Abstract
To determine the breastfeeding problems encountered in the postpartum period and effect of interventions done in relation to the problems based on breastfeeding studies in Turkey. This study is a systematic review and was conducted by performing a scan of the Turkish and English literature over the period October 2016–February 2017. The study included 27 articles and seven theses, which were published in 2000–2015 in Turkey and published in 2008–2017. Data are presented tabulating and the aggregate percentages were calculated for some data showing common characteristics. A total of 6736 parents and 592 babies were included in these studies. As a result of the combined percentage calculation based on the data of cross-sectional and case-control studies, the most frequently reported problems were having breastfeeding problem (24.5%), mother’s milk deficiency/worry about milk deficiency/thinking her baby is not satisfied/baby’s inadequate weight gain (15.7%), lack of knowledge and experience about breastfeeding/need for education and support (17.8%). Again, these studies showed that women stated the problems about have flat/depressed/small nipple (7.7%), pain/sensitivity (3.9%), swelling/fullness/engorgement (10.8%), redness (28.8%), crack/wound/bleeding (26.1%) and mastitis (5.6%). Methods of prenatal education/counselling/motivation/follow-up, strong motivation, proactive lactation management and social support, moist warm application, using of breast milk and olive oil and using of breast shield and feeding with container and pacifier using have been reported to be effective in the experimental/quasi-experimental and case report studies included in this systematic review. This study showed that women experienced a lot problem with breastfeeding and that more prenatal education/counselling/monitoring was used in reducing problems.
Keywords: Breastfeeding, care, midwifery, mother’s milk, nursing, postpartum period
Introduction
Breastfeeding is the best method for maternal health and the healthy growth and development of babies. The World Health Organization recommends that babies should be exclusively breastfed in the first six months of life (1). However, some problems that develop in the early postpartum period affect sucking and breastfeeding negatively in this period (2–4). Therefore, the rapid detection and resolution of breastfeeding problems encountered in the postpartum period is essential for maternal and infant health.
The Turkey Demographic and Health Survey reported that the rate of exclusive breastfeeding was 58% in the first two months of life and 10% in the 4th–5th months, although the proportion of babies who were breastfed during any period of life was substantially high in 2013 (5). There are many individual and cultural factors that influence breastfeeding babies. These factors have been reported to include womens’ education, employment status, sociocultural properties, concerns related to body image, psychological status, support received from healthcare workers, and decisions and desire for breastfeeding (6–8). Studies have suggested that especially the mother’s knowledge about breastfeeding and self-confidence, and the nursing technique used influenced the experience of breastfeeding problems and breastfeeding time (9, 10).
In the literature, it has been reported that there are some methods directed to individuals or groups that can be useful for the prevention and resolution of breastfeeding problems. These methods include providing education for mothers in the issues of breast care, correct nursing, techniques for increasing lactation, manual milking and storing milk, if necessary, and giving support to increase self-confidence (7, 11, 12). In addition, some studies mention use of creams, breastmilk and olive oil for nipples with the objective of preventing cracks and accelerating healing of cracks by enabling nipples to remain soft (13, 14). Again, it has been reported that the method of proactive lactation, which is defined as providing persistent help and support for the resolution of the mother’s individual problems, may also be used (15).
Breastfeeding problems that develop in the postpartum period have been proposed as an important condition that negatively influences exclusive breastfeeing and the breastfeeding period (11, 16). Some regional studies related to this issue have been conducted in our country. However, the extent and efficiency of the data obtained in these studies should be demonstrated wholly reflecting our cultural characteristics. The data obtained may contribute to studies directed to reducing breastfeeding problems and to increasing exclusive breastfeeding of babies.
The aim of the survey and the survey questions
In this systematic review, it was aimed to specify breastfeeding problems encountered in the postpartum period and the effect of the interventions related to these problems based on the results of the studies conducted in Turkey. The questions targeted to be answered in the survey are as follows: What are the breastfeeding problems encountered in the postpartum period? What are the interventions performed in order to reduce/prevent/solve breastfeeding problems?
Material and Methods
In this study, which is a systematic review, the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Checklist) was used in preparing the systematic review protocol and in writing the article (17). The Turkish test of this checklist is available (18).
Screening strategy
In this study, the Turkish and English literature between October 2016 and February 2017 were searched using the following search engines: Google Akademik (http://scholar.google.com.tr), PubMed, Ulusal Tez Merkezi (https://tez.yok.gov.tr/UlusalTezMerkezi/tarama.jsp), Dergi Park, Ulakbim and Türk Medline. The following key words were used for search: “emzirme ya/ya da anne sütü (breastfeeding and/or mother milk)”. A total of 34 studies that were conducted between 2000 and 2015 and published between 2008 and 2017 in Turkey and reported breastfeeding problems and solution methods, were included in this systematic review.
Specification and selection of the studies
Research articles and theses with cross-sectional, experimental/quasi-experimental, case-control, case presentation, and cohort designs, which had been conducted in Turkey and published in Turkish and English reporting the breastfeeding problems encountered in the postpartum period and the influence of interventions related to these problems, were included in this study. The details of article selection are shown in Figure 1.
Figure 1.
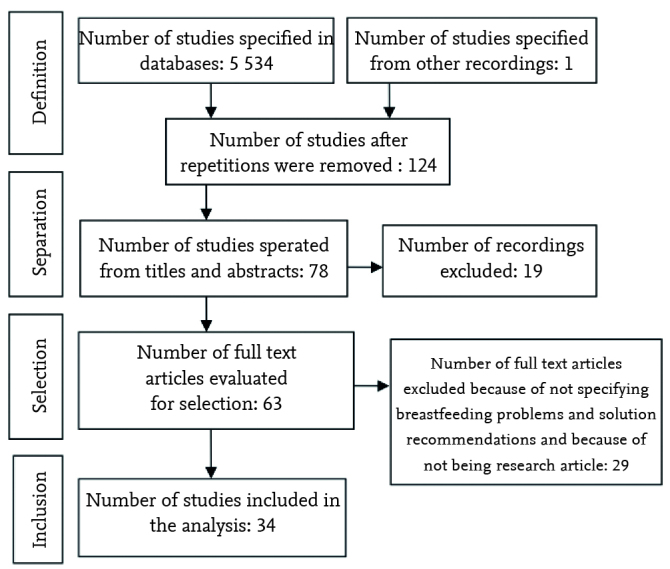
Selection and inclusion process of the studies
In this systematic review, the specification and selection of studies were realized independently by two investigators. When differences of opinion occured in relation with any study, consensus was achieved through discussion. Twenty-seven articles and seven theses were included in the assessement after selection was performed according to title, abstract, and full text.
Evaluation of the methodologic quality of the study
The methodologic quality of the articles included in this systematic review was evaluated by the secondary investigator and checked by the primary investigator. In this study, STROBE (“The Strengthening the Reporting of Observational Studies in Epidemiology”) (19) was used to evaluate the quality of observational studies (descriptive, cross-sectional, cohort and case-control) and “Critical Appraisal Skills Programme: Quality Appraisal Criteria for RTC Evidence” (CASP) was used to evaluate experimental and quasi-experimental studies (http://www.healthknowledge.org.uk/sites/default/files/documents/interactivel/fae/rct/CASP_11_Questions_for_an_RCT_with_HealthKnowledge_logo.pdf). The STROBE statement is a checklist composed of 22 articles, which indicate the parts to be written in an article during preperation of observational research articles. A Turkish version of the STROBE statement is available (20). CASP is a form composed of 10 articles and its Turkish text was prepared and used in this study. Quality assessment was made for two studies that were case reports. Quality assessment results for the articles can be obtained from the primary author, if requested.
Extraction and analysis of the data
A data extraction tool developed by the investigators was used to obtain the study data. With this data extraction tool, data related to the methods of the studies included in this systematic review, search methods, sample sizes, site and year of the studies, mean age, breast and breastfeeding problems experienced in the postpartum period, frequency of the problems, and the influence of the interventions related to these problems, could be obtained. The process of data extraction was performed by the secondary investigator independently and checked by the primary investigator.
Statistical Analysis
A meta-analysis could not be performed because the data obtained were not homogeneous and they were presented in tables. However, a combined percentage calculation was made in relation to some results reported commonly in the studies included in this systematic review.
Results
Search results
As a result of screening, 5534 records were reached initially. Sixty-three articles were reached as a result of the examination performed according to title, abstract, and full text, respectively. The data extraction process was performed with 34 studies after removing recurrent records, examinations according to inclusion criteria, and inclusion of additional studies. Explanations related to the selection of the articles are shown in Figure 1.
Methodologic quality assessment results
When the reporting qualities of the observational studies were evaluated over 22 points using the 22-article STROBE, the mean score was found as 16.8 (range, 14–21). In the assessment of the experimental/quasi-experimental studies using CASP, the mean score was found as 9.0 (range, 7–10).
Characteristics of the studies
A total of 34 studies related to breastfeeding problems experienced in the postnatal period and solution methods that were conducted in Turkey and published in English (15) and in Turkish (19) were included in this systematic review. It was observed that 16 of the studies were cross-sectional, 14 were experimental/quasi-experimental, two were case-control studies, and two were case reports. Twenty-seven articles and seven theses conducted between 2000 and 2015 and published between 2008 and 2017 were included in the study. The mean time period between the collection of data and the time when the data were published was 2.5 years in the studies. However, the year when the data were collected was not reported in six of the studies. A total of 6736 parents and 592 babies were included in the studies. The studies were conducted in 16 different provinces and seven different regions of Turkey; most studies were conducted in the Egean region (nine studies), the Maramara region (eight studies), and Middle Anatolia (nine studies). It was observed that the data were collected in the field in nine studies and in hospitals in 25 studies. It was found that the sample size of the studies ranged between 1 and 1080 and the time when the data were collected ranged between 0 and 60 months (Table 1, 2).
Table 1.
Characteristics of the observational studies included in the systematic review
| Authors (year) | Study design | Data collection tool | City | Year in which the study was conducted | Study field | Sample size | Mean maternal age, year (SD) | Screening time | Basic findings |
|---|---|---|---|---|---|---|---|---|---|
| Tokat et al. 2015 (31) | Cross-sectional | Questionnaire, ESDF and BSF | İzmir | 2010 | Hospital | 334 | 25.6±5.1 | The first 24 hours | With breastfeeding problems; 101 (30.2%) Breastfeeding problems; - Failure of sucking by the baby: 72 (21.6%) - Nipple problems: 24 (7.2%) - Insufficient breastmilk: 6 (1.8) |
| Yeşildal et al. 2008 (39) | Cross-sectional | Questionnaire | Düzce | 2006 | Hospital | 158 | 26.58±5.47 | 0–24 months | Discontinuing breastfeeding before six months: 21 (13.3%) Reasons for discontinuance; - Insufficient breastmilk/scantiness of breastmilk: 9 (5.7%) - Lack of sucking by the baby: 3 (1.9%) - Becoming pregnant again: 2 (1.3%) - Maternal illness/Maternal malnutrition/maternal use of drugs: 3 (1.9%) - Difficulty in breastfeeding techniques: 2 (1.3%) - Maternal preference for formula: 2 (1.3%) |
| Karaçam 2008 (40) | Cross-sectional | Questionnaire | Ankara | -- | Field | 514 | 26.21±5.20 | 1–5 months | Early start of solid foods: 244 (47.5%) Reasons; - Cesarean section: 72 (14.0%) - Frequent crying: 82 (16.0%) - Difficulty in pacifying the baby: 104 (20.2%) |
| Karaçam et al. 2010 (41) | Case-control | Questionnaire | Aydın | 2006–2007 | Hospital | 314 | 27.08±4.44 | 1 – 3 days | Breastfeeding problems; - Difficulty in sucking: 31 (9.9%) - Premature delivery: 3 (1.0%) - Insufficient breastmilk: 1 (0.3%) - Inability to suck because of cleft palate: 3 (1.0%) - Cracked nipple: 1 (0.3%) |
| Cihan and Karaçam 2017 (42) | Cross-sectional | Questionnaire | Aydın | 2015 | Hospital | 202 | 27.08±6.09 | 1–11 days | With breastfeeding problem: 45 (22.3%) Problems; - Cracked nipple: 17 (8.4%) - Deficient knowledge: 9 (4.5%) - Scantiness of breastmilk: 7 (3.5%) - Dented nipple: 8 (4.0%) - Preterm baby: 4 (2.0%) |
| Şencan et al. 2013 (43) | Cross-sectional | Questionnaire | Ankara | 2006–2007 | Hospital | 196 | 30.0±4.3 | 24–48-month | Problems; - Lack of experience: 50 (25.5%) babies - Flat-dented nipple: 21 (10.7%) - Cracks-wounds in nipple: 105 (53.6%) - Mastitis: 14 (7.1%) - Small, weak baby: 21 (10.7%) - Delayed feeding: 6 (3.1%) - Lack of education/assistance: 17 (8.7%) - Lack of appropriate environment for breastfeeding outside home: 40 (20.4%) |
| Gönenç and Vural 2015 (44) | Case-control | Questionnaire LATCH | Ankara | 2008–2009 | Hospital | 80 | 18–35 years | The first 24 hours | - Redness in nipple: 23 (28.8%) - Pain in nipple: 12 (15.0%) |
| Yılmazbaş et al. 2015 (45) | Cross-sectional | Questionnaire | İstanbul | 2013 | Hospital | 205 | 28.7±4.5 | 6–24 months | Problems developing in the first six months; - Mastitis/wound in nipple: 3 (1.5%) - Insufficient breastmilk: 61 (29.8%) - Inadequate weight gain: 13 (6.3%) - Drying up of breastmilk: 16 (7.8%) - Quitting of sucking by the baby: 11 (5.4%) - Inability to hold the nipple by the baby: 3 (1.5%) - Pregnancy in mother: 2 (1.0%) - Breastmilk jaundice: 1 (0.5%) |
| Akyüz et al. 2007 (46) | Cross-sectional | Questionnaire | Ankara | 2000 | Hospital | 120 | 27.0± 4.68 | - | Cracked nipple: 62 (51.7%) |
| Şahin et al. 2013 (24) | Cross-sectional | Questionnaire | Kayseri | -- | TSM ASM |
500 | 29.8±5.3 | 24–60 months | - Painful and cracked nipple; 230 (46.0%) - Concern for insufficient breastmilk: 171 (34.2%) - Excessive milk secretion complicating breastfeeding: 149 (29.8%) - Flat and dented nipple: 58 (11.6%) - Mastitis: 46 (9.2%) - Excessive fullness in breast: 45 (9.0%) - Obstructed ducts: 41 (8.2%) |
| Taş Arslan and Yeniterzi 2013 (47) | Cross-sectional | Questionnaire | Konya | 2011 | Hospital | 100 mothers 100 fathers |
Mother: 27.43±5.94 Father: 30.94±5.74 |
32–37-week preterm babies | Experiencing problems in breastfeeding: 28 (28.0%) Problems; - Inability of the baby to latch on the breast fully: 7 (7.0%) - Small nipple: 6 (6.0%) - Baby become tired and sleeps: 15 (15.0%) |
| Çatak et al. 2012 (48) | Cross-sectional | Questionnaire | Burdur | 2009–2010 | ASM | 1080 | -- | 0–18 months | Quitting breastfeeding: 232 (21.5%) Reasons for quitting breastfeeding; - Insufficient breastmilk; 98 (9.1%) - Rejection by the baby: 94 (8.7%) - Becoming pregnant: 20 (1.9%) - Nipple/breast problem 17 (1.6%) - Baby is ill/weak: 16 (1.5%) - Mother is ill/weak: 10 (0.9%) - Thinking that it is time to quit; 9 (0.8%) - Going back to work: 4 (0.4%) |
| Eskibozkurt 2008 (49) | Cross-sectional | Questionnaire | İstanbul | 2007 | Hospital | 300 mothers | -- | 1–3rd day | With breastfeeding problem: 37 (12.3%) Problems; - Pain and swelling: 12 (4.0%) - Insufficient breastmilk/thinking that baby was not satiated: 30 (10.0%) - Inadequate sucking by the baby: 16 (5.3%) - Difficulty in breastfeeding after cesarean section: 7 (2.3%) - Not knowing how to hold baby while breastfeeding: 12 (4.0%) |
| Bağlar 2008 (50) | Cross-sectional | Questionnaire, LATCH, Breastfeeding monitoring card | Kocaeli | 2007 | Hospital | 80 mothers | 30.60±4.06 | 0–6 months | Problems; Flat/dented nipple: 11 (13.8%) Cracked nipple: 19 (23.8%) |
| Ünalan et al. 2008 (51) | Cross-sectional | Questionnaire | İstanbul | 2006 | AÇSM | 358 | 28.35±5.24 | 0–12 months | Reasons for starting solid foods early; - Insufficiency of breastmilk/crying of baby: 158 (44.1%) - Thinking that it is time to start solid foods: 5 (1.4%) - Lack of weight gain: 22 (6.2%) - Social pressure: 12 (3.4%) - Health problem in mother or infant: 11 (3.1%) - Rejection of sucking by the baby: 7 (2.0%) - Going back to work: 4 (1.1%) - Considering formula as convenience: 1 (0.3%) |
| Bülbül et al. 2012 (52) | Cross-sectional | Questionnaire | İstanbul | 2011–2012 | Healthy child outpatient clinic | 200 | 28±5.5 | 24 months | Reasons for starting solid foods early; - Insufficient breastmilk: 67 (33.5%) - Insufficient weight gain: 22 (11.0%) - Thinking that it is time to start solid foods: 15 (7.5%) - Mother’s going back to work: 11 (5.5%) - Twin babies: 4 (2.0%) - Mother’s becoming pregnant: 1 (0.5%) - Mother’s becoming ill: 2 (0.5%) |
| Bolat et al. 2011 (53) | Cross-sectional | Questionnaire | İstanbul | 2009 | Healthy child outpatient clinic | 246 | 28.5 (17–43) | 0–6 months | Reasons for starting solid foods early; - Late initiation of breastfeeding: 61 (24.8%) - Lack of breastfeeding education during pregnancy: 72 (29.3%) - Preterm delivery: 14 (5.7%) |
| İnce et al. 2010 (54) | Cross-sectional | Questionnaire | Ankara Kayseri | 2009 | Healthy child ; outpatient clinic | 285 | 28.5±5.5 | 2 weeks – 3 months | With breastfeeding problem: 88 (31.0%) Problems with nursing - Inability to latch on to breast: 39 (13.7%) - Scantiness of breastmilk: 25 (8.8%) - Cracked nipple: 9 (3.2%) - Inability to suck well on the first day: 6 (2.1%) - Latching on to a single breast: 3 (1.1%) - Mastitis: 3 (1.1%) - Collection of breastmilk in breast: 2 (0.7%) - Dented nipple: 1 (0.4%) |
AÇSM: Center for maternal and infant health; ASM: Family health center; BSF: “Beast-feeding Self-Efficacy Form”; ESDF: Breastfeeding results assessment form; LATCH: Breastfeeding Identification Scale; TSM: Community Health Center
Table 2.
Characteristics and results of the experimental studies and case reports included in the systematic review
| Authors (years) | Study design | Data collection tool | City | Study Year | Study field | Sample size | Mean maternal age, years (SD) | Screening time | Intervention | Basic results |
|---|---|---|---|---|---|---|---|---|---|---|
| Çiftci and Arikan 2011 (55) | Semi-experimental | Questionnaire S-TAI | Erzurum | 2008–2009 | Home | Education: 32 Control: 30 |
-- | 2.5, 3, 4, 5 and 6th months | Nursing techniques education | Education reduced the level of maternal anxiety. |
| Yılmaz et al. 2014 (56) | Experimental | Questionnaire | Anakara | 2006–2008 | Hosp | Cup: 254 Feeding bottle: 268 |
Cup: 24.8± 3.1 feeding bottle: 24.6±3.3 |
Preterms born at the 32–35th weeks 3 and 6th months | Feeding with cup | Feeding preterm babies with cup increased exclusive breastfeeding in the 3rd and 6th months. |
| Kaya 2016 (57) | Experimental | Questionnaire, LATCH | Erzurum | 2013–2014 | Hospital | Pacifier group n=34 Control n=36 |
Pacifier group: 32.19±1.51 weeks Control: 32.71±0.94 weeks |
30–34 weeks preterm after 48 hours and before discharge | Use of pacifier | Use of pacifier improved sucking and shortened the time to switching to whole breastfeeding |
| Küçükoğlu and Çelebioğlu 2014 (58) | Semi-experimental | Questionnaire, BSF, LATCH, AÖF | Erzurum | 2010–2011 | Hospital | Education: 42 Control: 43 |
-- | 1 and 5th days 1–6th months |
Natural breast-feeding education | In low-birth-weight babies, education given to mother, increased self-confidence and breastfeeding success. |
| Karadağ 2008 (59) | Semi-experimental | Questionnaire | Kütahya | 2007–2008 | ASM | Experiment: 50 Control: 50 |
-- 18–35 year and above |
3rd trimester and postpartum 2nd month | Education during pregnancy | Education given during pregnancy was effective in reducing postpartum breast problems (tenderness, fullness, pain and cracks). |
| Büyükkayacı 2010 (60) | Experimental | Questionnaire Self-care strenght scale | Çorum | 2008 –2009 | House | 140 women Experiment: 70 Control: 70 |
29.1±2.5 | 0–6th weeks after cesarean section | Home care service | Home care service reduced breastfeeding problems observed between the 15th and 42nd days. |
| Ünsal Atan 2008 (13) | Experimental | Questionnaire, EGF and EİF | İzmir | 2006 –2007 | Hospital | - Breastmilk: 35 - Hot damp application: 35 - tea compress: 35 |
22.4±3.29 | 0–14 days First encounter 0–20 hours 14th day |
Comparison of applications of breastmilk, moist hot and tea pads on breast | Moist hot tea and moist hot applications were more effective in reducing nipple problems compared with breastmilk application. |
| Ekşioğlu 2016 (61) | Experimental | Questionnaire, EÖYÖ and LATCH | İzmir | 2013–2014 | Hospital | Intervention n=111 Control: 109 |
Intervention: 29.11±5.26 Control: 28.04±5.23 |
0–6 months | Breastfeeding education | Increased the rate of exclusive breastfeeding in the first six months and maternal self-efficacy for nursing. |
| Kirlek 2010 (14) | Experimental | Questionnaire, EGF, GKÖ | Aydın | 2009 –2010 | Hospital | Experiment: 26 Control: 13 |
Olive oil group: 25,15±4,01 Control: 25.69±4.15 |
0–10 days | Use of olive oil | Use of breastmilk and olive oil were similarly effective for pain and cracks in nipple. |
| Demirci 2015 (62) | Experimental | Questionnaire, LATCH | Bursa | 2013–2014 | Hospital | 80 mothers | 27.26±4.18 | The first 24 hours and 7 days | Use of breast shield | Use of breast shield in the postpartum period reduced development of cracks in nipples. |
| Geçkil et al. 2012 (63) | Experimental | Questionnaire | Adıyaman | 2008–2009 | ASM | 42 Experiment 52 Control |
Experiment: 29.52±5.71 Control: 28.03±5.30 |
0–7 months | Education for supporting breastfeeding, follow-up and motivation | Influenced positively exclusive breastfeeding, breastfeeding time and efficient maternal nursing behaviors. |
| Onbaşı et al. 2011 (64) | Experimental | Questionnaire | Edirne | -- | Hospital | Education: 90 Control: 100 |
-- Women aged 17 years and above |
Pregnant women presenting for delivery 6th month after delivery | Education given for one time in the prenatal period | The rate of exclusive breastfeeding in the first six months was significantly higher in the education group. |
| Üstüner and Bodur 2009 (65) | Experimental | Questionnaire | Giresun | -- | Hospital | Education and follow-up: 93 Control: 100 |
27.2±5.0 (17–44) | 0–6 months | Monthly follow-up and intensifying breastfeeding education | This intervention increased the rate of exclusive breastfeeding in the first six months (follow-up: 21,5% and control: 9.0%). |
| Aksu et al. 2011 (66) | Experimental | Questionnaire | Aydın | 2008 | House | Education/support: 27 Control: 27 |
Education/support: 22.5+3.5 Control: 23.0+4.6 |
2nd and 6th months | Breastfeeding education and support given at home on the postpartum 3rd day | This intervention increased exclusive breastfeeding in the first six months, breastfeeding time and breastfeeding knowledge. |
| Tetik et al. 2013 (67) | Case report | Case recording form | Ankara | -- | Hospital | 1 | 26 years | Male baby aged 8 weeks born at the 36th week | Strong motivation | On the 4th day of intervention, relactation process was initiated and breastfeeding support method was discontinued in 8 days. |
| Yikilmaz ve Wilson-Clay 2016 (15) | Case report | Case recording form | Denizli | -- | Hospital | 1 | 27 years | Baby born at the 38th week with a birth weight of 2250 g follow-up for 0–4 months | Proactive lactation management and social support | Mother who had nevus on nipple was enabled to breastfeed her baby in the first 4 months. |
AÖF: Antropometric measurement form; ASM: Family health center; BSF: “Beast-feeding Self-Efficacy Form”; EGF: Breastfeeding observation form; EİF: Breastfeeding follow-up form; EÖYÖ: Breastfeeding self-eficacy scale; GKÖ: Visual Comparison scale; LATCH: Breastfeeding Identification Scale; S-TAI: “State-trait anxiety inventory”
Breastfeeding problems observed in the postpartum period
The data of observational studies demonstrated that women mentioned numerous breastfeeding problems. As a result of combined percentage calculation, 24.5% of the women reported that they experienced breastfeeding problems. The women frequently reported the following breastfeeding problems: lack of maternal knowledge of breastfeeding technique/inadequate information and experience/need for education and assistance (17.8%), inadequate breastmilk/concern for inadequate breastmilk/thought that the baby was not satiated adequatlely/inadequate weight gain of the baby (15,7%). Again, it was found that women reported the following problems related to their breasts in these studies: redness/temperature change (28.8%), cracks/wound/bleeding (26.1%), swelling/fullness/engorgement (10.8%), flat/dented/small nipples (7.7%), pain/tenderness (3.9%), and mastitis (5.6%) (Table 3). The other problems reported are shown in Table 3.
Table 3.
Problems related to breastfeeding and their frequencies
| Breastfeeding problems | Number of studies | Number of participants | Number of subjects | Combined % |
|---|---|---|---|---|
| Experience of breastfeeding problems | 5 | 1221 | 299 | 24.5 |
| Inadequate breastmilk/lack of breastmilk/concern related to inadequate breastmilk/thought that the baby is not satiated adequately/inadequate weight gain of the baby | 12 | 4141 | 649 | 15.7 |
| Inadequate sucking by the baby/rejection of sucking/lack of sleep/difficulty in sucking | 9 | 3134 | 255 | 8.1 |
| Lack of maternal knowledge related to breastfeeding technique/inadequate information and experience/need for education and assistance | 6 | 1284 | 229 | 17.8 |
| Prematurity/inability to latch on to breast fully/small baby/weak baby/baby with health problem | 9 | 2986 | 118 | 3.7 |
| Nipple problems | 3 | 1596 | 146 | 9.2 |
| Pain/tenderness in the breasts | 3 | 665 | 26 | 3.9 |
| Swelling/fullness/engorgement | 1 | 500 | 54 | 10.8 |
| Erythema/temperature change in nipple | 1 | 80 | 23 | 28.8 |
| Fissure/wound/bleeding in nipple | 7 | 1697 | 443 | 26.1 |
| Mastitis | 4 | 1186 | 66 | 5.6 |
| Flat/indented/small nipple | 6 | 1363 | 105 | 7.7 |
| Excessive milk secretion | 1 | 500 | 149 | 29.8 |
| Obstructed mammary duct | 1 | 500 | 41 | 8.2 |
| Difficulty in breastfeeding after cesarean section | 2 | 814 | 79 | 9.7 |
| Delayed feeding/breastfeeding | 3 | 624 | 73 | 11.7 |
| Cleft palate | 1 | 314 | 3 | 1.0 |
| Inability to find an appropriate environment for breastfeeding outside home | 1 | 196 | 40 | 20.4 |
| Becoming pregnant | 4 | 1643 | 25 | 1.5 |
| Initiating solid food in the early stage (before the 6th month)/thinking that it is time for solid food | 5 | 2110 | 295 | 14.0 |
| Mother’s being ill/maternal use of medication | 3 | 1438 | 14 | 1.0 |
| Difficulty in pacifying the baby | 1 | 514 | 104 | 20.2 |
| Maternal preferance for formula/considering solid food as convenience | 2 | 516 | 3 | 0.6 |
| The mother’s going back to work | 3 | 1638 | 19 | 1.2 |
| Twin babies | 1 | 200 | 4 | 2.0 |
| Latching on to a single breast | 1 | 285 | 3 | 1.1 |
| Breastmilk jaundice | 1 | 205 | 1 | 0.5 |
Solution interventions related to breastfeeding problems experienced in the postpartum period
In the experimental/quasi-experimental studies and case reports included in the systematic review, it was reported that prenatal education/counselling/motivation/follow-up during pregnancy was efficient in reducing breastfeeding problems and in improving breastfeeding success; strong motivation, proactive lactation management, and social support were efficient in initiating the process of lactation; moist hot application and use of breastmilk, olive oil, and breast shields were efficienct in reducing breast problems, and feeding with cups and use of pacifiers were efficient in increasing the success of breastfeeding and nursing in preterm babies (Table 4).
Table 4.
Solution interventions related to breastfeeding problems
| Solution initiatives/intervention | Number of studies | Number of participants |
|---|---|---|
| Prenatal/postnatal education/counselling/motivation/follow-up | 9 | 1138 |
| Humid hot application | 1 | 105 |
| Use of breast shield | 1 | 80 |
| Feeding preterm babies with cup | 1 | 522 |
| Use of pacifier in preterm babies | 1 | 70 |
| Use of breastmilk and olive oil | 1 | 39 |
| strong motivation (in initiation of the process of lactation) | 1 | 1 |
| Proactive lactation management and social support | 1 | 1 |
Discussion
In this systematic review, it was observed that a significant portion of women (24.5%) experienced breastfeeding problems and these problems varied by maternal factors and factors related to breastmilk, baby, and breast. Again, this study showed that prenatal education/counselling/motivation/follow-up methods were efficient in reducing breastfeeding problems and in improving breastfeeding success. In addition, strong motivation, proactive lactation method and social support, moist hot application, and use of breast shields, feeding with cups and use of pacifiers were reported to be efficient in solving some specific problems. Although these results do not represent our country and cannot be generalized, they are important in terms of demonstrating important information covering many regions and provinces.
In this study, which was conducted based on the literature, it was observed that breastfeeding problems were substantially common in the postpartum period. Similar results have been reported in studies conducted in our country and other countries (21–25). These results show that breastfeeding problems should be strongly emphasized in terms of maternal and infant health.
In this systematic review, 12 studies showed that mothers had problems directed to the amount of breastmilk including “inadequate breastmilk/lack of breastmilk/concern for inadequate breastmilk/thought that the baby was not satiated adequately/inadequate weight gain.” In addition, it was reported that some mothers initiated solid food/thought it was time for starting solid foods before the sixth month in five studies, and mothers preferred formula and perceived formula convenient in two studies. In a study conducted in this issue, Mekuria et al. (26) reported that a significant portion of mothers (18%) started solid foods in the early stage because they thought that breastmilk was inadequate and insufficient for the baby. Meedya et al. (27) reported that women’s decision and feeling of self-efficacy were important in continuing breastfeeding. These results might indicate that healthcare workers should carefully evaluate this condition and take the necessary precautions because this could lead to early starting of solid foods.
In this systematic review, “lack of maternal knowledge of nursing technique/inadequate information and experience/need for education and assistance” were indicated as breastfeeding problems in six studies. In another study conducted in our country, the inability to reach midwives and nurses and inability to receive support for application were reported as breastfeeding problems (28). On the other hand, Swerts et al. (16) emphasized that nursing education and support was an important part of the role of midwives in the postpartum period. Yi et al. (29) showed that breastfeeding education increased maternal self-efficacy in this issue. These results are important in terms of emphasizing the midwives’ and nurses’ roles in nursing education, counselling, and support.
In nine of the studies included in this systematic review, it was found that some babies (approximately 4%) encountered problems related to breastfeeding including “inadequate sucking/rejecting sucking/not sleeping/difficulty in pacifying/difficulty in sucking, prematurity/inability to latch on to the breast completely/small baby/weak baby/baby with health problems.” According to these results, it can be stated that it is important and necessary for midwives and nurses to consider problems that are specific for individual babies.
In this systematic review, it was found that women commonly experienced preventable nipple problems including pain, tenderness, swelling, fullness, redness, temperature change, cracks, wounds, bleeding, and mastitis. In addition, some women encountered structural problems related to breast including flat/indented/small nipples. In a study conducted in this issue, Mekuria and Edris (26) reported that solid foods were started in some babies (7%) in the early stage because of breast/nipple problems. These results show that studies involving preventive and early diagnostic and therapeutic approaches related to breast and nipple problems should be conducted.
Another problem indicated in this study was “difficulty in breastfeeding after cesarean section.” Similarly, İsik et al. (30) reported cesarean section negatively influenced the time of initiation of breastfeeding and the frequency of breastfeeding in their study in which they compared cesarean section and normal vaginal delivery. In another study, Tokat et al. (31) reported that women who underwent cesarean section experienced breastfeeding problems with a higher rate. Sutherland et al. (32) also reported that cesarean section influenced initiation of breastfeeding and breastfeeding success negatively. Tewabe (33) reported that cesarean section delayed initiation of breastfeeding. These results are valuable in terms of demonstrating that cesarean section influences infant nutrition and thus infant health negatively.
In this systematic review, it was reported that some babies (approximately 12%) “were fed/breastfed in the late stage” in three studies. In a similar study, it was reported that the site and mode of delivery (cesarean section), the baby’s and mother’s being ill and delayed secretion of breastmilk delayed initiation of breastfeeding (33). This should be considered in maternal care and follow-up in the postpartum period.
In this study, it was stated that three babies experienced sucking problems because of cleft palate. In another study, it was reported that cleft palate and cleft lip were very important problems influencing breasfeeding of babies and the possibility of development of malnutrition was high in these babies (34). These results show that special breastfeeding methods should be developed for these babies and parents should be supported in this issue.
In this systematic review, it was observed that some mothers (1%) did not breastfed their babies because they were ill or they received medication in three studies. In a similar cross-sectional study conducted in Ethiopia, it was reported that mothers initiated breastfeeding in the late stage mostly (18%) because they were ill (33). In another study, it was reported that mothers started feeding their babies with solid foods because they were weak and ill (8%) (26). These results are important in terms of demonstrating the importance of maternal health state in breastfeeding.
Another breastfeeding problem found in this systematic review is “the mother’s going back to work.” Mekuria and Edris (26) reported that mothers started solid foods in the early stage for some babies (28%) because of incompatibility with work. In this study, some mothers additionally reported that they encountered breastfeeding problems including “inability to find appropriate nursing environment outside home, the baby’s sucking only a single breast, and breastmilk jaundice.” These results demonstrate the necessity for special regulations, education, and counselling for working mothers.
In one study included in this systematic review, twin babies were indicated as a breastfeeding problem. In another study conducted in this issue, it was reported that the rate of exclusive breastfeeding in the first six months was very low in twin babies (35). According to these results, it can be stated that individual nursing counselling should be given to mothers with twin babies.
In this systematic review, it was observed that some mothers experienced breastfeeding problems because they became pregnant again in four studies. This result is valuable in terms of demonstrating that family planning counselling in the postpartum period is very important in the continuance of breastfeeding.
In this systematic review, it was found that the most commonly reported (in nine studies) solution initiatives/interventions related to breastfeeding problems were “prenatal/postnatal education/counselling/motivation/follow-up.” In a systematic review conducted in this issue, Nguyen et al. (36) examined interventions that were successful in helping exclusive breastfeeding for one or more months in women who became mothers for the first time. In this study, support given by the family (especially the father), friends and other individuals, nursing education, counselling and support provided by breastfeeding nurse, physician and woman-baby-child peer support groups, nursing counselling and community breastfeeding support groups, the Baby-Friend Hospital Program, enabling early skin-to-skin contact, and print media were reported to be efficient methods (36). In a Cochrane systematic review conducted by Balogun et al. (12), it was reported that low quality evidence showing that nursing education given by healthcare professionals, nursing counselling given by individuals who were not healthcare professionals, and peer support were effective in increasing the rate of initiating breastfeeding was found. Other studies also emphasized that education and support given to mothers were important in successful breastfeeding (27, 37). On the other hand, Swerts et al. (16) reported that most midwives gave breastfeeding support as technical experts and preferred to give breastfeeding support, but encountered numerous obstacles in work environments in a systematic review. These results are important in terms of demonstrating the extent of the healthcare workers’ duties and responsibilities.
In a study included in the systematic review, a solution intervention related to breastfeeding problems was indicated as “feeding preterm babies with cups.” In the Cochrane systematic review conducted with five studies including also this study, it was reported that feeding with cups was somewhat useful in terms of breastfeeding rates in the first six months in preterm babies, but there was no evidence related to term babies in this issue (38).
In this systematic review, it was also specified that methods including “moist hot application, use of breast shields, use of pacifiers in preterm babies, use of breastmilk and olive oil, strong motivation (in initiating the process of lactation), proactive lactation management and social support” were also used in solving breastfeeding problems. However, similar studies related to this issue could not be found in the literature.
Conclusion and Recommendations
In this study, it was concluded that women commonly experienced breastfeeding problems in the postpartum period, but solution approaches developed specifically for these problems were limited. The following recommendations can be made based on these results:
Preventive precautions related to breastfeeding problems experienced frequently by mothers should be taken and individual solution methods related to these problems should be developed;
Healthcare workers who serve in formal and non-formal health education should be sensitive in the issue of breastfeeding problems and solution recommendations and should involve these topics in the lessons they give;
Healthcare managers should establish institutional politics to reduce breastfeeding problems, improve solution recommendations, and extend the scope of the service they give;
Qualitative and observational studies, which could provide more comprehensive data in the issue of solution of breastfeeding problems, and new experimental studies in which special solution methods for different problems will be investigated should be conducted.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - Z.K. Design - Z.K., M.S.; Supervision - Z.K.; Funding - Z.K., M.S.; Data Collection and/or Processing - Z.K., M.S.; Analysis and/or Interpretation - Z.K., M.S.; Literature Review - Z.K.; Writing - M.S.; Critical Review - Z.K.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.World Health Organization. Postnatal care for mothers and newborns: Highlights from the World Health Organization 2013 Guidelines. [Accessed on: 01 Ekim 2016]. Avaible from: http://www.who.int/maternal_child_adolescent/publications/WHO-MCA-PNC-2014-Briefer_A4.pdf.
- 2.Benoit B, Goldberg L, Campbell-Yeo M. Infant feding and maternal guilt: The application of a feminist phenomenological framework to guide clinician practices in breast feeding promotion. Midwifery. 2016;34:58–65. doi: 10.1016/j.midw.2015.10.011. https://doi.org/10.1016/j.midw.2015.10.011 [DOI] [PubMed] [Google Scholar]
- 3.Kartal B, Kaplan B, Buldu A, Ateş CS, Ekinci E. Doğum sonu dönemdeki kadınların emzirme özellikleri ve bunu etkileyen meme sorunları. İzm Üniv Tıp Derg. 2015;1:1–10. [Google Scholar]
- 4.Neifert M, Bunik M. Overcoming clinica barriers to exclusive breastfeeding. Pediatr Clin North Am. 2013;60:115–45. doi: 10.1016/j.pcl.2012.10.001. https://doi.org/10.1016/j.pcl.2012.10.001 [DOI] [PubMed] [Google Scholar]
- 5.Türkyılmaz AS, Adalı T, Çağatay Seçkiner P. Beslenme durumu ve çocuk sağlığı: Hacettepe Üniversitesi Nüfus Etütleri Enstitüsü 2013 Türkiye Nüfus ve Sağlık Araştırması. Ankara: Hacettepe Üniversitesi Nüfus Etütleri Enstitüsü, T.C. Kalkınma Bakanlığı ve TÜBİTAK; 2014. pp. 156–69. [Google Scholar]
- 6.Çölaraz N. Yenidoğan döneminde anne sütü ile beslenmeye başlanması üzerinde etkili olan sosyodemografik faktörlerin değerlendirilmesi. Türkiye Çocuk Hast Derg. 2012;6:215–20. [Google Scholar]
- 7.Ouyang Y-Q, Su M, Redding SR. A survey on difficulties and desires of breast-feeding women in Wuhan, China. Midwifery. 2016;37:19–24. doi: 10.1016/j.midw.2016.03.014. https://doi.org/10.1016/j.midw.2016.03.014 [DOI] [PubMed] [Google Scholar]
- 8.Taveras EM, Capra AM, Braveman PA, Jensvold NG, Escobar GJ, Lieu TA. Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics. 2003;112:108–15. doi: 10.1542/peds.112.1.108. https://doi.org/10.1542/peds.112.1.108 [DOI] [PubMed] [Google Scholar]
- 9.Kronborg H, Vaeth M. How are effective breastfeeding technique and pacifier use related to breastfeeding problems and breastfeeding duration. BIRTH. 2009;36:34–42. doi: 10.1111/j.1523-536X.2008.00293.x. https://doi.org/10.1111/j.1523-536X.2008.00293.x [DOI] [PubMed] [Google Scholar]
- 10.Yanikkerem E, Tuncer R, Yilmaz K, Aslan M, Karadeniz G. Breast-feeding knowledge and practicesamong mothers in Manisa, Turkey. Midwifery. 2009;25:e19–32. doi: 10.1016/j.midw.2007.10.012. https://doi.org/10.1016/j.midw.2007.10.012 [DOI] [PubMed] [Google Scholar]
- 11.Powell R, Davis M, Anderson AK. A qualitative look into mother’s breastfeeding experiences. J Neonatal Nurs. 2014;20:259–65. https://doi.org/10.1016/j.jnn.2014.04.001 [Google Scholar]
- 12.Balogun OO, O’Sullivan EJ, McFadden A, et al. Interventions for promoting the initiation of breastfeeding. Cochrane Database Syst Rev. 2016;11:CD001688. doi: 10.1002/14651858.CD001688.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atan ÜŞ. Doktora Tezi. İzmir: Ege Üniversitesi Sağlık Bilimleri Enstitüsü; 2008. Primipar emziren annelerde meme ucu sorunlarının önlenmesinde farklı yöntemlerin etkinliğinin incelenmesi; p. 305. [Google Scholar]
- 14.Kirlek F. yüksek lisans tezi. Aydın: Adnan Menderes Üniversitesi Sağlık Bilimleri Enstitüsü; 2010. Erken postpartum dönemde meme başı ağrısı ve çatlaklarının önlenmesinde anne sütü ve zeytinyağının etkisi; p. 206. [Google Scholar]
- 15.Yikilmaz ŞR, Clay BW. Successful breastfeeding outcome of a woman with a nevus of the nipple: A case study. J Hum Lact. 2016;32:361–3. doi: 10.1177/0890334415627026. https://doi.org/10.1177/0890334415627026 [DOI] [PubMed] [Google Scholar]
- 16.Swerts M, Westhof E, Bogaerts A, Lemiengre J. Supporting breast-feeding women from the perspective of the midwife: A systematic review of the literature. Midwifery. 2016;37:32–40. doi: 10.1016/j.midw.2016.02.016. https://doi.org/10.1016/j.midw.2016.02.016 [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, et al. Reprint—preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Physical Therapy. 2009;89:873–80. [PubMed] [Google Scholar]
- 18.Karaçam Z. Sistematik derleme metodolojisi: sistematik derleme hazırlamak için bir rehber. DEUHYO ED. 2013;6:26–33. [Google Scholar]
- 19.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12:1500–24. doi: 10.1016/j.ijsu.2014.07.014. https://doi.org/10.1016/j.ijsu.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, et al. Karaçam Z, translator. STROBE Bildirimi: Epidemiyolojide gözlemsel araştırma raporu yazımının güçlendirilmesi için bir rehber. Anadolu Hemşirelik ve Sağlık Bilimleri Dergisi. 2014;17:64–72. [Google Scholar]
- 21.Gerd AT, Bergman S, Dahlgren J, et al. Factors associated with discontinuation of breastfeeding before 1 month of age. Acta Paediatr. 2012;101:55–60. doi: 10.1111/j.1651-2227.2011.02405.x. https://doi.org/10.1111/j.1651-2227.2011.02405.x [DOI] [PubMed] [Google Scholar]
- 22.Örün E, Yalçın S, Madendağ Y, et al. Annelerin sosyodemografik ve psikopatolojik özellikleri ile bebeklerini ilk 1–1,5 ayda sadece anne sütü ile besleme durumlarına etkisi. Çocuk Sağlığı ve Hastalıkları Dergisi. 2009;52:167–75. [Google Scholar]
- 23.Riordan J, Wambach K. Breastfeeding and human lactation. 4th ed. Massachusetts: Jones and Bartlett Publishers; 2010. Perinatal and intrapartum care; pp. 236–9. [Google Scholar]
- 24.Şahin H, Yılmaz M, Aykut M, et al. Kayseri’de iki toplum sağlığı merkezine başvuran annelerde emzirme sorunları ve risk etmenleri. Türk Pediatri Arş. 2013;48:145–51. https://doi.org/10.4274/tpa.1034 [Google Scholar]
- 25.Walker M. Conquering common breast-feeding problems. J Perinat Neonatal Nurs. 2008;22:267–74. doi: 10.1097/01.JPN.0000341356.45446.23. https://doi.org/10.1097/01.JPN.0000341356.45446.23 [DOI] [PubMed] [Google Scholar]
- 26.Mekuria G, Edris M. Exclusive breastfeeding and associated factors among mothers in Debre Markos, Northwest Ethiopia: A cross-sectional study. Int Breastfeed J. 2015;10:1. doi: 10.1186/s13006-014-0027-0. https://doi.org/10.1186/s13006-014-0027-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meedya S, Fahy K, Parratt J, Yoxall J. Supporting women to achieve breastfeeding to six months postpartum – The theoretical foundations of a successful program. Women and Birth. 2015;28:265–71. doi: 10.1016/j.wombi.2015.06.006. https://doi.org/10.1016/j.wombi.2015.06.006 [DOI] [PubMed] [Google Scholar]
- 28.Demirtas B. Breastfeeding support received by Turkish first-time mothers. Int Nurs Rev. 2012;59:338–44. doi: 10.1111/j.1466-7657.2012.00977.x. https://doi.org/10.1111/j.1466-7657.2012.00977.x [DOI] [PubMed] [Google Scholar]
- 29.Yi CM, Yim IW, Chow CK. The effect of a self-efficacy-based educational programme on maternal breast feeding self-efficacy, breast feeding duration and exclusive breast feding rates: A longitudinal study. Midwifery. 2016;36:92–8. doi: 10.1016/j.midw.2016.03.003. https://doi.org/10.1016/j.midw.2016.03.003 [DOI] [PubMed] [Google Scholar]
- 30.İsik Y, Dag ZO, Tulmac OB, et al. Early postpartum lactation effects of cesarean and vaginal birth. Ginekologia Polska. 2016;87:426–30. doi: 10.5603/GP.2016.0020. https://doi.org/10.5603/GP.2016.0020 [DOI] [PubMed] [Google Scholar]
- 31.Tokat MA, Serçekus P, Yenal K, et al. Early Postpartum breast-feeding outcomes and breast-feeding self-efficacy in turkish mothers undergoing vaginal birth or cesarean birth with different types of anesthesia. Int J Nurs Knowl. 2015;26:73–9. doi: 10.1111/2047-3095.12037. https://doi.org/10.1111/2047-3095.12037 [DOI] [PubMed] [Google Scholar]
- 32.Sutherland T, Pierce CB, Blomquist JL, et al. Breastfeeding practices among first-time mothers and across multiple pregnancies. Matern Child Health J. 2012;16:1665–71. doi: 10.1007/s10995-011-0866-x. https://doi.org/10.1007/s10995-011-0866-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tewabe T. Timely initiation of breastfeeding and associated factors among mothers in Motta town, East Gojjam zone, Amhara regional state, Ethiopia, 2015: A cross-sectional study. BMC Pregnancy Childbirth. 2016;16:314. doi: 10.1186/s12884-016-1108-4. https://doi.org/10.1186/s12884-016-1108-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tungotyo M, Atwine D, Nanjebe D, et al. The prevalence and factors associated with malnutrition among infants with cleft palate and/or lip at a hospital in Uganda: A cross-sectional study. BMC Pediatr. 2017;17:17. doi: 10.1186/s12887-016-0775-7. https://doi.org/10.1186/s12887-016-0775-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cinar N, Kose D, Alvur M, et al. Mothers’ attitudes toward feeding twin babies in the first six months of life: a sample from Sakarya, Turkey. Iran J Pediatr. 2016;26:e5413. doi: 10.5812/ijp.5413. https://doi.org/10.5812/ijp.5413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nguyen MT, Snow G, Wheeler H, et al. Clinical question: In post-partum first-time mothers, what interventions are successful for helping women sustain exclusive breast feeding for one month or more? J Okla State Med Assoc. 2016;109:521–4. [PMC free article] [PubMed] [Google Scholar]
- 37.Haroon S, Das JK, Salam RA, et al. Breastfeeding promotion interventions and breastfeeding practices: A systematic review. BMC Public Health. 2013;13:S20. doi: 10.1186/1471-2458-13-S3-S20. https://doi.org/10.1186/1471-2458-13-S3-S20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Flint A, New K, Davies MW. Cup feeding versus other forms of supplemental enteral feeding for newborn infants unable to fully breastfeed. Cochrane Database Syst Rev. 2016:CD005092. doi: 10.1002/14651858.CD005092.pub2. [DOI] [PubMed] [Google Scholar]
- 39.Yesildal N, Aytar G, Kocabay K, et al. Breastfeeding practices in Duzce, Turkey. J Hum Lact. 2008;24:393–400. doi: 10.1177/0890334408322265. https://doi.org/10.1177/0890334408322265 [DOI] [PubMed] [Google Scholar]
- 40.Karaçam Z. Factors affecting exclusive breastfeeding of healthy babies aged zero to four months: A community-based study of Turkish women. J Clin Nurs. 2008;17:341–9. doi: 10.1111/j.1365-2702.2007.01936.x. [DOI] [PubMed] [Google Scholar]
- 41.Karaçam Z, Sen E, Amanak K. Effects of unplanned pregnancy on neonatal health in Turkey: A case–control study. Int J Nurs Pract. 2010;16:555–63. doi: 10.1111/j.1440-172X.2010.01881.x. https://doi.org/10.1111/j.1440-172X.2010.01881.x [DOI] [PubMed] [Google Scholar]
- 42.Cihan S, Karaçam Z. Erken doğum sonrası dönemde karşılaşılan emzirme problemleri ve problemlere ilişkin yapilan girişimler. I. Uluslararası Sağlık Bilimleri Kongresi; 29 Haziran-01 Temmuz 2017; p. 627. [Google Scholar]
- 43.Şencan İ, Tekin O, Tatli MM. Factors influencing breastfeeding duration: a survey in a Turkish population. Eur J Pediatr. 2013;172:1459–66. doi: 10.1007/s00431-013-2066-8. https://doi.org/10.1007/s00431-013-2066-8 [DOI] [PubMed] [Google Scholar]
- 44.Gönenç İM, Vural G. Epidural anestezi ile vajinal doğum yapan ve anestezisiz vajinal doğum yapan primipar annelerde ilk 24 saatte etkili emzirmenin değerlendirilmesi. Ankara Üniversitesi Tıp Fakültesi Mecmuası. 2015;68:81–6. https://doi.org/10.1501/Tipfak_0000000894 [Google Scholar]
- 45.Yılmazbaş P, Kural B, Uslu A, et al. Annelerin Gözünden ek besinlere başlama nedenleri ve annelerin mamalar hakkındaki düşünceleri. İst Tıp Fak Derg. 2015;78:76–82. https://doi.org/10.18017/iuitfd.13056441.2015.78/3.76-82. [Google Scholar]
- 46.Akyüz A, Kaya T, Şenel N. Annenin emzirme davranışının ve emzirmeyi etkileyen durumların belirlenmesi. TSK Koruyucu Hekimlik Bülteni. 2007;6:331–5. [Google Scholar]
- 47.Taş Arslan F, Yeniterzi E. Views of parents’ about taking human milk of premature infants. Perinatal Journal. 2013;21:77–84. https://doi.org/10.2399/prn.13.0212006 [Google Scholar]
- 48.Çatak B, Sütlü S, Kılınç SA, et al. Burdur ilinde bebeklerin emzirilme durumu ve beslenme örüntüsü. Pam Tıp Derg. 2012;5:115–22. [Google Scholar]
- 49.Eskibozkurt F. Yüksek lisans tezi. İstanbul: Marmara Üniversitesi Eğitim Bilimleri Enstitüsü; 2008. Yetişkin eğitimi açısından yeni doğum yapmış annelerin anne sütü ve emzirme ile ilgili bilgi düzeyinin tespiti; p. 198. [Google Scholar]
- 50.Bağlar D. Yüksek lisans tezi. İstanbul: Marmara Üniversitesi Sağlık Bilimleri Enstitüsü; 2008. Doğumdan sonra latch emzirme puanı ile ilk 6 aydaki emzirme durumu arasındaki ilişki; p. 106. [Google Scholar]
- 51.Ünalan PC, Akgün T, Çiftçili S, et al. Bebek dostu bir ana çocuk sağlığı merkezinden hizmet alan anneler neden bebeklerine erken ek gıda vermeye başlıyor? Türk Pediatri Arş. 2008;43:59–64. [Google Scholar]
- 52.Bülbül LG, Özcan AG, Hatipoğlu SS. Sağlam çocuk polikliniğinden izlenen iki yaş üzerindeki çocuklarda anne sütü ile beslenmeye etki eden faktörler. Şişli Etfal Hastanesi Tıp Bülteni. 2012;46:101–7. [Google Scholar]
- 53.Bolat F, Uslu S, Bolat G, et al. İlk altı ayda anne sütü ile beslenmeye etki eden faktörler. Çocuk Dergisi. 2011;11:5–13. https://doi.org/10.5222/j.child.2011.005 [Google Scholar]
- 54.İnce T, Kondolot M, Yalçın SS, et al. Annelerin emzirme danışmanlığı alma durumları. Çocuk Sağlığı ve Hastalıkları Dergisi. 2010;53:189–97. [Google Scholar]
- 55.Çiftci EK, Arikan D. The effect of training administered to working mothers on maternal anxiety levels and breastfeeding habits. J Clin Nurs. 2011;21:2170–8. doi: 10.1111/j.1365-2702.2011.03957.x. https://doi.org/10.1111/j.1365-2702.2011.03957.x [DOI] [PubMed] [Google Scholar]
- 56.Yilmaz G, Caylan N, Karacan CD, et al. Effect of cup feeding and bottle feeding on breastfeeding in late preterm infants: A randomized controlled study. J Hum Lact. 2014;30:174–9. doi: 10.1177/0890334413517940. https://doi.org/10.1177/0890334413517940 [DOI] [PubMed] [Google Scholar]
- 57.Kaya V, Aytekın A. Effects of pacifier use on transition to full breastfeeding and sucking skills in preterm infants: A randomised controlled trial. J Clin Nurs. 2016;26:2055–63. doi: 10.1111/jocn.13617. https://doi.org/10.1111/jocn.13617 [DOI] [PubMed] [Google Scholar]
- 58.Küçükoğlu S, Çelebioğlu A. Effect of natural-feeding education on successful exclusive breast-feeding and breast-feeding self-efficacy of low-birth-weight infants. Iran J Pediatr. 2014;l 24:49–56. [PMC free article] [PubMed] [Google Scholar]
- 59.Karadağ F. Yüksek lisans tezi. Afyonkarahisar: Afyon Kocatepe Üniversitesi Sağlık Bilimleri Enstitüsü; 2008. Gebelere lohusalık bakımı ve bebek bakımı konusunda verilen eğitimin etkinliğinin değerlendirilmesi; p. 115. [Google Scholar]
- 60.Büyükkayacı N. Doktora tezi. Kayseri: Erciyes Üniversitesi Sağlık Bilimleri Enstitüsü; 2010. Sezaryen sonrası erken taburcu olan kadınlara verilen evde bakım hizmetinin anne sağlığına ve öz bakım gücüne etkisi; p. 181. [Google Scholar]
- 61.Ekşioğlu A. Doktora tezi. İzmir: Ege Üniversitesi Sağlık Bilimleri Enstitüsü; 2016. Postpartum dönemde annelere verilen emzirme destek programının sadece anne sütü ile beslenme süresi üzerindeki etkisinin değerlendirilmesi; p. 216. [Google Scholar]
- 62.Demirci G. Yüksek lisans tezi. İstanbul: Marmara Üniversitesi Sağlık Bilimleri Enstitüsü; 2015. Doğum sonrası meme başı çatlaklarının oluşumunun önlenmesinde göğüs kalkanı kullanımının etkisi; p. 153. [Google Scholar]
- 63.Geçkil E, Şahin T, Tunçdemir A. Aile sağlığı elemanları tarafından uygulanan “emzirmeyi destekleme ve izleme programının” doğum sonrası ilk altı ayda annelerin etkili emzirme davranışları üzerine etkisi. TAF Prev Med Bull. 2012;11:273–80. [Google Scholar]
- 64.Onbaşı Ş, Duran R, Çiftdemir NA, et al. Doğum öncesi anne adaylarına verilen emzirme ve anne sütü eğitiminin emzirme davranışları üzerine etkisi. Türk Pediatri Arş. 2011;46:75–80. https://doi.org/10.4274/tpa.46.13 [Google Scholar]
- 65.Üstüner F, Bodur S. Bebeklerde aylık izlem ve hemşire tarafından annenin pekiştirici emzirme eğitimi ile ilk altı ay yalnızca anne sütü verme arasındaki ilişki. Genel Tıp Derg. 2009;19:25–32. [Google Scholar]
- 66.Aksu H, Küçük M, Düzgün G. The effect of postnatal breastfeeding education/support offered at home 3 days after delivery on breastfeeding duration and knowledge: A randomized trial. J Matern Fetal Neonatal Med. 2011;24:354–61. doi: 10.3109/14767058.2010.497569. https://doi.org/10.3109/14767058.2010.497569 [DOI] [PubMed] [Google Scholar]
- 67.Tetik BK, Artantaş AB, Güzeldemirci GB, et al. A case report of successful relactation. Turk J Pediatr. 2013;55:641–4. [PubMed] [Google Scholar]


