Abstract
Background:
Screening is the most important action in the early diagnosis of breast cancer. This study investigates the impact of educational intervention based on the integrated behavioral model on breast cancer screening behavior in women in Karaj City, 2016.
Methods:
This semi-experimental study was conducted on 138 women who were attended to health centers in Mohammad Shahr city. The samples were selected using cluster sampling and were randomly divided into two groups, experimental and control group. Data gathering tool was a four-part questionnaire (demographic characteristics, knowledge, Champion's Health Belief Scale, subjective norms). Two 50-min sessions were held for educational intervention in the experimental group. Training was presented through lecture, questioning and answering and group discussion. The data were completed in three steps (before, immediately after and 2 months after the intervention) and were analyzed using SPSS 16 software.
Results:
The results showed that the mean score of all structures except the perceived benefits of mammography and mammography behavior have a significant difference in the intervention group than the control group in 2 months after intervention (P < 0.001). In all the studied structures, except the perceived benefits of mammography (P = 0.083) and mammographic behavior (P = 0.156), there was a significant difference between the two groups before and immediately after the intervention (P < 0.001).
Conclusions:
The finding of this study showed that the efficiency and effectiveness of an educational intervention based on health belief model along with subjective norms that emphasize the opinions of others about the behaviors of individuals also has a very dramatic effect on the promotion of breast cancer screening behaviors.
Keywords: Breast cancer, education, integrated behavioral model, screening behaviors, subjective norms
Introduction
Cancer incidence and its mortality in the world are increasing. Breast cancer is the most common cancer in women and the fifth killing cancer in the world.[1] Based on several conducted studies, cancer is the third leading cause of death in Iran.[2,3,4,5] The prevalence of breast cancer in Global Studies was reported 12.5% that nearly one out of every eight women in their lifetime is at the risk of cancer.[6] According to the American Cancer Association estimates 205,300 new cases of breast cancer are reported, and 39,600 deaths from the disease occur in women each year.[7]
The incidence of breast cancer in Iran is 22 cases/100,000, its prevalence is 120 cases/100,000, and the mortality rate of 1200 deaths per year.[8] The prevalence of breast cancer is 30 cases/100,000 women in the central part of Iran, Isfahan. Moreover, the death rate due to breast cancer is reported 5.8/100,000 women in Tehran.[9] The growing trend of breast cancer in Iran is the most important point, the mean age of women with breast cancer is estimated 48.8 years. The greatest risk of malignancy is in women aged 40–49 and 23% of cancers occur in women <40 years and this means that Iranian women involved with breast cancer a decade earlier than their female counterparts in the developed countries.[10,11,12,13,14] An annual increase of about 6%–4% is added to this cancer.[10,11]
Breast cancer incidence increases steadily with age and incidence of the disease in developed countries is 50 percent in the whole world that can result from early diagnosis through screening and prevention programs.[15] The most important action in the early diagnosis of breast cancer and death resulting from it is screening.[16] Screening methods for early detection of this deadly disease include: mammography, breast self-examination (BSE), clinical examination.[17] The early diagnosis of breast cancer increases 5-year survival of patients to 97%. According to the reports, 48% of breast cancer is discovered by the patient, and 41% by mammography and only 11% of them are diagnosed in physical examination by a physician.[15,17] According to studies, 95% of advanced cancer and 65% of primary breast cancer are diagnosed by patients.[18] Several studies suggest that improving the level of public knowledge and attitude about breast cancer can have a positive role in screening behaviors of women.[19,20] Due to the high costs of its treatment and psychological and emotional burden for patients and their families, education, and prevention are very important.[14,21] Knowledge improvement and proper education are the most emphatic and important methods so that in several studies have a significant role in knowledge improvement.[7,22,23]
Using theories and models of health education and health promotion has a significant relationship with reducing high-risk disease behaviors.[17] Health belief model is one of the most widely used models in the field of prevention of diseases and also as a psychological model.[24,25,26,27,28,29] This model focuses on how person's perception creates motivation and motion and leads to behavior. According to this theory, when a person is encouraged to do health-promoting activities and has a positive expectation of this performance, value her health and considers disease as a threat or unavoidable serious consequences. According to this theory, women are encouraged to breast cancer screening test when believe: maybe at increased risk of breast cancer (perceived susceptibility), well-understand the depth of the risk and its various physical, mental, and social aspects (severity), to believe that early diagnosis reduces negative consequences (perceived benefits) and screening behavior does not cost a lot for a person (perceived barriers), and a person can perform the behavior (self-efficacy).[17,27,30,31,32,33] In a study conducted by Nasir Isfahani et al. On screening behaviors of BSE and mammography among health volunteers educational Intervention showed a significant increase, regarding health belief model structures, but on the contrary, there were no significant differences in screening behaviors between before and after the intervention. In that study, researchers recommended to review and address other factors such as subjective norms.[15] In fact, subjective norms are one of the constructs theory of planned behavior and are considered a predictor of behavioral intention and behavior. People in the community affected by various entities such as parents, spouse, and religious leaders and under their influence perform a behavior.[34] Regarding that cancer prevention is the priority of Alborz University of Medical Sciences and in conducted researches, the researchers could not find any conducted study on breast cancer in Karaj city, the importance of education about breast cancer is felt in this city. This study aimed to determine the effectiveness of the education based on the integrated behavioral model on breast cancer screening behaviors among women attending to health centers of Valadabad-e Bozorg and Kuchak in Karaj City in 2016.
Methods
Study design
This study is an experimental study conducted in two urban health care centers located in Mohammad Shahr of Karaj by the name of Valadabad-e Bozorg and Kuchak in 2016. Both of these centers were the same in social, economic and cultural conditions. The number of samples in this study were estimated 56 using similar studies[32] and by 20% loss it was 69, respectively, for each experimental and control group. Samples were selected by using cluster sampling. The centers were randomly divided into experimental (Valadabad-e Kuchak) and control (Valadbad-e Bozorg). Inclusion criteria were: literacy, a willingness to cooperate and active participation in training sessions, having a family file at the health centers, being older than 35 years and had no pregnancy or lactation, If not willing to participate or continue cooperation, there is the possibility and allowance of leaving.
Intervention
Data collection instrument
In this study, a questionnaire consists of five sections was used for data collection The first part of the questionnaire was about the demographic characteristics (age, education, occupation, spouse's education, family history of cancer, and information source about breast cancer).
The second part of the questionnaire contains questions related to the knowledge about breast cancer (13 questions) (From your point of view, how often should I go to a breast exam)? and self-examination of breast cancer (5 items) and for this purpose, the questionnaire of Noori Zadeh et al. was used. Content validity in the Nouri’ study was determined with using opinion and reform of 11 professors of Tabriz University of Medical Sciences. Instrument reliability was calculated using the internal stability test (Cronbach's alpha) of 0.77.[32] In the third section to assess the behavioral intention (for example: I go to do mammography every 2 years) and behavior (for example: Have you ever done a mammography?) for self-examination and mammography on breast cancer the questionnaire of Nasir Isfahani et al. was used.[15]
The questionnaire used in part IV was Champion's Health Belief Scale which includes 50 items and 7 sub-scale with 5-option question to assess perceived susceptibility (3 items with scores between 3 and 15) For example: I feel that I will suffer from breast cancer in the future and the perceived severity (7 items with the scores between 7 and 35) for example: It scares me, when I imagine myself suffering from breast cancer. Perceived barriers (9 items with the score between 9 and 45) for example: Monthly BSE would take a long time and perceived benefits (6 items with the score between 6 and 30) for example: With monthly BSE, it is less likely to die of breast cancer and perceived self-efficacy (10 item score between 50 and 10) for example: I can do monthly BSE correctly. Perceived benefits (6 items with the score between 6 and 30) for example, Mammography is painful and perceived barriers (9 items with the score between 9 and 45) for example: Mammogram is the best way to find small tumor in the breast. Reliability of the Persian version by Taymoori and Berry was used. Reliability in the Nouri's study was calculated for each Subscales with Cronbach's alpha: perceived susceptibility (0.82) and perceived severity (0.84), perceived benefits (0.80), perceived barriers (0.86), perceived self-efficacy (0.90), perceived benefits for mammography (0.72), and perceived benefits for mammography (0.73).[35]
In the fifth part of a researcher-made questionnaire to assess the subjective norms (12 questions) for example: My husband encouraged me to do the BSE once in a month. For BSE and mammography was used, and its scientific validity was determined through content validity and face validity. To validate content, the idea of 6 specialists were used, and for the face validity of the questionnaire, they were delivered to 30 women who attend to the health center of Valadabad and were neither in the experimental group nor in control group, and the necessary modifications were made. For reliability, internal consistency (Cronbach's alpha) was used by calculating the amount of 73% which is acceptable. A five-part questionnaire with 74 questions by experimental and control groups in three stages (before, immediately after and 2 months after the intervention) was completed.
Before the start of the study participants completed informed consent form to participate in the study and were assured about the confidentiality of information at all stages of the research.
Intervention
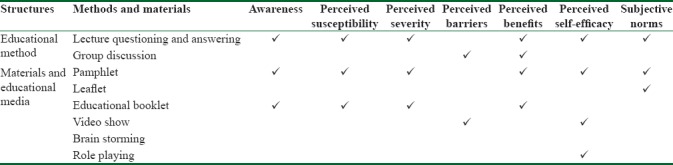
After analyzing the data obtained from pretest and according to educational necessities, educational content was prepared. Training was performed with the presentation of samples in the basij site (due to having the proper conditions for training), By a female doctor at the health center of Valadabad-e Kuchak (because of the specialized role of doctors in the diagnosis and treatment of diseases and also because some of the questions of subjective norms investigate the role of doctor on women's breast cancer screening behaviors). Due to space limitations in training and for better efficiency of training, participants were divided into two groups of 35 and 34. Regarding the education content and possibilities and limitations, for each group, two training sessions of 50 min were held. Training was presented through lecture, Questioning and answering and group discussion. In educational programs using researcher-made pamphlets, brief information about breast cancer, Symptoms of the disease and methods of screening and mammography was delivered to the participants and their families. To send a message to the husbands of participants, educational leaflets containing a message were used (Example: if you care your wife’ health, encourage her to do BSE). BSE correct procedures also was shown to the participants by using the film, Then one of the participants in class practice BSE to make it more tangible and participants become familiar with screening behavior Table 1.
Table 1.
Methods and training materials used to modify any of the integrated model structures
Immediately and 2 months after intervention questionnaire was completed by both of the groups. After completion of the study, educational content was delivered to the control group.
Statistical analysis
Data analysis was performed using descriptive, analytical statistics (R. M. ANOVA, independent t-test, Friedman, and Mann–Whitney) and SPSS 16 software (IBM Corporation, USA).
Results
A total of 138 women patients (69 patients in the experimental group, 69 in control group) over 35-year-old participated in this study. Chi-square test results show that there are no statistically significant differences between the two groups in demographic variables (P > 0.001) [Table 2].
Table 2.
Demographic variables in experimental and control groups
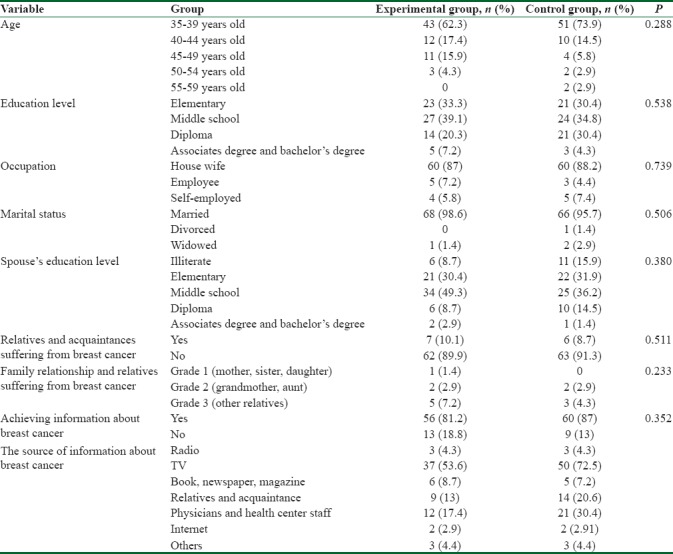
Regarding all variables, two groups before the intervention have no statistically significant differences except for knowledge, perceived susceptibility, perceived benefits, and perceived barriers to mammography based on an independent t-test (P > 0.05).
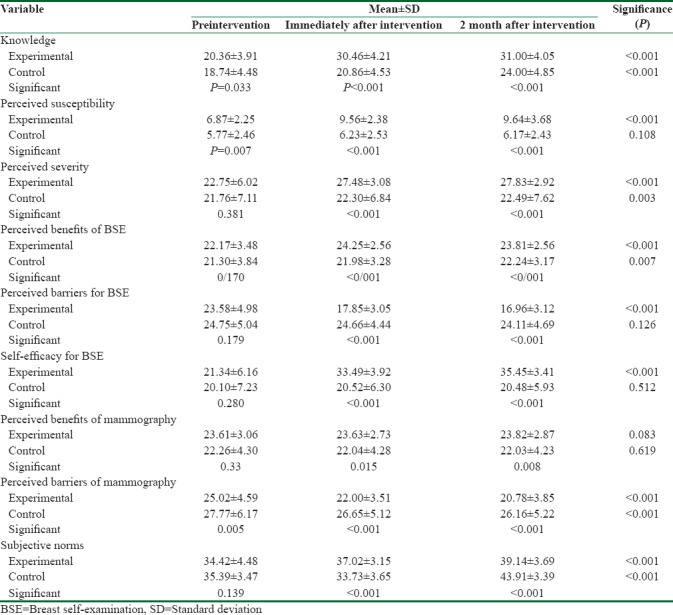
About the significance of differences in the chosen structures due to the lack of groups reassignment possibility (Geographical restrictions, cultural, economic, etc.). ANCOVA test was used to adjust these differences. There were significant differences in knowledge structure, perceived susceptibility and perceived severity, perceived benefits and perceived barriers and self-efficacy and perceived barriers for mammography, BSE and subjective norms after the training (P < 0.001), but there was no significant difference in the structure of perceived benefits of mammography (P > 0.001), R. M. ANOVA test results also showed that there was a statistically significant difference between the scores of knowledge, perceived susceptibility, perceived severity, perceived benefits and perceived barriers, self-efficacy, perceived barriers to mammography, BSE, subjective norms on three stages: before, immediately after and 2 months after intervention (P < 0.001), but in the perceived benefits of mammography this difference was not statistically significant (P = 0.083) [Table 3].
Table 3.
The comparison of the mean±standard deviation of integrated model structures before, immediately and 2 months after intervention in experimental and control groups
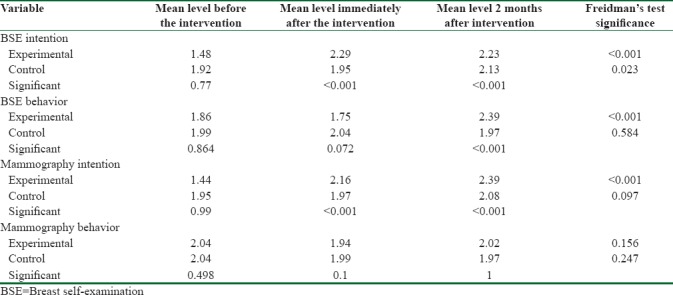
According to Mann-Whitney test, there was no significant difference between the average score of BSE behavioral intention (P = 0.77), BSE behavior (P = 0.864), mammography behavioral intention (P = 0.99), and mammography behavior (0.498) in the experimental group compared with the control group pretest (P > 0.001).
However, the significance level of BSE and mammography intention immediately after the intervention and also 2 months after the intervention was statistically significant (P < 0.001) Furthermore, BSE intention 2 months after the intervention was statistically significant (P < 0.001). However, there was no significant difference in mammography behavior (P > 0.001). Friedman test results show behavioral intention, BSE behavioral intention and mammography behavioral intention in experimental group before, immediately after and 2 months after educational intervention are in the significant level (P < 0.001). However, there was no significant difference in mammography behavior (P = 0.156) [Table 4].
Table 4.
Comparison of behavioral intention, breast self-examination behavior and mammography, before, immediately and 2 months after educational intervention in experimental and control groups
Discussion
This study aimed to evaluate the effect of an educational intervention based on the integrated model on the breast cancer screening behavior in women referred to health center of Mohammad shahr in Karaj. In this study, two groups in terms of demographic and background characteristics were similar at the beginning of intervention, and there was no statistically significant difference. Usually, the requirement of 2-groups intervention studies was assimilated that was observed in this research. Television was the main source of information about breast cancer in both experimental and control groups which is consistent with Nawab Rigi et al. study[10] but inconsistent with the study of ’ et al.[2]
That considered the doctors and staff as the main source of information. The results show the effectiveness of educational interventions to increase the knowledge about cancer and screening behaviors in the experimental group compared with the control group which was consistent with the conducted studies by Nasir Isfahani et al.[15] and Jahangiry et al.[17] The mean score of knowledge in experimental groups before, immediately after and 2 months after the intervention was significantly different and showed the increasing knowledge of breast cancer after intervention which was consistent with other studies.[17,36] Thus, educational intervention according to the purpose of the study can be effective as a predisposing factor for breast cancer screening and by using that the knowledge of women about breast cancer and its early diagnosis can be increased.
The mean difference in perceived susceptibility in the experimental group compared with the control group indicates the effectiveness of educational interventions in increasing the perceived Susceptibility of breast cancer in the experimental group. The results of conducted studies by Karimy et al.[37] and Jahangiry et al.[17] also indicate an increase in perceived susceptibility score after the educational intervention that is consistent with the findings of the present study.
Educational intervention was effective on the severity of breast cancer mean in the experimental group which is consistent with the findings of conducted studies by Jahangiry et al. that showed a significant increase in severity after the intervention.[17]
The results showed the effectiveness of educational interventions in increasing the perceived benefits of BSE in control group. The result of the study indicated that the educational intervention was effective in increasing the perceived benefits of BSE in test group compare the control group. Also, the mean score of BSE in three stages: before, immediately after and 2 months after the intervention was different, and this means that educational interventions were effective in increasing the mean score of perceived benefits regarding self-examination in the experimental group. The result is inconsistent with the Momenyan et al.[38] but consistent with Rahmati Najar Kolaie et al.[39] Karimy et al.,[37] and Tavafian et al.[36]
The results of the study show that the mean score of perceived benefits of breast mammography at the 0.001 level is not significant, this means that educational interventions in increasing the perceived benefits of mammography is not effective in the experimental group which is consistent with the results of the conducted study by Hadizadehtalasaz and Latifnejade[40] To verify above findings it can be said that the participated women in this study were informed of the benefits of mammography screening in reducing the risk of breast cancer or its worsening before training, so educational intervention was not effective.
A significant increase in the mean score of perceived barriers in experimental group about breast cancer and screening behaviors After the educational intervention is indicator of the effectiveness of intervention that is consistent with the results of Karimy et al.[37] Modi and et al.[2] and inconsistent with the conducted study by Hadizadehtalasaz and Latifnejade[40] The results of the study show that the score of perceived barriers of mammography after intervention at the 0.001 level was significant which presents the effect of the educational intervention on the perceived benefits of mammography increase that is consistent with the findings of the conducted study by Jahangiry et al.,[17] Taymoori and Berry[35] The results also show that mammography score of perceived barriers are significant in the control group. The reason of this change in the scores of the control group is not exactly clear, but filling pretest questionnaire can be one of the involved reasons and for other possible causes, can be noted that the participants may be trained through other methods and ways between the pretest and posttest. A significant increase in self-efficacy score after training indicates that the increase in the mean scores of self-efficacy presents that the educational intervention of breast cancer and screening behavior was effective in the experimental group. The conducted studies by Momenyan et al.,[38] Tvafiyan,[36] Aghamolai.[41] Confirms the findings of this study. The results of the study by Nawab Rigi et al. also suggest that self-efficacy is the predictor of BSE behavior.[10] To explain the results of this study it can be reasoned that an important factor in the formation of individuals’ self-efficacy is their family structure and this structure can affect person's belief in self-efficacy. Hence, it seems the cause of the significance of this relationship is the participation of subjects’ family in the training sessions and the distribution of leaflets between the husbands of women in group.
The results of the study show that the mean rates of BSE behavioral intention and mammography behavioral intention were significant after intervention this means that educational intervention was effective on groups that are consistent with conducted studies by Hatefnia et al.[42] Juon et al.[43] and Fletcher and et al., that represents an increase in intention for mammography in the experimental group after the intervention.[44]
A significant increase in perceived subjective norms score after intervention means that Educational intervention was effective in increasing the perceived subjective norms of breast cancer and screening behavior in the experimental group. Regarding person's belief in whether those who are around and important to her agree or disagree about doing it, The husband covered training tracts and sisters and mothers of the studied group were invited to attend the meetings, and the doctor was asked to explain about screening behavior to these people, this result is not unexpected. This study is consistent with the results of the conducted study by Hatefnia et al.[42] Syrjälä et al.[45] but is inconsistent with the results of the study which was done by but Astrom and Mashoto that shows that the subjective norms were not improved after the intervention.[46]
There was no significant difference between the average rate of BSE behavior immediately after the intervention, but 2 months after the intervention, this difference was statistically significant. Hence, we can conclude that the intervention is effective on the breast cancer self-examination behavior. In other words, intervention was not effective on doing mammography behavior that may be it is due to the short interval between pretest and follow-up. On the other hand, it seems that a longer time is required for screening behaviors and the number of training sessions should be increased because these groups of people refer the health centers less or health workers do not have enough time, or there are not enough staffs for education. Therefore, to have a perfect training on breast examination which is the third leading cause of women's death in Iran, it is suggested to have an extensive planning in health centers. Continuous training in this field for health caretakers is recommended. Consistent with these findings, the results of the study is inconsistent with the conducted studies by Karimy et al.[37] the Saat Saz et al.,[7] and Gözüm et al.[47] and also Russell et al. That showed there is 51% and 18% increase in breast screening respectively in intervention and the group that pamphlets were distributed.[48] Consistent with these findings Nasir Isfahani et al. showed that there was no significant difference in the mean score of breast screening behaviors in both groups before the intervention. Moreover, the difference in immediately and 2 months after the intervention has no significant difference as well.[15]
Finally, we can say that the decision of the people for doing or not doing breast screening behaviors is dependent on their opinions and attitudes that can be correctly changed by designing and implementing an interventional program based on health belief model and the theory of planned behavior.
Conclusions
In this study, to the strengthen the intervention with importance of by others effect on the behavior of the subjects, in addition to the health beliefs model, the structures of mental norms were used. The results of this study confirmed the effectiveness of the proposed integrated model behavior on women in breast cancer screening, because according to the findings of the study the role of the by others in encouraging women in screening behavior was verified. So, it can be used as a framework for interventions planning to promote breast cancer screening behaviors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. Health Topics. [Last accessed on 2016 Aug 22]. Available from: http://www.who.int/topics/cancer/en/
- 2.Moodi M, Mood MB, Sharifirad GR, Shahnazi H, Sharifzadeh G. Evaluation of breast self-examination program using health belief model in female students. J Res Med Sci. 2011;16:316–22. [PMC free article] [PubMed] [Google Scholar]
- 3.Mousavi SM, Gouya MM, Ramazani R, Davanlou M, Hajsadeghi N, Seddighi Z, et al. Cancer incidence and mortality in Iran. Ann Oncol. 2009;20:556–63. doi: 10.1093/annonc/mdn642. [DOI] [PubMed] [Google Scholar]
- 4.Emami Razavi SH, Aghajani H, Haghazali M, Nadali F, Ramazani R, Dabiri E, et al. The most common cancers in Iranian women. Iran J Public Health. 2009;38:109–12. [Google Scholar]
- 5.Yavari P, Abedi AR, Mehrabi Y. Mortality and changing epidemiological trends in Iran during 1970-2001. Hakim J. 2003;6:7–14. [Google Scholar]
- 6.Fouladi N, Pourfarzi F, Mazaheri E, Asl HA, Rezaie M, Amani F, et al. Beliefs and behaviors of breast cancer screening in women referring to health care centers in Northwest Iran according to the Champion Health Belief Model Scale. Asian Pac J Cancer Prev. 2013;14:6857–62. doi: 10.7314/apjcp.2013.14.11.6857. [DOI] [PubMed] [Google Scholar]
- 7.Saat Saz S, Rezaei R, Nazari R, Haji Hosseini F, Seyedi Andi SJ. Effect of educational intervention on condition of knowledge and practice. Iran J Breast Dis. 2009;2:28–35. [Google Scholar]
- 8.Asgharnia M, Faraji R, Zahiri Z, Salamat F, Mosavi Chahardah S, Sefati SA. Study of knowledge and practice of woman about breast cancer and its screening in the case of women who referred to Alzahra Hospital in Rasht during 2010-2011. Iran J Surg. 2013;21:35–42. [Google Scholar]
- 9.Movahedi M, Haghighat S, Khayamzadeh M, Moradi A, Ghanbari-Motlagh A, Mirzaei H, et al. Survival rate of breast cancer based on geographical variation in Iran, a national study. Iran Red Crescent Med J. 2012;14:798–804. doi: 10.5812/ircmj.3631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Navabi Rigi SH, Khojaste F, Bandani F. Breast cancer and breast self-examination: Knowledge and attitudes based on the health belief model in female students literature faculty of engineering university of Sistan and Baluchestan. J Breast Dis. 2012;5:65–72. [Google Scholar]
- 11.Setayeshi S, Akbari MA, Dargahi R, Haghighat Khah HR. Breast Cancer and Technical Analysis of its Diagnosis Methods: Logbook for Medical Physics Engineering and Radiology. Tehran: Bitarafan; 2011. pp. 13–4. [Google Scholar]
- 12.Attarian H, Pirzadeh A, Rezvani H. Clinico pathologic manifestations of Iranian patients with breast cancer. Pak J Med Sci. 2011;2:182–5. [Google Scholar]
- 13.Harirchi I, Karbakhsh M, Kashefi A, Momtahen AJ. Breast cancer in Iran: Results of a multi-center study. Asian Pac J Cancer Prev. 2004;5:24–7. [PubMed] [Google Scholar]
- 14.Akbari ME, Haghighatkhah H, Shafiee M, Akbari A, Bahmanpoor M, Khayamzadeh M, et al. Mammography and ultrasonography reports compared with tissue diagnosis – An evidence based study in Iran, 2010. Asian Pac J Cancer Prev. 2012;13:1907–10. doi: 10.7314/apjcp.2012.13.5.1907. [DOI] [PubMed] [Google Scholar]
- 15.Nasir Isfahani S, Ghaffari M, Hatami H, Sorui H. Tehran: Shahid Beheshti University of Medical Sciences; 2012. Effect of Health Belief Model-Based Education on Breast Cancer Screening Behaviors among Health Volunteers in Health Center of Isfahan. MSc [Thesis] [Google Scholar]
- 16.American Cancer Society. Cancer Facts & Figures 2012. Atlanta: American Cancer Society; 2012. [Last accessed on 2013 Dec 17]. pp. 9–10. Available from: http://www.cdc.gov/cancer . [Google Scholar]
- 17.Jahangiry L, Shojaei Zadeh D, Mahmoody M. Application of HBM on studying of knowledge and attitude of women referring to health centers of Azarshahr about prevention of breast cancer 2007. Tolooebehdasht. 2007;6:65–74. [Google Scholar]
- 18.Rastad H, Shokohi L, Dehghani SL, Motamed Jehromi M. Assesment of the awareness and practice of women vis- a- vis breast self-examination in Fasa in 2011. J Fasa Univ Med Sci. 2013;3:75–80. [Google Scholar]
- 19.Aliramaei N, Fathi M, Mahmoudi SH, Zabiri K. The screening breast cancer and mammography findings in women attending unity medical center radiology department Sanandaj. Iran J Breast Dis. 2009;2:12–9. [Google Scholar]
- 20.Ashrafi Asgharabad A, Khani Jani N, Saber M, Jalili S, Khedmati E. Knowledge and attitude of students at Alzahra university about breast self-examination. J Health Dev. 2012;1:112–20. [Google Scholar]
- 21.Ferlay J, Bray F, Pisani P, Parkin D. GlOBOC AN 2002: Cancer incidence, mortality and prevalence world wide. IARC Cancer. 2004;5:20. [Google Scholar]
- 22.Moodi M, Sharifirad GR, Tahergorabi Z, Mostafavi F. 1st ed. Vol. 16. Isfahan: Publication of Medical University of Isfahan; 2011. Get to Know Breast Cancer Pathway Toward Health; pp. 12–80. [Google Scholar]
- 23.Ghorbani M, Abdolahi AA, Royani S, Azizi R. Comparison knowledge, attitude and practice of breast self-examination. Iran J Breast Dis. 2009;2:36–42. [Google Scholar]
- 24.Sadeghnezhad F, Niknami SH, Ghaffari M. Effect of health education methods on promoting breast self-examination (BSE) Sci J Birjand Univ Med Sci. 2008;15:38–48. [Google Scholar]
- 25.Glanz K, Rimer BK, Lewis FM. Health Behavior and Health Education: Theory, Reaserch, and Practice. 3rd ed. New Jersey: Jossey-Bass; 2002. pp. 45–65. [Google Scholar]
- 26.Sharifirad G, Entezari MH, Kamran A, Azadbakht L. The effectiveness of nutritional education on the knowledge of diabetic patients using the health belief model. J Res Med Sci. 2009;14:1–6. [PMC free article] [PubMed] [Google Scholar]
- 27.Sahraei A, Novroozi A, Tahmasebi R. Predicting factors of breast self-examination based on health belief model a locus of control among women aged 20-50. Hayat J Sch Nurs Midwifery Tehran Univ Med Sci. 2013;19:27–39. [Google Scholar]
- 28.Ghaderi N, Taymoori P, Yousefi F, Nouri B. The prevalence of cigarette smoking among adolescents in Marivan City-Iran: Based on Health Belief Model (HBM) Int J Pediatr. 2016;4:3405–14. [Google Scholar]
- 29.Mohammadi S, Ghajari H, Valizade R, Ghaderi N, Yousefi F, Taymoori P, et al. Predictors of smoking among the secondary high school boy students based on the health belief model. Int J Prev Med. 2017;8:24. doi: 10.4103/ijpvm.IJPVM_264_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yuk Yee Y. Breast cancer: Knowledge and perceptions of chinese women in Hong Kong. Glob J Health Sci. 2009;1:97–105. [Google Scholar]
- 31.Shirly R, Asadolahi KH, Asadollahi P. Risk perception and preventive issues for breast cancer among female employees. Iran J Cancer Prev. 2010;3:166–73. [Google Scholar]
- 32.Noori Zadeh R, Bakhtiary Aghdam F, Sahebi L. Knowledge, health beliefs and breast cancer screening behaviors of women referring to health centers of Tabriz 2010. Iran J Breast Dis. 2010;3:43–51. [Google Scholar]
- 33.Nafisi N, Saghafi Niya M, Akbari M, Najafi S. Survey to determine knowledge and attitudes of women towards breast cancer. Breast Dis Q Iran. 2010;3:28–33. [Google Scholar]
- 34.Butler JT. 3rd ed. United States of America: Wadsworth: A Division of Thomson Learning Inc; Principles of Health Education and Health Promotion. [Google Scholar]
- 35.Taymoori P, Berry T. The validity and reliability of champion's health belief model scale for breast cancer screening behaviors among Iranian women. Cancer Nurs. 2009;32:465–72. doi: 10.1097/NCC.0b013e3181aaf124. [DOI] [PubMed] [Google Scholar]
- 36.Tavafian SS, Hasani L, Aghamolaei T, Zare S, Gregory D. Prediction of breast self-examination in a sample of Iranian women: An application of the health belief model. BMC Womens Health. 2009;9:37. doi: 10.1186/1472-6874-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karimy M, Niknami SH, Amin Shokravy F, Samsi M, Hatami A. The relationship of breast self-examination with self-esteem and perceived benefits/barriers of self-efficacy in health volunteers of Zarandieh city. Iran J Breast Dis. 2009;2:41–8. [Google Scholar]
- 38.Momenyan S, Rangraz Jedi M, Sanei Irani F, Adibi Garakhani Z, Sarvi F. Prediction of breast self-examination in a sample of nursing and midwifery students using health belief model. Qom Univ Med Sci J. 2014;8:28–33. [Google Scholar]
- 39.Rahmati Najar kolaie F, Ebadifard Azar F, Rimaz SH. Effects of training breast-cancer screening on female university students’ beliefs. Iranina Journal of Obstetrics Gynecology and Infertility. 2012;23:25–31. [Google Scholar]
- 40.Hadizadehtalasaz F, Latifnejade R. The effect of health education based on health belife model on attitude female students towards breast self examination. J Birjand Univ Med Sci Health Serv. 2004;1:25–30. [Google Scholar]
- 41.Aghamolaei T, Hasani L, Tavafian SS, Zare S. Improving breast self-examination: An educational intervention based on health belief model. Iran J Cancer Prev. 2011;4:82–7. [Google Scholar]
- 42.Hatefnia E, Niknami SH, Mamoudi M, Ghofranipour F, Lamyian M. The effect of health belief model education on knowledge attitude and behavior of Tehran pharmaceutical industry employees. Behbood. 2010;14:42–53. [Google Scholar]
- 43.Juon HS, Choi S, Klassen A, Roter D. Impact of breast cancer screening intervention on korean-american women in Maryland. Cancer Detect Prev. 2006;30:297–305. doi: 10.1016/j.cdp.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 44.Fletcher SW, Harris RP, Gonzalez JJ, Degnan D, Lannin DR, Stretcher VJ, et al. Increasing mammography utilization: A controlled study. J Natal Cancer Instr. 1993;85:12–112. doi: 10.1093/jnci/85.2.112. [DOI] [PubMed] [Google Scholar]
- 45.Syrjälä AM, Niskanen MC, Knuuttila ML. The theory of reasoned action in describing tooth brushing, dental caries and diabetes adherence among diabetic patients. J Clin Periodontol. 2002;29:427–32. doi: 10.1034/j.1600-051x.2002.290507.x. [DOI] [PubMed] [Google Scholar]
- 46.Astrom AN, Mashoto KO. Changes in oral health related knowledge, attitudes and behaviours following school based oral health education and atraumatic restorative treatment in rural Tanzania. Norsk Epidemiol. 2012;22:21–32. [Google Scholar]
- 47.Gözüm S, Karayurt O, Kav S, Platin N. Effectiveness of peer education for breast cancer screening and health beliefs in Eastern Turkey. Cancer Nurs. 2010;33:213–20. doi: 10.1097/NCC.0b013e3181cb40a8. [DOI] [PubMed] [Google Scholar]
- 48.Russell KM, Champion VL, Monahan PO, Millon-Underwood S, Zhao Q, Spacey N, et al. Randomized trial of a lay health advisor and computer intervention to increase mammography screening in African American women. Cancer Epidemiol Biomarkers Prev. 2010;19:201–10. doi: 10.1158/1055-9965.EPI-09-0569. [DOI] [PMC free article] [PubMed] [Google Scholar]


