Abstract
Aedes aegypti bears the common name “the yellow fever mosquito,” although, today, it is of more concern as the major vector of dengue, chikungunya, and, most recently, Zika viruses. In the present article, we review recent work on the population genetics of this mosquito in efforts to reconstruct its recent (approximately 600 years) history and relate these findings to epidemiological records of occurrences of diseases transmitted by this species. The two sources of information are remarkably congruent. Ae. aegypti was introduced to the New World 400–550 years ago from its ancestral home in West Africa via European slave trade. Ships from the New World returning to their European ports of origin introduced the species to the Mediterranean region around 1800, where it became established until about 1950. The Suez Canal opened in 1869 and Ae. aegypti was introduced into Asia by the 1870s, then on to Australia (1887) and the South Pacific (1904).
Keywords: Aedes aegypti, history, yellow fever, dengue, slave trade
Regardless of whether Aedes aegypti is “the most dangerous animal in the world” (Powell 2016), there is little doubt that this mosquito has caused immense human suffering over centuries. Early in the twentieth century it was identified as the carrier of the yellow fever virus. Yellow fever ravaged the New World and doubtlessly affected major historical events that define the Americas today (McNeill 2010). More recently it has been the major vector of pandemics of three other viral diseases: dengue, chikungunya, and Zika fevers. It has been hypothesized that, of the approximately 3500 named mosquitoes, Ae. aegypti has been the single most important vector of these viruses because of a common evolutionary history in Africa along with the native African vertebrate host, humans (Powell 2018).
Given its importance to public health and human history, unraveling Ae. aegypti's recent past (last 600 years) is important in order to understand how and when it came to occupy its present distribution, a distribution that determines human populations at risk for diseases it transmits. Not only will this help to understand historical disease patterns, it sheds light on threats this dynamic mosquito may pose in the future.
An obvious approach to this problem would be to simply consult the entomological literature for early reports of Ae. aegypti in different localities. Unfortunately, this is not possible as the taxonomy of Ae. aegypti (and many other mosquitoes) was rather muddled and unreliable until quite recently. For example, the medical team in Cuba working to identify the carrier of yellow fever called the mosquito they were using Culex fasciata, whereas there is little doubt it was Ae. aegypti. In fact, the original name, Aedes aegypti, was first used by Linnaeus in 1762 for a mosquito that was very likely not what is recognized today as Ae. aegypti (Mattingly 1957). Christophers (1960) summed up the problem: “The trouble was that it (Ae. aegypti) had so many aliases, almost one for every country and systematist.” The lack of consistency in use of species names, coupled with the absence of mosquito surveillance during the crucial period, 1500–1900, make such records unreliable, except in cases in which collections were deposited in museums and reexamined when nomenclature was clarified. Before approximately 1900 when it became known that mosquitoes transmit diseases, there was little reason for entomologists or public health workers to pay special attention to this little fly, except as a nuisance.
Two other, more reliable, sources of historical information are available. One is analysis of Ae. aegypti genomes in populations from different regions to trace back their history of connectedness, their phylogeography. Advances in population genomics have provided methods to estimate the number of generations since populations split and, by assuming generation times, this can provide estimates of dates of splits. A second source is to examine historical records of when and where diseases transmitted by Ae. aegypti are reported. This is possible for diseases that have distinctive symptoms recognizable before modern medical advances. For example malaria is clearly described in ancient Greece and Rome (Cunha and Cunha 2008). Yellow fever is similar: high fever, joint pain, and jaundice (yellowing of skin and whites of the eye) followed in later stages by black vomit resembling coffee grounds.
The purpose of this review is to illustrate how these two independent sources of information, genome analyses of mosquitoes and epidemiological history, mutually support a reasonably clear picture of the past 600 year history of Ae. aegypti.
Origin of the domestic form
Multiple lines of evidence indicate that Africa is the ancestral home of Ae. aegypti. Populations still exist in forests of sub-Saharan Africa with tree holes and other natural pockets of water serving as larval breeding sites (Lounibos 1981). These populations prefer nonhuman mammals as a blood source (Gouck 1972; Peterson 1977; McBride et al. 2014). A major step in its history was when this “wild” species of mosquito became “domesticated,” i.e., began to use human-generated water containers for larvae and humans as a blood source. It is this domesticated form of Ae. aegypti, closely associated with and dependent on human habitats, that spread around the tropical and subtropical world and has been the source of worldwide epidemics of diseases it transmits (Powell and Tabachnick 2013). These two “forms” of Ae. aegypti have been given subspecies name, Ae. aegypti formosus for the ancestral African type and Ae. aegypti aegypti for the domestic type outside Africa. For convenience, we will use Aaf and Aaa to refer to these two forms.
When and how this wild species became domesticated has been the source of much speculation. One popular idea was that domestication was a consequence of the expansion of the Sahara Desert (Peterson 1977; Tabachnick 1991). Favorable tropical forest habitat for Aaf in Africa once extended as far north as the Mediterranean (Kropelin et al. 2008). It is hypothesized that, as the Sahara expanded 4000–6000 years ago, populations of Ae. aegypti isolated north of the nascent desert were forced to start breeding in the only reliable source of water remaining, that stored by humans in their towns and villages. This implies that Ae. aegypti was resident around the Mediterranean, at least on its southern shores, thousands of years ago. The Mediterranean could therefore be the source of the New World introductions (European trade after the “discovery” of the Americas) as well as Asian populations via frequent Mediterranean European–Asia trade over the centuries.
There are two problems with this scenario. First, had a domesticated form of Ae. aegypti existed in northern Africa thousands of years ago as a result of the expanding Sahara, it would almost certainly have spread around the Mediterranean as it did after 1800 (Schaffner and Mathis 2014, discussed later), clear evidence that the climate is favorable for establishment of this species in much of the Mediterranean Basin. Phoenician Carthage (in what is now Tunisia) carried out extensive trade around the entire Mediterranean for hundreds of years before being conquered by Rome in 146 BCE. However, unlike historical reports of malaria, there are no reports of yellow fever anywhere in the Mediterranean Basin before sporadic cases in and near seaports in the 1700s and self-sustaining epidemics in the 1800s (see later).
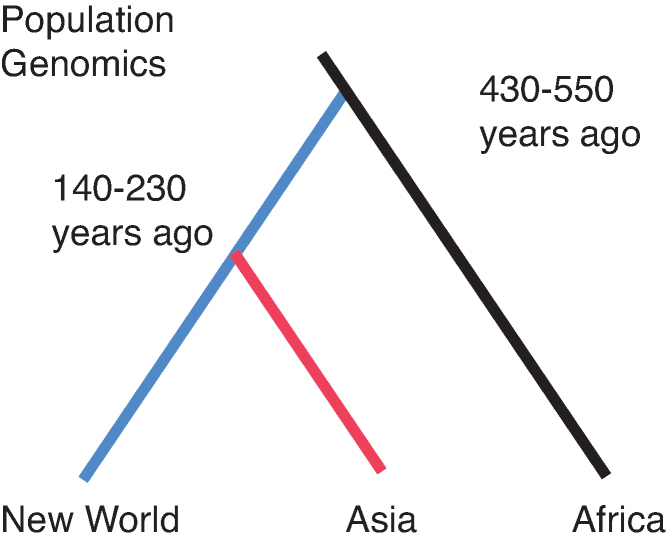
The second problem comes from genetic analyses of the mosquito. Genetic data strongly indicate that all domestic populations of Aaa outside Africa converged back to a single lineage, i.e., is monophyletic (Brown et al. 2014; Gloria-Soria et al. 2016; Kotsakiozi et al. 2018). Microsatellite data and DNA sequencing can now be used to estimate times when lineages split. Both data sets (Gloria-Soria et al. 2016; Crawford et al. 2017; Kotsakiozi et al. 2018) lead to estimates of 4000 to 5500 generations for this split. Assuming about ten generations per year for this mosquito in the tropics, this places the origin of domestic Aaa at 400–550 years ago (figure 1), much more recent than the expansion of the Sahara 4000–6000 years ago (Kropelin et al. 2008).
Figure 1.
Graphical representation of the Aedes aegypti split of lineages and the times of events estimated from genetic data. The blue line represents the introduction into the New World with Asia (red line) being derived from the New World. There are three types of data: microsatellites (Gloria-Soria et al. 2016, Kotsakiozi et al. 2018) and exome sequences (Crawford et al. 2017). Two types of analyses to estimate times were used: approximate Bayesian computation analysis, as implemented in DIYABC (Cornuet et al. 2014), and allele array frequency analyses (Pickrell and Prichard 2012).
A more likely scenario is that Ae. aegypti became domesticated in situ in West Africa when human settlements began to form adjacent to forests. Much of West Africa experiences prolonged annual droughts when natural sites for Ae. aegypti larvae dry out. For example, Luanda in coastal Angola experiences a 6-month dry period (May–October) with an average of 5 millimeters of rain per month and less than 1mm for four of those months (June–September; Deutscher Wetterdienst 2016). Obviously, any human-occupied village would be storing water during the dry season. Although the eggs of Ae. aegypti remain viable when dried for a few months, by 4 months, hatching drops to about 1% with no hatching at 5 months (Christophers 1960). A female mosquito searching for a place to oviposit at the beginning of the dry season would find the stored water in villages very attractive. Females eclosing from such containers in the dry season would have no choice but to oviposit back into the human-generated water containers. They likely also evolve a taste for a new blood source: humans.
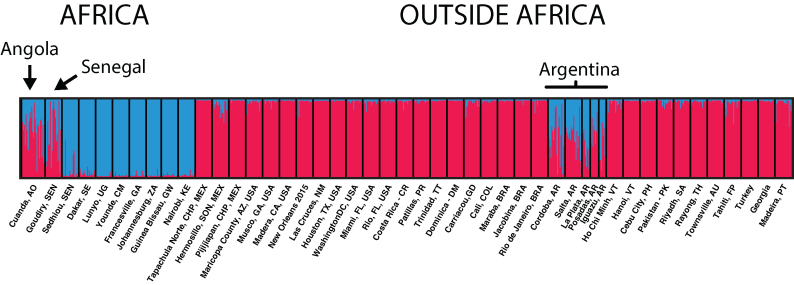
Ae. aegypti populations with mixed genetic signature typical of both the forest-breeding Aaf and domestic Aaa have been found in both Senegal and Angola (figure 2). These could represent the origins of the domestic lineage, what might be described as “proto-Aaa” populations (see supplement 1).
Figure 2.
STRUCTURE plot of selected Ae. aegypti populations based on microsatellites (as implemented in Pritchard et al. 2000). Two clusters are defined (in red and blue), and the probability of assignment of individuals to the clusters is given by the colors of each line. All data are in Gloria-Soria and colleagues (2016), except for Turkey, Georgia, and Angola (which are in Kotsakiozi et al. 2018).
Although the two subspecies recognized today evolved morphological and behavioral differences, there is no indication of reproductive isolation between them (but see Dickson et al. 2016 for a possible exception). Historically, forests and villages were in sufficient proximity that the two forms continued to interbreed frequently enough to prevent evolution of reproductive isolation. It was not until the two types were entirely isolated from one another by the Atlantic Ocean that they evolved independently and “proto-Aaa” became fully Aaa we recognize today. The dating of the split of Aaa from Aaf using genetic data assumes complete isolation (no gene flow), so the 400–550 year estimate (figure 1) is when the two types stopped exchanging genes, after the ecological/behavioral divergence began within Africa (see supplement 2).
Spread to the Americas
Populations of Aaa in the New World (North and South America) were the first to branch off from ancestral Aaf (figure 1). The time of this split (400–550 years ago) coincides with the rise of transatlantic shipping by Europeans. Beginning in the sixteenth century, ships originating in Europe would stop in West Africa to pick up native Africans for the slave trade before embarking on the crossing (Eltis and Richardson 2010). Doubtless they would also resupply with ample fresh water from coastal West African villages to last the 2–4 months needed to cross the Atlantic at that time. It is likely that eggs and larvae of Ae. aegypti would be included. Having already adapted to breeding in human-generated water storage containers preadapted these “proto-Aaa” mosquitoes to survive the long voyage.
The first reliable report of yellow fever in the New World was in 1648 in Havana and the Yucatan (McNeill 1976). Like the mosquito, the yellow fever virus is also native to Africa (Bryant et al. 2007; Powell 2018). This implies two things. First, by the mid-1600s, Aaa populations were established in high enough density to sustain yellow fever epidemics over a fairly wide area, at least in the Caribbean and Mexico. Second, slaves, sailors, and/or mosquitoes carrying the yellow fever virus must have survived the trip. The yellow fever virus remains infective in human carriers for only 7–10 days, adult mosquitoes seldom live more than a month, and transovarial transmission (vertical transmission in egg cytoplasm) of yellow fever virus is very rare (Aitken et al. 1979). This implies that multiple mosquito generations and transmission cycles occurred during the 2–4 months of the trip.
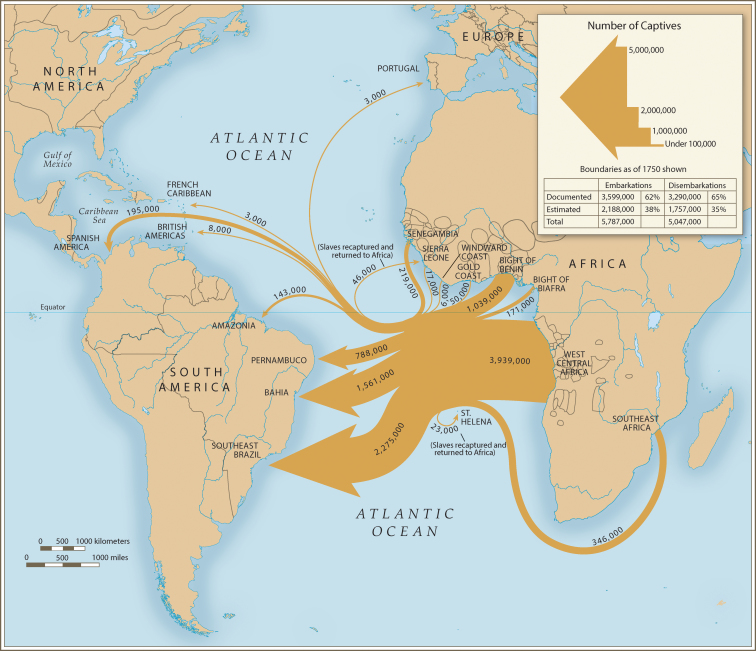
Where in West Africa might the first introductions to the New World have originated? In the earliest days of European slave trade, 1500–1650, approximately 70% of the trade was carried out by Portugal (Eltis and Richardson 2010) and Portuguese ships almost exclusively used what is today Angola as their source of slaves (figure 3). An Angolan source is consistent with the genetic patterns although we cannot rule out other West African locales such as Senegal (figure 2).
Figure 3.
Quantitative depiction of Portuguese slave trade. The thickness of the arrows is proportional to the number of native Africans transported. From Eltis and Richardson (2010), used with permission.
Where was Ae. aegypti first introduced into the New World? Figure 3 suggests that Brazil or northern Argentina would be likely candidates. Because of a campaign to eliminate Ae. aegypti from the New World carried out between about 1950 and 1970, Ae. aegypti was eliminated from Brazil and subsequently recolonized from sources outside Brazil (Kotsakiozi et al. 2017). However, northern Argentina harbors populations very distinct from contemporary Brazilian populations that have genetic signatures of being closely related to Aaf, indistinguishable from the “proto-Aaa” populations in Angola and Senegal today (figure 2). No other populations outside Africa have such a genetic signature (Gloria-Soria et al. 2016; Kotsakiozi et al. 2018). These Argentine populations could represent relict populations that escaped the eradication program (see supplement 3). Ae. aegypti in Argentina have been reported to breed in tree holes (Mangudo et al. 2015), further evidence of retaining characteristics of their African ancestors.
Back to the old world
Asia and the Pacific region (Australia and South Pacific Islands including Hawaii) have Aaa populations clearly derived from the New World (figure 1). How and when did Aaa get from the New World to Asia? European shipping may again hold the answer. The early Atlantic trade was triangular: starting in European ports, stopping in West Africa, proceeding to the New World, and returning to Europe. Just as these mosquitoes stowed away on the journey from Africa to the New World, they could well have been stowaways on the return trip to Mediterranean ports such as Spain and Portugal.
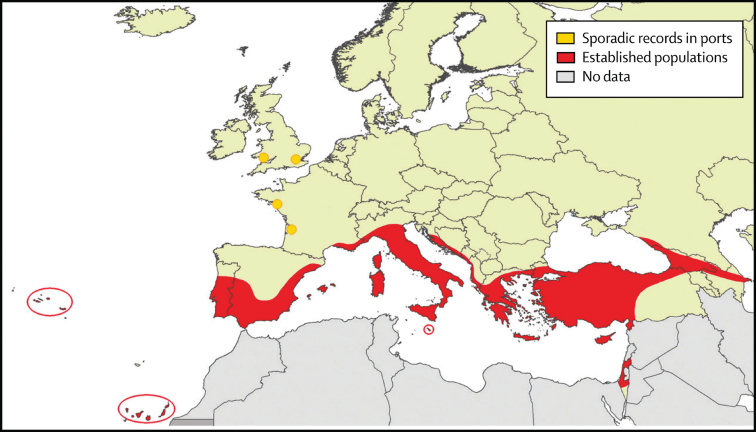
Although sporadic cases of yellow fever in Europe are reported in ports in which ships returned from the New World in the 1700s (Eager 1902), clear evidence of yellow fever transmission in Europe (autocthonous cases repeating annually) does not appear until 1800–1804, with severe outbreaks in several Spanish cities and Gibraltar resulting in more than 60,000 deaths (Augustin 1909; Sawchuk and Burke 1998). In letters written in 1801, the Queen of Spain describes suffering from a disease with symptoms typical of dengue (using the Spanish term quebranta huesos, break bone), despite never having been to the New World or Africa (Regau-Perez 1998). Aaa established itself around the Mediterranean (figure 4) and caused outbreaks of yellow fever and especially dengue in much of the Mediterranean throughout the nineteenth century and first half of the twentieth century. Greece was particularly hard hit in 1927–1928, with an estimated million cases of dengue and more than a thousand deaths (Rosen 1986). The time of establishment of Mediterranean populations around 1800 based on epidemiological data fits very well the population genomics data on the mosquito, assuming the now extinct Mediterranean populations were an intermediate between the New World and Asia, a “ghost taxon” in the tree in 1.
Figure 4.
Historical distribution of Ae. aegypti in European countries before 1960. Northern Africa also had the species but is not depicted in this figure. Modified from Schaffner and Mathis (2014).
Aaa virtually disappeared from the Mediterranean around 1950 because of a combination of DDT application to control malaria-carrying Anopheles and, probably more importantly, improved sanitation and plumbing that eliminated the need to store water in houses, thus destroying this larval niche (Curtin 1967; Holstein 1967). Contemporary populations of Aaa around the Black Sea (Schaffner and Mathis 2014) could represent remnants of what once inhabited the Mediterranean. Although our recent genetic study of Black Sea Aaa indicated that these populations were ancestral to Asia, we could not unambiguously determine whether the Black Sea populations directly descended from the New World (Kotsakiozi et al. 2018).
Asia/Australia/Pacific
The Suez Canal opened in 1869 and the first definitive cases of chikungunya in Asia appear in the 1870s (Carey 1971) and urban dengue in the 1890s (Smith 1956). Enigmatically, Asia has never experienced yellow fever, so presence of this distinctive disease cannot be used to time the introduction of Aaa. Aaa's spread through Asia to the Pacific was rapid, probably because of the well-established trade routes in this part of the world by the late 1800s. The first reliable report of Aaa in Australia is in 1887, based on a museum specimen confirmed to be Ae. aegypti by modern workers (Lee et al. 1987). The first report of dengue in Australia is in 1897 (Hare 1898). [Interestingly, the Ae. aegypti specimen collected by Skuse in Brisbane in 1887 was called by him Culex Bancroftii, later changed to Stegomyia fasciata by Theobald in 1901 (Lee et al. 1987). This further highlights the ambiguity of nomenclature at that time.]
Australian Aaa today are genetically very close to S. Pacific populations that include the Philippines, Tahiti, and Hawaii (Gloria-Soria et al. 2016). The first reliable reports of Ae. aegypti on South Pacific Islands are from collections made in 1904 and called Aedes argenteus by Buxton and colleagues (Buxton 1927; Buxton and Hopkins 1927), later confirmed to be Ae. aegypti. Dengue did not arrive on the islands until the 1940s, speculated to have been introduced by troop movements during World War II (Monath 1994).
Formally, we cannot rule out the possibility that Asia/Australia/Pacific was colonized directly from the New World possibly from ships from the west coast of South America. Or there is what has been called the “First Fleet,” a group of 11 ships that left England in 1787 with 1100 convicts that stopped in Rio de Janeiro before traveling around the Cape of Good Hope to found penal colonies in Australia (Frost 2012).
However, the founding of Asia/Australia/Pacific directly from the New World without a Mediterranean intermediate is hard to reconcile with our observation that Black Sea populations are as old as, likely even older than, all contemporary Asia/Australia/Pacific populations (Kotsakiozi et al. 2018). This, coupled with the epidemiological data indicating the presence of Aaa in the Mediterranean before the opening of the Suez Canal and the appearance of aegypti-borne diseases in Asia very shortly after the opening, argues for the Mediterranean being an intermediate between the New World and Asia/Australia/Pacific.
Conclusions
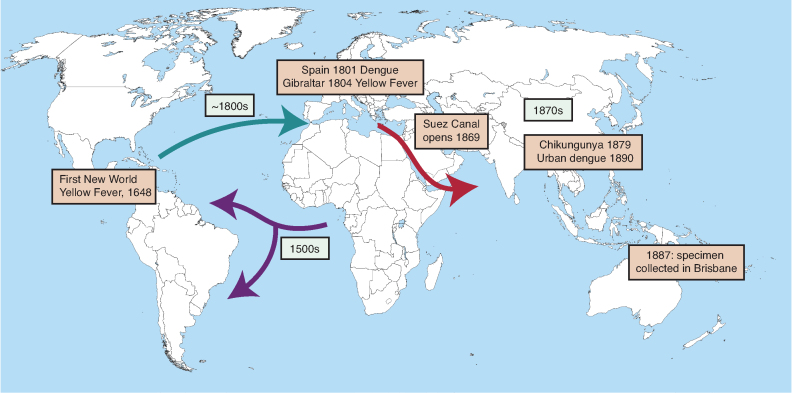
Figure 5 summarizes our present view of the last 600-year history of Ae. aegypti. Although speculation is involved in reaching our conclusions, we have presented a coherent hypothesis consistent with available data. The reinforcing nature of entirely independent types of data (mosquito genetics and epidemiologic history) lends credence to the hypothesis. However, this is a scientific hypothesis subject to falsification as further data arises.
Figure 5.
Summary of the history of Ae. aegypti over the last 600 years. The proposed routes of movement are shown by arrows with proposed dates. Major epidemiological events are noted in boxes. The times are consistent with dates of separation of mosquito populations estimated from genetic data (figure 1).
Supplementary Material
Acknowledgments
We thank Nigel Beebe and Anna-Bella Failloux for information on first introductions into Australia and South Pacific Islands, respectively. Frances Schaffner kindly provided information on Europe and as well as figure 4. Ronald Smith provided guidance in understanding the history of climates in Africa. Scott Ritchie and John McNeill made helpful comments. Research in our laboratory, on which this article is partly based, is supported by the National Institutes of Health, National Institutes of Allergies and Infectious Diseases.
References cited
- Aitken THG, Tesh RB, Beaty BJ, Rosen L. 1979. Transovarial transmission of yellow fever by mosquitoes (Aedes aegypti). American Journal of Tropical Medicine and Hygiene 28: 119–121. [DOI] [PubMed] [Google Scholar]
- Augustin G. 1909. History of Yellow Fever. Searcy and Pfaff, New Orleans. [Google Scholar]
- Brown JE, Evans B, Zheng W, Abas V, Barrera-Martinez L, Egizi A, Zhao H, Caccone A, Powell JR.. 2014. Human impacts have shaped historical and recent evolution in Aedes aegypti, the dengue and yellow fever mosquito. Evolution 68: 514–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant JE, Holmes EC, Barrett ADT. 2007. Out of Africa: A molecular perspective on the introduction of yellow fever into the Americas. PLOS Pathogens 3 (art. e75). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton PA. 1927. Sur les moustiques de Tahiti et du groupe des iles de la Societe. Bulletin Societe Estuedes Oceaniennes 21: 306–308. [Google Scholar]
- Buxton PA, Hopkins GHE. 1927. Researches in Polynesia and Melanesia: An Account of Investigations in Samoa, Tonga, the Ellice Group, and the New Hebrides in 1924, 1925. London School of Tropical Medicine Memorias no. 1. [Google Scholar]
- Carey DE. 1971. Chikungunya and dengue: A case of mistaken identity? Journal of History of Medicine and Allied Sciences 26:243–362. [DOI] [PubMed] [Google Scholar]
- Christophers R. 1960. Aedes aegypti the Yellow Fever Mosquito. Cambridge University Press, Cambridge. [Google Scholar]
- Cornuet J-M, Pudlo P, Veyssier J, Dehne-Garcia A, Gautier M, Leblois R, Marin J-M, Estoup A. 2014. DIYABC v2.0: A software to make approximate Bayesian computation inferences about population history using single nucleotide polymorphism, DNA sequence and microsatellite data. Bioinformatics 30:1187–1189. [DOI] [PubMed] [Google Scholar]
- Crawford JE, Alves JM, Palmer WJ, Day JP, Sylla M, Ramasamy R, Surendran SN, Black WC, Pain A, Jiggins FA. 2017. Population genomics reveals that an anthropophilic population of Aedes aegypti mosquitoes in West Africa recently gave rise to American and Asian populations of this major disease vector. BMC Biology 15:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunha CB, Cunha BA. 2008. Brief history of clinical diagnosis of malaria: From Hippocrates to Osler. Journal of Vector Borne Diseases 45: 194–199. [PubMed] [Google Scholar]
- Curtin TJ. 1967. Status of Aedes aegypti in the eastern Mediterranean. Journal of Medical Entomology 4: 48–50. [DOI] [PubMed] [Google Scholar]
- Deutscher Wetterdienst 2016. https://www.dwd.de/DWD/klima/beratung/ak/ak_661600_kt.
- Dickson LB, Sharakhova MV, Timoshevskiy VA, Fleming KL, Caspary A, Sylla M, Black WC. 2016. Reproductive incompatibility involving Senegalese Aedes aegypti (L.) is associated with chromosome rearrangements. PLOS Neglected Tropical Diseases 10 (art. e0004626). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eager JM. 1902. Yellow fever in Europe: A general historical review. Yellow Fever Institute Bulletin, nos. 3–6 section A, 5–24. [Google Scholar]
- Eltis D, Richardson D. 2010. Atlas of the Transatlantic Slave Trade. Yale University Press. [Google Scholar]
- Frost A. 2012. The First Fleet: The Real Story. Black Inc. [Google Scholar]
- Gloria-Soria A, et al. 2016. Global genetic diversity of Aedes aegypti. Molecular Ecology 25: 5377–5395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gouck HK. 1972. Host preferences of various strains of Aedes aegypti as determined by an olfactometer. Bulletin of the World Health Organization 47: 680–683. [PMC free article] [PubMed] [Google Scholar]
- Hare RE. 1898. The 1897 epidemic of dengue in North Queensland. Australian Medical Gazette, 28 March 1898, 98–107. [Google Scholar]
- Holstein M. 1967. Dynamics of Aedes aegypti distribution, density and prevalence in the Mediteranean area. Bulletin of the World Health Organization 36: 541–543. [PMC free article] [PubMed] [Google Scholar]
- Kotsakiozi P, Gloria-Soria A, Caccone A, Evans B, Schama R, Martins AJ, Powell JR. 2017Tracking the return of Aedes aegypti to Brazil, the major vector of the dengue, chikungunya and Zika viruses. PLOS Neglected Tropical Diseases 11 (e0005653). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotsakiozi P, Gloria-Soria A, Schaffner F, Robert V, Powell JR. 2018. Aedes aegypti in the Black Sea: Recent introduction or ancient remnant? Parasites and Vectors 11: 396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kropelin S, Vershuren D, Lezine AM, Eggermont H, Cocquyt C, Francus P, Cazet JP, Fagot M, Rumes B, Russell JM, Darius F, Conley DJ, Shuster M, von Suchodoletz H, Engstrom DR. 2008. Climate-driven ecosystem succession in the Sahara: The past 6,000 years. Science 320:765–768. [DOI] [PubMed] [Google Scholar]
- Lee DJ, Hicks MM, Griffiths M, Debenham ML, Bryan JH, Russell RC, Geary M, Marks EN. 1987. The Culicidae of the Australasian Region. 4 Genus Aedes - Subgenera Scutomyia, Stegomyia, Verrallina. 324 in School of Public Health and Tropical Medicine Monograph Series, Entomology Monograph no. 2, Australian Government Publishing Service. [Google Scholar]
- Lounibos LP. 1981. Habitat segregation among African treehole mosquitoes. Ecological Entomology 6: 129–154. [Google Scholar]
- Mangudo C, Aparicio JP, Gleiser RM. 2015. Tree holes as larval habitats for Aedes aegypti in urban, suburban and forest habitats in a dengue affected area. Bulletin of Entomological Research 105:679–684. [DOI] [PubMed] [Google Scholar]
- Mattingly PF. 1957. Genetical aspects of the Aedes aegypti problem. I. Taxonomy and bionomics. Annals of Tropical Medicine and Parasitology 51: 392–408. [PubMed] [Google Scholar]
- McBride CS, Baier F, Omondi AB, Spitzer SA, Lutomiah J, Sang R, Ignell R, Vosshall LB. 2014. Evolution of mosquito preference for humans linked to an odorant receptor. Nature 515: 222–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeill JR. 2010. Mosquito Empires. Cambridge University Press, New York. [Google Scholar]
- McNeill WH. 1976. Plagues and People. Doubleday, New York. [Google Scholar]
- Monath TP. 1994. Dengue: The risk to developed and developing countries. Proceedings of the National Academy of Sciences 91: 2395–2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen JL. 1977. Behavioral Differences in Two Subspecies of Aedes aegypti (Diptera L: Culicidae) in East Africa: PhD thesis, University Notre Dame. [Google Scholar]
- Pickrell JK, Pritchard JK. 2012. Inference of population splits and mixtures from genome-wide allele frequency data. PLOS Genetics 8 (art. e1002967). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell JR. 2016. New contender for most lethal animal. Nature 540: 525. [DOI] [PubMed] [Google Scholar]
- Powell JR. 2018. Mosquito-borne human viral diseases: Why Aedes aegypti? American Journal of Tropical Medicine and Hygiene, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell JR, Tabachnick WJ. 2013. History of domestication and spread of Aedes aegypti. Memorias Instituto Oswald Cruz 108: 11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pritchard JK, Stephens M, Donnelly P. 2000. Inference of population structure using multilocus genotype data. Genetics 155: 945–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigau-Perez JG. 1998. The early use of break-bone fever (quebranta huesos, 1771) and dengue (1801) in Spanish. American Journal of Tropical Medicine and Hygiene 59: 272–274. [DOI] [PubMed] [Google Scholar]
- Rosen L. 1986. Dengue in Greece in 1927 and 1928 and the pathogenesis of dengue hemorrhagic fever: New data and different conclusions. American Journal of Tropical Medicine and Hygiene 35:642–653. [DOI] [PubMed] [Google Scholar]
- Sawchuyk LA, Burke SDA. 1998. Gibraltar's 1804 yellow fever scourge: The search for scapegoats. Journal of the History of Medicine 53: 3–42. [DOI] [PubMed] [Google Scholar]
- Schaffner F, Mathis A. 2014. Dengue and dengue vectors in the WHO European region: Past, present, and scenarios for the future. Lancet Infectious Diseases 14: 1771–1780. [DOI] [PubMed] [Google Scholar]
- Smith CEG. 1956. The history of dengue in tropical Asia, and its probable relationship to the mosquito Aedes aegypti. Journal of Tropical Medicine and Hygiene 59: 243–251. [PubMed] [Google Scholar]
- Tabachnick WJ. 1991. Evolutionary genetics and the yellow fever mosquito. American Entomologist 37: 14–26. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.