Abstract
Background:
In planning high-quality research in any aspect of care for children and young people with life-limiting conditions, it is important to prioritise resources in the most appropriate areas.
Aim:
To map research priorities identified from existing research prioritisation exercises relevant to infants, children and young people with life-limiting conditions, in order to inform future research.
Design:
We undertook a systematic scoping review to identify existing research prioritisation exercises; the protocol is publicly available on the project website.
Data sources:
The bibliographic databases ASSIA, CINAHL, MEDLINE/MEDLINE In Process and Embase were searched from 2000. Relevant reference lists and websites were hand searched. Included were any consultations aimed at identifying research for the benefit of neonates, infants, children and/or young people (birth to age 25 years) with life-limiting, life-threatening or life-shortening conditions; their family, parents, carers; and/or the professional staff caring for them.
Results:
A total of 24 research prioritisation exercises met the inclusion criteria, from which 279 research questions or priority areas for health research were identified. The priorities were iteratively mapped onto an evolving framework, informed by World Health Organization classifications. This resulted in identification of 16 topic areas, 55 sub-topics and 12 sub-sub-topics.
Conclusion:
There are numerous similar and overlapping research prioritisation exercises related to children and young people with life-limiting conditions. By mapping existing research priorities in the context in which they were set, we highlight areas to focus research efforts on. Further priority setting is not required at this time unless devoted to ascertaining families’ perspectives.
Keywords: Delphi technique, consensus, infant, infant, newborn, child, adolescent, palliative care, humans
What is already known about the topic?
There is limited high-quality research in many aspects of care for infants, children and young people with life-limiting conditions.
It is important to minimise waste in research and maximise use of limited resources.
A range of research prioritisation exercises for a variety of aspects of care or conditions exist within the broad scope of this population.
What this paper adds?
This paper provides a unique overview of where and by whom a wide range of research priorities for infants, children and young people with life-limiting conditions have been agreed.
The research priorities identified are mapped in the context in which they were agreed, while common topics and themes are highlighted.
Implications for practice, theory or policy
This article presents an overview of consensus derived research priorities for infants, children and young people with life-limiting conditions, providing the opportunity for a coherent approach to improving the evidence base for this area of practice.
This study highlights the need for broader consideration of stakeholder perspectives when undertaking research prioritisation exercises.
However, further identification of research priorities cannot be justified at this time unless ascertaining the perspectives of children and young people and their families.
Background
The number of children with life-limiting or life-threatening conditions has been rising with latest figures estimating 49,000 children and young people with a life-limiting condition in the United Kingdom and approximately 21 million worldwide.1,2 These include conditions for which there is no reasonable hope of cure and from which children or young people will die, as well as conditions for which curative treatment may be feasible but can fail, such as cancer or heart failure. In children and young people, more than 300 diagnoses are life-limiting or life-threatening,3 including Duchene muscular dystrophy, severe cerebral palsy, neurodegenerative conditions and severe congenital anomalies. Although many of the individual diagnoses are rare, as a group children and young people with a life-limiting condition are a larger patient population than many other long-term conditions in children and young people, such as diabetes mellitus.4 Many of these children are living longer due to the use of medical technologies, for example, ventilation and gastrostomy feeding, and more aggressive treatment of complications and they are often high users of healthcare services.5,6 The recent UK National Institute for Health and Care Excellence guidance on End-of-life care for children and young people, although focussed on end-of-life care, highlighted the lack of evidence base on which the care of these children and young people was based.7 The recent Lancet Commission on Palliative Care and Pain Relief states that globally, nearly 2·5 million children die in need of palliative care and pain relief, and over 90% of paediatric deaths associated with serious health-related suffering are avoidable.8 The American Academy of Paediatrics guidelines and recommendations on paediatric hospice and palliative care are based on available evidence and consensus expert opinion while acknowledging the need for further clinical and health service research.9
Involving children and young people with life-limiting conditions in medical research has in the past been seen as difficult, for example, around issues of access, clinical considerations and obtaining informed consent.10 This has resulted in clinical decisions having to be based on converting the findings of research in adults to apply to children. For example, drugs are licenced for specific indications and patient groups based on the results of clinical trials, usually carried out in the adult population, age 18–65 years. It is common therefore in the absence of evidence for children to be prescribed medicines in ways that are not included in the licence. Children and young people are different biochemically and physiologically from adults, so this is not a satisfactory solution.11 However, over the last decade or so, initiatives such as the International Alliance for Better Medicines for Children in 2006 have been set up and it has become commonly agreed that children are not ‘little adults’.12 Ethical considerations have been overcome, so children and young people are encouraged to be involved in investigations into the most effective diagnoses, treatments and delivery of care specifically for them.13–15
Involving children, including those with life-limiting conditions, directly in research about their lives and the services they use is, however, more established.16–19 So the evidence base generally for all aspects of care for children and young people and understanding of what is important to patients and their families has grown. But there are still some significant gaps in terms of evidence with respect to particular populations and/or the scope, or comprehensiveness of that evidence.7,10,20
The identification of priority areas for research using consensus methods is recognised as a good way of ensuring that finite research resources are used to maximum effect.21,22 Prior knowledge and preparatory Internet searches identified a significant number of published research prioritisation exercises relevant, in varying degrees, to neonates, infants, children and young people with life-limiting conditions and their parents and carers in the United Kingdom.23–26 We therefore planned to examine the focus, context and questions identified by existing prioritisation exercises in this area by undertaking a scoping review to
Systematically identify existing research prioritisation exercises relevant to infants, children and young people with life-limiting conditions and their families and carers
Formulate the findings into a framework, mapping existing priorities
Methods
The exploratory nature of the review, the broad scope and anticipated volume of literature was suited to scoping review methods. In addition, the absence of any validated quality appraisal tools for consensus exercises precluded a systematic review. The scoping review was undertaken using systematic methods and is reported in line with the PRISMA statement.27 The review protocol was agreed and made publicly available on the Martin House Research Centre website28 prior to screening studies against inclusion criteria; scoping review protocols are not accepted for registration on PROSPERO. Amendments made to the protocol were highlighted and dated.
Eligibility criteria
Studies using any consensus consultation method were included. Studies had to include at least two rounds of consultation.
Excluded were research and development analyses and knowledge gap analyses as these are different concepts to agreeing research priorities.
There were no restrictions on the people or stakeholders undertaking the prioritisation exercise. Research prioritisation exercises aimed at identifying research for the benefit of neonates (birth to <28 days), children and/or young people (28 days to age 25) with life-limiting, life-shortening and/or life-threatening conditions; their family, parents, carers; and/or the professional staff caring for them. We used the definitions for life-limiting, life-shortening and life-threatening conditions (hereafter encompassed in the term life-limiting) adopted by Together for Short Lives:29
Life-limiting/life-shortening conditions are those for which there is no reasonable hope of cure and from which children or young people will die. Some of these conditions cause progressive deterioration rendering the child increasingly dependent on parents and carers.
Life-threatening conditions are those for which curative treatment may be feasible but can fail, such as cancer, which are also included. Children in long-term remission or following successful curative treatment are not included in this review.
Exercises seeking to identify research priorities for mixed age groups (children and/or young people and adults) were included if details of the priorities were reported separately for children and young people. Likewise, exercises setting priorities for our target age groups but not exclusively those with life-limiting conditions were included if priorities specifically related to life-limiting conditions were reported.
The outcomes of interest were the top 10 priorities for future research, such as topic areas or specific research questions presented as the main result of the consultation. Secondary lists, for example, priorities for a sub-group of participants, were excluded.
Search sources and strategy
To identify studies for inclusion, we searched ASSIA, CINAHL, MEDLINE/MEDLINE In Process and Embase. The search strategy was developed by an experienced information specialist in collaboration with the rest of the review team. The strategy consisted of thesaurus and free text terms for ‘research prioritisation’ combined (using AND) with terms for children and young people and their families. The search strategies are presented in Supplementary File 1.
The reference lists of included papers and relevant websites, such as the James Lind Alliance (JLA) Prioritisation Setting Partnership (PSP) website, were hand-searched for on-going and completed research prioritisation exercises.
There were no restrictions on the setting in which the exercise was undertaken or for the research priorities set. However, to aid generalisability to settings with similar healthcare provision, we restricted exercises to those in the English language and undertaken in Organisation for Economic Co-operation and Development countries. Healthcare, treatment and service delivery for children and young people with life-limiting conditions have changed considerably over the last few decades. In addition, the identification of priorities for future research implies that subsequent research is likely to have been undertaken. For these reasons, the searches were restricted to exercises published from 2000 to date.
Study selection and data collection
Study selection was performed independently by two researchers with discrepancies resolved through discussion or by recourse to a third researcher. Titles and abstracts were screened first, and then at second screening full papers were assessed for inclusion.
A data extraction form was designed and piloted independently by two researchers. Once finalised, one researcher data extracted the included studies and a second researcher checked 30% of the records. Discrepancies were resolved by discussion or by recourse to a third researcher.
Items data extracted were as follows: publication details, funding, aims and objectives, study country/ies, setting, health condition/s, age group, methods used to achieve consensus, degree of consensus, priorities identified and planned use of priorities.
Strategy for collating, summarising and reporting the data
We charted the data and collated, summarised and reported the results based on the enhancements of Levac et al.30 to the scoping review framework suggested by Arksey and O’Malley.31 This included the research team collectively developing the data extraction tables and discussing sequential iterations and piloting until an appropriate data set had been agreed. Simple narrative and descriptive statistics were used for reporting the included study characteristics and methods.
For the synthesis, we used the World Health Organization (WHO)-established classifications of functioning, disability and health as a starting point for developing a framework.32 Three researchers independently categorised the identified priorities into the framework. Many of the authors had grouped their questions or issues into topic areas which were also used to inform the process. Repeated discussions and iterations took place, including consideration of the factors that informed prioritisation decision-making.33
Results
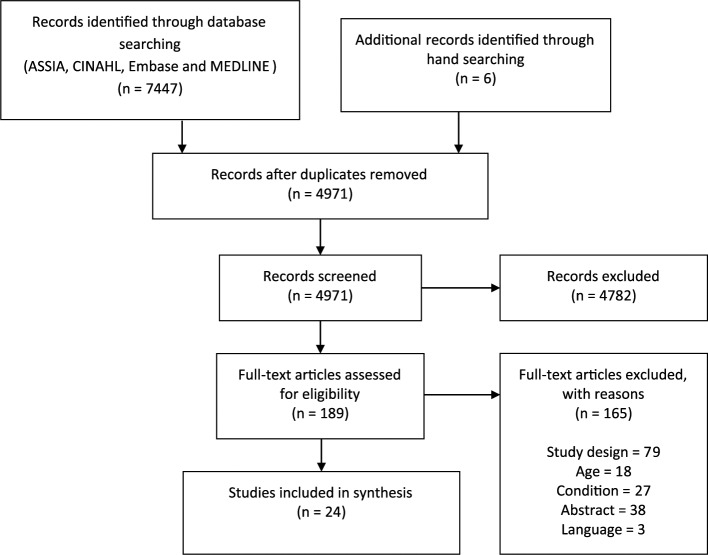
The electronic searches, run in February 2017, identified a total of 7447 records which were loaded into EndNote v7 bibliographic software and de-duplicated leaving a total of 4971 records for screening. The study flow chart is presented in Figure 1.
Figure 1.
Study flow chart.
Initial screening identified 189 records for full text assessment, from which 24 studies were found to meet the inclusion criteria. A table of characteristics of the included studies is provided in Table 1. A list of excluded studies and the full data extraction tables are available on request from the authors.
Table 1.
Characteristics of research prioritisation exercises (RPE).
| Author | Aim or purpose of the RPE (country) | Consultation method (number of rounds) | Participants in consultations | Health condition/setting | CYP age range | Format for presentation of priorities |
|---|---|---|---|---|---|---|
| Baker et al.23 | To identify and prioritise areas of paediatric palliative care research through a consensus of PPC providers and parents of patients (United States) | Delphi (4 rounds) | Parents/families: health professionals | ‘Life-threatening disease’/Paediatric palliative care | Not stated | 20 priorities grouped in 4 themes: decision making, quality improvement, care coordination to include mechanisms of support and symptom management |
| Clinton-McHarg et al.25 | Determining research priorities for young people with haematological cancer using a value-weighting approach (Australia) | Value-weighting survey method (2 stages) | Patients/CYP: parents/families: health professionals: researchers/clinical academics: AHPs: volunteers/carers/charities | Haematological cancer | Adolescents and young adults, aged between 15 and 25 years | Priorities for funding allocation grouped under four domain headings: research approach, research areas, psychosocial research and research populations |
| Morris et al.26 | To engage young people, parent carers and clinicians in a systematic process to identify and prioritise research questions regarding ways to improve the health and well-being of children and young people with neurodisability (United Kingdom) | James Lind Alliance research priority setting partnership (3 rounds) | Patients/CYP: parents/families: health professionals: researchers/clinical academics: AHPs: teachers | Neurodisability/health service and community | Children and young people (not defined) | Top 10 research questions |
| Bradley et al.34 | Objective: to identify and prioritise key research areas for AHP and nursing research in cystic fibrosis (International/Europe) | Delphi (4 rounds) | Patients/CYP: health professionals: AHPs: volunteers/carers/charities | Cystic fibrosis | Any age | 10 research themes |
| Brenner et al.35 | To identify RPs for children’s nursing in an acute care setting from the perspective of Ireland | Delphi (3 rounds) | Nurses | Any requiring acute nursing care/tertiary children’s hospital | Not reported | 27 priorities grouped in 6 themes: resuscitation concerns, clinical care concerns, end-of-life care, childhood pain, family-centred care and chronic illness |
| Downing et al.36 | To identify and prioritise global RPs for children’s palliative care | Delphi (3 rounds) | Health professionals: researchers/ clinical academics: social workers: teachers: priests | Any requiring palliative care/International Children’s Palliative Care Network | Not stated | Top 10 priorities listed (but includes 13 as 3 priorities tied on importance) with associated broad research category: psychological issues, clinical care, policies and procedures, education, clinical care, interventions and models of care, legislation and ethics, and other |
| Fletcher-Johnston et al.37 | To identify RPs of researchers and clinicians in adolescent healthcare practices across Canada in relation to healthcare transitions for children with chronic life-threatening conditions | Delphi (3 rounds) | Health professionals: researchers/clinical academics: AHPs: social workers | ‘Chronic life-threatening conditions’ | ‘Adolescents’ (RPE focuses on healthcare transitions) | Top 5 research questions |
| Liossi et al.38 | To prioritise clinical therapeutic uncertainties in paediatric pain and palliative care (United Kingdom) | Nominal Group Technique (modified) (3 decision stages) | Parents/families: Health professionals | Paediatric pain and palliative care/The Pain and Palliative Care Clinical Studies Group (CSG) (of the UK NIHR Clinical Research Network-Children) | Not stated, although final RPs cover 0–18 years | Top 10 research priorities in PICO format |
| Malcolm et al.39 | To identify and prioritise future research priorities for children’s hospice care in Scotland from the perspective of key stakeholder groups | Delphi (3 rounds) | Parents/families: health professionals: social workers: teachers: volunteers/carers/charities: policy makers: national organisations in palliative care | Any LLC/Children’s Hospice Association Scotland hospices | Not stated | Top 15 research priorities |
| Quinn et al.40 | To identify key research priorities for paediatric palliative care in Ireland | Delphi (4 rounds) | Health professionals: researchers/clinical academics | Any LLC/National University, children’s hospitals and voluntary sector | Not stated | Top 9 research priorities |
| Ramelet and Gill41 | To identify national PICU nursing research priorities in Australia and New Zealand | Delphi (3 rounds) | Nurses | Any requiring PIC nursing/PICU | Not stated (mention infants, children and adolescents) | Top 9 research priorities |
| Steele et al.42 | To achieve consensus among palliative care practitioners and researchers regarding the identification of pertinent lines of research (Canada) | Delphi (3 rounds) | Health professionals: social workers: administrator | Any requiring palliative and end-of-life care/PEDPALNET, a pan-Canadian research collaboration for paediatric palliative and end-of-life care | Not stated | 4 priority research questions |
| Tume et al.43 | To identify and prioritise nursing research topics of importance as defined by European PIC nurses | Delphi (3 rounds) | Health professionals: researchers/clinical academics | Any requiring PIC nursing care/PICU (or ICU with children) | Not reported | Top 20 research statements. Also present top 9 research domains |
| Uhm et al.44 | To discover the research questions for preterm birth and to grade them according to their importance for infants and families (United Kingdom) | Nominal Group Technique and James Lind Alliance’s five stages of prioritisation (3 rounds) | Patients/CYP: parents/families: health professionals: volunteers/carers/charities | Pre-term birth | Inferred: babies born before 32 weeks gestation | Top 15 research priority questions.a |
| Wielenga et al.45 | To identify and prioritise neonatal intensive care nursing research topics across Europe | Delphi (3 rounds) | Nurses | Any requiring NICU care/European NICU | Neonates | Top 20 research statements. Also present top 8 research domains |
| Zeigler and Decker-Walters 46 | To establish research questions and priorities in psychosocial care for adolescents with implantable cardioverter defibrillators (United States) | Delphi (3 rounds) | Health professionals: researchers/clinical academics: AHPs | Any requiring an implantable cardioverter defibrillator (ICD) | Adolescents (age range not reported) | Top 10 issues |
| Aylott47 | To identify nursing RPs in PICUs offering ECMO therapy (United Kingdom) | Delphi (3 rounds) | Nurses | Any requiring ECMO therapy/PICU | Not stated (involves mainly mature newborns) | 11 priorities grouped under 4 headings: labour intensity, consumerism, ethical dilemmas and clinical |
| de Vries et al.48 | Inform organisational decision-making and policy development regarding future research priorities and inform the wider community of the research intentions for a hospice in New Zealand | Delphi (3 rounds) | Patients/CYP: parents/families: health professionals: volunteers/carers/charities | End of life/hospice | Any age | 10 priorities (CYP family, etc.) under 4 topic headings: decision-making, bereavement and loss, symptom management, and recognition of need and response of service. 23 priorities (staff, etc.) under 6 topic headings: symptom management, aged care,b education, community, patient/family, bereavement and support for young people |
| Fochtman and Hinds 49 | To identify the nursing research priorities in a paediatric clinical trials cooperative group (United States) | Delphi (2 rounds) | Nurses | Oncology patients/Nursing Oncology Group | Paediatric (not defined) | Top 10 research priorities |
| Medlow and Patterson50 | To determine and implement priorities within Australian adolescent and young adult cancer research | Value-weighting survey method (2 stages) | Patients/ CYP: parents/families: health professionals: social workers: policy makers | Cancer | Adolescent and young adults (AYA) | Distribution of funding for research topics is displayed in 4 groupings: biomedical and clinical medicine research sub-topics, psychosocial research sub-topics, health services research sub-topics, research populations and stages of care |
| Monterosso et al.51 | Priorities for paediatric cancer nursing research in Western Australia | Delphi (2 rounds) | Nurses | Cancer/sole paediatric tertiary referral centre in Western Australia | Inferred: site caters for children age 15 years and less | Top 10 research topics overall. Also priorities for research categories; and topics important to patient care, topics important to family care and topics important to nursing |
| Soanes et al.52 | To establish nursing research priorities on a paediatric haematology, immunology oncology, and infectious diseases unit (United Kingdom) | Delphi (4 rounds) | Nurses | Cancer/paediatric oncology unit | Not stated | 21 priorities are grouped under 4 categories: nursing procedures, professional issues, psychosocial care needs and care delivery systems |
| Williams et al.53 | To identify research priorities with nurses at a tertiary children’s hospital in the United Kingdom | Nominal group technique (4 rounds) | Nurses | Any condition warranting hospital care/one tertiary children’s hospital (GOSH) | Not stated | Top 5 research themes |
| Wilson et al.54 | Identify research priorities for nursing care of infants, children and adolescents at a tertiary paediatric hospital in Western Australia | Delphi (3 rounds) | Nurses | Any condition requiring referral to a tertiary centre/sole paediatric tertiary referral centre | Infants, children and adolescents | Top 10 items overall. Also present top research topics: of greatest value to patients; of greatest value to families; and topics that would most facilitate health in CYP to reduce hospitalisation |
CYP: children and young people; PICO: population, intervention, comparator and outcome; PICU: Paediatric Intensive Care Unit; ICU: Intensive Care Unit; NICU: Neonatal Intensive Care Unit; ECMO: extracorporeal membrane oxygenation; NIHR: National Institute for Health Research; LLC: Life-Limiting Condition.
Three of the top 10 priorities excluded as relate to mothers/birth rather than care of newborn.
Priorities excluded as not relevant to CYP.
Theoretical consensus models used
The consensus method most frequently used in the included consultations was the Delphi Consensus method. The majority of consultations used questionnaires to obtain responses, mainly distributed electronically, but a few were distributed as hard copies.
Settings
Most of the consultations were undertaken in single countries. Three consultations were Europe wide, and a fourth attempted global reach. The majority of consultations were undertaken in, and for use by, centres providing specialist care such as paediatric palliative care (including hospices), neo-natal/paediatric intensive care or oncology units.
Participants in the consultations
Details of participants’ professions/roles were generally not clearly reported, but the majority were health professionals, including academic health professionals. Other participants included academics, social workers, volunteers, carers, charity staff, teachers, policy makers and priests.
Only eight studies reported including children and young people and/or parents and family members (Table 1). None of the included studies only consulted with these groups. There were some reports on the difficulties of recruiting children, young people and parents, but the majority of papers did not mention any attempts to include family members or explain why they had not.
The number of individuals taking part in a consultation exercise overall, and within individual rounds, varied considerably and not all study reports included details of numbers at every stage.
Focus for research priorities
The priority setting exercises either focussed on conditions, such as cancer or cystic fibrosis, an overarching ‘any life-limiting condition’, or a specified care need, such as requiring paediatric palliative/end-of-life care, or other therapies.
The majority of papers reported age descriptively, for example, ‘children and young adults’ or ‘paediatric’, rather than specifying an age range.
Planned use of priorities
The majority of research prioritisation exercises were undertaken with the intension of the results being used by the wider health professional and research communities.23,26,34–46 Others were undertaken to provide priorities for the benefit of funding and commissioning agencies, raising the profile of paediatric palliative care,38 ensuring the perspective of the family was considered in neonatal research.44 Eight studies were undertaken specifically to inform the research agenda of those undertaking the exercise for their particular setting.47–54
Seventeen studies referred to searching for existing prioritisation exercises in the background to their papers, either not finding any relevant to their area of interest or justifying a repeat for differences in service delivery between countries. Fourteen studies discussed the priorities identified in the context of existing research; two of these reported modifying the priorities in light of finding relevant research.
Research priorities
From the 24 studies meeting the inclusion criteria, we identified 279 research questions or priority areas for research. The majority of studies presented up to 10 top priorities, 11 listed between 12 and 33 and one listed 82 items. The range was 4–82, the average was 17 and the median was 11. Eight of the studies reported more than one final list of priorities: these were differentiated by topics, categories or by groups of participants in six cases, and in two cases, as well as ranking questions, the authors ranked research domains.
The priorities were variously called research priorities, items, themes, questions, statements or issues and were framed in different ways. We use the collective term ‘research priorities’ from here on. This ranged from detailed specific questions including population, intervention, comparator and outcome (PICO),38 to less explicit, more exploratory questions such as what is best practice for a specific stage of care.40,41 Some studies simply listed, or included, one or two word topic areas.25,34,45
Synthesis of research priorities
As the majority of studies sought to identify 10 or less research priorities, and given our objective to identify issues/topic areas considered most pressing or causing greatest concern, we limited inclusion in our synthesis of the data to a maximum of 10 of the overall top priorities reported.
This yielded a total of 279 research priorities from the included studies. Some studies presented lists of priorities under more than one category, and some had less than 10 priorities (hence the odd number). The complete list of synthesised research priorities identified by the included studies is very large and therefore presented by topic, in Supplementary File 2.
Some studies concerned specific types of service or setting (palliative, hospice and end-of life care; tertiary referral centres; oncology; and PICU and NICU). In terms of the scope of the studies with respect to diagnostic categories, they were grouped as either life-limiting conditions or cancer.
An iterative analysis of the research priorities generated 16 topic areas across which were subsumed 55 sub-topics and 12 sub-sub-topics. These are presented in Table 2 and a high-level summary of the key issues is provided here:
Table 2.
Research priority topics and sub-topics.
| Topics | Sub-topics |
|---|---|
| Epidemiology/population (including access to services) | Incidence and prevalence Access to services Needs Prevention Populations Stages of care |
| Measurement and assessment | Global outcomes (e.g. quality of life) Pain and breathlessness Sedation Antibiotics Psychosocial issues |
| Service delivery and models of care | Service delivery and models of care Settings of care: service delivery and outcomes Inpatient versus outpatient Home-based care Virtual/tele-care Joint working Shared care Care coordination and intra/multi-agency working Transitions between service or care settings Palliative and end-of-life care: service models Patient experience Safety and quality Infection control Medication errors Patient observation schedules Staff patient ratios |
| Health interventions: pharmacological and/or invasive | Active treatments for conditions or prevention of complications Minimising impacts of treatments: preparation and pre-medication Respiration and ventilation (including weaning/withdrawal) Feeding and nutrition Survivorship and late effects Fertility |
| Symptom management and control | Symptom management Pain management strategies and practices (including weaning/withdrawal) Pain: non-pharmacological interventions Pain: drug trials |
| Other interventions: physical health and functioning | Management of musculo-skeletal function Continence Communication Sleep General physical health |
| Intervention adherence | |
| Emotional and psychological issues | Coping and resilience Impacts, needs and experiences Children and young people Parents and carers Siblings Support systems and structures Interventions |
| Participation and inclusion | Preventing discrimination and exclusion Independence and young adulthood Mobility |
| Communication and decision-making | Documenting care Communication between staff/within team Communication between staff and children/parents/families Treatment and care decision-making |
| Other family needs and support | Service organisation and provision Parents as carers Supporting self-management |
| Practices related to palliative and end-of-life care | Advance care planning and preparing for death Identification of best practice |
| Bereavement | Needs and support for children and young people Needs and support for parents and other family members |
| Ethics | |
| Workforce | Retention and well-being Training and education |
| Funding research | Setting research questions Areas |
Epidemiology/population (including access to services). The need to and feasibility of collecting data; barriers and facilitators to accessing services; the needs of CYP and their parents; and strategies for health promotion.
Measurement and assessment. Understanding what quality of life means; assessment of symptoms; levels of sedation in babies; assessment of antibiotic levels; and psychosocial issues for children with cancer.
Service delivery and models of care. Best models for organisation and delivery of care; differences in quality and cost; how to maintain good governance; use of tele-care; barriers and facilitators to shared care; inter- and multi-agency collaboration; effective transfer between services; palliative care outcomes of importance to CYP and families; and effective ways to measure, prevent, record aspects of care.
Health interventions: pharmacological and/or invasive. Avoiding necrotising enterocolitis; preparing children for cancer treatment; best practice in ventilation; meeting nutritional needs; and long-term effects of cancer treatments.
Symptom management and control. Effective management of symptoms, for example, pain control, in different settings and different stages; non-pharmacological interventions; and drug trials.
Other interventions: physical health and functioning. Optimum timing and delivery of interventions; long-term safety and effectiveness of techniques to manage spasticity; achieving, or improving, continence; effective communication with CYP with neurodisability; strategies to manage sleep disturbance in CYP with neurodisability; and facilitating engagement in physical activity.
Intervention adherence. Barriers and facilitators.
Emotional and psychological issues. Factors to protect or risk factors when adjusting to living with a LLC; coping mechanisms; anxiety, breathlessness and sleeplessness as clusters; emotional and psychological challenges and experience for CYP; needs of parents, siblings and wider family; support systems and practices; and promotion of well-being.
Participation and inclusion. Promoting positive attitudes; supporting independence in terms of participation and mobility.
Communication and decision-making. Recording care; communications within multi-disciplinary teams; communications between staff and CYP and their families; and shared decision-making.
Other family needs and support. Impact on the family; support for family; support for CYP to self-manage.
Practices related to palliative and end-of-life care. Understanding and supporting parent expectations; understanding what dying well means.
Bereavement. CYP experience of and coping with bereavement; care and support needs of families.
Ethics. parental role in ethical decision-making; ethical dilemmas for staff.
Workforce. Recruitment, retention and support for staff; training to equip staff to deliver high-quality evidence-based care; and strategies to help staff communicate with CYP and their families.
Funding. Who and how research questions should be set; where funding should be targeted.
Discussion
Main findings/results of the study
In this scoping review, we aimed to map research priorities identified from existing research prioritisation exercises relevant to infants, children, and young people with life-limiting conditions. Extensive searches of bibliographic databases and hand searching identified 24 research prioritisation exercises that met the inclusion criteria. From these 279 research questions or priority areas for health research were identified. The content of these research priorities was subject to a thematic analysis which generated 16 topic areas with numerous sub-topics across these areas. This demonstrates the wide range of research priorities identified by existing studies, with major themes including medical treatments, condition and symptom management; non-medical aspects of care and support; and topics of shared interest and expertise. No single research prioritisation exercise captured the total range. This demonstrates the value of our prudent use of resources having taken the approach of a scoping review.
Given the number and diversity of life-limiting conditions and the range of services involved in their care, the large number of published exercises and identified priorities was not unexpected. While these studies generated a large volume of research priorities, it was possible to organise these into a relatively small number of overarching and meaningful topic areas.
The research prioritisation exercises included in this review were wide-ranging in terms of purpose, inclusivity of stakeholders and experts, topic areas and scope. However, a key limitation of many studies was the lack of involvement of children and young people and parents in the research prioritisation exercise or, where sought, only minimal involvement was secured.23,25,26,34,38,39,48,50 It was not possible to map the priorities by condition or by age group as we thought might be possible based on the systematic approach to undertaking research prioritisation taken by the JLA PSP.55 The rigorous methods used by the JLA set a standard to aspire to, but which are challenging even for the JLA to meet. For example, we included the JLA PSP on neurodisability, where the authors report the problems of including children and young people in the consensus process.26 An issue echoed in other studies where attempts were made. While including children and young people, parents and other family members are always likely to be challenging given the nature of the conditions concerned, it is still disappointing that so few studies reported even considering perspectives other than those of the health professionals. Even within the involvement of health professionals, this almost exclusively included doctors and nurses, with very little involvement of other relevant professions such as physiotherapists, speech and language therapists, occupational therapists, clinical psychology, and dieticians. This is concerning given the evidence from various fields that what is important to patients can be different to what is important to clinicians.56–59 Also, other professional groups outside of the healthcare sectors such as social workers, priests/chaplains and teachers may bring new insights and perspectives. A useful and efficient way forward to address this inequity and imbalance in the stakeholder groups involved in identifying research priorities to date would be to use the findings from this review as a basis for consultation with families and particular professional groups. We recently carried out such an exercise to inform and guide the work of our newly established research centre.28
The number of exercises identified may illustrate a widespread awareness of the lack of evidence in this area, and the interest in providing the evidence in a way that maximises value.22 We limited the search period from post-2000 to February 2017. It may be that some progress has been made in producing research evidence. We are aware that the JLA PSP on neurodisability has informed the commissioning of research by the UK’s National Institute for Health Research. However, within the studies included in this review, only a few reported that research priorities were limited to those where there was a known degree of uncertainty. It was beyond the remit of this review to evaluate the current evidence available against each of the topic and sub-topics identified by our synthesis.
Undertaking thorough literature searches to justify carrying out any study is good research practice. So, while this review is a valuable resource, it does not negate the need for evidence reviews to inform future research and decisions regarding the commissioning of research.
The drivers behind the production of the prioritisation exercises varied. For many, the reason for doing the exercise was specific to a profession or service at a single site. This may have been in the belief that priorities would vary between sites and professions. However, again the overlap of priorities in this scoping review demonstrates the commonality of issues that need to be addressed. When more research has been carried out and it becomes appropriate to take a fresh look at priorities, we believe a more comprehensive approach would be justified.
Strengths and weaknesses/limitations of the study
A key strength of our review is in the systematic methods used to ensure only those consultations that met our pre-specified criteria were included. Our focus on research priorities for children and young people meant we had to exclude studies that included all ages but did not present the results in a way in which we could identify those relevant to children and young people. This meant included studies where the top 10 priorities were clearly not relevant to children and young people but also somewhere they may have been relevant but not necessarily arrived at with this age group specifically in mind. For example, we had to exclude a well-conducted JLA PSP which set priorities for clinical research in primary brain and spinal cord tumours related to any age and which included paediatric representatives on the panel.60 We also excluded studies that focussed on the Emergency Department setting as generally the population and conditions presenting are very mixed and priorities therefore not focussed on children and young people with life-limiting conditions.61,62 This demonstrates the rigour of our selection process but also underlines further the extensive number of priority setting exercises closely related to the 24 studies that met our inclusion criteria.
As this is a scoping review, we have not included an appraisal of the quality of the included studies. Given the potential for consensus priorities to influence the future direction of research bids and funding, consideration should be given to the way in which the consensus has been carried out. There is extensive literature on consensus methods,33,63–66 and now on the reporting of Delphi studies in palliative care.67 In synthesising the included priorities, we used the existing recognised terminology related to children and young people with life-limiting conditions as a starting point for the framework. Although three researchers independently allocated priorities to topics in an iterative analytical process, we have to acknowledge a level of subjectivity in the synthesis. At all times, we were conscious of the need to acknowledge the drivers behind individual studies and the factors that informed the decision-making processes. For example, it was important to know who set the questions, in what context and with what degree of consensus.33
We placed no restrictions on the setting in which priorities were set. However, the epidemiology of life-limiting conditions in children, their management, the availability of services and treatments and outcomes are very different in the high resource and low-/middle-resource countries; therefore, the research priorities here will be very different. So, to aid generalisability to settings with similar healthcare provision, we restricted inclusion to those in the English language and undertaken in Organisation for Economic Co-operation and Development countries.
What this study adds
We believe this scoping review presents a unique overview of research priorities, arrived at through consensus processes, with respect to infants, children and young people with life-limiting, life-threatening and life-shortening conditions. By detailing the individual consultations and presenting our synthesis of the priorities identified, we provide evidence of the range and focus of areas for improving the evidence base for care of this population and their families. As such it provides a useful resource for researchers, professionals, funders and commissioners of research and other stakeholders involved in supporting evidence informed practice. The findings provide an opportunity at this time to maximise the use of limited research resources by focussing on filling priority evidence gaps.
Conclusion
By taking a systematic scoping approach to identification of existing research prioritisation exercises and providing transparency in our methods, we believe we present a reliable overview of the priorities already set in this area. Anyone wishing to develop a programme of research or planning a specific project could use this review as a starting point, and justification, for choosing topics or questions. Users will of course need first to check whether research has been done or is in progress, on priorities before proceeding
There are a significant number of research prioritisation exercises related to children and young people with life-limiting conditions. By mapping the priorities while being sensitive to the context in which they were set, we have achieved our aim to provide an overview of existing research priorities.
Supplemental Material
Supplemental material, 800172_Supplementary_File_1_Search_Strategies for Research prioritisation exercises related to the care of children and young people with life-limiting conditions, their parents and all those who care for them: A systematic scoping review by Alison Booth, Jane Maddison, Kath Wright, Lorna Fraser and Bryony Beresford in Palliative Medicine
Supplemental Material
Supplemental material, 800172_Supplementary_File_2_Table_of_research_priorities_by_topic for Research prioritisation exercises related to the care of children and young people with life-limiting conditions, their parents and all those who care for them: A systematic scoping review by Alison Booth, Jane Maddison, Kath Wright, Lorna Fraser and Bryony Beresford in Palliative Medicine
Acknowledgments
The team would like to thank Jenny Parry for her work obtaining copies of papers for the review. A.B. conceived the approach, all authors contributed to the design of the review and approved the protocol. K.W. developed the search strategy and ran the searches. A.B. and J.M. undertook the screening and data extraction with B.B. and L.F. providing arbitration; A.B., J.M., B.B. and L.F. synthesised the priorities identified. A.B. drafted the paper and J.M., K.W., B.B. and L.F. provided critical comments. The final version was approved by all authors.
Footnotes
Data management and sharing: The data extraction tables are available from the authors on request.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This review was undertaken as part of the Martin House Research Centre programme of work.
Research ethics and patient consent: Research ethics and consent were not required for this review of published studies.
ORCID iD: Alison Booth  https://orcid.org/0000-0001-7138-6295
https://orcid.org/0000-0001-7138-6295
References
- 1. Connor SR, Downing J, Marston J. Estimating the global need for palliative care for children: a cross-sectional analysis. J Pain Symptom Manag 2017; 53: 171–177. [DOI] [PubMed] [Google Scholar]
- 2. Fraser LK, Miller M, Hain R, et al. Rising national prevalence of life-limiting conditions in children in England. Pediatrics 2012; 129: e923–e929. [DOI] [PubMed] [Google Scholar]
- 3. Hain R, Devins M, Hastings R, et al. Paediatric palliative care: development and pilot study of a ‘Directory’ of life-limiting conditions. BMC Palliat Care 2013; 12: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Royal College of Paediatrics and Child Health. National paediatric diabetes audit. London: Royal College of Paediatrics and Child Health, 2014. [Google Scholar]
- 5. Feudtner C, DiGiuseppe DL, Neff JM. Hospital care for children and young adults in the last year of life: a population-based study. BMC Med 2003; 1: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ananth P, Melvin P, Feudtner C, et al. Hospital use in the last year of life for children with life-threatening complex chronic conditions. Pediatrics 2015; 136: 938–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. National Institute for Health and Care Excellence (NICE). End of life care for infants, children and young people with life-limiting conditions: planning and management. London: NICE, 2016. [PubMed] [Google Scholar]
- 8. Knaul FM, Bhadelia A, Rodriguez NM, et al. The Lancet Commission on Palliative Care and Pain Relief – findings, recommendations, and future directions. Lancet Glob Health 2018; 6: S5–S6. [Google Scholar]
- 9. American Academy of Pediatrics Policy Statement. Pediatric Palliative Care and Hospice Care Commitments, Guidelines, and Recommendations. Section on hospice and palliative medicine and committee on hospital care. Pediatrics 2013; 132: 966. [DOI] [PubMed] [Google Scholar]
- 10. Hudson BF, Oostendorp LJ, Candy B, et al. The under reporting of recruitment strategies in research with children with life-threatening illnesses: a systematic review. Palliat Med 2017; 31: 419–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bourns IM. Unlicensed medicines in the UK – legal frameworks, risks, and their management. Med Access@Point Care 2017; 1: e22–e28. [Google Scholar]
- 12. Gazarian M. Delivering better medicines to children: need for better integration between the science, the policy, and the practice. Paediatr Drugs 2009; 11: 41–44. [DOI] [PubMed] [Google Scholar]
- 13. Blyth CC, Chen SC, Slavin MA, et al. Not just little adults: candidemia epidemiology, molecular characterization, and antifungal susceptibility in neonatal and pediatric patients. Pediatrics 2009; 123: 1360–1368. [DOI] [PubMed] [Google Scholar]
- 14. Einarsdóttir J. Research with children: methodological and ethical challenges. Eur Early Child Educ 2007; 15: 197–211. [Google Scholar]
- 15. World Health Organisation. Children are not little adults. In: Children’s environmental health training modules, June 2016, www.who.int/ceh/capacity/training_modules/en/
- 16. Coyne I, Sheehan A, Heery E, et al. Improving transition to adult healthcare for young people with cystic fibrosis: a systematic review. J Child Health Care 2017; 21: 312–330. [DOI] [PubMed] [Google Scholar]
- 17. Ambresin AE, Bennett K, Patton GC, et al. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. J Adolescent Health 2013; 52: 670–681. [DOI] [PubMed] [Google Scholar]
- 18. Beresford B, Stuttard L. Young adults as users of adult healthcare: experiences of young adults with complex or life-limiting conditions. Clin Med 2014; 14: 404–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gibson F, Aldiss S, Horstman M, et al. Children and young people’s experiences of cancer care: a qualitative research study using participatory methods. Int J Nurs Stud 2010; 47: 1397–1407. [DOI] [PubMed] [Google Scholar]
- 20. Simpson LA, Peterson L, Lannon CM, et al. Special challenges in comparative effectiveness research on children’s and adolescents’ health. Health Affair 2010; 29: 1849–1856. [DOI] [PubMed] [Google Scholar]
- 21. Cuello-García CA. Setting research priorities to avoid waste – the time is right. J Pediatr 2015; 167: 219–221. [Google Scholar]
- 22. Chalmers I, Bracken MB, Djulbegovic B, et al. How to increase value and reduce waste when research priorities are set. Lancet 2014; 383: 156–165. [DOI] [PubMed] [Google Scholar]
- 23. Baker JN, Levine DR, Hinds PS, et al. Research priorities in pediatric palliative care. J Pediatr 2015; 167: 467–470.e463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Browne LR, Shah MI, Studnek JR, et al. 2015 pediatric research priorities in prehospital care. Prehosp Emerg Care 2016; 20: 311–316. [DOI] [PubMed] [Google Scholar]
- 25. Clinton-McHarg T, Paul C, Sanson-Fisher R, et al. Determining research priorities for young people with haematological cancer: a value-weighting approach. Eur J Cancer 2010; 46: 3263–3270. [DOI] [PubMed] [Google Scholar]
- 26. Morris C, Simkiss D, Busk M, et al. Setting research priorities to improve the health of children and young people with neurodisability: a British Academy of Childhood Disability-James Lind Alliance Research Priority Setting Partnership. BMJ Open 2015; 5: e006233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Martin House Research Centre. Research prioritisation exercise – Martin House Research Centre, https://www.york.ac.uk/healthsciences/research/public-health/projects/martinhouse/projects/prior-exercise/ (2017, accessed 19 December 2017).
- 29. Together for Short Lives. Definitions for terms and phrases used in children’s palliative care, http://www.togetherforshortlives.org.uk/professionals/childrens_palliative_care_essentials/definitions (2017, accessed 06 March 2017).
- 30. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010; 5: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method 2005; 8: 19–32. [Google Scholar]
- 32. World Health Organisation. International Classification of Functioning, Disability and Health (ICF), http://www.who.int/classifications/icf/en/ (accessed 20 December 2017).
- 33. Lomas J, Fulop N, Gagnon D, et al. On being a good listener: setting priorities for applied health services research. Milbank Q 2003; 81: 363–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bradley JM, Madge S, Morton AM, et al. Cystic fibrosis research in allied health and nursing professions. J Cyst Fibros 2012; 11: 387–392. [DOI] [PubMed] [Google Scholar]
- 35. Brenner M, Hilliard C, Regan G, et al. Research priorities for children’s nursing in Ireland: a Delphi study. J Pediatr Nurs 2014; 29: 301–308. [DOI] [PubMed] [Google Scholar]
- 36. Downing J, Knapp C, Muckaden MA, et al. Priorities for global research into children’s palliative care: results of an International Delphi Study. BMC Palliat Care 2015; 14: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fletcher-Johnston M, Marshall SK, Straatman L. Healthcare transitions for adolescents with chronic life-threatening conditions using a Delphi method to identify research priorities for clinicians and academics in Canada. Child Care Hlth Dev 2011; 37: 875–882. [DOI] [PubMed] [Google Scholar]
- 38. Liossi C, Anderson A-K, Howard RF. Development of research priorities in paediatric pain and palliative care. Br J Pain 2016; 11: 9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Malcolm C, Knighting K, Forbat L, et al. Prioritization of future research topics for children’s hospice care by its key stakeholders: a Delphi study. Palliat Med 2009; 23: 398–405. [DOI] [PubMed] [Google Scholar]
- 40. Quinn C, McCarthy S, Devins M, et al. Prioritisation of future research topics in paediatric palliative care in Ireland: a Delphi study. Int J Palliat Nurs 2017; 23: 88–97. [DOI] [PubMed] [Google Scholar]
- 41. Ramelet AS, Gill F. A Delphi study on National PICU nursing research priorities in Australia and New Zealand. Aust Crit Care 2012; 25: 41–57. [DOI] [PubMed] [Google Scholar]
- 42. Steele R, Bosma H, Johnston MF, et al. Research priorities in pediatric palliative care: a Delphi study. J Palliat Care 2008; 24: 229–239. [PubMed] [Google Scholar]
- 43. Tume LN, van den Hoogen A, Wielenga JM, et al. An electronic Delphi study to establish pediatric intensive care nursing research priorities in twenty European countries. Pediatr Crit Care Med 2014; 15: e206–e213. [DOI] [PubMed] [Google Scholar]
- 44. Uhm S, Crowe S, Dowling I, et al. The process and outcomes of setting research priorities about preterm birth – a collaborative partnership. Infant 2014; 10: 178–181. [Google Scholar]
- 45. Wielenga JM, Tume LN, Latour JM, et al. European neonatal intensive care nursing research priorities: an e-Delphi study. Arch Dis Child Fetal Neonatal Ed 2015; 100: F66–F71. [DOI] [PubMed] [Google Scholar]
- 46. Zeigler VL, Decker-Walters B. Determining psychosocial research priorities for adolescents with implantable cardioverter defibrillators using Delphi methodology. J Cardiovasc Nurs 2010; 25: 398–404. [DOI] [PubMed] [Google Scholar]
- 47. Aylott M. Research priorities: a Delphi survey. Paediatr Nurs 2000; 12: 16–20. [Google Scholar]
- 48. de Vries K, Walton J, Nelson K, et al. An examination of the research priorities for a hospice service in New Zealand: a Delphi study. Palliat Support Care 2016; 14: 232–240. [DOI] [PubMed] [Google Scholar]
- 49. Fochtman D, Hinds PS. Identifying nursing research priorities in a pediatric clinical trials cooperative group: the Pediatric Oncology Group experience. J Pediatr Oncol Nurs 2000; 17: 83–87. [DOI] [PubMed] [Google Scholar]
- 50. Medlow S, Patterson P. Determining research priorities for adolescent and young adult cancer in Australia. Eur J Cancer Care 2015; 24: 590–599. [DOI] [PubMed] [Google Scholar]
- 51. Monterosso L, Dadd G, Ranson K, et al. Priorities for paediatric cancer nursing research in Western Australia: a Delphi study. [Erratum appears in Contemp Nurse 2002 Apr;12(2):135]. Contemp Nurse 2001; 11: 142–152. [DOI] [PubMed] [Google Scholar]
- 52. Soanes L, Gibson F, Bayliss J, et al. Establishing nursing research priorities on a paediatric haematology, oncology, immunology and infectious diseases unit: a Delphi survey. Eur J Oncol Nurs 2000; 4: 108–117. [DOI] [PubMed] [Google Scholar]
- 53. Williams A, Sell D, Oulton K, et al. Identifying research priorities with nurses at a tertiary children’s hospital in the United Kingdom. Child Care Hlth Dev 2017; 43: 211–221. [DOI] [PubMed] [Google Scholar]
- 54. Wilson S, Ramelet AS, Zuiderduyn S. Research priorities for nursing care of infants, children and adolescents: a West Australian Delphi study. J Clin Nurs 2010; 19: 1919–1928. [DOI] [PubMed] [Google Scholar]
- 55. James Lind Alliance Priority Setting Partnerships NETSCC Team and Cowan K. The James Lind Alliance guidebook (Version 6), February 2016. Southampton: James Lind Alliance. [Google Scholar]
- 56. Haywood KL, Collin SM, Crawley E. Assessing severity of illness and outcomes of treatment in children with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME): a systematic review of patient-reported outcome measures (PROMs). Child Care Hlth Dev 2014; 40: 806–824. [DOI] [PubMed] [Google Scholar]
- 57. Michener LA. Patient- and clinician-rated outcome measures for clinical decision making in rehabilitation. J Sport Rehabil 2011; 20: 37–45. [DOI] [PubMed] [Google Scholar]
- 58. Kirwan JR, Newman S, Tugwell PS, et al. Progress on incorporating the patient perspective in outcome assessment in rheumatology and the emergence of life impact measures at OMERACT 9. J Rheumatol 2009; 36: 2071–2076. [DOI] [PubMed] [Google Scholar]
- 59. Serrano-Aguilar P, Trujillo-Martin MM, Ramos-Goni JM, et al. Patient involvement in health research: a contribution to a systematic review on the effectiveness of treatments for degenerative ataxias. Soc Sci Med 2009; 69: 920–925. [DOI] [PubMed] [Google Scholar]
- 60. MacDonald L. Top 10 priorities for clinical research in primary brain and spinal cord. Final report of the Neuro-oncology Group Priority Setting Partnership in Neuro-Oncology, June 2015. Southampton: James Lind Alliance. [Google Scholar]
- 61. Hartshorn S, O’Sullivan R, Maconochie IK, et al. Establishing the research priorities of paediatric emergency medicine clinicians in the UK and Ireland. Emerg Med J 2015; 32: 864–868. [DOI] [PubMed] [Google Scholar]
- 62. Quest TE, Asplin BR, Cairns CB, et al. Research priorities for palliative and end-of-life care in the emergency setting. Acad Emerg Med 2011; 18: e70–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Practical Assess Res Eval 2007; 12(10): 1–8. [Google Scholar]
- 64. Murphy MK, Black NA, Lamping DL, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Asses 1998; 2: i–iv, 1–88. [PubMed] [Google Scholar]
- 65. Sinha IP, Smyth RL, Williamson PR. Using the Delphi technique to determine which outcomes to measure in clinical trials: recommendations for the future based on a systematic review of existing studies. PLoS Med 2011; 8: e1000393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Viergever RF, Olifson S, Ghaffar A, et al. A checklist for health research priority setting: nine common themes of good practice. Health Res Policy Sy 2010; 8: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Junger S, Payne SA, Brine J, et al. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med 2017; 31: 684–706. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 800172_Supplementary_File_1_Search_Strategies for Research prioritisation exercises related to the care of children and young people with life-limiting conditions, their parents and all those who care for them: A systematic scoping review by Alison Booth, Jane Maddison, Kath Wright, Lorna Fraser and Bryony Beresford in Palliative Medicine
Supplemental material, 800172_Supplementary_File_2_Table_of_research_priorities_by_topic for Research prioritisation exercises related to the care of children and young people with life-limiting conditions, their parents and all those who care for them: A systematic scoping review by Alison Booth, Jane Maddison, Kath Wright, Lorna Fraser and Bryony Beresford in Palliative Medicine