors may have contributed to catastrophic outcomes in three quarters of anesthesia malpractice claims in which patients died or sustained permanent brain damage from 2002–2013. Consistent with a model describing the crucial role of situational awareness in anesthesia,1 these findings suggest that lack of situational awareness may play an important role in the genesis of patient harm.
Previously, using all available closed claims, Cheney identified a decrease in the proportion of anesthesia malpractice claims for death and brain damage between 1975–2000.24 Our study identified a plateau in the proportion of claims for death and severe brain damage in anesthesia malpractice claims involving intraoperative care by a single anesthesiologist extending through 2013. The reasons for this are not clear, and potential factors such as increasing patient co-morbidities were beyond the scope of the current inquiry. However, this finding suggests that further improvements in anesthesia patient safety require new theoretical approaches to analyze adverse events. Situational awareness represents one such approach.1
This is the first study to develop a detailed protocol to assess the role of situational awareness errors in anesthesia-related severe injury. Using a detailed protocol with anesthesia-specific examples (Table 1), inter-rater reliability was substantial with respect to whether an error occurred (κ = 0.69) and acceptable (κ = 0.53) with respect to assessment of the specific level of error. We defined non-use of anesthesia monitors as errors of perception. Unlike aviation where standard gauges are present in every cockpit, in anesthesia practice the decision to use or not use many monitoring devices is part of the anesthesia plan, based on the patient, procedure, and other factors. While one could argue that lack of some monitors such as capnography during monitored anesthesia care is a poor plan and therefore an error on the level of projection, we considered such errors as perception errors, based upon the situational awareness scientific literature.14 If a monitor is not used, the information is not available, similar to lack of specific preoperative tests that results in absence of information for potential perception. This definition of perception errors is based on the premise that gathering information is an active process, beyond simple vigilance.1,18,19
The frequency of situational awareness errors in this study (74%) was consistent with the range in studies that investigated situational awareness errors in anesthesia incident reports (82%)10 and aviation (59 – 88 %).14 The types of errors in malpractice claims differed in relative frequency from critical incident reports where there was a risk but no actual injury. In incident reports, perception errors were also the most frequent, but projection errors (15%) were almost twofold less frequent than in this study of malpractice claims (29%).10 The Australian study did not analyze levels of situational awareness.9 Different case characteristics, the voluntary character of the incident reporting system, and the subjective view of the reports significantly limit comparability.
Perception Errors
Many of the perception errors stemmed from lack of, or lack of attention to, respiratory monitoring. This is consistent with Bhanankar’s finding that 44% of claims due to oversedation during MAC were judged to be preventable by better use of, or by additional monitoring.25 Another common perception error was missing preoperative information, often associated with inadequate preoperative evaluation (Table 3). This finding speaks to a common anesthesia situation that, while not emphasized in previous analyses of anesthesia malpractice claims, represents an important safety risk to patients. Anesthesiologists may elect to proceed with a routine procedure in the absence of important preoperative history and test results. While alternative analytic models could be applied to these cases, in the framework of situational awareness they represent errors at the most basic level – missing information essential to comprehension and planning of a safe anesthetic course.
Comprehension Errors
The most common comprehension errors involved respiratory and cardiovascular events (especially massive hemorrhage). Previous analysis of massive hemorrhage claims revealed team communication and management problems which led to death and brain damage.26 The situational awareness theoretical approach provides new insights into diagnostic error or diagnostic delay of massive hemorrhage. This illustrates the value of different theoretical models for similar events: both models provide important clinical insights into anesthesia patient safety problems potentially demanding differing solutions.
The comprehension errors related to respiratory management most commonly involved lack of comprehension of the ongoing clinical difficulty and the need to change course. Clinical algorithms and emergency manuals may have potential in such situations by limiting the repetition of the same clinical approach when improvement is not forthcoming. This has been shown previously in an analysis of claims for difficult airway management in which claims for difficult intubation on induction of anesthesia after adoption of the ASA difficult airway algorithm had improved outcomes compared to earlier claims. 27
Projection Errors
The projection errors frequently involved anticipation of difficult airways and pulmonary aspiration. In addition, procedure planning in an inappropriate environment (such as very sick patients in offices or outpatient settings) is a liability risk that has not been revealed in previous closed claims analyses using alternative analytic frameworks. Fire risk is not a new finding but significant in the context of the current analysis that was restricted to claims for death and brain damage. Most on-patient fires involve burns, generally of lower severity than the claims included in this study.28 The situational awareness framework provided a unique perspective with increased emphasis on the importance of anticipating fire risks and incorporating risk and prevention planning into the preoperative anesthesia plan and checklist.
Clinical Implications and Recommendations
Perception errors may be prevented by directing attention to additional or other more relevant sources of information. Regular scanning and processing of all the information available may avoid misdiagnosis based on heuristic reasoning.29 Implementing standards which define a minimum of vital parameters for certain procedures or the WHO surgical safety checklist30 may have positive impact. Accurate assessment and improved availability of preoperative history and test results may prevent perception errors.
Comprehension and projection involve long-term memory content which may be difficult to access during a critical incident. A “call-for-help” and use of cognitive aides (e.g., emergency checklists or manuals) may help. 31–34 Assistance from other anesthesiologists may provide additional processing capacity for the integration of basic information. Cognitive aids enhance comprehension and projection.31,34 The situational awareness framework also offers systematic approaches to reduce errors,35,36 such as the user-centric design of information and training curricula including simulation.37 Situational awareness-relevant learning objectives are addressed in anesthesia crisis resource management education and include self-checking behavior and specific communication strategies.36 Situational awareness-specific training principles focus, among other things, on strengthening mental models, trainee feedback, and common errors.35,38
Limitations
This study has numerous limitations. The study analysis relied on narratives that were not prospectively collected with the intent to assess situational awareness errors in a standardized manner. Therefore, important information to determine underlying causes was missing. The non-random, retrospective collection of data may reflect selection and hindsight bias. In contrast to incident reports, the Anesthesia Closed Claims Project malpractice narratives were created by trained experts using a larger set of information and not just reports from single individuals. Nevertheless, it is likely that the poor outcomes within the claims bias the reviewers toward a very rigorous assessment of standards of care.39 We did not consider the database assessment of appropriateness of care when we made our independent assessment of errors. As all claims in this investigation had poor outcome (death or permanent brain damage), any outcome bias would apply to the entire study sample. Another limitation is selection bias in that only selected companies were willing to provide claims data. Furthermore, there is always uncertainty as to the veracity of the medical documentation and depositions in malpractice claims.
The Anesthesia Closed Claims Project represents a large opportunity sample, and as such, the data do not necessarily reflect the actual quantity of situational awareness errors in U.S. anesthesia malpractice claims. Despite these limitations, using the situational awareness framework for the analysis of anesthesia closed malpractice claims provided information about the potential role of situational awareness in the genesis of patient harm in events that would be difficult to analyze prospectively. Other analytical frameworks such as educational needs assessment or different human factors models might reveal different safety problems and point to different solutions, but that does not negate the lessons learned through application of a situational awareness framework in this study. While we didn’t address changes in errors over time, it nonetheless reveals the potential for situational awareness methods to contribute toward reducing catastrophic injury.
Conclusions
Lack of situational awareness may have contributed to a large proportion of recent catastrophic anesthesia malpractice claims, providing further support for the premise that situational awareness is a core element for anesthesia decision-making and patient safety. Operationalized definitions of situational awareness errors were developed and reliably applied to the analysis of real-world anesthesia cases with severe injury. We hope that this novel adaptation of methods from aviation to clinical medicine will stimulate further research and development of strategies to prevent patient harm.
Summary statement:
Anesthesiologist situational awareness errors may have contributed to injury in 74% of malpractice claims for death or brain damage. These findings suggest that a lack of situational awareness may play an important role in the genesis of patient harm.
Acknowledgments:
The authors acknowledge the closed claims reviewers from the ASA and participation of the following liability insurance companies who have given permission to be acknowledged: Anesthesia Service Medical Group, Inc., San Diego, CA; COPIC Insurance Company, Denver, CO; ISMIE Mutual Insurance Company, Chicago, IL; MAG Mutual Insurance Company, Atlanta, GA; Medical Liability Mutual Insurance Company, New York, NY; Midwest Medical Insurance Company, Minneapolis, MN; NORCAL Mutual Insurance Company, San Francisco, CA; Physicians Insurance A Mutual Company, Seattle, WA; Preferred Physicians Medical Risk Retention Group, Overland Park, KS; Risk Management Foundation, Cambridge, MA; State Volunteer Mutual Insurance Company, Brentwood, TN; The Doctors’ Company, Napa, CA; The University of Texas System, Austin, TX.
Disclosure of funding: Supported in part by the American Society of Anesthesiologists (ASA) and the Anesthesia Quality Institute (AQI), Schaumburg, IL. All opinions expressed are those of the authors and do not reflect the policy of the ASA or AQI. REDCap (Research Electronic Data Capture) electronic data capture tools hosted at University of Washington was provided by the Institute of Translational Health Science (ITHS) through UL1 RR025014 from NCRR/NIH. Additional support was provided by institutional funding.
Footnotes
Conflict of interest: None of the authors has a conflict of interest.
Preliminary findings were presented at the American Society of Anesthesiologists annual meeting in New Orleans, LA October 14, 2014. (Burden AR, et al: Situational Awareness Errors in Anesthesia Malpractice Claims. Abstract A4137) and at the American Society of Anesthesiologists annual meeting in Chicago, IL October 24, 2016 (Burden AR, et al: Situational Awareness Errors in Anesthesia Malpractice Claims: Errors of Perception, Comprehension and Projection Leading to Catastrophic Outcomes. Abstract A3207.)
References
- 1. Schulz CM, Endsley MR, Kochs EF, Gelb AW, Wagner KJ: Situation awareness in anesthesia: Concept and research. Anesthesiology 2013; 118:729–42 [DOI] [PubMed] [Google Scholar]
- 2. Fletcher GCL, McGeorge P, Flin RH, Glavin RJ, Maran NJ: The role of non-technical skills in anaesthesia: A review of current literature. Br J Anaesth 2002; 88:418–29 [DOI] [PubMed] [Google Scholar]
- 3. Endsley MR: A taxonomy of Situation Awareness Errors, Human Factors in Aviation Operations. Edited by Fuller R, Johnston N, McDonald N. Aldershot (England), Ashgate Publishing, 1995, pp 287–92 [Google Scholar]
- 4. Fioratou E, Flin R, Glavin R, Patey R: Beyond monitoring: Distributed situation awareness in anaesthesia. Br J Anaesth 2010; 105:83–90 [DOI] [PubMed] [Google Scholar]
- 5. Catchpole K, Mishra A, Handa A, McCulloch P: Teamwork and error in the operating room: Analysis of skills and roles. Ann Surg 2008; 247:699–706 [DOI] [PubMed] [Google Scholar]
- 6. World Health Organization: Human Factors in Patient Safety Review of Topics and Tools. (2009). Retrieved May 25, 2016, from http://www.who.int/patientsafety/research/methods_measures/human_factors/human_factors_review.pdf
- 7. Way LW, Stewart L, Gantert W, Liu K, Lee CM, Whang K, Hunter JG: Causes and prevention of laparoscopic bile duct injuries: Analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg 2003; 237:460–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mishra A, Catchpole K, Dale T, McCulloch P: The influence of non-technical performance on technical outcome in laparoscopic cholecystectomy. Surg Endosc 2008; 22:68–73 [DOI] [PubMed] [Google Scholar]
- 9. Rutherford JS, Flin R, Irwin A: The non-technical skills used by anaesthetic technicians in critical incidents reported to the Australian Incident Monitoring System between 2002 and 2008. Anaesth Intensive Care 2015; 43:512–7 [DOI] [PubMed] [Google Scholar]
- 10. Schulz CM, Krautheim V, Hackemann A, Kreuzer M, Kochs EF, Wagner KJ: Situation awareness errors in anesthesia and critical care in 200 cases of a critical incident reporting system. BMC Anesthesiol 2016; 16:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Singh H, Giardina TD, Petersen LA, Smith MW, Paul LW, Dismukes K, Bhagwath G, Thomas EJ: Exploring situational awareness in diagnostic errors in primary care. BMJ Quality & Safety 2012; 21:30–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sitterding MC, Ebright P, Broome M, Patterson ES, Wuchner S: Situation awareness and interruption handling during medication administration. West J Nurs Res 2014; 36:891–916 [DOI] [PubMed] [Google Scholar]
- 13. Korkiakangas T, Weldon SM, Bezemer J, Kneebone R: Nurse-surgeon object transfer: Video analysis of communication and situation awareness in the operating theatre. Int J Nurs Stud 2014; 51:1195–206 [DOI] [PubMed] [Google Scholar]
- 14. Endsley MR: Situation Awareness and Human Error: Designing to Support Human Performance. Proceedings of the High Consequence Systems Surety Conference, Albuquerque 1999 [Google Scholar]
- 15. Cheney FW: The American Society of Anesthesiologists Closed Claims Project: What have we learned, how has it affected practice, and how will it affect practice in the future? Anesthesiology 1999; 91:552–6 [DOI] [PubMed] [Google Scholar]
- 16. Cheney FW, Posner K, Caplan RA, Ward RJ: Standard of care and anesthesia liability. JAMA 1989; 261:1599–603 [PubMed] [Google Scholar]
- 17. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG: Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Endsley MR: Toward a theory of situation awareness in dynamic systems. Human Factors 1995; 37:32–64 [Google Scholar]
- 19. Endsley MR: Situation awareness misconceptions and misunderstandings. J Cogn Eng Decis Mak 2015; 9:4–32 [Google Scholar]
- 20. Jones DG, Endsley MR: Sources of situation awareness errors in aviation. Aviation, Space, and Environmental Medicine 1996; 67:507–12 [PubMed] [Google Scholar]
- 21. Sowka MP: The medical malpractice closed claims study. Conducted by the National Association of Insurance Commissioners. Conn Med 1981; 45:91–101 [PubMed] [Google Scholar]
- 22. Landis JR, Koch GG: The measurement of observer agreement for categorical data. Biometrics 1977; 33:159–74 [PubMed] [Google Scholar]
- 23. Bureau of Labor Statistics US Department of Labor: Consumer Price Index inflation calculator , Bureau of Labor Statistics, US Department of Labor, Available at http://www.bls.gov/data/home.htm; Accessed March 3, 2016
- 24. Cheney FW, Posner KL, Lee LA, Caplan RA, Domino KB: Trends in anesthesia-related death and brain damage: A closed claims analysis. Anesthesiology 2006; 105:1081–6 [DOI] [PubMed] [Google Scholar]
- 25. Bhananker SM, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB: Injury and liability associated with monitored anesthesia care. Anesthesiology 2006; 104:228–34 [DOI] [PubMed] [Google Scholar]
- 26. Dutton RP, Lee LA, Stephens LS, Posner KL, Davies JM, Domino KB: Massive hemorrhage: A report from the Anesthesia Closed Claims Project. Anesthesiology 2014; 121:450–8 [DOI] [PubMed] [Google Scholar]
- 27. Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW: Management of the difficult airway: A closed claims analysis. Anesthesiology 2005; 103:33–9 [DOI] [PubMed] [Google Scholar]
- 28. Mehta SP, Bhananker SM, Posner KL, Domino KB: Operating room fires: A closed claims analysis. Anesthesiology 2013; 118:1133–9 [DOI] [PubMed] [Google Scholar]
- 29. Stiegler MP, Gaba DM: Decision-making and cognitive strategies. Simul Healthc 2015; 10:133–8 [DOI] [PubMed] [Google Scholar]
- 30. Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, Herbosa T, Joseph S, Kinbatala PL, Lapitan MC, Merry AF, Moorthy K, Reznick RK, Taylor B, Gawande AA: A surgical checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009; 360:491–9 [DOI] [PubMed] [Google Scholar]
- 31. Borshoff DC: The Anaesthetic Crisis Manual, 1st rev ed. edition. Perth (Australia), Leeuwin Press, 2013 [Google Scholar]
- 32. European Society of Anaesthesiology. Emergency Quick Reference Guide. Retrieved May 27, 2016 from http://html.esahq.org/patientsafetykit/resources/checklists.html
- 33. Howard SK, Chu LF, Goldhaber-Fiebert SN, Gaba DM, Harrison TK (Stanford Anesthesia Cognitive Aid Group). Emergency Manual: Cognitive aids for perioperative critical events. Creative Commons BY-NC-ND. 2014. (Version 2) (http://creativecommons.org/licenses/by-nc-nd/3.0/legalcode). Retrieved May 25, 2016 from http://emergencymanual.stanford.edu/ [Google Scholar]
- 34. Operating Room Crisis Checklists. Ariadne Labs: A Joint Center for Health Systems Innovation, 2013. Retrieved May 27, 2016 from http://www.projectcheck.org/crisis-checklist-templates.html
- 35. Endsley MR, Jones DG: Designing for Situation Awareness: An Approach to User-Centered Design, 2nd Edition. Boca Raton, CRC Press, 2011, pp147–68, 235–56 [Google Scholar]
- 36. Onal E, Craddock C, Chapman A, Endsley MR: From theory to practice: Designing for situation awareness to transform shovel operator interfaces, reduce costs, and increase safety. CIM Journal 2013; 4:1517–25 [Google Scholar]
- 37. Gaba DM, Fish KJ, Howard SK, Burden AR: Teaching anesthesia crisis resource management, Crisis Management in Anesthesiology, 2nd Edition. Edited by Gaba DM, Fish KJ, Howard SK, Burden AR. Philadelphia, Elsevier, 2015, 54–57, 61–63 [Google Scholar]
- 38. Gaba DM, Fish KJ, Howard SK, Burden AR: Principles of crisis resource management, Crisis Management in Anesthesiology, 2nd Edition. Edited by Gaba DM, Fish KJ, Howard SK, Burden AR. Philadelphia, Elsevier, 2015, pp 36–47 [Google Scholar]
- 39. Caplan RA, Posner KL, Cheney FW: Effect of outcome on physician judgments of appropriateness of care. JAMA 1991; 265:1957–60 [PubMed] [Google Scholar]