Abstract
Objective.
Offspring of anxious parents are at heightened risk for developing anxiety disorders. Preventive interventions for these youths are promising but not universally effective, creating a need to identify outcome predictors. Peer experiences (e.g. peer victimization, social support) are associated with youth anxiety trajectories, but have been relatively unexplored in this context. Thus, this study tested whether peer experiences predicted anxiety-related outcomes in families participating in a randomized-controlled trial of a child anxiety prevention program for families with a clinically anxious parent. Parental anxiety severity was also examined as a moderator of relations between peer experiences and subsequent child anxiety.
Method.
Participants were 121 families (child mean age=8.69, 55.90% girls). Hierarchical logistic and linear regressions were used to test whether baseline peer-related factors predicted increased anxiety symptom severity and anxiety disorder onset over 12 months.
Results.
Youths reporting greater perceived peer victimization at baseline were more likely to develop an anxiety disorder and had more severe anxiety symptoms 12 months later. Lower social support from classmates also predicted increased anxiety severity, but this effect became nonsignificant after accounting for peer victimization. Further, parental anxiety severity moderated the peer victimization-child anxiety severity link: higher child-reported peer victimization predicted increased anxiety in offspring of highly- and moderately-anxious but not low anxious parents.
Conclusions.
Children’s reports of peer victimization appear important for understanding which youth may not respond to preventive interventions in high risk families—especially for children with more severely anxious parents. Implications for the focus of selective anxiety prevention programs are discussed.
Keywords: Anxiety disorders, peer relationships, prevention, parental anxiety
Decades of research suggest that anxiety runs in families. Offspring of anxious parents are nearly four times as likely as those with psychologically healthy parents to have an anxiety disorder themselves (Hirshfeld-Becker, Micco, Simoes, & Henin, 2008). Preventive interventions targeting children with clinically anxious parents can reduce the development of anxiety in offspring (Ginsburg, Drake, Tein, Teetsel, & Riddle, 2015). However, some youths who receive such interventions still develop clinically-significant anxiety. Thus, there is a need to identify factors that increase the likelihood of positive prevention outcomes for these high-risk youth. Theory (e.g., Sullivan, 1953) and research (Hawker & Boulton, 2000) suggest children’s peer experiences might play an important role in such outcomes.
Two well-researched examples of such peer experiences are peer victimization and low social support. Peer victimization, defined as “actions taken by one or more youths with the intention of inflicting physical or psychological injury or pain on another youth” (Vernberg, Jacobs, & Hershberger, 1999, p. 386), is cross-sectionally and prospectively linked with overall internalizing problems, including anxiety, in youth (for meta-analyses, see Hawker & Boulton, 2000; Reijntjes, Kamphuis, Prinzie, & Telch, 2010). In one study, adolescents (N=6,208) reporting frequent peer victimization at age 13 were 2–3 times more likely to develop generalized anxiety disorder, social phobia, specific phobia, agoraphobia, or panic disorder five years later; effects were unattributable to increases in depression (Stapinski et al., 2014). Conversely, close friendships may protect children from internalizing difficulties (Nangle et al., 2003). Low perceived peer support is linked with higher childhood anxiety (Rigby, 2000), whereas higher perceived peer support has protected against anxiety symptoms following negative life events (Moore & Varela, 2010). Overall, high peer victimization and low social support might blunt youths’ opportunities to accumulate “successful” peer interactions, leading to increased anxiety over time.
Offspring of anxious parents may be particularly susceptible to peer-related difficulties. Parents’ role in shaping children’s social competence is well-documented (Parke & Ladd, 1992), and high parental anxiety symptoms are linked to lower social functioning in offspring (Anthony, Anthony, Glanville, & Shaffer, 2005). Research on parent-youth attachment also suggests that children learn expectations about relationships based on early relationships with caregivers, which guide their subsequent peer interactions (Brumariu & Kerns, 2013). Parents with anxiety disorders are more likely than psychologically healthy parents to have insecurely attached offspring (Ollendick & Benoit, 2012), potentially due to their tendency to employ parenting styles linked with elevated child anxiety symptoms (DiBartolo & Helt, 2007). Thus, peer experiences may be important to consider in prevention efforts targeting offspring of anxious parents.
Present Study
This study explored whether children’s baseline perceived peer victimization and social support predicted the onset of anxiety disorders, as well as increased anxiety symptom severity, one year later in youths participating in a randomized-controlled trial evaluating a youth anxiety prevention program targeting families with a clinically anxious parent. Baseline parental anxiety severity was tested as a moderator of relations between baseline peer experiences and child anxiety disorder onset and symptom severity one year later. We predicted that these relations would be strongest in offspring with more, compared to less, severely anxious parents.
Method
Participants.
Participants were 121 volunteer families recruited through print/radio advertisements and mailings to local physicians for an RCT for families with at least one parent meeting criteria for a current anxiety disorder, and at least one child without an anxiety disorder (Ginsburg, Drake, Tein, Teetsel, & Riddle, 2015). The baseline sample included 136 families; we focus on the 121 families who completed the 12-month follow-up assessment. One parent and one child per family were enrolled in the study, although all family members were invited to participate in the program. Families meeting eligibility criteria were randomized to receive the intervention or an Information Monitoring control. This study was conducted in an outpatient research clinic at the Johns Hopkins University. The Johns Hopkins University Institutional Review Board approved all study procedures. Parents and youths provided written informed consent and assent prior to study enrollment.
Youth were 6–13 years old (M(SD)=8.69(1.80); 55.90% girls; 84.60% Caucasian), did not meet criteria for an anxiety disorder, were not receiving anxiety treatment, and had no medical/psychiatric conditions contraindicating study interventions (e.g., suicidality), based on administration of the Anxiety Disorders Interview Schedule for DSM-IV-child and parent versions (ADIS-C/P-IV; Silverman & Albano, 1996). At least one parent per family (ages 27–53, M(SD)=40.79(4.99); 79.80% mothers) met criteria for a current primary anxiety disorder; none had comorbid conditions contraindicating study participation (e.g., substance use disorder) based on ADIS-IV-adult version administration (Brown, DiNardo, & Barlow, 1994). Comorbid parental psychiatric disorders were permitted but had to have lower severity than the anxiety disorder. Most parents presented with primary generalized anxiety (69.12%), panic (12.50%) or social anxiety disorder (11.7%); 7.43% presented with comorbid major depressive disorder. Most parents were married (89%), reported annual incomes of over $80,000 (79.3%), and had graduated from college (84.80%).
All families were expected to complete a battery of questionnaires and interviews at baseline, post-intervention, and 6- and 12-month follow-up points. Attrition at 12-month follow-up was 11.2% (see Ginsburg et al. [2015] for CONSORT diagram). All measures in this study (detailed below) were administered at all study time-points; however, we focused exclusively on baseline data (for measures of peer victimization, social support, and parent anxiety) and 12-month follow-up data (for measures of anxiety severity and disorder onset) for two reasons. First, we were interested in the effects of baseline peer experiences on long-term changes in children’s anxiety outcomes, which carry a specific set of implications for identifying children more or less likely to benefit from a given intervention (e.g., compared to changes in peer experiences during treatment). Post-intervention (8-week), 6-month, and 12-month data were unrelated to this goal. Second, nonresponse rates at 6-month follow-up were especially high (30.88%) compared to 12-month follow-up.
Intervention and control conditions.
The Coping and Promoting Strength program is a family-based intervention including eight 60-minute sessions, plus three optional booster sessions. Families met individually with a therapist trained in the intervention, which includes psychoeducation about anxiety, problem-solving skills, in-vivo desensitization, and contingency management for increasing children’s autonomy. Participants randomized to the control condition received an educational pamphlet discussing anxiety disorders and treatments, intended to mimic usual care (NIH, 2009).
Study measures.
Baseline peer victimization: Youth-Report.
Peer Questions were created by study staff to assess youths’ recent peer victimization experiences. Youths reported whether “you are currently experiencing any of the following:” not being invited to a party/event by peers; teased by peers; ignored by peers; not picked to be on a team by peers; talked about peers behind your back; and laughed at by peers. Affirmative responses were summed to yield a peer victimization score (range=0–6). Exploratory factor analyses based on tetrachoric correlations using maximum likelihood estimation and promax rotation supported a single-factor structure (the first factor explained 60.45% of variance). The Peer Questions were administered during the Child ADIS interviews. Internal consistency at baseline was α=.72.
Baseline social support from peers: Youth-report.
The Classmates and Close Friends subscales (each comprised of 6 items) of the Social Support Scale for Children (SSS-C; Harter, 1985; see Lipski et al., 2014 for further psychometric support) were used to assess perceived peer social support. The “Classmates” items evaluate perceived support from one’s broader peer group (“Some kids have classmates they can become friends with BUT Other kids don’t have classmates they can become friends with”); “Close Friend” items tap perceived support from a specific close friend (“Some kids have a close friend who really understands them BUT Other kids don’t have a close friend who understands them”). Items are scored from 1–4 and averaged within each subscale; higher scores represent higher perceived support. Internal consistency at baseline for the Classmates and Close Friend subscales were α=.67 and α=.78, respectively.
Youth anxiety diagnosis and severity.
The ADIS-C/P-IV (Silverman & Albano, 1996), a semi-structured interview that assesses DSM-IV anxiety disorders in youth ages 6–18, was administered at baseline, post-intervention, and 6- and 12-month follow-ups. Interviews were administered to parents and children by independent evaluators (IEs) unaware of intervention condition. Child- and parent-reports were integrated based on clinical judgment of the IEs and clinical supervisor (a senior child psychiatrist, unaware of intervention condition). Interviewers provided Clinical Severity Ratings (CSRs) for each diagnosis on a 0–8 scale. Anxiety onset was operationalized as whether children met criteria for any DSM-IV anxiety disorder (CSR≥4) at any study assessment point. ADIS-C/P CSRs across all anxiety disorders were summed to index anxiety symptom severity at 12-month follow-up. In this study, inter-rater agreement on a randomly selected 25% of ADIS-C/P administrations was 97% for parents and children.
Baseline parental anxiety symptom severity.
To assess anxious parents’ baseline anxiety symptom severity, we used the State-Trait Anxiety Inventory-Trait (STAI-T; Spielberger, 1983). The STAI-T is a measure of stable anxiety symptoms. The Trait scale includes 20 items rated from 1–4; summed item scores yield a Total Score of stable anxiety symptoms. The STAI-T has shown excellent test-retest reliability (rs=0.73–0.86) and correlates highly with other adult anxiety measures (Speilberger, 1983). Mean STAI-T score was 48.97 in this study: well above the identified cut-point (40) for clinically-significant adult anxiety symptoms (Knight, Waal-Manning, & Spears, 1983). Internal consistency at baseline was α=.92 for the STAI-T.
Analytic plan.
We first conducted hierarchical logistic regressions to test whether peer victimization and social support predicted anxiety disorder onset during the 12-month follow-up period. Covariates were included in step 1 of regressions (family income; child age/gender; intervention condition; pretreatment total anxiety CSR. Given very small numbers of non-Caucasian/non-Hispanic youths, we did not control for youth race/ethnicity).1 Individual peer predictor variables were added in step 2. If multiple hypothesized peer-related predictors emerged, we conducted an additional regression including all significant predictors to examine their relative effects. Second, we used hierarchical linear regressions to test whether peer factors predicted increases in anxiety severity at 12-month follow-up (covariates were entered in step 1; individual peer variables, in step 2). Again, if multiple predictors emerged as significant, we assessed their relative effects through an additional regression including all significant predictors.
Finally, using the PROCESS macro (Hayes, 2013), we tested parental anxiety severity as a moderator of predictive associations. For continuous DVs, PROCESS yields the significance of the change in R2 produced by interactions between independent (youth peer experiences) and moderator variables (parental anxiety severity). For binary DVs, PROCESS produces maximum-likelihood based confidence intervals for this same interaction term. For significant moderation effects, we used the macro to calculate simple slopes for associations between youth peer experiences and anxiety disorder onset/symptom increases for low (−1 SD below the mean), moderate (mean), and high (+1 SD above the mean) parental anxiety levels, using bootstrapping procedures with 2,000 samples.
To address minimal item-level data missing from baseline questionnaires (<1%), we used a sequential regression multivariate imputation algorithm in SPSS Version 23. Ten imputed datasets were generated; however, results based on original and imputed data did not significantly differ. Additionally, due to attrition, anxiety outcome data based on the ADIS-C/P were available for 121 of the originally enrolled families. All analyses include these 121 families.2
Results
Preliminary Analyses.
Table 1 presents descriptive statistics and correlations for all study variables, child gender, and child age. No study variables were significantly associated with child age (based on pearson correlations) or gender (based on point-biserial correlations). No significant differences in peer variables emerged by intervention condition, family income, child gender, or child race/ethnicity. Older children reported higher perceived social support from a close friend than did younger children, t(135)=2.17, p=.03, d=.37. Baseline anxiety severity did not differ across intervention condition on any aforementioned demographic factors.
Table 1.
Means, standard deviations, and bivariate correlations for all peer variables, parental anxiety severity, child baseline anxiety symptom severity, and child age and gender
| Mean (SD) | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
| 1. Peer Questions (Child-report) | 1.41 (1.69) | .45** | −.18* | 11 | −.11 | .05 | .15† |
| 2. Social Support, Classmates (Child-report) | 3.40 (.45) | .49** | −.10 | −.09 | .11 | −.05 | |
| 3. Social Support, Close Friend (Child-report) | 3.58 (.50) | -- | −.04 | .15 | .16 | .00 | |
| 4. Parental anxiety severity (Parent-report) | 48.97 (11.07) | -- | .09 | .07 | .04 | ||
| 5. Child age | 8.69 (1.80) | -- | .03 | .03 | |||
| 6. Child gender+ | N/A | -- | −.13 | ||||
| 7. Baseline anxiety child severity (Total Anxiety Clinical Severity Rating) | 7.90 (4.42) | -- |
Note. p < .10
p < .05
p < .01
Point-biserial correlations were used to assess relations between youth gender and other study variables.
Peer experiences and onset of anxiety disorders.
We first tested whether child-reported peer victimization or social support predicted child anxiety disorder onset one year later (Table 2). Greater perceived peer victimization predicted significantly increased likelihood of children’s developing an anxiety disorder, χ2 (1, N=121) =4.11, p=.043, OR=1.40. For each additional peer victimization experience youths reported at baseline, there was a 40% increase in the odds of anxiety disorder onset over the following year. Neither child-reported social support from close friends nor classmates predicted increased likelihood of anxiety disorder onset.
Table 2.
Results of logistic regressions testing peer experiences as predictors of child anxiety disorder onset over 12 months.
| Step and variable | b | SE | Wald statistic | Odds ratio (95% Confidence Interval) | χ2 | ΔR2 |
|---|---|---|---|---|---|---|
| Step 1 | χ2 (5)=26.20** | .33 | ||||
| Intervention group | −2.93 | .86 | 11.69 | .09 (.02, .40)** | ||
| Annual family income | −39 | .20 | 3.91 | .67 (.45, 1.00) | ||
| Youth age | .10 | .16 | .46 | 1.11 (.82, 1.51) | ||
| Female gender | .83 | .57 | 3.29 | .36 (.12, 1.08) | ||
| Baseline youth anxiety severity | .10 | .07 | 2.26 | 1.10 (.97, 1.26) | ||
| Step 2 | χ2 (1) = 4.11* | .04* | ||||
| Peer Victimization | .34 | .17 | 4.02 | 1.40 (1.01,1.95)* | ||
| Intervention group | −2.99 | .88 | 11.70 | .05 (.01,.28)** | ||
| Annual family income | − 43 | .33 | 3.85 | .65 (40, 1.03)* | ||
| Youth age | .13 | .16 | .69 | 1.14 (.83, 1.57) | ||
| Female gender | −1.01 | .59 | 2.94 | .36 (.11, 1.16) | ||
| Baseline youth anxiety severity | .09 | .07 | 1.72 | 1.09 (.95,1.25) | ||
| Step 1 | χ2 (5)=26.20** | .33 | ||||
| Intervention group | −2.93 | .86 | 11.69 | .09 (.02,.40)** | ||
| Annual family income | −39 | .20 | 3.91 | .67 (.45,1.00) | ||
| Youth age | .10 | .16 | .46 | 1.11 (.82,1.51) | ||
| Female gender | .83 | .57 | 3.29 | .36 (.12, 1.08) | ||
| Baseline youth anxiety severity | .10 | .07 | 2.26 | 1.10 (.97, 1.26) | ||
| Step 2 | χ2 (1) = 1.44 | .01 | ||||
| Social Support – Classmates | −93 | .79 | 1.40 | .39 (.09, 1.84) | ||
| Intervention group | −2.99 | .88 | 11.70 | .05 (.01, .28)** | ||
| Annual family income | −55 | .25 | 4.94 | .57 (40, 1.03)* | ||
| Youth age | .07 | .17 | .16 | 1.07 (.76, 1.52) | ||
| Female gender | −91 | .65 | 1.99 | .40 (.11, 1.43) | ||
| Baseline youth anxiety severity | .13 | .08 | 2.72 | 1.14 (.97, 1.34) | ||
| Step 1 | χ2 (5)=26.20** | .33 | ||||
| Intervention group | −2.93 | .86 | 11.69 | .09 (.02, .40)** | ||
| Annual family income | −.39 | .20 | 3.91 | .67 (.45, 1.00) | ||
| Youth age | .10 | .16 | .46 | 1.11 (.82, 1.51) | ||
| Female gender | .83 | .57 | 3.29 | .36 (.12, 1.08) | ||
| Baseline youth anxiety severity | .10 | .07 | 2.26 | 1.10 (.97, 1.26) | ||
| Step 2 | χ2 (1) = .12 | .00 | ||||
| Social Support – Close Friend | −.22 | .64 | 1.92 | .80 (.23, 2.79) | ||
| Intervention group | −3.05 | .89 | 9.86 | .05 (.01, .27)** | ||
| Annual family income | −57 | .25 | 5.32 | .57 (35, .92)* | ||
| Youth age | .16 | .17 | .88 | 1.17 (.84, 1.64) | ||
| Female gender | −1.01 | .62 | 2.64 | .36 (.11, 1.23) | ||
| Baseline youth anxiety severity | .11 | .07 | 2.30 | 1.12 (.97, 1.30) |
Note.p<.01
p<.05
We then tested parental anxiety severity as a moderator of these relations. The parental anxiety X peer victimization interaction was non-significant for youth anxiety disorder onset, β=−0.02, p=.43, 95% CI [−.05, .02]. Additionally, neither the Social Support-Classmates X Parental Anxiety interaction (β=0.48, p=.06, 95% CI[−.02, .98]) nor the Social Support-Close Friend X Parental Anxiety interaction (β=0.01, p=.93, 95% CI[−.19, .21]) significantly predicted anxiety disorder onset. Thus, no support emerged for parental anxiety severity as a moderator of perceived peer experiences and 12-month anxiety disorder onset.
Peer experiences and increases in anxiety severity.
Greater baseline child-perceived peer victimization experiences were associated with significant increases in child anxiety severity at 12-month follow-up, ΔR2 =.08, F(1, 115)=13.96, p<.001, f2=.09 for peer victimization (see Table 3). Lower baseline youth-reported social support from classmates (but not a close friend) was also associated with increased anxiety severity at 12-month follow-up, ΔR2 =.03, F(1, 115)=5.23, p=.024, f2=.04 for social support from classmates.
Table 3.
Results of individual hierarchical linear regressions testing peer experiences as predictors of increases in youth anxiety severity from baseline to 12-month follow-up.
| Predictor (Step 2 variable) | Dependent variable | Predictor (Step 2 variable) | Dependent variable | Predictor (Step 2 variable) | Dependent variable | |||
|---|---|---|---|---|---|---|---|---|
| 12-month youth anxiety severity | 12-month youth anxiety severity | 12-month youth anxiety severity | ||||||
| b | ΔR2 | b | ΔR2 | b | ΔR2 | |||
| Step 1 | .30** | Step 1 | .30** | Step 1 | .30** | |||
| Intervention group | 2.09** | Intervention group | 2.09** | Intervention group | 2.09** | |||
| Annual family income | −.43 | Annual family income | −.43 | Annual family income | −.43 | |||
| Youth age | −17 | Youth age | −.17 | Youth age | −.17 | |||
| Female gender | 1.35* | Female gender | 1.35* | Female gender | 1.35* | |||
| Baseline youth anxiety severity | .40** | Baseline youth anxiety severity | .40** | Baseline youth anxiety severity | .40** | |||
| b | ΔR2 due to predictor | b | ΔR2 due to predictor | b | ΔR2 due to predictor | |||
| Step 2 | .08** | Step 2 | .03* | Step 2 | .01 | |||
| Peer Victimization | .66** | Social Support – Classmates | −1.62* | Social Support – Close friends | .84 | |||
| Intervention group | 2.67** | Intervention group | 2.91** | Intervention group | 2.91** | |||
| Annual family income | −.41 | Annual family income | −.49 | Annual family income | −.46 | |||
| Youth age | .08 | Youth age | .03 | Youth age | .08 | |||
| Female gender | 1.38* | Female gender | 1.38* | Female gender | 1.42* | |||
| Baseline youth anxiety severity | .37** | Baseline youth anxiety severity | .46** | Baseline youth anxiety severity | .43** | |||
Note. Regression coefficients are unstandardized.
p<.01
p<.05
We conducted another linear regression to assess both significant predictors’ relative effects on increased anxiety severity from baseline to 12-month follow-up. Controlling for covariates (added in step 1), child-reported peer victimization and social support from classmates (both added in step 2) jointly explained 8.00% of variance in child anxiety severity increases at 12-month follow-up, ΔR2=.08, ΔF(3, 111)=7.13, p=.001, f2=.09. However, only child-reported peer victimization emerged as an individually significant predictor, b=.56, t=2.93, p=.004, 95% CI[.18, .95], suggesting a unique small-to-medium effect of baseline child-perceived peer victimization on 12-month anxiety severity increases.
Finally, we tested parental anxiety severity as a moderator of these relations. The Parental Anxiety X Peer Victimization interaction produced a significant R2 change for youth anxiety severity at 12-month follow-up, ΔF(1, 114)=7.61, ΔR2=0.04, p=0.007 (Figure 1). The peer victimization-child anxiety severity link was strongest among children with higher-anxiety parents (β=1.69, t=4.36, p<.001, 95% CI[.92, 2.47]), weaker but significant for children with moderate-anxiety parents (β=1.00, t=3.44, p=.001, 95% CI[0.42, 1.58]), and non-significant for children with lower-anxiety parents (β=0.31, t=−.81, p=.42, 95% CI[−0.45, 1.07]).
Figure 1.
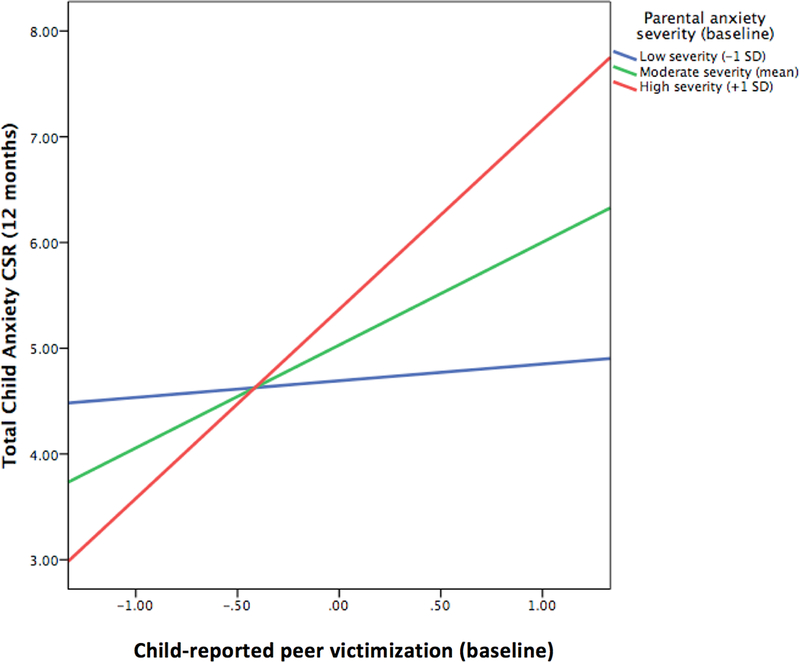
Parental anxiety severty moderates relations between child-reported peer victimization experiences and increased child anxiety symptom severity 12 months later.
Neither the Social Support-Classmates X Parental Anxiety interaction (ΔF(1, 114)=1.32, ΔR2=0.01, p=0.25) nor the Social Support-Close Friend X Parental Anxiety interaction (ΔF(1, 114)=.48, ΔR2=0.00, p=0.49) significantly predicted 12-month child anxiety severity. Thus, parental anxiety severity did not moderate the relation of lower child-perceived social support to increased 12-month anxiety severity.
Discussion
This study examined whether children’s perceived peer victimization and low social support predicted subsequent anxiety symptom severity and disorder onset in children participating in an RCT evaluating a youth anxiety prevention program targeting families with a clinically anxious parent. Higher baseline perceived peer victimization (e.g., being teased, ignored, or laughed at) predicted increased child anxiety symptom severity, and likelihood of anxiety disorder onset, 12 months later. Specifically, each additional baseline peer victimization experience children reported indicated a 40% increase in their odds of developing an anxiety disorder during the follow-up period. Lower social support from classmates (but not a close friend) also predicted increased child anxiety severity. However, when the relative strengths of predictors were assessed, only child-perceived peer victimization predicted increased anxiety symptoms at 12-month follow-up. Finally, parental anxiety severity emerged as a significant moderator: perceived peer victimization predicted increased anxiety in offspring of high- and moderate-anxiety parents, but not among those with lower-anxiety parents.
Extending research identifying peer experiences as important contributors to overall youth anxiety symptoms and disorders (Rigby, 2000), findings suggest that such experiences may impact prevention outcomes for high-risk youth, particularly those with highly anxious parents. Youth anxiety prevention programs seldom target peer-related difficulties, focusing instead on individual coping skills, exposure-based exercises, and family interactions (Fisak, Richard, & Mann, 2011). This study suggests that assessing and addressing negative peer experiences might enhance existing prevention programs’ effects. Previously, group-based social skills programs have demonstrated effectiveness in the treatment of youth social anxiety (Fisher, Masia-Warner, & Klein, 2004). Separately, Interpersonal Psychotherapy-Adolescent Skills Training (a depression prevention program teaching skills linked to understanding and adaptively responding to social challenges) has significantly reduced adolescents’ overall anxiety (independent of positive effects on depression; Young et al, 2012) and social anxiety (La Greca, Ehrenreich-May, Mufson, & Chan, 2016). Given present findings, promoting positive social skills and reduction of relationship difficulties within selective anxiety preventive programs—especially those targeting offspring of anxious parents—may promote similarly positive outcomes.
Additionally, assessing youths’ peer experiences and parental anxiety before prevention program administration might facilitate personalization of interventions. The National Institute of Mental Health has recently supported a shift toward personalized psychological intervention, which combines assessments of individual characteristics with programs tailored around those characteristics to optimize intervention response (Ng & Weisz, 2015). Incorporating knowledge of predictor and moderator variables into clinical decision-making—e.g., peer victimization and parental anxiety severity—may facilitate personalized anxiety prevention for high-risk youth. For example, if a child reports high peer victimization prior to beginning a preventive anxiety intervention and her parent reports moderate-to-severe anxiety, she might benefit from an intervention module designed to improve social/peer-related coping skills. Such a module may be administered alongside or instead of family- or youth-focused strategies, depending on the child’s profile of difficulties.
Some aspects of results warrant further consideration. First, more individual predictors related to increased anxiety severity than to anxiety disorder onset. Similarly, parental anxiety severity moderated changes in child anxiety severity but not disorder onset. This is likely due to the reduced statistical power and precision that accompanies prediction of dichotomous (versus continuous) outcome variables (Streiner, 2002). Indeed, dichotomizing a continuous outcome variable can reduce power to detect effects by the same amount as would discarding one-third of available data (Cohen, 1983). Thus, variables that predicted and moderated changes in anxiety severity only may remain valuable to consider. Second, perceived peer victimization outperformed perceived social support in predicting youth anxiety outcomes. This contrasts with longitudinal research suggesting that both factors uniquely predict increased youth internalizing and overall psychopathology (Bailey, 2009; Rigby, 2000). Notably, in this study, there was less variance in youths’ perceived social support than in perceived peer victimization, which may have rendered the latter factor’s effects more detectable. Regardless, these peer-related experiences are commonly linked (Bailey, 2009), and both may warrant consideration in the context of youth anxiety prevention.
Third, youth-reported perceived social support from classmates, but not a close friend, predicted increased anxiety severity. Youths’ levels of perceived social support in these /domains were near-identical, suggesting substantive differences in their relations to anxiety. This pattern may have resulted because this study’s social support scale assessed support from one close friend. Perhaps one supportive friendship is insufficient to buffer adverse impacts of low perceived support from one’s broader peer group. Alternatively, a child’s closest friend may not attend her school, whereas she sees classmates near-daily. Supportive but intermittent interactions with a close friend may have less impact than day-to-day low support from classmates.
Fourth, female youth gender (a covariate in present analyses) significantly predicted greater 12-month anxiety severity increases. This finding corroborates literature identifying female gender as a risk factor for anxiety across the lifespan (McLean & Anderson, 2009). Although youth gender did not moderate 12-month intervention outcomes (reported in the primary outcomes paper for this intervention: Ginsburg et al., 2015), its predictive role validates the need for increased anxiety prevention efforts targeting girls—particularly those with additional risk factors. Although beyond the scope of this investigation, future work may assess the joint influences of female gender, peer experiences, and parental anxiety on youth anxiety outcomes.
This study has limitations that suggest future research. First, this study could not address all peer-related experiences potentially relevant to youth anxiety prevention outcomes (e.g., physical bullying). Relatedly, we focused on youths’ perceived peer victimization and social support. Future studies may explore how observed peer experiences might shape youth prevention outcomes. Further, psychometric support for the Peer Questions scale—developed for this prevention trail—remains limited; additional research is needed to clarify its psychometric properties and specificity in predicting anxiety outcomes. Second, we focused on the moderating role of parental anxiety severity; additional, presently unexplored forms of parental psychopathology (e.g. depression) may also be helpful to consider. Third, this study focused on baseline peer experiences predicting anxiety prevention outcomes. Results may carry specific implications for personalizing interventions for high-risk youth based on initial, pre-intervention assessments. However, youths’ perceived peer experiences may also change during or following interventions—and these changes might also influence outcomes. Exploring such relations might reveal peer-related mechanisms of youth intervention response. Fourth, low onset rates for specific anxiety disorder types (e.g., only 3 participating children met criteria for social anxiety disorder at any assessment point) precluded our exploring peer experiences as predictors of specific anxiety sub-types. Future work might examine peer-related predictors of anxiety sub-types, particularly social anxiety, given its particularly robust links with more frequent peer victimization (Stapinski et al., 2014). Finally, several factors render present findings’ generalizability unclear. Participating parents might have been less functionally impaired than other clinically-anxious parents (e.g., they had few comorbid diagnoses). Participating youths had no baseline anxiety disorders, incompletely representing high-risk youth samples. Participants were volunteer, largely Caucasian, high-income, dual-parent families—i.e., families motivated for support, and with few socioeconomic stressors linked to anxiety in offspring of anxious parents (Beidel & Turner, 1997). Non-volunteer, lower-resource, and/or single-parent families might experience greater difficulty attending and engaging in sessions. Future trials with socioeconomically diverse samples may assess these possibilities.
Overall, results suggest that baseline perceived peer victimization can shape children’s response to a prevention program targeting offspring with clinically anxious parents, particularly for children with whose parents endorse more severe anxiety symptoms. Findings may inform the focus and design of interventions for high-risk children, potentially enhancing modest effects of existing prevention programs.
Acknowledgments
Funding Information: This study was supported by a grant (R01 MH077312) awarded to Dr. Golda Ginsburg by the National Institute of Mental Health.
Footnotes
ClinicalTrials.gov: NCT00847561
Given high rates of comorbidity between anxiety and depression, it is often useful to include depressive symptoms as a covariate in assessing anxiety-specific outcomes. However, no child participating in this study met diagnostic criteria for major depressive disorder (MDD) at any assessment point over the course of the study, based on the ADIS C/P. Further, children’s mean MDD clinical severity rating (CSR) at baseline was .03 out of 8, and 97.8% of youths’ baseline MDD CSRs were 0. Based on the lack of MDD—or even subclinical MDD (e.g., CSR of 3)—in participating youths, depressive symptoms are extremely unlikely to have confounded results in this present study. Accordingly, we did not control for depression symptom severity (based on MDD CSRs) in analyses.
Raw Total Anxiety CSR values at 12-month follow-up were available for 107 of the 121 youths whose 12-month follow-up data was collected. The original study was conducted within a survival analysis framework. Thus, the last observation carry-forward (LOCF) was used to estimate 12-month CSRs for youths diagnosed with an anxiety disorder throughout the study. Specifically, Total Anxiety CSR values were carried forward from either the post-assessment or 6-month assessment, depending on the point at which children met criteria for an anxiety diagnosis. Results did not differ when using the LOCF-adjusted severity variable (n=121) and unadjusted severity variable (n=107) as outcomes.
References
- Anthony LG, Anthony BJ, Glanville DN, Naiman DQ, Waanders C, & Shaffer S (2005). The relationships between parenting stress, parenting behaviour and preschoolers’ social competence and behaviour problems in the classroom. Infant and Child Development, 14(2), 133–154. 10.1002/icd.385 [DOI] [Google Scholar]
- Bailey LD (2009). Peer victimization and psychosocial outcomes in adolescents: role of social support and disclosure (Unpublished doctoral dissertation). University of Miami, Miami, FL. [Google Scholar]
- Beidel DC, & Turner SM (1997). At risk for anxiety: I. Psychopathology in the offspring of anxious parents. Journal of the American Academy of Child & Adolescent Psychiatry, 36(7), 918–924. 10.1097/00004583-199707000-00013 [DOI] [PubMed] [Google Scholar]
- Brown TA, DiNardo PA, & Barlow DH (1994). Anxiety Disorders Interview Schedule for DSM-IV. New York, Graywind Publications. [Google Scholar]
- Brumariu LE, & Kerns KA (2013). Pathways to anxiety: Contributions of attachment history, temperament, peer competence, and ability to manage intense emotions. Child Psychiatry and Human Development, 44, 504–515. 10.1007/s10578-012-0345-7 [DOI] [PubMed] [Google Scholar]
- Cohen J (1983) The Cost of Dichotomization. Applied Psychological Measurement, 7, 249–253. [Google Scholar]
- Deković M, & Meeus W (1997). Peer relations in adolescence: Effects of parenting and adolescents’ self-concept. Journal of Adolescence, 20(2), 163–176. 10.1006/jado.1996.0074 [DOI] [PubMed] [Google Scholar]
- DiBartolo PM, & Helt M (2007). Theoretical models of affectionate versus affectionless control in anxious families: A critical examination based on observations of parent–child interactions. Clinical Child and Family Psychology Review, 10(3), 253–274. 10.1007/s10567-007-0017-5 [DOI] [PubMed] [Google Scholar]
- Fisak BJ, Richard D, & Mann A (2011). The prevention of child and adolescent anxiety: A meta-analytic review. Prevention Science, 12(3), 255–268. 10.1007/s11121-011-0210-0 [DOI] [PubMed] [Google Scholar]
- Fisher PH, Masia-Warner C, & Klein RG (2004). Skills for social and academic success: A school-based intervention for social anxiety disorder in adolescents. Clinical Child and Family Psychology Review, 7(4), 241–249. 10.1007/s10567-004-6088-7 [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Drake KL, Tein JY, Teetsel R, & Riddle MA (2015). Preventing onset of anxiety disorders in offspring of anxious parents: a randomized controlled trial of a family-based intervention. American Journal of Psychiatry, 172(12), 1207–1214. 10.1176/appi.ajp.2015.14091178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawker DS, & Boulton MJ (2000). Twenty years’ research on peer victimization and psychosocial maladjustment: a meta-analytic review of cross-sectional studies. Journal of Child Psychology and Psychiatry, 41(4), 441–455. 10.1111/1469-7610.00629 [DOI] [PubMed] [Google Scholar]
- Harter S (1985). Manual for the Social Support Scale for Children. University of Denver. [Google Scholar]
- Hirshfeld‐Becker DR, Micco JA, Simoes NA, & Henin A (2008). High-risk studies and developmental antecedents of anxiety disorders. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 148(2), 99–117. 10.1002/ajmg.c.30170 [DOI] [PubMed] [Google Scholar]
- Knight RG, Waal-Manning HJ, & Spears GF (1983). Some norms and reliability data for the Stait-Trait Anxiety Inventory and the Zung Self-Rating Depression Scale. British Journal of Clinical Psychology, 22, 245–249. 10.1111/j.2044-8260.1983.tb00610.x [DOI] [PubMed] [Google Scholar]
- La Greca AM, Ehrenreich-May J, Mufson L, & Chan S (2016). Preventing Adolescent Social Anxiety and Depression and Reducing Peer Victimization: Intervention Development and Open Trial. Child & Youth Care Forum, 45, 905–926. 10.1007/s10566-016-9363-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipski DM, Sifers SK, & Jackson Y (2014). A study of the psychometric properties of the social support scale for children. Journal of Psychopathology and Behavioral Assessment, 36(2), 255–264. 10.1007/s10862-013-9383-0 [DOI] [Google Scholar]
- McLean CP, & Anderson ER (2009). Brave men and timid women? A review of the gender differences in fear and anxiety. Clinical Psychology Review, 29, 496–505. 10.1016/j.cpr.2009.05.003 [DOI] [PubMed] [Google Scholar]
- Moore KW, & Varela RE (2010). Correlates of long-term posttraumatic stress symptoms in children following Hurricane Katrina. Child Psychiatry & Human Development, 41, 239–250. 10.1007/s10578-009-0165-6 [DOI] [PubMed] [Google Scholar]
- Nangle DW, Erdley CA, Newman JE, Mason CA, & Carpenter EM (2003). Popularity, friendship quantity, and friendship quality: Interactive influences on children’s loneliness and depression. Journal of Clinical Child and Adolescent Psychology, 32, 546–555. 10.1207/S15374424JCCP3204_7 [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health: Anxiety Disorders (brochure). Bethesda, MD, National Institutes of Health, 2009. [Google Scholar]
- Ng MY, & Weisz JR (in press). Building a science of personalized intervention for youth mental health. Journal of Child Psychology and Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollendick TH, & Benoit KE (2012). A parent–child interactional model of social anxiety disorder in youth. Clinical Child and Family Psychology Review,15(1), 81–91. 10.1007/s10567-011-0108-1 [DOI] [PubMed] [Google Scholar]
- Parke RD, & Ladd GW (1992). Family-peer relationships: Modes of linkage. Psychology Press. [Google Scholar]
- Reijntjes A, Kamphuis JH, Prinzie P, & Telch MJ (2010). Peer victimization and internalizing problems in children: A meta-analysis of longitudinal studies. Child Abuse and Neglect, 34, 244–252. 10.1016/j.chiabu.2009.07.009 [DOI] [PubMed] [Google Scholar]
- Rigby KEN (2000). Effects of peer victimization in schools and perceived social support on adolescent well-being. Journal of Adolescence, 23, 57–68. 10.1006/jado.1999.0289 [DOI] [PubMed] [Google Scholar]
- Silverman WK & Albano AM (1996). The Anxiety Disorders Interview Schedule for Children for DSM-IV: (Child and Parent Versions). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Stapinski LA, Bowes L, Wolke D, Pearson RM, Mahedy L, Button KS…Araya R (2014). Peer victimization during adolescence and risk for anxiety disorders in adulthood: A prospective cohort study. Depression and Anxiety, 31, 574–582. 10.1002/da.22270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streiner DL (2002). Breaking up is hard to do: the heartbreak of dichotomizing continuous data. Canadian Journal of Psychiatry, 47, 262–266. [DOI] [PubMed] [Google Scholar]
- Sullivan HS (1953). The interpersonal theory of psychiatry. New York: Norton. [Google Scholar]
- Vernberg EM, Jacobs AK, & Hershberger SL (1999). Peer victimization and attitudes about violence during early adolescence. Journal of Clinical Child Psychology, 28, 386–395 [DOI] [PubMed] [Google Scholar]
- Young JF, Makover HB, Cohen JR, Mufson L, Gallop RJ, & Benas JS (2012). Interpersonal psychotherapy-adolescent skills training: Anxiety outcomes and impact of comorbidity.Journal of Clinical Child & Adolescent Psychology, 41, 640–653. 10.1080/15374416.2012.704843 [DOI] [PMC free article] [PubMed] [Google Scholar]


