Abstract
Anemia associated with heart failure is a frequent condition, which may lead to heart function deterioration by the activation of neuro-hormonal mechanisms. Therefore, a vicious circle is present in the relationship of heart failure and anemia. The consequence is reflected upon the patients’ survival, quality of life, and hospital readmissions. Anemia and iron deficiency should be correctly diagnosed and treated in patients with heart failure. The etiology is multifactorial but certainly not fully understood. There is data suggesting that the following factors can cause anemia alone or in combination: iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunction. There is data suggesting the association among iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunction. The main pathophysiologic mechanisms, with the strongest evidence-based medicine data, are iron deficiency and inflammation. In clinical practice, the etiology of anemia needs thorough evaluation for determining the best possible therapeutic course. In this context, we must correctly treat the patients’ diseases; according with the current guidelines we have now only one intravenous iron drug. This paper is focused on data about anemia in heart failure, from prevalence to optimal treatment, controversies, and challenges.
Keywords: anemia, heart failure, intravenous iron, ferric carboxymaltose, quality of life
Introduction
Heart failure (HF) represents a highly prevalent worldwide disease. It is estimated that its incidence will significantly rise within the near future. The proportion of patients with HF in the United States may increase by 46% and to >8 million by 2030 (1). Despite significant progress in therapeutic methods and tools, a large number of patients remain symptomatic, with limited capacity at exertion and a high mortality risk. These patients often associate other conditions that may complicate disease management, the most frequent being chronic kidney disease, anemia, and diabetes mellitus.
Definition
According to the World Health Organization (WHO), anemia is defined as low hemoglobin levels (<12 g/dL in women and <13 g/dL in men) (2). The WHO criteria are used on a large scale to define anemia; however, age and race are considered.
Prevalence
Anemia prevalence in patients with HF is variable (range, 9%–69.6%) based on the definition of anemia and the type of population studied (3). Patients included in the IV New York Heart Association (NYHA) class, who are refractory to medication, associate anemia in 80% of cases (4).
The etiology of anemia in heart failure
Despite anemia being a common occurrence in patients with HF, a direct causal link has not yet been established with either HF or the presence of other comorbidities. Accordingly, in practice, the etiology of anemia needs thorough evaluation to determine the best possible therapeutic course. The mechanisms responsible for anemia in patients with HF are still unclear. The following six factors have been suggested to cause anemia alone or in combination: iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunction. The main pathophysiologic mechanisms, with the strongest evidence-based medicine data, are iron deficiency and inflammation.
1. Iron deficiency
A ferritin level of <30 µg/L is usually suggestive of the presence of iron deficiency; it is classified as absolute (ferritin level <100 µg/L) or functional (ferritin level, 100-300 µg/L and transferrin saturation, <20%).
The mechanism responsible for iron deficiency involves multiple components. A combination of these mechanisms is presented in Figure 1. Nutritional deficiency in HF is associated with a reduced quantity of food ingested caused by dysgeusia, a low dietary intake of sodium, and even a dysfunction of hypothalamus-regulated appetite. Simultaneously, anomalies of the intestinal wall are involved, such as a rise in bacterial concentration and adherence to the intestinal epithelium, as well as a rise in paracellular permeability leading to cardiac cachexia and a systemic inflammation (5). Secondary to treatment with antiplatelet and/or anticoagulant therapy, irritation of the digestive mucosa may lead to microscopic loss of blood within the gastrointestinal system. Intestinal wall edema specific to advanced stages of heart disease may also further contribute to development of iron deficiency (6).
Figure 1.

The main mechanisms responsible for iron deficiency in heart failure
2. Inflammation
The pro-inflammatory status associated with chronic disease represents a key element in developing anemia and may contribute to its genesis through several mechanisms (Fig. 2).
Figure 2.
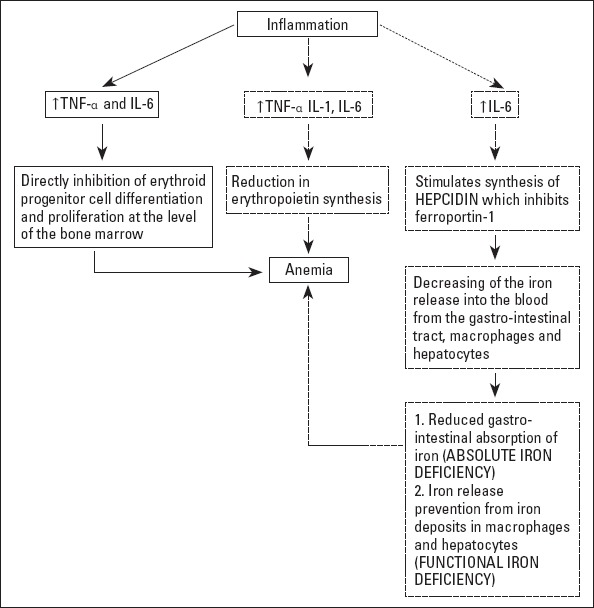
The main mechanisms involved in pro-inflammatory status associated with heart failure.
IL-1 - interleukin-1; IL-6 - interleukin-6; TNF-α - tumor necrosis factor α
The plasma levels of tumor necrosis factor α (TNF-α), interleukin-1 (IL-1), and interleukin-6 (IL-6) are elevated in patients with cardiac failure (7), and they determine a reduction in erythropoietin synthesis (the second arm of Fig. 2). TNF-α and IL-6 directly inhibit erythroid progenitor cell differentiation and proliferation at the level of the bone marrow (the first arm of Fig. 2). IL-6 stimulates synthesis of hepcidin, an acute phase protein, which in turn inhibits ferroportin-1 (responsible for the release of iron into the blood from the gastrointestinal tract, macrophages, and hepatocytes). Hepcidin increase leads to reduced gastrointestinal iron absorption and prevents iron release from iron deposits in macrophages and hepatocytes (8). Intestinal absorption is thus deficient and may result in absolute iron deficiency, whereas iron is sequestered in the reticuloendothelial system, leading to low bioavailability for the hematopoietic marrow and causing functional iron deficiency (the third arm of Fig. 2). As hepcidin is renal filtered and excreted, plasma levels are even higher in renal failure, which may partially explain the iron deficiency associated with this context (9).
In a study covering 321 patients, hepcidin levels were according to the level of HF (10). Patients in early HF stages (NYHA class I) have shown higher levels of hepcidin and ferritin than healthy subjects. After the aggravation of HF symptoms, a similar decline is associated in hepcidin, ferritin, and hemoglobin levels. Furthermore, an inversely proportional relationship has been shown between hepcidin and inflammatory marker levels (11). The initial stages of HF are characterized by high levels of hepcidin regulated by mechanisms outside the inflammatory system, whereas in the later stages, iron deficiency develops, leading to low hepcidin levels.
Anemia caused by liver congestion is associated with low levels of plasma iron and transferrin and elevated levels of hepcidin. This is possible because in congested liver, inflammation levels are high, leading to a rise in iron levels. Therefore, there is a rise in hepcidin secretion, which causes low digestive iron absorption and its release from the reticulo-endothelial system, causing iron deficiency associated with liver congestion (11).
3. Erythropoietin
Erythropoietin is a growth factor produced by renal peritubular cells; its synthesis is stimulated by tissue hypoxia when renal function is intact. Erythropoietin plasmatic levels rise significantly when hemoglobin levels are reduced. As an answer to global tissue hypoxia, erythropoietin levels are elevated in HF, albeit not comparable with hemoglobin levels. This discrepancy may be explained by resistance of the hematogenic marrow to erythropoietin (12). Evidence of modified erythropoietin synthesis has been found in most patients with HF and inflammatory anemia (13). Patients with high or normal levels of erythropoietin associate a reduced response to this hormone as a consequence of structural changes. Malnutrition and pro-inflammatory cytokines play an important role in the development of erythropoietin resistance (14).
Renal dysfunction is associated with a threefold rise in anemia prevalence. Anemia levels are directly proportional with the severity of renal dysfunction, as well as low erythropoietin levels (15). Erythropoietin shows pleiotropic effects over some non-erythropoietin cells. As an answer to oxidative, metabolic stress or renal lesions, erythropoietin may be synthesized by a few other types of non-renal tissues. The myocardium is one of the tissues, which produces erythropoietin-specific receptors; when stimulated by this hormone, the myocardial tissue produces hypoxia-induced factor-1, which stimulates erythropoietin gene transcription.
4. Renin-angiotensin-aldosterone system
Angiotensin II stimulates erythropoietin production and erythropoiesis by reducing oxygen delivery to erythropoietin-producing cells. Even though these effects are beneficial in preventing the development of anemia, renin–angiotensin–aldosterone system (RAAS) activation represents a major pathway in the progression of HF, and as a consequence, a therapeutic target. In this context, using angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) may hamper erythropoietin production and its effect on the bone marrow. At the same time, treatment with ACE inhibitors results in plasma level reduction. However, clinical trials have shown a low but significant decrease in hemoglobin in patients treated with ACEI (16). For example, treatment with enalapril was associated to an intent-to-treat model, with a rise in the risk of developing new anemia at 1 year by 56% (17). The levels of N acetyl-seryl-aspartyl-lysin-prolyn, an erythropoiesis inhibitor, rise with ACEI usage, causing a fall in erythropoiesis and anemia (18).
Interrupting the administration of ACEI in dialysis patients has determined a rise in hemoglobin levels to the point that a reduction in erythropoietin dosage was necessary in selected cases (19).
5. Beta-blocker treatment
Beta-blockers represent the standard treatment for patients with HF. Compared with metoprolol, carvedilol determines a small but significant reduction in hemoglobin levels. Erythropoietin-secreting cells show an extensive sympathetic system nerve supply, whereas erythroid progenitor cells have adrenergic beta 1, beta 2, and alpha surface receptors. By only blocking the beta 2 receptors, erythropoietin synthesis and erythroid progenitor cells proliferation are reduced.While carvedilol blocks all three receptor types, metoprolol acts only upon the beta 1 type and therefore does not cause anemia (20).
6. Hemodilution
Anemia may also represent a consequence of high plasma levels caused by water and sodium retention. A study of patients with advanced HF, who were considered for transplant and were clinically euvolemic, has shown that the incidence of anemia induced by hemodilution was 46% of all the cases (21). However, other studies have shown that clinically euvolemic patients associate a normal plasmatic level (22). These aspects require further investigations to be fully confirmed.
7. Others
It has been shown that HF is associated with medullar dysfunction, which has a simultaneous impact on several hematopoietic lines (23).
In intensive care units, it has been shown that a significant amount of patient`s blood is used for laboratory investigations. Therefore, a blood test should only be requested when absolutely necessary, and not as routine practice (24).
Data gathered by the FDA Adverse Event Reporting System has shown that digoxin therapy may determine anemia (25).
Physiopathological consequences of anemia
In the presence of chronic anemia, low tissue oxygenation results, which leads to the development of compensatory mechanisms: hemodynamic and non-hemodynamic.
The two main non-hemodynamic mechanisms are erythropoiesis stimulation, which leads to an increased capacity of oxygen transport, and a lowering of hemoglobin affinity for oxygen, leading to a rise in oxygen levels being transported to the tissues. These are rapid and reversible mechanisms, allowing for immediate changes in binding and releasing oxygen to peripheral tissue (22).
The hemodynamic compensatory mechanisms are significantly more complex and slower and associate numerous unfavorable effects. Initially, there is a reduction in the peripheral vascular resistance as a consequence of both low hematocrit values and the vasodilation mediated by high levels of nitric oxide. These events lead to low blood pressure, which causes a reflex rise in cardiac debit, to maintain balanced blood pressure and tissue perfusion. A rise in sympathetic and RAAS activity determines vasoconstriction and low renal perfusion. Water and salt retention results, with plasmatic and extracellular expansion. Over the long term, these mechanisms are responsible for the development of HF in patients with severe anemia (<7 g/dL). In patients who associate HF, a lower grade anemia may lead to heart function deterioration by activation of neurohormonal mechanisms.
Prognosis
Iron deficiency and mortality in patients with heart failure
A meta-analysis involving 34 studies and over 1.50,000 patients has concluded that anemia is present in one-third of the patients with HF and is associated with significantly higher mortality rates, independent from the presence or absence of systolic dysfunction (26).
Several observational studies have shown that iron deficiency is associated with a rise in mortality in patients with HF. The unfavorable prognosis associated with iron deficiency was not influenced by the presence or absence of anemia (27). Moreover, it has been determined that patients with iron deficiency without anemia have a two-fold mortality risk compared with patients with anemia without iron deficiency. This data seems to imply that the presence of iron deficiency entails a less favorable prognosis than anemia (11). In contrast, a study of patients with a history of HF treated in the ambulatory setting has not found a correlation between iron deficiency and mortality by all causes (28).
This rise in mortality is also documented in patients with acute HF. Research on 719 patients admitted for acute HF phenomena has underlined an independent rise in one-year mortality in patients with anemia (29).
It seems that there are no significant differences between mortality risks of anemia in patients with preserved or impaired systolic function (30).
Iron deficiency and physical exercise intolerance, low quality of life, and hospital admission frequency
Both anemia and iron deficiency are associated with a decrease in effort capacity and quality of life, as well as a rise in hospital admission frequency.
The causal relationship between iron deficiency and decreased effort capacity has been demonstrated by published studies even in the absence of anemia. Low effort capacity is linked with mitochondrial dysfunction and low mitochondrial iron deposits, leading to low energetic efficiency. The consequences of iron deficiency over cognitive performance and the effect on behavior have been documented and successfully reversed by iron supplementation (31).
Patients with iron deficiency also have low quality of life levels, mostly determined by physical limitations in daily activities. The negative impact of iron deficiency on quality of life has been proved independent from anemia (11).
The causative mechanisms responsible for low quality of life and effort capacity remain unclear. Myocardium and skeletal muscle dysfunction determined by iron deficiency are central to the physiopathology of HF. Experimental research conducted on ischemic mice myocardium has shown a rise in hepcidin expression determined by hypoxia. Regardless, these changes, their pathophysiological consequences and their relationship with iron metabolism are not fully understood. However, the association between anemia, iron deficiency, and sympathetic activation with a rise in cardiac debit, left ventricular hypertrophy, and finally left ventricular dilation has been proven (5).
Sports medicine has provided initial data indicating a link between iron deficiency and skeletal muscle function. A normal iron status has been associated with a rise in stamina and aerobic capacity. Anemic rats with iron deficiency received blood transfusions and/or a diet rich in iron. A rise in effort capacity was only detected in animals receiving iron supplements. This data has resulted from studies on healthy subjects with iron deficiency. Whether the conclusions apply to patients with HF is yet to be determined (5).
Treatment
A strong link between anemia and a rise in mortality, as well as a decline in life quality, has determined strong interest for detecting the most efficient treatment methods. It has been suggested that the treatment of anemia may break the vicious cycle represented by the cardio-renal anemia syndrome, a crucial step in enhancing the response to the treatment of HF.
Transfusion
One possible method to treat anemia in HF is blood transfusion, but its usage is limited to cases with severe anemia and is associated with several risks (immune system suppression, iron overcharge, susceptibility to infection, and sensitization to leukocyte antigens) (32).
Hence, transfusion should be avoided as a long-term method and should be only used in the acute phase of severe anemia.
Erythropoiesis-stimulating agents
Another treatment method is using erythropoiesis-stimulating agents. A meta-analysis including 11 clinical randomized trials studying 794 patients with HF and anemia who were treated with erythropoiesis-stimulating agents concluded that this treatment favorably influences symptomatology and functional capacity and reduces clinical events (33).
However, recent studies of patients with chronic kidney disease have demonstrated an association between erythropoiesis-stimulating agents and an elevated risk of cardiovascular events, including arterial hypertension, stroke, thromboembolic events, as well as a less favorable prognostic for oncological patients. One of the possible causes for the rise in cardiovascular mortality could be the decrease in iron deposits as a result of hematopoiesis stimulation. These events could lead to reactive thrombocytosis and the development of cardiovascular and embolic events.
The widest double-blind randomized clinical trial, including 2,278 patients, has discovered that correcting anemia with darbepoetin alpha did not reduce mortality or hospitalization rates. Even more, a significant rise in thromboembolic events has been recorded (34). Accordingly, employing erythropoiesis-stimulating agents in patients with anemia and HF is only recommended in individuals who also suffer from chronic kidney disease.
Oral iron supplements
There are multiple pathophysiological reasons why oral iron treatment in patients with HF has not been thoroughly studied and why injectable iron is preferred. Significantly, there are numerous gastrointestinal consequences of oral iron, which negatively impact compliance. At the same time, alterations in the digestive system associated with HF lead to a marked reduction of iron absorption, whereas high levels of hepcidin found in HF also reduce the intestinal iron absorption and block iron in the reticulo-endothelial system. Proton pump inhibitors are drugs widely used in patients with HF and can interfere with iron absorption by lowering the gastric pH. Moreover, the maximum quantity that may be absorbed intestinally is 10 mg, leading to an oral iron treatment plan spanning over a long period of time.
In this context, just a few studies have evaluated the role of oral iron treatment in patients with HF. IRON-HF is a multicentric, randomized, placebo-controlled (35), double-blind study evaluating patients with HF (FE <40%) and anemia (Hb <12 g/dL; transferrin saturation <20%; and ferritin <500 µg/L). Twenty-three patients were randomized into three groups: the first group received intravenous iron; the second was treated with oral iron, and the third received a placebo. The conclusions of the study, after a 3-month screening period, suggest that oral iron is equivalent to the intravenous solution in regard to their performance in correcting anemia. However, intravenous iron seems superior in regard to enhancing functional capacity. A retrospective study (36) including 105 patients with iron deficiency and systolic dysfunction of the left ventricle who were treated with oral iron has recorded results comparable with the intravenous option in correcting the iron deficiency.
Recently, a randomized trial including 225 patients with iron deficiency and HF has found no statistically significant difference between patients receiving oral iron versus placebo in regard to peak VO2, the 6-minute walking test, NT-pro-BNP value, or the score resulting from the Kansas City Cardiomyopathy Questionnaire (37).
Considering the limited amount of evidence resulting from a limited number of patients or a limited screening period, it is not yet advisable to recommend oral iron in patients with HF, as randomized trials including a significant number of patients are needed to clarify the expected answers.
Injectable iron preparations
The latest HF Guidelines (2016) recommend routine evaluation of iron deficiency in patients with HF and ferric carboxymaltose therapy for alleviating symptoms determined by cardiac failure, enhancing quality of life and effort capacity (38).
Several studies (39-45) have been set out to establish the effect of injectable iron treatment in patients with HF (Table 1). All showed important benefits of this therapeutic option in patients with HF through correction of anemia, as well as the beneficial effects over effort capacity (assessed by NYHA classification and 6-minute walk test) and quality of life.
Table 1.
Design and results of studies with injectable iron treatment in patients with heart failure
| Study | Patients | Design | Anemia/ ID | Treatment | Follow-up | Outcomes |
|---|---|---|---|---|---|---|
| Bolger et al.39 (2006) | 16 | Open | Anemia | Iron sucrose max 1000 mg | 92 days | Corrected anemia and improved NYHA class, MLWHF score and 6MWD |
| Toblli et al.40 (2007) | 40 | Randomized, double-blind | Anemia and ID | Iron sucrose 1000 mg | 6 months | Corrected anemia and reduced NT-pro BNP, CRP, improved NYHA class, MLWHF score and 6MWD |
| Usmanov et al.41 (2008) | 32 | Open | Anemia with ID | Iron sucrose 3200 mg | 26 weeks | Corrected anemia and improved cardiac remodeling and NYHA class |
| Okonko et al.42 (2008) FERRIC-HF study | 35 | Randomized | Anemia and ID | Iron sucrose 200 mg/week for 16 weeks | 18 weeks | Improved peak VO2, NYHA class |
| Anker et al.43 (2009) FAIR-HF study | 459 | Randomized, double-blind | Iron deficiency | Ferric carboxymaltose 200 mg/week until corrected | 24 weeks | Improved Patient Global Assessment, NYHA class, 6MWD, KCCQ score |
| Gaber et al.44 (2012) | 40 | Open | Iron deficiency | Iron dextran 200 mg/week until correction | 12 weeks | Improved myocardial function systolic and diastolic function determined by tissue Doppler and strain rate |
| Ponikowski et al.45(2015) CONFIRM_HF study | 304 | Randomized, double-blind | Iron deficiency | Ferric carboxymaltose 500-2500 mg | 52 weeks | Improved 6MWD, NYHA class, KCCQ score, decreased risk of hospitalization |
HF - heart failure; ID - iron deficiency; MLWHF - Minnesota living with heart failure; 6MWD - 6-minute walking test; KCCQ - Kansas City Cardiomyopathy Questionnaire; NYHA - New York Heart Association
All-cause mortality and hospitalizations were reduced in some studies (41-42), but the duration of follow-up for these patients was short (26 weeks), and we do not understand the long-term effect of this treatment. It was observed that this treatment could improve cardiac remodeling (41) and left ventricular ejection fraction (44). Levels of N-terminal-pro-brain natriuretic peptide and C reactive protein decreased after iron treatment (40).
The improved symptoms are thought to be associated with increased hemoglobin levels and thus increased peripheral oxygen delivery. However, the results from FAIR-HF study suggest other mechanism involvement, since the group with iron deficiency without anemia had improvement in functional capacity without significant changes in the hemoglobin level. One possible explanation for this effect is the improved oxygen utilization in skeletal muscle (45).
Some meta-analyses have evaluated the effect of injectable iron treatment in patients with HF. One analysis showed positive changes impacting the NYHA class, quality of life, 6-minute walk test, and left ventricle ejection fraction, as well as the number of hospital admissions (46). Another one indicated reduced hospital admission levels, less adverse events, as well as NYHA class and left ventricle ejection fraction improvement (47). No analysis detected any outcome relating to reduced mortality during the screening period of only 6 months.
The most recent meta-analysis (48) shows that iron therapy enhances physical exercise capacity and quality of life and reduces HF symptoms. No impact on mortality of any cause was found; however, unscheduled hospital admissions decreased, as well as of combined mortality risk of any cause, cardiovascular hospital admissions, and cardiovascular death risk. In addition it reduced the risk of the combined endpoint of all-cause death or cardiovascular hospitalization, and the combined endpoint of cardiovascular death or hospitalization for worsening HF.
Conclusions
Anemia is frequently associated with HF. The etiology of this association is multifactorial and certainly not fully understood. The main pathophysiologic mechanisms, with the strongest evidence-based medicine data, are iron deficiency and inflammation. ACEIs and ARBs are essential drugs recommended in HF, but they might represent one of the causes of anemia related to this chronic disease. The adrenergic beta 1, beta 2, and alpha blockers such as carvedilol or digoxin, useful drugs recommended in HF, were also incriminated.
It seems that there are not enough evidences regarding oral iron in this aspect. The current guidelines of HF recommend only one intravenous iron (ferric carboxymaltose) for the treatment of anemia. However, in the literature, there is no clear way to proceed after the correction of iron deficiency. The clinical judgment is important here, but we also need to know the risks of iron overload: bacterial infections, increased oxidative stress, which could lead to endothelial dysfunction, and increased risk of coronary events. In this context, further randomized trial should be performed to evaluate the long-term impact of iron treatment on patients and the right period of treatment.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept – O.S., M.F., P.A., L.S.; Design – O.S., M.F., V.S., L.S.; Supervision – M.F., V.S., L.S.; Fundings – O.S., P.A., V.S., L.S.; Materials – O.S., A.S., P.D., P.A.; Data collection and/or processing – O.S., M.F., A.S., V.S., L.S.; Analysis and/or interpretation – O.S., M.F., P.D., P.A.; Literature search – O.S., M.F., V.S., L.S.; Writing – O.S., M.F., L.S.; Critical review – O.S., M.F., P.D., A.S., P.A., V.S., L.S.
References
- 1.Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. American Heart Association Advocacy Coordinating Committee;Council on Arteriosclerosis, Thrombosis and Vascular Biology;Council on Cardiovascular Radiology and Intervention;Council on Clinical Cardiology;Council on Epidemiology and Prevention;Stroke Council. Forecasting the impact of heart failure in the United States:a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–19. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.von Haehling S, Anker MS, Jankowska EA, Ponikowski P, Anker SD. Anemia in chronic heart failure:Can we treat?What to treat? Heart Fail Rev. 2012;17:203–10. doi: 10.1007/s10741-011-9283-x. [DOI] [PubMed] [Google Scholar]
- 3.Groenveld HF, Januzzi JL, Damman K, van Wijngaarden J, Hillege HL, van Veldhuisen DJ, et al. Anemia and Mortality in Heart Failure Patients- A Systematic Review and Meta-Analysis. J Am Coll Cardiol. 2008;52:818–27. doi: 10.1016/j.jacc.2008.04.061. [DOI] [PubMed] [Google Scholar]
- 4.Beavers CJ, Alburikan KA, Rodgers Jo E, Dunn SP, Reed BN. Distinguish in Anemia and Iron Deficiency of Heart Failure:Signal for Severity of Disease or Unmet Therapeutic Need? Pharmacotherapy. 2014;34:719–32. doi: 10.1002/phar.1412. [DOI] [PubMed] [Google Scholar]
- 5.Jankowska EA, von Haehling S, Anker SD, Macdougall IC, Ponikowski P. Iron deficiency and heart failure:diagnostic dilemmas and therapeutic perspectives. Eur Heart J. 2013;34:816–29. doi: 10.1093/eurheartj/ehs224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Testa M, Yeh M, Lee P, Fanelli R, Loperfido F, Berman JW, et al. Circulating levels of cytokines and their endogenous modulators in patients with mild to severe congestive heart failure due to coronary artery disease or hypertension. J Am Coll Cardiol. 1996;28:964–71. doi: 10.1016/s0735-1097(96)00268-9. [DOI] [PubMed] [Google Scholar]
- 7.Gunawardena S, Dunlap ME. Anemia and Iron Deficiency in Heart Failure. Curr Heart Fail Rep. 2012;9:319–27. doi: 10.1007/s11897-012-0112-x. [DOI] [PubMed] [Google Scholar]
- 8.Silverberg DS, Wexler D, Schartz D. Is Correction of Iron Deficiency a New Addition to the Treatment of the Heart Failure? Int J Mol Sci. 2015;16:14056–74. doi: 10.3390/ijms160614056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jankowska EA, Malyszko J, Ardehali H, Koc-Zorawska E, Banasiak W, von Haehling S, et al. Iron status in patients with chronic heart failure. Eur Heart J. 2013;34:827–34. doi: 10.1093/eurheartj/ehs377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fitzsimons S, Doughty RN. Iron deficiency in patients with heart failure. Eur Heart J Cardiovasc Pharmacother. 2015;1:58–64. doi: 10.1093/ehjcvp/pvu016. [DOI] [PubMed] [Google Scholar]
- 11.Murphy CL, McMurray JJ. Approaches to the treatment of anemia in patients with chronic heart failure. Heart Fail Rev. 2008;13:431–8. doi: 10.1007/s10741-008-9085-y. [DOI] [PubMed] [Google Scholar]
- 12.Opasich C, Cazzola M, Scelsi L, De Feo S, Bosimini E, Lagioia R, et al. Blunted erythropoietin production and defective iron supply for erythropoiesis as major causes of anemia in patients with chronic heart failure. Eur Heart J. 2005;26:2232–7. doi: 10.1093/eurheartj/ehi388. [DOI] [PubMed] [Google Scholar]
- 13.Felker GM, Adams KF, Gattis WA, O'Connor CM. Anemia as a Risk Factor and Therapeutic target in heart failure. J Am Coll Cardiol. 2004;44:959–66. doi: 10.1016/j.jacc.2004.05.070. [DOI] [PubMed] [Google Scholar]
- 14.Kılıçgedik A, Dündar C, Tigen MK. Anemia in heart failure. Anadolu Kardiyol Derg. 2012;12:65–70. doi: 10.5152/akd.2012.011. [DOI] [PubMed] [Google Scholar]
- 15.Tang YD, Katz SD. Anemia in chronic heart failure:prevalence, etiology, clinical correlates, and treatment options. Circulation. 2006;113:2454–61. doi: 10.1161/CIRCULATIONAHA.105.583666. [DOI] [PubMed] [Google Scholar]
- 16.Ishani A, Weinhandl E, Zhao Z, Gilbertson DT, Collins AJ, Yusuf S, et al. Angiotensin-converting enzyme inhibitor as a risk factor for the development of anemia, and the impact of incident anemia on mortality in patients with left ventricular dysfunction. J Am Coll Cardiol. 2005;45:391–9. doi: 10.1016/j.jacc.2004.10.038. [DOI] [PubMed] [Google Scholar]
- 17.van der Meer P, Lipsic E, Westenbrink D, van de Wal RM, Schoemaker RG, Vellenga E, et al. Levels of hematopoiesis inhibitor N-acetyl-seryl-aspartyl-lysyl-proline partially explain the occurrence of anemia in heart failure. Circulation. 2005;112:1743–7. doi: 10.1161/CIRCULATIONAHA.105.549121. [DOI] [PubMed] [Google Scholar]
- 18.Vasu S, Kelly P, Lawson WE. Anemia in heart failure--a concise review. Clin Cardiol. 2005;28:454–8. doi: 10.1002/clc.4960281003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Komajda M, Anker SD, Charlesworth A, Okonko D, Metra M, Di Lenarda A, et al. The impact of new onset anemia on morbidity and mortality in chronic heart failure:results from COMET. Eur Heart J. 2006;27:1440–6. doi: 10.1093/eurheartj/ehl012. [DOI] [PubMed] [Google Scholar]
- 20.Androne AS, Katz SD, Lund L, LaManca J, Hudaihed A, Hryniewicz K, et al. Hemodilution is common in patients with advanced heart failure. Circulation. 2003;107:226–9. doi: 10.1161/01.cir.0000052623.16194.80. [DOI] [PubMed] [Google Scholar]
- 21.Anand IS. Heart failure and anemia:mechanisms and pathophysiology. Heart Fail Rev. 2008;13:379–86. doi: 10.1007/s10741-008-9088-8. [DOI] [PubMed] [Google Scholar]
- 22.Westenbrink BD, Voors AA, de Boer RA, Schuringa JJ, Klinkenberg T, van der Harst P, et al. Bone marrow dysfunction in chronic heart failure patients. Eur J Heart Fail. 2010;12:676–84. doi: 10.1093/eurjhf/hfq061. [DOI] [PubMed] [Google Scholar]
- 23.Klutstein MW, Tzivoni D. Anaemia and heart failure:aetiology and treatment. Nephrol Dial Transplant. 2005;20(Suppl 7):vii7–10. doi: 10.1093/ndt/gfh1100. [DOI] [PubMed] [Google Scholar]
- 24.Lin Y, He S, Feng R, Xu Z, Chen W, Huang Z, et al. Digoxin-induced anemia among patients with atrial fibrillation and heart failure:clinical data analysis and drug-gene interaction network. Oncotarget. 2017;8:57003–11. doi: 10.18632/oncotarget.18504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drakos SG, Anastasiou-Nana MI, Malliaras KG, Nanas JN. Anemia in chronic heart failure. Congest Heart Fail. 2009;15:87–92. doi: 10.1111/j.1751-7133.2009.00049.x. [DOI] [PubMed] [Google Scholar]
- 26.Groenveld HF, Januzzi JL, Damman K, van Wijngaarden J, Hillege HL, van Veldhuisen DJ, et al. Anemia and mortality in heart failure patients a systematic review and meta-analysis. J Am Coll Cardiol. 2008;52:818–27. doi: 10.1016/j.jacc.2008.04.061. [DOI] [PubMed] [Google Scholar]
- 27.Wong CC, Ng AC, Kritharides L, Sindone AP. Iron Deficiency in Heart Failure:Looking Beyond Anaemia. Heart Lung Circ. 2016;25:209–16. doi: 10.1016/j.hlc.2015.06.827. [DOI] [PubMed] [Google Scholar]
- 28.Parikh A, Natarajan S, Lipsitz SR, Katz SD. Iron deficiency in community-dwelling US adults with self-reported heart failure in the National Health and Nutrition Examination Survey III:prevalence and associations with anemia and inflammation. Circ Heart Fail. 2011;4:599–606. doi: 10.1161/CIRCHEARTFAILURE.111.960906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Migone de Amicis M, Chivite D, Corbella X, Cappellini MD, Formiga F. Anemia is a mortality prognostic factor in patients initially hospitalized for acute heart failure. Intern Emerg Med. 2017;12:749–56. doi: 10.1007/s11739-017-1637-5. [DOI] [PubMed] [Google Scholar]
- 30.Groenveld HF, Januzzi JL, Damman K, van Wijngaarden J, Hillege HL, van Veldhuisen DJ, et al. Anemia and mortality in heart failure patients a systematic review and meta-analysis. J Am Coll Cardiol. 2008;52:818–27. doi: 10.1016/j.jacc.2008.04.061. [DOI] [PubMed] [Google Scholar]
- 31.Cohen-Solal A, Leclercq C, Mebazaa A, de Groote P, Damy T, Isnard R, et al. Diagnosis and treatment of iron deficiency in patients with heart failure:expert position paper from French cardiologists. Arch Cardiovasc Dis. 2014;107:563–71. doi: 10.1016/j.acvd.2014.07.049. [DOI] [PubMed] [Google Scholar]
- 32.Palazzouli A, Ruocco G, Pellegrini M, De Gori C, Del Castillo G, Giordano N, et al. The role of erythropoietin stimulating agents in anemic patients with heart failure:solved and unresolved questions. Ther Clin Risk Manag. 2014;10:641–50. doi: 10.2147/TCRM.S61551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kotecha D, Ngo K, Walters JA, Manzano L, Palazzuoli A, Flather MD. Erythropoietin as a treatment of anemia in heart failure:systematic review of randomized trials. Am Heart J. 2011;161:822–31. doi: 10.1016/j.ahj.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 34.Swedberg K, Young JB, Anand IS, Cheng S, Desai AS, Diaz R, et al. RED-HF Committees;RED-HF Investigators. Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med. 2013;368:1210–9. doi: 10.1056/NEJMoa1214865. [DOI] [PubMed] [Google Scholar]
- 35.Beck-da-Silva L, Piardi D, Soder S, Rohde LE, Pereira-Barretto AC, de Albuquerque D, et al. IRON-HF study:a randomized trial to assess the effects of iron in heart failure patients with anemia. Int J Cardiol. 2013;168:3439–42. doi: 10.1016/j.ijcard.2013.04.181. [DOI] [PubMed] [Google Scholar]
- 36.Niehaus ED, Malhotra R, Cocca-Spofford D, Semigran M, Lewis GD. Repletion of Iron Stores With the Use of Oral Iron Supplementation in Patients With Systolic Heart Failure. J Card Fail. 2015;21:694–7. doi: 10.1016/j.cardfail.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 37.Lewis GD, Malhotra R, Hernandez AF, McNulty SE, Smith A, Felker GM, et al. NHLBI Heart Failure Clinical Research Network. Effect of Oral Iron Repletion on Exercise Capacity in Patients With Heart Failure With Reduced Ejection Fraction and Iron Deficiency:The IRONOUT HF Randomized Clinical Trial. JAMA. 2017;317:1958–66. doi: 10.1001/jama.2017.5427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure:The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 39.Bolger AP, Bartlett FR, Penston HS, O'Leary J, Pollock N, Kaprielian R, et al. Intravenous iron alone for the treatment of anemia in patients with chronic heart failure. J Am Coll Cardiol. 2006;48:1225–7. doi: 10.1016/j.jacc.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 40.Toblli JE, Lombraña A, Duarte P, Di Gennaro F. Intravenous iron reduces NT-pro-brain natriuretic peptide in anemic patients with chronic heart failure and renal insufficiency. J Am Coll Cardiol. 2007;50:1657–65. doi: 10.1016/j.jacc.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 41.Usmanov RI, Zueva EB, Silverberg DS, Shaked M. Intravenous iron without erythropoietin for the treatment of iron deficiency anemia in patients with moderate to severe congestive heart failure and chronic kidney insufficiency. J Nephrol. 2008;21:236–42. [PubMed] [Google Scholar]
- 42.Okonko DO, Grzeslo A, Witkowski T, Mandal AK, Slater RM, Roughton M, et al. Effect of intravenous iron sucrose on exercise tolerance in anemic and nonanemic patients with symptomatic chronic heart failure and iron deficiency FERRIC-HF:a randomized, controlled, observer-blinded trial. J Am Coll Cardiol. 2008;51:103–12. doi: 10.1016/j.jacc.2007.09.036. [DOI] [PubMed] [Google Scholar]
- 43.Anker SD, Comin Colet J, Filippatos G, Willenheimer R, Dickstein K, Drexler H, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med. 2009;361:2436–48. doi: 10.1056/NEJMoa0908355. [DOI] [PubMed] [Google Scholar]
- 44.Gaber R, Kotb NA, Ghazy M, Nagy HM, Salama M, Elhendy A. Tissue Doppler and strain rate imaging detect improvement of myocardial function in iron deficient patients with congestive heart failure after iron replacement therapy. Echocardiography. 2012;29:13–8. doi: 10.1111/j.1540-8175.2011.01532.x. [DOI] [PubMed] [Google Scholar]
- 45.Ponikowski P, van Veldhuisen DJ, Comin-Colet J, Ertl G, Komajda M, Mareev V, et al. Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency†. Eur Heart J. 2015;36:657–68. doi: 10.1093/eurheartj/ehu385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Avni T, Leibovici L, Gafter-Gvili A. Iron supplementation for the treatment of chronic heart failure and iron deficiency:systematic review and meta-analysis. Eur J Heart Fail. 2012;14:423–9. doi: 10.1093/eurjhf/hfs017. [DOI] [PubMed] [Google Scholar]
- 47.Kapoor M, Schleinitz MD, Gemignani A, Wu WC. Outcomes of patients with chronic heart failure and iron deficiency treated with intravenous iron:a meta-analysis. Cardiovasc Hematol Disord Drug Targets. 2013;13:35–44. doi: 10.2174/1871529x11313010004. [DOI] [PubMed] [Google Scholar]
- 48.Jankowska EA, Tkaczyszyn M, Suchocki T, Drozd M, von Haehling S, Doehner W, et al. Effects of intravenous iron therapy in iron-deficient patients with systolic heart failure:a meta-analysis of randomized controlled trials. Eur J Heart Fail. 2016;18:786–95. doi: 10.1002/ejhf.473. [DOI] [PubMed] [Google Scholar]


