Abstract
This study (1) determined if clinical elevations of sluggish cognitive tempo (SCT) and attention-deficit/hyperactivity disorder (ADHD) symptom distributions in a large community sample of children would allow for identifying separate SCT only, ADHD only, and SCT+ADHD clinical groups, (2) examined co-occurrence of clinically elevated SCT and ADHD, (3) evaluated whether these clinical groups differed in their gender distribution, co-occurring mental health symptoms, and impairment in academic and social functioning, and (4) explored patterns of independence and overlap when clinically elevated depressive symptoms were considered in tandem with SCT and ADHD. Participants were mothers, fathers, and teachers of 2,142 children (50.51% boys; ages 8–13 years) from 32 schools in Spain. All three informants completed measures of SCT, ADHD, oppositional defiant disorder (ODD), anxiety, depression, shyness, social impairment, and academic impairment. Cut-scores for the top 5% of the sample were used to create SCT only, ADHD only, SCT+ADHD, and comparison groups. Across informants, 4.97–5.53% met criteria for clinically elevated ADHD only, and 2.30–2.80% met criteria for clinically elevated SCT only. 27–35% of the ADHD group also met the criteria for the SCT group whereas 44–54% of the SCT group met the criteria for the ADHD group (primarily based on inattentive symptoms). The ADHD only group had higher ODD scores than the SCT only group, whereas the SCT only group generally had higher shyness and internalizing scores (particularly depression) than the ADHD only group. Additional analyses that also included clinically elevated depression found that 28–46% of the children with elevated SCT had elevations in neither ADHD nor depression. This study moves the field toward examining both the empirical and clinical differentiation of SCT and ADHD. Findings are discussed regarding how SCT may fit in diagnostic nosologies and models of psychopathology.
Keywords: ADHD, comorbidity, depression, diagnosis, prevalence, sluggish cognitive tempo, functional impairment
General Scientific Summary:
There is ongoing interest in whether sluggish cognitive tempo (SCT), characterized by excessive daydreaming, mental fogginess or confusion, slowed behavior/thinking, losing one’s train of thought, and drowsiness/sleepiness, can or should be differentiated from attention-deficit/hyperactivity disorder (ADHD). The present study indicates that children with elevated SCT have both co-occurrence with and independence from children with ADHD or depression, coupled with distinct patterns of functioning.
There is both longstanding and recent interest in whether sluggish cognitive tempo (SCT), characterized by excessive daydreaming, mental fogginess or confusion, slowed behavior/thinking, losing one’s train of thought, and drowsiness/sleepiness, can or should be differentiated from attention-deficit/hyperactivity disorder (ADHD) (Becker, Marshall, & McBurnett, 2014). A recent meta-analysis of factor analytic studies provides strong support for the empirical differentiation of SCT and ADHD (Becker, Leopold, et al., 2016). What is far less established is whether there is clinical differentiation of SCT and ADHD. That is, even though these symptom dimensions are separable in factor analytic studies, far fewer studies have examined whether SCT and ADHD also part ways in terms of demographic patterns and functional outcomes, particularly when individuals are considered based on clinical levels of symptomatology (Barkley, 2014; Becker, Leopold, et al., 2016; Mueller et al., 2014).
Most studies examining the clinical differentiation of SCT and ADHD have used dimensional models to determine whether SCT and ADHD are differentially associated with functional outcomes when controlling for each other. These studies have generally found SCT to be independently associated with internalizing symptoms, social impairments (particularly withdrawal/isolation), and, though less clearly so, academic difficulties. In contrast, studies have found ADHD to be independently associated with externalizing behaviors, social impairments (particularly peer rejection), and a range of academic difficulties and impairments (for reviews, see Barkley, 2014; Becker & Barkley, 2018; Becker, Leopold, et al., 2016; Mueller et al., 2014). Although important, these studies have not examined the overlap in children with clinically-elevated SCT and/or ADHD symptoms and whether children with elevated SCT and/or ADHD have a distinct pattern of functioning. Such studies are important to advance our understanding of the patterns of co-occurrence and clinical correlates of SCT and ADHD and whether SCT may be its own psychiatric disorder (Barkley, 2014).
Barkley (2012, 2013) provided the strongest support yet for SCT being conceptualized as an attentional disorder distinct from ADHD with nationally representative studies of children and adults in the United States. These landmark studies showed for the first time that in large, community-based studies a subset of individuals with clinically elevated SCT, but without elevated ADHD, can be identified, and vice versa. Specifically, using parent ratings in the study with children, 59% of the children with elevated SCT also had elevated ADHD, whereas 39% of children with elevated ADHD also had elevated SCT (Barkley, 2013). A higher proportion of males was found in the ADHD groups (with or without SCT) compared to the SCT only or control groups. Furthermore, the ADHD groups were characterized by more severe parent ratings of daily life executive functioning (EF) deficits and home-school impairment compared to the SCT only group, though the SCT group had higher EF deficit and impairment rating scores compared to comparison children. In contrast, children in the SCT groups (with or without ADHD) had the highest rates of a parent-reported depression diagnosis. In fact, it has been questioned whether SCT is distinct from depression. Extant studies indicate that SCT and depression are empirically distinct (Becker et al., 2018; Becker, Luebbe, Fite, Stoppelbein, & Greening, 2014; Lee, Burns, Snell, & McBurnett, 2014; Willcutt et al., 2014). However, we are unaware of any study that has examined independence and overlap of children with clinically elevated SCT and/or depressive symptoms.
The current study is the first replication and extension of Barkley’s study of U.S. children (Barkley, 2013). We sought to replicate Barkley’s study be using a large, community-based sample to examine the degree of overlap in groups of children with clinically elevated SCT and/or ADHD, as well as whether a higher proportion of males would be found in the ADHD groups compared to the SCT only and comparison groups. We sought to extend Barkley’s study in four key ways. First, we collected ratings by mothers, fathers, and teachers to examine whether SCT and ADHD groups could be similarly found across all three informants. Second, our sample was comprised of children in Spain, thus extending the findings by Barkley (2013) to Spanish children in an effort to extend the transcultural validity of SCT (Lee, Burns, & Becker, 2018), particularly as it pertains to clinical differentiation. Third, we examined whether the clinical groups had differential patterns in co-occurring externalizing and internalizing symptoms, social functioning (including global impairment, shyness, and peer rejection), and academic impairment. Fourth, given the strong association between SCT and depressive symptoms (Becker, Leopold, et al., 2016), as well as parent-reported depression diagnosis (Barkley, 2013), after examining rates of overlap between SCT and ADHD we also examined patterns of overlap when children with clinically elevated depressive symptoms were also included.
Study Objectives
The primary objectives of this study were to (1) determine if clinical elevations (i.e., the top 5%) of the SCT, ADHD-IN, and ADHD-HI symptom distributions in a large community sample of children would identify separate SCT only, ADHD only, and SCT+ADHD clinical groups, (2) examine co-occurrence of clinically elevated SCT and ADHD, (3) evaluate whether these clinical groups differed in their gender distribution, co-occurring mental health symptoms, and impairment in academic and social functioning, and (4) explore patterns of independence and overlap when clinically elevated depressive symptoms were considered in tandem with SCT and ADHD. We had the following hypotheses:
Independence and overlap of SCT and ADHD groups.
We predicted that a clinical SCT group would be identified across mother, father, and teacher ratings in a large community sample. Based on Barkley’s (Barkley, 2013) United States sample, we expected that approximately 40% of the children with clinically elevated SCT would not display clinical ADHD, and that approximately 60% of children in the ADHD group would not meet criteria for the SCT group.
Gender differences for SCT and ADHD groups.
It was predicted that the SCT only group would not differ in the percentage of boys and girls whereas the ADHD only group would have significantly more boys than girls.
Differences in externalizing and internalizing symptoms.
It was first predicted that the three clinical groups would have significantly higher ODD, anxiety, and depression scores than the comparison group. However, we expected the clinical groups to part ways in their levels of externalizing (i.e., ODD) and internalizing (i.e., anxiety, depression) symptoms. We hypothesized that the ADHD only group and the SCT+ADHD groups would have significantly higher ODD scores than the SCT only group. Conversely, we hypothesized that the SCT only and the SCT+ADHD groups would have significantly higher anxiety and depression scores than the ADHD only group.
Differences in social and academic impairment.
It was first predicted that the three clinical groups would have significantly higher general academic impairment, general social impairment, peer rejection, and shyness scores than the comparison group. The second prediction was that the SCT+ADHD group would have greater general academic and social impairment than the SCT only or ADHD only groups; we did not make hypotheses regarding general academic/social impairment between the SCT and ADHD only groups given mixed findings in the literature regarding the unique contributions of these psychopathologies with these general outcomes. The third prediction was that the SCT only and SCT+ADHD groups would have significantly higher shyness scores than the ADHD only group (with no difference in shyness between the SCT only and SCT+ADHD groups). Conversely, the ADHD only group was expected to have significantly higher peer rejection scores than the SCT only and SCT+ADHD groups.
Independence and overlap of SCT and ADHD groups with a depression group.
Based on parent-report, Barkley (2013) found rates of having a depression diagnosis to be 1.2%, 2.9%, 4.7%, and 9.5% in the comparison, ADHD only, SCT only, and SCT+ADHD groups. Given our use of ratings scales with shared method variance to measure all psychopathology symptoms, we expected similar if not higher rates of co-occurrence in our sample. However, since no previous study has examined patterns of independence and co-occurrence across clinically elevated SCT, ADHD, and depressive symptoms, we did not make specific hypotheses for this objective.
Methods
Participants
The participants were mothers, fathers, and teachers of 2,142 children (50.51% boys) in third through sixth grades (ages 8–13 years; M=10.30, SD=1.21) from 32 schools on the Balearic Islands, Spain. Mothers and fathers provided ratings on 1,649 and 1,358 children, respectively (i.e., 1,777 unique children were rated by parents). A total of 196 teachers provided ratings on 1,773 children with each teacher rating an average of 10.93 (SD = 6.05) children. Approximately 85% of the children lived with both parents and approximately 13% with a single parent (approximately 2% missing). In terms of the educational level of the mothers (fathers), 17% (25%) had completed ten years of education with 19% (22%) 12 years (high school graduation), 23% (21%) technical degrees (i.e., three to five years of education after high school), and 37% (29%) university degrees (approximately 4% missing). The overall demographics of the 32 schools was approximately 90% Caucasian children and 10% North African children. Additional details regarding recruitment procedures and sample characteristics can be found elsewhere (Sáez, Servera, Becker, & Burns, 2018; Sáez, Servera, Burns, & Becker, 2018). This study was approved by the Research Ethics Committee (Institutional Review Board [IRB]) of the University of the Balearic Islands (protocol #07CER14).
Measures
Child and Adolescent Behavior Inventory (CABI).
Parents and teachers completed the CABI (Burns, Lee, Servera, McBurnett, & Becker, 2015a, 2015b). The CABI measures SCT (16 symptoms), ADHD-IN (nine symptoms), ADHD-HI (nine symptoms), ODD (eight symptoms), anxiety (six symptoms) depression (six symptoms), social impairment (four items for parents—quality of interactions with parents, other adults, siblings, and peers; two items for teachers—quality of interactions with adults and peers at school), and academic impairment (five items: quality of homework/classwork, reading skills, arithmetic skills, writing skills, and global academic skills). Parents and teachers were instructed to base their ratings on the past month. Mothers and fathers were also told to make their ratings independently. The symptoms were rated on a 6-point scale (i.e., 0=almost never [never or about once per month], 1=seldom [about once per week], 2=sometimes [several times per week], 3=often [about once per day], 4=very often [several times per day], and 5=almost always [many times per day]. A 7-point scale was used for the academic and social impairment items (i.e., 0=severe difficulty, 1=moderate difficulty, 2=slight difficulty, 3=average performance [average interactions] for grade level, 4=slightly above average, 5=moderately above average, and 6=excellent performance [excellent interactions] for grade level). The academic impairment and social impairment items were reverse keyed so that higher scores indicated greater academic and social impairment. Earlier studies provide support for the reliability (internal consistency, test-retest, inter-rater) and validity of the CABI scale scores (Becker, Burns, Schmitt, Epstein, & Tamm, 2017; Bernad, Servera, Becker, & Burns, 2016; Khadka, Burns, & Becker, 2016; Lee et al., 2018). In the current study, Cronbach’s alpha values for mothers varied from .72 (anxiety) to .95 (ADHD-IN), fathers from .75 (anxiety) to .95 (ADHD-IN and academic impairment), and teachers from .85 (anxiety) to .97 (ADHD-IN and SCT). Inter-factor correlations from a CFA ranged from .66 (anxiety) to .87 (academic impairment) for mothers and fathers, .18 (social impairment) to .72 (academic impairment) for mothers and teachers, and .14 (social impairment) to .69 (academic impairment) for fathers and teachers.
Child Social Preference Scale (CSPS).
The CSPS (Coplan, Prakash, O’Neil, & Armer, 2004) was developed as a parent-report measure of children’s conflicted shyness (e.g., experiencing social fears/withdrawal despite a desire to interact socially) and social disinterest (e.g., lacking a strong motivation to engage in social interaction). Only the conflicted shyness scale (7 items; e.g., “My child will turn down social initiations from other children because he/she is shy”) was used in the current study because the alphas for the social disinterest scale were too low to justify its use (i.e., .31, .32, and .53 for mothers, fathers, and teachers, respectively). Previous research supports the reliability and validity of the CSPS conflicted shyness scale, including associations with temperamental wariness of social novelty, teacher-rated anxiety and behavioral withdrawal, and observed reticent behavior and parallel play during free play with peers (Coplan et al., 2004). For the present study, the CSPS was adapted for completion by teachers (changing “My child…” to “This child…”) in addition to mothers and fathers. For each item, parents (teachers) responded to the question “How much is your child (this child) like that?” on a five-point scale (ranging from 1 = not at all to 5 = a lot). The internal consistency values ranged from .78 to .87 for mothers, fathers, and teachers. Inter-factor correlations from a CFA were .75 for mothers with fathers with the values being .16 and .20 for mothers with teachers and fathers with teachers, respectively.
Dishion Social Acceptance Scale (DSAS).
Two items from the DSAS (Dishion, 1990) were used to create the measure of social rejection. Specifically, teachers rated the proportion of classmates who “like” and “dislike” the child on a 5-point scale (very few [less than 25%]; some [25 to 49%]; about half [50%]; many [51% to 75%]; and almost all [greater than 75%]), and these two items were used to index peer rejection (the “like” item reversed). The Cronbach’s alpha for the two-item measure was .85.
Analytic Strategy
Version 14 of the Stata statistical software was used to perform the analyses. Given the children were clustered within classes (i.e., teachers), the intraclass correlation (ICC) was calculated for the measures. The ICC values ranged from .09 to .22 for teacher measures with the ICC values being less than .03 (most less than .01) for mother and father measures. The cluster variable was used to correct the standard errors in the analyses with teachers while this procedure was not used for the mother and father ratings since the ICC values were less than .05 (Mehmetoglu & Jakobsen, 2016, p. 203).
Results
Missing Information
For ratings by teachers (n=1,773), there was no missing information (items left blank) on any of the scales. For the ratings by mothers (n=1,649) and fathers (n=1,358), there was no missing information on SCT and ADHD items. The creation of the four groups from the SCT and ADHD items thus did not involve any missing information. For mother and father outcome measures, zero to eight children had a missing total score value (most measures only had one or two cases missing). Children with complete information on an outcome measure were used in the analyses for mothers and fathers.
Creation of Comparison, ADHD only, SCT only, and SCT+ADHD Groups
Table 1 shows the cut-scores for the top 5% of the sample for the ADHD-IN, ADHD-HI, and SCT distributions for the three sources. These cut-off scores were used to create the SCT only, ADHD only, SCT+ADHD, and comparison groups. The SCT only group had scores in the top 5% on the SCT dimension but scores less than the top 5% on ADHD-IN and ADHD-HI dimensions. The ADHD only group had scores in the top 5% of the ADHD-IN or ADHD-HI distributions but scores less than the top 5% on the SCT dimension. The SCT+ADHD group had scores in the top 5% of the SCT dimension and in the top 5% of the ADHD-IN or ADHD-HI dimension. The children who did not meet the criteria for SCT only, ADHD only, and SCT+ADHD groups were all assigned to the comparison group for each source.1
Table 1.
Cut Scores for Top Five Percent of the Sample on Attention-Deficit/Hyperactivity Disorder (ADHD) Inattention (IN), ADHD Hyperactivity/Impulsivity (HI), and Sluggish Cognitive Tempo (SCT) Symptom Dimensions
| ADHD-IN | ADHD-HI | SCT | |
|---|---|---|---|
| Mothers’ Ratings (n = 1649) | |||
| Cut score | ≥ 3.78 | ≥ 3.44 | ≥ 2.07 |
| Percent of sample | 4.91% | 4.67% | 4.98% |
| N | 81 | 77 | 82 |
| Fathers’ Ratings (n = 1358) | |||
| Cut score | ≥ 3.33 | ≥ 3.33 | ≥ 1.93 |
| Percent of sample | 4.86% | 4.86% | 5.00% |
| N | 66 | 66 | 68 |
| Teachers’ Ratings (n = 1773) | |||
| Cut score | ≥ 4.22 | ≥ 3.22 | ≥ 3.40 |
| Percent of sample | 4.57% | 4.79% | 4.62% |
| N | 81 | 85 | 82 |
Note. Ratings occurred on a 0 to 5 scale (see text for anchors). The total number of children high on the ADHD-IN or ADHD-HI dimensions (i.e., 158, 132, and 166 for mothers, fathers, and teachers, respectively) is higher than the number of children in the ADHD group (i.e., 126, 108, and 135 for mothers, fathers, and teachers, respectively, see Tables 2 and 3) because some children had elevations on both ADHD-IN and ADHD-HI dimensions (i.e., ADHD combined presentation) and were therefore counted only once when creating the ADHD clinical group.
Table 2 shows the number of children in the comparison, ADHD-only, SCT only, SCT+ADHD groups for mothers (i.e., 90.05%, 4.97%, 2.30%, and 2.67%, respectively), fathers (i.e., 89.25%, 5.74%, 2.80%, and 2.21%, respectively), and teachers (i.e., 89.85%, 5.53%, 2.54%, and 2.09%, respectively). The sample was too small to have separate ADHD inattentive, hyperactive/impulsive, and combined presentation groups so the three ADHD presentations were contained within the ADHD group. The next section does, however, note the ADHD presentation rates in the SCT and ADHD groups.
Table 2.
Percent and Number of Children in Comparison, ADHD, SCT, and SCT+ADHD Groups
| Comparison | ADHD | SCT | SCT+ADHD | |
|---|---|---|---|---|
| Mothers’ Ratings | ||||
| Percent of Sample | 90.05% | 4.97% | 2.30% | 2.67% |
| N | 1485 | 82 | 38 | 44 |
| Fathers’ Ratings | ||||
| Percent of Sample | 89.25% | 5.74% | 2.80% | 2.21% |
| N | 1212 | 78 | 38 | 30 |
| Teachers’ Ratings | ||||
| Percent of Sample | 89.85% | 5.53% | 2.54% | 2.09% |
| N | 1593 | 98 | 45 | 37 |
Note. ADHD = attention-deficit/hyperactivity disorder; SCT = sluggish cognitive tempo.
Overlap of SCT and ADHD Groups
Table 3 shows the overlap between the SCT and ADHD groups and the percentages for the ADHD inattentive, hyperactive/impulsive, and combined presentations within the ADHD and SCT groups. Across informants, 27% to 35% of the ADHD group also met the criteria for the SCT group whereas 44% to 54% of the SCT group met the criteria for the ADHD group. Within the ADHD group, the percentage of each presentation was approximately the same across mothers, fathers, and teachers (i.e., inattentive: 37% to 39%; hyperactive/impulsive: 36% to 40%; and combined: 22% to 25%). Within the SCT group, the percentages for the three presentations varied more (i.e., inattentive: 24% [fathers] to 40% [teachers]; hyperactive/impulsive: 0% [teachers] to 6% [mothers]; and combined: 5% [teachers] to 16% [fathers]).
Table 3.
Overlap and Percent of Attention-Deficit/Hyperactivity Disorder (ADHD) Presentations within the ADHD and Sluggish Cognitive Tempo (SCT) Groups
| ADHD Presentation |
||||
|---|---|---|---|---|
| Rater | Inattentive | Hyperactive- Impulsive |
Combined | |
| ADHD Group | Percent with SCT within ADHD group |
|||
| M (n=126) | 34.92% (n=44) | 38.89% (n=49) | 35.71% (n=45) | 25.40% (n=32) |
| F (n=108) | 27.78% (n=30) | 38.89% (n=42) | 38.89% (n=42) | 22.22% (n=24) |
| T (n=135) | 27.41% (n=37) | 37.04% (n=50) | 40.00% (n=54) | 22.97% (n=31) |
| SCT Group | Percent with ADHD within SCT Group |
|||
| M (n=82) | 53.65% (n=44) | 34.14% (n=28) | 6.10% (n=5) | 13.41% (n=11) |
| F (n=68) | 44.12% (n=30) | 23.52% (n=16) | 4.41% (n=3) | 16.18% (n=11) |
| T (n=82) | 45.12% (n=37) | 40.24% (n=33) | 0.00% (n=0) | 4.81% (n=4) |
Note. Overlap refers to the percent of the group that also met the criteria for the other group. M = mothers; F = fathers; T = teachers.
ADHD-IN, ADHD-HI, and SCT Scores for SCT and ADHD Groups
Table 4 shows the ADHD-IN, ADHD-HI, and SCT means for the four groups. These means reflect the procedures used to create the four groups. A Bonferroni correction was used for the subsequent tests within this section (i.e., per-comparison alpha equaled p < .008 for the six comparisons for each measure). First, the comparison group had significantly lower ADHD-IN, ADHD-HI, and SCT scores than the ADHD only, SCT only, and SCT+ADHD groups for the three sources with one exception. The exception was that the ADHD-HI scores did not differ significantly for the comparison and SCT only group for teachers. Second, the SCT+ADHD group had significantly higher ADHD-IN and ADHD-HI scores than the ADHD only and SCT only groups. Third, the SCT only and SCT+ADHD groups had significantly higher SCT scores than the ADHD only group for the three sources while the SCT only and SCT+ADHD groups did not differ on SCT scores. Fourth, the SCT only group had significantly lower ADHD-HI and ADHD-IN scores than the ADHD only group for the three sources with the one exception being a non-significant difference for ADHD-IN scores for teachers.
Table 4.
ADHD and SCT Symptom Means for Comparison, ADHD, SCT, and SCT+ADHD Groups
| 1. Comparison | 2. ADHD | 3. SCT | 4. SCT+ADHD | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure | M | SE | M | SE | M | SE | M | SE | F | contrasts | Eta2 |
| Mothers’ Ratings | |||||||||||
| ADHD-IN | 0.89a | 0.02 | 3.35b | 0.14 | 2.73c | 0.11 | 4.21d | 0.08 | 446* | 1 < 3 < 2 < 4 | .45 |
| ADHD-HI | 0.75a | 0.02 | 3.47b | 0.13 | 1.57c | 0.17 | 2.46d | 0.22 | 326* | 1 < 3 < 4 < 2 | .37 |
| SCT | 0.45a | 0.01 | 1.09b | 0.07 | 2.58c | 0.08 | 2.87c | 0.08 | 609* | 1 < 2 < 3, 4 | .53 |
| Fathers’ Ratings | |||||||||||
| ADHD-IN | 0.84a | 0.02 | 2.98b | 0.14 | 2.35c | 0.11 | 3.99d | 0.12 | 340* | 1 < 3 < 2 < 4 | .43 |
| ADHD-HI | 0.73a | 0.02 | 3.26b | 0.12 | 1.46c | 0.14 | 2.57d | 0.26 | 286* | 1 < 3 < 4 < 2 | .39 |
| SCT | 0.42a | 0.01 | 0.99b | 0.06 | 2.30c | 0.07 | 2.57c | 0.12 | 448* | 1 < 2 < 3, 4 | .50 |
| Teachers’ Ratings | |||||||||||
| ADHD-IN | 0.81a | 0.04 | 3.46b | 0.14 | 3.55b | 0.07 | 4.59c | 0.05 | 1359* | 1 < 2, 3 < 4 | .43 |
| ADHD-HI | 0.41a | 0.03 | 3.48b | 0.15 | 0.57a | 0.12 | 1.26c | 0.22 | 155* | 1, 3 < 4 < 2 | .48 |
| SCT | 0.66a | 0.03 | 1.59b | 0.11 | 3.90c | 0.07 | 4.12c | 0.09 | 806* | 1 < 2 < 3, 4 | .43 |
Note. Row means with different superscripts differ significantly at p < .05 (Bonferroni correction with per-comparison p < .008). ADHD = attention-deficit/hyperactivity disorder; IN = inattention; HI = hyperactivity/impulsivity, SCT = sluggish cognitive tempo.
p < .0001.
Gender Differences for SCT and ADHD Groups
Table 5 shows the percent of boys and girls in the groups. The percent of boys and girls did not differ significantly (Bonferroni correction with a per-comparison alpha of p < .0125) within the comparison and SCT only groups for the three sources whereas the percent of boys was significantly higher than girls for the ADHD only group for each source. For the SCT+ADHD group, the percent of boys was significantly higher than girls for teacher ratings only.
Table 5.
Gender Differences for Comparison, ADHD, SCT, and SCT+ADHD Groups
| 1. Comparison | 2. ADHD | 3. SCT | 4. SCT+ADHD | |
|---|---|---|---|---|
| Gender | Percent | Percent | Percent | Percent |
| Mothers’ Ratings | ||||
| Boys | 48.62% (n = 722)a | 75.61% (n = 62)a | 50.00% (n = 19)a | 54.55% (n = 24)a |
| Girls | 51.38% (n = 763)a | 24.39% (n = 20)b | 50.00% (n = 19)a | 45.45% (n = 20)a |
| Fathers’ Ratings | ||||
| Boys | 49.01% (n = 594)a | 67.95% (n = 53)a | 63.16% (n = 24)a | 60.00% (n = 18)a |
| Girls | 50.99% (n = 618)a | 32.05% (n = 25)b | 36.84% (n = 14)a | 40.00% (n = 12)a |
| Teachers’ Ratings | ||||
| Boys | 48.71% (n = 776)a | 80.61% (n = 79)a | 57.78% (n = 26)a | 72.97% (n = 27)a |
| Girls | 51.29% (n = 817)a | 19.39% (n = 19)b | 42.22% (n = 19)a | 27.03% (n = 10)b |
Note. Column percentages with different superscripts within each source differ significantly at p < .05 (Bonferroni correction with per-comparison p < .0125). ADHD = attention-deficit/hyperactivity disorder; SCT = sluggish cognitive tempo.
External Correlates for SCT and ADHD Groups
Table 6 shows the external correlates for the comparison, ADHD only, SCT only, and SCT+ADHD groups for mothers, fathers, and teachers. Our discussion of the external correlates of group membership is separated by externalizing (i.e., ODD), internalizing (i.e., anxiety and depression), social difficulties (i.e., shyness, social rejection, and general social impairment), and academic impairment. A Bonferroni correction was used for the subsequent tests within this section (i.e., per-comparison alpha p < .008 for the six comparisons for each measure).
Table 6.
External Correlate Differences between Comparison, ADHD, SCT, and SCT+ADHD Groups
| 1. Comparison | 2. ADHD | 3. SCT | 4. SCT+ADHD | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| External Correlates | M | SE | M | SE | M | SE | M | SE | F | constracts | Eta2 |
| Mothers’ Ratings | |||||||||||
| Oppositional defiant disorder | 0.72a | 0.02 | 2.16b | 0.14 | 1.52c | 0.18 | 2.18b | 0.20 | 140** | 1 < 3 < 2, 4 | .20 |
| Anxiety | 0.50a | 0.02 | 0.91b | 0.07 | 1.37c | 0.15 | 1.41c | 0.14 | 68** | 1 < 2 < 3, 4 | .11 |
| Depression | 0.22a | 0.01 | 0.84b | 0.12 | 1.23c | 0.17 | 1.77d | 0.18 | 204** | 1 < 2 < 3 < 4 | .27 |
| Shyness | 1.87a | 0.02 | 2.02a | 0.09 | 2.39b | 0.14 | 2.37b | 0.14 | 14** | 1, 2 < 3, 4 | .03 |
| Social impairment | 1.79a | 0.04 | 2.45b | 0.15 | 2.73b | 0.20 | 3.01b | 0.22 | 17** | 1 < 2, 3, 4 | .03 |
| Academic impairment | 2.50a | 0.05 | 3.71b | 0.17 | 3.91b | 0.18 | 4.59c | 0.14 | 46** | 1 < 2, 3 < 4 | .08 |
| Fathers’ Ratings | |||||||||||
| Oppositional defiant disorder | 0.63a | 0.02 | 2.13b | 0.14 | 1.16c | 0.13 | 2.15b | 0.23 | 58** | 1 < 3 < 2, 4 | .25 |
| Anxiety | 0.49a | 0.02 | 0.94b | 0.10 | 1.17b | 0.14 | 1.59c | 0.24 | 23** | 1 < 2, 3 < 4 | .11 |
| Depression | 0.19a | 0.01 | 0.70b | 0.10 | 0.87b | 0.11 | 1.51c | 0.23 | 35** | 1 < 2, 3 < 4 | .24 |
| Shyness | 1.87a | 0.02 | 2.00ab | 0.09 | 2.18b | 0.11 | 2.23b | 0.18 | 4* | 1 < 3, 4 | .01 |
| Social impairment | 1.80a | 0.05 | 2.51b | 0.18 | 2.37b | 0.25 | 2.63b | 0.24 | 10** | 1 < 2, 3, 4 | .02 |
| Academic impairment | 2.37a | 0.05 | 3.73b | 0.14 | 3.81b | 0.19 | 4.33b | 0.17 | 77** | 1 < 2, 3, 4 | .08 |
| Teachers’ Ratings | |||||||||||
| Oppositional defiant disorder | 0.47a | 0.03 | 2.57b | 0.16 | 0.98c | 0.17 | 1.20c | 0.20 | 70** | 1 < 3, 4 < 2 | .25 |
| Anxiety | 0.43a | 0.03 | 1.07b | 0.11 | 1.24b | 0.17 | 1.68b | 0.22 | 27** | 1 < 2, 3, 4 | .12 |
| Depression | 0.34a | 0.03 | 1.20b | 0.12 | 2.20c | 0.19 | 2.31c | 0.17 | 85** | 1 < 2 < 3, 4 | .27 |
| Shyness | 1.68a | 0.03 | 1.94a | 0.10 | 2.68b | 0.13 | 2.59b | 0.13 | 35** | 1, 2 < 3, 4 | .09 |
| Social rejection | 1.66a | 0.03 | 3.03b | 0.15 | 2.70b | 0.18 | 2.86b | 0.21 | 50** | 1 < 2, 3, 4 | .14 |
| Social impairment | 1.92a | 0.08 | 3.28b | 0.15 | 3.38b | 0.23 | 3.61b | 0.23 | 50** | 1 < 2, 3, 4 | .07 |
| Academic impairment | 2.22a | 0.06 | 3.54b | 0.14 | 4.51c | 0.08 | 5.11d | 0.14 | 251** | 1 < 2 < 3 < 4 | .13 |
Note. Row means with different superscripts differ at p < .05 (Bonferroni correction with per-comparison p < .008). ADHD = attention-deficit/hyperactivity disorder. SCT = sluggish cognitive tempo.
p < .01
p < .0001.
Externalizing behaviors.
The ADHD only, SCT only, and SCT+ADHD groups had significantly (ps < .05) higher ODD scores than the comparison group for each source. In addition, for mothers and fathers, the ADHD only and SCT+ADHD groups had significantly (ps < .05) higher ODD scores than the SCT only group with the ADHD only and SCT+ADHD groups not differing significantly on ODD scores. For teachers, the ADHD only group had significantly (ps < .05) higher ODD scores than the SCT only and SCT+ADHD groups with the SCT only and SCT+ADHD groups not differing significantly on ODD scores.
Internalizing behaviors.
The three clinical groups had significantly higher anxiety and depression scores than the comparison group for each source. For mothers, the SCT only and SCT+ADHD groups had significantly higher anxiety and depression scores than the ADHD only group. In addition, the SCT+ADHD group had significantly higher depression scores than the SCT only group with this comparison not being significant for anxiety. For fathers, the ADHD only and SCT only groups did not differ significantly on anxiety and depression scores, and the SCT+ADHD group had significantly higher anxiety and depression scores than the other two clinical groups. For teachers, the SCT only and SCT+ADHD groups, although not differing from each other, had significantly higher depression scores than the ADHD only group. The three clinical groups did not differ on anxiety scores for teacher ratings.
Social difficulties.
For social impairment and social rejection, the three clinical groups had significantly higher social impairment and social rejection scores than the comparison group. The three clinical groups, however, did not differ significantly on social impairment and social rejection. For the shyness measure, the SCT only and SCT+ADHD groups had significantly higher shyness scores that the comparison and ADHD only groups for mothers and teachers with the comparison and ADHD only groups not differing significantly on shyness for mothers, teachers, and fathers. For fathers, the three clinical groups did not differ significantly on shyness.
Academic impairment.
The three clinical groups had significantly (ps < .05) higher academic impairment scores than the comparison group for all three sources. For mothers, the SCT+ADHD group had significantly higher academic impairment scores than the other two clinical groups which did not differ significantly from each other. For fathers, the three clinical groups did not differ significantly in academic impairment. For teachers, the SCT+ADHD group had significantly higher academic impairment than the other two clinical groups and the SCT only group had significantly higher academic impairment than the ADHD only group.
Overlap of SCT and ADHD Groups with a Depression Group
The percent of children in the top 5% of the depression symptom dimension in the comparison, ADHD only, SCT only, and SCT+ADHD groups for mothers was 1.55%, 15.85%, 39.47%, and 54.54%, respectively. For fathers, the percentages were 2.31%, 19.23%, 18.42%, and 50.00%, respectively. For teachers, the percentages were 1.95%, 18.37%, 46.67%, and 37.84%, respectively. Thus, SCT group membership was not synonymous with ADHD or depression group membership.
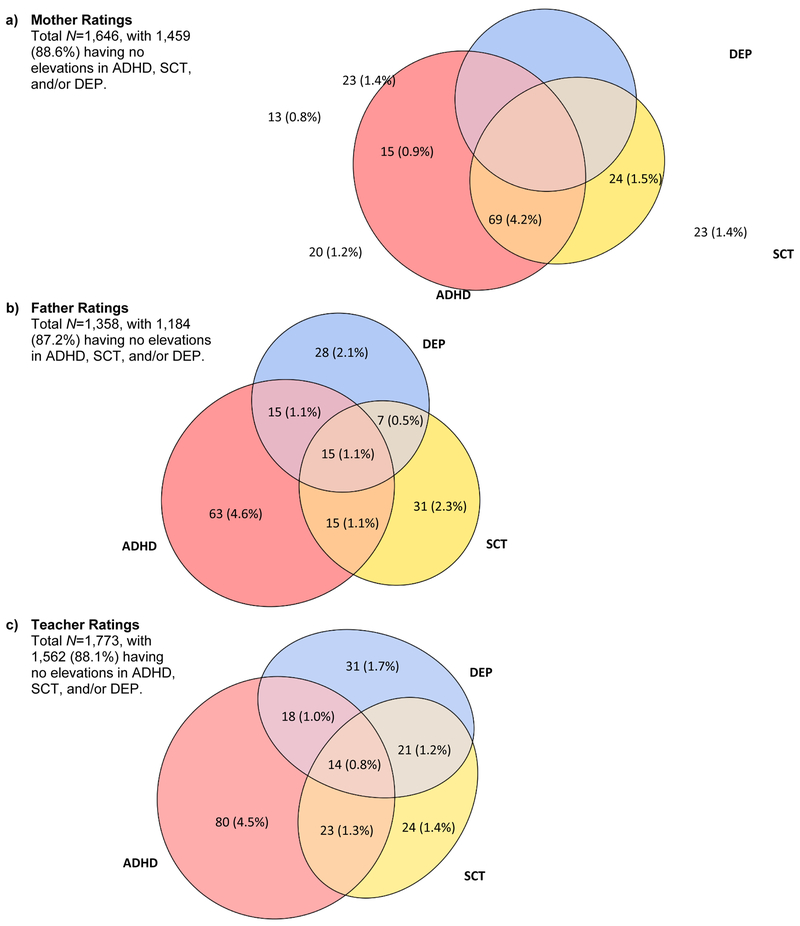
Patterns of overlap between clinically elevated SCT, ADHD, and depression are displayed in Figure 1. It is important to recall that the ADHD group was defined based on elevations in inattention and/or hyperactivity-impulsivity, resulting in a larger number of children being classified with ADHD than with SCT or depression. The percentage of children with clinically elevated SCT who had elevations in neither ADHD nor depression was 28.0%, 45.6%, and 29.3% across mother, father and teacher ratings, respectively (see Figure 1).
Figure 1.
Patterns of overlap in clinically elevated attention-deficit/hyperactivity disorder, sluggish cognitive tempo, and depressive symptoms across (a) mother, (b) father, and (c) teacher ratings.
Note. For each informant, numbers outside parentheses indicate number of children; percentages inside parentheses represent percent of the total sample. For mothers, N=1,646 instead of the 1,649 used in primary analyses since three mothers had incomplete depression data and are thus not represented in the figure. ADHD = attention-deficit/hyperactivity disorder. DEP = depression. SCT = sluggish cognitive tempo.
Discussion
This study advances the research on SCT by demonstrating the clinical differentiation of SCT and ADHD. Using a large, community-based sample and multi-informant design, findings demonstrate that (1) children with clinically elevated SCT can be identified across mother, father, and teacher ratings, (2) approximately half of children with clinically elevated SCT do not also display clinically elevated ADHD, (3) children with elevated SCT or ADHD differ in expected ways in their patterns of co-occurring externalizing and internalizing symptoms, social functioning, and academic impairment, and (4) elevated SCT shows both independence and co-occurrence with elevated depressive symptoms.
Independence and Co-occurrence of Clinically Elevated SCT, ADHD, and Depression
Over twenty studies conducted in clinical and community samples, and across the life span, have shown that SCT symptoms are empirically distinct from ADHD symptoms (Becker, Leopold, et al., 2016). Yet empirical differentiation is only a precursor to also demonstrating clinical differentiation. Barkley’s study of U.S. children (Barkley, 2013) provided the first large-scale empirical support that there exist some children who display elevated SCT symptoms but do not display elevated ADHD symptoms. Using ratings completing by either mothers or fathers, Barkley found that children with clinically elevated SCT could be identified and, crucially, that approximately 40% of children with elevated SCT did not meet criteria for elevated ADHD symptoms. Like Barkley, we defined clinically elevated SCT as the top ~5% and similarly found that approximately half of the children with elevated SCT were also classified with elevated ADHD symptoms. We also found rates of elevated SCT only to be quite similar across all three informants, ranging from 2.3% to 2.8%, thus demonstrating replicability across informants as well as for the first time identifying an SCT only group using teacher ratings. The percentage of children with elevated SCT only dropped to 1.4–2.3% when clinical elevations in depression were also considered, but this drop was expected and a sizeable proportion of the SCT group still evidenced neither ADHD nor depression. This is a key finding that has not previously been reported and supports the distinction, as well as co-occurrence, of elevated SCT symptoms with depression in addition to ADHD.
As expected (Barkley, 2013; Camprodon-Rosanas et al., 2016; Carlson & Mann, 2002), among children with elevated SCT, those who also had ADHD were most likely to meet for elevated ADHD based on predominantly inattentive rather than hyperactive-impulsive or combined symptom elevations. Nevertheless, as also found in previous studies (Barkley, 2013; Hinshaw, Carte, Sami, Treuting, & Zupan, 2002; Marshall, Evans, Eiraldi, Becker, & Power, 2014), a subset of children with elevated ratings of SCT met criteria for co-occurring ADHD combined presentation. Far fewer children with elevated SCT met criteria for predominantly hyperactive-impulsive presentation, and none when teacher ratings were used. In fact, when teacher ratings were used, children with elevated SCT only did not differ from comparison children in their hyperactivity-impulsivity scores. Some studies have reported different findings for SCT when teacher or parent ratings were examined (Burns, Becker, Servera, Bernad, & García-Banda, 2017; Watabe, Owens, Evans, & Brandt, 2014). There is also some indication that teachers may be better able to differentiate SCT from ADHD (Garner, Marceaux, Mrug, Patterson, & Hodgens, 2010; McBurnett, Pfiffner, & Frick, 2001), and our findings further suggest that how SCT presents and is observed in the home vs. school context remains an important avenue for continued examination. It is possible that teachers are better informants for identifying a “pure” SCT group with levels of hyperactivity-impulsivity comparable to children with neither SCT nor ADHD.
Group Differences in Functional Outcomes
In considering functional outcomes, the SCT, ADHD, and SCT+ADHD clinical groups clearly differed from the comparison group as expected, as well as from each other. As the SCT+ADHD group was expected to be the most severe group, perhaps the most interesting findings are between the SCT only and ADHD groups. As hypothesized, across all three informants, children with ADHD only had higher ODD symptoms than children with SCT only. In contrast, children with SCT only generally had more internalizing symptoms than children with ADHD only, though this difference was not found when father ratings were used and was only found for depression when teacher ratings were used. These findings parallel other studies that have shown SCT and ADHD to part ways in the comorbid symptoms with which they are associated, with SCT being clearly linked to internalizing symptoms and ADHD clearly linked to externalizing behaviors (Becker & Barkley, 2018; Becker, Leopold, et al., 2016).
In addition, though the clinical groups did not differ in global social impairment ratings, children with elevated SCT had higher shyness scores than children with ADHD only. This finding echoes previous studies linking SCT specifically to social withdrawal and isolation (Becker, Garner, Tamm, Antonini, & Epstein, 2017; Carlson & Mann, 2002; Marshall et al., 2014; Rondon, Hilton, Jarrett, & Ollendick, 2018). Finally, there was some informant-specificity in terms of academic impairment, whereby children with SCT only had more global academic impairment than children with ADHD only when teacher ratings were used, but not when mother or father ratings were used. As discussed above, SCT may be particularly impairing in the school setting (Burns et al., 2017), though conflicting findings have also been reported (Watabe et al., 2014). ADHD is also clearly associated with academic impairment (DuPaul & Langberg, 2015), making the interrelations of SCT, ADHD, and academics a particularly ripe area for further investigation.
SCT in Models of Psychopathology
Taken together, what do these findings mean for the place of SCT in models of psychopathology or diagnostic nosologies? We propose that three possibilities are most in line with our study findings (see also Becker & Willcutt, 2018). First, as argued by Barkley (2012, 2013, 2014; Saxbe & Barkley, 2014), SCT may be conceptualized as its own psychiatric disorder, which he has termed Concentration Deficit Disorder. In line with this possibility, we found support for an SCT only group of children with a distinct pattern of impairments. We further found that children with elevated SCT symptoms did not fully overlap with children with elevated depressive symptoms. This provides some of the strongest support to date that SCT may be a distinct disorder, with findings strikingly similar across parent and teacher informants. Still, it should be noted that we were not able to evaluate whether an SCT only group can be identified when other related disorders (e.g., sleep disturbances) are included, when other methods (e.g., clinical interviews) are used, or when group stability is examined over time. Furthermore, the design of this study precluded examining several aspects of diagnostic validity (e.g., natural history, family genetic/environmental factors) that will be important for studies to evaluate if SCT is to have sufficient evidence for classification as its own disorder (see Becker et al., 2016, for a discussion). Nevertheless, our findings underscore the importance of thoroughly evaluating the possibility that SCT may be a distinct disorder, with a particular need for studies that use longitudinal designs and multiple units of analysis. SCT appears to be quite stable throughout childhood and adolescence (Leopold et al., 2016). Still, there is also evidence that SCT increases somewhat with age (Barkley, 2012; Becker, Leopold, et al., 2016; Leopold et al., 2016), perhaps paralleling increases in depression in adolescence and early adulthood which makes the examination of clinically elevated SCT in adolescent and adult samples a key research priority. For example, it is unknown if rates of clinically elevated SCT will increase across development and, if so, whether SCT remains clinically distinct from depression and other psychopathologies that also increase in adolescence and early adulthood (e.g., social anxiety disorder, bipolar disorder, personality disorders).
A second possibility is that SCT may be a specifier, or subtype, within ADHD. This is somewhat in line with the abandoned DSM-5 proposal for an ADHD restrictive presentation characterized by high levels of inattention but low levels of hyperactivity-impulsivity, which did not have empirical support in a large meta-analysis by Willcutt and colleagues (Willcutt et al., 2012). Still, there is clear overlap between SCT and ADHD, and SCT is strongly associated with inattention particularly (Becker, Leopold, et al., 2016; McBurnett et al., 2001). Moreover, some of the impairments linked to SCT (e.g., social withdrawal, internalizing symptoms) are the same impairments linked to DSM-III-era attention deficit disorder (ADD) without hyperactivity (Milich, Balentine, & Lynam, 2001).
A third, and related, possibility is that SCT may be a specifier across psychopathologies. Although the primary focus of research to date is whether and how SCT can be differentiated from ADHD, our study provides clear evidence that SCT overlaps with ADHD as well as depression. There is emerging evidence that SCT also overlaps with other psychopathologies including autism and sleep disorders (Becker, Garner, & Byars, 2016; Langberg, Becker, Dvorsky, & Luebbe, 2014; Reinvall et al., 2017). For this reason, SCT may be a useful specifier across disorders. In line with this idea, SCT has been proposed as a transdiagnostic construct that even if not conceptualized as a distinct disorder may nonetheless be important for understanding the course, impairments, and treatment of other disorders (Becker, Leopold, et al., 2016; Becker & Willcutt, 2018). SCT has been almost entirely studied in the context of, and in relation to, ADHD, and it is time to broaden the lens and investigate the presence and impact of SCT across a wide range of mental disorders.
Furthermore, it is not currently clear how clinical elevations in SCT should best be defined. Like Barkley (2013), we classified children as having elevated SCT using a cut-point of the top 5%. We classified elevated ADHD symptoms in the same manner, and findings were highly similar when a symptom count procedure was used instead (see Footnote 1). In contrast to ADHD, there is not currently a clear, agreed-upon symptom set for SCT, and so in turn there are no established symptom counts used to define SCT elevations. As with most psychopathologies, it is likely that SCT is dimensional rather than taxonic (Becker & Willcutt, 2018), yet categorical decisions are often desired in research and required for clinical care. An important direction for future research interested in the empirical classification of SCT is to evaluate different approaches to categorization (e.g., cut-points, symptom counts) in addition to how SCT may fit within emerging dimensional classification systems (Kotov et al., 2017; Lahey, Krueger, Rathouz, Waldman, & Zald, 2017).
Study Strengths and Limitations
Strengths of this study include the use of a large, community-based sample and multiple informants, though several limitations are also important to note. First, this was a cross-sectional study, which precludes making causal inferences. Little is known of the developmental trajectory of SCT (though see Leopold et al., 2016), and it is likewise unknown if an SCT only group can be identified over time, a key issue given the strong association SCT has with both ADHD inattention and depression. Second, to recruit a large sample with multiple raters, this study was limited to rating scale measures. However, the distinctions found between co-occurrence and clinical correlates reduces concerns regarding shared method variance. Future studies would benefit from using clinical interviews for assessing psychopathology, as well as multiple methods and units of analysis for assessing a range of biological, psychosocial, and academic variables. Despite these limitations, the current study offers a major contribution to the extant literature and moves the field toward examining both the empirical and clinical differentiation of SCT and ADHD.
Acknowledgement:
This research was supported by a grant from the Ministry of Economy and Competitiveness of Spanish Government under award number PSI2014–52605-R (AEI/FEDER, UE) and a predoctoral fellowship co-financed by MINECO (Spanish Government) and the European Social Fund (BES-2015–075142). Stephen Becker is supported by award number K23MH108603 from the National Institute of Mental Health (NIMH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (NIH) or the Spanish Government. We thank Cristina Trias for assistance with the study.
Footnotes
Barkley (2013) used a symptom count procedure (i.e., 6 or more ADHD-IN [93.1 or higher percentile] and 6 or more ADHD-HI symptoms [95.2 or higher percentile] with an often or very often rating) to select children in the clinical range on these two dimensions. Given no specific number of SCT symptoms indicate the clinical range, he selected a percentile on the SCT dimension to match the severity of the ADHD-IN and ADHD-HI selection criteria (i.e., 94.3 or higher percentile). This procedure resulted in 89.1% in the comparison group, 5.3% in the ADHD only group, 2.3% in the SCT only group, and 3.4% in the SCT+ADHD group with 8.7% and 5.7% of the sample meeting the symptom count criteria for ADHD and SCT, respectively, in Barkley’s study (2013). These percentages are almost identical to our percentages. We also repeated our analyses with a similar symptom count group creation procedure. This alternative procedure yielded similar findings as reported in the paper.
References
- Barkley RA (2012). Distinguishing sluggish cognitive tempo from attention-deficit/hyperactivity disorder in adults. Journal of Abnormal Psychology, 121, 978–990. doi:10.1037/a0023961 [DOI] [PubMed] [Google Scholar]
- Barkley RA (2013). Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: Executive functioning, impairment, and comorbidity. Journal of Clinical Child and Adolescent Psychology, 42, 161–173. doi:10.1080/15374416.2012.734259 [DOI] [PubMed] [Google Scholar]
- Barkley RA (2014). Sluggish cognitive tempo (concentration deficit disorder?): Current status, future directions, and a plea to change the name. Journal of Abnormal Child Psychology, 42, 117–125. doi:10.1007/s10802-013-9824-y [DOI] [PubMed] [Google Scholar]
- Becker SP, & Barkley RA (2018). Sluggish cognitive tempo In Banaschewski T, Coghill D, & Zuddas A (Eds.), Oxford textbook of attention deficit hyperactivity disorder (pp. 147–153). Oxford: Oxford University Press. [Google Scholar]
- Becker SP, Burns GL, Garner AA, Jarrett MA, Luebbe AM, Epstein JN, & Willcutt EG (2018). Sluggish cognitive tempo in adults: Psychometric validation of the Adult Concentration Inventory. Psychological Assessment, 30, 296–310. doi:10.1037/pas0000476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Burns GL, Schmitt AP, Epstein JN, & Tamm L (2017). Toward establishing a standard symptom set for assessing sluggish cognitive tempo in children: Evidence from teacher ratings in a community sample. Assessment. Advance online publication. doi:10.1177/1073191117715732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Garner AA, & Byars KC (2016). Sluggish cognitive tempo in children referred to a pediatric Sleep Disorders Center: Examining possible overlap with sleep problems and associations with impairment. Journal of Psychiatric Research, 77, 116–124. doi:10.1016/j.jpsychires.2016.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Garner AA, Tamm L, Antonini TN, & Epstein JN (2017). Honing in on the social difficulties associated with sluggish cognitive tempo in children: Withdrawal, peer ignoring, and low engagement. Journal of Clinical Child and Adolescent Psychology. Advance online publication. doi:10.1080/15374416.2017.1286595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Leopold DR, Burns GL, Jarrett MA, Langberg JM, Marshall SA, . . . Willcutt EG (2016). The internal, external, and diagnostic validity of sluggish cognitive tempo: A meta-analysis and critical review. Journal of the American ACademy of Child and Adolescent Psychiatry, 55, 163–178. doi:10.1016/j.jaac.2015.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Luebbe AM, Fite PJ, Stoppelbein L, & Greening L (2014). Sluggish cognitive tempo in psychiatrically hospitalized children: Factor structure and relations to internalizing symptoms, social problems, and observed behavioral dysregulation. Journal of Abnormal Child Psychology, 42, 49–62. doi:10.1007/s10802-013-9719-y [DOI] [PubMed] [Google Scholar]
- Becker SP, Marshall SA, & McBurnett K (2014). Sluggish cognitive tempo in abnormal child psychology: an historical overview and introduction to the special section. Journal of Abnormal Child Psychology, 42, 1–6. doi:10.1007/s10802-013-9825-x [DOI] [PubMed] [Google Scholar]
- Becker SP, & Willcutt EG (2018). Advancing the study of sluggish cognitive tempo via DSM, RDoC, and hierarchical models of psychopathology. European Child and Adolescent Psychiatry. Advance online publication. doi:10.1007/s00787-018-1136-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernad MD, Servera M, Becker SP, & Burns GL (2016). Sluggish cognitive tempo and ADHD inattention as predictors of externalizing, internalizing, and impairment domains: A 2-year longitudinal study. Journal of Abnormal Child Psychology, 44, 771–785. doi:10.1007/s10802-015-0066-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns GL, Becker SP, Servera M, Bernad MD, & García-Banda G (2017). Sluggish cognitive tempo and attention-deficit/hyperactivity disorder (ADHD) inattention in the home and school contexts: Parent and teacher invariance and cross-setting validity. Psychological Assessment, 29, 209–220. doi:10.1037/pas0000325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns GL, Lee S, Servera M, McBurnett K, & Becker SP (2015a). Child and Adolescent Behavior Inventory - Parent Version 1.0. Pullman, WA: Author. [Google Scholar]
- Burns GL, Lee S, Servera M, McBurnett K, & Becker SP (2015b). Child and Adolescent Behavior Inventory - Teacher Version 1.0. Pullman, WA: Author. [Google Scholar]
- Camprodon-Rosanas E, Batlle S, Estrada-Prat X, Aceña-Díaz M, Petrizan-Aleman A,… Ribas-Fitó N (2016). Sluggish cognitive tempo in a child and adolescent outpatient clinical setting. Journal of Psychiatric Practice, 22, 355–362. doi: 10.1097/PRA.0000000000000177 [DOI] [PubMed] [Google Scholar]
- Carlson CL, & Mann M (2002). Sluggish cognitive tempo predicts a different pattern of impairment in the attention deficit hyperactivity disorder, predominantly inattentive type. Journal of Clinical Child and Adolescent Psychology, 31, 123–129. doi:10.1207/S15374424JCCP3101_14 [DOI] [PubMed] [Google Scholar]
- Coplan RJ, Prakash K, O’Neil K, & Armer M (2004). Do you “want” to play? Distinguishing between conflicted shyness and social disinterest in early childhood. Developmental Psychology, 40, 244–258. doi:10.1037/0012-1649.40.2.244 [DOI] [PubMed] [Google Scholar]
- Dishion TJ (1990). The peer context of troublesome child and adolescent behavior In Leone PE (Ed.), Understanding troubled and troubling youth: Multiple perspectives (pp. 128–153). Thousand Oaks, CA: Sage. [Google Scholar]
- DuPaul GJ, & Langberg JM (2015). Educational impairments in children with ADHD In Barkley RA (Ed.), Attention-deficit/hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). New York: Guilford. [Google Scholar]
- Garner AA, Marceaux JC, Mrug S, Patterson C, & Hodgens B (2010). Dimensions and correlates of attention deficit/hyperactivity disorder and sluggish cognitive tempo. Journal of Abnormal Child Psychology, 38, 1097–1107. doi:10.1007/s10802-010-9436-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Carte ET, Sami N, Treuting JJ, & Zupan BA (2002). Preadolescent girls with attention-deficit/hyperactivity disorder: II. Neuropsychological performance in relation to subtypes and individual classification. Journal of Consulting and Clinical Psychology, 70, 1099–1111. [DOI] [PubMed] [Google Scholar]
- Khadka G, Burns GL, & Becker SP (2016). Internal and external validity of sluggish cognitive tempo and ADHD inattention dimensions with teacher ratings of Nepali children. Journal of Psychopathology and Behavioral Assessment, 38, 433–442. doi:10.1007/s10862-015-9534-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, . . . Zimmerman M (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454–477. doi:10.1037/abn0000258 [DOI] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 143, 142–186. doi:10.1037/bul0000069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langberg JM, Becker SP, Dvorsky MR, & Luebbe AM (2014). Are sluggish cognitive tempo and daytime sleepiness distinct constructs? Psychological Assessment, 26, 586–597. doi:10.1037/a0036276 [DOI] [PubMed] [Google Scholar]
- Lee S, Burns GL, & Becker SP (2018). Toward establishing the transcultural validity of sluggish cognitive tempo: Evidence from a sample of South Korean children. Journal of Clinical Child and Adolescent Psychology, 47, 61–68. doi:10.1080/15374416.2016.1144192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Burns GL, Snell J, & McBurnett K (2014). Validity of the sluggish cognitive tempo symptom dimension in children: Sluggish cognitive tempo and ADHD-inattention as distinct symptom dimensions. Journal of Abnormal Child Psychology, 42, 7–19. doi:10.1007/s10802-013-9714-3 [DOI] [PubMed] [Google Scholar]
- Leopold DR, Christopher ME, Burns GL, Becker SP, Olson RK, & Willcutt EG (2016). Attention-deficit/hyperactivity disorder and sluggish cognitive tempo throughout childhood: Temporal invariance and stability from preschool through ninth grade. Journal of Child Psychology and Psychiatry, 57, 1066–1074. doi:10.1111/jcpp.12505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall SA, Evans SW, Eiraldi RB, Becker SP, & Power TJ (2014). Social and academic impairment in youth with ADHD, predominately inattentive type and sluggish cognitive tempo. Journal of Abnormal Child Psychology, 42, 77–90. doi:10.1007/s10802-013-9758-4 [DOI] [PubMed] [Google Scholar]
- McBurnett K, Pfiffner LJ, & Frick PJ (2001). Symptom properties as a function of ADHD type: an argument for continued study of sluggish cognitive tempo. Journal of Abnormal Child Psychology, 29, 207–213. [DOI] [PubMed] [Google Scholar]
- Mehmetoglu M, & Jakobsen TG (2016). Applied statistics using Stata: A guide for the social sciences. Thousand Oaks, CA: SAGE. [Google Scholar]
- Milich R, Balentine AC, & Lynam DR (2001). ADHD combined type and ADHD predominantly inattentive type are distinct and unrelated disorders. Clinical Psychology-Science and Practice, 8, 463–488. doi:DOI 10.1093/clipsy/8.4.463 [Google Scholar]
- Mueller AK, Tucha L, Koerts J, Groen Y, Lange KW, & Tucha O (2014). Sluggish cognitive tempo and its neurocognitive, social and emotive correlates: A systematic review of the current literature. Journal of Molecular Psychiatry, 2, 5. doi:10.1186/2049-9256-2-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinvall O, Kujala T, Voutilainen A, Moisio AL, Lahti-Nuuttila P, & Laasonen M (2017). Sluggish cognitive tempo in children and adolescents with higher functioning autism spectrum disorders: Social impairments and internalizing symptoms. Scandanavian Journal of Psychology, 58, 389–399. doi:10.1111/sjop.12379 [DOI] [PubMed] [Google Scholar]
- Rondon AT, Hilton DC, Jarrett MA, & Ollendick TH (2018). Sleep, internalizing problems, and social withdrawal: Unique associations in clinic-referred youth with elevated sluggish cognitive tempo symptoms. Journal of Attention Disorders. Advance online publication. doi: 10.1177/1087054718756197 [DOI] [PubMed] [Google Scholar]
- Sáez B, Servera M, Becker SP, & Burns GL (2018). Optimal items for assessing sluggish cognitive tempo in children across mother, father, and teacher ratings. Journal of Clinical Child and Adolescent Psychology. Advance online publication. doi:10.1080/15374416.2017.1416619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sáez B, Servera M, Burns GL, & Becker SP (2018). Advancing the multi-informant assessment of sluggish cognitive tempo: Child self-report in relation to parent and teacher ratings of SCT and impairment. Journal of Abnormal Child Psychology. Advance online publication. doi:10.1007/s10802-018-0436-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxbe C, & Barkley RA (2014). The second attention disorder? Sluggish cognitive tempo vs. attention-deficit/hyperactivity disorder: Update for clinicians. Journal of Psychiatric Practice, 20, 38–49. doi: 10.1097/01.pra.0000442718.82527.cd [DOI] [PubMed] [Google Scholar]
- Watabe Y, Owens JS, Evans SW, & Brandt NE (2014). The relationship between sluggish cognitive tempo and impairment in children with and without ADHD. Journal of Abnormal Child Psychology, 42, 105–115. doi:10.1007/s10802-013-9767-3 [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Chhabildas N, Kinnear M, DeFries JC, Olson RK, Leopold DR, . . . Pennington BF (2014). The internal and external validity of sluggish cognitive tempo and its relation with DSM-IV ADHD. Journal of Abnormal Child Psychology, 42, 21–35. doi:10.1007/s10802-013-9800-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tannock R, . . . Lahey BB (2012). Validity of DSM-IV attention deficit/hyperactivity disorder symptom dimensions and subtypes. Journal of Abnormal Psychology, 121, 991–1010. doi:10.1037/a0027347 [DOI] [PMC free article] [PubMed] [Google Scholar]