Abstract
Percutaneous renal biopsy (PRB) is an important procedure in the diagnostic and prognostic evaluation of renal disorders. Despite the relative simplicity, it can be a possible cause of iatrogenic renovascular injury. We describe two cases of iatrogenic pseudoaneurysm, a major post-biopsy complication, in two pediatric patients with persistent micro- and macro-hematuria, promptly diagnosed using color Doppler ultrasound, confirmed with renal arteriography and treated with embolization.
Keywords: Pseudoaneurysm, Percutaneous renal biopsy, Ultrasound, Complications, Pediatric patients
Sommario
La biopsia renale percutanea (BRP) è una procedura fondamentale nella valutazione diagnostica e prognostica delle patologie renali. Nonostante la relativa semplicità, può esser causa di danno renovascolare iatrogeno. Descriviamo due casi di pseudoaneurisma iatrogeno, una complicanza maggiore post-bioptica, in due pazienti pediatrici con micro e macroematuria persistente, tempestivamente diagnosticata con eco-color Doppler, confermata con arteriografia renale e trattata mediante embolizzazione.
Introduction
Percutaneous renal biopsy (PRB) is an important procedure in the diagnosis, prognosis and management of renal disorders in children. Despite the relative simplicity and the improvements in the PRB technique, it can be associated with minor and major complications. Ultrasound (US) examination is the primary imaging method to identify PRB complications because it is simple, rapid, cheap, accessible and non-invasive. Integration with color Doppler is fundamental because most of the PRB complications are vascular in origin; so, it allows to detect bleeding and assess vascular damage. We describe two cases of iatrogenic pseudoaneurysm, a major post-biopsy complication, in two pediatric patients with persistent micro- and macro-hematuria, promptly diagnosed using color Doppler US, confirmed with renal arteriography and treated with embolization.
Case 1
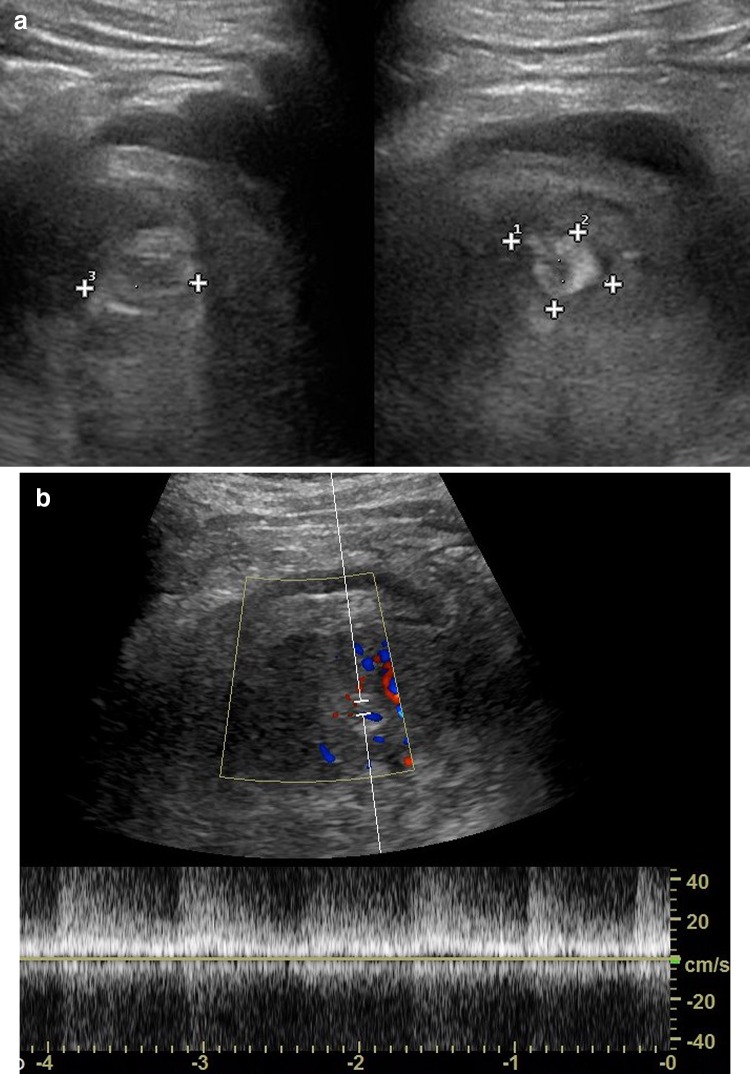
A 12-year-old male patient with Schonlein–Henoch purpura and persistent micro- and macro-hematuria came to our Radiology Department to perform an abdominal US 2 h after PRB. Renal US examination performed with convex probe (3–6 MHz) and linear probe (7.5–18 MHz)—Esaote My Lab Twice—showed a small intracortical hematoma at lower pole of the left kidney. A second US examination performed 23 h after PRB showed a larger intracortical hematoma associated with a rounded hyper-echogenic areola with a central pulsating hypo-echogenic core which showed turbulent flow on color Doppler (Fig. 1a, b). Near this areola, there was a triangular hyper-echogenic area with capsular base, which showed a significant reduction of the vascular flow compared to the surrounding renal parenchyma (Fig. 2). Peripherally, in the posterior–lateral side, a developing hypo–hyper-echogenic double-layered fluid collection in a various stage of reorganization was also detected between Gerota’s fascia and the renal parenchyma (Fig. 3). These findings were suggestive of the presence of an iatrogenic pseudoaneurysm.
Fig. 1.
a, b Case 1. On gray-scale US, a rounded hyper-echogenic areola (between x cursors) with a central hypo-echogenic core is seen at the lower pole of the left kidney (a). Spectral analysis shows turbulent flow with an increased high flow velocity (b)
Fig. 2.
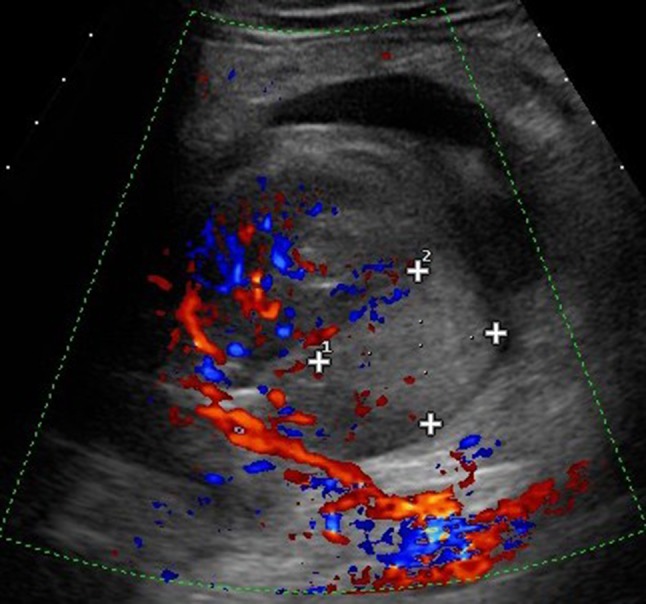
Case 1. On color Doppler US, note the triangular hyper-echogenic area with capsular base (between x cursors), which shows a significant reduction of the vascular flow compared to the surrounding renal parenchyma
Fig. 3.
Case 1. On gray-scale US, a hypo–hyper-echogenic double-layered fluid collection in a various stage of reorganization (between x cursors) is seen between Gerota’s fascia and the renal parenchyma, in the posterior–lateral side of left kidney
An abdominal contrast-enhanced computed tomography (CT) confirmed the presence of peri/pararenal collection and intracortical hematoma. CT also documented, during the arterial phase, the presence of an arterious vessel dilation corresponding to the pulsating areola detected on US (Fig. 4).
Fig. 4.

Case 1. Abdominal contrast-enhanced CT (axial plane)—arterial phase—shows the pseudo-aneurysmatic formation (arrow) in the renal cortex of the left kidney
Biochemical examinations showed anemia and activation of intravascular coagulation (Hb: 10.6 g/dl, HCT 30.1%, fibrinogen: 653 mg/dl, D-dimer: 1248 ng/ml) with increasing hemoglobinuria.
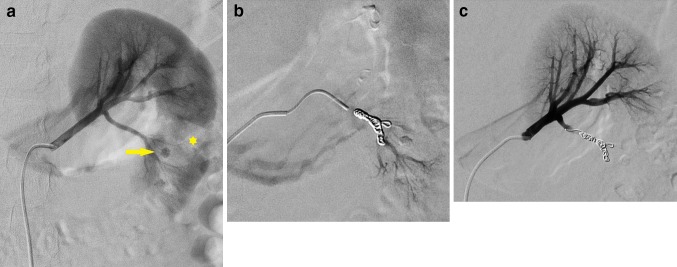
A renal arteriography with selective catheterization of left renal artery confirmed the presence of a pseudoaneurysm arising from a branch of a lower pole artery. After superselective catheterization of an interlobar branch, a complete embolization of the lesion with microspirals was performed and a resolution of the active bleeding was observed (Fig. 5a–c). In the following days, a normalization of blood-coagulation parameters and a progressive clinical improvement were observed.
Fig. 5.
a–c Case 1. Digital angiography with selective catheterization of the left renal artery. On the pre-embolization image (a), note the pseudoaneurysm (arrow) and the perfusion defect of the adjacent renal parenchyma (*). After embolization, a gradual occlusion of vascular lesion in the various control angiograms is seen (b, c)
Case 2
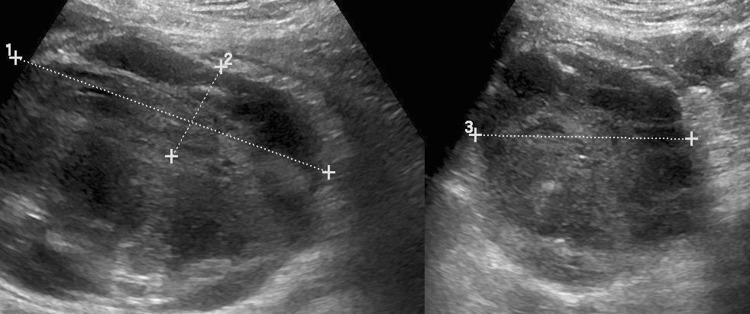
A 13-year-old girl with frequent episodes of macro-hematuria, high blood pressure and poor renal function came to our observation to perform a renal US 2 h after PRB. On gray-scale US, a small rounded anechoic cyst-like lesion was seen at the lower pole of the left kidney, where the previous biopsy was performed. On color Doppler US, this area showed a heterogeneous fill-in with aliasing artifacts and a turbulent blood flow, which was suggestive of an iatrogenic pseudoaneurysm (Fig. 6a–c). A thin fluid peri-renal collection around lower pole of the left kidney was also detected.
Fig. 6.
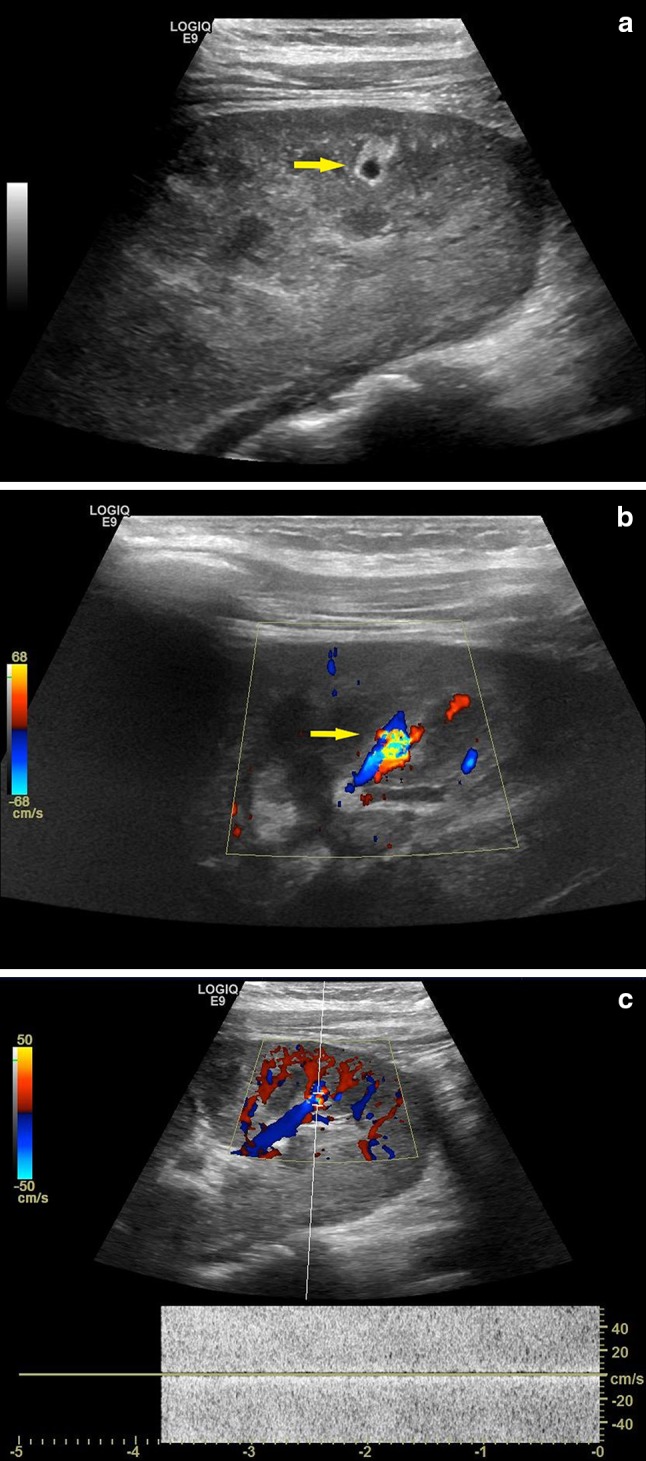
a–c Case 2. On gray-scale US (a) a small rounded anechoic cyst-like lesion (arrow) is seen. Color Doppler US shows heterogeneous fill-in with aliasing artifacts (b) and turbulent blood flow on spectral analysis (c)
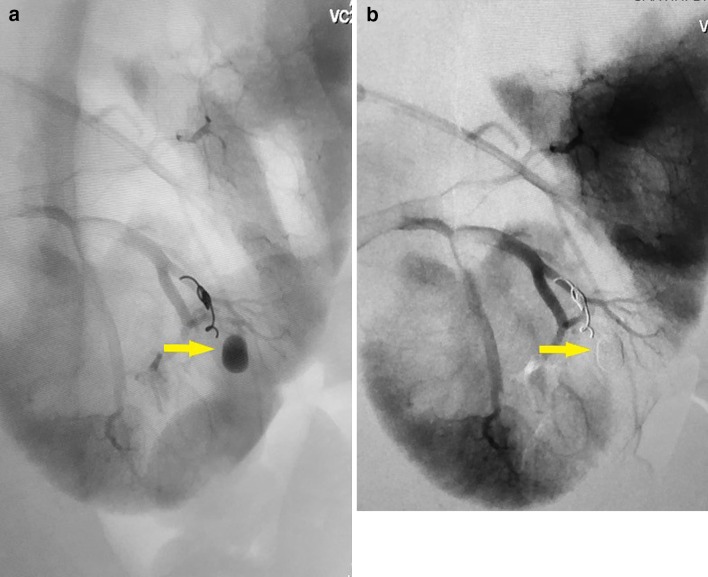
An abdominal contrast-enhanced CT showed, during the arterial phase, a small hypervascular area at the lower pole of the left kidney, corresponding to an iatrogenic pseudoaneurysm of an interlobar artery (Fig. 7). A renal arteriography finally confirmed the presence of a pseudoaneurysm arising from an interlobar artery. The lesion was treated with embolization with complete resolution of the bleeding and improvements of renal function (Fig. 8a, b).
Fig. 7.
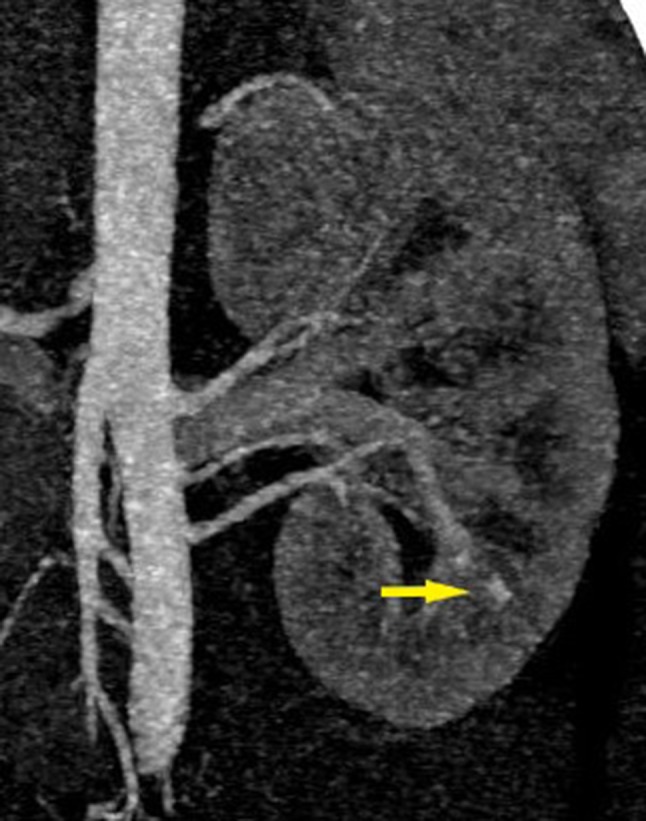
Case 2. Abdominal contrast-enhanced CT (coronal plane with MIP reconstruction)—arterial phase—shows a small pseudoaneurysm at the lower pole of the left kidney
Fig. 8.
a, b Case 2. Digital angiography with selective catheterization of the left renal artery (a) shows the pseudoaneurysm arising from an interlobar artery (arrow). In a successive control angiogram (b), note the complete occlusion of the vascular lesion (arrow)
Discussion
PRB of native and transplanted kidneys plays a relevant role in diagnosis, prognosis and management of several renal diseases in children [1, 2]. Its main role is to investigate possible causes of native kidney failure and the pathogenesis of rejection after renal transplantation. It is crucial to determine the severity and/or activity of nephropathy.
US is usually combined with biopsy during all the steps of the procedure: before procedure, to locate the optimal site of biopsy, generally at the lower pole of the left kidney, and to highlight abnormalities and/or malformations that may represent contraindications to the procedure itself; during the execution, to control the needle approaching the renal capsule; in the follow-up, to evaluate possible onset of complications.
Despite US guidance and automatic devices greatly improved the biopsy technique and significantly reduced the incidence of complications, this procedure is burden with iatrogenic renovascular damages and, therefore, renal complications [3–5].
The overall biopsy-related complication rate in pediatric patients reported by previous literature is around 5.2–23.5% [6]. Complications after PRB can be categorized into minor or major [7]. In minor complications, only pain management and clinical observation are required, as in the case of transient hematuria, subcapsular hematomas and small asymptomatic arteriovenous fistulas (AVF) generally disappear spontaneously within a few weeks after biopsy [8–11]. Major complications, such as pseudoaneurysms and symptomatic AVFs (0.1–6.6% of all PRB-related complications reported by previous literature), are generally associated with persistent hemorrhage and may need blood transfusion and invasive radiological (embolization) or surgical procedures (partial or total nephrectomy) [12]. Hematomas represent the most frequent complication of renal biopsy [13, 14]. On gray-scale US, hematomas show variable echogenicity in relation to the evolution stage: hypo-echogenicity is observed during the acute phase but they become rapidly hyper-echogenic, typically within 1–2 h, because of fibrin deposits. The appearance gradually becomes more complex and irregular due to the organization of clots and the edematous infarction. In our first case, the hematoma was partially organized, showing a hyper-echogenic component, resulting from an older bleeding and a hypo-echogenic portion, referred to a more recent bleeding.
Pseudoaneurysm represents a very rare major complication. It is caused by an incomplete arterial wall injury within the kidney that leads to a contained hemorrhage [7]. It usually affects intra-renal vessels and rarely the renal artery. It may undergo spontaneous thrombosis; however, this phenomenon is rare in renal vessels because of their high flow, which instead determines a progressive increase of its diameter. A possible further life-threatening complication is the rupture of pseudoaneurysm wall with bleeding in the retroperitoneal space or less frequently in the peritoneal cavity [15]. Detection of pseudoaneurysm is crucial. On gray-scale US, pseudoaneurysms can look like large pulsating vessels with ovoid or irregularly rounded morphology, as in our first case, or, more simply, like small rounded anechoic cyst-like lesions, as in our second case; therefore, they can be overlooked or misinterpreted if color Doppler is not performed [7]. Color Doppler analysis shows a turbulent flow and a characteristic appearance similar to a “mosaic of colors” due to the “aliasing” artifact with high systolic–diastolic velocities. In larger pseudoaneurysms (> 5 mm), it is possible to observe the typical swirling blood flow with the “Yin–Yang sign” [15].
Contrast-enhanced ultrasound (CEUS) with sulfur hexafluoride could be very helpful in diagnosis and follow-up of renal pseudoaneurysms. However, CEUS is still off-label in children for this use; so, it is almost exclusively used in adults [16].
The optimal observation period to identify major complications after PRB is 24 h as reported in many previous studies [17, 18]. Marwah and Korbet observed that 98% of complications overall and 100% of serious complications occurred within 23–24 h after PRB [19]. According to these studies, we performed the first US examination 2 h after PRB monitoring our patients in the successive 24 h. In fact, in one of our cases, the pseudoaneurysm was early noticed at the first US examination after PRB; while in the other case, it was observed later, after 23 h.
In our patients, Doppler US was performed first of all with convex probe (3–6 MHz) to obtain an overview of the kidney and then with a linear high-frequency probe (7.5–18 MHz) which allowed a detailed vision of the peripheral cortical vascularity in children due to their reduced tissue thickness. The higher spatial resolution of the linear probe permits a correct evaluation of interlobular vessels and shows vascular lesions that may occur.
The gold standard in diagnosing pseudoaneurysm is the angiography. However, in first instance, CT is often used because it is rapid, minimally invasive and gives the possibility to obtain a three-dimensional reconstruction of the hemorrhagic process and renal anatomy. When the suspected diagnosis is confirmed, the angiography is performed.
Angiography helps to define unclear anatomy seen on non-invasive examinations and allows concurrent treatment with selective embolism [20]. In our cases, arteriography confirmed the presence of the pseudoaneurysms seen on US images. Endovascular selective angio-embolization is the first-line treatment for renal pseudoaneurysms. It is a safe and effective therapeutic procedure and prevents the mortality and morbility of surgery [21]. Both our patients were treated with success by superselective transcatheter arterial embolization.
In conclusion, Doppler US examination is an essential tool to detect vascular complications, such as pseudoaneurysms, that may occur after PRB. A close follow-up with Doppler US in the first 24 h after PRB can ensure an early recognition and treatment of major complications. The use of high-frequency linear probes, in addiction to convex probes, is very helpful to detect in detail vascular anatomy of the peripheral cortex of the kidney and potential vascular lesions in children due to their reduced tissue thickness.
Abbreviations
- PRB
Percutaneous renal biopsy
- US
Ultrasound
- CT
Computed tomography
- ESPR
European Society of Pediatric Radiology
- AVF
Arteriovenous fistula
- CEUS
Contrast-enhanced ultrasound
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Walker PD. The renal biopsy. Arch Pathol Lab Med. 2009;133(2):181–188. doi: 10.5858/133.2.181. [DOI] [PubMed] [Google Scholar]
- 2.Riccabona M, Lobo ML, Willi U, Avni F, Damasio B, Ording-Mueller LS, et al. ESPR uroradiology task force and ESUR Paediatric Work Group—imaging recommendations in paediatric uroradiology, part VI: childhood renal biopsy and imaging of neonatal and infant genital tract. Minutes from the task force session at the annual ESPR Meeting 2012 in Athens on childhood renal biopsy and imaging neonatal genitalia. Pediatr Radiol. 2014;44:496–502. doi: 10.1007/s00247-013-2852-5. [DOI] [PubMed] [Google Scholar]
- 3.Maya ID, Maddela P, Barker J, Allon M. Percutaneous renal biopsy: comparison of blind and real-time ultrasound-guided technique. Semin Dial. 2007;20:355–358. doi: 10.1111/j.1525-139X.2007.00295.x. [DOI] [PubMed] [Google Scholar]
- 4.Hussain F, Mallik M, Marks SD, Watson AR. British Association of Paediatric Nephrology. Renal biopsies in children: current practice and audit of outcomes. Nephrol Dial Transplant. 2010;25:485–489. doi: 10.1093/ndt/gfp434. [DOI] [PubMed] [Google Scholar]
- 5.Bollée G, Martinez F, Moulin B, Meulders Q, Rougier JP, Baumelou A, et al. Renal biopsy practice in France: results of a nationwide study. Nephrol Dial Transpl. 2010;25:3579–3585. doi: 10.1093/ndt/gfq254. [DOI] [PubMed] [Google Scholar]
- 6.Yu MC, Lee F, Huang WH, Hsueh S. Percutaneous ultrasound-guided renal biopsy in children: the need for renal biopsy in pediatric patients with persistent asymptomatic microscopic hematuria. Biomed J. 2014;37:391–397. doi: 10.4103/2319-4170.132878. [DOI] [PubMed] [Google Scholar]
- 7.Aytac G, Yigit G, Alper S. Doppler US evaluation of renal biopsy complications in children. Diagn Interv Radiol. 2013;19:15–19. doi: 10.4261/1305-3825.DIR.5968-12.1. [DOI] [PubMed] [Google Scholar]
- 8.Riccabona M, Schwinger W, Ring E. Arteriovenous fistula after renal biopsy in children. J Ultrasound Med. 1998;17:505–508. doi: 10.7863/jum.1998.17.8.505. [DOI] [PubMed] [Google Scholar]
- 9.Skalova S, Rejtar P. Safety profile of paediatric percutaneous ultrasonography-guided renal biopsies. Singap Med J. 2010;51:481–483. [PubMed] [Google Scholar]
- 10.Sinha MD, Lewis MA, Bradbury MG, Webb NJ. Percutaneous real-time ultrasound-guided renal biopsy by automated biopsy gun in children: safety and complications. J Nephrol. 2006;19:41–44. [PubMed] [Google Scholar]
- 11.Feneberg R, Schaefer F, Zieger B, Waldherr R, Mehls O, Scherer K. Percutaneous renal biopsy in children: a 27-year experience. Nephron. 1998;79:438–446. doi: 10.1159/000045090. [DOI] [PubMed] [Google Scholar]
- 12.Mavili E, Dönmez H, Ozcan N, Sipahioglu M, Demirtas A. Transarterial embolization for renal arterial bleeding. Diagn Interv Radiol. 2009;15:143–147. [PubMed] [Google Scholar]
- 13.Manno C, Strippoli GF, Arnesano L, Bonifati C, Campobasso N, Gesualdo L, et al. Predictors of bleeding complications in percutaneous ultrasound-guided renal biopsy. Kidney Int. 2004;66(4):1570–1577. doi: 10.1111/j.1523-1755.2004.00922.x. [DOI] [PubMed] [Google Scholar]
- 14.Castoldi MC, Del Moro RM, D’Urbano ML, Ferrario F, Porri MT, Maldifassi P, D’Amico G, et al. Sonography after renal biopsy: assessment of its role in 230 consecutive cases. Abdom Imaging. 1994;19:72–77. doi: 10.1007/BF02165869. [DOI] [PubMed] [Google Scholar]
- 15.Saad NE, Saad WE, Davies MG, Waldman DL, Fultz PJ, Rubens DJ. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics. 2005;25(1):S173–S189. doi: 10.1148/rg.25si055503. [DOI] [PubMed] [Google Scholar]
- 16.Helck A, Hoffmann RT, Sommer WH, Notohamiprodjo M, Albyaa H, Reiser M, et al. Diagnosis, therapy monitoring and follow up of renal artery pseudoaneurysm with contrast-enhanced ultrasound in three cases. Clin Hemorheol Microcirc. 2010;46(2–3):127–137. doi: 10.3233/CH-2010-1339. [DOI] [PubMed] [Google Scholar]
- 17.Whittier WL, Korbet SM. Timing of complications in percutaneous renal biopsy. J Am Soc Nephrol. 2004;15:142–147. doi: 10.1097/01.ASN.0000102472.37947.14. [DOI] [PubMed] [Google Scholar]
- 18.Stiles KP, Yaun CM, Chung EM, Lion RD, Lane JD, Abbott KC. Renal Biopsy in high-risk patients with medic diseases of the kidney. Am J Kidney Dis. 2000;36:419–433. doi: 10.1053/ajkd.2000.8998. [DOI] [PubMed] [Google Scholar]
- 19.Marwah DS, Korbet SM. Timing of complications in percutaneous renal biopsy: what is the optimal of observation? Am J Kidney Dis. 1996;28:47–52. doi: 10.1016/S0272-6386(96)90129-8. [DOI] [PubMed] [Google Scholar]
- 20.Amoros Torres A, Palmero Marti JL, Ramirez Backhaus M, Ferrer Puchol MD, et al. Intrarenal pseudoaneurysm after percutaneous nephrolithotomy. Renal angiography and selective embolization. Arch Esp Urol. 2013;66(3):317–320. [PubMed] [Google Scholar]
- 21.Ngo TC, Lee JJ, Gonzalgo ML. Renel pseudoaneurysm: an overview. Nat Rev Urol. 2010;7(11):619–625. doi: 10.1038/nrurol.2010.163. [DOI] [PubMed] [Google Scholar]