Abstract
Objective:
The goals of the current study were to determine the average affective experiences in the weeks and months after a hip fracture and assess how these experiences relate to physical and mental health functioning over time.
Method:
Positive and negative affect were assessed over time in a sample of older adults recruited after surgery for hip fracture (n 500) and a comparison sample of older adults without hip fracture (n 102) for 1 year longitudinally.
Results:
For most of the individuals with a hip fracture, positive affect tended to increase over time and negative affect tended to decrease over time, suggesting that most people had at least some recovery of affect. In addition, individuals who showed a slower decrease in negative affect had higher levels of depression 1 year later, and individuals who showed a sharper increase in positive affect had superior physical function 1 year later.
Conclusion:
The current study provides evidence that both positive and negative affect in the first 12 weeks of recovery from hip fracture are potential targets for intervention to maximize psychological and physical recovery in the ensuing year.
Keywords: hip fracture, positive affect, negative affect, longitudinal, latent trajectory
Hip fracture is a prevalent and debilitating injury among older adults that is associated with considerable impairment, including physical dependence and disability, decreased social activity, increased symptoms of depression (e.g., Magaziner, Simonsick, Kashner, Hebel, & Kenzora, 2000), and increased mortality (Braithwaite, Col, & Wong, 2003). Given the prevalence (300,000 persons in the United States annually; U.S. Congress, Office of Technology Assessment, 1994) and severity of hip fractures, determining how to help individuals recover most effectively could reduce the burden of this event from multiple perspectives, including medical costs, mental and physical health of the individual, and burden on family caregivers. Researchers have converged on the notion that the psychological state of the individual who has had a hip fracture is highly relevant for determining how well that person recovers (e.g., Fredman, Hawkes, Black, Bertrand, & Magaziner, 2006). Yet much remains unknown about the role of affect in recovery from hip fracture, including the following: (a) the trajectory of affect after a hip fracture, (b) which variables predict this trajectory, and (c) how this trajectory relates to important physical and mental health outcomes. First, prior research and theory on the previous questions are reviewed and then aims for advancing knowledge in these areas are outlined.
Much of the previous literature on the first issue, affective trajectory, has focused on the associated increase in depression following a hip fracture. Previous research indicates that medical events such as hip fracture and associated physical disability can lead to an increased risk for depression (e.g., Lenze et al., 2001). In addition, Mossey, Mutran, Knott, and Craik (1989) found that individuals with higher postsurgery depression scores had poorer physical and mental health recovery. Taken together, these findings indicate a bidirectional relationship between depression and physical functioning. Regarding the mechanism behind this relationship, Lenze et al. (2001) proposed a model in which depression leads to various physical and psychological consequences, such as lack of motivation and decreased appetite, which in turn lead to greater physical disability. However, hip fracture patients represent a heterogeneous group (i.e., not all patients will develop depression), and it is unclear from previous literature how a hip fracture impacts affect in general beyond raising the risk for depression.
Furthermore, affect is not a unitary construct, but rather is comprised of both positive and negative affect, both of which relate to depression (Brown, Chorpita, & Barlow, 1998). Indeed, previous evidence supports the deleterious impact of negative affect on physical health (Dua, 1994). Finch, Baranik, Liu, and West (2012) theorized a reciprocal relationship between negative affect and health, whereby elevated negative affect triggers health problems through associated physical changes such as sleep disturbance (Steptoe, Dockray, & Wardle, 2009), and health problems result in higher levels of negative affect by causing elevations in stress and physical discomfort (Watson & Pennebaker, 1989). In addition to support for a relationship between negative affect and physical health, the role of positive affect in physical recovery has also been investigated.
In support of the role of reduced positive affect in detracting from recovery, Fredman and colleagues (2006) investigated the relationship between trait positive affect, depression, and physical recovery from a hip fracture in a sample of older adults and found that participants with high positive affect had significantly better physical functioning at each follow-up point than participants with high depressive symptoms. Although these results support an association between positive affect and physical recovery after a hip fracture, it is unclear whether those with higher trait positive affect tend to show superior physical health in general or whether the presence of higher positive affect during recovery confers a specific benefit. In addition, as mentioned earlier, the relative contribution of positive and negative affect remains unclear. Thus, to extend this research, levels of both positive and negative affect throughout the recovery process were assessed to determine the relative influence of each.
Accordingly, the current study concerns a large longitudinal investigation of hip fracture patients who were well-characterized in terms of positive and negative affect, physical functioning, and cognitive functioning at multiple time points. Auto-regressive latent trajectory analyses (ALT; Curran & Bollan, 2001) were used because this approach is best suited to the theoretical questions of interest. That is, to investigate trajectories of affect, slopes (the patterns of change in positive and negative affect over time), and intercepts (where people started off), were calculated for each individual. Recovery was defined as an increase in positive affect over time (i.e., post hip fracture) and a decrease in negative affect over time. A general tendency for an increase in positive affect and a decrease in negative affect over time in patients with hip fracture was expected, which would be reflected by a significant average slope for both positive and negative affect. Significant variability in the patterns of change (slopes) for both positive and negative affect was also expected, indicating that the extent to which people recover varies across individuals. Notably, prior researchers have examined whether there might be groups of participants who tend to show similar trajectories after medical injuries (i.e., rapid recovery group, slow recovery group, etc.). Though these analyses present an interesting alternative approach, there was no theoretical reason to expect groups and thus the more statistically powerful approach of focusing on continuous measures was used.
Regarding the second issue raised earlier, concerning what variables predict who recovers, one of the goals of the current study was to test how certain psychosocial variables might influence trajectories of affect over time to determine who might be at risk for maladaptive affective patterns during recovery. To that end, variables that have either been shown to relate to affect or might be expected to relate to affect after a medical event, such as social support, depression, age, general physical health, and education were identified and included as baseline predictors of affect trajectories. It was expected that lower social support, higher depression, higher age, more cumulative illnesses, lower education, and being single or divorced would be associated with worse recovery of affect.
Finally, per the third issue of whether affective recovery predicts future recovery, tests of how patterns of positive and negative affect related to important indices of physical and psychological functioning 1 year postfracture were conducted. One of the primary questions was whether patterns of positive and negative affect would relate to physical functioning as has been shown with trait positive affect and depression in previous research (Fredman et al., 2006; Lenze et al., 2001). The relationship between affective recovery and cognitive functioning was also of interest. Previous research supports that positive affect facilitates aspects of cognitive functioning such as creative problem solving (e.g., Isen, Daubman, & Nowicki, 1987), whereas depression predicts decreased cognitive functioning (Austin, Mitchell, & Goodwin, 2001). Thus, it was theorized that patients who experience lower levels of positive affect (or higher negative affect) as a result of a hip fracture will have decreased cognitive functioning. Finally, tests of whether patterns of affect during recovery translate into psychological consequences that are still present at 1 year postfracture were conducted. Depression and a measure of stressful life events were used as indicators of general psychological functioning because these variables were conceptualized as constructs that would be highly likely to capture and track psychological distress of many forms. It was hypothesized that the slopes of affect would predict the number of stressful life events experienced, level of depression, physical functioning, and cognitive functioning at 1 year postsurgery, above and beyond baseline measures.
Hypotheses were informed by a theoretical model of the factors that contribute to affective recovery after a stressful event and how that affective recovery then influences future outcomes. It was theorized that certain baseline variables would influence the affective reactions to a hip fracture. For example, certain premorbid variables such as social support and depression might identify individuals who are at greater risk for a more maladaptive reaction. It was also expected that the levels of positive and negative affect during recovery would influence the extent of recovery down the road by influencing behaviors such as engagement in rehabilitation. For example, a person with lower social support might be at higher risk for experiencing lower positive affect after a hip fracture because of less contact with supportive people. Lower levels of positive affect might then lead to decreased motivation to perform rehabilitation exercises thus leading to decreased physical recovery over time. This example presents just one of many pathways linking psychosocial variables to behaviors to physical health. Ultimately, in keeping with the hypotheses of previous researchers (Finch et al., 2012), bidirectional relationships between emotions and health were expected, resulting in vicious cycles whereby maladaptive emotional reactions lead to physical health problems, which in turn lead to maladaptive emotional reactions, and so on. To assist in interpretation of change over time in the hip fracture group, a comparison group of healthy controls matched by age, gender, and ethnic/racial composition was included. This group was included to test whether any patterns or relationships found in the patient group could not be better explained by normative age-related processes.
Method
Participants
A sample of individuals (N = 602) including hip fracture participants (n = 500) and nonfracture comparisons (n = 102) completed a series of clinician-administered psychological, functional, and cognitive assessments. Participants received $100 for their participation. Participants were predominately women (n = 446, 73.8%) and White (n = 559, 92.5%), with a mean age of 78.40 years (SD = 8.55; range = 60 to 101). Other ethnicities reported were Black (n = 41, 6.8%) and Asian or Pacific Islander (n = 3, 0.5%). Years of education ranged from 2 to 26 (M = 13.40, SD = 2.94). Please see Table 1 for descriptives separated by group.
Table 1.
Participant Characteristics
| Age | Gender | Education | Race | Baseline positive affect | Baseline negative affect | Baseline MADRS | Baseline DSSI | Baseline CIRS-G | Baseline HFR | |
|---|---|---|---|---|---|---|---|---|---|---|
| Patients | 78.37 (8.62) | 1.75 (.43) | 13.05 (2.85)* | 93.2% White | 10.76 (3.24)* | 10.55 (4.67)* | 3.19 (4.25) | 10.31 (2.06) | 12.64 (3.71)* | 94.74 (9.81) |
| Controls | 77.61 (7.53) | 1.68 (.47) | 15.07 (2.78)* | 90.2% White | 13.31 (2.98)* | 6.85 (2.21)* | 2.96 (3.30) | 9.97 (1.57) | 8.86 (4.14)* | 98.21 (3.67) |
Note. MADRS Montgomery Asberg Depression Rating Scale; DSSI Duke Social Support Index; CIRS-G Cumulative Illness Rating Scale for Geriatrics; HFR Hip Fracture Recovery Scale. Mean values are listed with SDs in parentheses.
Significant difference, p < .001.
Patients were recruited from the orthopedic departments of eight St. Louis-area hospitals between 2 and 14 days after surgical hip fracture repair. Control participants were community-dwelling, cognitively intact older adults recruited primarily from Washington University Medical School’s adult volunteer pool. The comparison group was matched to the patient group by age, gender, and ethnic/racial composition. Exclusion criteria included language, visual, or hearing barriers to participation, a nonoperable fracture or refracture through prosthesis, metastatic cancer, inability to provide informed consent or cooperate with protocol, the presence of a current major depressive episode at baseline that predated the hip fracture (or baseline evaluation for nonfracture comparisons), presence of dementia or persistent delirium, or the use of depressogenic medications (e.g., high-dose steroids). Table 2 displays the percentage of participants at each residential setting type at each time point, as well as which assessments were given at each time point.
Table 2.
Residential Settings and Assessments Administered Across Time
| Baseline | Week 1 | Week 2 | Week 4 | Week 8 | Week 12 | Week 26 | Week 52 | |
|---|---|---|---|---|---|---|---|---|
| Setting | ||||||||
| Home no supervision | — | 5.2% | 15.3% | 30.6% | 41.8% | 47.2% | 49.5% | 50.1% |
| Home partial supervision | — | 4.6% | 7.2% | 9.3% | 9.7% | 10.1% | 9.9% | 7.2% |
| Home fulltime supervision | — | 6.4% | 13.5% | 17.4% | 14.7% | 13.9% | 9.1% | 5.2% |
| Assisted living | — | 0.6% | 0.6% | 1.7% | 1.9% | 2.7% | 2.5% | 4.8% |
| Rehab facility | — | 19.5% | 10.4% | 2.9% | 1.2% | 0.2% | 1.0% | 1.9% |
| Skilled nursing facility with rehab | — | 48.2% | 37.3% | 19.9% | 8.1% | 4.1% | 2.7% | 0.4% |
| Skilled nursing facility without rehab | — | 0.2% | 0.2% | 0.4% | 0.0% | 0.4% | 0.2% | 1.0% |
| Assessments | PANAS | PANAS | PANAS | PANAS | PANAS | PANAS | PANAS | PANAS |
| MADRS | MADRS | MADRS | MADRS | MADRS | MADRS | MADRS | MADRS | |
| DSSI | DSSI | |||||||
| CIRS-G | GALES | GALES | GALES | GALES | ||||
| RBANS | RBANS | |||||||
| HFR | HFR | HFR | HFR | HFR | HFR | HFR | HFR |
Note. PANAS = Positive and Negative Affect Schedule; MADRS Montgomery Asberg Depression Rating Scale; DSSI Duke Social Support Index; CIRS-G = Cumulative Illness Rating Scale for Geriatrics; GALES = Geriatric Adverse Life Events Scale; RBANS = Repeatable Battery for the Assessment of Neuropsychology Status; HFR = Hip Fracture Recovery Scale. Setting information is not given for baseline because the majority of patients were in the hospital.
Measures
The Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988) contains two scales employing a 1 (very slightly or not at all) to 5 (extremely) Likert-type scale. An abbreviated version of the measure that assesses positive activated affect and negative activated affect with 5 items each (Mackinnon et al., 1999) was used. Participants were asked to rate the items in terms of how they felt over the last week. In the current study, the excited item from the positive affect scale was excluded based on previous research suggesting that responses on this item may differ based on age, marital status, and education (Mackinnon et al., 1999). Overall, the scales used here have shown good internal consistency, a two-factor structure, and invariance across age in previous research (Mackinnon et al., 1999). The scales at each of these five time points considered showed adequate to good internal consistency (s from .68 to .82); notably the reliability of the slope and intercept parameters estimated from the five time points should be superior to the individual administration internal consistencies.
The Montgomery Asberg Depression Rating Scale (MADRS; Montgomery & Asberg, 1979) is a 10-item measure of severity of depressive symptoms. A 7-day and a 24-hr version were used. Montgomery and Asberg (1979) reported high interrater reliability and sensitivity to change. In the current study, the 7-day version from baseline and Week 52 was used and internal consistency was adequate (α.65 and .71, respectively).
The Duke Social Support Index (DSSI; Koenig et al., 1993) is a 23-item abbreviated version of the original scale (Landerman, George, Campbell, & Blazer, 1989). The DSSI measures three major dimensions of social support: social interaction, subjective support, and instrumental support. Koenig and colleagues (1993) reported good reliability and validity of the three subscales. In the current study, the subjective support subscale was used as our indicator of social support; higher scores indicate less subjective support. At baseline, the subjective support subscale had good internal consistency (α = 78).
The Cumulative Illness Rating Scale for Geriatrics (CIRS-G; Miller et al., 1992) is an adaptation of the original CIRS scale (Linn, Linn & Gurel, 1968) that measures chronic medical illness in geriatric populations. The CIRS-G has good interrater reliability and face validity (Miller et al., 1992). Internal consistency is not given for this measure because it is not assumed that a checklist of medical conditions should necessarily be internally consistent.
The Geriatric Adverse Life Events Scale (GALES; Devanand, Kim, Paykina, & Sackeim, 2002) is a 26-item measure of the type and impact of life events often experienced by older adults. For each item, the respondent first evaluates whether the event occurred and then rates the event from not at all stressful to very stressful, if applicable. Internal consistency is not given because it is not assumed that a checklist should necessarily be internally consistent.
The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS; Randolph, Tierney, Mohr, & Chase, 1998) is a clinician-administered neuropsychological battery used for the detection of cognitive deficits in older adults. The RBANS was administered at Week 4 and Week 52. There were two forms to eliminate any memory effects. Participants received one of the forms at the first assessment and received the opposite form at the later assessment.
The Hip Fracture Recovery Scale (HFR) includes items that assess basic activities of daily living and instrumental activities of daily living that were assembled for the current study. The final component is a mobility rating. To obtain the most comprehensive estimate of physical functioning, we used the total score. This scale is used in the analyses as an index of physical recovery from the hip fracture. At baseline and Week 52, internal consistency for the total score was very good (αs > .87).
Procedure
The following procedure was approved by the Washington University in St. Louis Institutional Review Board. Participants were assessed at 8 time points. All measures were administered verbally, with visual aids when measures were given in person. Time points were as follows: baseline, Week 1, Week 2, Week 4, Week 8, Week 12, Week 26, and Week 52 postsurgery. For both groups of participants, the baseline, Week 4, and Week 52 assessments were conducted in person and the other assessments were conducted via telephone. All three of the in-person interviews were completed in the participant’s home for control participants. Participants provided written consent at the baseline assessment. For the hip fracture group, the baseline appointment usually occurred at the hospital 2 to 7 days postsurgery, and the remaining in-person assessments were conducted at varying locations including hospitals, rehabilitation and/or skilled nursing facilities, and patient homes. The possible effects of in-person visits on affect were accounted for during the modeling process (see Results).
Data Analytic Procedure
Longitudinal measurement invariance testing.
PANAS items from Week 1 to Week 12 were included in the analyses. Tests of longitudinal invariance were conducted using the weighted least squares with robust standard errors and mean- and variance-adjusted chi-square (WLSMV) estimator implemented in the Mplus program (Version 4; Muthén & Muthén, 1998–2009; Vandenberg & Lance, 2000). This testing was important for determining whether the affect items appeared to capture the same construct over time and whether the participants responded to the items in the same manner over time. In each case, an acceptably invariant model was achieved (i.e., only as many parameters as necessary were unconstrained to achieve acceptable fit) and factor scores were outputted for use in further analyses.
Multiple imputation.
Multiple imputation analyses were conducted in Amelia II (Honaker, King, & Blackwell, 2006–2008) to address missing data, primarily from the predictor variables. About 30% of the patients (151 out of 500) had at least some missing data. Multiple imputation was performed on a dataset that included factor scores for the affect variables (e.g., those outputted from longitudinal invariance models), as well as the predictor and outcome variables in their original form.
Auto-regressive latent trajectory (ALT) analyses.
ALT analyses (Curran & Bollan, 2001) were used to estimate intercepts and slopes of the positive and negative affect factor scores outputted from the longitudinal invariance testing. For the ALT analyses, the robust maximum likelihood (MLM) estimator was used because the factor scores estimated from each time point were unlikely to be multivariate normal. Global model fit was evaluated using the following: Tucker-Lewis Index (TLI; Tucker & Lewis, 1973), Comparative Fit Index (CFI; Bentler, 1990), the root mean square error of approximation (RMSEA; Steiger & Lind, 1980), and the square root-mean-square residual (SRMR; Bentler, 1995; Jöreskog & Sörbom, 1981). Generally, the following values indicate a good fit of the model to the data: TLI and CFI from .95 to 1.0, RMSEA below .06, and SRMR below .08 (cf. Hu & Bentler, 1999).
Initial tests produced inadequate fit that appeared to stem from the affects at Week 4 being higher than a linear trajectory would predict. Given that this assessment (unlike the others) was conducted in person, there was concern that participants may have experienced increased activation because of being in the presence of another person. Thus, an additional slope factor (coded 0, 0, 1, 0, 0) was calculated so that slope parameter estimates would be made in the context of a slope representing method variance (in person or not). Variables representing whether the participant was at home or not (vs. assisted living facility, etc.) were also included for the first three time points, because some of the variance in affect was likely because of variability in the participants’ residential settings. The parameters of the slope for the last two time points were adjusted in an iterative fashion until fit ceased to improve, resulting in each case in a slope that was only partially linear. Finally, autoregressive parameters (each time point regressed on the next time point) were included if indicated to improve model fit (Curran & Bollan, 2001).
Multiple group model tests.
Multiple instances of perfectly related items prevented the use of longitudinal invariance testing in the controls’ data. Attempts to circumvent this problem through multiple imputation were also unsuccessful. Therefore, analyses with both patients and controls were conducted on the raw data. The purpose of these analyses was to ensure that any changes in the patients could not be better explained by normative age-related changes unrelated to hip fracture. Thus, these analyses are useful in comparing the two groups, but given that tests of longitudinal invariance and estimation of missing data were not conducted, the slope values from these analyses are not the best estimates of these values.
Results
Tests of Group Demographic Differences
The groups showed a significant difference in years of education, t(540) = 6.15, p < .001, with the controls reporting more years of education (M = 15.07, SD 2.78) than the patients (M = 13.05, SD = 2.85). The groups did not differ with respect to age t(594) = .83, p = .407, gender,χ2(1, N = 603) 2.51, p = .113, or ethnicity χ2(2, N = 603) 2.31, p = .32.1
Positive Affect Tended to Increase Over Time
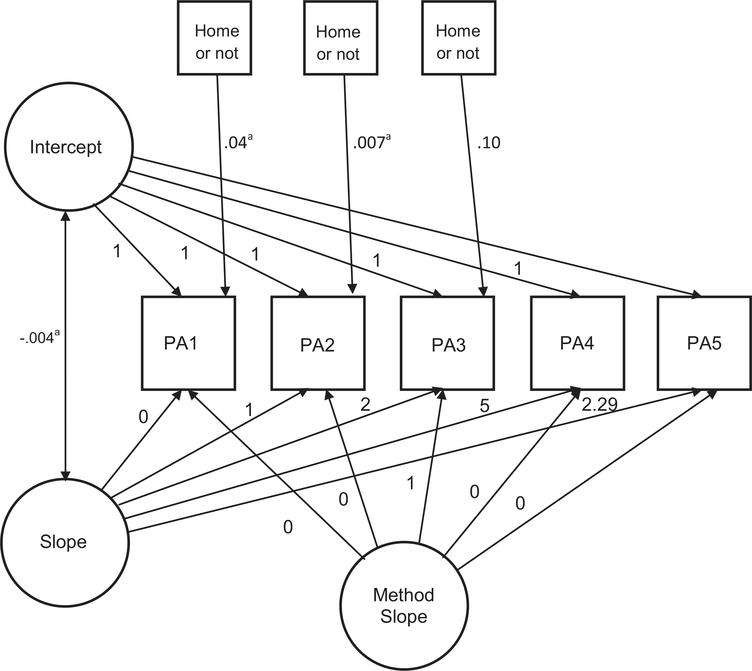
To test the hypothesis that patients would show a general trend of increasing positive affect over time, an intercept and slope of positive affect were estimated across five time points. The final positive affect model included a slope of positive affect, a slope representing assessment method, and relationships between the first three time points and the home-or-not variables. Autoregressive parameters were not included because they failed to improve model fit. Fit for the final model was adequate to good (CFI = .98, TLI = .98, RMSEA = .07, SRMR = .07). For the intercept, there was a nonsignificant mean (p = .375) and a significant variance (variance = .64, p < .001). As hypothesized, there was a general trend of increasing positive affect over time (M = .024, p < .001) and significant variance among individual slopes (variance = .01, p < .001). The slope was nearly linear with a peak at Week 8 and then a decrease at Week 12, suggesting that patients showed an increase in positive affect over time that peaked and then leveled off. There was also significant variation between individuals in terms of the course or rate of their recoveries (i.e., not everyone recovered to the same extent or at the same rate). The home-or-not variables were nonsignificantly related to positive affect for Week 1 and Week 2 (ps > .78), but at Week 4, patients who were living at home had higher positive affect (fully standardized parameter [fsp] = .10, p = .011). Figure 1 displays the positive affect model.
Figure 1.
People recover some, but not all, positive affect over time after hip fracture. Initial level and systematic change in positive affect are shown at five time points with an additional slope representing assessment method and variables representing whether patients were residing at home or some other residential setting. a Nonsignificant parameter; other parameters p < .05.
Negative Affect Tended to Decrease Over Time
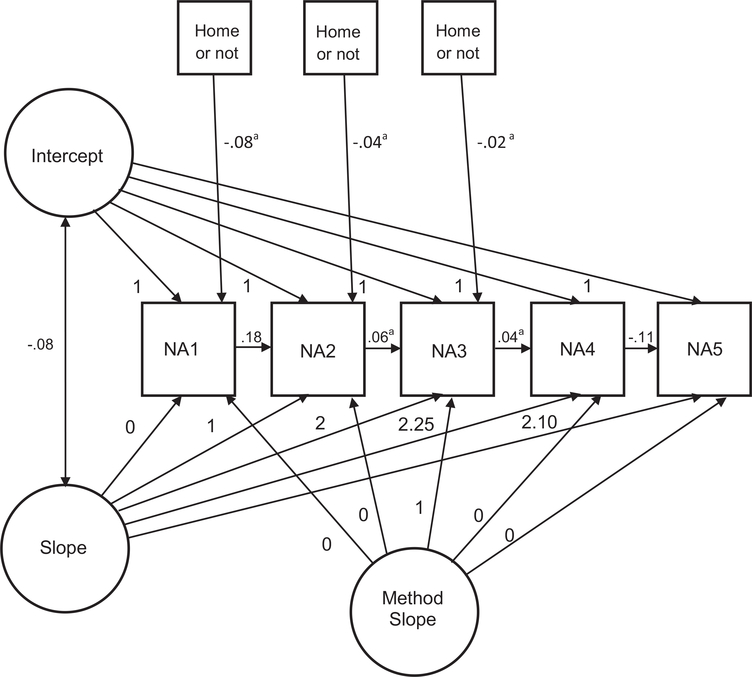
To test the hypothesis that patients would show a general trend of decreasing negative affect over time, an intercept and slope of negative affect were estimated across five time points. The final model included a negative affect slope, a method variance slope, autoregressive parameters, and the home-or-not variables and had acceptable to excellent fit (CFI = .99, TLI = .98, RMSEA = .07, SRMR = .06). The model indicated a significant mean intercept (M = .08, p = .049) and a significant intercept variance (variance = .68, p < .001). As hypothesized, there was a significant mean slope (M = −.25, p < .001) and a significant variance for slope (variance = .09, p < .001). The slope was near linear with a decrease in negative affect followed by a plateau. In sum, it appears that patients showed a decline in negative affect over time, though there was significant variation among individuals in terms of the trajectories or rates of recovery. Two out of four of the autoregressive parameters were significant: negative affect at Week 1 significantly predicted negative affect at Week 2 (fsp = 18, p < .001) and negative affect at Week 8 significantly predicted negative affect at Week 12 (fsp = −.11, p <.001), indicating special relationships in negative affect at those time points above and beyond intercept and slope. The home-or-not variables were not significantly related to negative affect, though the home-or-not variables at Week 1 and Week 2 approached significance (fsp = −.08, p = .063; fsp = −.04, p = .071, respectively). Figure 2 displays the negative affect model.
Figure 2.
People tend to recover most of their decreased negative affect over time after hip fracture. Initial level and systematic change in negative affect are shown at five time points with an additional slope representing assessment method and variables representing whether patients were residing at home or some other residential setting. Autoregressive parameters are also included. a Nonsignificant parameter; other parameters p <.001.
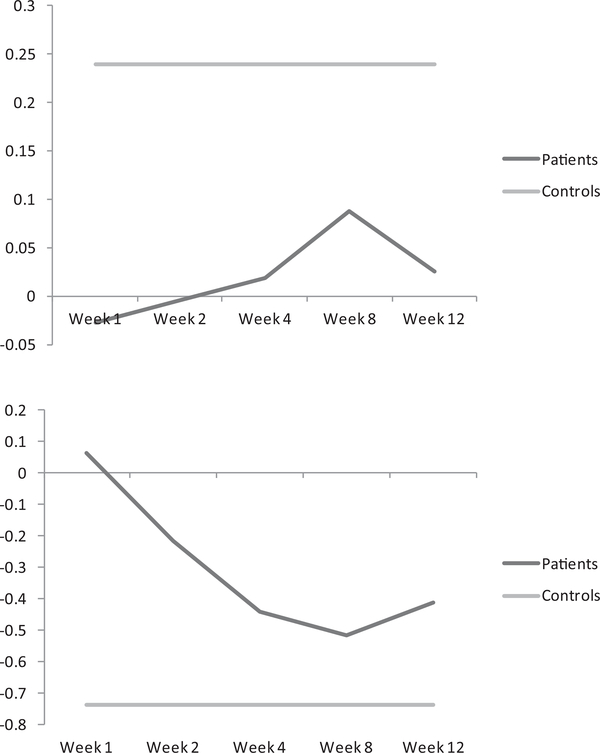
Slopes in Patients Differ Significantly From Controls
To test whether the results could be attributed to normal agerelated changes, models that included both controls and patients were analyzed. A model in which the slopes were allowed to vary across the groups was compared with a model in which they were constrained for both positive and negative affect. In both cases, the unconstrained model was significantly better fitting than the constrained model (ps < .001), suggesting that the slopes were not attributable to normative age related changes and that the trajectories of affect were significantly different between the two groups. Figures 3 presents the best estimates of the slopes for positive and negative affect over time, constructed using the factor scores from the longitudinal invariance testing. Because it was not possible to calculate the best estimates of the controls’ slopes2, the controls’ intercept values are shown for each time point as a comparison and reference point for levels of positive and negative affect that might be considered a full recovery. The intercept values were converted to the same metric as the patients’ values.3
Figure 3.
Slope of positive affect (top) and negative affect (bottom) over time in patients with controls’ intercept shown for comparison. The metric of the y-axis represents factor scores based on the longitudinal invariance testing conducting in patients. The controls’ intercept value has been converted to this metric from raw scores.
Relationships Between Baseline and Outcome Variables and Intercepts and Slopes
An initial model combining positive and negative affect models in patients fit well (CFI = .99, TLI = .98, RMSEA = .05, SRMR = .07). Predictor and outcome variables were added simultaneously, and clearly nonsignificant variables were dropped from the model (p > .10). The final model fit acceptably to well (CFI = .95, TLI = .92, RMSEA = .08, SRMR = .07). The following results are displayed in Table 3.
Table 3.
Prediction of Intercept and Slope of Positive and Negative Affect, as Well as Those Intercepts and Slopes Predicting Outcome Variables at Week 52
| Variable | Positive affect intercept | Positive affect slope | Negative affect intercept | Negative affect slope |
|---|---|---|---|---|
| Predictors (baseline) | ||||
| Age | −.25** | −.13** | — | — |
| Social support | −.23** | — | .13* | .27** |
| Education | .11* | — | .10* | |
| Gender | .20** | — | .02* | |
| CIRS-G | — | — | .09* | — |
| Depression | — | — | .27** | — |
| Outcomes (Week 52) | ||||
| Depression | — | — | .48* | .56* |
| RBANS | — | .08 | — | — |
| Hip fracture recovery | — | .12* | — | — |
| GALES NL | — | — | .09** | .46* |
| GALES SS | — | — | .09* | .48* |
Note. CIRS-G = Cumulative Illness Ratings Scale for Geriatrics; RBANS = Repeatable Battery for Assessment of Neuropsychological Status; GALES NL = Geriatric Adverse Life Events Scale Number of Life Events subscale; GALES SS = Geriatric Adverse Life Events Scale Subjective Stress subscale. Note that Social Support is scored with higher values indicating less support. Variables with — were not significantly related (ps > .10).
p < .05.
p < .001.
Variables predicting slope and intercept.
Older people started off with lower positive affect at Week 1 (fsp = −.25, p < .001), whereas people with higher social support, more education, and women started off with higher positive affect (fsp = −.23, p < .001, fsp .11, p < .019; fsp = .20, p < .001, respectively). People with higher education and women also reported greater negative affect at Week 1 (fsp = .10, p = .016; fsp = .13, p = .002). People with greater cumulative illness and higher depression scores also reported greater initial negative affect (fsp = .09, p = .029; fsp = .27, p < .001), whereas people with greater social support reported lower initial negative affect (fsp = .13, p = .017). Age significantly predicted the slope of positive affect (fsp = .13, p = .005), such that recovery of positive affect was lower when age was higher. Baseline social support significantly predicted the slope of negative affect (fsp = .27, p = .003), such that people with higher social support showed a faster decline in negative affect.
Variables predicted by slope and intercept.
All variables predicted at Week 52 were predicted above and beyond an initial measurement of the same variable (at baseline except as noted below). People who started off higher in negative affect reported more stress from stressful life events (fsp = .09, p < .001) and higher depression (fsp = .48, p = .007) at Week 52. The positive affect intercept did not significantly predict any of the outcome variables (ps > .10).
Slower decline in negative affect predicted higher depression at Week 52 above and beyond baseline MADRS score (fsp = .56, p = .004). In addition, people with a slower decline in negative affect reported more stressful life events and greater associated stress at Week 52 (fsp = .46, p = .01; fsp = .48, p = .007). Notably, the stressful life events subscales (GALES) were not given at baseline so the subscales from Week 2 were included in the analyses to account for earlier levels of stressful life events.
People who had greater recovery in positive affect showed greater physical hip fracture recovery at Week 52 above and beyond hip fracture recovery score at baseline (fsp = .12, p = .005). In addition, the slope of positive affect trended toward significantly predicting RBANS score at Week 52 (fsp = .08, p = .054), such that people who showed greater recovery in positive affect had higher RBANS scores at Week 52. Notably, because the RBANS was not conducted at baseline, RBANS score at Week 4 was included in the analysis (which could be considered an excessively restrictive control).
Discussion
The current study examined the trajectory of recovery in positive and negative affect after a hip fracture, along with the predictors and consequences of different degrees of recovery. Three key conclusions are drawn. First, although most people recovered at least partially from higher negative affect and lower positive affect, there was significant variation in the extent to which people recovered. Second, some of this variation was predicted by baseline or premorbid variables such as age, education, social support, and depressive symptoms. Specifically, individuals with higher social support showed a faster decline in negative affect, consistent with research indicating that an extensive social network may have a protective role in times of distress. In addition, older individuals showed a slower increase in positive affect, suggesting that age may be a risk factor for poorer affective responses after hip fracture. Third, the patterns of positive and negative affect were related to psychological and physical functioning indices such as depression and physical functioning at 1-year postfracture.
The results provide several contributions to the current understanding of how affect and physical health are related. First, the results are the first to depict the average recovery in positive and negative affect after hip fracture. Hip fracture is associated with an increase in negative affect with a trajectory toward levels comparable with controls at Week 12. In addition, the results indicated that most patients experienced a decline in positive affect following hip fracture. For most patients, positive affect increased over time with a peak at Week 8 followed by a leveling off at Week 12. In fact, it appears that the patients’ trajectory is divergent from that of the controls’ at Week 12. Thus, unlike negative affect, it appears that positive affect did not return to values approaching those of the controls by Week 12.
A second key contribution was the assessment of how baseline variables related to trajectories of affect over time. Consistent with previous research (e.g., Magaziner et al., 1990) certain psychosocial variables were protective. Individuals with higher social support at baseline showed a faster decline in negative affect over time, as well as a lower starting off point, suggesting that having higher social support may not only aid in recovery from hip fracture, but may also be a source of immediate resiliency. This finding suggests that interventions aimed at decreasing social isolation in older hip fracture patients might facilitate improved outcomes. Conversely, individuals who were older at the time of their hip fracture reported lower positive affect initially and showed less overall recovery in positive affect, suggesting that older patients may be particularly prone to deficits in positive affect after experiencing a hip fracture. Education and gender appeared to relate to increased emotion response in general; individuals with higher education and women reported higher levels of both positive and negative affect initially. Furthermore, individuals with more cumulative illness and higher depression were characterized by greater initial negative affect. However, none of these variables (gender, education, cumulative illness, and depression) predicted the overall trajectory of positive or negative affect, suggesting that they are more predictive of initial responding rather than an overall trajectory. Should these results be replicated, it would be advantageous for caregivers to know that these subsets of individuals might respond with greater positive or negative affect initially, but will not necessarily have a faster or slower course of recovery.
A third key contribution was the investigation of how the trajectories of affect related to important outcome indices. Patients characterized by a slower decline in negative affect reported higher levels of depression, more stressful life events, and more associated stress from the stressful life events 1-year postfracture. This group of findings suggests that higher levels of negative affect during the recovery process predict negative mental health consequences over time, which in turn may have implications for increased risk for additional comorbid conditions and health care utilization. In terms of the implications of these findings, it is theorized that individuals who have a harder time adjusting to life after a hip fracture may enter a downward spiral in which they experience more stress and depression. Thus, a temporary increase in negative affect is to be expected, but individuals who fail to recover over time will likely see their distress continue to grow. In terms of positive affect, those who showed better recovery reported better physical functioning and, at a trend level, better cognitive functioning 1-year postfracture, which may indicate that positive affect plays a key role in how well individuals regain their physical and possibly cognitive abilities.
These findings also strengthen converging evidence that positive affect may be related to recovery of physical functioning as prior studies have indicated (e.g., Fredman et al., 2006). Furthermore, the results extend this research by showing that physical functioning recovery is specifically related to levels of positive affect during the recovery process. The current study builds on previous studies by including baseline physical functioning in the analyses, thereby providing stronger support for the hypothesis that higher positive affect during recovery causes superior physical functioning outcomes. Taken together, it appears that positive affect may be important for both physical and mental functioning, highlighting the importance of finding ways to elicit positive affect for individuals in the recovery process.
Whereas positive affect during the recovery process was protective, negative affect was associated with higher depression, more stressful life events, and more associated stress at Week 52. This finding is consistent with the previous finding (e.g., Magaziner et al., 2000) that hip fracture is associated with negative mental health consequences. Specifically, it appears that the amount of negative affect experienced during recovery may be a determining factor for which individuals will become more depressed or report higher stress 1-year postfracture.
The results should be considered in light of the study’s limitations. First, assessment modality varied across the time points. Testing of whether loadings and thresholds could be constrained across time was conducted to address this concern, but, nevertheless, greater consistency in assessment modality would have been preferred. Second, baseline assessments of most of our variables were included in our model, but cognitive functioning was not assessed at baseline because it is inappropriate to assess cognitive functioning in the near-term after hip fracture and surgery. To address this concern, cognitive functioning at Week 4 was included. Third, whereas participants were recruited from many hospitals in the St. Louis area, it is possible that these results do not extend to other geographical areas. Although it would be challenging methodologically, including a preillness assessment of affect in future research would help to further tease apart the causal relationship between affect and physical functioning.
Given the high prevalence of and long-lasting detrimental consequences associated with hip fracture, these findings have implications for the care of older adults recovering from this injury. The general trajectories of positive and negative affect over the course of recovery suggest that a particular focus on mental health during hospitalization and rehabilitation may greatly enhance both psychosocial and physical outcomes. Screening individuals for levels of negative affect during the recovery process may help to prevent later development of, or increases in, depressive symptoms. Should the current findings be replicated, future researchers should investigate the efficacy of engaging vulnerable individuals (i.e., those low in positive affect and/or high in negative affect) within the first 12 weeks after a hip fracture with cognitive–behavioral techniques such as cognitive restructuring or increased contact with loved ones to reduce the risk of long-lasting physical and mental health consequences. Additional attention should be paid to the psychological status of the eldest hip fracture patients, for whom recovery of positive affect appears to be particularly challenging. The significant relationship between positive affect recovery and physical (and, potentially, cognitive) functioning further underlines the importance of developing interventions aimed at increasing positive affect after a hip fracture. For example, designing interventions that help individuals to reengage with meaningful activities or social events after a hip fracture could help them to recover positive affect.
After the initial increase in negative emotions and decrease in positive emotions after a hip fracture and associated surgery, individuals tended to show a recovery in their emotional health. That is, on average, hip fracture patients showed a decrease in negative affect and an increase in positive affect over time. Although there was a general tendency to recover emotionally, the patterns of affect during the recovery process predicted levels of depression, physical functioning, and cognitive ability 1-year post fracture. These findings call for more research on the role of emotions in the process of recovering from a major medical event. Though the link between positive affect and physical recovery seems evident, the mechanisms behind this relationship remain unknown and require further investigation. In conclusion, affective responses to a hip fracture predict both psychological and physical functioning over time, providing a potential target for the enhancement of recovery from this debilitating injury.
Acknowledgments
This research was funded by R01 MH074596 to Eric J. Lenze. Ellen F. Binder is a consultant and receives research support from Lilly U.S.A., Inc., and Regeneron Pharmaceuticals.
Footnotes
The groups could not be compared in terms of the number of participants reporting an Asian or Pacific Islander ethnicity because of expected cell sizes less than 5. There were 0 such participants in the controls and 3 in the patients group.
It was not possible to calculate the best estimate of slope in the controls because of several perfectly related items that prevented the use of longitudinal invariance testing. Notably, the most likely source of longitudinal variance (repeated assessment) should have consistent effects across groups and is therefore unlikely to affect the comparisons of slopes. It was also not possible to correct for method variance in analyses involving controls because the model would not tolerate the addition of a method variance slope, likely because of the more modest sample size in controls. Again, this restriction should have minimal impact on comparison between groups. However, it is plausible that this restriction might impact the estimate of control’s intercepts very slightly (overestimating the baseline mental health of controls).
To translate the controls’ intercept values to the same metric as the patients’ values, factor scores were estimated for the controls from a model including item-level data for both patients and controls at single time point and then entered these values into a regression with raw scores predicting the factor scores. In this way, a formula for translating the controls’ raw data into the factor scores of the same metric as the patients’ values was calculated. More sophisticated ways of obtaining the same basic results were contraindicated by (a) the smaller number of controls and (b) the aforementioned (see footnote 2) perfectly related items across time points in the control data.
Contributor Information
Julia K. Langer, Department of Psychology, Washington University in St. Louis
Jaclyn S. Weisman, Department of Psychology, Washington University in St. Louis
Thomas L. Rodebaugh, Department of Psychology, Washington University in St. Louis
Ellen F. Binder, Internal Medicine/Division of Geriatrics and Nutritional Science, Washington University in St. Louis
Eric J. Lenze, Department of Psychiatry, Washington University in St. Louis
References
- Austin M-P, Mitchell P, & Goodwin GM (2001). Cognitive deficits in depression: Possible implications for functional neuropathology. The British Journal of Psychiatry, 178, 200–206. doi:10.1192/bjp.178.3.200 [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. doi:10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Bentler PM (1995). EQS: Structural equations program manual (Version 5.0). Los Angeles, CA: BMDP Statistical Software. [Google Scholar]
- Braithwaite RS, Col NF, & Wong JB (2003). Estimating hip fracture morbidity, mortality, and costs. Journal of American Geriatric Society, 51, 364–370. doi:10.1046/j.1532-5415.2003.51110.x [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, & Barlow DA (1998). Structural relationships among dimensions of the DSM–IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107, 179–192. doi:10.1037/0021843X.107.2.179 [DOI] [PubMed] [Google Scholar]
- Curran PJ, & Bollan KA (2001). The best of both worlds: Combining autoregressive and latent curve models In Collins LM & Sayer AG (Eds.), New methods for the analysis of change (pp. 107–135). Washington, DC: American Psychological Association. doi:10.1037/10409004 [Google Scholar]
- Devanand DP, Kim MK, Paykina N, & Sackeim HA (2002). Adverse life events in elderly patients with major depression or dysthymic disorder and in healthy-control subjects. The American Journal of Geriatric Psychiatry, 10, 265–274. doi:10.1097/00019442-20020500000005 [PubMed] [Google Scholar]
- Dua JK (1994). Comparative predictive value of attributional style, negative affect, and positive affect in predicting self-reported physical health and psychological health. Journal of Psychosomatic Research, 38, 669–680. doi:10.1016/0022-3999(94)90019-1 [DOI] [PubMed] [Google Scholar]
- Finch JF, Baranik LE, Liu Y, & West SG (2012). Physical health, positive and negative affect, and personality: A longitudinal analysis. Journal of Research in Personality, 46, 537–545. doi:10.1016/j.jrp.2012.05.013 [Google Scholar]
- Fredman L, Hawkes WG, Black S, Bertrand RM, & Magaziner J (2006). Elderly patients with hip fracture with positive affect have better functional recovery over 2 years. Journal of the American Geriatrics Society, 54, 1074–1081. doi:10.1111/j.1532-5415.2006.00786.x [DOI] [PubMed] [Google Scholar]
- Honaker J, King G, & Blackwell M (2006–2008). Amelia II: A program for missing data (Version 1.2–17). [Software]. Available from http://gking.harvard.edu/amelia/
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. doi: 10.1080/10705519909540118 [Google Scholar]
- Isen AM, Daubman KA, & Nowicki GP (1987). Positive affect facilitates creative problem solving. Journal of Personality and Social Psychology, 52, 1122–1131. doi:10.1037/0022-3514.52.6.1122 [DOI] [PubMed] [Google Scholar]
- Jöreskog KG, & Sörbom D (1981). LISREL V: Analysis of linear structural relationships by the method of maximum likelihood. Chicago, IL: National Educational Resources. [Google Scholar]
- Koenig HG, Westlund RE, George LK, Hughes DC, Blazer DG, & Hybels C (1993). Abbreviating the Duke Social Support Index for use in chronically ill elderly individuals. Psychosomatics : Journal of Consultation and Liaison Psychiatry, 34, 61–69. doi:10.1016/S00333182(93)71928-3 [DOI] [PubMed] [Google Scholar]
- Landerman R, George LK, Campbell RT, & Blazer DG (1989). Alternative models of the stress buffering hypothesis. American Journal of Community Psychology, 17, 625–642. doi:10.1007/BF00922639 [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, . . . Reynolds CF (2001). The association of late-life depression and anxiety with physical disability: A review of the literature and prospectus for future research. The American Journal of Geriatric Psychiatry, 9, 113–135. doi:10.1097/00019442-200105000-00004 [PubMed] [Google Scholar]
- Linn BS, Linn MW, & Gurel L (1968). Cumulative illness rating scale. Journal of the American Geriatrics Society, 16, 622–626. [DOI] [PubMed] [Google Scholar]
- Mackinnon A, Jorm AF, Christensen H, Korten AE, Jacomb PA, & Rodgers B (1999). A short form of the Positive and Negative Affect Schedule: Evaluation of factorial validity and invariance across demographic variables in a community sample. Personality and Individual Differences, 27, 405–416. doi:10.1016/S0191-8869(98)00251-7 [Google Scholar]
- Magaziner J, Hawkes W, Hebel R, Zimmerman SI, Fox KM, Dolan M, Felsenthal G, & Kenzora J (2000). Recovery from hip fracture in eight areas of function. The Journals of Gerontology: Series A: Biological Sciences and Medical Sciences, 55, M498–M507. doi: 10.1093/gerona/55.9.M498 [DOI] [PubMed] [Google Scholar]
- Magaziner J, Simonsick EM, Kashner M, Hebel JR, & Kenzora JE (1990). Predictors of functional recovery one year following hospital discharge for hip fracture: A prospective study. The Journals of Gerontology: Series A: Biological Sciences and Medical Sciences, 45, M101–M107. [DOI] [PubMed] [Google Scholar]
- Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, & Reynolds III CF (1992). Rating chronic medical illness burden in geropsychiatric practice and research: Application of the Cumulative Illness Rating Scale. Psychiatry Research, 41, 237–248. doi:10.1016/0165-1781(92)90005-N [DOI] [PubMed] [Google Scholar]
- Montgomery SA, & Asberg MARIE (1979). A new depression scale designed to be sensitive to change. The British Journal of Psychiatry, 134, 382–389. doi:10.1192/bjp.134.4.382 [DOI] [PubMed] [Google Scholar]
- Mossey JM, Mutran E, Knott K, & Craik R (1989). Determinants of recovery 12 months after hip fracture: The importance of psychosocial factors. American Journal of Public Health, 79, 279–286. doi:10.2105/AJPH.79.3.279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2009). Mplus user’s guide (5th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Randolph C, Tierney MC, Mohr E, & Chase TN (1998). The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): preliminary clinical validity. Journal of Clinical and Experimental Neuropsychology, 20, 310–319. doi:10.1076/jcen.20.3.310.823 [DOI] [PubMed] [Google Scholar]
- Steiger JH, & Lind JC (1980, May). Statistically-based tests for the number of factors. Paper presented at the meeting of the Psychometric Society, Iowa City, Iowa. [Google Scholar]
- Steptoe A, Dockray S, & Wardle J (2009). Positive affect and psychobiological processes relevant to health. Journal of Personality, 77, 1747–1776. doi:10.1111/j.1467-6494.2009.00599.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker LR, & Lewis C (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38, 1–10. doi:10.1007/BF02291170 [Google Scholar]
- U.S. Congress, Office of Technology Assessment. (1994, July). Hip fracture outcomes in people age 50 and over [Background Paper, OTA-BPH-120]. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- Vandenberg RJ, & Lance CE (2000). A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organizational Research Methods, 3, 4–70. doi:10.1177/109442810031002 [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. doi:10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Watson D, & Pennebaker JW (1989). Health complaints, stress, and distress: Exploring the central role of negative affectivity. Psychological Review, 96, 234–254. doi:10.1037/0033-295X.96.2.234 [DOI] [PubMed] [Google Scholar]