Abstract
Background:
Family carers provide vital support for patients towards end-of-life, but caregiving has considerable impact on carers’ own health. The scale of this problem is unknown, as previous research has involved unrepresentative samples or failed to fully capture caregiving close to death.
Aim:
To quantify level of psychological morbidity and general health among a census sample of carers of people with cancer at end-of-life, compared to population reference data.
Design:
National 4-month post-bereavement postal census survey of family carers of people who died from cancer, retrospectively measuring carers’ psychological health (General Health Questionnaire-12) and general health (EuroQoL EQ-Visual Analogue Scale) during the patient’s last 3 months of life.
Participants:
N = 1504 (28.5%) of all 5271 people who registered the death of a relative from cancer in England during 2 weeks in 2015 compared with data from the Health Survey for England 2014 (N = 6477–6790).
Results:
Psychological morbidity at clinically significant levels (General Health Questionnaire-12 ⩾4) was substantially higher among carers than the general population (83% vs 15%), with prevalence five to seven times higher across all age groups. Overall, carers’ general health scores were lower than population scores, median 75 (interquartile range, 50–80) versus 80 (interquartile range, 70–90), but differences were more marked at younger ages. Female carers had worse psychological morbidity and general health than male carers.
Conclusion:
Levels of psychological morbidity among family carers during end-of-life caregiving are far higher than indicated by previous research, indicating a substantial public health problem. Consistent assessment and support for carers to prevent breakdown in caregiving may produce cost savings in long term.
Keywords: Family caregivers, mental health, palliative, end of life, cancer, survey, health status
What is already known about the topic?
Family carers make a crucial contribution to end-of-life care, but existing research indicates they suffer worse mental health than other carers, study controls, patients and the general population, with prevalence estimates for clinically significant depression at 39%–57% and anxiety at 34%–47%.
Previous findings are unlikely to be representative of the population of carers providing end-of-life care, as studies have either recruited carers through specialist or palliative care settings where carers may be better supported or have failed to fully capture care during the final months of life.
What this paper adds?
This study provides the most representative data on carer health during end-of-life caregiving for people with cancer to date, based on a national census retrospective survey.
Carers’ level of clinically significant psychological morbidity (83%) during caregiving was found to be five to seven times higher than general population levels, far higher than indicated by previous evidence.
Carers’ general health during caregiving was lower than for the general population, but differences were more marked among younger carers with scores converging towards older age.
Implications for practice, theory or policy
The prevalence of clinical morbidity among carers providing end-of-life care indicates a substantial, but hitherto hidden, public health problem.
Findings emphasise a need for more consistent assessment and support for carers as part of end-of-life care, with signposting to more specialist mental health input where needed.
Introduction
Family carers make a crucial contribution to end-of-life care, providing substantial hours of care, offsetting health service costs and facilitating patient choice. Nationally representative samples indicate that the majority of family carers (62%) provide up to 19 h care per week in England.1 However, during end-of-life care, the hours of caregiving escalate to a median of nearly 70 h care per week.2 Supporting patients to stay at home at end-of-life could generate considerable healthcare cost savings; lifetime healthcare costs are greatest in the last year of life and hospital care accounts for the largest component.3 Furthermore, end-of-life care at home is the preference of the majority of patients.4 The most important factor in sustaining end-of-life care at home and meeting patient preferences is the availability of family carers.5,6 However, end-of-life caregiving substantially affects carers’ own health: negative impacts from caregiving increase progressively with care hours provided7 and severity of patients’ disease.8,9 During caregiving, carers of palliative patients experience greater impacts on emotional health,10 quality of life11 and physical health10–12 compared to carers of non-palliative patients. End-of-life carers also report worse mental and physical health than non-caregiving controls,13,14 and worse mental health compared to the general population,8,14–18 although some of these studies show end-of-life carers to have similar or better physical health than the norm.15–17 End-of-life carers may also suffer more anxiety18,19 or depression20 than patients themselves. Overall reported results seem to show the greatest and most consistent impacts on carers’ psychological health and patterns appear very similar across English-speaking countries and Europe.8–21
Previous research does not enable us to quantify the level of psychological impact on the end-of-life carer population. The majority of studies have recruited carers from oncology/tertiary care15,19–21 or palliative care services.11,13,14,16–18 Their reported rates of mental ill health among end-of-life carers during caregiving are high, ranging from 34% to 47% for anxiety15,18,19,21 and 39% to 57% for clinical depression,14,20 based on standard measures. However, generalisation from these studies to the end-of-life carer population should be cautious; specialist services may produce better outcomes than non-specialist services, but those referred to them may also have the most complex needs. Only Dumont et al.8 recruited both through generalist and specialist care, and reported carer psychological morbidity at 41%–62% (increasing with decreasing patient function), but again did not use population level data. There have been only two end-of-life carer population studies,10,12 both using secondary analysis of single item, non-standard scales for impact, for example, on ‘emotional stress’,10 preventing comparison with standard measurements of psychological morbidity. Furthermore, most studies have included considerable proportions of carers of patients who are not in the final 3–4 months of life and who may still be relatively well.10,14–21
We therefore lack robust, population level data on the health impact of end-of-life care on caregivers. Information on the health consequences of end-of-life caregiving, and the number and types of carers affected, are needed for appropriate service planning. Registers of end-of-life carers are often incomplete and screening for health problems ad hoc. Ensuring that carers are able to continue caregiving is ultimately about supporting the patient. This is particularly important as an increase in the percentage of family carers within the population1 and a rising number of deaths22 are likely to increase the numbers involved in end-of-life family caregiving. There are already an estimated 500,000 family carers per annum providing end-of-life care in the United Kingdom.23 It is important to establish the level of health problems within this population to inform service developments required to support carers to sustain end-of-life care and to address carers’ own health needs during caregiving.
The aims of this article are (1) to quantify the level of psychological health problems and general health among a population sample of carers during caregiving for someone with cancer in their last 3 months of life and (2) to compare our carer data with reference data for England for comparable age and gender groups. An in-depth analysis of predictors of carers’ psychological and general health outcomes will be the subject of a forthcoming paper.
Method
The design was a nationwide, cross-sectional census retrospective post-bereavement survey of family members of people who died from cancer. Methods have been further described elsewhere.2 This retrospective design enables access to a representative sample of end-of-life carers independent of their contact with services and permits assessment of health status during a consistent, comparable time period closely before death. In contrast, prospective studies normally have to rely on recruitment through selected services, can only control timing of measurement relative to death through prolonged longitudinal design and have high attrition close to death. Carers were surveyed 4 months post-bereavement as the optimum time point to allow appropriate distance to the death, yet ensure good accuracy of recall. Survey data were compared with prospective data from a representative sample of the population from the Health Survey for England (HSE) 2014.
Sample and recruitment
The Office for National statistics (ONS) drew sample details from Death Certificates of all people domiciled in the UK who registered the death of a relative from cancer (International Classification of Diseases, 10th Revision (ICD-10) codes C000-C979) between 1 and 16 May 2015 in England (N = 5271). Exclusions were death of a child (<18 years old); death occurred somewhere other than home, hospice, hospital or care home; reported to the coroner; person registering death was not a relative; address of relative was missing; or address, gender or age of deceased was missing. While the eventual aim is to expand the survey to carers of people with conditions other than cancer, we initially tested the method with a smaller, defined group of carers to ascertain how feasible it was to ask a census sample of bereaved carers detailed questions about their caregiving via postal survey. We here focused on cancer as the condition which most commonly has been the subject of palliative and end-of-life research, enabling comparison with previous studies.8,11,13,15–21
The ONS sent survey packs (invitation letter, information sheet, decline slip and survey) and two subsequent reminders to non-responders (t1 = letter and decline slip, t2 = second survey pack) to the relative reporting the death. Packs were sent 4 months post-bereavement and reminders at 1-month intervals. The invitation letter clarified that the survey was about the support provided by family and friends for people with cancer at the end of life. If recipients did not feel they were the best person to complete the survey, they were invited to pass it on to someone more appropriate. Responses were made to the research team by post, online or via telephone interview.
The University of Manchester’s Research Ethics committee approved the study (Ref: 14430; 12.02.2015). Completion and return of a postal or online survey was taken as informed consent to participate. Participants in telephone interviews gave verbal consent. All data received by the research team were fully anonymised and disclosure controlled. Data from the HSE are publicly available through the UK Data Service to researchers registering a specific project (Usage number 103114).
Data collection
The survey included questions on demographics, decedents’ diagnosis, participants’ relationship to the decedent and care provided.2
Psychological health was measured through the General Health Questionnaire (GHQ)-12,24 a 12-item standardised measure of psychological morbidity. Items include being able to make decisions or concentrate, feeling under strain or thinking of oneself as worthless. Responses are made on 4-point scales. A higher score indicates worse morbidity. General health was measured using the EuroQoL EQ-Visual Analogue Scale (EQ-VAS),25 a single-item scale of health with 0 being ‘the worst health’ and 100 being ‘the best health you can imagine’. Discussions with the GHQ and EQ-VAS licence holders established that these tools could be used for retrospective data collection, with minor amendments to wording, and that there was a precedent for this. However, licence constraints meant different time frames had to be adopted between these tools: respondents were asked to consider how they felt on a typical day towards the end of the decedent’s life in terms of the last few weeks of their relative’s life for the GHQ-12 and the last 3 months for the EQ-VAS.
GHQ-12 and EQ-VAS permit comparison with the HSE. HSE is conducted annually using a multi-stage, stratified probability sample, representative of the English population resident in private households.26 Data were collected via face-to-face, computer-assisted interviews with a trained researcher. A separate, self-completion questionnaire was administered in the presence of the interviewer which included the GHQ-12 and EQ-5D VAS to measure how they felt ‘over the past few weeks’ and ‘today’, respectively.26
For our own data set, ONS supplied anonymised, linked data for the whole sampling frame consisting of age and gender of deceased, final underlying cause and contributing causes of death (ICD-10 codes), place of death, and area index of multiple deprivation (IMD) for the decedent to enable assessment of the representativeness of participants.
Analysis
Differences between participants and non-participants on variables supplied by the ONS were investigated using chi-square for categorical variables and analysis of variance (ANOVA) for continuous variables (reported in detail elsewhere).2
For GHQ-12 4-point scales, we used the scoring method of 0-0-1-1 with total scores ranging from 0 to 12. Research indicates this is the better method for differentiating caseness for mental illness, with a score of ⩾4 being the optimal threshold within England with 85% sensitivity and 89% specificity for clinically significant psychological morbidity.24
Study findings were compared with HSE 2014 data26 using descriptive statistics: GHQ-12 caseness was presented as percentages and GHQ-12 and EQ-VAS scores as means with standard deviations (SD) and medians with interquartile ranges (IQR). No imputation or other statistical correction was made of missing data, which ranged from 1.4% (gender) to 14.5% (EQ-VAS).
Results
Participants
Surveys were completed by 1504 carers (28.5%). Participants were predominantly female (64%) with a median age of 60 (IQR, 52–69) years, mainly caring for a spouse (45%) or parent (43%), and 96% defined themselves as White. Twenty-five percent had a university degree and an additional 22% had education beyond age 16. Median patient age was 76 (IQR, 67–84) years, 53% were male, and 36% died at home, 30% in hospital, 20% in hospice and 15% in a care home. Main primary causes of death were lung cancer (20%), colorectal (10%), prostate (8%) and breast cancer (7%). Distribution over IMD quintiles, from most to least deprived, was 14%, 17%, 22%, 23% and 25%, respectively. Compared with non-participants, participants were significantly more likely to have registered the death of patients dying at home and from less deprived areas (see Rowland et al.2 for further details). Of those who responded to questions about time spent on support and care for their relative (1365/1504), 99% reported spending some time, with the median time spent being 69:30 h per week (IQR, 28:37–115:15) in their relative’s last 3 months of life (see Rowland et al.2 for further details on hours and tasks).
Carer health outcomes
Figure 1 shows total percentages for clinically significant psychological morbidity for carers during end-of-life caregiving compared with the population. End-of-life carers’ caseness for psychological morbidity was five to seven times higher than for the corresponding population age groups (Table 1).27 Furthermore, carers’ median GHQ-12 score was 6–8 across age groups, well above the cutoff point for caseness of 4, and in clear contrast to a consistent population median of 0. Caseness was highest among younger carers (ages 25–54: 89%–92%), but reduced with age (ages 55–74: 80%–82%; ages 75+: 74%). In contrast, likely cases of psychological morbidity in the population remained fairly consistent across ages (11%–17%). Male carers consistently fared better than women carers on GHQ-12 caseness and scores (differences of 7%–19% points and 1–3 in median scores, respectively), except for similar results at age 35–44. While this reflects population gender differences for psychological morbidity, both male and female carers had rates of caseness considerably above population rates.
Figure 1.
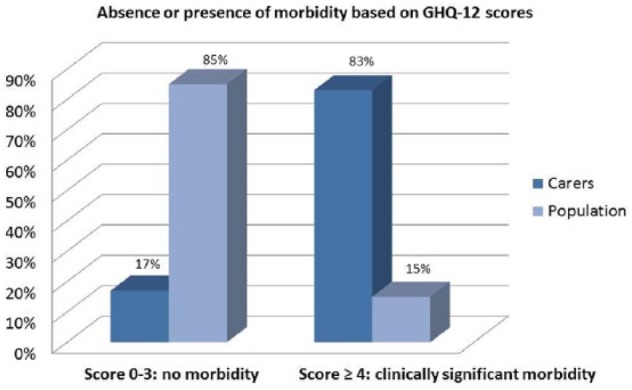
Prevalence (%) of clinically significant psychological morbidity among carers during end-of-life caregiving compared to population data (Health Survey for England 2014).
Table 1.
GHQ-12 Scores: reference data for England and survey data for carers during ‘the last few weeks’ of the patient’s life. Reference data in grey column (weighted), carer data in white column. Scored as 0–12 with 12 being poorest health; caseness threshold is ≥4.
| 18–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65–74 | 75+ | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | N | 769 | 3 | 1176 | 37 | 1186 | 94 | 1263 | 322 | 990 | 435 | 825 | 363 | 581 | 190 | 6790 | 1444 |
| Caseness (%) | 123 (16.0) |
*
* |
194 (16.5) | 33 (89.2) | 168 (14.1) | 86 (91.5) | 193 (15.3) | 288 (89.4) | 147 (14.9) | 357 (82.1) | 91 (11.0) | 291 (80.2) | 83 (14.2) | 141 (74.2) | 999 (14.7) | 1199 (83.0) | |
| Mean | 1.5 | * | 1.5 | 7.5 | 1.4 | 6.8 | 1.5 | 7.3 | 1.4 | 6.8 | 1.1 | 6.3 | 1.4 | 5.8 | 1.4 | 6.7 | |
| SD | 2.4 | * | 2.67 | 2.81 | 2.66 | 2.51 | 2.89 | 2.93 | 2.84 | 3.26 | 2.36 | 3.23 | 2.50 | 3.28 | 2.66 | 3.16 | |
| Median | 0 | * | 0 | 8 | 0 | 7 | 0 | 7 | 0 | 7 | 0 | 6 | 0 | 6 | 0 | 7 | |
| 25th Percentile | 0 | * | 0 | 6 | 0 | 5 | 0 | 5 | 0 | 4 | 0 | 4 | 0 | 3 | 0 | 4 | |
| 75th Percentile | 2 | * | 2 | 10 | 2 | 9 | 2 | 10 | 1 | 10 | 1 | 9 | 2 | 8 | 2 | 9 | |
| Males | N | 387 | 1 | 572 | 15 | 584 | 39 | 624 | 106 | 479 | 139 | 397 | 120 | 251 | 75 | 3295 | 495 |
| Caseness (%) | 52 (13.4) |
*
* |
82 (14.3) | 12 (80.0) | 67 (11.5) | 36 (92.3) | 88 (14.1) | 90 (84.9) | 55 (11.5) | 100 (71.9) | 40 (10.0) | 83 (69.2) | 30 (12.1) | 52 (69.3) | 414 (12.6) | 374 (75.6) | |
| Mean | 1.3 | * | 1.3 | 6.1 | 1.3 | 6.6 | 1.4 | 6.6 | 1.1 | 5.8 | 0.9 | 5.3 | 1.2 | 5·2 | 1.2 | 5.8 | |
| SD | 2.19 | * | 2.38 | 2.67 | 2.56 | 2.50 | 2.89 | 2.83 | 2.50 | 3.63 | 2.21 | 3.26 | 2.36 | 3.28 | 2.50 | 3.26 | |
| Median | 0 | * | 0 | 6 | 0 | 7 | 0 | 7 | 0 | 5 | 0 | 5 | 0 | 5 | 0 | 6 | |
| 25th Percentile | 0 | * | 0 | 4 | 0 | 5 | 0 | 5 | 0 | 3 | 0 | 2 | 0 | 3 | 0 | 4 | |
| 75th Percentile | 2 | * | 2 | 8 | 1 | 8 | 1 | 8 | 1 | 9 | 0 | 8 | 1 | 8 | 1 | 8 | |
| Females | N | 382 | 2 | 604 | 22 | 602 | 55 | 639 | 216 | 511 | 296 | 428 | 241 | 330 | 114 | 3496 | 946 |
| Caseness (%) | 71 (18.6) |
*
* |
113 (18.7) | 21 (95.5) | 100 (16.7) | 50 (90.9) | 106 (16.5) | 198 (91.7) | 92 (18.0) | 257 (86.8) | 51 (12.0) | 207 (85.9) | 52 (15.9) | 89 (78.1) | 586 (16.8) | 824 (87.1) | |
| Mean | 1.7 | * | 1.7 | 8.4 | 1.6 | 6.9 | 1.7 | 7.6 | 1.7 | 7.2 | 1.2 | 6.8 | 1·5 | 6.3 | 1.6 | 7.1 | |
| SD | 2.60 | * | 2.91 | 2.58 | 2.74 | 2.53 | 2.89 | 2.93 | 3.10 | 2.97 | 2.48 | 3.10 | 2.60 | 3.23 | 2.80 | 3.02 | |
| Median | 1 | * | 0 | 9 | 0 | 7 | 0 | 8 | 0 | 8 | 0 | 7 | 0 | 6 | 0 | 7 | |
| 25th Percentile | 0 | * | 0 | 7 | 0 | 5 | 0 | 6 | 0 | 5 | 0 | 5 | 0 | 4 | 0 | 5 | |
| 75th Percentile | 2 | * | 2 | 10 | 2 | 9 | 2 | 10 | 2 | 10 | 1 | 9 | 2 | 9 | 2 | 10 | |
GHQ: General Health Questionnaire; SD: standard deviation.
The UK reference data come from NatCen Social Research.27 Available from: http://doi.org/10.5255/UKDA-SN-7919-2.
UK reference data are weighted using the interview weight for individual responses.
N too low for meaningful reporting of statistics and preservation of participant anonymity.
Carers’ general health scores during end-of-life caregiving were generally lower than population scores (Table 2), although median scores converged towards older age, with carers age 75+ scoring better than population counterparts. Carers’ median EQ-VAS health score was lowest among younger carers (ages 25–44: score 63–70) and then remained level (score 75) at older ages. In contrast, population scores were highest for ages 25–44 (score 85), but decreased very slightly with age, with a drop to score 70 for age 75+. Male carers had better median EQ-VAS scores than female carers across all age groups (differences of 5–20 in median score). In contrast, median EQ-VAS population scores were very similar for men and women.
Table 2.
EQ-VAS Scores: reference data for England and survey data for carers during ‘the last three months’ of the patient’s life. . Reference data in grey column (weighted), carer data in white column.
| 18–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65–74 | 75+ | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | N | 760 | 2 | 1159 | 28 | 1147 | 79 | 1222 | 279 | 934 | 400 | 749 | 325 | 506 | 165 | 6477 | 1278 |
| Mean | 80.0 | * | 80.0 | 57.0 | 80.2 | 69.7 | 78.9 | 67.5 | 76.4 | 69.5 | 76.9 | 68.9 | 69.1 | 70.5 | 78.1 | 68.8 | |
| SD | 17.05 | * | 17.00 | 25.48 | 16.50 | 18.35 | 17.91 | 21.21 | 20.09 | 21.98 | 17.74 | 22.67 | 20.63 | 19.56 | 18.18 | 21.61 | |
| Median | 80 | * | 85 | 63 | 83 | 70 | 83 | 75 | 80 | 75 | 80 | 75 | 70 | 75 | 80 | 75 | |
| 25th Percentile | 70 | * | 70 | 36 | 70 | 60 | 70 | 50 | 70 | 56 | 70 | 50 | 55 | 55 | 70 | 50 | |
| 75th Percentile | 90 | * | 90 | 80 | 90 | 85 | 90 | 85 | 90 | 85 | 90 | 90 | 85 | 90 | 90 | 80 | |
| Males | N | 382 | 1 | 570 | 10 | 566 | 31 | 608 | 91 | 459 | 128 | 370 | 106 | 218 | 58 | 3175 | 425 |
| Mean | 80.4 | * | 81.0 | 69.0 | 79.7 | 72.6 | 79.0 | 72.7 | 77.4 | 72.9 | 77.7 | 75.6 | 69.4 | 75.7 | 78.6 | 73.8 | |
| SD | 15.15 | * | 15.68 | 16.47 | 16.46 | 17.01 | 17.33 | 17.76 | 18·85 | 21.87 | 17.33 | 19.87 | 20.71 | 18.03 | 17.34 | 19.50 | |
| Median | 80 | * | 85 | 68 | 80 | 80 | 82 | 75 | 80 | 80 | 80 | 80 | 70 | 80 | 80 | 80 | |
| 25th Percentile | 70 | * | 75 | 50 | 70 | 60 | 70 | 65 | 70 | 60 | 70 | 65 | 50 | 64 | 70 | 63 | |
| 75th Percentile | 90 | * | 90 | 80 | 90 | 85 | 90 | 85 | 90 | 90 | 90 | 90 | 88 | 90 | 90 | 90 | |
| Females | N | 378 | 1 | 589 | 18 | 580 | 48 | 614 | 188 | 475 | 272 | 379 | 217 | 288 | 106 | 3303 | 850 |
| Mean | 79.6 | * | 79.1 | 50.4 | 80.7 | 67.8 | 78.7 | 65.0 | 75.4 | 67.8 | 76.1 | 65.5 | 68.8 | 67.6 | 77.6 | 66.2 | |
| SD | 18.79 | * | 18.15 | 27.51 | 16.54 | 19.11 | 18.5 | 22.30 | 21.19 | 21.88 | 18.13 | 23.31 | 20.42 | 19.88 | 18.95 | 22.18 | |
| Median | 82 | * | 81 | 48 | 85 | 70 | 83 | 70 | 80 | 73 | 80 | 70 | 70 | 70 | 80 | 70 | |
| 25th Percentile | 75 | * | 70 | 30 | 70 | 51 | 70 | 50 | 69 | 51 | 70 | 50 | 55 | 50 | 70 | 50 | |
| 75th Percentile | 90 | * | 90 | 76 | 90 | 80 | 90 | 80 | 90 | 80 | 90 | 80 | 85 | 85 | 90 | 80 | |
EQ-VAS: EuroQoL EQ-Visual Analogue Scale; SD: standard deviation.
The UK reference data come from NatCen Social Research.27 Available from: http://doi.org/10.5255/UKDA-SN-7919-2.
UK reference data are weighted using the interview weight for individual responses.
N too low for meaningful reporting of statistics and preservation of participant anonymity.
If we consider the sub-sample of the general population that reported providing help to anyone with problems relating to physical/ mental ill health or disability/ old age, caseness within this group was 12%–28% and EQ-VAS median scores were 75–80 (data not shown).27
Discussion
Main findings
Carers’ retrospective reports in this census-based study indicate that prevalence of caseness for psychological morbidity was five to seven times higher among carers during end-of-life caregiving compared to the general population.27 Their prevalence of psychological morbidity (83%) was also considerably higher than for end-of-life carers in previous studies (34%–47% for anxiety15,18,19,21 and 39%–57% for clinical depression);14,20 for general carers in England who provide ⩾20 h of care per week (34% for women and 19% for men, based on GHQ-12);7 and for those in HSE 2014 reporting helping someone with a health problem or disability (12%–28%).27 The general health of carers during end-of-life caregiving was also overall lower than within the general population.27 Differences were greatest among younger age groups (15–23 EQ-VAS score difference, ages 25–44), but converged with increasing age, with carers age 75+ scoring slightly higher than the population.
Female carers had worse psychological health than male carers, in line with previous research and general population data.9,27 Women carers overall also had worse general health than men, whereas the population data showed no similar consistent gender difference.27 The carer gender difference between men and women in both psychological and general health may indicate that women are disproportionally affected in their carer role. Women are more likely to undertake end-of-life caregiving and at more intense levels than men.28
Strengths and limitations
Our study design has generated the most representative population level information on end-of-life carer health to date, being based on a census sample of all cancer deaths in England in a defined period. The retrospective design enabled us to capture carer data for all cancer deaths regardless of patients’ access to specialist or palliative care and to gain information on the period closest to death, thus overcoming the limitations of previous studies10,11,13–21 and providing a more realistic picture of the true impact of end-of-life caregiving on carer health. Our findings show prevalence of clinically significant psychological morbidity to be far higher among end-of-life carers during final months of caregiving than indicated by previous research. Given the consistency in findings from carer studies across Europe and English-speaking countries, similarly high levels of psychological morbidity are likely to be present during caregiving in the final months of life across these nations.
In contrast, we found carers’ general health to be similar to or better than the population among some age groups. Licence restrictions for the standard measurement tools used in our study meant carers reported on their general health for the patients’ last 3 months and psychological health for their last few weeks, therefore the psychological health scores may be worse because they represent the time closer to death. However, findings correspond with previous studies where differences in psychological health appear more consistent and marked than for physical health.15–17
The study was limited to carers of patients who died from cancer. This makes it similar to other palliative carer studies, where cancer is predominant.8,11,13,15–21 Cancer furthermore represents a substantial proportion of all deaths (28.5%).29 However, our findings may be less representative of end-of-life family caregiving for conditions with different disease trajectories to cancer where, for instance, a clear end-of-life period is more difficult to define.30 Within the study sample, survey participants were similar to non-participants for patient age, gender, and diagnosis. However, carers with greater socioeconomic status and resources to deal with caregiving may be over-represented, as participants were more likely to care for patients from less deprived areas who died at home than non-participants. Participants may therefore have better general health than other end-of-life carers.31 Ethnic minorities also appeared under-represented compared to the population. Furthermore, we do not know if survey response rates were affected by the level of psychological morbidity being experienced by carers. Nevertheless, if survey participants were the only ones to suffer clinically significant psychological morbidity, caseness among carers in the total census sample would still be 23%, well above the population level. However, it is more plausible that those with worse psychological health were less likely to respond to a postal survey and therefore that psychological morbidity in the carer population is truly high and potentially higher than indicated by our results.
Finally, the retrospective data collection may affect the accuracy of reporting. We collected carers’ retrospective reports of health via self-completed postal questionnaires and compared these with HSE contemporary reports of health via self-completed questionnaires in the presence of an interviewer. A recent review of the health literature32 found strong agreement between patients’ retrospective and contemporary physical and mental health reports for a majority of comparisons, but with stronger agreement for shorter intervals (<3 months). The review found no consistency in the direction of differences between retrospective and contemporary measurement: retrospective scores were better than contemporary scores in one study, worse in two, no different in two and dependent on the measure in one study. Therefore, the evidence so far does not suggest that retrospective measurement will lead to inflated measures of poor health. However, we need to consider whether carers’ post-bereavement distress in our study may affect their retrospective reports of health and make scores more negative. Evidence shows that pre-bereavement psychological morbidity in fact is a strong predictor of post-bereavement distress.9,33 Therefore, even if there is some influence of carers’ current state on their recollection, reports are still likely to give a reasonable indication of carers’ psychological health pre-bereavement.9,33 Nevertheless, given the importance of retrospective data collection for end-of-life care research, further study of the relationship between prospective and retrospective reports is warranted. To date, few studies have addressed this issue even in the health literature as a whole.32
What this study adds
This study found far higher prevalence of psychological morbidity among carers during end-of-life caregiving than indicated by previous research,14,15,18–21 with clinically significant morbidity being the norm. This represents a large, hitherto unrecognised public health burden, the consequences of which need to be further established. If results are representative of end-of-life carers in England in general, over 400,000 of the estimated half a million end-of-life carers per annum23 may be at risk for substantial psychological morbidity, with effects likely to carry on into bereavement.9,33 If only representative of cancer carers, over 100,000 p.a. may still be affected. Women and younger carers may be particularly affected and warrant additional attention.
Carers may willingly accept a health risk associated with caring for a loved one at end of life and the substantial hours entailed.34 We should be careful not to pathologise the impact of caregiving, but must ensure carers are not ‘broken’ by the experience. Evidence indicates that the impact of caregiving can be mitigated through good, early service support and the addressing of carer support needs during caregiving.35–38 Therefore, considerable benefit may be gained from relatively small-scale investment to ensure carers are consistently assessed and supported in their caregiving role as part of existing end-of-life provision, with signposting to more specialist mental health input where needed. It is promising that the new Carers Action Plan 2018–202039 for England focuses on identification of carers within primary care and make further specific reference to end-of-life care. However, this plan largely focuses on social care provision, whereas end-of-life carers need considerable support from healthcare practitioners to meet the challenges of caring for a dying person and preserving their own health.40 In reality, healthcare practitioners will naturally remain focused on the patient, particularly in the face of mounting healthcare service pressures. Therefore, support that meets the need for carers during end-of-life care is unlikely to materialise unless separate space and provision are made for consistent assessment and support for carers as part of end-of-life healthcare provision. Carers are our biggest resource in supporting patients at end of life. If they are stretched beyond breaking point, there would be considerable economic, health and social care cost implications, for example, in terms of replacing lost hours of patient care, increased end-of-life acute care admissions, carer health problems pre- and post-bereavement and productivity losses if carers can no longer participate in employment. Investment in support for carers may therefore lead to considerable gains in the longer term. Future research should consider end-of-life caregiving for carers of patients dying from conditions other than cancer and perspectives of ethnic minorities and investigate the effectiveness and cost-effectiveness of models of end-of-life carer support in maintaining carer psychological health and functioning, sustaining care at home and preventing acute inpatient admissions.
Acknowledgments
We thank all the family carers who participated in the study and the lay advisory group and carer group members who helped us design the survey. We also wish to thank Mark Pilling and Eva Batistatou for input to the design and statistical analysis, respectively; the Office of National Statistics (ONS) for their assistance with the survey; and the UK Data Service for supplying data from the Health Survey for England. Neither the ONS nor the UK Data Service bear any responsibility for the further analysis or interpretation of the data as presented here. G.G., B.H. and B.v.d.B. contributed to the design of the study with G.G. as Principal Investigator. C.R. led on data acquisition and analysis. G.G., B.H., B.v.d.B. and C.R. contributed to interpretation of findings. G.G. wrote the manuscript and all authors critically revised the manuscript for important intellectual content, approved the final version and take public responsibility for appropriate portions of the content.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: The study was funded by Dimbleby Cancer Care. It received support from the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care (NIHR CLAHRC) Greater Manchester. The views expressed in this article are those of the authors and not necessarily those of the NHS, NIHR or the Department of Health.
ORCID iDs: Gunn Grande  https://orcid.org/0000-0003-2200-1680
https://orcid.org/0000-0003-2200-1680
Christine Rowland  https://orcid.org/0000-0001-8628-4638
https://orcid.org/0000-0001-8628-4638
Bernard van den Berg  https://orcid.org/0000-0002-9554-0194
https://orcid.org/0000-0002-9554-0194
Barbara Hanratty  https://orcid.org/0000-0002-3122-7190
https://orcid.org/0000-0002-3122-7190
References
- 1. Buckner L, Yeandle S. Valuing carers 2015: the rising value of carers’ support. Report to Carers UK, https://www.sheffield.ac.uk/polopoly_fs/1.546409!/file/Valuing-Carers-2015.pdf (accessed 9 August 2017).
- 2. Rowland C, Hanratty B, Pilling M, et al. The contributions of family care-giving at end-of-life: a national post-bereavement census survey of cancer carers’ hours of care and expenditures. Palliat Med 2017; 31(4): 346–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gardiner C, Ingleton C, Ryan T, et al. What cost components are relevant for economic evaluation of palliative care, and what approaches are used to measure these costs? A systematic review. Palliat Med 2017; 31(4): 323–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gomes B, Calanzani N, Gysels M, et al. Heterogeneity and changes in preferences for dying at home: a systematic review. BMC Palliat Care 2013; 12: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Costa V. The determinants of place of death: an evidence-based analysis. Ont Health Technol Assess Ser 2014; 14(16): 1–78. [PMC free article] [PubMed] [Google Scholar]
- 6. Wahid AS, Sayma M, Jamshaid S, et al. Barriers and facilitators influencing death at home: a meta-ethnography. Palliat Med 2018; 32: 314–328. [DOI] [PubMed] [Google Scholar]
- 7. Hirst M. Carer distress: a prospective, population-based study. Soc Sci Med 2005; 61: 697–708. [DOI] [PubMed] [Google Scholar]
- 8. Dumont S, Turgeon J, Allard P, et al. Caring for a loved one with advanced cancer: determinants of psychological distress in family caregivers. J Palliat Med 2006; 9(4): 912–921. [DOI] [PubMed] [Google Scholar]
- 9. Stajduhar KI, Funk L, Toye C, et al. Part 1: home-based family caregiving at the end of life: a comprehensive review of published quantitative research (1998–2008). Palliat Med 2010; 24: 573–593. [DOI] [PubMed] [Google Scholar]
- 10. Wolff JL, Dy SM, Frick KD, et al. End-of-life care: findings from a national survey of informal caregivers. Arch Intern Med 2007; 167(1): 40–46. [DOI] [PubMed] [Google Scholar]
- 11. Weitzner MA, McMillan SC, Jacobsen PB. Family caregiver quality of life: differences between curative and palliative cancer treatment settings. J Pain Symptom Manage 1999; 17(6): 418–428. [DOI] [PubMed] [Google Scholar]
- 12. Williams AM, Wang L, Kitchen P. Differential impacts of care-giving across three caregiver groups in Canada: end-of-life care, long-term care and short-term care. Health Soc Care Community 2014; 22(2): 187–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chentsova-Dutton Y, Shuchter S, Hutchin S, et al. The psychological and physical health of hospice caregivers. Ann Clin Psychiatry 2000; 12(1): 19–27. [DOI] [PubMed] [Google Scholar]
- 14. Haley WE, LaMonde LA, Han B, et al. Family caregiving in hospice: effects on psychological and health functioning among spousal caregivers of hospice patients with lung cancer or dementia. Hosp J 2001; 15(4): 1–18. [DOI] [PubMed] [Google Scholar]
- 15. Grov EK, Dahl AA, Moum T, et al. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Ann Oncol 2005; 16(7): 1185–1191. [DOI] [PubMed] [Google Scholar]
- 16. Zapart S, Kenny P, Hall J, et al. Home-based palliative care in Sydney, Australia: the carer’s perspective on the provision of informal care. Health Soc Care Community 2007; 15(2): 97–107. [DOI] [PubMed] [Google Scholar]
- 17. Kenny PM, Hall JP, Zapart S, et al. Informal care and home-based palliative care: the health-related quality of life of carers. J Pain Symptom Manage 2010; 40(1): 35–48. [DOI] [PubMed] [Google Scholar]
- 18. Goetze H, Brahler E, Gansera L, et al. Psychological distress and quality of life of palliative cancer patients and their caring relatives during home care. Support Care Cancer 2014; 22(10): 2775–2782. [DOI] [PubMed] [Google Scholar]
- 19. Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. Can Med Assoc J 2004; 170(12): 1795–1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Braun M, Mikulincer M, Rydall A, et al. Hidden morbidity in cancer: spouse caregivers. J Clin Oncol 2007; 25(30): 4829–4834. [DOI] [PubMed] [Google Scholar]
- 21. Rumpold T, Schur S, Amering M, et al. Informal caregivers of advanced-stage cancer patients: every second is at risk for psychiatric morbidity. Support Care Cancer 2016; 24(5): 1975–1982. [DOI] [PubMed] [Google Scholar]
- 22. Gomes B, Higginson IJ. Where people die (1974–2030): past trends, future projections and implications for care. Palliat Med 2008; 22: 33–41. [DOI] [PubMed] [Google Scholar]
- 23. Payne S, Hudson P. Assessing the family and caregivers. In: Walsh D, Caraceni AT, Fainsinger R, et al. (eds) Palliative Medicine. 1st ed New York: Elsevier, 2008, pp. 320–325. [Google Scholar]
- 24. Goldberg DP, Gater R, Sartoris N, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997; 27: 191–197. [DOI] [PubMed] [Google Scholar]
- 25. Brooks R. EuroQol: the current state of play. Health Policy 1996; 37(1): 53–72. [DOI] [PubMed] [Google Scholar]
- 26. Health & Social Care Information Centre. Health survey for England 2014: volume 2: methods and documentation (HSCIC 2015), pp. 154–155, https://files.digital.nhs.uk/publicationimport/pub19xxx/pub19295/hse2014-methods-and-docs.pdf (accessed 11 June 18).
- 27. NatCen Social Research, University College London. Department of Epidemiology and Public Health. Health Survey for England, 2014. [data collection]. 2nd ed. UK Data Service (SN: 7919), 2016, 10.5255/UKDA-SN-7919-2 [DOI]
- 28. Abernethy A, Burns C, Wheeler J, et al. Defining distinct caregiver subpopulations by intensity of end-of-life care provided. Palliat Med 2009; 23(1): 66–79. [DOI] [PubMed] [Google Scholar]
- 29. Office for National Statistics. Deaths registered in England and Wales: 2016. ONS, 2017, https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsregistrationsummarytables/2016 (accessed 16 August 2017).
- 30. Murray SA, Kendall M, Boyd K, et al. Illness trajectories and palliative care. BMJ 2005; 330: 1007–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Marmot M. Fair Society healthy lives. Strategic review of health inequalities in England post 2010. The Marmot Review, London, 2010, http://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review/fair-society-healthy-lives-exec-summary-pdf.pdf (accessed 25 August 2017). [Google Scholar]
- 32. Kwong E, Black N. Retrospectively patient-reported pre-event health status showed strong association and agreement with contemporaneous reports. J Clin Epidemiol 2017; 81: 22–32. [DOI] [PubMed] [Google Scholar]
- 33. Chan D, Livingston G, Jones L, et al. Grief reactions in dementia carers: a systematic review. Int J Geriatr Psychiatry 2013; 28(1): 1–17. [DOI] [PubMed] [Google Scholar]
- 34. Van den Berg B, Bleichrodt H, Eeckhoudt L. The economic value of informal care: a study of informal caregivers’ and patients’ willingness to pay and willingness to accept for informal care. Health Econ 2005; 14: 363–376. [DOI] [PubMed] [Google Scholar]
- 35. Dionne-Odom JN, Azuero A, Lyons KD, et al. Benefits of early versus delayed palliative care to informal family caregivers of patients with advanced cancer: outcomes from the enable III randomized controlled trial. J Clin Oncol 2015; 33(13): 1446–1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Grande G, Austin L, Ewing G, et al. Assessing the impact of a Carer Support Needs Assessment (CSNAT) intervention in palliative home care: a stepped wedge cluster trial. BMJ Support Palliat Care 2017; 7: 326–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Aoun SM, Grande G, Howting D, et al. The impact of the carer support needs assessment tool (CSNAT) in community palliative care using a stepped wedge cluster trial. PLoS ONE 2015; 10(4): e0123012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ewing G, Brundle C, Payne S, et al. The carer support needs assessment tool (CSNAT) for use in palliative and end of life care at home: a validation study. J Pain Symptom Manage 2013; 46(3): 395–405. [DOI] [PubMed] [Google Scholar]
- 39. Department of Health & Social Care. Carers action plan 2018–2020: supporting carers today, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/713781/carers-action-plan-2018-2020.pdf (accessed 4 June 2018).
- 40. Ewing G, Grande GE. Development of a carer support needs assessment tool (CSNAT) for end of life care practice at home: a qualitative study. Palliat Med 2013; 27(3): 244–256. [DOI] [PubMed] [Google Scholar]


