To the Editor,
We read with interest the review by Orso et al. [1].
The review focused on the use of transthoracic ultrasound (TUS) in the diagnosis of pneumonia in children and conclusions are made that more studies with a thorough methodology are needed. We agree that the use of TUS in the pediatric population is harmless, easy and low cost, but would like to emphasize that thoracic imaging studies rely primarily on computed tomography (CT) and chest X-ray (CXR), and TUS should be used for monitoring or guiding invasive procedures. The use of TUS depends both on the resolution of the image and the operator [2]. Also, according to the Health Technology Assessment, any imaging technique needs to be validated by the gold standard technique [3]. Hence, CXR study is usually required to detect comorbidities involving the diaphragm, the heart, the mediastinum, the aortic arch, the esophagus, the trachea and the inner lesions without adhesion to the explorable pleural surface (including those having adherence to that part of the pleura behind the scapula and in the mediastinum). Owing to the presence of the thoracic cage, TUS can explore about 70% of the pleural surface, and other limitations and pitfalls may occur, at least in adults, in this area [4]. The use of TUS as complementary to CXR is, therefore, warranted in children, as in adult pneumonia. Additionally, several studies did not report, also for ethical reasons, any data on the comparison between CT, namely the gold standard for diagnosis of pulmonary disorders, and TUS.
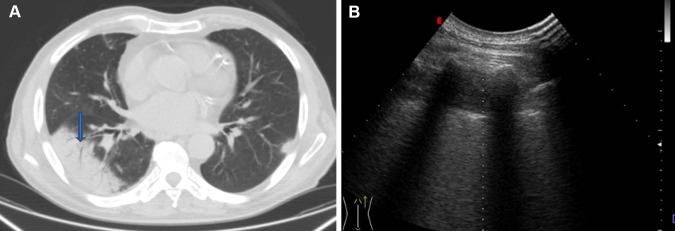
We also agree with the authors not paying emphasis on the results concerning “linear/arborescent bronchograms” [1]. Indeed, it should be stressed that no study or meta-analysis has so far demonstrated that such hyperechoic images specifically correspond to the CT imaging finding of the air bronchogram. Additionally, the CT detection of the air bronchogram is not associated with the US visualization in any case (Fig. 1). Finally, we have shown that such images can also be detected in lung neoplasm masses and are, therefore, not specific for pneumonia [5].
Fig. 1.
a CT scan showing subpleural pneumonia with air bronchogram (blue arrow) and b corresponding ultrasound image showing hypoechoic subpleural lesion in the absence of hyperechogenic spots or streaks from an air bronchogram
We would also acknowledge that other important factors strongly influencing the TUS pattern of a visualized lesion are the expertise and specific training of the operators, the inter-observer agreement, the ultrasound devices employed and their settings, and the probes used. Also, a complete TUS examination is complicated in neonates and in children because of the involuntary and numerous movements of the thoracic cage. The lack of any reference to these important points and acknowledgments of these main limits of TUS in many studies is an important bias influencing the quality of the results [5].
We could, therefore, conclude that we need to be wary, as proper interpretation of the information obtained from TUS studies requires the need to distinguish between true images and artifacts. This point is particularly relevant when TUS is not used in the context of a wider imaging study of the chest including CXR or, where necessary, CT scan.
Compliance with ethical standards
Conflict of interest
The authors have no conflict of interest.
References
- 1.Orso D, Ban A, Guglielmo N. Lung ultrasound in diagnosing pneumonia in childhood: a systematic review and meta-analysis. J Ultrasound. 2018 doi: 10.1007/s40477-018-0306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Toma P. Lung ultrasound in bronchiolitis. Eur J Pediatr. 2013;172(5):713. doi: 10.1007/s00431-013-1941-7. [DOI] [PubMed] [Google Scholar]
- 3.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Make Int J Soc Med Decis Make. 1991;11(2):88–94. doi: 10.1177/0272989X9101100203. [DOI] [PubMed] [Google Scholar]
- 4.Sperandeo M, Rotondo A, Guglielmi G, Catalano D, Feragalli B, Trovato GM. Transthoracic ultrasound in the assessment of pleural and pulmonary diseases: use and limitations. Radiol Med (Torino) 2014;119(10):729–740. doi: 10.1007/s11547-014-0385-0. [DOI] [PubMed] [Google Scholar]
- 5.Sperandeo M, Filabozzi P, Carnevale V. Ultrasound diagnosis of ventilator-associated pneumonia: a not-so-easy issue. Chest. 2016;149(5):1350–1351. doi: 10.1016/j.chest.2016.02.684. [DOI] [PubMed] [Google Scholar]