Abstract
Posttraumatic stress disorder is associated with elevated risk of both alcohol use disorder (AUD) and related conduct problems, which are associated with behavioral and emotional dysregulation. We conducted an intensive longitudinal burst design study with 10 weeks of experience sampling over the course of 1.5 years with 250 veterans of recent conflicts. We tested time-series models of daily associations between posttraumatic stress symptoms (PTSS), alcohol dependence syndrome, and conduct problems. Exacerbations of PTSS predicted higher dependence syndrome and conduct problems the next day. This effect was significant after controlling for both concurrent (i.e., same-day) associations between drinking and the outcomes as well as the strength of associations between the outcomes from one day to the next (i.e., autoregression). Affect lability and disinhibition were hypothesized vulnerability factors increasing the strength of within-person predictors of dependence syndrome and conduct problems. Lability and disinhibition were associated with greater dependence syndrome symptoms and conduct problems over the follow-up period. Consistent with expectation, lability rather than disinhibition increased the association between drinking and dependence syndrome as well as the strength of association between dependence syndrome symptoms from one day to the next. Moderating effects of disinhibition in the conduct problems model were not significant. Importantly, results indicated reciprocal associations over time. Lability potentiated the association between dependence syndrome symptoms and next day PTSS, whereas disinhibition potentiated the association between conduct problems and next day PTSS. Results demonstrate complex dynamic associations between PTSS, AUD symptoms, and conduct problems over time indicative of broad regulatory impairments.
Keywords: PTSD, EMA, Alcohol use disorder, affect dysregulation, impulsivity
General Scientific Summary:
This study suggests that day-to-day changes in PTSD symptoms confer increased risk for symptoms of alcohol use disorder (AUD) and problems such as interpersonal conflict due to associated deficits in the ability to regulate behavior and emotion. In addition, AUD symptoms predict transient increases in PTSD symptoms the next day, creating a complex self-perpetuating system. Alcohol use disorder, in part, may be manifest in the strength of temporal associations of disorder symptoms from day-to-day.
Summary
Many veterans struggle with PTSS, alcohol use disorder, and a range of conduct problems that reduce their quality of life after service. However, these problems are not static, but rather dynamic processes within the individual. The present results illustrate that these outcomes exhibit complex temporal interdependencies. Veterans have good days and bad days, and, as supported by the results of this study, have periods of remission interspersed with periods of distress, dyscontrolled alcohol use, and problems with social relationships. Common to each of these outcomes are disruptions in basic regulatory processes. Disinhibition increased reciprocal associations between PTSS and conduct problems. Affective lability was indicative of a vulnerable emotional regulatory system manifesting in deficits in regulating alcohol consumption and strengthening of reciprocal associations between PTSS and alcohol dependence syndrome. Addressing disruptions in any of these basic regulatory processes has the potential to produce meaningful clinical changes in PTSD, alcohol use, and associated problems and improve veterans’ quality of life as a result.
Posttraumatic stress disorder (PTSD), alcohol use disorder (AUD), and conduct problems frequently co-occur (Grant, Goldstein, Saha, & et al., 2015; Smith, Goldstein, & Grant, 2016; Stappenbeck, Hellmuth, Simpson, & Jakupcak, 2014). Dimensional models of pathology explain the co-occurrence of AUD and conduct problems as manifestations of disinhibition externalizing spectra (Kotov et al., 2017; Kramer, Polusny, Arbisi, & F Krueger, 2014). PTSD, in contrast, is considered an internalizing disorder related to emotional distress (Kotov et al., 2017). The Hierarchical Taxonomy Of Psychopathology (HiTOP) model and related dimensional models of psychopathology suggest that co-occurrence of internalizing and externalizing symptomatology is a function of a higher order “super spectra” (Kotov et al., 2017; Kramer et al., 2014). Though these models provide insights into underlying vulnerability factors at the between-person level, symptoms of PTSD, alcohol dependence, and conduct problems vary greatly within-person across time. Indeed, 75% or more of the variance in health-risk behaviors and symptoms may exist within-, rather than between-person (Cooper, 2010; Simons, Wills, Emery, & Spelman, 2016). Individuals report alternation between periods of wellbeing and periods of symptom exacerbation. Furthermore, evidence suggests that co-occurrence of these problems is not only due to shared liability, but rather due to causal associations between symptoms, across domains. That is, exacerbation of posttraumatic stress symptoms (PTSS) increases alcohol use and associated problems (Anker et al., 2017; Armour, Fried, Deserno, Tsai, & Pietrzak, 2017; Gaher et al., 2014; Possemato et al., 2015; Wilson et al., 2017). Furthermore, there is evidence that associations between PTSD and AUD symptoms may be reciprocal (Read, Wardell, & Colder, 2013). This suggests that the presentation of symptoms is a dynamic process within the individual. There is a gap in the literature in that research has yet to model these dynamic associations across time to advance understanding of these complex processes in veterans. Hence, the purpose of this study was to model temporal associations between PTSS, drinking, alcohol dependence syndrome, and conduct problems and to test the effects of two vulnerability factors, affect lability and disinhibition, on the temporal associations.
PTSD and Alcohol Use: Functional Associations
Several lines of research suggest that PTSD and alcohol use disorders are functionally associated. PTSD frequently precedes rather than follows the development of alcohol and other substance use disorders (Reed, Anthony, & Breslau, 2007; Swendsen et al., 2010). Laboratory research has demonstrated increases in alcohol craving in response to trauma cues in individuals with comorbid PTSD and alcohol dependence (Coffey et al., 2002; Coffey et al., 2010). Finally, experience sampling and other daily process designs indicate significant within-person associations between PTSS and alcohol use (Cohn, Hagman, Moore, Mitchell, & Ehlke, 2014; Gaher et al., 2014; Kaysen et al., 2014; Possemato et al., 2015; Simpson, Stappenbeck, Luterek, Lehavot, & Kaysen, 2014).
Covariation of PTSS and alcohol use within the person is consistent with several potential temporal associations. For example, PTSS could be a leading indicator of change in alcohol; alcohol a leading indicator of change in PTSS, or the two constructs could exhibit a reciprocal association over time. Alternatively, changes in PTSS symptoms and alcohol use could both stem from time-varying changes in regulatory processes (Jones, Christiansen, Nederkoorn, Houben, & Field, 2013). Relatively few daily process studies have tested lagged effects and the results have been somewhat mixed. For example, Gaher and colleagues (2014) found a significant positive effect of PTSD during the day and subsequent nighttime alcohol consumption in a veteran sample. Similarly, Simpson and colleagues (2014) found significant effects of PTSD symptoms on next day drinking in a community sample. Possemato and colleagues (2015) reported significant positive concurrent associations and 1-day lagged associations, but inverse associations over shorter (3 hour) lags. Studies have also tested a “mutual maintenance” hypothesis, whereby PTSD and alcohol consumption exhibit reciprocal associations (Kaysen et al., 2011). Overall, results have been equivocal. Simpson and colleagues (2014) did not find an effect of drinking on next day PTSS. In addition, Possemato et al. (2015) reported an inverse (rather than positive) lagged effect of drinking across their 3-hour lag. However, both of these studies have limitations with respect to relatively small samples (n = 92 to 143) and brief monitoring periods (7 to 28 days). Other longitudinal designs using repeated retrospective assessments have found reciprocal associations (Nickerson et al., 2014; Read et al., 2013) and PTSD symptoms have been shown to decline with substance use abstinence following treatment (Coffey, Schumacher, Brady, & Cotton, 2007).
To date, the majority of daily process studies are framed around a self-medication model and do not examine associations between PTSD symptoms and alcohol-related problems. Alcohol use (e.g., number of drinks consumed) and alcohol-related problems (e.g., drinking more than intended, social or interpersonal problems that may be exacerbated by alcohol) may have distinct predictors (Glantz, Weinberg, Miner, & Colliver, 1999; Simons et al., 2017) and level of alcohol consumption does not sufficiently account for variation in associated alcohol-related problems (Sadava, 1985). However, studies that have assessed negative consequences at the daily level indicate that PTSD symptoms are associated with alcohol problems over and above daily drinking (Gaher et al., 2014; Hruska, Pacella, George, & Delahanty, 2017; Wilson et al., 2017). Exacerbations of PTSS may reduce effective deliberative control and enhance associative processes resulting in deficits in adaptive regulatory control (Lieberman, 2007; McCarthy, Curtin, Piper, & Baker, 2010). In this regard, exacerbations in PTSS may result in dyscontrolled drinking characteristic of dependence syndrome and contribute to a wide variety of conduct related problems (e.g., interpersonal conflict) that can occur independent of drinking level. This perspective is consistent with between-subjects research indicating that associations between PTSD and alcohol-related problems are mediated by both affect and behavioral dysregulation (Miller, Vogt, Mozley, Kaloupek, & Keane, 2006; Read, Merrill, Griffin, Bachrach, & Khan, 2014; Simons et al., 2017). This suggests that the functional association extends beyond coping with negative affect and symptoms and that there are two distinct pathways linking PTSD and alcohol related problems. We propose that these two pathways are associated with different types of problems: The negative affect pathway being primarily associated with the development of alcohol dependence syndrome and the disinhibition pathway being associated with other externalizing behaviors that are associated with PTSD and alcohol use (i.e., conduct problems such as assault, interpersonal conflict, etc.).
Affective and Behavioral Dysregulation
Although PTSD, AUD, and associated conduct problems are highly comorbid there is considerable variation in these associations across persons suggesting that individual characteristics may moderate associations between PTSS and externalizing problems. Affective lability refers to the frequency, speed, and range of changes in affective states. Labile affect indicates deficits in regulatory control of emotion and is associated with borderline personality disorder, bipolar disorder, and substance use disorder (Henry et al., 2008; Tarter et al., 2003; Trull et al., 2008). Previous research indicates that lability is associated with alcohol and other substance use disorder symptoms over and above mean level of negative affect (Jahng et al., 2011; Mohr, Arpin, & McCabe, 2015; Simons, Wills, & Neal, 2014; Weinstein, Mermelstein, Shiffman, & Flay, 2008). Emotional instability in the context of substance use may foster the development of conditioned response biases characteristic of compulsive substance use (McCarthy et al., 2010). Here we propose that affect lability acts as a vulnerability factor predicting greater higher level and growth of dependence syndrome symptoms overtime and increasing the strength of within-person associations between PTSS, drinking, and dependence syndrome symptoms.
Disinhibition is a central risk factor for both substance use disorder as well as conduct problems (Belcher, Volkow, Moeller, & Ferré, 2014; Young et al., 2009). Interpersonal conflict, assault, and sexual risk behavior all occur at increased rates among people characterized by greater disinhibition (Hahn, Simons, & Simons, 2016; Leone, Crane, Parrott, & Eckhardt, 2016; Veith, Russell, & King, 2017). In the HiTOP model, the externalizing disinhibition dimension has links to both substance use disorder and disorders of conduct (e.g., antisocial personality disorder, conduct disorder; Kotov et al., 2017). (Dis)inhibition is traditionally characterized by a lack of constraint. A complementary perspective emphasizes the predominance of associative processes and heightened reactivity to stimuli (Carver, Johnson, & Timpano, 2017; Lieberman, 2007). Alcohol intoxication is also theorized to increase maladaptive behavioral responses by narrowing cognitive processing to salient cues, contributing to greater reactivity to the immediate environment (Steele & Josephs, 1990). Similarly, extreme emotion can result in reductions of deliberate control and increases in reflexive responding (Jones et al., 2013; Lieberman, 2007; Tomko et al., 2015). Hence, both PTSS symptoms and alcohol may be expected to result in momentary shifts in disinhibited behavior (e.g., interpersonal conflict). Trait disinhibition may be expected to exacerbate this process. In this regard, disinhibition and related constructs moderate within-person associations between drinking and alcohol-related problems (Neal & Carey, 2007; Simons, Gaher, Oliver, Bush, & Palmer, 2005; Simons, Simons, Maisto, Hahn, & Walters, 2018; Simons, Wills, et al., 2016).
Current study
This experience sampling study used an intensive measurement burst design to test hypotheses regarding the temporal associations between PTSS, drinking, alcohol dependence syndrome, and conduct problems. The measurement burst design incorporated experience sampling in seven 1 to 3 week measurement “bursts” over the course of approximately 1.5 years. The design has several benefits. First, we were able to obtain 10 weeks of experience sampling while minimizing fatigue. Acute exacerbations of PTSS, dependence syndrome symptoms, and conduct problems may be relatively infrequent and hence it is important to obtain a sufficient number of time points to characterize the pattern of associations. Second, we were able to test hypotheses regarding both day-to-day effects as well as systematic change over the longer study period.
Self-medication has been a predominant theoretical rationale linking PTSS and AUD (Haller & Chassin, 2014). However, we argue that dysregulation of emotion and behavior associated with PTSS increases the likelihood of both alcohol dependence syndrome as well as conduct problems over and above drinking level, a pattern that is not well accounted for by individuals increasing drinking to cope with symptoms. We used time-series analytic techniques to test the hypothesis that PTSS would be a leading indicator of both alcohol dependence syndrome and conduct problems. The analyses incorporated autoregressive effects and growth factors to model temporal trends while accounting for autocorrelational structure in the data, and drinking was included as a covariate. The analytic model thus provides a robust test of the within-person (lagged) effect of PTSS on subsequent (next day) dependence syndrome and conduct problems independent of temporal trends, drinking behavior, and the autoregressive effect (e.g., yesterday’s dependence predicting today’s dependence). In addition, we tested for potential reciprocal effects consistent with a mutual maintenance perspective by estimating whether increases in dependence syndrome or conduct problems are leading indicators of PTSS symptoms. We hypothesized that dependence syndrome but not conduct problems would be a leading indicator of PTSS symptoms.
Dysregulation in affect (lability) and behavior (disinhibition) at baseline were hypothesized to be vulnerability factors. In this regard, lability and disinhibition were expected to predict higher initial levels and growth of dependence syndrome symptoms and conduct problems, respectively, over the follow-up period. In addition, lability and disinhibition were hypothesized to moderate within-person associations between PTSS, drinking, and the outcomes. Finally, we tested whether lability and disinhibition predict the strength of autoregressive effects of the outcomes. The autoregressive parameter indicates the extent to which deviations from the individual’s expected value at time t-1 (i.e., yesterday) predict subsequent behavior at time t (today). Stronger autoregressive parameters indicate a slower return to baseline or conversely, a carry-over effect of past behavior that is not accounted for by the other time-varying constructs (Hamaker & Grasman, 2015). For example, a stronger autoregressive effect of dependence syndrome symptoms over time may imply greater perpetuation of AUD symptoms and deficits in the ability to modulate drinking behavior in response to changing environmental contingencies. In this regard, the autoregressive parameter may be conceptualized as the manifestation of the latent alcohol use disorder itself. Consistent with previous research and theory, we anticipated that affect lability effects would be more pronounced in the dependence syndrome relative to conduct problems model (McCarthy et al., 2010; Simons et al., 2017).
Method
Participants
Participants were 276 Operation Iraqi Freedom, Operation Enduring Freedom, and Operation New Dawn (OIF/OEF/OND) veterans aged 21 to 51 (M = 33.31, SD = 6.57). Fourteen percent were women. The sample was 82% white, 10% black, 3% multiracial, 1% Asian, and 5% other races or did not respond. Eight percent were Hispanic. Approximately 50% were currently married, 26% never married, and 23% currently divorced or separated. Mean yearly income was $38,726.12 (SD = 28,108.65). Highest level of education was as follows: high school diploma or General Equivalency Diploma (GED; 33%), trade school (9%), associate degree (22%), bachelor degree (28%), graduate degree (6%), some college education but no degree (3%). Additional detail regarding sample characteristics can be found in a previous paper based on this sample (Simons et al., 2017). The analysis sample for the multilevel models was 250 (see retention and compliance section).
Procedure
OIF/OEF/OND veterans were recruited from two communities (Tampa Bay area, FL and Vermillion / Sioux Falls, SD). Participants were recruited from the local Veteran Affairs Medical Centers, local universities, and surrounding communities via newspaper advertisements, flyers, mail correspondence, and clinician referral. Inclusion criteria included OIF/OEF/OND veteran status, current or past history of alcohol use, and ability to read English at eighth grade level. Exclusion criteria included psychosis and severe alcohol dependence (i.e., presenting acute medical risk). Participants completed a baseline assessment and then were enrolled in an experience sampling method (ESM) study for approximately 1.5 years. Participants were provided with a Samsung Galaxy Player 5.0 loaded with the Android momentary assessment software (Simons & Gropel, 2012). As part of the baseline assessment, the Structured Clinical Interview for DSM-IV-TR (American Psychiatric Association, 2000) Patient Edition (SCID-I / P; First, Spitzer, Gibbon, & Williams, January, 2010) was administered. This included the anxiety and substance use disorder modules, which were used to assess PTSD and AUD for sample description.
The ESM study was a measurement burst design with 10 weeks of sampling in 7 bursts across the 1.5 years. Burst 1 was 2 weeks, burst 4 was 3 weeks, and bursts 2, 3, 5, 6 and 7 were 1 week in length. The two longer bursts were included to increase the number of consecutive days for analysis of lagged effects. The bursts were separated by approximately 3 months and research staff contacted participants to schedule the appointments. The experience sampling assessments used here included a self-initiated morning assessment that was to be completed between waking and 10 a.m. and 8 random assessments that occurred between 10 a.m. and 2 a.m. Random prompts were followed by a reminder prompt 15 minutes later and then expired after 30 minutes. Participants could disable prompts when sleeping or when they would otherwise be unsafe or unable to respond (e.g., driving). Each morning and random assessment took approximately 2 to 3 minutes to complete. All procedures were approved by the respective institutional review boards. Participants were paid $25 for the baseline assessment and up to $100 per week in the ESM study contingent on performance. Participation was voluntary and responses were confidential.
Diagnostic Interview
Structured Clinical Interview for DSM-IV-TR Axis I-Patient Edition
(SCID-I / P; First et al., January, 2010). The psychotic screen, substance use, mood, and anxiety modules were administered to participants by trained clinical interviewers. This was used for determining PTSD and AUD for sample description and to assesses exclusion criteria (psychosis and severe alcohol dependence). Previous research supports the concurrent validity of the SCID I/P AUD diagnoses among veterans (DeMarce, Lash, Parker, Burke, & Grambow, 2013). Inter-rater reliability of the SCID I/P for AUD (Kappa = 0.65 – 1.0) and PTSD (Kappa = 0.77 – 1.0) is moderate to strong in previous research (Lobbestael, Leurgans, & Arntz, 2011; Zanarini & Frankenburg, 2001).
Baseline Measures
Affect Lability.
Lability was assessed by the Affective Lability Scales – Short form (Oliver & Simons, 2004). The subscales reflect affective lability in respect to vacillating between depression and elation (8 items), anxiety and depression (5 items), and anger and euthymic mood (5 items). Each item was rated on a 4-point anchored rating scale (1 = Very undescriptive of me, 4 = Very descriptive of me). The construct validity is supported by moderate associations with theoretically related constructs (e.g., urgency, emotional control, affect intensity; behavioral inhibition, behavioral activation; Dir, Karyadi, & Cyders, 2013; Emery & Simons, 2017; Oliver & Simons, 2004), criterion variables (e.g., AUD symptoms, suicide attempts; Aas et al., 2017; Lagerberg et al., 2017), and expected associations with clinical diagnoses (e.g., bipolar disorder; Aas et al., 2015; Marwaha et al., 2016). The mean of the three subscales was the measure of lability (α = .88).
Disinhibition.
Disinhibition was comprised of three indicators reflecting impulsivity (5 items; (Eysenck, Pearson, Easting, & Allsopp, 1985)), distractibility (6 items; (Kendall & Williams, 1982)), and impatience (3 items; (Kendall & Williams, 1982)). Each item was rated on a 5-point anchored rating scale (1 = Not at all true, 5 = Very true). These subscales load on a replicable latent factor of poor behavioral control in previous research (Simons et al., 2017; Simons, Wills, et al., 2016; Wills, Pokhrel, Morehouse, & Fenster, 2011). Construct validity is supported by expected associations with theoretically related constructs and criterion variables (e.g., behavioral activation, self-control, substance use and associated problems; Emery & Simons, 2017; Wills, Simons, & Gibbons, 2015). Cronbach’s alpha in the current sample was .78.
Alcohol Use Disorders Identification Test (AUDIT).
The AUDIT (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001; Bohn, Babor, & Kranzler, 1995) was used to assess hazardous drinking for the purpose of sample description. Each item was rated on an anchored rating scale. The AUDIT is a well-established 10-item screening measure with excellent psychometric properties (Babor et al., 2001; Donovan, Kivlahan, Doyle, Longabaugh, & Greenfield, 2006). A cut-score of 8 or higher indicates potential hazardous alcohol use (Babor et al., 2001).
PTSD Checklist-Military Version for DSM-IV (PCL).
The PCL (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Weathers, Litz, Herman, Huska, & Keane, 1993) was used to assess PTSD symptoms at baseline for sample description. Each item was rated on a 5-point anchored rating scale (1 = Not at all, 5 = Extremely).The scale has good sensitivity (0.82) and specificity (0.83) in predicting PTSD diagnoses in veterans (Weathers et al., 1993). Cronbach’s alpha in the current sample was 0.97.
Experience sampling measures
Posttraumatic stress symptoms (PTSS).
Each random prompt included a checklist of 15 dichotomous DSM-IV PTSD symptoms occurring in the past 30 minutes. Only 15 of the 17 potential symptoms were included in the random assessments because two items refer to sleep behavior. These two symptoms regarding difficulty sleeping and distressing dreams about their traumatic event were assessed by two dichotomous items in the self-initiated morning assessment. The PTSD variable was the percentage of items endorsed across all assessments. To scale the variance, this was multiplied by 17. Previous research supports the criterion validity of the sampling protocol (Gaher et al., 2014).
Drinking.
Each random prompt assessed number of standard drinks consumed in the past 30 minutes on a 7-point scale (0 to 6 or more drinks). The total number of drinks across all assessments was the drinking variable. In the preliminary analysis, an exposure variable equal to the number of completed assessments accounts for individual differences in response rates. Previous research supports the validity of the sampling protocol against a gold standard of transdermal alcohol monitoring (Simons, Wills, Emery, & Marks, 2015).
Alcohol dependence syndrome.
Random prompts included checklists of seven dichotomous dependence syndrome symptoms experienced in the last 30 minutes (e.g., felt alcohol effects less, drank when promised not to, tried unsuccessfully to limit, drank more than intended). In addition, the self-initiated morning assessment included dichotomous items assessing hangover, withdrawal symptoms, inability to stop drinking, and additional items unlikely to be endorsed during the random assessments (e.g., blackout, passing out). The total number of symptoms endorsed across all assessments was the dependence syndrome outcome. In the analyses, an exposure variable equal to the number of completed assessments accounts for individual differences in response rates. Previous research supports the criterion validity of the sampling protocol in respect to DSM-IV alcohol dependence diagnostic criteria (Simons, Dvorak, Batien, & Wray, 2010; Simons et al., 2014).
Conduct problems.
Random prompts included checklists of eight conduct problems experienced in the last 30 minutes (e.g., getting into an argument, acting mean, risk taking, damaging relationship). In addition, the self-initiated morning assessment included assessments of five additional items that may be missed during the random assessments (e.g., risky sex, physical assault). Each item was rated dichotomously and assessed behavior independent of drinking. The total number of problems endorsed across all assessments was the conduct problems outcome. In the analyses, an exposure variable equal to the number of completed assessments accounted for individual differences in response rates. Previous research with similar item sets support the criterion validity of the protocol (Simons et al., 2005; Simons et al., 2018; Simons, Wills, et al., 2016).
Analysis plan
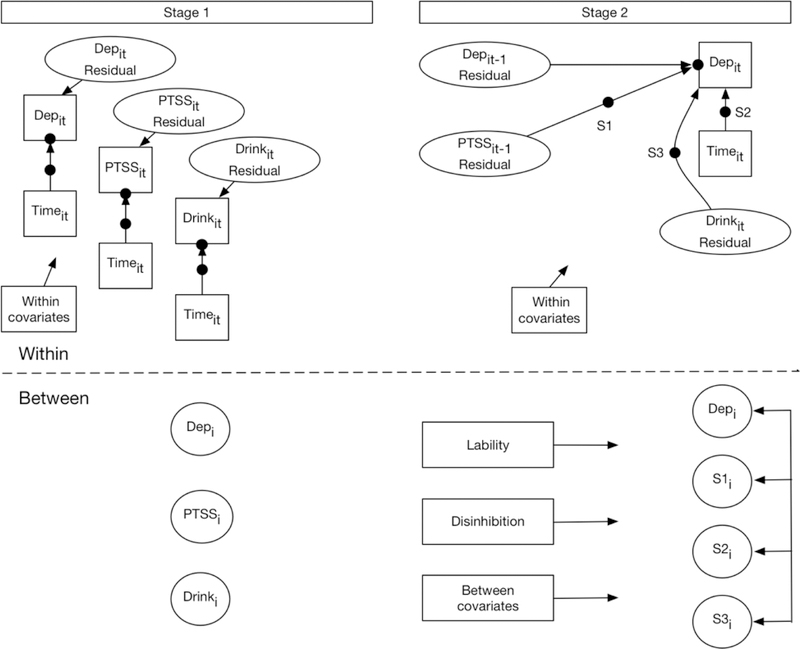
We took a two-stage approach to the data analysis (see Figure 1). Models were estimated in Stata 14 (StataCorp, 2015). First, we estimated four multilevel models with days (Level 1 (L1)) nested in person (Level 2 (L2)) predicting daily PTSS, drinking, dependence syndrome, and conduct problems. The models included time in the study, time squared, and six day-of-the-week dummy-coded indicators as predictors.1 The models included a random intercept and a random slope for the linear and quadratic effects of the time variable (days since baseline). PTSS were modeled as a continuous outcome. Drinking, dependence syndrome, and conduct problems were modeled as count variables using a negative binomial distribution and an exposure variable to account for differences in number of daily surveys completed. For each model, time-specific residual scores were estimated. These estimates reflect the deviations from individuals’ expected scores removing temporal trend and day of the week effects.
Figure 1.
Conceptual diagram of the two-stage data analytic approach. The dependence syndrome (Dep.) model is used for illustration. Solid dots are random intercepts and slopes. The “i” subscript stands for individual. Time (t) is days since initiating study. Hence, it-1 is a 1-day lagged effect for person i. The path from Depit-1 → Depit is the autoregressive effect. For clarity, some elements are omitted (e.g., exposure, time2, day of the week indicators, interactions between L2 variables and L1 variables with fixed slopes, etc. ).
Second, we used these residual scores as predictors in the analytic models. Each model included the 1-day lagged residual for the outcome (i.e., autoregressive effect). The model for conduct problems and alcohol dependence syndrome included the 1-day lagged residual PTSS score and the concurrent drinking residual score. In addition, the models included six day-of-the-week indicators, elapsed time since initiating study, and the time quadratic term at L1. At L2, the models included grand mean centered lability, disinhibition, gender, age, site, and the subject mean of time in study. Time, time quadratic term, PTSS, and drinking slopes were predicted by lability, disinhibition, gender, and age. These tested the hypothesized interaction effects of lability and disinhibition controlling for gender and age. To ensure the time interactions reflected the influence of L2 variables on within-person growth, corresponding interactions with L2 (subject mean) time were also included (Enders & Tofighi, 2007). Conduct problems and dependence syndrome symptoms were count outcomes with a negative binomial reference distribution. An exposure variable equal to the number of assessments completed each day was included and hence the models estimate a rate. We included random variance components for the time, time quadratic, PTSS, drinking, and autoregressive slopes if they were substantially different from zero. The slope and intercept components were allowed to covary.
To test the reciprocal effect, a mixed-effect model was estimated with PTSS as the outcome and the following L1 predictors: elapsed time in study, the time quadratic term, six day-of the-week indicators, and the 1-day lagged residual scores for dependence syndrome, conduct problems, and drinking. At level 2, gender, age, site, lability, disinhibition, and subject mean time in study were included. Consistent with the above models, gender, age, lability, and disinhibition had effects on the L1 time, time quadratic, PTSS, drinking, dependence, and conduct problems slopes.
This two-stage approach has several advantages. First, the estimated residuals all have a person-mean of zero and reflect deviations not only from the person’s mean, but deviations from the person’s expected value on a given day in their time series. Thus, the inclusion of lagged residuals allow for the estimation of lagged within-person effects, and the inclusion of estimated person-level intercepts, linear, and quadratic slopes allow for the estimation of between-person effects. Second, use of the lagged residual scores of the outcome of interest explicitly addresses the serial auto-correlation. Third, these person-centered, detrended, scores account for variations in response rate due to the inclusion of the exposure variable for the count outcomes. Fourth, multivariate longitudinal models of this nature (particularly with count outcomes) cannot be estimated with conventional software making the two-stage approach necessary.
Results
Retention and protocol compliance
Of the 276 completing the baseline assessment, 271 initiated the experience sampling. The analysis sample was comprised of the 250 participants who provided at least 1 week of data with > 33% response rate for the analyses.2 The analysis sample completed 75% of random prompts and 87% of self-initiated morning assessments. On average participants provided 56.2 (median = 65) days of data each and the mean time in the study was 1.57 (0.62) years. Retention in the study (defined by subject mean elapsed days) was modestly inversely associated with lability, PTSS, and conduct problems (r’s ≤ .21).
Descriptive statistics
Table 1 includes descriptive statistics for the analytic sample. Table 2 presents the between-person correlations. Baseline lability and disinhibition exhibited small to moderate associations with dependence syndrome symptoms and conduct problems but not drinking level. PTSD symptoms exhibited strong associations with both conduct problems and dependence syndrome symptoms and small to moderate associations with drinking level. The baseline diagnostic interview indicated that 39% of participants met DSM-IV-TR criteria for a current PTSD diagnosis and an additional 5% had a lifetime history of PTSD. The mean score on the PCL was 47.02 (SD = 18.89). Based on a cut-score of 50 on the PCL, approximately 44% were predicted to meet criteria for a PTSD diagnosis (U.S. Department of Veteran Affairs, 2012). Finally, 61.20%, reported at least 1 criteria B (re-experiencing), 1 criteria C (avoidance and numbing), and 1 criteria D (arousal) symptom, suggesting potential subthreshold PTSD (Pietrzak, Goldstein, Southwick, & Grant, 2011). Fourteen percent of participants met DSM-IV-TR criteria for a current alcohol dependence diagnosis, 14% were in early remission or sustained partial remission, and 13% were in sustained full remission. One percent met criteria for a current alcohol abuse diagnosis. On the AUDIT, 55% scored 8 or higher, indicating potential hazardous alcohol use.
Table 1.
Descriptive statistics
| Variable | N | M or % | SD | min | max | skewness | kurtosis |
|---|---|---|---|---|---|---|---|
| Site | 118SD/132FL | 52.8%FL | |||||
| Gender | 36W/214M | 85.6%M | |||||
| Age | 250 | 33.42 | (6.43) | 21.00 | 51.00 | 0.58 | 2.71 |
| ALS | 250 | 2.10 | (0.77) | 1.00 | 4.00 | 0.38 | 2.32 |
| Disinh | 250 | 2.11 | (0.69) | 1.00 | 4.94 | 0.91 | 3.95 |
| SM time | 250 | 0.77 | (0.33) | 0.01 | 1.98 | −0.38 | 4.26 |
| Time | 14041 | 0.86 | (0.62) | 0.00 | 3.20 | 0.38 | 2.76 |
| PTSS | 14041 | 1.51 | (2.59) | 0.00 | 17.00 | 2.60 | 10.63 |
| Drinks | 14041 | 1.80 | (3.53) | 0.00 | 43.00 | 4.40 | 32.21 |
| Conduct prob. | 14041 | 1.21 | (3.03) | 0.00 | 39.00 | 4.75 | 34.23 |
| Dependence syn. | 14041 | 0.62 | (2.25) | 0.00 | 38.00 | 6.83 | 64.89 |
Note. Boldface are the experience sampling measures. FL= Florida site, SD = South Dakota, W. women, M = men. Disinh= Disinhibition, SM time= subject mean elapsed time in study in years, Time = elapsed time in years, PTSS= posttraumatic stress symptoms, drinks = daily drinks, conduct problems daily conduct problems, dependence symptoms = daily dependence symptoms. Drinks, conduct problems, and dependence syndrome symptoms are counts for the day across all assessments. PTSS symptoms are mean number of symptoms endorsed per assessment.
Table 2.
Between person correlations
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Site | 1.00 | |||||||||
| 2. Gender | −.16* | 1.00 | ||||||||
| 3. Age | .07 | .04 | 1.00 | |||||||
| 4. ALS | .34*** | −.03 | .11 | 1.00 | ||||||
| 5. Disinhibition | .19** | −.06 | .02 | .60*** | 1.00 | |||||
| 6. Time | −.28*** | −.02 | −.04 | −.16** | −.02 | 1.00 | .01 | −.04*** | .05*** | .06*** |
| 7. PTSS | .33*** | −.02 | .17** | .44*** | .34*** | −.21** | 1.00 | .06*** | .43*** | .28*** |
| 8. Drinks | .09 | .10 | .10 | .12 | .03 | −.08 | .27*** | 1.00 | .16*** | .32*** |
| 9. Conduct pro. | .17* | .02 | .11 | .28*** | .30*** | −.15* | .68*** | .47*** | 1.00 | .52*** |
| 10. Dep. syn. | .12 | .06 | .11 | .21** | .17** | −.10 | .56*** | .62*** | .83*** | 1.00 |
Note. N = 250. Site is coded 1=South Dakota, 2 = Florida. Gender is coded 0 = women, 1 = men. Time, PTSS, Drinks, Conduct pro., and Dep. syn. are the person means. Time = subject mean elapsed time in study, ALS=affect lability scale, pro. =Problems, Dep. Syn.= dependence syndrome. Within-person correlations are above the diagonal.
p < 0.05
p < 0.01
p < 0.001
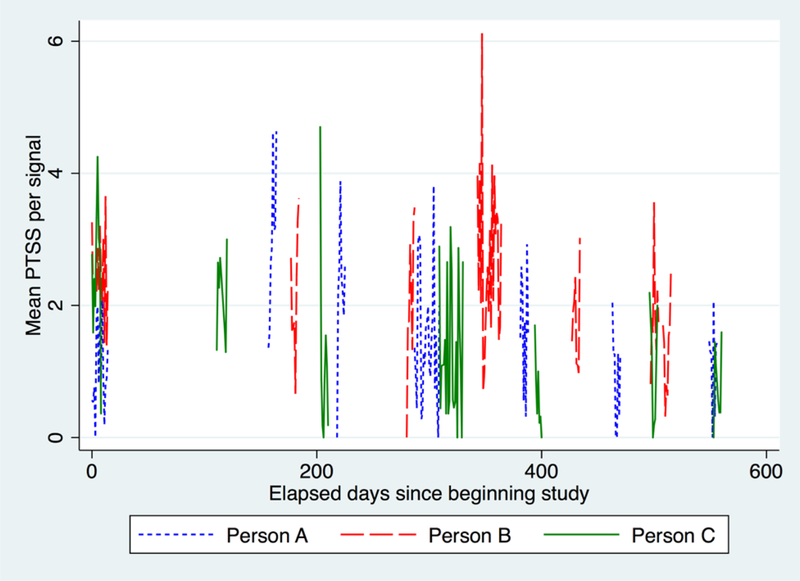
During the ESM period, participants endorsed no PTSD symptoms on 38% of days. The mean number of symptoms per assessment was at least 1 on 35% of days, 2 on 23% of days, 3 on 17% of days, 4 on 13% of days, and 5 on 9% of days. The intraclass correlation coefficient (ICC) for PTSS was 0.75, indicating 25% of the variance in PTSS was at the within-persons level. The average within-person standard deviation of daily PTSS symptoms per signal was 1.04, indicating substantial variation in symptoms day-to-day. Figure 2 illustrates variation in symptoms across days. Participants reported drinking on 53% of days and drinking approximately 5 standard drinks (M = 5.86, SD = 5.15) per drinking day. For the drinking, dependence syndrome, and conduct problems count outcomes, we calculated ICC based on presence / absence of the outcome using the formula for dichotomous outcomes (Snijders & Bosker, 1999). The ICCs were 0.27 (drinking), 0.43 (dependence syndrome), and 0.45 (conduct problems). This indicates that the majority of variability in the likelihood of each across days was at the within-persons level.
Figure 2.
Graph of three participants to illustrate variation in posttraumatic stress symptoms (PTSS) symptoms across days and bursts. The sample average within-person SD of PTSS symptoms is 1.04. The within-person SD of these participants ranges from 1.02 to 1.09. The PTSS intraclass correlation coefficient (ICC) = 0.75, indicating 25% of the variance is at the within-person level. PTSS symptoms were chosen for illustration because they exhibit the lower bound of within-person variation of the outcomes.
Multilevel models
Dependence syndrome.
The dependence syndrome model included a random intercept, and random slopes for time, time squared, lagged (residual of) PTSS, and (residual of) drinking. Model results are contained in Tables 3 and 4. The results indicated a significant association between the residual PTSSt-1 and dependence syndromet. The Incident Rate Ratio (IRR) indicates that the incident rate of dependence syndrome symptoms at time t increased by 13% for every unit increase in the residual for PTSS at time t-1. This within-person effect was significant after controlling for the residual of dependence syndrome at time t-1 (i.e., the autoregression), drinking at time t, the temporal trend, and the day of the week covariates. It is thus is a robust test of the prospective association between PTSS and subsequent dependence syndrome symptoms at the within-person level. In addition to the PTSSt-1 effect, there were significant within-person effects of both lagged dependence syndrome symptoms (i.e., at time t-1) and concurrent drinking (i.e., at time t). The IRR indicated that for every unit increase in dependence syndrome symptoms at time t-1 there was a 4% increase in the incident rate of dependence syndrome symptoms at time t. For drinking, the IRR indicates that for every unit increase in drinkingt, the incident rate of dependence syndrome at time t increased by 13.32 times. Given the cross-level interactions, these within-person associations reflect the effect at mean levels of age, lability, disinhibition, and gender (i.e., average effect given the proportion of men and women).
Table 3.
Multilevel model of dependence syndrome
| Variable | b | se | z | p | 95%CI | IRR |
|---|---|---|---|---|---|---|
| Time | 0.09 | 0.23 | 0.40 | 0.692 | −0.36, 0.54 | 1.10 |
| x Gender | −0.31 | 0.58 | −0.54 | 0.588 | −1.45, 0.82 | 0.73 |
| x Age | 0.01 | 0.03 | 0.30 | 0.765 | −0.06, 0.08 | 1.01 |
| x ALS | −0.15 | 0.34 | −0.44 | 0.662 | −0.83, 0.53 | 0.86 |
| x Disinh | 0.01 | 0.36 | 0.04 | 0.968 | −0.70, 0.73 | 1.01 |
| Time2 | −0.12 | 0.12 | −1.00 | 0.319 | −0.36, 0.12 | 0.88 |
| x Gender | 0.53 | 0.31 | 1.70 | 0.090 | −0.08, 1.14 | 1.69 |
| x Age | −0.01 | 0.02 | −0.79 | 0.427 | −0.05, 0.02 | 0.99 |
| x ALS | 0.14 | 0.18 | 0.76 | 0.447 | −0.22, 0.49 | 1.15 |
| x Disinh | −0.06 | 0.19 | −0.33 | 0.740 | −0.44, 0.31 | 0.94 |
| PTSS resid t−1 | 0.12 | 0.03 | 3.41 | 0.001 | 0.05, 0.19 | 1.13 |
| x Gender | 0.02 | 0.05 | 0.43 | 0.668 | −0.08, 0.13 | 1.02 |
| x Age | −0.00 | 0.00 | −1.24 | 0.217 | −0.01, 0.00 | 1.00 |
| x ALS | 0.01 | 0.04 | 0.36 | 0.721 | −0.06, 0.09 | 1.01 |
| x Disinh | −0.00 | 0.03 | −0.01 | 0.996 | −0.07, 0.07 | 1.00 |
| Depend resid t−1 | 0.04 | 0.01 | 5.05 | <0.001 | 0.03, 0.06 | 1.04 |
| x Gender | −0.08 | 0.03 | −2.75 | 0.006 | −0.14, −0.02 | 0.92 |
| x Age | −0.00 | 0.00 | −0.41 | 0.681 | −0.00, 0.00 | 1.00 |
| x ALS | 0.03 | 0.01 | 2.49 | 0.013 | 0.01, 0.06 | 1.03 |
| x Disinh | −0.01 | 0.01 | −0.51 | 0.612 | −0.03, 0.02 | 0.99 |
| Drink resid | 2.59 | 0.15 | 17.51 | <0.001 | 2.30, 2.88 | 13.32 |
| x Gender | −0.04 | 0.39 | −0.11 | 0.915 | −0.80, 0.72 | 0.96 |
| x Age | 0.00 | 0.02 | 0.15 | 0.877 | −0.04, 0.05 | 1.00 |
| x ALS | −0.42 | 0.21 | −1.99 | 0.046 | −0.84, −0.01 | 0.66 |
| x Disinh | −0.28 | 0.24 | −1.17 | 0.241 | −0.74, 0.19 | 0.76 |
| Site | 0.03 | 0.20 | 0.17 | 0.868 | −0.36, 0.42 | 1.03 |
| Gender | −0.31 | 0.32 | −0.98 | 0.325 | −0.93, 0.31 | 0.73 |
| Age | −0.01 | 0.02 | −0.74 | 0.461 | −0.05, 0.02 | 0.99 |
| ALS | 0.53 | 0.18 | 2.89 | 0.004 | 0.17, 0.88 | 1.69 |
| Disinh | 0.45 | 0.19 | 2.30 | 0.022 | 0.07, 0.83 | 1.57 |
| SM time | −0.37 | 0.32 | −1.15 | 0.252 | −1.00, 0.26 | 0.69 |
| SM time x gender | −0.85 | 1.09 | −0.78 | 0.437 | −2.98, 1.29 | 0.43 |
| SM time x Age | −0.04 | 0.05 | −0.90 | 0.367 | −0.13, 0.05 | 0.96 |
| SM time x ALS | −0.54 | 0.53 | −1.00 | 0.316 | −1.58, 0.51 | 0.59 |
| SM time x Disinh | 0.27 | 0.57 | 0.48 | 0.628 | −0.83, 1.38 | 1.32 |
| Constant | −3.91 | 0.13 | −31.00 | <0.001 | −4.16, −3.67 |
Note. N = 14041 (250 persons), Log Likelihood = −9047.74, χ2(41)=562.99. Boldface are within-person effects. Italics are the effects of the between variables on L1 slopes. Days of week are omitted due to space. Symptoms were lower on Monday and higher on Friday and Saturday relative to Sunday. Depend = dependence syndrome. SM time = subject mean elapsed time in study. Disinh.=disinhibition. ALS= affect lability scale. Time is time elapsed since starting the study. Resid=residual.
Table 4.
Multilevel model of dependence syndrome - Random variances and covariances
| Random variance (covariance) | b | se | 95%CI |
|---|---|---|---|
| Time | 4.51 | 0.79 | 3.20, 6.37 |
| Time2 | 1.01 | 0.21 | 0.67, 1.51 |
| PTSS resid t-1 | 0.02 | 0.01 | 0.01, 0.04 |
| Drink resid | 1.78 | 0.37 | 1.19, 2.66 |
| Intercept | 1.96 | 0.28 | 1.48, 2.60 |
| (Time2, Time) | −1.97 | 0.39 | −2.74, −1.21 |
| ( PTSS resid t-1, Time) | 0.04 | 0.05 | −0.06, 0.15 |
| (Drink resid, Time) | −0.63 | 0.35 | −1.32, 0.06 |
| (Intercept, Time) | −0.96 | 0.39 | −1.73, −0.19 |
| (PTSS resid t-1, Time2) | −0.01 | 0.03 | −0.06, 0.05 |
| (Drink resid, Time2) | 0.11 | 0.19 | −0.26, 0.48 |
| (Intercept, Time2) | 0.43 | 0.20 | 0.04, 0.83 |
| (Drink resid, PTSS resid t-1) | −0.03 | 0.04 | −0.11, 0.04 |
| (Intercept, PTSS resid t-1) | −0.09 | 0.04 | −0.17, −0.01 |
| (Intercept, Drink resid) | −0.54 | 0.23 | −0.99, −0.10 |
Note. N = 14041 (250 persons), Log Likelihood = −9047.74, χ2(41)=562.99. Time is time elapsed since starting the study. Resid=residual. t-1 is a 1 day lag.
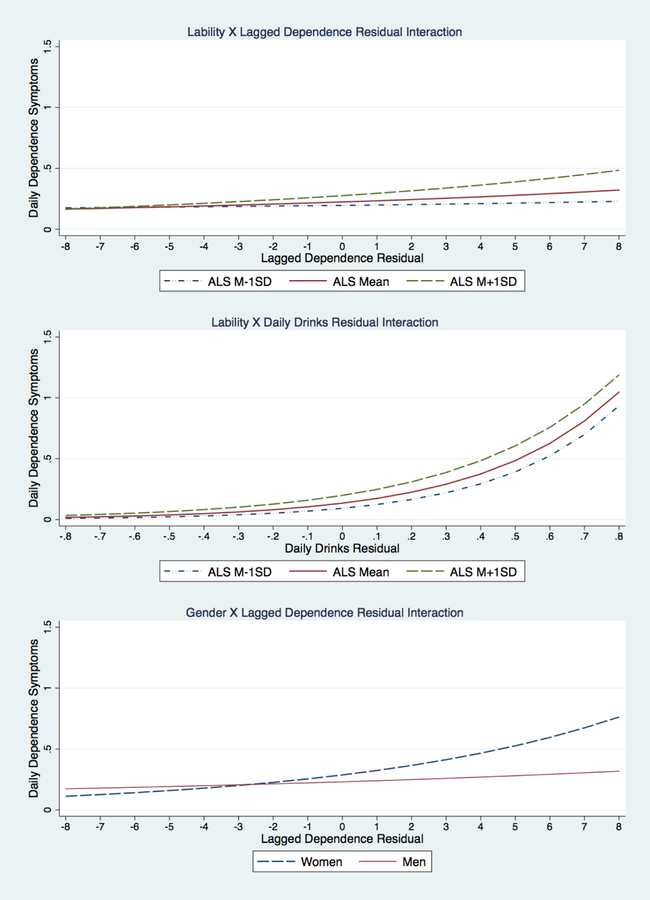
Lability at baseline was associated with more dependence syndrome symptoms over the follow-up period and moderated the within-person drinking effect and the autoregressive effect (See Figure 3). Consistent with our hypothesis, lability predicted stronger associations between drinking and dependence symptoms and stronger autoregressive effects. However, lability did not predict growth in symptoms (i.e., it did not moderate the effect of time). There was also a significant effect of gender on the autoregression parameter (see Figure 3) with women exhibiting stronger autoregressive effects.
Figure 3.
Plots of interactions from the dependence syndrome analysis. Daily drinks are scaled by dividing by 10. Lagged dependence effects are the autoregression over a 1-day lag. Time is elapsed days (scaled to years) since beginning study. ALS=affect lability scale. Disinh = Disinhibition.
Conduct problems.
The conduct problems model included random variance components for the time, time squared, and the lagged PTSS effect. Model results are contained in Tables 5 and 6. The results indicated a significant average association between PTSSt-1 and conduct problemst. The IRR indicated that for every unit increase in the lagged PTSS residual led to a 13% increase in the incident rate of conduct problems. This within-person effect was significant after controlling for conduct problems at time t-1 (i.e., autoregression), drinking at time t, the temporal trend, and the day of the week covariates. In addition to the PTSSt-1 effect, there were significant within-person effects of both lagged conduct problems (i.e., at time t-1) and concurrent drinking (i.e., at time t). The IRR indicated that for every unit increase in conduct problems at time t-1 there was a 7% increase in the incident rate of conduct problems at time t. For drinking, the IRR indicates that for every unit increase in drinkingt there is a 47% increase in the incident rate of conduct problems at time t. Given the cross-level interactions, these within-person associations reflect the effect at mean levels of age, lability, disinhibition, and gender (i.e., average effect given the proportion of men and women).
Table 5.
Multilevel model of conduct problems
| Variable | b | se | z | p | 95%CI | IRR |
|---|---|---|---|---|---|---|
| Time | 0.00 | 0.18 | 0.02 | 0.984 | −0.35, 0.36 | 1.00 |
| x Gender | 0.38 | 0.49 | 0.78 | 0.436 | −0.58, 1.34 | 1.46 |
| x Age | 0.00 | 0.03 | 0.03 | 0.974 | −0.05, 0.05 | 1.00 |
| x ALS | −0.07 | 0.29 | −0.26 | 0.796 | −0.64, 0.49 | 0.93 |
| x Disinh | −0.02 | 0.30 | −0.06 | 0.950 | −0.61, 0.58 | 0.98 |
| Time2 | −0.09 | 0.10 | −0.87 | 0.382 | −0.28, 0.11 | 0.92 |
| x Gender | 0.09 | 0.27 | 0.33 | 0.738 | −0.44, 0.62 | 1.09 |
| x Age | −0.00 | 0.01 | −0.18 | 0.854 | −0.03, 0.03 | 1.00 |
| x ALS | 0.02 | 0.16 | 0.10 | 0.920 | −0.29, 0.32 | 1.02 |
| x Disinh | −0.00 | 0.16 | −0.01 | 0.991 | −0.32, 0.32 | 1.00 |
| PTSS resid t-1 | 0.12 | 0.02 | 5.38 | <0.001 | 0.08, 0.16 | 1.13 |
| x Gender | 0.06 | 0.03 | 1.79 | 0.074 | −0.01, 0.13 | 1.06 |
| x Age | 0.00 | 0.00 | 0.89 | 0.374 | −0.00, 0.01 | 1.00 |
| x ALS | −0.04 | 0.02 | −1.69 | 0.090 | −0.09, 0.01 | 0.96 |
| x Disinh | 0.00 | 0.02 | 0.17 | 0.867 | −0.04, 0.05 | 1.00 |
| Conduct resid t-1 | 0.07 | 0.01 | 10.53 | <0.001 | 0.05, 0.08 | 1.07 |
| x Gender | −0.07 | 0.02 | −3.56 | <0.001 | −0.10, −0.03 | 0.94 |
| x Age | −0.00 | 0.00 | −1.09 | 0.275 | −0.00, 0.00 | 1.00 |
| x ALS | −0.00 | 0.01 | −0.37 | 0.714 | −0.02, 0.01 | 1.00 |
| x Disinh | −0.01 | 0.01 | −1.03 | 0.302 | −0.03, 0.01 | 0.99 |
| Drink resid | 0.38 | 0.05 | 7.92 | <0.001 | 0.29, 0.48 | 1.47 |
| x Gender | −0.06 | 0.18 | −0.35 | 0.727 | −0.40, 0.28 | 0.94 |
| x Age | −0.01 | 0.01 | −2.03 | 0.042 | −0.03, −0.00 | 0.99 |
| x ALS | 0.03 | 0.07 | 0.35 | 0.730 | −0.12, 0.17 | 1.03 |
| x Disinh | −0.11 | 0.07 | −1.62 | 0.106 | −0.25, 0.02 | 0.89 |
| Site | 0.26 | 0.17 | 1.55 | 0.120 | −0.07, 0.59 | 1.30 |
| Gender | −0.47 | 0.25 | −1.92 | 0.055 | −0.95, 0.01 | 0.62 |
| Age | −0.01 | 0.01 | −0.58 | 0.563 | −0.03, 0.02 | 0.99 |
| ALS | 0.61 | 0.14 | 4.34 | <0.001 | 0.33, 0.89 | 1.84 |
| Disinh | 0.53 | 0.15 | 3.50 | <0.001 | 0.23, 0.82 | 1.69 |
| SM time | −0.42 | 0.26 | −1.61 | 0.107 | −0.94, 0.09 | 0.65 |
| SM time x Gender | 0.64 | 0.89 | 0.72 | 0.471 | −1.11, 2.40 | 1.90 |
| SM time x Age | −0.09 | 0.04 | −2.23 | 0.025 | −0.16, −0.01 | 0.92 |
| SM time x ALS | 0.43 | 0.44 | 0.98 | 0.326 | −0.43, 1.30 | 1.54 |
| SM time x Disinh | 0.09 | 0.45 | 0.21 | 0.834 | −0.78, 0.97 | 1.10 |
| Constant | −2.64 | 0.09 | −28.35 | <0.001 | −2.82, −2.45 |
Note. N = 14041 (250 persons), Log Likelihood = −15051.74, χ2(41)=473.98. Boldface are within-person effects. Italics are the effects of the between variables on L1 slopes. Days of week are omitted due to space. Symptoms were higher on Friday relative to Sunday. SM time = subject mean elapsed time in study. Disinh.=disinhibition. ALS= affect lability scale. Time is time elapsed since starting the study. Resid=residual.
Table 6.
Multilevel model of conduct problems - Random variances and covariances
| Random variance (covariance) | b | se | 95%CI |
|---|---|---|---|
| Time | 4.20 | 0.64 | 3.12, 5.65 |
| Time2 | 1.10 | 0.19 | 0.78, 1.54 |
| PTSS resid t-1 | 0.01 | 0.00 | 0.00, 0.02 |
| Intercept | 1.29 | 0.16 | 1.02, 1.65 |
| (Time2, Time) | −1.98 | 0.33 | −2.64, −1.33 |
| (PTSS resid t-1, Time) | −0.02 | 0.03 | −0.08, 0.05 |
| (Intercept, Time) | −0.43 | 0.25 | −0.92, 0.05 |
| (PTSS resid t-1, Time2) | −0.00 | 0.02 | −0.03, 0.03 |
| (Intercept, Time2) | 0.15 | 0.13 | −0.11, 0.41 |
| (Intercept, PTSS resid t-1) | −0.05 | 0.02 | −0.10, −0.01 |
Note. N = 14041 (250 persons), Log Likelihood = −15051.74, χ2(41)=473.98. Time is time elapsed since starting the study. Resid=residual. t-1 is a 1 day lag.
Both lability and disinhibition at baseline were associated with more conduct problems over the follow-up period. However, neither lability nor disinhibition predicted the between-person differences in growth in conduct problems over the course of the study. Moderating effects of disinhibition and lability on the lagged PTSS, concurrent drinking, and autoregressive slopes were not significant. However, the autoregressive effect was found to vary as a function gender. The autoregressive effect was stronger for women (similar finding to dependence). Finally, there was a stronger inverse association between subject mean time in the study and conduct problems for older participants (see Figure 4).
Figure 4.
Plots of interactions from the conduct problem analysis. Daily drinks are scaled by dividing by 10. Lags are t-1 day. Time is elapsed days (scaled to years) since beginning study. Daily PTSS are mean symptoms per assessment. ALS=affect lability scale. Disinh = Disinhibition.
Reciprocal effects on PTSS.
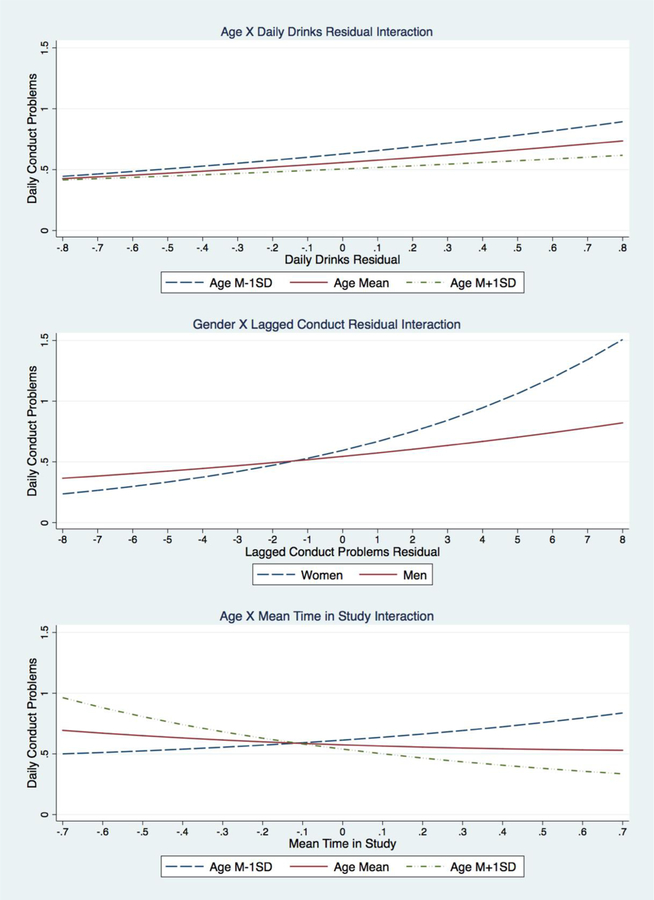
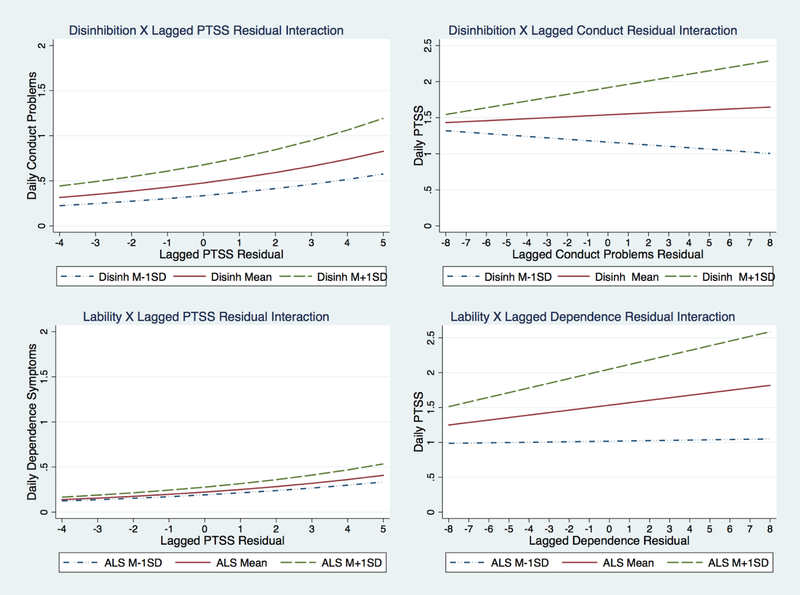
The PTSS model included random variance components for time, time squared, and lagged dependence syndrome, lagged conduct problems, concurrent drinking, and the PTSS autoregressive effect. Model results are in Tables 7 and 8. On average, PTSS symptoms did not exhibit significant change over time (i.e., the effect of time was not significant). The temporal trend (i.e., time and time2) varied as a function of lability. At higher levels of lability (M + 1SD), the association between time and PTSS symptoms was a U-shaped function, whereas at lower levels of lability (M − 1SD), it was an inverse U-shaped function. This is perhaps simply indicative of those with relatively high or low lability at baseline regressing to the mean over time. There was a significant association between dependence syndromet-1 and PTSSt, and this effect was stronger for those with higher lability. The average effect of lagged conduct problems was not significant, but the effect was stronger for those participants with higher levels of disinhibition (M + 1SD, b = 0.05, p = .004). Figure 5 depicts the lability by dependence syndromet-1 and disinhibition by conduct problemst-1 interactions along with the respective associations between PTSS and the outcomes from the previous models to illustrate the reciprocal effects over time. Drinking had an insignificant inverse association, which varied as a function of age. Younger participants (i.e., age M − 1 SD) had a significant inverse association between drinkingt-1 and PTSSt (b = −0.20, p = .006).
Table 7.
Multilevel model of reciprocal effects on PTSS
| Variable | b | se | z | p | 95% CI |
|---|---|---|---|---|---|
| Time | −0.08 | 0.18 | −0.43 | 0.670 | −0.44, 0.28 |
| x Gender | 0.44 | 0.52 | 0.84 | 0.400 | −0.58, 1.46 |
| x Age | 0.02 | 0.03 | 0.73 | 0.464 | −0.04, 0.08 |
| x ALS | −0.70 | 0.31 | −2.28 | 0.023 | −1.30, −0.10 |
| x Disinh | 0.58 | 0.34 | 1.73 | 0.083 | −0.08, 1.24 |
| Time2 | 0.05 | 0.10 | 0.55 | 0.585 | −0.14, 0.25 |
| x Gender | −0.05 | 0.28 | −0.17 | 0.862 | −0.59, 0.50 |
| x Age | −0.02 | 0.02 | −1.43 | 0.153 | −0.05, 0.01 |
| x ALS | 0.34 | 0.16 | 2.07 | 0.038 | 0.02, 0.66 |
| x Disinh | −0.27 | 0.18 | −1.49 | 0.137 | −0.62, 0.08 |
| PTSS resid t-1 | 0.23 | 0.02 | 10.71 | <0.001 | 0.19, 0.27 |
| x Gender | −0.10 | 0.05 | −1.92 | 0.055 | −0.20, 0.00 |
| x Age | 0.00 | 0.00 | 0.22 | 0.826 | −0.01, 0.01 |
| x ALS | 0.04 | 0.03 | 1.16 | 0.246 | −0.03, 0.10 |
| x Disinh | −0.03 | 0.03 | −0.79 | 0.432 | −0.09, 0.04 |
| Depend resid t-1 | 0.03 | 0.01 | 2.90 | 0.004 | 0.01, 0.06 |
| x Gender | −0.02 | 0.03 | −0.57 | 0.571 | −0.08, 0.05 |
| x Age | −0.00 | 0.00 | −0.38 | 0.706 | −0.00, 0.00 |
| x ALS | 0.04 | 0.02 | 2.23 | 0.026 | 0.00, 0.08 |
| x Disinh | −0.02 | 0.02 | −0.92 | 0.357 | −0.05, 0.02 |
| Conduct resid t-1 | 0.01 | 0.01 | 1.15 | 0.251 | −0.01, 0.03 |
| x Gender | 0.04 | 0.03 | 1.45 | 0.148 | −0.02, 0.10 |
| x Age | −0.00 | 0.00 | −1.70 | 0.089 | −0.01, 0.00 |
| x ALS | −0.03 | 0.02 | −1.57 | 0.117 | −0.06, 0.01 |
| x Disinh | 0.05 | 0.02 | 2.73 | 0.006 | 0.01, 0.08 |
| Drink resid t-1 | −0.07 | 0.05 | −1.43 | 0.152 | −0.16, 0.03 |
| x Gender | 0.10 | 0.16 | 0.67 | 0.504 | −0.20, 0.41 |
| x Age | 0.02 | 0.01 | 2.66 | 0.008 | 0.01, 0.04 |
| x ALS | −0.04 | 0.08 | −0.49 | 0.622 | −0.20, 0.12 |
| x Disinh | −0.13 | 0.08 | −1.57 | 0.117 | −0.30, 0.03 |
| Site | 0.81 | 0.26 | 3.11 | 0.002 | 0.30, 1.31 |
| Gender | −0.18 | 0.38 | −0.47 | 0.639 | −0.92, 0.57 |
| Age | 0.06 | 0.02 | 2.79 | 0.005 | 0.02, 0.09 |
| ALS | 1.02 | 0.21 | 4.75 | <0.001 | 0.60, 1.43 |
| Disinh | 0.31 | 0.23 | 1.31 | 0.189 | −0.15, 0.76 |
| SM time | −0.77 | 0.40 | −1.94 | 0.053 | −1.56, 0.01 |
| SM time x Gender | −0.70 | 1.44 | −0.49 | 0.624 | −3.52, 2.11 |
| SM time x Age | −0.10 | 0.06 | −1.64 | 0.100 | −0.21, 0.02 |
| SM time x ALS | −0.99 | 0.68 | −1.46 | 0.145 | −2.33, 0.34 |
| SM time x Disinh | 0.34 | 0.69 | 0.49 | 0.625 | −1.02, 1.70 |
| Constant | 1.62 | 0.13 | 12.42 | <0.001 | 1.36, 1.87 |
Note. N = 14020 (250 persons), Log Likelihood = −21728.75, χ2(46)=376.72. Boldface are within-person effects. Italics are the effects of the between variables on L1 slopes. Days of week are omitted due to space. Symptoms were higher on Monday- Friday relative to Sunday. SM time = subject mean elapsed time in study. Disinh.=disinhibition. ALS= affect lability scale. Time is time elapsed since starting the study. Resid=residual. Depend = dependence syndrome
Table 8.
Multilevel model of reciprocal effects on PTSS - Random variances and covariances
| Random variance (covariance) | b | se | 95%CI |
|---|---|---|---|
| Time | 6.78 | 0.74 | 5.48, 8.39 |
| Time2 | 1.85 | 0.22 | 1.46, 2.33 |
| Depend resid t-1 | 0.00 | 0.00 | 0.00, 0.01 |
| Conduct resid t-1 | 0.01 | 0.00 | 0.01, 0.01 |
| Drink resid t-1 | 0.08 | 0.03 | 0.03, 0.18 |
| PTSS resid t-1 | 0.05 | 0.01 | 0.03, 0.06 |
| Intercept | 3.67 | 0.36 | 3.03, 4.45 |
| (Time, Time2) | −3.15 | 0.38 | −3.90, −2.40 |
| (Time, Depend resid t-1) | 0.00 | 0.02 | −0.04, 0.04 |
| (Time, Conduct resid t-1) | 0.04 | 0.02 | 0.00, 0.09 |
| (Time, Drink resid t-1) | −0.03 | 0.10 | −0.22, 0.17 |
| (Time, PTSS resid t-1) | 0.03 | 0.04 | −0.06, 0.11 |
| (Time, Intercept) | −0.43 | 0.38 | −1.18, 0.33 |
| (Time2, Depend resid t-1) | 0.01 | 0.01 | −0.01, 0.03 |
| (Time2, Conduct resid t-1) | −0.04 | 0.01 | −0.07, −0.02 |
| (Time2, Drink resid t-1) | 0.04 | 0.05 | −0.05, 0.13 |
| (Time2, PTSS resid t-1) | 0.00 | 0.02 | −0.04, 0.05 |
| (Time2, Intercept) | −0.13 | 0.20 | −0.53, 0.27 |
| (Depend resid t-1, Conduct resid t-1) | 0.00 | 0.00 | 0.00, 0.00 |
| (Depend resid t-1, Drink resid t-1) | 0.00 | 0.01 | −0.01, 0.01 |
| (Depend resid t-1, PTSS resid t-1) | 0.00 | 0.00 | −0.01, 0.00 |
| (Depend resid t-1, Intercept) | −0.02 | 0.02 | −0.06, 0.02 |
| (Conduct resid t-1, Drink resid t-1) | 0.01 | 0.01 | −0.01, 0.02 |
| (Conduct resid t-1, PTSS resid t-1) | 0.00 | 0.00 | −0.01, 0.00 |
| (Conduct resid t-1, Intercept) | 0.02 | 0.02 | −0.02, 0.05 |
| (Drink resid t-1, PTSS resid t-1) | −0.02 | 0.01 | −0.04, 0.00 |
| (Drink resid t-1, Intercept) | −0.14 | 0.09 | −0.31, 0.04 |
| (PTSS resid t-1, Intercept) | 0.10 | 0.03 | 0.04, 0.17 |
Note. N = 14020 (250 persons), Log Likelihood = −21728.75, χ2(46)=376.72. Time is time elapsed since starting the study. Resid=residual. Depend = dependence syndrome
Figure 5.
Plots of interactions from the PTSS analysis (right column). Daily PTSS are mean symptoms per assessment. Lags are t-1 day. ALS=affect lability scale. Disinh = Disinhibition. The left column of graphs are effects of PTSS on conduct problems (upper left) and dependence syndrome (lower left). Interactions on left are not significant but are included to illustrate the reciprocal association as a function of the moderators (e.g., PTSSt-1 -> Dependence syndromet -> PTSSt+1).
Discussion
The results indicate complex within-person associations between PTSS, alcohol dependence syndrome, and conduct problems. The pattern of associations suggests that the acute exacerbation of PTSS fosters dysregulated behavior and emotion resulting in subsequent increases in alcohol dependence syndrome and conduct problems. The significant associations over and above concurrent alcohol consumption and associations with conduct problems irrespective of alcohol consumption suggest that this process is not simply due to conscious efforts to medicate aversive symptoms. Furthermore, there was evidence of reciprocal associations whereby increases in alcohol dependence syndrome were associated with subsequent increases in PTSS. Consistent with hypothesis, the strength of lagged associations during the follow-up period from PTSS t-1 → Alcohol dependence syndromet → PTSSt+1 was stronger for individuals with higher affect lability at baseline, suggesting that affect lability was a vulnerability factor. Behavioral disinhibition exhibited similar characteristics, increasing associations between conduct related problems and PTSS. Finally, lability acted to increase the strength of autocorrelation of dependence syndrome symptoms across time, consistent with a pattern of regulatory deficits contributing to elevated levels of alcohol dependence syndrome. Overall, there was little systematic change during the follow-up period but considerable variability in growth trajectories consistent with the variability in initial status in the sample.
Alcohol dependence syndrome
PTSS was moderately correlated with alcohol dependence syndrome at the within-persons level and strongly correlated with alcohol dependence syndrome at the between-persons level. Notably, these associations were considerably stronger than observed correlations between PTSS and alcohol consumption. Results of the multivariate model showed that day-to-day deviations from veterans’ expected level of posttraumatic stress symptoms predicted increases in alcohol dependence syndrome symptoms the next day. This was a robust association after controlling for autoregressive effects of dependence syndrome, the individual’s temporal trend of symptoms over time, concurrent drinking level, and day of the week indicators. This was consistent with previous research with veterans showing within-person associations between daytime PTSS and subsequent nighttime alcohol-related problems (Gaher et al., 2014). We extended this finding in several ways including a larger sample, longer sampling period, differentiating alcohol dependence syndrome from correlated conduct problems, and advances in the statistical model to address autocorrelation factors. Auto- correlation/regression refers to the association of a variable with itself across successive time periods. For example, the dependence syndrome analysis regressed the dependence syndrome score each day on the person’s dependence syndrome score the previous day or, more precisely, the previous day’s residual score (i.e., deviations from the person’s expected value). In a sense, we modeled the popular maxim “the best predictor of future behavior is past behavior.”
In addition, findings showed evidence of a bi-directional association consistent with a mutual maintenance model (Kaysen et al., 2011; Read et al., 2013). However, mutual maintenance models frequently construe the PTSS → AUD association as reflecting self-medication and previous experience sampling studies have not shown positive effects of alcohol consumption on subsequent symptoms (Possemato et al., 2015; Simpson et al., 2014). Though our results are not inconsistent with a self-medication interpretation, several aspects suggest that the observed pattern reflects broad deficits in regulation of behavior and affect resulting in a pattern of alcohol consumption that was dyscontrolled rather than a traditional stress-coping type pattern (cf. Gaher et al., 2014; Read et al., 2014). This was illustrated by the effect of PTSS after controlling for number of drinks, larger bivariate associations between PTSS and both dependence syndrome and conduct problems relative to alcohol consumption, the association of PTSS symptoms with next day alcohol dependence syndrome, and the observed associations with conduct problems that are assessed independent of drinking.
Consistent with hypothesis, affect lability was a vulnerability factor. Participants with more labile affect at baseline exhibited stronger within-person associations between drinking and dependence syndrome symptoms, stronger autocorrelation of dependence symptoms across time, and stronger lagged associations between dependence syndrome symptoms and PTSS. Volatile, high intensity affect can reduce deliberative processing and when paired over time with alcohol, contribute to strong, relatively automatic, response biases characteristic of dependence syndrome (Lieberman, 2007; McCarthy et al., 2010; Wiers et al., 2007). Higher autocorrelation may reflect underregulation (Hamaker & Grasman, 2015), that is, deficits in the individual’s ability to maintain homeostasis because momentary deviations from the individual’s expected value are exhibiting prolonged and stronger effects on subsequent behavior or feeling states (i.e., the individual has not been effective in restoring baseline). In this regard, autoregressive effects of dependence syndrome symptoms reflect the impaired regulation of alcohol characteristic of alcohol use disorder. Though speculative, the autoregressive parameter may be conceptualized to reflect the latent disorder itself when symptoms are assessed in a time-series rather than as static indicators of the presence of psychopathology as a person-level disorder or trait. In this regard, the autoregressive parameter may quantify the behavioral manifestation of the neuroadaptation underlying addiction (Koob & Volkow, 2010, 2016; Volkow, Koob, & McLellan, 2016). The extended amygdala is posited to be central to the neurocircuitry underlying the withdrawal/negative affect stage of substance use disorder and the hippocampus, insula, and basolateral amygdala are posited to be underlie the preoccupation/anticipation stage (Koob & Volkow, 2010, 2016; Volkow et al., 2016). These neural structures are fundamental to emotional regulation and functional differences are linked to lability, trauma exposure, and PTSD (Bruce et al., 2012; Forster, Simons, & Baugh, 2017; Silvers et al., 2016; Simons, Simons, et al., 2016).
Lability was associated with not just higher mean levels of symptoms but stronger autocorrelation of symptoms across time, highlighting its relevance to pathogenesis. In contrast, and consistent with expectation, disinhibition did not potentiate within–person predictors of dependence syndrome symptoms and lability did not potentiate within-person predictors of conduct problems. However, lability and disinhibition each exhibited independent associations with higher levels of dependence syndrome symptoms as well as conduct problems over the follow-up period. This pattern differed from baseline analyses with this sample, which demonstrated specific associations of lability with dependence syndrome symptoms and disinhibition with conduct problems (Simons et al., 2017). Hence, there was inconsistent support for the hypothesized differentiation of lability and disinhibition effects on dependence syndrome and conduct problems, respectively. Addiction has been termed a reward deficit and stress surfeit disorder (Koob, 2013) and neural circuitry involves both structures associated with emotional regulation (e.g., amygdala) as well as inhibitory control (e.g., prefrontal cortex; Koob & Volkow, 2010; Koob & Volkow, 2016) and the joint effects of lability and disinhibition on AUD symptoms are consistent with this.
Conduct problems
PTSS exhibited moderate to strong correlations with conduct problems at both the within- and between- persons level. Furthermore, results of the multivariate model showed that acute exacerbations of PTSS predicted increases in conduct problems the next day. Conduct problems, such as interpersonal conflict, were assessed independent of drinking and hence these were not alcohol-related problems per se though they exhibit expected within-person covariation with drinking. Symptoms of PTSD include a wide range of intense negative emotional states, verbal and physical aggression, and reckless behavior (American Psychiatric Association, 2013). Hence, conduct problems such as assault may, to some extent, be construed as isomorphic with the presenting symptoms of the disorder. Here we showed a prospective association of PTSS with conduct problems the following day. This pattern may reflect temporal variation in the ability to regulate behavior (Jones et al., 2013; Tomko et al., 2015). Intense emotion may undermine effective behavioral control (Lieberman, 2007). Alternatively, resource models suggest that efforts to manage behavior or symptoms may result in depletion of resources for effective subsequent regulation (Baumeister, Schmeichel, Vohs, Kruglanski, & Higgins, 2007; Simons, Wills, et al., 2016). Although both disinhibition and lability were associated with greater conduct problems over the follow-up period, neither moderated within-person predictors of conduct problems. Interestingly, for those characterized by high disinhibition, there was evidence of conduct problems predicting exacerbation of PTSS the following day. This pattern may bare similarity to stress-generation models of depression whereby symptoms predict dependent (i.e., influenced by individual characteristics) interpersonal stress which in turn increase subsequent symptoms (Liu & Alloy, 2010). Indeed, recent research demonstrates prospective effects of PTSD symptoms on subsequent dependent life stress in veterans that are consistent with a stress-generation model (Maniates, Stoop, Miller, Halberstadt, & Wolf, 2018). However, on average, dependence syndrome, but not conduct problems, predicted subsequent PTSS symptoms. Although behavioral problems associated with drinking are part of the current conceptualization of AUD, these results indicated that alcohol-related impairments, relative to general conduct problems, may have a more causal role in the course of PTSD.
Clinical implications
We focus on four primary clinical implications. First, perhaps the most basic implication stems from the observed reciprocal associations between PTSD and AUD symptoms at the daily level. Integrated treatment for these presenting problems is likely essential for optimal treatment response. Second, the lagged effects of PTSD on AUD symptoms, the vulnerability effects of lability, and the centrality of heightened negative affectivity in fostering the response biases observed in AUD (Volkow et al., 2016) indicate that novel substance use treatment approaches that focus on affect regulation (e.g., Stasiewicz et al., 2013) may be a promising approach for veterans with comorbid PTSD and AUD. Third, these results, both in respect to AUD and associated conduct problems emphasize the role of impairments in basic regulatory control. Hence, interventions that aim to enhance the incentive value, or availability, of alternative sources of reinforcement (Volkow et al., 2016), or decrease the response biases toward alcohol (Manning et al., 2016; Wiers et al., 2015) or trauma stimuli (Coffey et al., 2016) through exposure or conditioning may be vital. Finally, in additional to affect dysregulation, deficits in executive control are implicated and hence improving executive functioning and decision making may an important treatment goal (Valls-Serrano, Caracuel, & Verdejo-Garcia, 2016; Volkow et al., 2016).
Strengths and Limitations
This study has a number of notable strengths including the intensive experience sampling protocol, the relatively large N for this type of protocol, and the burst design, which results in the longest experience sampling study of veterans to date. The Bay Pines VA Healthcare System is one of the busiest VA healthcare systems in the country and provides specialized residential mental health programs (U.S. Department of Veteran Affairs, 2018). The higher levels of PTSS symptoms reported by participants at the FL site is consistent with this and supports the criterion validity of the sampling protocol. In addition, the statistical analyses were a sophisticated and novel approach to addressing the challenges posed by these data. That is, modeling the longer-term trend while accounting for within-person dynamic effects from multiple variables has not been examined with measurement burst designs (see Curran & Bauer, 2011 for similar modeling with panel data). This simultaneous modeling is important to not bias the trend effects or the dynamic effects (see Kwok, West, & Green, 2007). Additionally, the use of lagged residuals as opposed to lagged observed scores enables the study of the average within-person time-dependent effects (see Hamaker, Kuiper, & Grasman, 2015). That is, estimates from lagged observed scores combine between-person differences with within-person effects. Allowing for these lagged effects to be random extends previous work and allows for individual-level within-person lagged effects. Furthermore, the modeling approach accounted for the non-normality present in many of the variables using the negative binomial distribution. Although the study design and analysis had many strengths, the study is not without limitations. Women were slightly overrepresented relative to the proportion of OIF/OEF/OND veterans nationally (11.6%; Department of Veterans Affairs, 2017). Nonetheless, the sample was predominantly men and hence the pattern of results may not optimally reflect the experience of women veterans. Neither PTSD nor AUD were required for participation and hence the sample exhibited a broad range of functioning at baseline. Such variation makes these analyses less amenable to examine systematic change over time in respect to improvement or worsening of symptoms in the sample as a whole. Finally, although the analytic models address temporal relationships, they do not provide a basis for causal inference.
Acknowledgments
Research was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Number R01AA020519. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Department of Veterans Affairs, or the United States Government. This research was supported with resources and the use of facilities at the Sioux Falls VA Health Care System, Bay Pines VA Health Care System, and the University of South Dakota.
Footnotes
The inclusion of the quadratic growth term was recommended by a reviewer. Although the fixed effects for the quadratic growth parameter were not significant in the models, the inclusion of this term and its random variance component resulted in better fit to the data and hence it was included.
The quality of experience sampling data is dependent upon the representativeness of the sampled behavior. This is a function of the time course of the behavior, the sampling frame and frequency, and response rates (Csikszentmihalyi & Larson, 1987; Stone & Shiffman, 1994). Poor compliance with the sampling protocol increase the likelihood that the sampled behavior is not representative of the person (Stone & Shiffman, 2002). Similarly, high rates of missing data (e.g., attrition) threaten validity due to selection biases. We chose the cut off of 33% to balance these issues, reducing the inclusion of non-representative bursts while striving to minimize attrition. Though 33% is somewhat arbitrary, we have used this previously with good success (Simons, Wills, et al., 2016). Of these 250, combining both missing/excluded days and missed prompts within a day results in a compliance rate of approximately 65% (250 persons * 70 days * 8 prompts = 140,000 expected random prompts; 91,442 (completed prompts) / 140000 = .65.
Contributor Information
Jeffrey S. Simons, The University of South Dakota, Sioux Falls VA Health Care System
Raluca M. Simons, The University of South Dakota, Sioux Falls VA Health Care System
Jessica A. Keith, Bay Pines VA Health Care System
Kevin J. Grimm, Arizona State University
Scott F. Stoltenberg, The University of Nebraska – Lincoln
Carol O’Brien, Bay Pines VA Health Care System.
Kate Andal, Sioux Falls VA Health Care System.
References
- Aas M, Henry C, Bellivier F, Lajnef M, Gard S, Kahn JP, … Etain B (2017). Affective lability mediates the association between childhood trauma and suicide attempts, mixed episodes and co-morbid anxiety disorders in bipolar disorders. Psychological Medicine, 47, 902–912. 10.1017/S0033291716003081 [DOI] [PubMed] [Google Scholar]
- Aas M, Pedersen G, Henry C, Bjella T, Bellivier F, Leboyer M, … Etain B (2015). Psychometric properties of the Affective Lability Scale (54 and 18-item version) in patients with bipolar disorder, first-degree relatives, and healthy controls. Journal of Affective Disorders, 172, 375–380. 10.1016/j.jad.2014.10.028 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Anker JJ, Forbes MK, Almquist ZW, Menk JS, Thuras P, Unruh AS, & Kushner MG (2017). A network approach to modeling comorbid internalizing and alcohol use disorders. Journal of Abnormal Psychology, 126, 325–339. 10.1037/abn0000257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armour C, Fried EI, Deserno MK, Tsai J, & Pietrzak RH (2017). A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in U.S. military veterans. Journal of Anxiety Disorders, 45, 49–59. 10.1016/j.janxdis.2016.11.008 [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). The alcohol use disorders identification test (AUDIT): Guidelines for use in primary care. World Health Organization, Department of Mental Health and Substance Abuse
- Baumeister RF, Schmeichel BJ, Vohs KD, Kruglanski AW, & Higgins ET (2007). Self-regulation and the executive function: The self as controlling agent Social psychology: Handbook of basic principles (2nd ed.) (pp. 516–539). New York, NY US: Guilford Press. [Google Scholar]
- Belcher AM, Volkow ND, Moeller FG, & Ferré S (2014). Personality Traits and Vulnerability or Resilience to Substance Use Disorders. Trends Cogn Sci, 18, 211–217. 10.1016/j.tics.2014.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 669–673. [DOI] [PubMed] [Google Scholar]
- Bohn MJ, Babor TF, & Kranzler HR (1995). The Alcohol Use Disorders Screening Test (AUDIT): Validation of a screening instrument for use in medical settings. Journal of Studies on Alcohol, 56, 423–432. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Buchholz KR, Brown WJ, Yan L, Durbin A, & Sheline YI (2012). Altered emotional interference processing in the amygdala and insula in women with Post-Traumatic Stress Disorder. Neuroimage Clin, 2, 43–49. 10.1016/j.nicl.2012.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Johnson SL, & Timpano KR (2017). Toward a Functional View of the P Factor in Psychopathology. Clin Psychol Sci, 5, 880–889. 10.1177/2167702617710037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SF, Saladin M, Drobes DJ, Brady KT, Dansky BS, & Kilpatrick DG (2002). Trauma and substance cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug and Alcohol Dependence, 65, 115–127. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Schumacher JA, Brady KT, & Cotton BD (2007). Changes in PTSD symptomatology during acute and protracted alcohol and cocaine abstinence. Drug and Alcohol Dependence, 87, 241–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SF, Schumacher JA, Nosen E, Littlefield AK, Henslee AM, Lappen A, & Stasiewicz PR (2016). Trauma-focused exposure therapy for chronic posttraumatic stress disorder in alcohol and drug dependent patients: A randomized controlled trial. Psychology of Addictive Behaviors, 30, 778–790. 10.1037/adb0000201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SF, Schumacher JA, Stasiewicz PR, Henslee AM, Baillie LE, & Landy N (2010). Craving and Physiological Reactivity to Trauma and Alcohol Cues in PTSD and Alcohol Dependence. Experimental and Clinical Psychopharmacology, 18, 340–349. 10.1037/a0019790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn A, Hagman BT, Moore K, Mitchell J, & Ehlke S (2014). Does negative affect mediate the relationship between daily PTSD symptoms and daily alcohol involvement in female rape victims? Evidence from 14 days of interactive voice response assessment. Psychology of Addictive Behaviors, 28, 114–126. 10.1037/a0035725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML (2010). Toward a person x situation model of sexual risk-taking behaviors: illuminating the conditional effects of traits across sexual situations and relationship contexts. Journal of Personality and Social Psychology, 98, 319–341. 10.1037/a0017785 [DOI] [PubMed] [Google Scholar]
- Csikszentmihalyi M, & Larson R (1987). Validity and reliability of the Experience-Sampling Method. Journal of Nervous and Mental Disease, 175, 526–536. 10.1097/00005053-198709000-00004 [DOI] [PubMed] [Google Scholar]
- Curran PJ, & Bauer DJ (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual Review of Psychology, 62, 583–619. 10.1146/annurev.psych.093008.100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMarce JM, Lash SJ, Parker JD, Burke RS, & Grambow SC (2013). Validity of the Structured Clinical Interview for DSM-IV Among Veterans Seeking Treatment for Substance Use Disorders. International Journal Of Mental Health And Addiction, 11, 546–556. 10.1007/s11469-013-9435-4 [Google Scholar]
- Department of Veterans Affairs. (2017). Women Veterans Health Care Retrieved from https://www.womenshealth.va.gov/WOMENSHEALTH/latestinformation/facts.asp. [Google Scholar]
- Dir AL, Karyadi K, & Cyders MA (2013). The uniqueness of negative urgency as a common risk factor for self-harm behaviors, alcohol consumption, and eating problems. Addictive Behaviors, 38, 2158–2162. 10.1016/j.addbeh.2013.01.025 [DOI] [PubMed] [Google Scholar]
- Donovan DM, Kivlahan DR, Doyle SR, Longabaugh R, & Greenfield SF (2006). Concurrent validity of the Alcohol Use Disorders Identification Test (AUDIT) and AUDIT zones in defining levels of severity among out-patients with alcohol dependence in the COMBINE study. Addiction, 101, 1696–1704. [DOI] [PubMed] [Google Scholar]
- Emery NN, & Simons JS (2017). A reinforcement sensitivity model of affective and behavioral dysregulation in marijuana use and associated problems. Experimental and Clinical Psychopharmacology, 25, 281–294. 10.1037/pha0000131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, & Tofighi D (2007). Centering predictor variables in cross-sectional multilevel models: a new look at an old issue. Psychological Methods, 12, 121. [DOI] [PubMed] [Google Scholar]
- Eysenck SB, Pearson PR, Easting G, & Allsopp JF (1985). Age norms for impulsiveness, venturesomeness and empathy in adults. Personality and Individual Differences, 6, 613–619. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (January, 2010). Structured Clinical Interview of DSM-IV-TR Axis I Disorders Research Version, Patient Edition With Psychotic Screen (SCID-I/P W/ PSY SCREEN) New York: New York State Psychiatric Institute. [Google Scholar]
- Forster GL, Simons RM, & Baugh LA (2017). Revisiting the Role of the Amygdala in Posttraumatic Stress Disorder. In Ferry B (Ed.), The Amygdala-Where Emotions Shape Perception, Learning and Memories: InTech. [Google Scholar]
- Gaher RM, Simons JS, Hahn AM, Hofman NL, Hansen J, & Buchkoski J (2014). An experience sampling study of PTSD and alcohol-related problems. Psychology of Addictive Behaviors, 28, 1013–1025. 10.1037/a0037257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glantz MD, Weinberg NZ, Miner LL, & Colliver JD (1999). The etiology of drug abuse: Mapping the paths. In Glantz MD & Hartel CR (Eds.), Drug abuse: Origins & interventions (pp. 3 – 45). Washington, DC: American Psychological Association. [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, & et al. (2015). Epidemiology of dsm-5 alcohol use disorder: Results from the national epidemiologic survey on alcohol and related conditions iii. JAMA Psychiatry, 72, 757–766. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn AM, Simons RM, & Simons JS (2016). Childhood Maltreatment and Sexual Risk Taking: The Mediating Role of Alexithymia. Archives of Sexual Behavior, 45, 53–62. 10.1007/s10508-015-0591-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller M, & Chassin L (2014). Risk pathways among traumatic stress, posttraumatic stress disorder symptoms, and alcohol and drug problems: a test of four hypotheses. Psychology of Addictive Behaviors, 28, 841–851. 10.1037/a0035878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamaker EL, & Grasman RP (2015). To center or not to center? Investigating inertia with a multilevel autoregressive model. Frontiers in psychology, 5, 1–15. 10.3389/fpsyg.2014.01492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamaker EL, Kuiper RM, & Grasman RPPP (2015). A critique of the cross-lagged panel model. Psychological Methods, 20, 102–116. 10.1037/a0038889 [DOI] [PubMed] [Google Scholar]
- Henry C, Van den Bulke D, Bellivier F, Roy I, Swendsen J, M’Baïlara K, … Leboyer M (2008). Affective lability and affect intensity as core dimensions of bipolar disorders during euthymic period. Psychiatry Research, 159, 1–6. [DOI] [PubMed] [Google Scholar]
- Hruska B, Pacella ML, George RL, & Delahanty DL (2017). The association between daily PTSD symptom severity and alcohol-related outcomes in recent traumatic injury victims. Psychology of Addictive Behaviors, 31, 326–335. 10.1037/adb0000262 [DOI] [PubMed] [Google Scholar]
- Jahng S, Solhan MB, Tomko RL, Wood PK, Piasecki TM, & Trull TJ (2011). Affect and alcohol use: an ecological momentary assessment study of outpatients with borderline personality disorder. Journal of Abnormal Psychology, 120, 572–584. 10.1037/a0024686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A, Christiansen P, Nederkoorn C, Houben K, & Field M (2013). Fluctuating disinhibition: implications for the understanding and treatment of alcohol and other substance use disorders. Front Psychiatry, 4, 140 10.3389/fpsyt.2013.00140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Atkins DC, Moore SA, Lindgren KP, Dillworth T, & Simpson T (2011). Alcohol Use, Problems, and the Course of Posttraumatic Stress Disorder: A Prospective Study of Female Crime Victims. J Dual Diagn, 7, 262–279. 10.1080/15504263.2011.620449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Atkins DC, Simpson TL, Stappenbeck CA, Blayney JA, Lee CM, & Larimer ME (2014). Proximal relationships between PTSD symptoms and drinking among female college students: Results from a daily monitoring study. Psychology of Addictive Behaviors, 28, 62–73. 10.1037/a0033588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, & Williams CL (1982). Assessing the cognitive and behavioral components of children’s self-management. In Karoly P & Kanfer FH (Eds.), Self-management and behavior change (pp. 240 – 284). New York: Pergamon Press. [Google Scholar]
- Koob GF (2013). Addiction is a Reward Deficit and Stress Surfeit Disorder. Front Psychiatry, 4, 72 10.3389/fpsyt.2013.00072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, & Volkow ND (2010). Neurocircuitry of addiction. Neuropsychopharmacology, 35, 217–238. 10.1038/npp.2009.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, & Volkow ND (2016). Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry, 3, 760–773. 10.1016/S2215-0366(16)00104-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, … Zimmerman M (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454–477. doi: 10.1037/abn000025810.1037/abn000025810.1037/abn0000258.supp10.1037/abn0000258.supp (Supplemental) [DOI] [PubMed] [Google Scholar]
- Kramer M, Polusny M, Arbisi P, & F Krueger R (2014). Comorbidity of PTSD and SUDs: Toward an etiologic understanding
- Kwok O. m., West SG, & Green SB (2007). The impact of misspecifying the within-subject covariance structure in multiwave longitudinal multilevel models: A Monte Carlo study. Multivariate Behavioral Research, 42, 557–592. [Google Scholar]
- Lagerberg TV, Aminoff SR, Aas M, Bjella T, Henry C, Leboyer M, … Melle I (2017). Alcohol use disorders are associated with increased affective lability in bipolar disorder. Journal of Affective Disorders, 208, 316–324. 10.1016/j.jad.2016.09.062 [DOI] [PubMed] [Google Scholar]
- Leone RM, Crane CA, Parrott DJ, & Eckhardt CI (2016). Problematic drinking, impulsivity, and physical IPV perpetration: A dyadic analysis. Psychology of Addictive Behaviors, 30, 356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman MD (2007). Social cognitive neuroscience: a review of core processes. Annual Review of Psychology, 58, 259–289. 10.1146/annurev.psych.58.110405.085654 [DOI] [PubMed] [Google Scholar]
- Liu RT, & Alloy LB (2010). Stress generation in depression: A systematic review of the empirical literature and recommendations for future study. Clinical Psychology Review, 30, 582–593. 10.1016/j.cpr.2010.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobbestael J, Leurgans M, & Arntz A (2011). Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II). Clin Psychol Psychother, 18, 75–79. 10.1002/cpp.693 [DOI] [PubMed] [Google Scholar]
- Maniates H, Stoop TB, Miller MW, Halberstadt L, & Wolf EJ (2018). Stress-Generative Effects of Posttraumatic Stress Disorder: Transactional Associations Between Posttraumatic Stress Disorder and Stressful Life Events in a Longitudinal Sample. Journal of Traumatic Stress, 31, 191–201. 10.1002/jts.22269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning V, Staiger PK, Hall K, Garfield JB, Flaks G, Leung D, … Verdejo-Garcia A (2016). Cognitive Bias Modification Training During Inpatient Alcohol Detoxification Reduces Early Relapse: A Randomized Controlled Trial. Alcoholism, Clinical and Experimental Research, 40, 2011–2019. 10.1111/acer.13163 [DOI] [PubMed] [Google Scholar]
- Marwaha S, Gordon-Smith K, Broome M, Briley PM, Perry A, Forty L, … Jones L (2016). Affective instability, childhood trauma and major affective disorders. Journal of Affective Disorders, 190, 764–771. 10.1016/j.jad.2015.11.024 [DOI] [PubMed] [Google Scholar]
- McCarthy DE, Curtin JJ, Piper ME, & Baker TB (2010). Negative reinforcement: Possible clinical implications of an integrative model. In Kassel JD (Ed.), Substance abuse and emotion (pp. 15–42). Washington, DC US: American Psychological Association. [Google Scholar]
- Miller MW, Vogt DS, Mozley SL, Kaloupek DG, & Keane TM (2006). PTSD and substance-related problems: the mediating roles of disconstraint and negative emotionality. Journal of Abnormal Psychology, 115, 369–379. [DOI] [PubMed] [Google Scholar]
- Mohr CD, Arpin S, & McCabe CT (2015). Daily affect variability and context‐specific alcohol consumption. Drug and Alcohol Review, 34, 581–587. [DOI] [PubMed] [Google Scholar]
- Neal DJ, & Carey KB (2007). Examining the association between alcohol intoxication and alcohol-related problems: An event-level analysis. Psychology of Addictive Behaviors, 21, 194–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickerson A, Barnes JB, Creamer M, Forbes D, McFarlane AC, O’Donnell M, … Bryant RA (2014). The temporal relationship between posttraumatic stress disorder and problem alcohol use following traumatic injury. Journal of Abnormal Psychology, 123, 821–834. 10.1037/a0037920 [DOI] [PubMed] [Google Scholar]
- Oliver MNI, & Simons JS (2004). The Affective Lability Scales: Development of a Short-form Measure. Personality and Individual Differences, 37, 1279–1288. 10.1016/j.paid.2003.12.013 [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I Comorbidity of Full and Partial Posttraumatic Stress Disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25, 456–465. 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Possemato K, Maisto SA, Wade M, Barrie K, McKenzie S, Lantinga LJ, & Ouimette P (2015). Ecological momentary assessment of PTSD symptoms and alcohol use in combat veterans. Psychology of Addictive Behaviors, 29, 894–905. 10.1037/adb0000129 [DOI] [PubMed] [Google Scholar]
- Read JP, Merrill JE, Griffin MJ, Bachrach RL, & Khan SN (2014). Posttraumatic stress symptoms and alcohol problems: Self‐medication or trait vulnerability? The American Journal on Addictions, 23, 108–116. 10.1111/j.1521-0391.2013.12075.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Wardell JD, & Colder CR (2013). Reciprocal associations between PTSD symptoms and alcohol involvement in college: A three-year trait-state-error analysis. Journal of Abnormal Psychology, 122, 984–997. 10.1037/a0034918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed PL, Anthony JC, & Breslau N (2007). Incidence of drug problems in young adults exposed to trauma and posttraumatic stress disorder: do early life experiences and predispositions matter? Archives of General Psychiatry, 64, 1435–1442. 10.1001/archpsyc.64.12.1435 [DOI] [PubMed] [Google Scholar]
- Sadava SW (1985). Problem behavior theory and consumption and consequences of alcohol use. Journal of Studies on Alcohol, 46, 392–397. [DOI] [PubMed] [Google Scholar]
- Silvers JA, Hubbard AD, Biggs E, Shu J, Fertuck E, Chaudhury S, … Stanley B (2016). Affective lability and difficulties with regulation are differentially associated with amygdala and prefrontal response in women with Borderline Personality Disorder. Psychiatry Research, 254, 74–82. 10.1016/j.pscychresns.2016.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Batien BD, & Wray TB (2010). Event-level associations between affect, alcohol intoxication, and acute dependence symptoms: Effects of urgency, self-control, and drinking experience. Addictive Behaviors, 35, 1045–1053. 10.1016/j.addbeh.2010.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Gaher RM, Oliver MNI, Bush JA, & Palmer MA (2005). An experience sampling study of associations between affect and alcohol use and problems among college students. Journal of Studies on Alcohol, 66, 459 – 469. [DOI] [PubMed] [Google Scholar]
- Simons JS, & Gropel M (2012). Android Momentary Assessment Tool [Google Scholar]
- Simons JS, Simons RM, Maisto SA, Hahn AM, & Walters KJ (2018). Daily associations between alcohol and sexual behavior in young adults. Experimental and Clinical Psychopharmacology, 26, 36–48. 10.1037/pha0000163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Simons RM, O’Brien C, Stoltenberg SF, Keith JA, & Hudson JA (2017). PTSD, alcohol dependence, and conduct problems: Distinct pathways via lability and disinhibition. Addictive Behaviors, 64, 185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Wills TA, Emery NN, & Marks RM (2015). Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addictive Behaviors, 50, 205–212. 10.1016/j.addbeh.2015.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Wills TA, Emery NN, & Spelman PJ (2016). Keep calm and carry on: Maintaining self-control when intoxicated, upset, or depleted. Cognition and Emotion, 30, 1415–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Wills TA, & Neal DJ (2014). The many faces of affect: A multilevel model of drinking frequency/quantity and alcohol dependence symptoms among young adults. Journal of Abnormal Psychology, 123, 676–694. 10.1037/a0036926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons RM, Simons JS, Olson D, Baugh L, Magnotta V, & Forster G (2016). Posttraumatic Stress and Alcohol Use Among Veterans: Amygdala and Anterior Cingulate Activation to Emotional Cues. Psychology of Addictive Behaviors, 10.1037/adb0000200 [DOI] [PubMed] [Google Scholar]
- Simpson TL, Stappenbeck CA, Luterek JA, Lehavot K, & Kaysen DL (2014). Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology, 123, 237–247. 10.1037/a0035193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SM, Goldstein RB, & Grant BF (2016). The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: Data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Journal of Psychiatric Research, 82, 16–22. 10.1016/j.jpsychires.2016.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijders TAB, & Bosker RJ (1999). Multilevel Analysis: An introduction to basic and advanced multilevel modeling London: Sage Publications. [Google Scholar]
- Stappenbeck CA, Hellmuth JC, Simpson T, & Jakupcak M (2014). The effects of alcohol problems, PTSD, and combat exposure on nonphysical and physical aggression among Iraq and Afghanistan war veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 6, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stasiewicz PR, Bradizza CM, Schlauch RC, Coffey SF, Gulliver SB, Gudleski GD, & Bole CW (2013). Affect regulation training (ART) for alcohol use disorders: development of a novel intervention for negative affect drinkers. Journal of Substance Abuse Treatment, 45, 433–443. 10.1016/j.jsat.2013.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2015). Stata Statistical Software: Release 14 College Station, TX: StataCorp LP. [Google Scholar]
- Steele CM, & Josephs RA (1990). Alcohol myopia: Its prized and dangerous effects. American Psychologist, 45, 921–933. 10.1037/0003-066X.45.8.921 [DOI] [PubMed] [Google Scholar]
- Stone AA, & Shiffman S (1994). Ecological momentary assessment (EMA) in behavorial medicine. Annals of Behavioral Medicine, 16, 199–202. [Google Scholar]
- Stone AA, & Shiffman S (2002). Capturing momentary, self-report data: A proposal for reporting guidelines. Annals of Behavioral Medicine, 24, 236–243. 10.1207/S15324796ABM2403_09 [DOI] [PubMed] [Google Scholar]
- Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, Merikangas KR, … Kessler RC (2010). Mental disorders as risk factors for substance use, abuse and dependence: results from the 10-year follow-up of the National Comorbidity Survey. Addiction, 105, 1117–1128. 10.1111/j.1360-0443.2010.02902.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, … Clark D (2003). Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. American Journal of Psychiatry, 160, 1078–1085. [DOI] [PubMed] [Google Scholar]
- Tomko RL, Lane SP, Pronove LM, Treloar HR, Brown WC, Solhan MB, … Trull TJ (2015). Undifferentiated negative affect and impulsivity in borderline personality and depressive disorders: A momentary perspective. Journal of Abnormal Psychology, 124, 740–753. 10.1037/abn0000064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, & Watson D (2008). Affective instability: measuring a core feature of borderline personality disorder with ecological momentary assessment. Journal of Abnormal Psychology, 117, 647–661. 10.1037/a0012532 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veteran Affairs. (2012). Using the PTSD Checklist (PCL) Retrieved from http://www.ptsd.va.gov/professional/pages/assessments/ptsd-checklist.asp.
- U.S. Department of Veteran Affairs. (2018). Bay Pines VA Healthcare System Retrieved from https://www.baypines.va.gov/BAYPINES/about/index.asp
- Valls-Serrano C, Caracuel A, & Verdejo-Garcia A (2016). Goal Management Training and Mindfulness Meditation improve executive functions and transfer to ecological tasks of daily life in polysubstance users enrolled in therapeutic community treatment. Drug and Alcohol Dependence, 165, 9–14. 10.1016/j.drugalcdep.2016.04.040 [DOI] [PubMed] [Google Scholar]
- Veith AC, Russell TD, & King AR (2017). PID-5 trait mediation of childhood maltreatment effects. Personality and Individual Differences, 104, 58–63. https://doi.org/10.1016/j.paid.2016.07.024 [Google Scholar]
- Volkow ND, Koob GF, & McLellan AT (2016). Neurobiologic Advances from the Brain Disease Model of Addiction. New England Journal of Medicine, 374, 363–371. 10.1056/NEJMra1511480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, & Keane T (1993). The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the International Society of Traumatic Stress Studies, San Antonio, TX http://www.pdhealth.mil/library/downloads/PCL_sychometrics.doc [Google Scholar]
- Weinstein SM, Mermelstein R, Shiffman S, & Flay B (2008). Mood variability and cigarette smoking escalation among adolescents. Psychology of Addictive Behaviors, 22, 504–513. 10.1037/0893-164X.22.4.504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiers CE, Stelzel C, Gladwin TE, Park SQ, Pawelczack S, Gawron CK, … Bermpohl F (2015). Effects of cognitive bias modification training on neural alcohol cue reactivity in alcohol dependence. American Journal of Psychiatry, 172, 335–343. 10.1176/appi.ajp.2014.13111495 [DOI] [PubMed] [Google Scholar]
- Wiers RW, Bartholow BD, van den Wildenberg E, Thush C, Engels RCME, Sher KJ, … Stacy AW (2007). Automatic and controlled processes and the development of addictive behaviors in adolescents: A review and a model. Pharmacology, Biochemistry and Behavior, 86, 263–283. 10.1016/j.pbb.2006.09.021 [DOI] [PubMed] [Google Scholar]
- Wills TA, Pokhrel P, Morehouse E, & Fenster B (2011). Behavioral and emotional regulation and adolescent substance use problems: A test of moderation effects in a dual-process model. Psychology of Addictive Behaviors, 25, 279–292. 10.1037/a0022870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Simons JS, & Gibbons FX (2015). Self-control and substance use prevention: A translational analysis Handbook of adolescent drug use prevention: Research, intervention strategies, and practice (pp. 121–139). Washington, DC, US: American Psychological Association. [Google Scholar]
- Wilson SM, Krenek M, Dennis PA, Yard SS, Browne KC, & Simpson TL (2017). Daily associations between PTSD, drinking, and self-appraised alcohol-related problems. Psychology of Addictive Behaviors, 31, 27–35. 10.1037/adb0000238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SE, Friedman NP, Miyake A, Willcutt EG, Corley RP, Haberstick BC, & Hewitt JK (2009). Behavioral Disinhibition: Liability for Externalizing Spectrum Disorders and Its Genetic and Environmental Relation to Response Inhibition Across Adolescence. Journal of Abnormal Psychology, 118, 117–130. 10.1037/a0014657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, & Frankenburg FR (2001). Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Comprehensive Psychiatry, 42, 369–374. 10.1053/comp.2001.24556 [DOI] [PubMed] [Google Scholar]