Abstract
Since 2014, average premiums for health plans available in the Affordable Care Act marketplaces have increased. We examine how premium price changes affected the amount consumers pay after subsidies for the lowest-cost bronze and silver plans available by age in the federally facilitated exchanges. Between 2015 and 2016, benchmark plan premiums increased in 83.3% of counties. Overall, rising benchmark premiums were associated with lower average after-subsidy premiums for the lowest-cost bronze and silver plans for older subsidy-eligible adults, but with higher after-subsidy premiums for younger adults purchasing the same plans, regardless of income. With recent discussions to replace or overhaul the Affordable Care Act, it is critical that we learn from the successes and failures of the current policy. Our findings suggest that the subsidy design, which makes rising premiums costlier for younger adults looking to purchase an entry-level plan, may be contributing to adverse selection and instability in the marketplace.
Keywords: Patient Protection and Affordable Care Act, health insurance exchanges, insurance pools
Introduction
Starting in 2014, the Patient Protection and Affordable Care Act (ACA) established marketplaces where consumers could easily compare and purchase health insurance plans. To increase the affordability of premiums, subsidies are available to individuals as advance tax credits based on their income and the benchmark plan premium (i.e., the silver plan with the second-lowest premium in their area). The ultimate goal of the policy is to ensure access to affordable quality care for all, with a particular emphasis on preventive care (U.S. Department of Health & Human Services, 2016). Since the ACA aims to give more Americans access to affordable, quality health insurance, it is crucial to understand how changes in unsubsidized premiums affect how much consumers actually pay for entry-level plans after subsidies. We focused our analysis on the lowest-cost bronze plan because individuals without access to an affordable bronze plan are exempt from the mandate under ACA, and consumers generally overemphasize premiums when choosing an insurance plan, making the lowest-cost bronze plan the most appealing entry-level plan for many adults (Abaluck & Gruber, 2011; Spranca et al., 2000). In addition, we also examined the lowest-cost silver plan, which had the highest enrollment of any plan in the marketplace (Hodges, 2016). Overall, 23% of marketplace enrollees chose bronze plans in 2016 and 20% chose the lowest-cost silver plan (Hodges, 2016; Office of the Assistant Secretary for Planning and Evaluation, 2016).
New Contribution
It has been widely reported that insurance rates for benchmark plans available in the federally facilitated marketplaces increased by an average of 22% in 2017. Many articles have also noted that when premiums increase, so do subsidies (Gabel et al., 2017; J. Hsu, Overhage, Price, Fung, & Newhouse, 2016). How changes in premiums affect consumers of various ages, however, is still somewhat unclear and vitally important, since attracting sufficient numbers of younger, healthier individuals is crucial to achieving a balanced risk pool and curtailing continued premium growth. In a previous analysis, we showed that younger individuals with lower income often pay as much or more than older individuals for bronze plans (Graetz, Kaplan, Kaplan, Bailey, & Waters, 2014). In this article, we examine how market trends in premium prices affect the after-subsidy premium for the lowest-cost bronze and silver plans offered in the federal marketplaces between 2015 and 2016 for older and younger adults by income.
Method
Marketplace Overview
Marketplace plans are categorized into four metal levels (bronze, silver, gold, and platinum) based on the percentage of health care costs that the plan expects to pay for the average enrollee. Bronze plans have the lowest premiums, but the highest out-of-pocket cost-sharing amounts. Households with incomes between 100% and 400% of the federal poverty level (FPL) qualify for premium subsidies. Premium subsidies are calculated so that the benchmark plan can be purchased using a fixed percentage of income. Therefore, if benchmark premiums increase, the subsidy amounts that eligible individuals can receive will also increase. A subsidy can be used to purchase any marketplace plan. In addition to premium subsidies, households with incomes between 100% and 250% FPL are eligible to receive additional cost-sharing subsidies if they enroll in a silver plan.
We focused our analysis on the lowest-cost bronze and silver plans for several reasons. First, individuals without access to an affordable bronze plan are exempt from the mandate under the ACA. Second, since bronze plans are the least expensive plans, marginal marketplace participants are likely trying to decide between purchasing a bronze plan or paying the penalty for not having coverage. Third, silver plans have the highest enrollment in the marketplace overall, and the lowest-cost silver plan had the highest enrollment of any plan, across all metal levels (Hodges, 2016; Office of the Assistant Secretary for Planning and Evaluation, 2016). One reason for this may be the cost-sharing subsidies that are only available for silver plans. Finally, in case the lowest-cost bronze plan was an outlier with respect to other bronze plans, we included a sensitivity analysis using the second lowest-cost bronze plan in the county (see Appendix A).
Data
We obtained plan premium data for nontobacco users for all plans across all U.S. counties in states participating in the federally facilitated marketplaces (34 states) in 2015 and 2016 (Centers for Medicare & Medicaid Services, 2015).
Analyses
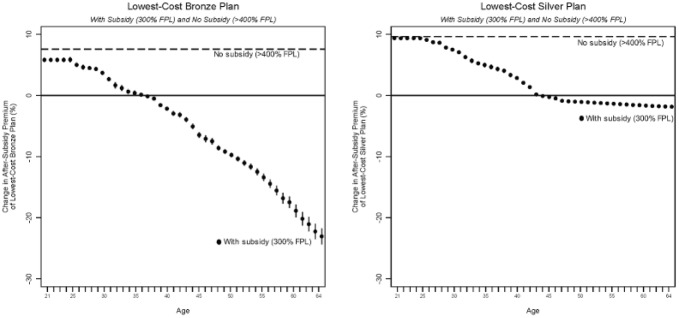
To determine the after-subsidy premium amount that individuals would pay for a bronze or silver plan, we subtracted the subsidy amount from the relevant plan premium for various ages and income levels. Methods used to calculate subsidies and after-subsidy premiums are explained in detail in our previous article (Graetz et al., 2014). Theoretically, the after-subsidy premium for the lowest-cost bronze and silver plan could move in the same or a different direction as the benchmark premium, since subsidies change according to the benchmark premium. To examine this relationship, we used quantile regression to measure the median percent change in the after-subsidy premium associated with a 10% increase in the benchmark plan premium for both the lowest-cost bronze and silver plans between 2015 and 2016. To examine how benchmark premium changes affected consumers differently based on income level and age, separate quantile regressions were estimated for adults for each age between 21 and 64 who were either subsidy-eligible (300% FPL) or not subsidy-eligible (>400% FPL). Results from the quantile regression models for each age are shown as a graph in Figure 1. All data analyses were conducted using Stata software, Version 14.2 (StataCorp LLC, College Station, TX).
Figure 1.
Percent change in after-subsidy premium for the lowest-cost bronze and silver plans associated with a 10% increase in benchmark plan premium: With subsidy (300% FPL) versus no subsidy (>400% FPL) for individuals aged 21 to 64 years old.
Note. The dashed line represents percent change for individuals with incomes above 400% FPL (i.e., not subsidy-eligible), and circles represent the associated change and 95% confidence intervals for individuals with incomes at 300% FPL. FPL is the federal poverty level. In 2016, 300% FPL was $35,310 for an individual and $72,750 for a family of four; 400% FPL was $47,080 for an individual and $97,000 for a family of four. We used a linear model to measure the percent change in the after-subsidy premium for the lowest-cost bronze and silver plans associated with a 10% increase in benchmark plan premiums between 2015 and 2016. The figure shows the results from 43 models for each age from 21 to 64.
Results
Table 1 shows the average premium and deductible amounts for a 27-year-old and 60-year-old nontobacco user in 2015, and the average change between 2015 and 2016. Overall, premiums for the lowest-cost bronze plan increased by 15.8% and benchmark plan premiums increased by 11.5%. Between 2015 and 2016, benchmark plan premiums increased in 83.3% of counties. Among these counties, almost all (99.6%) also had an increase in the lowest-cost bronze plan premium. For enrollees who received subsidies in 2015, the subsidy increase was the same as the change in the benchmark premiums. However, many younger subsidy-eligible adults did not receive subsidies because the benchmark plan premium fell below the subsidy cap. In these counties, only 7.3% of 27-year-olds with a household income of 300% FPL actually received a subsidy in 2015, while 100% of 60-year-olds with the same income received a subsidy. Thus, for subsidy-eligible individuals, the average subsidy change for a 27-year-old was $9.45, much less than the $35.90 increase in the benchmark premium. For 60-year-olds the average benchmark premium and subsidy increased by the same amount, $92.53. Premiums for the lowest-cost bronze plan, before subsidies, increased by $33.68 and $86.89 for a 27-year-old and 60-year-old, respectively. Consequently, a subsidy-eligible 27-year-old faced an average increase of $24.23 in the after-subsidy premium of the lowest-cost bronze plan, while a subsidy-eligible 60-year-old faced an average decrease of $5.64 for the same plan.
Table 1.
2015-2016 Premiums and Medical Deductibles for the Lowest-Cost Bronze and Silver Plans, and the Benchmark Plan.
| Overall | Benchmark increased | Benchmark decreased | |
|---|---|---|---|
| Counties, n (%) | 2,512 (100%) | 2,092 (83.3%) | 420 (16.7%) |
| 2015 Mean plan premium: 27-year-old | |||
| Lowest-cost bronze plan | $181.14 | $178.98 | $191.89 |
| Lowest-cost silver plan | $226.25 | $223.59 | $239.50 |
| Second lowest-cost silver plan (Benchmark) | $234.89 | $231.69 | $250.85 |
| 2015-2016 Mean change in plan premium: 27-year-old | |||
| Lowest-cost bronze plan | $28.61 | $33.68 | $3.35 |
| Lowest-cost silver plan | $26.97 | $35.18 | −$13.96 |
| Second lowest-cost silver plan (Benchmark) | $27.04 | $35.90 | −$17.11 |
| 2015-2016 Mean change in subsidy: 300% FPL | $7.63 | $9.45 | −$1.41 |
| 2015 Mean plan premium: 60-year-old | |||
| Lowest-cost bronze plan | $466.74 | $460.67 | $496.94 |
| Lowest-cost silver plan | $583.17 | $575.73 | $620.22 |
| Second lowest-cost silver plan (Benchmark) | $605.52 | $596.67 | $649.62 |
| 2015-2016 Mean change in plan premium: 60-year-old | |||
| Lowest-cost bronze plan | $73.81 | $86.89 | $8.68 |
| Lowest-cost silver plan | $69.53 | $90.74 | −$36.13 |
| Second lowest-cost silver plan (Benchmark) | $69.66 | $92.53 | −$44.30 |
| 2015-2016 Mean change in subsidy: 300% FPL | $69.65 | $92.53 | −$44.30 |
| 2015-2016 Percent change in plan premium: All ages | |||
| Lowest-cost bronze plan | 15.8% | 18.9% | 1.7% |
| Lowest-cost silver plan | 11.9% | 15.8% | −5.8% |
| Second lowest-cost silver plan (Benchmark) | 11.5% | 15.5% | −6.8% |
| 2015 Mean medical deductible: All ages | |||
| Lowest-cost bronze plan | $5,843.76 | $5,782.48 | $6,148.99 |
| Lowest-cost silver plan | $3,569.49 | $3,545.60 | $3,688.45 |
| Second lowest-cost silver plan (Benchmark) | $3,138.02 | $3,116.78 | $3,243.81 |
| 2015-2016 Percent change in medical deductible: All ages | |||
| Lowest-cost bronze plan | 3.6% | 3.9% | 1.9% |
| Lowest-cost silver plan | 6.2% | 3.0% | 21.6% |
| Second lowest-cost silver plan (Benchmark) | 3.8% | 0.6% | 19.1% |
Note. FPL = federal poverty level. Premium amounts shown are for nontobacco users.
In the 16.7% of counties where the benchmark premiums decreased, monthly subsidies decreased by an average of $1.41 and $44.31 for individuals aged 27 and 60 years, respectively. Among these counties, the lowest-cost bronze plan premium decreased in fewer than half of counties (37.5%), and the average monthly premium actually increased by $3.35 and $8.68 for individuals aged 27 and 60 years, respectively. Thus, subsidy-eligible individuals who purchased lowest-cost bronze plans in counties where benchmark premiums decreased faced an average increase in their monthly after-subsidy premium of $4.76 and $52.98 for ages 27 and 60, respectively. Similar patterns were observed for individuals who enrolled in the second lowest-cost bronze plan (shown in Appendix Table A1) and lowest-cost silver plan (Table 1).
In addition to premiums, medical deductible amounts, which represent a large share of beneficiaries’ cost-sharing, also faced average increases. The lowest-cost bronze plan had the highest average deductible in 2015 compared to other plans, approximately $5,844, and this amount increased by 3.6% in 2016. With the exception of the lowest-cost bronze plan, counties that had decreases in the benchmark plan premium had much higher increases in the deductible amounts between 2015 and 2016 (Table 1).
Figure 1 shows the median percent change in the after-subsidy premium for the lowest-cost bronze and silver plan associated with a 10% increase in the benchmark plan premium for ages 21 to 64 years. In the figure, the dashed line represents after-subsidy changes for individuals who were not subsidy-eligible, with incomes at or above 400% FPL, and the circles represent changes for those who were subsidy-eligible, with incomes at 300% FPL. For individuals not eligible for subsidies, increases in the benchmark premium were always associated with increases in the median bronze and silver premiums. For subsidy-eligible individuals, the patterns were similar at both metal levels, where a 10% increase in the benchmark premium was associated with a median increase in the after-subsidy premium for younger enrollees, but a decrease in the after-subsidy premium for older enrollees. For example, for individuals not receiving subsidies (≥400% FPL), a 10% increase in the monthly benchmark premium was associated with a 7.2% (95% confidence interval [CI]: [7.0, 7.4]) and 9.6% (95% CI: [9.5, 9.8]) increase in the lowest-cost bronze and silver plan premiums for all adults (ages 21 to 64). The same 10% increase for a subsidy-eligible consumer was associated with a median increase of 3.9% (95% CI: [3.6, 4.3]) and 7.0% (95% CI: [6.7, 7.2]) in the after-subsidy premium of the lowest-cost bronze and silver plan for a 27-year-old, but a decrease of 19.2% (95% CI: [−20.1, −18.2]) and 2.2% (95% CI: [−2.5, −1.9]) in the after-subsidy premiums for a 60-year-old.
Discussion
Our analysis demonstrates that consumers were affected differently by premium changes depending on their age and income level. For older consumers receiving subsidies, rising benchmark premiums were associated with lower after-subsidy premiums for the lowest-cost bronze and silver plans. This was because, on average, the subsidy amount that they received increased by a greater amount than the increase in the lowest-cost bronze and silver plan premium. However, younger subsidy-eligible consumers experienced higher average after-subsidy premiums for these same plans, despite the fact that subsidies increased along with benchmark premiums. In the 17% of counties with falling benchmark premiums, average premiums for the lowest-cost bronze plan increased. As a result, subsidy-eligible individuals purchasing a bronze plan in these counties faced higher after-subsidy premiums.
Due to complex subsidy calculations, increases in benchmark premiums will lead to decreases in after-subsidy premium costs if the increase in the premium for the benchmark plan is larger than the increase in the premium of the plan that is purchased. If on average all plans have the same percentage increase from year to year, this would mean that the average subsidy increase (amount) would be greater than the increase in premiums for any plan that is cheaper than the benchmark plan. Thus, increasing premiums could benefit consumers who receive a subsidy and choose any plan that is cheaper than the benchmark, including the lowest-cost silver plan or any bronze plan. Because benchmark premiums for younger consumers are often lower than the subsidy cap, many young adults with subsidy-eligible incomes (100% to 400% FPL) do not receive any monthly premium subsidy (Graetz et al., 2014). Thus, when premiums go up for subsidy-eligible young adults whose premiums fall below the cap, unlike their older counterparts, they do not always benefit from higher subsidies.
According to the Department of Health and Human Services, more than 87% of individuals who enrolled in a 2015 plan through the federal health insurance marketplace qualified for a federal premium subsidy (Office of the Assistant Secretary for Planning and Evaluation, 2015). A recent analysis of ACA coverage effects found that premium subsidies were responsible for 40% of the gains in coverage, suggesting that after-subsidy costs are an important driver of enrollment (Frean, Gruber, & Sommers, 2016). Thus, the majority of older individuals who enrolled in a bronze plan or the lowest-cost silver plan in 2016 were better off in counties where benchmark plan premium prices increased. Conversely, younger adults who enrolled in the same plans faced higher average after-subsidy premium costs, regardless of changes in the benchmark premium or their income. Consumers of all ages not receiving subsidies were worse off in counties where benchmark premiums increased. Finally, although some individuals actually benefitted from increasing premiums, taxpayers did not—increasing benchmark plan premiums result in higher subsidy amounts and, thus, in higher federal costs. This in an important point, as the long-term sustainability of the marketplaces depends not only on the affordability of insurance for individual consumers but also the affordability of the program for the government (Hsu, 2016).
Our findings suggest that the current construction of subsidies may be fueling an adverse selection process (Cutler & Zeckhauser, 2000) that is destabilizing the ACA marketplaces. To achieve a balanced risk pool and curtail continued premium growth, the ACA marketplaces need to attract sufficient numbers of younger, healthier individuals. With each successive annual round of premium increases, after-subsidy premium prices will attract older members and drive out younger persons, leading to additional premium increases. Without a significant change in the subsidy structure, this “un-virtuous” spiral will continue.
For example, subsidies are currently designed so that a 27-year-old and a 60-year-old earning 300% FPL are expected to pay up to 9.5% of their income to purchase a benchmark plan. While this amount may be reasonable for older or sicker individuals who expect to have relatively high use of health care services, it may be too costly for younger healthier adults, who foresee low need for health care, and may be mostly driven by the desire to avoid penalties. Our previous finding, which showed that subsidies distort the age curve by making it more expensive for younger, lower income consumers to purchase entry-level plans relative to older consumers (Graetz et al., 2014), combined with our current finding that rising premiums are more costly for younger adults, raises serious concerns over the design of premium subsidies and the long-term sustainability of the ACA marketplaces.
Our analyses of the current premium subsidy design can inform ongoing discussions on how to improve the affordability of health insurance plans via the use of premium subsidies. Specifically, to maintain a more balanced risk-pool, the premium subsidy design should lower costs for younger, healthier, subsidy-eligible individuals who typically have lower demand for health care services relative to older adults. Possible ways to encourage greater enrollment among younger, healthier adults in marketplace plans include making the premium subsidy amount tied to the lowest-cost bronze plan instead of the second lowest-cost silver plan or adjusting subsidy amounts by age to deliberately make it cheaper for younger adults to enroll.
Our study has a few limitations. First, we focused our primary analysis on the lowest-cost bronze and silver plan. However, we conducted additional sensitivity analyses using the second lowest-cost bronze plan and found similar results (see Appendix A). Overall, we expect these trends to be similar for consumers choosing any plan that is cheaper than the benchmark plan. Second, our analysis focuses exclusively on premium costs and medical deductibles, and does not include other types of cost-sharing. However, since marketplace plans are categorized by the expected percentage of costs covered by the plan, while the cost-sharing structure may change, we do not expect the overall cost-sharing amounts to change significantly from year to year. Third, because we did not have complete premium data for the state-facilitated marketplaces, we were unable include them in our analysis.
In conclusion, we found that rising premiums in the marketplaces affected consumers differently depending on their age and their income. Rising premiums are costlier for younger adults, who faced average higher after-subsidy premium costs regardless of their income, while older subsidy-eligible adults actually benefit from rising premiums. As a result, this feature of the subsidy design may be contributing to adverse selection and instability in the marketplaces. Given current efforts to repeal or repair the ACA, it is critical that we learn from the successes and failures of the ACA in order to inform future policies. Our findings suggest that policies aimed at curbing premium increases and encouraging health insurance enrollment through subsidies should be devised in a way that curtails adverse selection, not encourages it.
Appendix A
Table A1.
2015-2016 Premiums and Medical Deductibles for the Second Lowest-Cost Bronze and Silver Plans.
| Overall | Benchmark increased | Benchmark decreased | |
|---|---|---|---|
| Counties, n (%) | 100% | 2092 (83.3%) | 420 (16.7%) |
| 2015 Average plan premium: 27-year-old | |||
| Second lowest-cost bronze | $189.11 | $186.78 | $200.70 |
| Second lowest-cost silver plan (Benchmark) | $234.89 | $231.69 | $250.85 |
| 2015-2016 Average change in plan premium: 27-year-old | |||
| Second lowest-cost bronze | $27.82 | $32.98 | $2.09 |
| Second lowest-cost silver plan (Benchmark) | $27.04 | $35.90 | ($17.11) |
| 2015-2016 Average change in subsidy: 300% FPL | $7.63 | $9.45 | ($1.41) |
| 2015 Average plan premium: 60-year-old | |||
| Second lowest-cost bronze | $487.29 | $480.77 | $519.76 |
| Second lowest-cost silver plan (Benchmark) | $605.52 | $596.67 | $649.62 |
| 2015-2016 Average change in plan premium: 60-year-old | |||
| Second lowest-cost bronze | $71.71 | $85.02 | $5.41 |
| Second lowest-cost silver plan (Benchmark) | $69.66 | $92.53 | ($44.30) |
| 2015-2016 Change in subsidy: 300% FPL | $69.65 | $92.53 | ($44.30) |
| 2015-2016 % Change in plan premium: All ages | |||
| Second lowest-cost bronze | 14.7% | 17.7% | 1.0% |
| Second lowest-cost silver plan (Benchmark) | 11.5% | 15.5% | −6.8% |
| 2015 Average medical deductible: All ages | |||
| Second lowest-cost bronze | $5,357.46 | $5,372.07 | $5,284.70 |
| 2015-2016 % Change in medical deductible: All ages | |||
| Lowest-cost bronze plan | 3.6% | 3.9% | 1.9% |
Note. FPL = federal poverty level. In 2016, 300% FPL is $35,310 for an individual and $72,750 for a family of four; 400% FPL is $47,080 for an individual and $97,000 for a family of four.
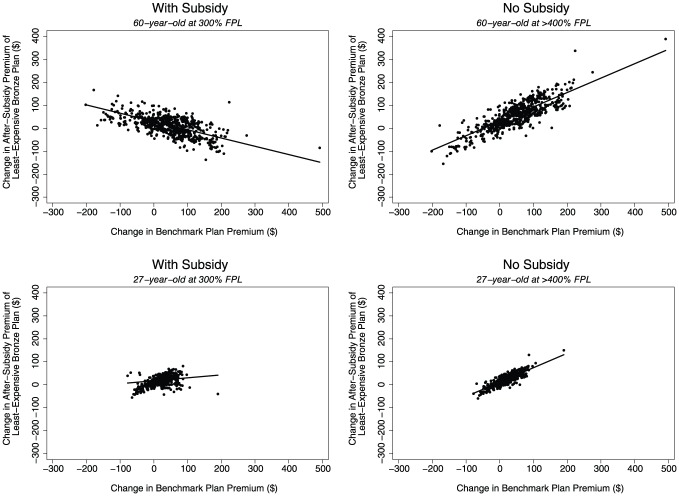
Figure A1 presents a scatterplot of the 2015-2016 change in benchmark premiums versus the change in after-subsidy premiums for the lowest-cost bronze plan for individuals who were subsidy-eligible (300% FPL) and not subsidy-eligible (>400% FPL); results for a 60-year-old and a 27-year-old are shown. As the benchmark premiums increased, the average after-subsidy cost of the lowest-cost bronze plan increased for all adults not receiving subsidies and for younger adults receiving subsidies, but it actually decreased for subsidy-eligible 60-year-olds.
Figure A1.
2015-2016 Change in after-subsidy premium for the least-expensive bronze plan by the change in benchmark* plan premium: With subsidy (300% FPL) versus no subsidy (>400% FPL) for a 60-year-old and 27-year-old.
Note. FPL = federal poverty level. In 2016, 300% FPL is $35,310 for an individual and $72,750 for a family of four; 400% FPL is $47,080 for an individual and $97,000 for a family of four.
*Second lowest-cost silver plan.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Abaluck J., Gruber J. (2011). Choice inconsistencies among the elderly: Evidence from plan choice in the Medicare Part D program. American Economic Review, 101, 1180-1210. doi: 10.1257/aer.101.4.1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. (2015). Data.HealthCare.gov. Retrieved from https://data.healthcare.gov/
- Cutler D. M., Zeckhauser R. J. (2000). The anatomy of health insurance. Handbook of Health Economics, 1, 563-643. [Google Scholar]
- Frean M., Gruber J., Sommers B. D. (2016). Disentangling the ACA’s coverage effects—Lessons for policymakers. New England Journal of Medicine, 375, 1605-1608. doi: 10.1056/NEJMp1609016 [DOI] [PubMed] [Google Scholar]
- Gabel J. R., Arnold D. R., Fulton B. D., Stromberg S. T., Green M., Whitmore H., Scheffler R. M. (2017). Consumers buy lower-cost plans on covered California, suggesting exposure to premium increases is less than commonly reported. Health Affairs, 36, 8-15. doi: 10.1377/hlthaff.2016.0902 [DOI] [PubMed] [Google Scholar]
- Graetz I., Kaplan C. M., Kaplan E. K., Bailey J. E., Waters T. M. (2014). The U.S. health insurance marketplace: Are premiums truly affordable? Annals of Internal Medicine, 161, 599-604. doi: 10.7326/M14-0757 [DOI] [PubMed] [Google Scholar]
- Hodges K. (2016, June 28). Key findings from the health insurance marketplaces: Net premiums and plan choice. Paper presented at the 2016 Annual Research Meeting of Academy Health, Boston, MA Retrieved from https://academyhealth.confex.com/academyhealth/2016arm/meetingapp.cgi/Session/4923 [Google Scholar]
- Hsu J. (2016). The ACA and risk pools—Insurer losses in the setting of noncompliant plans. New England Journal of Medicine, 374, 2105-2107. doi: 10.1056/NEJMp1602981 [DOI] [PubMed] [Google Scholar]
- Hsu J., Overhage L., Price M., Fung V., Newhouse J. P. (2016, November 16). Higher marketplace benchmark plan premiums could reduce post-subsidy premiums for many. Retrieved from http://healthaffairs.org/blog/2016/11/16/higher-marketplace-benchmark-plan-premiums-could-reduce-post-subsidy-premiums-for-many/
- Office of the Assistant Secretary for Planning and Evaluation. (2015, October 3). Health Insurance Marketplace 2015 open enrollment period: March enrollment report. Retrieved from http://aspe.hhs.gov/pdf-report/health-insurance-marketplace-2015-open-enrollment-period-march-enrollment-report
- Office of the Assistant Secretary for Planning and Evaluation. (2016, March 11). Health Insurance Marketplaces 2016 open enrollment period: Final enrollment report. Retrieved from https://aspe.hhs.gov/sites/default/files/pdf/187866/Finalenrollment2016.pdf
- Spranca M., Kanouse D. E., Elliott M., Short P. F., Farley D. O., Hays R. D. (2000). Do consumer reports of health plan quality affect health plan selection? Health Services Research, 35(5, Pt. 1), 933-947. [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services. (2016). Strategic Goal 1: Strengthen health care. Retrieved from http://www.hhs.gov/about/strategic-plan/strategic-goal-1/