Abstract
Collateral blood flow plays a pivotal role in steno-occlusive internal carotid artery (ICA) disease to prevent irreversible ischaemic damage. Our aim was to investigate the effect of carotid artery disease upon cerebral perfusion and cerebrovascular reactivity and whether haemodynamic impairment is influenced at brain tissue level by the existence of primary and/or secondary collateral. Eighty-eight patients with steno-occlusive ICA disease and 29 healthy controls underwent MR examination. The presence of collaterals was determined with time-of-flight, two-dimensional phase contrast MRA and territorial arterial spin labeling (ASL) imaging. Cerebral blood flow and cerebrovascular reactivity were assessed with ASL before and after acetazolamide. Cerebral haemodynamics were normal in asymptomatic ICA stenosis patients, as opposed to patients with ICA occlusion, in whom the haemodynamics in both hemispheres were compromised. Haemodynamic impairment in the affected brain region was always present in symptomatic patients. The degree of collateral blood flow was inversely correlated with haemodynamic impairment. Recruitment of secondary collaterals only occurred in symptomatic ICA occlusion patients. In conclusion, both CBF and cerebrovascular reactivity were found to be reduced in symptomatic patients with steno-occlusive ICA disease. The presence of collateral flow is associated with further haemodynamic impairment. Recruitment of secondary collaterals is associated with severe haemodynamic impairment.
Keywords: Stroke, cerebral hemodynamics, carotid artery, MRI, MRI angiography, perfusion-weighted MRI
Introduction
Collateral blood flow plays a pivotal role in patients with an occlusion in one of the cerebral arteries to maintain adequate oxygenation and cell function.1 A stenosis or occlusion of the internal carotid artery (ICA) decreases the perfusion pressure on the afflicted side. This pressure drop may lead to collateral blood flow and redistribution of blood from the contralateral internal carotid artery (ICA) or the posterior circulation towards the afflicted hemisphere. The circle of Willis (CoW) is considered to be the primary collateral flow route and can supplement the affected brain tissue area with blood through the anterior communicating artery (AComA) or the posterior communicating artery (PComA).1,2 Other collateral pathways such as collateral flow via the ophthalmic artery or leptomeningeal collaterals are considered to be secondary collateral flow routes, meaning that these collaterals are only recruited when the primary collaterals are insufficient or fail.3,4
Patients with recently symptomatic steno-occlusive carotid artery disease are at increased risk for stroke, with an annual risk of 5–6% for recurrent stroke. This risk is raised to 9–18% per year in patients with compromised cerebral haemodynamics and poor collateral blood flow.5,6 The presence of leptomeningeal collaterals on a diagnostic angiogram is predictive of recurrent ischaemic stroke.7 This suggests that secondary collaterals are associated with increased haemodynamic compromise.3,4 Previous studies, however, found no correlation between recurrent ischaemic stroke and haemodynamic impairment measured as cerebrovascular reactivity (CVR) with transcranial Doppler.7
Arterial spin labeling (ASL) MR perfusion imaging has made it possible to measure within the brain tissue both the cerebral blood flow (CBF) and its territorial distribution.8,9 By combining perfusion measurements with a vasodilatory challenge, the CVR can be assessed as a measure for haemodynamic impairment at brain tissue level. Furthermore, in combination with MR angiography, selective ASL can be used to evaluate the territorial distribution of blood and assess collateral pathways.
The aim of the current study was to investigate the effect of large carotid artery disease upon cerebral perfusion and CVR and whether haemodynamic impairment is influenced at brain tissue level by the existence of primary and/or secondary collaterals. We therefore compared the CVR between healthy subjects, symptomatic and asymptomatic patients with severe ICA stenosis or occlusion and assessed the presence of primary and secondary collateral blood flow by combining MR angiography flow patterns at the CoW with territorial ASL perfusion MRI assessment of collateral perfusion territories.
Materials and methods
This study was approved by the institutional ethical review board of the University Medical Center Utrecht according to the Declaration of Helsinki ‘Ethical Principles for Medical Research Involving Human Subjects' and in accordance with the guidelines for Good Clinical Practice (CPMP/ICH/135/95) and written informed consent was obtained from each participant before inclusion.
Subjects
One-hundred seventeen subjects were included in the study. Eighty-eight were functionally independent patients with steno-occlusive ICA disease and 29 were healthy control subjects. All patients were admitted within an 18-month period to the University Medical Center Utrecht, a tertiary comprehensive stroke center, because of carotid artery disease. Group comparisons were done for healthy control subjects, patients with asymptomatic ICA steno-occlusive disease and patients with symptomatic steno-occlusive disease.
Thirty-six of the patients were asymptomatic and had an ICA stenosis of >50% (n = 27) or occlusion (n = 9). Fifty-two were symptomatic and had an ICA stenosis > 50% (n = 23) or occlusion (n = 29). All patients were evaluated by a stroke neurologist. Symptomatic patients had had a transient ischaemic attack (TIA) or non-disabling ischaemic stroke ipsilateral to the afflicted ICA in the previous three months. A TIA was characterized by distinct focal neurological dysfunction or monocular blindness with clearing of sign and symptoms within 24 h. A stroke was characterised by one or more minor (non-disabling) completed strokes with persistence of symptoms or signs for more than 24 h. Patients with severe disabling stroke (modified Rankin core 3–5) were excluded from this study. Patients with diabetes mellitus, severe renal or liver dysfunction, which are contraindications for the use of acetazolamide (ACZ), or disabling stroke (modified Rankin scale score of 3–5), were excluded from this study.10 Diagnosis and grading of the ICA stenosis or occlusion were performed with duplex ultrasonography11 and confirmed with either computed tomography or magnetic resonance (MR) angiography as measured according to the NASCET criteria.5
Imaging protocol
Imaging was performed on a 3T MRI (Achieva, Philips Medical Systems, the Netherlands). The imaging protocol included anatomical T1-weighted imaging, time-of-flight MR angiography (TOF MRA), diffusion- weighted imaging (DWI), T2-weighted fluid attenuation inversion recovery (FLAIR) imaging, and perfusion and territorial ASL imaging.
CBF was measured with a pseudo-continuous ASL (p-CASL) scan. CVR was assessed, according to a previously published protocol, by measuring the amount of CBF increase 15 min after a vasodilatory ACZ challenge.8 A bolus of 14 mg/kg ACZ (Goldshield Pharmaceuticals, UK), with a maximum dose of 1200 mg, was used. An inversion recovery sequence was acquired to measure the magnetization of arterial blood (M0), to quantify CBF, and to segment brain tissue into gray and white matter.12
The labeling plane of the p-CASL scan was positioned in a fixed location with respect to the acquisition volume, i.e. parallel to it and 90 mm below the center slice. Labeling was performed by employing a train of 18° Hanning shaped RF pulses of 0.5 ms at an interval of 1 ms, with a balanced gradient scheme.13,14 The control images were acquired by adding 180° to the phase of all even RF pulses. For each scan, 38 averages of control/label pairs were acquired, resulting in 5 min scan time. For perfusion and territorial scans, the parameters were as follows: TR/TE, 4000/14 ms; field-of-view (FOV), 240 × 240 mm2; matrix size, 80 × 80; slices, 17; slice thickness, 7 mm; no slice gap; single shot echo-planer imaging; label duration, 1650 ms; post labeling delay, 1525 ms; background suppression with a saturation pulse preceding the labeling and two inversion pulses, 1680 and 2830 ms after the saturation pulse.
Territorial ASL imaging was performed with a planning-free vessel encoded (VE) p-CASL to establish the collateral blood flow patterns and perfusion territories of the right and left ICA (RICA and LICA) and the basilar artery (BA).15 Selective labeling was accomplished through manipulating the spatial labeling efficiency by applying additional gradients between the labeling pulses in sets of five variations, i.e. no label (control), full non-selective label (global perfusion), right-to-left encoded label (with 50 mm between full label and control), and two anterior-to-posterior encoded label variations (with 18 mm between full label and control, each shifted 9 mm from each other).16 For each variation, 15 averages were acquired, resulting in 5 min scan time.
FLAIR, DWI and TOF MRA images were acquired with standard protocols supplied by the MR vendor. The direction of collateral blood flow was determined according to a previously published imaging protocol with two consecutive two-dimensional phase-contrast (2DPC) MRI measurements; one phase-encoded in the anterior–posterior direction and one in the right–left direction.17
Image processing
Image processing was performed in MATLAB (Mathworks, MA, USA). Perfusion images were calculated as CBF in mL·100 mL−1·min−1 from the p-CASL images according to a previously published model that corrects for T1 decay, T2* decay and the different delay times of the imaging slices.18,19 The T2* transversal relaxation rate and T1 of arterial blood at 3T were assumed to be, respectively, 50 ms and 1680 ms.20,21 The blood magnetization at thermal equilibrium (M0) for all subjects was determined by selecting a region of interest in the cerebral spinal fluid and iteratively fitting the inversion recovery data by a non-linear least-square method.12 The water content of blood was assumed to be 0.76 mL mL−1 of arterial blood.12 To avoid partial voluming of white matter, a surrogate T1-weighted image was calculated from the inversion recovery sequence by calculating the reciprocal of the quantitative T1.12 This was segmented into grey and white matter probability maps with SPM8 (Wellcome Trust, England), and a corrective threshold was furthermore applied to ensure maximal exclusion of all white matter. CBF before (baseline CBF) and after administration of ACZ was calculated using the resulting grey matter mask. CVR, as a measure for hemodynamic impairment, was defined as the percentage increase in CBF after ACZ administration.
The territorial perfusion maps of the right and left internal carotid arteries (RICA and LICA), and both right and left vertebral arteries (RVA and LVA) were calculated from the VE p-CASL images using a previously published Bayesian framework.22,23 Locations of the vessels (RICA, LICA, RVA, LVA), determined in each subject from a single slice of the MRA located in the neck, were provided as prior information. If a particular vessel could not be identified, it was not included in the Bayesian analysis. To determine the boundaries of the RICA, LICA, and BA, the perfusion territories were manually outlined by one observer (NH) for vessel on their respective territorial perfusion maps. In case of the BA, the combined territorial perfusion map of the RVA and LVA was used.
To examine the extent of the cerebral perfusion territories between patients with different primary collaterals, the outlined regions of interest (ROIs) of the RICA, LICA and BA were brought into MNI space by registering the surrogate T1-weighted image with a standard MNI template using the DARTEL tool in SPM8.24 After determining the grouped perfusion territories of the cerebral arteries, as described below, the grouped ROIs of the anterior cerebral artery (ACA), MCA, and PCA were brought back into subject space by an inverse transformation.
Assessment of collateral blood flow
Two types of collateral blood flow were distinguished, including primary collaterals through the CoW and secondary collateral flow through leptomeningeal vessels and the ophthalmic artery.2
The morphology of the CoW was evaluated by an expert reader (NH) by evaluating the time-of-flight MRA images (supplemental Figure 1). Each CoW was assessed for the presence of the AComA, precommunicating (A1) segment of the ACA, PComA, and precommunicating (P1) segment of the PCA. Presence of collateral blood flow was established by evaluating the blood flow direction through the CoW by means of the 2DPC images. It was determined that no collateral blood flow was present when the ACA and MCA were supplied by the ipsilateral ICA, and the PCA was supplied by the BA. Anterior collateral blood flow was defined as flow from the contralateral side via the AComA towards the ACA (supplemental Figure 1(b)), and subsequently via retrograde flow in the A1 segment of the ACA towards the MCA. Posterior-to-anterior collateral blood flow was defined as flow via the PComA towards the MCA. Anterior-to-posterior collateral flow was defined as blood flow via the PComA towards the PCA, for example, due to a hypoplastic or absent P1 segment of the PCA, also known as a fetal-type CoW (supplemental Figure 1(c)).
Secondary collateral blood flow by leptomeningeal collaterals was determined to be present when a brain region was fed by more than one brain-feeding artery. Each territorial perfusion map was assessed for the contribution of the RICA, LICA and BA to the territories of the ACA, MCA and PCA.
Haemodynamic measurements
CBF and CVR were measured in the ACA, MCA and PCA territory of the ipsi- and contralateral hemispheres. Regions of interest were made at group level from the territorial perfusion maps transformed to standardized MNI space. Figure 1 shows a detailed description of the method of ROI determination.
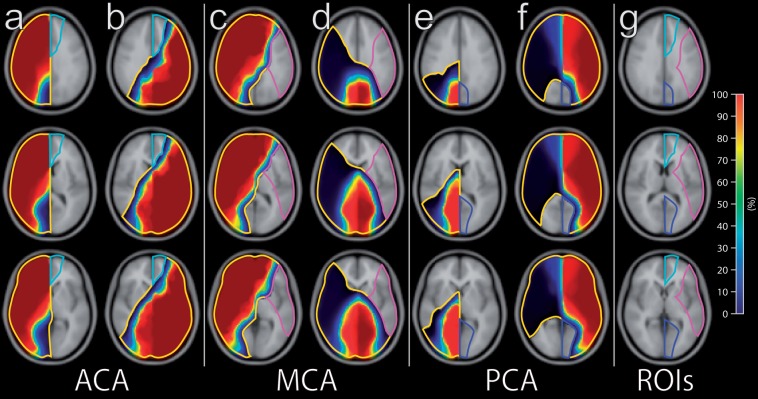
Figure 1.
Transverse flow territory maps projected onto a standard brain template and visual demonstration of how the ROI’s were constructed. Colors correspond to the colorbar, which indicates the percentage of patients who demonstrated perfusion in that region of the brain. Panel A and B show how the ACA territory was delineated. The median border was defined by superimposing all the ICA’s without collateral blood flow, in which the ACA is supplied by its ipsilateral ICA (a). The border between the ACA and MCA was determined by superimposing all the contralateral ICAs from patients with anterior collateral blood, in which the ACA is supplied by the contralateral ICA (b). Panel C and D show how the MCA territory was delineated. The border between the ACA and MCA was determined by superimposing all the ipsilateral ICAs from patients with anterior collateral blood flow, where the ACA territory was fed by the contralateral ICA (c). The border between the MCA and PCA was determined by superimposing all the BAs from patients without collateral blood flow involving the posterior circulation on that side, in which the PCA is supplied by the BA (d). Panel E and F show how the PCA territory was delineated. The border between both PCA’s (Figure 1(e)), and the PCA and vertebrobasilar supply of the cerebellum was determined by superimposing all the ICA’s from patients with anterior-to-posterior collateral flow, in which the contralateral PCA is supplied by the ICA and the entire cerebellum is still supplied by the vertebrobasilar artery. To ensure that the tissue within the ACA, MCA and PCA was only fed by that specific artery, ROI were determined conservatively as only that tissue that was fed in all patients (Figure 1(g)).
ACA: anterior cerebral artery; ICA: internal carotid artery; MCA: middle cerebral artery; PCA: posterior cerebral artery; ROI: region of interest.
Statistical analyses
Differences in degree of stenosis between asymptomatic and symptomatic patients with ICA stenosis or occlusion were compared using Kruskal-Wallis H test. Differences in measurements of baseline CBF and CVR between healthy subjects, subjects with ICA stenosis or occlusion were compared with one-way analysis of variance (ANOVA). Differences between subjects with ICA stenosis or occlusion, without collateral flow or with primary or secondary collateral flow were also compared with ANOVA. A Tukey test was used post-hoc if ANOVA showed a statistically significant difference between groups. A paired t-test and independent t-test were used for comparisons in patients of the same group and between two groups, respectively. A p-value ≤0.05 was considered statistically significant. SPSS (SPSS Inc., Chicago, Illinois, version 23) was used for statistical analysis.
Results
The demographic and clinical characteristics of the participants are outlined in Table 1. There were no statistically significant differences in the degree of ICA stenosis between asymptomatic and symptomatic patients with ICA stenosis on the ipsilateral side (h = 0.03, p = 0.86) and contralateral side (h = 0.98, p = 0.32) and between asymptomatic and symptomatic patients with ICA occlusion on the contralateral side (h = 0.10, p = 0.76).
Table 1.
Demographic and clinical characteristics of the study population.
| Healthy subjects | Asymptomatic patients |
Symptomatic patients |
|||
|---|---|---|---|---|---|
| ICA stenosis | ICA occlusion | ICA stenosis | ICA occlusion | ||
| Number | 29 | 27 | 9 | 23 | 29 |
| Male, n (%) | 13 (45%) | 19 (70%) | 6 (67%) | 23 (74%) | 21 (72%) |
| Age, mean years ± SD | 62 ± 8.2 | 66 ± 7.3 | 62 ± 11 | 69 ± 7.2 | 56 ± 14 |
| Degree of ICA stenosis, n | |||||
| 0–49% | 29 | 0 | 0 | 0 | 0 |
| 50–69% | 0 | 10 | 0 | 5 | 0 |
| 70–99% | 0 | 17 | 0 | 18 | 0 |
| Occluded | 0 | 0 | 9 | 0 | 29 |
| Degree of contralateral ICA stenosis, n | |||||
| 0–49% | 0 | 19 | 6 | 17 | 16 |
| 50–69% | 8 | 10 | 1 | 5 | 9 |
| 70–99% | 0 | 2 | 2 | 1 | 4 |
| Occluded | 0 | 0 | 0 | 0 | 0 |
| Presenting events, n | |||||
| Transient ischaemic attack | – | – | – | 17 | 13 |
| Ischaemic stroke | – | – | – | 8 | 15 |
| Retinal ischaemia | – | – | – | 4 | 1 |
ICA: internal carotid artery.
Haemodynamic measurements
Table 2 summarizes baseline CBF and CVR per hemisphere and cerebral perfusion territory for healthy subjects, patients with an asymptomatic ICA stenosis/occlusion and patients with a symptomatic ICA stenosis/occlusion. There were no differences (paired t-test) in CBF and CBV between the ACA, MCA and PCA territories within each group.
Table 2.
Baseline cerebral blood flow and cerebrovascular reactivity in each perfusion territory per patient group.
| Cerebral blood flow/cerebrovascular
reactivity |
|||||
|---|---|---|---|---|---|
| Hemisphere | N | ACA | MCA | PCA | |
| Healthy subjects | Both | 29 | 52 ± 8.1/48 ± 9.9 | 53 ± 7.7/49 ± 10 | 47 ± 9.8/61 ± 10 |
| Asymptomatic patients | |||||
| Patients with ICA stenosis | Ipsilateral | 27 | 49 ± 8.2/45 ± 9.4 | 47 ± 7.6/43 ± 8.1 | 44 ± 6.7/59 ± 10 |
| Contralateral | 50 ± 9.4/44 ± 9.6 | 49 ± 6.6/45 ± 9.8 | 44 ± 7.3/60 ± 11 | ||
| Patients with ICA occlusion | Ipsilateral | 9 | 48 ± 8.6/35 ± 11a | 43 ± 6.6a/32 ± 10b | 42 ± 8.6/48 ± 10 |
| Contralateral | 47 ± 9.1/38 ± 11 | 47 ± 6.1/39 ± 10 | 42 ± 8.5/50 ± 11 | ||
| Symptomatic patients | |||||
| Patients with ICA stenosis | Ipsilateral | 23 | 44 ± 6.9b/34 ± 7.8bc | 41 ± 6.0b/32 ± 7.5bc | 42 ± 5.9/57 ± 11 |
| Contralateral | 45 ± 6.8/45 ± 8.7 | 43 ± 4.8/45 ± 9.1 | 42 ± 5.2/58 ± 11 | ||
| Patients with ICA occlusion | Ipsilateral | 29 | 44 ± 9.4a/19 ± 10bd | 40 ± 8.8b/13 ± 9.8bd | 42 ± 9.2/35 ± 12b |
| Contralateral | 48 ± 9.7/35 ± 13b | 49 ± 9.0/28 ± 9.7b | 43 ± 8.8/36 ± 11b | ||
ACA: anterior cerebral artery; ICA: internal carotid artery; MCA: middle cerebral artery; PCA: posterior cerebral artery.
Difference (p < 0.001) in baseline CBF or cerebrovascular reactivity in each of the indicated cerebral perfusion territories between the indicated patient groups and the healthy subjects.
Difference (p < 0.001) in baseline CBF or cerebrovascular reactivity in each of the indicated cerebral perfusion territories between the indicated patient groups and the healthy subjects.
Difference (p < 0.005) in cerebrovascular reactivity in each of the indicated cerebral perfusion territories between patients with symptomatic ICA stenosis, and patients with asymptomatic ICA stenosis.
Difference (p < 0.001) in cerebrovascular reactivity in each of the indicated cerebral perfusion territories between patients with symptomatic ICA occlusion, and patients with asymptomatic ICA occlusion.
Asymptomatic patients
In patients with an asymptomatic ICA stenosis, there were no differences in baseline CBF and CVR within the different territories when compared to the contralateral hemisphere and healthy control subjects. In patients with an asymptomatic ICA occlusion, baseline CBF was statistically significantly reduced (p < 0.005) in the MCA territory, and CVR was statistically significantly impaired (p < 0.05) in the ACA and MCA territories distal to the ipsilateral occlusion when compared to the healthy control subjects.
Symptomatic patients
In both patients with a symptomatic ICA stenosis and occlusion, baseline CBF and CVR were statistically significantly reduced (p < 0.01) in the ACA and MCA territories on the side of the ICA stenosis/occlusion when compared to the healthy control subjects. In the patients with an ICA occlusion, CVR was also statistically significantly reduced (p < 0.001) in the ACA and MCA territories of the hemisphere contralateral to the occlusion when compared to the healthy control subjects.
Primary collateral flow
Table 3 summarizes baseline CBF and CVR for patients with ICA stenosis or occlusion. The haemodynamic measurements are described for those with no collateral flow, anterior collateral flow, poster-to-anterior collateral flow or secondary collateral flow. There were no differences (paired t-test) in CBF and CBV between the ACA, MCA and PCA territories within each group.
Table 3.
Baseline cerebral blood flow and cerebrovascular reactivity in each perfusion territory per patient group.
| Cerebral blood flow/cerebrovascular
reactivity |
|||||
|---|---|---|---|---|---|
| Hemisphere | N | ACA | MCA | PCA | |
| Patients with ICA stenosis | |||||
| No collateral flow | Ipsilateral | 35 | 47 ± 7.9/39 ± 7.9 | 45 ± 7.5/37 ± 9.0 | 44 ± 6.4/58 ± 10 |
| Contralateral | 48 ± 8.2/45 ± 9.3 | 47 ± 6.2/45 ± 9.9 | 44 ± 6.5/57 ± 9.6 | ||
| Anterior collateral flow | Ipsilateral | 15 | 45 ± 8.4/33 ± 8.5a | 43 ± 7.4/36 ± 9.0 | 42 ± 6.5/58 ± 10 |
| Contralateral | 48 ± 9.6/43 ± 8.7 | 43 ± 6.9/45 ± 8.4 | 42 ± 6.1/60 ± 11 | ||
| Secondary collateral flow | Ipsilateral | 0 | |||
| Contralateral | |||||
| Patients with ICA occlusion | |||||
| Anterior collateral flow | Ipsilateral | 11 | 48 ± 9.1/24 ± 14 | 43 ± 7.6/27 ± 13 | 44 ± 8.4/44 ± 14 |
| Contralateral | 50 ± 9.5/40 ± 15 | 49 ± 9.4/32 ± 14 | 44 ± 9.2/48 ± 15 | ||
| Posterior-to-anterior | Ipsilateral | 17 | 41 ± 8.8/24 ± 12 | 39 ± 8.5/16 ± 11b | 37 ± 9.4/41 ± 14 |
| collateral flow | Contralateral | 44 ± 9.1/36 ± 13 | 47 ± 9.1/34 ± 13 | 40 ± 8.5/40 ± 14 | |
| Secondary collateral flow | Ipsilateral | 10 | 42 ± 8.7/20 ± 13 | 38 ± 9.3/9 ± 10c | 43 ± 8.3/31 ± 13 |
| Contralateral | 49 ± 9.4/37 ± 14 | 48 ± 5.9/29 ± 10 | 44 ± 7.7/34 ± 10 | ||
ACA: anterior cerebral artery; ICA: internal carotid artery; MCA: middle cerebral artery; PCA: posterior cerebral artery.
Difference (p < 0.05) in cerebrovascular reactivity in the ipsilateral ACA territory between patients with anterior collateral flow, and patients with no collateral flow.
Difference (p < 0.005) in cerebrovascular reactivity in the ipsilateral MCA territory between patients with anterior collateral flow, and patients with posterior-to-anterior collateral flow.
Difference (p < 0.001) in cerebrovascular reactivity in the ipsilateral MCA territory between patients with anterior collateral flow, and patients with secondary collateral flow.
Stenosis patients
Anterior collateral flow occurred in 15 of the 50 patients with an ICA stenosis. Figure 2 shows an example of a symptomatic patient without collateral blood flow, and supplemental Figure 2 shows an example of a symptomatic patient with an anterior collateral blood flow. Anterior collateral flow occurred statistically significantly (p = 0.015, two-sided Fisher’s exact test) more often in symptomatic patients with an ICA stenosis (11 with vs. 12 without) than in asymptomatic patients (4 with vs. 23 without). None of the patients had secondary posterior collateral of secondary collateral blood flow.
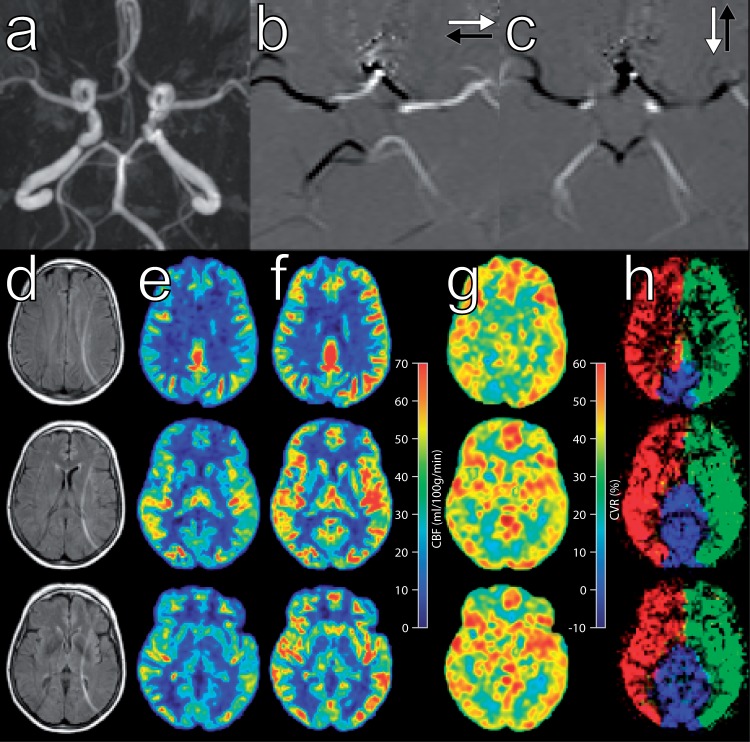
Figure 2.
Case example of a 64-year-old female asymptomatic patient with right-sided ICA stenosis >70%. Time-of-flight MR angiogram images (a) of the circle of Willis show the presence of all vessels. 2D phase contrast images (b,c) show blood flowing from right-to-left in white and left-to-right in black (b), and flowing from anterior-to-posterior in white and posterior-to-anterior in black (c). FLAIR images (d) from cranial (top) to caudal (bottom) correspond with ASL perfusion images before (e) and after (f) acetazolamide, CVR images (g), and territorial ASL maps (h) of the right (red), left (green) carotid arteries and the basilar artery (blue). There is no evidence of reduced cerebral perfusion (e, f), and the cerebrovascular reactivity (g) is unimpaired. The perfusion territories (h) are symmetrical according to the morphology of the circle of Willis.
Patients with ICA stenosis and anterior collateral flow had statistically significant reduced (p < 0.05) CVR in the ACA territory of the afflicted hemisphere when compared to patients without anterior collateral flow.
Occlusion patients
Anterior collateral flow occurred in 11 of the 38 patients with an ICA occlusion, posterior collateral flow in 17 patients and 10 patients had secondary collateral flow. There was difference between symptomatic (8 vs. 11) and asymptomatic (3 vs. 6) patients for the occurrence of anterior collateral flow or posterior-to-anterior collateral flow (p = 1.0, two-sided Fisher’s exact test) to the MCA territory.
Patients with posterior-to-anterior collateral flow were found to have a statistically significant reduced (p < 0.005) CVR in the MCA territory of the afflicted hemisphere compared to patients with anterior collateral flow towards the MCA territory. Examples of symptomatic patients with ICA occlusion and anterior and posterior collateral flow to the MCA territory are shown, respectively, in Figure 3 and supplemental Figure 3.
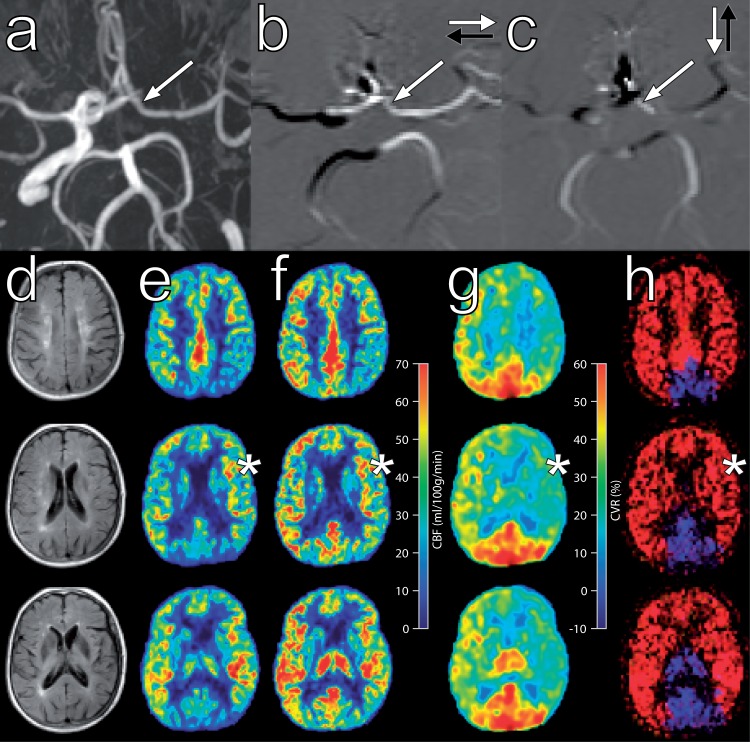
Figure 3.
Case example of a 68-year-old female asymptomatic patient with a left-sided ICA occlusion. There is anterior collateral flow from right to left via the AcomA and retrograde flow in the left A1 segment (a-c, arrow) towards the left MCA territory from the contralateral ICA. FLAIR images (d) correspond with ASL perfusion images before (e) and after (f) acetazolamide, CVR images (g), and territorial ASL maps (h). Reduced CBF at baseline (e), after a vasodilatory challenge (f) and impaired CVR (g) is present in both hemispheres. CVR (g) is most notable impaired in the left MCA territory (g, star). Territorial ASL images show anterior collateral flow from the contralateral ICA (h, red) towards the left MCA territory (h, star).
Secondary collateral flow
Secondary collateral flow occurred only in 10 of the 29 patients with a symptomatic ICA occlusion. Figure 4 shows an example of a symptomatic patient with an ICA occlusion and secondary collateral flow. There was no secondary collateral flow in the patients with an ICA stenosis, or patients with an asymptomatic ICA occlusion.
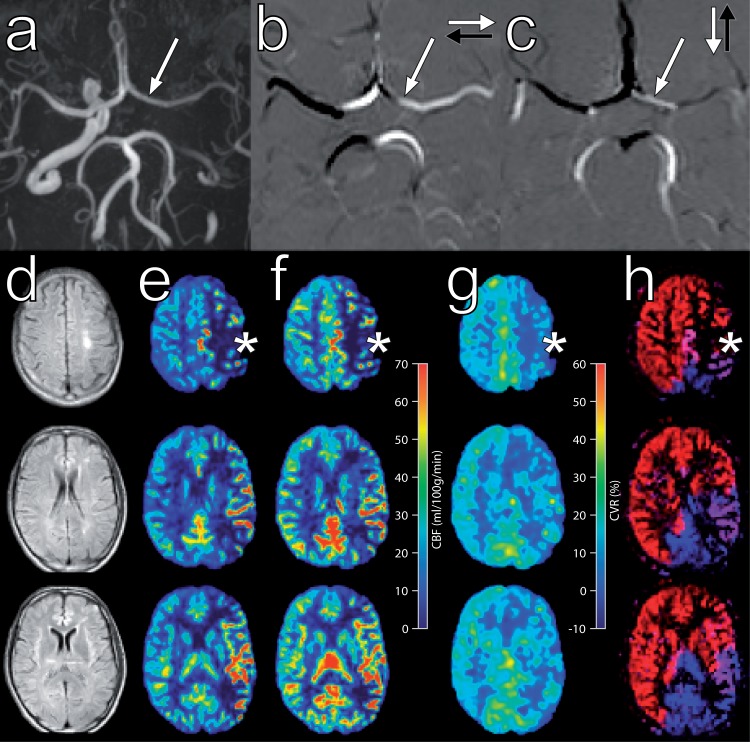
Figure 4.
Case example 47-year-old male patient with left-sided ICA occlusion. There is absence of flow in the left ICA (a, arrow) with distinct primary anterior collateral flow towards the contralateral MCA (b and c, arrow). FLAIR images (d) correspond with ASL perfusion images before (e) and after (f) acetazolamide, CVR images (g), and territorial ASL maps (h). An overlap region in the territorial ASL images (h, star) can be seen where blood from secondary collaterals (purple) fed by the basilar artery (blue) mix with blood from the primary collaterals (red) to supply part of the MCA territory. There is an infarct visible in the left hemisphere (d, arrow) where primary and secondary collaterals mix. Reduced baseline CBF (e, star) can be appreciated against the left hemisphere, without increase after the vasodilatory challenge (f, star). CVR (g) is severely impaired in the left MCA territory (g, star).
The patients with secondary collateral flow were found to have statistically significant reduced (p < 0.001) CVR in the MCA territory of the afflicted hemisphere compared to patients with anterior collateral flow. In patients with secondary collateral flow, there was no differences in baseline CBF (36 ± 11 vs. 38 ± 9.3 ml/100 gr/min; p = 0.10, paired t-test) and CVR (9.2 ± 10% vs. 9.4 ± 11%; p = 0.89, paired t-test) in the region fed by secondary collaterals and the MCA territory on the side of the occlusion.
Discussion
In the current study, we were able to assess the presence of collateral blood flow and haemodynamic impairment in a cohort of both asymptomatic and symptomatic patients with steno-occlusive ICA disease. Both baseline CBF and CVR were found to be reduced in symptomatic patients with ICA stenosis or occlusion. Reduced CVR correlated with the presence of different types of collateral blood flow.
Our results show that cerebral haemodynamics are unimpaired in patients with asymptomatic ICA stenosis, but affected in asymptomatic patients with ICA occlusion, indicating that occlusion of an ICA leads to insufficient capacity of the afferent cerebral blood supply to sustain a normal autoregulatory response. In symptomatic patients with ICA stenosis, the vasodilatory capacity of the parenchymal arterioles seems to be reduced or exhausted in the ipsilateral (afflicted) hemisphere. Since asymptomatic patients with ICA stenosis have sufficient capacity of the major brain-feeding arteries and there was a comparable degree of ICA stenosis, haemodynamic impairment in symptomatic patients might be due to reduced vasodilatory capacity of afflicted brain parenchyma.
In patients with ICA occlusion, no difference was found in types of primary collateral flow between asymptomatic and symptomatic patients. Anterior collateral flow to the ACA territory occurred in all patients with ICA occlusion. In patients with posterior-to-anterior collateral flow, haemodynamic impairment in the afflicted hemisphere was more severe, compared to patients with anterior collateral flow towards the MCA territory; it was, however, not more prevalent in asymptomatic or symptomatic patients. We may speculate that posterior-to-anterior instead of anterior collateral flow towards the MCA territory is a sign of inadequate capacity of the contralateral ICA.
Secondary collateral flow only occurred in symptomatic patients with ICA occlusion. These patients were found to have severe haemodynamic impairment of the afflicted hemisphere. We also found CVR was just as severely impaired in the brain tissue supplied by secondary collaterals as it was in the MCA territory supplied by primary collaterals. In these patients with a chronic occlusion, we hypothesize that the occurrence of secondary collaterals is due to critically insufficient primary collateral redistribution via the CoW. It has previously been reported that the presence of ophthalmic or leptomeningeal (secondary) collateral flow in patients was associated with impaired CVR.25 We believe it is a sign of severely impaired cerebral haemodynamics, and we speculate ischaemic damage to brain parenchyma even occurs in spite of secondary collateral flow.
The advantage of this study has been the establishment of a measurement of cerebral perfusion and haemodynamics in combination with assessment of collateral flow patterns with one modality in a single session. Other modalities than MR might have been more proficient, such as digital subtraction angiography (DSA), in detecting the type of collateral flow; these techniques, however, lack the direct cross-sectional comparison we have accomplished with ASL MR imaging. Furthermore, territorial ASL has found to provide excellent information on collateral flow comparable to DSA.26 The currently employed planning-free VE p-CASL technique in combination with a Bayesian inference analysis has been previously shown to be comparable with other more robust techniques to depict exact cerebral perfusion territories.27 TOF MR angiography and 2DPC MR imaging for the assessment of primary collaterals, in combination with territorial ASL MR imaging for secondary collaterals, with additional CBF and CVR measurements have enabled us to assess the haemodynamic status of individual patients with no more than 15 min scan time added to a standard MR protocol.
A limitation of this study is the lack of clinical follow-up data in patients. The presence of secondary collaterals was earlier found to be predictive of recurrent ischaemic stroke.3,4,7 Previous studies with transcranial Doppler, however, did not find a correlation between recurrent ischaemic stroke and impaired CVR.28 These earlier studies are either based solely on angiographic collateral supply patterns3,4,7 or CVR measurements in a single vessel or territory without collateralization information,28 which may in part explain the discrepancy. Furthermore, the CVR measurements are higher than in the previously published papers that compared p-CASL reactivity to Oxygen-15 PET.29 Although the baseline CBF measures are comparable, the variability of vasoactive stimuli may explain the differences in CBF values after ACZ. Although this may lead to generally higher CVR values throughout the brain, we expect that this does not affect our evaluation of the effect of collateral within the brain. Finally, only a few number of patients had steno-occlusive vertebrobasilar circulation. The results of this study are therefore only representative of the anterior circulation.
In conclusion, we have shown that patients with an asymptomatic ICA stenosis rarely have haemodynamic impairment, as opposed to asymptomatic patients with ICA occlusion, in whom both hemispheres are compromised. The presence of collateral flow is associated with further haemodynamic impairment. Recruitment of secondary collaterals is associated with severe haemodynamic impairment, indicating critically insufficient blood supply via primary collaterals and only occurs in symptomatic patients with ICA occlusion. In future, this knowledge of haemodynamic impairment and collateral blood flow at brain tissue level may help personalize treatment and select those who benefit most from revascularization therapy.
Supplementary Material
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: R.P.H. Bokkers receives support from the Dutch Heart Foundation (Grant 2013T047).
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ contributions
Nolan S Hartkamp made a substantial contribution to the concept and design, acquisition of data, analysis, interpretation of data and drafting of the article. Esben T Petersen made a substantial contribution to the concept and design, acquisition of data, analysis, interpretation of data and drafting of the article. Michael A Chappell made a substantial contribution to the concept and design, acquisition of data or analysis and interpretation of data, and drafted the article. Thomas W Okell made a substantial contribution to the concept and design, acquisition of data or analysis and interpretation of data, and drafted the article. Maarten Uyttenboogaart made a substantial contribution to the interpretation of data and drafting of the article. Clark J. Zeebregts made a substantial contribution to the interpretation of data and drafting of the article. Reinoud PH Bokkers made a substantial contribution to the concept and design, acquisition of data, analysis, interpretation of data, drafting of the article and approved the final version to be published.
Supplementary material
Supplementary material for this paper can be found at the journal website: http://journals.sagepub.com/home/jcb
References
- 1.Derdeyn CP, Grubb RLJ, Powers WJ. Cerebral hemodynamic impairment: methods of measurement and association with stroke risk. Neurology 1999; 53: 251–259. [DOI] [PubMed] [Google Scholar]
- 2.Liebeskind DS. Collateral circulation. Stroke 2003; 34: 2279–2284. [DOI] [PubMed] [Google Scholar]
- 3.Muller M, van der Graaf Y, Algra A, et al. Carotid atherosclerosis and progression of brain atrophy: the SMART-MR study. Ann Neurol 2011; 70: 237–244. [DOI] [PubMed] [Google Scholar]
- 4.Hofmeijer J, Klijn CJM, Kappelle LJ, et al. Collateral circulation via the ophthalmic artery or leptomeningeal vessels is associated with impaired cerebral vasoreactivity in patients with symptomatic carotid artery occlusion. Cerebrovasc Dis 2002; 14: 22–26. [DOI] [PubMed] [Google Scholar]
- 5.Barnett HJ, Taylor DW, Eliasziw M, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 1998; 339: 1415–1425. [DOI] [PubMed] [Google Scholar]
- 6.Klijn CJ, Kappelle LJ, Algra A, et al. Outcome in patients with symptomatic occlusion of the internal carotid artery or intracranial arterial lesions: a meta-analysis of the role of baseline characteristics and type of antithrombotic treatment. Cerebrovasc Dis 2001; 12: 228–234. [DOI] [PubMed] [Google Scholar]
- 7.Persoon S, Luitse MJA, de Borst GJ, et al. Symptomatic internal carotid artery occlusion: a long-term follow-up study. J Neurol Neurosurg Psychiatry 2011; 82: 521–526. [DOI] [PubMed] [Google Scholar]
- 8.Bokkers RPH, van Osch MJP, van der Worp HB, et al. Symptomatic carotid artery stenosis: impairment of cerebral autoregulation measured at the brain tissue level with arterial spin-labeling MR imaging. Radiology 2010; 256: 201–208. [DOI] [PubMed] [Google Scholar]
- 9.Hartkamp NS, Petersen ET, De Vis JB, et al. Mapping of cerebral perfusion territories using territorial arterial spin labeling: techniques and clinical application. NMR Biomed 2013; 26: 901–912. [DOI] [PubMed] [Google Scholar]
- 10.van Swieten JC, Koudstaal PJ, Visser MC, et al. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988; 19: 604–607. [DOI] [PubMed] [Google Scholar]
- 11.Nederkoorn PJ, Mali WPTM, Eikelboom BC, et al. Preoperative diagnosis of carotid artery stenosis: accuracy of noninvasive testing. Stroke 2002; 33: 2003–2008. [DOI] [PubMed] [Google Scholar]
- 12.Chalela JA, Alsop DC, Gonzalez-Atavales JB, et al. Magnetic resonance perfusion imaging in acute ischemic stroke using continuous arterial spin labeling. Stroke 2000; 31: 680–687. [DOI] [PubMed] [Google Scholar]
- 13.Wu W, Fernández-Seara M, Detre JA, et al. A theoretical and experimental investigation of the tagging efficiency of pseudocontinuous arterial spin labeling. Magn Reson Med 2007; 58: 1020–1027. [DOI] [PubMed] [Google Scholar]
- 14.Dai W, Garcia D, de Bazelaire C, et al. Continuous flow-driven inversion for arterial spin labeling using pulsed radio frequency and gradient fields. Magn Reson Med 2008; 60: 1488–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong EC. Vessel-encoded arterial spin-labeling using pseudocontinuous tagging. Magn Reson Med 2007; 58: 1086–1091. [DOI] [PubMed] [Google Scholar]
- 16.Gevers S, Bokkers RP, Hendrikse J, et al. Robustness and reproducibility of flow territories defined by planning-free vessel-encoded pseudocontinuous arterial spin-labeling. AJNR Am J Neuroradiol 2012; 33: E21–E25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rutgers DR, Klijn CJ, Kappelle LJ, et al. A longitudinal study of collateral flow patterns in the circle of Willis and the ophthalmic artery in patients with a symptomatic internal carotid artery occlusion. Stroke 2000; 31: 1913–1920. [DOI] [PubMed] [Google Scholar]
- 18.Alsop DC, Detre JA. Reduced transit-time sensitivity in noninvasive magnetic resonance imaging of human cerebral blood flow. J Cereb Blood Flow Metab 1996; 16: 1236–1249. [DOI] [PubMed] [Google Scholar]
- 19.Bokkers RPH, van der Worp HB, Mali WPTM, et al. Noninvasive MR imaging of cerebral perfusion in patients with a carotid artery stenosis. Neurology 2009; 73: 869–875. [DOI] [PubMed] [Google Scholar]
- 20.Golay X, Petersen ET, Hui F. Pulsed star labeling of arterial regions (PULSAR): a robust regional perfusion technique for high field imaging. Magn Reson Med 2005; 53: 15–21. [DOI] [PubMed] [Google Scholar]
- 21.St Lawrence KS, Wang J. Effects of the apparent transverse relaxation time on cerebral blood flow measurements obtained by arterial spin labeling. Magn Reson Med 2005; 53: 425–433. [DOI] [PubMed] [Google Scholar]
- 22.Chappell MA, Okell TW, Payne SJ, et al. A fast analysis method for non-invasive imaging of blood flow in individual cerebral arteries using vessel-encoded arterial spin labelling angiography. Med Image Anal 2012; 16: 831–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chappell MA, Okell TW, Jezzard P, et al. A general framework for the analysis of vessel encoded arterial spin labeling for vascular territory mapping. Magn Reson Med 2010; 64: 1529–1539. [DOI] [PubMed] [Google Scholar]
- 24.Ashburner J. A fast diffeomorphic image registration algorithm. Neuroimage 2007; 38: 95–113. [DOI] [PubMed] [Google Scholar]
- 25.Müller M, Schimrigk K. Vasomotor reactivity and pattern of collateral blood flow in severe occlusive carotid artery disease. Stroke 1996; 27: 296–299. [DOI] [PubMed] [Google Scholar]
- 26.Chng SM, Petersen ET, Zimine I, et al. Territorial arterial spin labeling in the assessment of collateral circulation: comparison with digital subtraction angiography. Stroke 2008; 39: 3248–3254. [DOI] [PubMed] [Google Scholar]
- 27.Hartkamp NS, Helle M, Chappell MA, et al. Validation of planning-free vessel-encoded pseudo-continuous arterial spin labeling MR imaging as territorial-ASL strategy by comparison to super-selective p-CASL MRI. Magn Reson Med 2014; 71: 2059–2070. [DOI] [PubMed] [Google Scholar]
- 28.Persoon S, Kappelle LJ, van Berckel BNM, et al. Comparison of oxygen-15 PET and transcranial Doppler CO2-reactivity measurements in identifying haemodynamic compromise in patients with symptomatic occlusion of the internal carotid artery. EJNMMI Res 2012; 2: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heijtel DFR, Mutsaerts HJMM, Bakker E, et al. Accuracy and precision of pseudo-continuous arterial spin labeling perfusion during baseline and hypercapnia: a head-to-head comparison with 15O H2O positron emission tomography. Neuroimage 2014; 92: 182–192. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.