Introduction
After acute coronary syndrome (ACS), various antiplatelet agents are used to prevent stent thrombosis, death, and recurrent myocardial infarction. The currently available antiplatelet agents are clopidogrel, prasugrel, and ticagrelor. The European Society of Cardiology guidelines recommend ticagrelor as a first choice antiplatelet regimen after ACS (1).
Diffuse alveolar hemorrhage (DAH) is a very rare complication, but combined with hemoptysis, diffuse lung infiltration, and acute respiratory failure, it will be a life-threatening one. Ticagrelor and prasugrel have a faster onset and more significant platelet inhibition than clopidogrel. Although dyspnea is frequently reported in patients receiving ticagrelor, DAH due to ticagrelor use is very rare in the literature (2, 3). Thus, we present two cases of antiplatelet-related DAH occurring after ticagrelor therapy.
Case Report
A 57-year-old man was admitted to the emergency service with a disturbing chest pain spreading to the back and arms for about 4 h. His past medical history was noteworthy for hypertension, and he was taking 10 mg amlodipin once a day. Electrocardiography revealed ST segment elevation in v1-6 leads and ST segment depression in d2-3 aVF. After anterior myocardial infarction was diagnosed, 300 mg acetylsalicylic acid and 180 mg ticagrelor loading doses were given. Coronary angiography was performed, and a direct stent to the left anterior descending artery (LAD) was successfully implanted. A routine dosage of 100 U/kg unfractionated heparin was given intravenously during the intervention. Due to the successful revascularization of the occluded coronary artery, maintenance anticoagulant treatment was not given after the coronary intervention. After follow-up at the coronary intensive care unit, the patient developed acute hemoptysis on the 2nd day. There was not any obvious reason that can be related to hemoptysis. Chest X-ray on the 1st day just after coronary angiography was normal (Fig. 1a). However, bilateral diffuse interstitial infiltration was observed on X-ray and computed tomography (CT) after hemoptysis was started (Fig. 1b, 1c). Based on radiological findings, DAH due to ticagrelor emerged as the most obvious reason for hemoptysis. Ticagrelor was stopped and continuous oxygen inhalation was started at 2 L/min. On the 5th day, hemoptysis was stopped, and an improvement in radiological findings was seen on control chest X-ray (Fig. 1d). Clopidogrel instead of ticagrelor was started as the second antiaggregant therapy, and the patient was discharged from the hospital on the 7th day.
Figure 1.
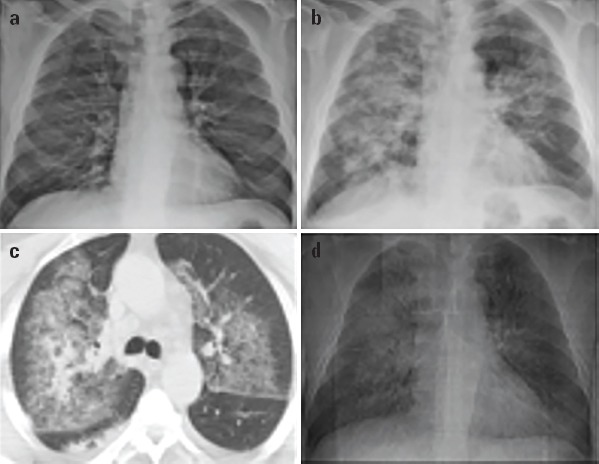
(a) Chest radiograph of the patient before hemoptysis; (b) bilateral peribronchial consolidation after acute respiratory distress; (c) thoracic computed tomography taken during acute respiratory distress; (d) improvement of pulmonary infiltrates on the 5th day
The second patient was a 64-year-old man who presented to the emergency service with a typical chest pain. His past medical history was negligible, and he was not taking any medications. Electrocardiography showed anterior myocardial infarction. Loading doses of 300 mg acetylsalicylic acid and 180 mg ticagrelor were given. Patient was taken into the catheter laboratory, and percutaneous coronary intervention to LAD was performed successfully. Before stent implantation, 100 U/kg unfractionated heparin was given. GpIIa/IIIb inhibitors were not used during or after the procedure. Due to the successful revascularization of the occluded coronary artery, maintenance anticoagulant treatment was not given after the coronary intervention. Six hours after the operation, the patient developed acute hemoptysis. A chest X-ray and thoracic CT showed bilateral peribronchial consolidation (Fig. 2a, 2b). Ticagrelor was stopped and oxygen therapy started. On the 2nd day, hemoptysis stopped, and the infiltration of the lung areas decreased on chest radiography (Fig. 1c). The patient was discharged on the 8th day with clopidogrel as the second antiplatelet regimen.
Figure 2.
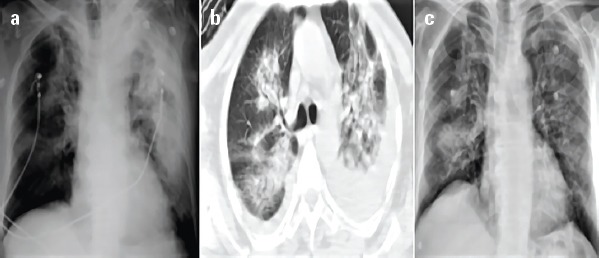
(a) Bilateral peribronchial consolidation after hemoptysis; (b) thoracic computed tomography taken during acute respiratory distress; (c) improvement of pulmonary infiltrates on the 8th day
Discussion
Alveolar hemorrhage caused by antiplatelet medication is a rare complication of ACS. There is only a limited number of case reports related to DAH due to ticagrelor in the literature before (2, 3). Yıldırım et al. (2) reported a 54-year-old man who took ticagrelor therapy due to ACS and developed DAH 4 days after ticagrelor use. However, the patient died due to septic shock on the 35th day. Whitmore et al. (3) reported a patient who used ticagrelor 90 mg BID and aspirin 100 mg daily following stenting. Their patient presented with hemoptysis, and CT imaging showed bilateral ground-glass opacities consistent with pulmonary hemorrhage. They stopped ticagrelor therapy and continued with aspirin, and DAH improved (3). These two cases were relatively more unstable than our patients after procedure. One of them had a cardiac arrest after the admission and died due to sepsis. The second one presented to the hospital with pneumonia. However, our cases were stable after coronary angiography and developed hemoptysis abruptly.
DAH is a life-threatening clinical syndrome characterized by common radiographic findings of pulmonary hemorrhage, hypoxic respiratory insufficiency, and hemoptysis. The most common causes of DAH are pulmonary capillary hypertension, systemic vasculitis (microscopic polyangiitis, Wegener granulomatosis), and rheumatologic diseases (rheumatoid arthritis, systemic lupus erythematosus). The diagnosis of DAH is based on clinical, radiographic, bronchoscopic, and pathologic examination. Sometimes, the diagnosis of DAH is made by exclusion of other reasons related to dyspnea. DAH is frequently clinically confused with acute pulmonary edema and may lead to false diagnosis.
The most probable cause of DAH in our cases was the antiplatelet action of ticagrelor. Patients were discharged from hospital with clopidogrel, and there was no bleeding event after discharge. Although clopidogrel also has an antiplatelet effect, ticagrelor has a stronger effect on platelet aggregation. This may be the explanation of hemoptysis with ticagrelor but not clopidogrel. Another explanation may be that ticagrelor induced pneumonia due to drug hypersensitivity. Histopathologic diagnosis is required for demonstrating this drug reaction. However, biopsy was not done in our patients. Therefore, exclusion of this cause is not possible at this time.
The proper treatment of DAH depends on the underlying reason. Immunosuppressive treatment is the basis of treatment in patients with DAH associated with systemic vasculitis and rheumatic diseases (4). However, there is no definitive treatment algorithm for DAH due to antiplatelet agents. First, all drugs with antiplatelet or antithrombotic effect should be cut and reversed as soon as possible. Second, oxygen, bronchodilators, intubation, and mechanical ventilation should be given.
In the present case, it is important to consider the differential diagnosis of DAH due to antithrombotic treatment. After other causes of DAH were excluded, the symptoms of DAH were improved in follow-up, and patients were discharged from hospital with transitions from ticagrelor to clopidogrel.
References
- 1.Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, et al. ESC Scientific Document Group. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2018;53:34–78. doi: 10.1093/ejcts/ezx334. [DOI] [PubMed] [Google Scholar]
- 2.Yıldırım F, Kara İ, Okuyan H, Abacı A, Türkoğlu M, Aygencel G. Diffuse alveolar hemorrhage associated with low molecular weight heparin and dual anti-platelet therapy after percutaneous coronary intervention. Clin Respir J. 2017;11:1071–3. doi: 10.1111/crj.12455. [DOI] [PubMed] [Google Scholar]
- 3.Whitmore TJ, O'Shea JP, Starac D, Edwards MG, Waterer GW. A case of pulmonary hemorrhage due to drug-induced pneumonitis secondary to ticagrelor therapy. Chest. 2014;145:639–41. doi: 10.1378/chest.13-1502. [DOI] [PubMed] [Google Scholar]
- 4.Lara AR, Schwarz MI. Diffuse alveolar hemorrhage. Chest. 2010;137:1164–71. doi: 10.1378/chest.08-2084. [DOI] [PubMed] [Google Scholar]


