Abstract
Background:
While evidence suggests bidirectional associations between cigarette use and substance (alcohol or drug) use, how these associations are reflected across the range of currently available tobacco products is unknown. This study examined whether ever tobacco use predicted subsequent substance use, and ever substance use predicted subsequent tobacco use among 11,996 U.S. youth (12–17 years) from Waves 1 (2013–2014) and 2 (2014–2015) of the Population Assessment of Tobacco and Health (PATH) Study.
Methods:
Ever use of cigarettes, e-cigarettes, traditional cigars, cigarillos, filtered cigars, pipe, hookah, snus pouches, smokeless tobacco excluding snus pouches, dissolvable tobacco, bidis, kreteks, alcohol, marijuana, prescription drugs, and other drugs (cocaine and other stimulants, heroin, inhalants, solvents, and hallucinogens) was assessed at Wave 1 followed by past 12-month use assessments at Wave 2. The analyses included covariates (demographics, mental health, sensation seeking, prior use) to mitigate confounding.
Results:
Ever tobacco use predicted subsequent substance use. The magnitude of the associations was lowest for alcohol, higher for marijuana, and highest for other drugs. Ever substance use also predicted subsequent tobacco use. Specifically, ever alcohol, marijuana, and non-prescribed Ritalin/Adderall use predicted tobacco-product use. Ever e-cigarette and cigarette use exclusively and concurrently predicted subsequent any drug (including and excluding alcohol) use. E-cigarette and cigarette use associations in the opposite direction were also significant; the strongest associations were observed for exclusive cigarette use.
Conclusion:
Tobacco and substance use prevention efforts may benefit from comprehensive screening and interventions across tobacco products, alcohol, and drugs, and targeting risk factors shared across substances.
Keywords: Tobacco Products, Marijuana, Drugs, Youth, Bidirectional, Epidemiologic Studies
1. Introduction
Cigarette smoking is the leading preventable cause of morbidity and mortality in the United States (U.S.) (U.S. Department of Health and Human Services, 2014). Despite overall declines in conventional cigarette use in the past several decades, non-cigarette tobacco-product use among U.S. youth has been increasing (Arrazola et al., 2015; Johnston et al., 2017). Wave 1 (2013–2014) estimates from the Population Assessment of Tobacco and Health (PATH) Study show that, overall, 22% of youths had ever used tobacco (Kasza et al., 2017). The prevalence of ever use of cigarettes and e-cigarettes was 13% and 11%, respectively, followed by cigars (cigarillos were most prevalent at 6.5%) and hookah at 7.5% each. Similarly, although several national studies have shown declining trends in youth substance (alcohol or drugs) use (Johnston et al., 2017), lifetime prevalence of use of some substances remain as high or higher than tobacco-product use, including alcohol (28%), illicit drugs (25%), and marijuana (16%) (Center for Behavioral Health Statistics and Quality, 2016). Further, substance misuse and substance use disorders remain major public health problems that often begin in adolescence and have serious social, psychological, physical, and economic consequences (U.S. Department of Health and Human Services (HHS) and Office of the Surgeon General, 2016).
Tobacco use and substance use frequently co-occur (Richter et al., 2017), with the use of one often associated with the use of the other. Limited longitudinal evidence among youth suggests that tobacco use predicts marijuana use; and marijuana use increases the risk of tobacco use (Ramo et al., 2012). Only a few studies among high school students have examined associations of emerging non-cigarette tobacco product (e.g., e-cigarettes, cigars, and hookah) use with substance use (McCabe et al., 2017; Palamar et al., 2014; Schuster et al., 2013). These cross-sectional studies found that the use of alcohol, marijuana, and other drugs was associated with greater past 30-day (McCabe et al., 2017; Schuster et al., 2013) or past-year (Palamar et al., 2014) use of these tobacco products.
No study, to our knowledge, has included a comprehensive assessment of tobacco products and substances or tested bidirectional associations in a national study of U.S. youth. Therefore, using data from the PATH Study, an ongoing longitudinal study of U.S. adults and youth, the present study examined if (1) ever tobacco use predicted subsequent substance use, and (2) ever substance use predicted subsequent tobacco use across 12 tobacco products and alcohol, marijuana, prescription drugs, and other drugs (cocaine and other stimulants, heroin, inhalants, solvents, and hallucinogens).
2. Methods
2.1. Study Design and Participants
This paper reports data from youth (12–17 years) recruited at Wave 1 (2013–2014) and followed approximately 10- to 13-months later at Wave 2 (2014–2015) (average period of follow-up: 52 weeks). The time between the interviews varied as a function of respondents’ schedules, the time needed to contact respondents, and the grouping of multiple respondents within a household. Of the 13,651-youth recruited at Wave 1, analyses were restricted to 11,996 respondents (10,081 respondents ages 12–17-years and 1,915 respondents who turned 18 years at Wave 2) with data on both waves.
Recruitment employed a stratified address-based, area-probability sampling design at Wave 1. An in-person household screener was used at Wave 1 to select youth and adults from households for participation. The weighted response rate for the household screener was 54.0%. Among screened households, the weighted response rate for the Wave 1 youth interview was 78.4%. Conditional on Wave 1 participation, weighted response rates at Wave 2 among those between 12 and 17 years and those who turned 18 years were 88.4% and 85.7%, respectively. The Wave 1 weighting procedures adjusted for differential probabilities of selection, nonresponse, and then calibrated to achieve consistency with reliable independent population estimates for the U.S. civilian, noninstitutionalized population. At Wave 2, after adjusting for nonresponse, additional adjustments were made to protect against potential bias from attrition.
Nonresponse bias analyses for Waves 1 and 2 (available at http://doi.org/10.3886/ICPSR36231) evaluated the extent to which Wave 1 estimates might depart from population parameters and the representativeness of the Wave 2 responding sample. Many characteristics of Wave 1 youth respondents were consistent with the 1-year estimates from the 2013 American Community Survey (ACS), with the exception of ethnicity. When the full sample estimates were adjusted for nonresponse among youth, they more closely approximated the 2013 ACS estimates. However, ever cigarette use estimates for youth from the PATH Study remained lower than those found by national school-based studies (Kasza et al., 2017). Analyses comparing Wave 2 respondents to non-respondents found no differences based on Wave 1 ever substance use (Dai et al., 2018). The Wave 2 nonresponse bias analysis showed that Wave 1 ever tobacco users were less likely to respond to the Wave 2 youth interview than never users (86.6% vs. 89%). Wave 1 ever tobacco use estimates were lower for Wave 2 youth respondents compared to non-respondents prior to incorporating weight adjustments. However, the PATH Study weights corrected for potential nonresponse bias in tobacco-use outcomes analyzed.
After obtaining consent from parents and emancipated youth and assent from youth, data were collected using Audio-Computer Assisted Self-Interviews administered in English or Spanish. Further information on the PATH Study design and methods has been published elsewhere (Hyland et al., 2017). Details on interview procedures, questionnaires, sampling, and weighting, and information on accessing the data are available at https://doi.org/10.3886/Series606. The PATH Study was conducted by Westat and approved by the Westat Institutional Review Board.
2.2. Measures
2.2.1. Tobacco Use.
Participants self-reported ever use (including one or two puffs/times) of the following tobacco products at Wave 1: cigarettes, e-cigarettes, traditional cigars, cigarillos, filtered cigars, pipe, hookah, smokeless tobacco (i.e., loose snus, moist snuff, dip, spit, or chewing tobacco), snus pouches, kreteks, bidis, and dissolvable tobacco. The questionnaire included brief descriptions and pictures of each product (except cigarettes). Additional questions were asked of cigar users to determine cigar type.
At Wave 2, participants were asked about past 12-month use of the same tobacco products. Those who reported using a tobacco product in the past 12 months were defined as past 12-month users of that respective product. As past 12-month bidi and kretek use was not assessed in the adult interview, these data were not available for youth who turned 18 years at Wave 2. Therefore, past 12-month use variables were created for all tobacco products except bidis and kreteks.
Additional summary variables for both waves were created as follows: ‘any tobacco use’ defined as use of any tobacco product (except bidis and kreteks in the substance use predicting tobacco use analyses), ‘any cigar use’ defined as use of traditional cigars, cigarillos, or filtered cigars, and ‘any smokeless tobacco’ defined as use of snus pouches, smokeless tobacco excluding snus pouches, or dissolvable tobacco.
2.2.2. Substance Use.
Participants self-reported ever use of the following substances at Wave 1: alcohol, marijuana (including blunts), non-prescribed use of Ritalin® or Adderall®, painkillers, sedatives, or tranquilizers, and cocaine or crack, other stimulants methamphetamine or speed), heroin, inhalants, solvents, and hallucinogens, with items adapted from the National Epidemiologic Survey on Alcohol and Related Conditions (National Institutes of Health (NIH), 2004–2005) and the National Health and Nutrition Examination Survey (Centers for Disease Control and Prevention (CDC), 2011–2012). Past 12-month use of the same substances was assessed at Wave 2.
In both waves, ‘other drug use’ was defined as the use of cocaine or crack, other stimulants methamphetamine or speed), heroin, inhalants, solvents, or hallucinogens. In addition, ‘alcohol or any drug use’ and ‘any drug excluding alcohol’ were defined as the use of any of these substances.
2.2.3. Covariates.
Information was collected on demographics including age, gender, and race/ethnicity. Missing data on age and gender were imputed as described in the PATH Study Restricted Use Files User Guide (United States Department of Health and Human Services et al.). Sensation seeking, a risk factor for substance use (Hoyle et al., 2002), was assessed via three modified items from the Brief Sensation Seeking Scale: 1) “I like to do frightening things”, 2) “I like new and exciting experiences even if I have to break the rules”, and 3) “I prefer friends who are exciting and unpredictable”. Response options for each item (strongly agree, agree, neither agree nor disagree, disagree and strongly disagree) were summed to create overall (range: 0–12) and mean scores (Conway et al., 2018). The scale was found to be internally consistent among youth in the PATH Study (Cronbach’s α=0.76).
Past-year mental health problems were assessed at Wave 1 via internalizing and externalizing problem subscales of the Global Appraisal of Individual Needs - Short Screener (GAIN-SS) (Dennis et al., 2006), modified for the PATH Study. These subscales identify individuals at risk for mental health disorders using a continuous measure of severity, and have been previously validated (Garner et al., 2013) and recommended for use in epidemiological samples by the PhenX Toolkit (Hamilton et al., 2011). The number of responses endorsed in the past year was summed for both subscales (complete data for subscale components were required). Based on the number of symptoms endorsed, mental health problems were categorized into no/low (0–2 symptoms), moderate (3–7 symptoms), or high (8–11 symptoms) severity (Conway et al., 2018).
2.3. Statistical Analysis
We examined distributions of past 12-month substance use at Wave 2 by ever tobacco use at Wave 1 and past 12-month tobacco use at Wave 2 by ever substance use at Wave 1. For the summary variables, complete data were required to categorize participants as non-users but not required to categorize participants as users.
Multivariable logistic regression models were used to evaluate the associations between tobacco use and substance use. We adjusted estimates for demographic and personality factors associated with multiple problem behaviors (Stone et al., 2012). These included possible confounders such as age, gender, race/ethnicity, sensation seeking, past-year mental health problems, and Wave 1 ever tobacco or substance use in the models predicting Wave 2 tobacco use and substance use, respectively (Supplementary tables 1 and 2)1. Use of other tobacco products and substances were included as covariates to control for confounding by dual or poly-use.
As approximately 40% of U.S. youth tobacco users use two or more tobacco products, with cigarettes plus e-cigarettes being the most common combination (Kasza et al., 2017), we examined bidirectional associations between a four-category variable for e-cigarette and cigarette use (none, exclusive e-cigarette use, exclusive cigarette use, and e-cigarette and cigarette use) and substance use. These models excluded other tobacco products users at Waves 1 and 2, respectively. Additionally, as Wave 1 analyses showed significant gender-by-tobacco interactions with substance use (Conway et al., 2018), gender was examined as a potential moderator of the bidirectional tobacco use and substance use associations.
Estimates were weighted to represent the U.S. youth population; variances and confidence intervals (CIs) were estimated using the balanced repeated replication (BRR) method (McCarthy, 1969) with Fay’s adjustment set to 0.3 to increase estimate stability (Judkins, 1990). Adjusted odds ratios (AORs) and 95% CIs were calculated for all regression analyses. Two-sided p-values of <.05 were considered statistically significant. Estimates based on fewer than 50 observations in the denominator or the relative standard error greater than 0.30 were suppressed (Klein et al., 2002). All analyses were conducted using SAS Survey Procedures, version 9.4 (SAS Institute Inc., Cary, NC).
3. Results
Demographic characteristics of the study population have been previously published (Conway et al., 2018; Kasza et al., 2017). At Wave 2, an estimated four in ten (41.4%) U.S. youth used alcohol or any drugs in the past 12 months, with alcohol (33.2%) and marijuana (16.6%) being the most prevalent (Table 1, total row). Non-prescribed painkillers or sedatives were used in the past 12 months by 6.9% of youth. The past 12-month substance use estimates at Wave 2 were higher among Wave 1 never compared to ever substance users, except for marijuana. About one-quarter of youth used tobacco products during the past 12-months (Table 2, total row). Ecigarettes (14.4%), cigarettes (12.9%), hookah (9.8%), and any cigars (9.3%) were the most commonly used tobacco products in the past 12 months. Whereas estimates of past 12-month use of cigarettes, cigarillos, and smokeless tobacco excluding snus pouches at Wave 2 were higher among Wave 1 ever compared to never tobacco users, Wave 2 estimates of use of e-cigarettes, traditional cigars, filtered cigars, pipes, hookah, and snus pouches were higher among Wave 1 never compared to ever tobacco users.
Table 1.
The Association between Wave 1 Ever Tobacco Use and Wave 2 Past 12-month Substance Use among 11,996 Wave 1 Youth (12–17 years) in the PATH Study.
| Wave 2 Past 12-month Substance Use |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alcohol or Any Drug |
Any Drug (excluding alcohol) |
Alcohol |
Marijuanad |
|||||||||||||||
| na | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | CIc | %b | SEb | |
| Among Wave 1 Never Substance Usersi | 18.9 | 0.5 | - | 10.7 | 0.4 | - | 17.7 | 0.5 | - | 7.6 | 0.3 | |||||||
| Among Wave 1 Ever Substance Usersi | 22.4 | 0.5 | - | 11.5 | 0.3 | - | 15.5 | 0.5 | - | 9.0 | 0.3 | |||||||
| Total | 41.4 | 0.7 | - | 22.2 | 0.5 | - | 33.2 | 0.7 | - | 16.6 | 0.4 | |||||||
| Wave 1 Ever Tobacco Use | ||||||||||||||||||
| Cigarettes | ||||||||||||||||||
| N | 9377 | 36.6 | 0.8 | referent | 17.0 | 0.5 | referent | 29.3 | 0.7 | referent | 11.2 | 0.4 | ||||||
| Y | 1474 | 73.7 | 1.4 | 1.3 | 1.1 | 1.6 | 56.4 | 1.7 | 1.9 | 1.6 | 2.2 | 59.5 | 1.3 | 1.1 | 0.9 | 1.3 | 51.9 | 1.8 |
| E-cigarettes | ||||||||||||||||||
| N | 9676 | 37.3 | 0.7 | referent | 18.1 | 0.5 | referent | 30.0 | 0.8 | referent | 12.4 | 0.4 | ||||||
| Y | 1163 | 77.0 | 1.5 | 1.7h | 1.4 | 2.1 | 57.5 | 1.7 | 1.8 | 1.5 | 2.1 | 62.0 | 1.5 | 1.3 | 1.1 | 1.5 | 52.8 | 1.8 |
| Any cigar | ||||||||||||||||||
| N | 9839 | 38.4 | 0.7 | referent | 19.0 | 0.5 | referent | 30.8 | 0.7 | referent | 13.2 | 0.4 | ||||||
| Y | 802 | 79.8 | 1.7 | 1.5 | 1.2 | 1.9 | 62.5 | 2.2 | 1.8 | 1.4 | 2.2 | 65.0 | 1.9 | 1.2 | 1.0 | 1.5 | 59.1 | 2.2 |
| Traditional cigars | ||||||||||||||||||
| N | 10478 | 40.7 | 0.7 | referent | 21.4 | 0.5 | referent | 32.8 | 0.7 | referent | 15.8 | 0.4 | ||||||
| Y | 236 | 79.9 | 2.9 | 1.4 | 1.0 | 2.0 | 65.1 | 3.6 | 1.9 | 1.3 | 2.6 | 62.3 | 3.0 | 1.0 | 0.7 | 1.3 | 60.6 | 3.8 |
| Cigarillos | ||||||||||||||||||
| N | 9973 | 38.9 | 0.7 | referent | 19.4 | 0.5 | referent | 31.3 | 0.7 | referent | 13.6 | 0.4 | ||||||
| Y | 697 | 79.7 | 1.8 | 1.5 | 1.2 | 1.9 | 63.7 | 2.2 | 1.9 | 1.5 | 2.3 | 64.1 | 1.9 | 1.2 | 0.9 | 1.4 | 60.6 | 2.3 |
| Filtered cigars | ||||||||||||||||||
| N | 10413 | 40.6 | 0.7 | referent | 21.3 | 0.5 | referent | 32.6 | 0.7 | referent | 15.6 | 0.4 | ||||||
| Y | 257 | 82.8 | 2.5 | 1.3 | 0.9 | 1.9 | 67.0 | 3.3 | 1.7 | 1.2 | 2.3 | 69.1 | 3.2 | 1.1 | 0.8 | 1.5 | 63.7 | 3.3 |
| Pipe | ||||||||||||||||||
| N | 10636 | 40.9 | 0.7 | referent | 21.7 | 0.5 | referent | 32.9 | 0.7 | referent | 16.1 | 0.5 | ||||||
| Y | 212 | 79.7 | 3.3 | 1.3 | 0.9 | 2.1 | 62.1 | 3.9 | 1.5 | 1.1 | 2.1 | 61.1 | 3.9 | 0.9 | 0.6 | 1.4 | 56.7 | 3.9 |
| Hookah | ||||||||||||||||||
| N | 10040 | 38.6 | 0.7 | referent | 19.2 | 0.5 | referent | 30.8 | 0.7 | referent | 13.5 | 0.4 | ||||||
| Y | 807 | 79.3 | 1.6 | 1.7 | 1.4 | 2.1 | 61.0 | 2.1 | 1.9 | 1.6 | 2.3 | 65.7 | 1.8 | 1.4 | 1.2 | 1.7 | 57.3 | 2.1 |
| Any smokeless tobaccog | ||||||||||||||||||
| N | 10247 | 40.1 | 0.7 | referent | 20.9 | 0.5 | referent | 32.1 | 0.7 | referent | 15.2 | 0.5 | ||||||
| Y | 508 | 71.7 | 2.5 | 1.1h | 0.8 | 1.3 | 51.7 | 2.4 | 1.2 | 1.0 | 1.5 | 60.0 | 2.6 | 1.0 | 0.8 | 1.3 | 48.1 | 2.5 |
| Smokeless tobacco excluding snus pouches | ||||||||||||||||||
| N | 10305 | 40.3 | 0.7 | referent | 21.0 | 0.5 | referent | 32.2 | 0.7 | referent | 15.3 | 0.5 | ||||||
| Y | 456 | 71.5 | 2.6 | 1.0 | 0.8 | 1.3 | 51.9 | 2.5 | 1.2 | 1.0 | 1.5 | 60.4 | 2.5 | 1.0 | 0.8 | 1.3 | 48.2 | 2.6 |
| Snus pouches | ||||||||||||||||||
| N | 10578 | 41.0 | 0.7 | referent | 21.8 | 0.5 | referent | 32.9 | 0.7 | referent | 16.1 | 0.5 | ||||||
| Y | 181 | 77.1 | 3.7 | 1.3 | 0.8 | 1.8 | 57.5 | 4.3 | 1.4 | 1.0 | 1.9 | 64.3 | 4.2 | 1.2 | 0.8 | 1.6 | 54.4 | 4.5 |
| Wave 2 Past 12-month Substance Use |
||||||||||||||||||
| Marijuanad |
Ritalin/Adderalle |
Painkillers/Sedativese |
Other Drugs f |
|||||||||||||||
| AORb | 95% | CIc | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | CIc | |
| Among Wave 1 Never Substance Usersi | - | 1.7 | 0.2 | - | 5.0 | 0.2 | - | 1.5 | 0.1 | - | ||||||||
| Among Wave 1 Ever Substance Usersi | - | 0.6 | 0.1 | - | 1.9 | 0.1 | - | 0.5 | 0.1 | - | ||||||||
| Total | - | 2.3 | 0.2 | - | 6.9 | 0.3 | - | 2.0 | 0.2 | - | ||||||||
| Wave 1 Ever Tobacco Use | ||||||||||||||||||
| Cigarettes | ||||||||||||||||||
| N | referent | 1.5 | 0.2 | referent | 6.3 | 0.3 | referent | 1.2 | 0.1 | referent | ||||||||
| Y | 2.1 | 1.7 | 2.5 | 8.0 | 0.8 | 1.5 | 1.1 | 2.2 | 10.6 | 1.0 | 1.2h | 0.9 | 1.5 | 7.6 | 0.8 | 2.1 | 1.5 | 2.9 |
| E-cigarettes | ||||||||||||||||||
| N | referent | 1.3 | 0.1 | referent | 6.3 | 0.3 | referent | 1.2 | 0.1 | referent | ||||||||
| Y | 1.9 | 1.6 | 2.2 | 10.5 | 1.1 | 3.2 | 2.3 | 4.4 | 11.4 | 1.2 | 1.3h | 1.0 | 1.8 | 8.6 | 1.0 | 2.5 | 1.7 | 3.5 |
| Any cigar | ||||||||||||||||||
| N | referent | 1.8 | 0.2 | referent | 6.6 | 0.3 | referent | 1.3 | 0.1 | referent | ||||||||
| Y | 1.9 | 1.5 | 2.4 | 8.6 | 1.1 | 1.3 | 0.8 | 1.8 | 10.5 | 1.3 | 1.1h | 0.8 | 1.5 | 10.7 | 1.3 | 3.0 | 2.0 | 4.6 |
| Traditional cigars | ||||||||||||||||||
| N | referent | 2.2 | 0.2 | referent | 6.7 | 0.3 | referent | 1.7 | 0.2 | referent | ||||||||
| Y | 1.8 | 1.3 | 2.5 | 7.7 | 1.9 | 0.9 | 0.5 | 1.8 | 11.9 | 2.1 | 1.4h | 0.9 | 2.1 | 13.7 | 2.5 | 2.5 | 1.4 | 4.4 |
| Cigarillos | ||||||||||||||||||
| N | referent | 1.9 | 0.2 | referent | 6.6 | 0.3 | referent | 1.4 | 0.1 | referent | ||||||||
| Y | 2.0 | 1.6 | 2.4 | 8.9 | 1.1 | 1.3 | 0.9 | 1.8 | 10.7 | 1.4 | 1.1h | 0.8 | 1.6 | 10.8 | 1.4 | 2.7 | 1.8 | 4.0 |
| Filtered cigars | ||||||||||||||||||
| N | referent | 2.1 | 0.2 | referent | 6.7 | 0.3 | referent | 1.6 | 0.1 | referent | ||||||||
| Y | 1.6 | 1.2 | 2.2 | 12.1 | 2.2 | 1.6 | 1.0 | 2.6 | 13.2 | 2.2 | 1.4 | 0.9 | 2.2 | 17.4 | 3.2 | 3.7 | 2.3 | 6.1 |
| Pipe | ||||||||||||||||||
| N | referent | 2.2 | 0.2 | referent | 6.8 | 0.3 | referent | 1.8 | 0.2 | referent | ||||||||
| Y | 1.4 | 1.0 | 1.9 | 11.1 | 2.3 | 1.4 | 0.9 | 2.3 | 11.8 | 2.5 | 1.3 | 0.8 | 1.9 | 12.1 | 2.6 | 1.9 | 1.2 | 3.2 |
| Hookah | ||||||||||||||||||
| N | referent | 1.7 | 0.2 | referent | 6.5 | 0.3 | referent | 1.4 | 0.1 | referent | ||||||||
| Y | 2.1 | 1.7 | 2.5 | 10.6 | 1.2 | 2.3 | 1.6 | 3.5 | 11.2 | 1.2 | 1.2h | 0.9 | 1.6 | 9.4 | 1.3 | 2.6 | 1.7 | 3.7 |
| Any smokeless tobaccog | ||||||||||||||||||
| N | referent | 2.0 | 0.2 | referent | 6.6 | 0.3 | referent | 1.7 | 0.2 | referent | ||||||||
| Y | 1.2 | 1.0 | 1.5 | 8.5 | 1.4 | 1.3 | 0.8 | 2.0 | 12.5 | 1.6 | 1.7 | 1.2 | 2.4 | 8.9 | 1.3 | 1.6 | 1.0 | 2.4 |
| Smokeless tobacco excluding snus pouches | ||||||||||||||||||
| N | referent | 2.0 | 0.2 | referent | 6.6 | 0.3 | referent | 1.7 | 0.2 | referent | ||||||||
| Y | 1.2 | 1.0 | 1.5 | 8.8 | 1.5 | 1.3 | 0.8 | 2.1 | 13.1 | 1.7 | 1.8 | 1.3 | 2.5 | 8.8 | 1.4 | 1.5 | 0.9 | 2.4 |
| Snus pouches | ||||||||||||||||||
| N | referent | 2.2 | 0.2 | referent | 6.8 | 0.3 | referent | 1.8 | 0.2 | referent | ||||||||
| Y | 1.4 | 0.9 | 2.0 | 7.9 | 2.2 | 1.0 | 0.5 | 1.9 | 13.4 | 2.8 | 1.8 | 1.1 | 2.9 | 12.1 | 2.7 | 2.0 | 1.1 | 3.8 |
n represents unweighted sample sizes.
Percents (%) and standard errors (SEs) represent weighted estimates.
Adjusted odds ratios (AORs) and 95% confidence intervals (CIs) from multivariable logistic regression models adjusting for age, gender, race/ethnicity, sensation seeking, past-year mental health problems at Wave 1, ever substance use at Wave 1, and other tobacco product use at Wave 1.
Includes past 12-month use of cigars as blunts.
Refers to prescription drugs that were not prescribed for the participant or taken only for the experience or feeling they caused.
Refers to cocaine or crack, other stimulants (i.e. methamphetamine or speed), or heroin, inhalants, solvents, or hallucinogens.
Refers to snus pouches, smokeless tobacco excluding snus pouches, or dissolvable tobacco.
Indicates gender interaction is significant at p < 0.05.
Indicates Wave 2 past-12 month substance use among Wave 1 never and ever users of the same type of substance.
Unreliable estimates (for dissolvable tobacco, bidis, and kreteks) were suppressed based on relative standard error greater than 0.30 or denominator sample size less than 50.
Models were restricted to observations with non-missing data; unweighted sample sizes ranged from 10,448 (for the any cigar and alcohol or any drug model) to 10,535 (for the pipe and non-prescribed painkiller/sedative model).
Statistically significant associations at p < 0.05 indicated in bold text.
Table 2.
The Association between Wave 1 Ever Substance Use and Wave 2 Past 12-month Tobacco Use among 11,996 Wave 1 Youth (12–17 years) in the PATH Study.
| Wave 2 Past 12-month Tobacco Use | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any tobaccod |
Cigarettes |
E-cigarettes |
Any cigar |
|||||||||||||||||||
| na | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | |||
| Among Wave 1 Never Tobacco Usersj | 9.4 | 0.3 | - | 4.1 | 0.2 | - | 8.1 | 0.4 | - | 4.2 | 0.2 | - | ||||||||||
| Among Wave 1 Ever Tobacco Usersj | 15.9 | 0.3 | - | 8.8 | 0.3 | - | 6.3 | 0.3 | - | 5.1 | 0.2 | - | ||||||||||
| Total | 25.4 | 0.4 | - | 12.9 | 0.3 | - | 14.4 | 0.5 | - | 9.3 | 0.3 | - | ||||||||||
| Wave 1 Ever Substance Use | ||||||||||||||||||||||
| Any Drug (excluding alcohol) | ||||||||||||||||||||||
| N | 8408 | 16.5 | 0.5 | referent | 6.7 | 0.3 | referent | CO CO |
0.5 | referent | 4.7 | 0.3 | referent | |||||||||
| Y | 2172 | 59.5 | 1.0 | 1.9 | 1.6 | 2.3 | 37.2 | 1.0 | 2.0 | 1.7 | 2.3 | 37.0 | 1.3 | 1.9i | 1.6 | 2.2 | 27.2 | 1.1 | 1.8 | 1.4 | ||
| Alcohol | ||||||||||||||||||||||
| N | 8253 | 15.1 | 0.5 | referent | 6.4 | 0.3 | referent | 8.2 | 0.4 | referent | 4.0 | 0.3 | referent | |||||||||
| Y | 2406 | 59.1 | 1.0 | 2.0 | 1.7 | 2.3 | 34.8 | 1.1 | 1.6 | 1.2 | 1.9 | 35.6 | 1.3 | 1.5 | 1.3 | 1.8 | 27.0 | 1.0 | 2.3 | 1.8 | ||
| Marijuanaf | ||||||||||||||||||||||
| N | 9172 | 17.2 | 0.5 | referent | 6.9 | 0.3 | referent | 9.3 | 0.5 | referent | 4.8 | 0.2 | referent | |||||||||
| Y | 1500 | 74.5 | 1.1 | 2.4 | 2.0 | 2.9 | 49.9 | 1.3 | 2.5 | 2.1 | 3.0 | 46.7 | 1.5 | 2.0i | 1.6 | 2.4 | 36.7 | 1.3 | 2.1 | 1.8 | ||
| Ritalin/Adderallg | ||||||||||||||||||||||
| N | 10421 | 24.1 | 0.5 | referent | 11.9 | 0.3 | referent | 13.5 | 0.5 | referent | 8.4 | 0.3 | referent | |||||||||
| Y | 255 | 77.8 | 2.8 | 2.7 | 1.8 | 4.0 | 53.8 | 3.4 | 1.8 | 1.3 | 2.6 | 54.8 | 3.7 | 1.9 | 1.4 | 2.6 | 45.8 | 3.3 | 2.1 | 1.6 | ||
| Painkillers/Sedativesg | ||||||||||||||||||||||
| N | 9755 | 23.9 | 0.5 | referent | 12.0 | 0.4 | referent | 13.3 | 0.5 | referent | 8.6 | 0.3 | referent | |||||||||
| Y | 870 | 42.6 | 1.6 | 1.4 | 1.1 | 1.7 | 24.2 | 1.5 | 1.2 | 1.0 | 1.5 | 28.1 | 1.7 | 1.5 | 1.2 | 1.9 | 17.9 | 1.4 | 1.3 | 1.0 | ||
| Other drugsh | ||||||||||||||||||||||
| N | 10488 | 24.5 | 0.5 | referent | 12.1 | 0.3 | referent | 13.8 | 0.5 | referent | 8.6 | 0.3 | referent | |||||||||
| Y | 172 | 82.5 | 3.0 | 1.5 | 0.9 | 2.6 | 70.4 | 3.9 | 2.6 | 1.7 | 4.1 | 60.7 | 3.8 | 1.6 | 1.2 | 2.2 | 52.9 | 4.1 | 2.1 | 1.4 | ||
| Wave 2 Past 12-month Tobacco Use | ||||||||||||||||||||||
| Any cigar |
Traditional cigars |
Cigarillos |
Filtered cigars |
Pipe |
||||||||||||||||||
| CIc | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | CIc | ||
| Among Wave 1 Never Tobacco Usersj | 2.8 | 0.2 | - | 3.3 | 0.2 | - | 1.7 | 0.1 | - | 0.8 | 0.1 | - | ||||||||||
| Among Wave 1 Ever Tobacco Usersj | 1.6 | 0.1 | - | 4.0 | 0.2 | - | 1.5 | 0.1 | - | 0.7 | 0.1 | - | ||||||||||
| Total | 4.4 | 0.2 | - | 7.3 | 0.3 | - | 3.2 | 0.2 | - | 1.5 | 0.1 | - | ||||||||||
| Wave 1 Ever Substance Use | ||||||||||||||||||||||
| Any Drug (excluding alcohol) | ||||||||||||||||||||||
| N | 2.2 | 0.2 | referent | 3.6 | 0.2 | referent | 1.3 | 0.1 | referent | 0.7 | 0.1 | referent | ||||||||||
| Y | 2.2 | 12.3 | 0.8 | 1.5 | 1.1 | 2.0 | 21.4 | 1.0 | 1.8 | 1.4 | 2.2 | 10.5 | 0.7 | 1.9 | 1.4 | 2.5 | 4.3 | 0.4 | 1.4 | 0.9 | 2.1 | |
| Alcohol | ||||||||||||||||||||||
| N | 1.7 | 0.2 | referent | 3.2 | 0.3 | referent | 1.2 | 0.2 | referent | 0.5 | 0.1 | referent | ||||||||||
| Y | 2.9 | 13.0 | 0.7 | 2.4 | 1.8 | 3.2 | 20.6 | 0.9 | 1.9 | 1.5 | 2.4 | 9.8 | 0.8 | 1.5 | 1.0 | 2.3 | 4.6 | 0.5 | 2.5 | 1.5 | 4.1 | |
| Marijuanaf | ||||||||||||||||||||||
| N | 2.2 | 0.2 | referent | 3.6 | 0.2 | referent | 1.4 | 0.1 | referent | 0.7 | 0.1 | referent | ||||||||||
| Y | 2.6 | 16.7 | 1.1 | 1.7 | 1.2 | 2.2 | 29.2 | 1.2 | 2.2 | 1.8 | 2.7 | 14.2 | 1.0 | 1.9 | 1.4 | 2.6 | 6.1 | 0.6 | 1.7 | 1.1 | 2.7 | |
| Ritalin/Adderallg | ||||||||||||||||||||||
| N | 3.7 | 0.2 | referent | 6.5 | 0.3 | referent | 2.8 | 0.2 | referent | 1.3 | 0.1 | referent | ||||||||||
| Y | 2.9 | 25.0 | 3.2 | 2.1 | 1.4 | 3.1 | 33.3 | 3.4 | 1.6 | 1.2 | 2.2 | 18.9 | 3.0 | 1.7 | 1.1 | 2.6 | 8.4 | 2.0 | 1.7 | 0.9 | 3.1 | |
| Painkillers/Sedativesg | ||||||||||||||||||||||
| N | 3.9 | 0.2 | referent | 6.6 | 0.3 | referent | 2.8 | 0.2 | referent | 1.3 | 0.1 | referent | ||||||||||
| Y | 1.6 | 8.4 | 1.0 | 1.2 | 0.9 | 1.6 | 13.9 | 1.4 | 1.2 | 0.9 | 1.6 | 8.2 | 1.0 | 1.7 | 1.2 | 2.2 | 3.8 | 0.7 | 1.7i | 1.1 | 2.7 | |
| Other drugsh | ||||||||||||||||||||||
| N | 3.9 | 0.2 | referent | 6.7 | 0.3 | referent | 2.8 | 0.2 | referent | 1.3 | 0.1 | referent | ||||||||||
| Y | 3.2 | 26.1 | 3.9 | 1.6 | 1.0 | 2.6 | 40.0 | 4.5 | 1.7 | 1.1 | 2.7 | 28.2 | 3.5 | 2.5 | 1.7 | 3.7 | 15.0 | 3.0 | 2.9 | 1.6 | 5.1 | |
| Wave 2 Past 12-month Tobacco Use | ||||||||||||||||||||||
| Hookah |
Any smokeless tobaccoe |
Smokeless tobacco excluding snus pouches |
Snus pouches |
|||||||||||||||||||
| %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95% | CIc | %b | SEb | AORc | 95%c | CIc | %b | SEb | AORc | 95% | CIc | |||
| Among Wave 1 Never Tobacco Usersj | 5.0 | 0.2 | - | 2.0 | 0.2 | - | 1.7 | 0.1 | - | 1.3 | 0.1 | - | ||||||||||
| Among Wave 1 Ever Tobacco Usersj | 4.8 | 0.3 | - | 2.6 | 0.2 | - | 2.2 | 0.2 | - | 0.8 | 0.1 | - | ||||||||||
| Total | 9.8 | 0.3 | - | 4.6 | 0.3 | - | 3.9 | 0.2 | - | 2.1 | 0.2 | - | ||||||||||
| Wave 1 Ever Substance Use | ||||||||||||||||||||||
| Any Drug (excluding alcohol) | ||||||||||||||||||||||
| N | 5.5 | 0.3 | referent | 3.1 | 0.2 | referent | 2.7 | 0.2 | referent | 1.3 | 0.1 | referent | ||||||||||
| Y | 26.8 | 1.0 | 1.4 | 1.2 | 1.7 | 10.2 | 0.8 | 1.0 | 0.7 | 1.3 | 8.6 | 0.7 | 0.9 | 0.7 | 1.2 | 5.2 | 0.6 | 1.1 | 0.7 | 1.5 | ||
| Alcohol | ||||||||||||||||||||||
| N | 4.6 | 0.3 | referent | 2.6 | 0.2 | referent | 2.2 | 0.2 | referent | 1.0 | 0.1 | referent | ||||||||||
| Y | 27.3 | 0.9 | 2.0 | 1.7 | 2.4 | 11.1 | 0.9 | 1.5 | 1.1 | 2.0 | 9.7 | 0.8 | 1.5 | 1.1 | 2.0 | 5.8 | 0.6 | 1.7 | 1.2 | 2.4 | ||
| Marijuanaf | ||||||||||||||||||||||
| N | 5.7 | 0.3 | referent | 3.3 | 0.2 | referent | 2.8 | 0.2 | referent | 1.3 | 0.1 | referent | ||||||||||
| Y | 35.6 | 1.3 | 1.7 | 1.4 | 2.1 | 12.7 | 1.0 | 0.9 | 0.6 | 1.2 | 10.7 | 0.9 | 0.8 | 0.6 | 1.1 | 7.0 | 0.8 | 1.1 | 0.7 | 1.7 | ||
| Ritalin/Adderallg | ||||||||||||||||||||||
| N | 9.1 | 0.3 | referent | 4.1 | 0.3 | referent | 3.6 | 0.2 | referent | 1.8 | 0.1 | referent | ||||||||||
| Y | 41.5 | 3.3 | 1.8 | 1.3 | 2.5 | 22.2 | 3.1 | 1.9 | 1.3 | 2.8 | 17.9 | 2.8 | 1.6 | 1.1 | 2.4 | 13.3 | 2.4 | 2.3 | 1.4 | 3.7 | ||
| Painkillers/Sedativesg | ||||||||||||||||||||||
| N | 9.1 | 0.3 | referent | 4.3 | 0.3 | referent | 3.7 | 0.2 | referent | 2.0 | 0.2 | referent | ||||||||||
| Y | 19.0 | 1.4 | 1.2 | 1.0 1.6 | 8.3 | 1.1 | 1.3 | 0.9 | 1.9 | 7.0 | 1.0 | 1.3 | 0.9 | 1.9 | 3.9 | 0.8 | 1.2 | 0.7 | 2.0 | |||
| Other drugsh | ||||||||||||||||||||||
| N | 9.4 | 0.3 | referent | 4.4 | 0.3 | referent | 3.8 | 0.2 | referent | 2.0 | 0.2 | referent | ||||||||||
| Y | 41.9 | 4.2 | 1.3 | 0.9 | 1.9 | 17.9 | 3.2 | 0.9 | 0.6 | 1.6 | 16.0 | 3.3 | 1.0 | 0.6 | 1.8 | 9.8 | 2.7 | 1.0 | 0.5 | 2.0 | ||
n represents unweighted sample sizes.
Percents (%) and standard errors (SEs) represent weighted estimates.
Adjusted odds ratios (AORs) and 95% confidence intervals (CIs) from multivariable logistic regression models adjusting for age, gender, race/ethnicity, sensation seeking, past-year mental health problems at Wave 1, ever tobacco use at Wave 1, and other substance at Wave 1.
Refers to cigarettes, e-cigarettes, traditional cigars, cigarillos, filtered cigars, pipe, hookah, snus pouches, smokeless tobacco excluding snus pouches, or dissolvable tobacco.
Refers to snus pouches, smokeless tobacco excluding snus pouches, or dissolvable tobacco.
Includes past 12-month use of cigars as blunts.
Refers to prescription drugs that were not prescribed for the participant or taken only for the experience or feeling they caused.
Refers to cocaine or crack, other stimulants (i.e. methamphetamine or speed), or heroin, inhalants, solvents, or hallucinogens.
Indicates gender interaction is significant at p < 0.05.
Indicates Wave 2 past-12 month tobacco use among Wave 1 never and ever users of the same type of tobacco product.
Unreliable estimates (for dissolvable tobacco) were suppressed based on relative standard error greater than 0.30 or denominator sample size less than 50.
Models were restricted to observations with non-missing data; unweighted sample sizes ranged from 10,365 (for the any drug and any tobacco model) to 10,562 (for the non-prescribed Ritalin/Adderall and cigarettes model).
Statistically significant associations at p < .05 indicated in bold text.
3.1. Tobacco Use Predicting Substance Use
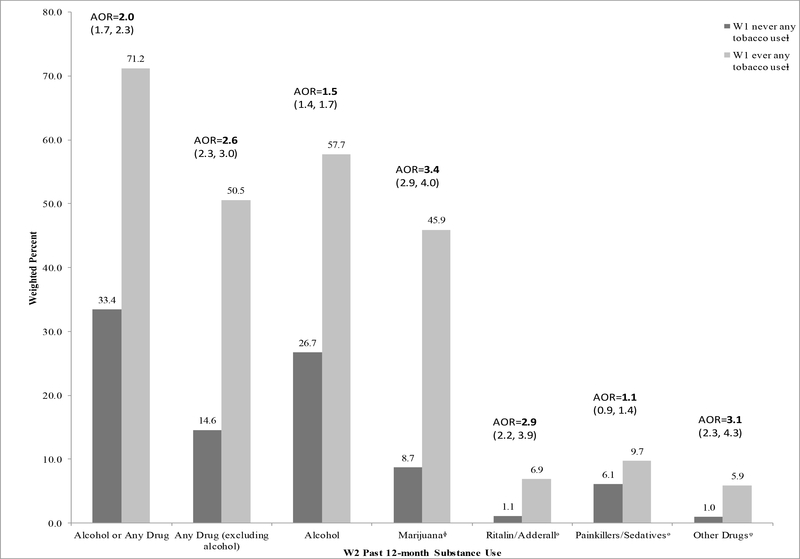
Figure 1 shows the unadjusted prevalence of past 12-month substance use at Wave 2 by ever any tobacco use at Wave 1. Any tobacco users at Wave 1 had a two-fold higher prevalence of Wave 2 alcohol use, and five- to six-fold higher prevalence of Wave 2 use of marijuana, nonprescribed Ritalin/Adderall, and other drugs compared to never tobacco users. Similarly, any tobacco product use at Wave 1 predicted any drug use at Wave 2 whether alcohol was included (AOR=2.0; 95% CI: 1.7, 2.3) or excluded (AOR=2.6; 95% CI: 2.3, 3.0) after adjusting for demographics, sensation seeking, past-year mental health problems, and ever substance use at Wave 1 (see also Supplementary Table 1)2.
Figure 1.
Prevalence of Wave 2 (W2) Past 12-month Substance Use by Wave 1 (W1) Ever Any Tobacco Use Among 11,996 Wave 1 Youth (12–17 years) in the PATH Study.
Note: Adjusted odds ratios (AORs) and 95% confidence intervals (CIs) from multivariable logistic regression models adjusting for age, gender, race/ethnicity, sensation seeking, past-year mental health problems at Wave 1, and ever substance use at Wave 1. ᶲIncludes past 12-month use of cigars as blunts. ᶱRefers to prescription drugs that were not prescribed for the participant or taken only for the experience or feeling they caused. ⱡRefers to cigarettes, e-cigarettes, traditional cigars, cigarillos, filtered cigars, pipe, hookah, snus pouches, smokeless tobacco excluding snus pouches, kreteks, bidis, or dissolvable tobacco. Models were restricted to observations with non-missing data; unweighted sample sizes ranged from 10493 (for the any tobacco and alcohol or any drug model) to 10538 (for the any tobacco and non-prescribed painkiller/sedative model). Statistically significant associations at p<.05 indicated in bold text.
Table 1 presents the adjusted associations between ever tobacco-product use at Wave 1 and past 12-month substance use at Wave 2. Except for pipes, snus pouches, and smokeless tobacco excluding snus pouches, tobacco-product use was associated with a two-fold higher odds of subsequent marijuana use. Across tobacco products, statistically significant associations were consistently observed for other drug use; the only non-significant association was observed for smokeless tobacco excluding snus pouches. The magnitude of the associations with other drugs ranged from 1.6 (for any smokeless tobacco) to 3.7 (for filtered cigars).
Notably, e-cigarette use was associated with subsequent substance use across all substances assessed, except for non-prescribed painkillers/sedatives. The strongest associations were observed for non-prescribed Ritalin/Adderall (OR=3.2; 95% CI: 2.3, 4.4) and other drugs (OR=2.5; 95% CI: 1.7, 3.5). Only use of e-cigarettes (AOR=1.3; 95% CI: 1.1, 1.5), any cigars (AOR=1.2; 95% CI: 1.0, 1.5), and hookah (AOR=1.4; 95% CI: 1.2, 1.7) were associated with higher odds of subsequent alcohol use. Snus pouches (AOR=1.8; 95% CI: 1.1, 2.9) and smokeless tobacco excluding snus pouches (AOR=1.8; 95% CI: 1.3, 2.5) were significantly associated with subsequent non-prescribed painkiller/sedative use, whereas no significant associations were observed for other tobacco products.
Compared to never e-cigarette and never cigarette use at Wave 1 (Supplementary Table 3)3, ever exclusive e-cigarette use (AOR=2.1; 95% CI: 1.5, 3.0), exclusive cigarette use (AOR=1.5; 95% CI: 1.1, 2.0), and e-cigarette and cigarette use (AOR=2.1; 95% CI: 1.4, 3.3) were each associated with higher odds of subsequent past 12-month alcohol or any drug use. Associations for any drug (excluding alcohol) and marijuana use increased in magnitude for-ever exclusive ecigarette use, exclusive cigarette use, and e-cigarette and cigarette use compared to never ecigarette and never cigarette use. Ever exclusive e-cigarette use and exclusive cigarette use were significantly associated with subsequent alcohol use. Whereas ever exclusive e-cigarette use and e-cigarette and cigarette use were significantly associated with subsequent use of non-prescribed Ritalin/Adderall, estimates for exclusive cigarette use were unreliable.
Gender moderated the association between ever e-cigarette use and subsequent past 12month alcohol or any drug use; a slightly stronger association was observed for male (AOR=1.9; 95% CI: 1.5, 2.4) compared to female users (AOR=1.4; 95% CI: 1.0, 1.9). Significant gender interactions were also observed for the association between ever any smokeless tobacco use and subsequent alcohol or any drug use, as well as ever use of any tobacco, cigarettes, e-cigarettes, ecigarette and cigarette use, any cigars, traditional cigars, cigarillos, and hookah with subsequent non-prescribed painkiller/sedative use. Although the patterns were generally consistent showing either stronger associations for male compared to female users or significant associations for male users but not for female users, these associations were not significant in gender-stratified analyses.
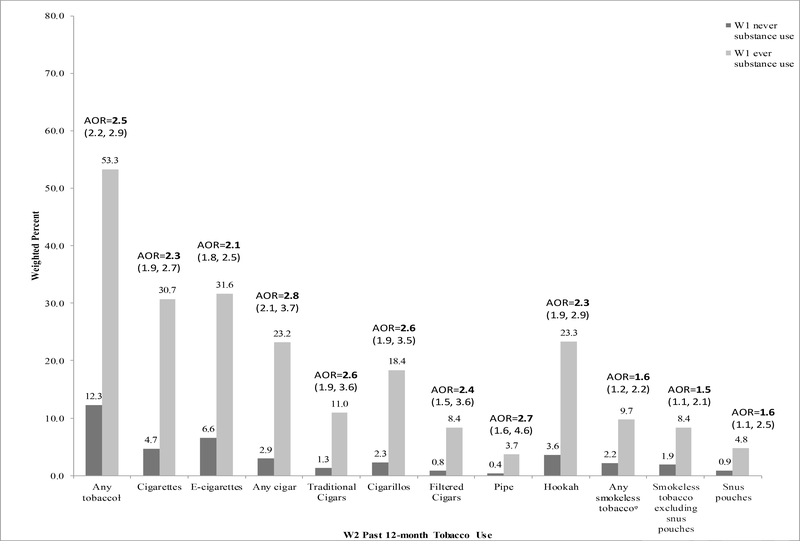
3.2. Substance Use Predicting Tobacco Use
Figure 2 shows the unadjusted prevalence of past 12-month tobacco-product use at Wave 2 by ever substance use at Wave 1. Ever alcohol or any drug users had a four to ten-fold higher prevalence of Wave 2 tobacco use across all products compared to never alcohol or any drug users. Ever alcohol or any drug use predicted tobacco use after adjusting for demographics, sensation seeking, past-year mental health problems, and ever tobacco use at Wave 1 (AOR=2.5; 95% CI: 2.2, 2.9) (see also Supplementary Table 2)4. Associations were consistent and robust across the tobacco products assessed.
Figure 2.
Prevalence of Wave 2 (W2) Past 12-month Tobacco Use by Wave 1 (W1) Ever Any Substance Use Among 11,996 Wave 1 Youth (12–17 years) in the PATH Study.
Note: Adjusted odds ratios (AORs) and 95% confidence intervals (CIs) from multivariable logistic regression models adjusting for age, gender, race/ethnicity, sensation seeking, past-year mental health problems at Wave 1, and ever tobacco use at Wave 1. ᵠRefers to snus pouches, smokeless tobacco excluding snus pouches, or dissolvable tobacco. ⱡRefers to cigarettes, e-cigarettes, traditional cigars, cigarillos, filtered cigars, pipe, hookah, snus pouches, smokeless tobacco excluding snus pouches, or dissolvable tobacco. Unreliable estimates (for dissolvable tobacco) were suppressed based on relative standard error greater than 0.30 or denominator sample size less than 50. Models were restricted to observations with non-missing data; unweighted sample sizes ranged from 10397 (for the alcohol or any drug and any tobacco model) to 10568 (for the alcohol or any drug and cigarette model). Statistically significant associations at p<.05 indicated in bold text.
Table 2 presents the adjusted associations between ever substance use at Wave 1 and past 12-month tobacco-product use at Wave 2. Ever marijuana use was associated with a 2 to 2.5-fold higher odds of use for all tobacco products except snus pouches and smokeless tobacco excluding snus pouches. Ever use of alcohol and non-prescribed Ritalin/Adderall also consistently predicted higher odds of subsequent tobacco use. Some of these associations were non-significant, especially for tobacco products with low prevalence (filtered cigars and pipes).
Associations for use of non-prescribed painkillers/sedatives and other drugs were not consistent across tobacco products. Ever non- prescribed painkiller/sedative use was associated only with use of e-cigarettes (AOR=1.5; 95% CI: 1.2, 1.9), filtered cigars (AOR=1.7; 95% CI: 1.2, 2.2), and pipes (AOR=1.7; 95% CI: 1.1, 2.7). Ever other drug use predicted use of cigarettes (AOR=2.6; 95% CI: 1.7, 4.1), e-cigarettes (AOR=1.6; 95% CI: 1.2, 2.2), any cigars (AOR=2.1; 95% CI: 1.4, 3.2), and pipes (AOR=2.9; 95% CI: 1.6, 5.1).
In multinomial regression analyses, Wave 1 ever (versus never) use of alcohol or any drug, any drug (excluding alcohol), and marijuana were each significantly associated with subsequent past 12-month exclusive e-cigarette use, exclusive cigarette use, and e-cigarette and cigarette use compared to no past 12-month use of e-cigarettes and cigarettes; the strongest associations were observed for exclusive cigarette use (Supplementary Table 4)5. Whereas ever non-prescribed Ritalin/Adderall use was associated with subsequent exclusive cigarette use and e-cigarette and cigarette use, estimates for exclusive e-cigarette use were unreliable. Ever non-prescribed painkiller/sedative use was associated only with subsequent e-cigarette use.
Gender moderated the associations between ever any drug (excluding alcohol) use and marijuana use and subsequent e-cigarette use. In both instances, associations were slightly stronger among male (AOR=2.1; 95% CI: 1.7, 2.6 for-ever any drug (excluding alcohol) and AOR=2.3; 95% CI: 1.9, 3.0 for marijuana use) compared to female users (AOR=1.6; 95% CI: 1.2, 2.1 forever any drug (excluding alcohol) and AOR=1.6; 95% CI: 1.2, 2.1 for marijuana use). Although significant gender interactions were observed for associations between non-prescribed painkillers/sedatives and pipe use, models for female youths did not converge.
4. Discussion
Findings reveal bidirectional associations between tobacco use and substance use among U.S. youth, indicating that ever tobacco use predicted subsequent alcohol or any drug use, and ever alcohol or any drug use predicted subsequent tobacco use. Associations were robust to numerous potential confounders including demographic characteristics, sensation seeking, past-year mental health problems, as well as the prior and concurrent use of other tobacco products and substances.
Across tobacco products, associations were consistent with marijuana (except pipes, smokeless tobacco, and snus pouches) and other drugs (except smokeless tobacco), thus supporting the notion that tobacco use generally predicts any drug (marijuana, prescription drugs, and other drugs) use in U.S. youth. Findings confirm longitudinal associations between ever cigarette use and subsequent marijuana use among youth (Ramo et al., 2012), and extend them to use of nonprescribed Ritalin/Adderall and other drugs. Ever e-cigarette use, particularly exclusive use, and ever hookah use predicted subsequent alcohol use, possibly as a function of social use or greater access and availability of these products among youth. E-cigarettes were the only tobacco product consistently associated with the use of all substances except non-prescribed painkillers/sedatives. These associations were significant not only for-ever e-cigarette and cigarette use, but also forever exclusive e-cigarette use such that ever e-cigarette and cigarette use predicted any drug use (excluding alcohol) in a gradient with associations increasing in magnitude from exclusive ecigarette use to exclusive cigarette use and e-cigarette and cigarette use. The strongest associations with ever e-cigarette and cigarette use were observed for marijuana and non-prescribed Ritalin/Adderall, which may point to the use of these tobacco products and substances within social or recreational settings (Leon and Martinez, 2017). Whereas previous studies have reported longitudinal associations between ever and past 30-day e-cigarette use and cigarette smoking initiation and past 30-day cigarette smoking, respectively (Soneji et al., 2017), our findings extend these associations to substance use, highlighting the need to additionally monitor alcohol and any drug use among youth e-cigarette users, particularly among users of both cigarettes and ecigarettes. Lastly, while ever use of other tobacco products (i.e., cigarettes, e-cigarettes, cigars, pipes, and hookah) was not associated with subsequent painkiller/sedative use, ever use of smokeless tobacco and snus pouches strongly predicted subsequent non-prescribed painkiller/sedative use. The specificity of these associations may point to differences in use patterns for these tobacco products and non-prescribed painkillers/sedatives, potentially driven by factors associated with living in rural areas where both smokeless tobacco use and opioid misuse are prevalent (Keyes et al., 2013; National Center for Chronic Disease Prevention and Health Promotion and Office on Smoking and Health, 2012).
Associations in the opposite direction were also significant. Ever alcohol and nonprescribed Ritalin/Adderall use consistently predicted subsequent tobacco use across all products assessed. Likewise, ever marijuana use predicted subsequent tobacco use across all products except smokeless tobacco. That ever alcohol and marijuana use predict subsequent use of hookah and cigars not only advances prior cross-sectional studies of youth (Palamar et al., 2014; Schuster et al., 2013) but also extends findings to other tobacco products (e.g., e-cigarettes). Across all substances assessed, ever alcohol and any drug use predicted subsequent e-cigarette use. Similar associations were observed in the combined e-cigarette and cigarette analyses; however, the strongest associations were observed for the exclusive cigarette users. The bidirectional associations between e-cigarette and cigarette use and any drug use (including and excluding alcohol) not only extend cross-sectional findings among U.S. high school seniors (McCabe et al., 2017), but may also suggest common factors underlying the use of e-cigarettes, cigarettes, and any drugs.
Prior cross-sectional analyses of youth from Wave 1 of the PATH Study (Conway et al., 2018) showed stronger associations with substance use among female compared to male users for cigarettes, any cigar, cigarillos, hookah, and smokeless tobacco (including snus pouches). However, no gender interactions were observed for these products in the current longitudinal analyses. Interestingly, associations with alcohol or any drug use were stronger for male e-cigarette users than female users. In the reverse direction, associations with e-cigarette use were stronger for male any drug (excluding alcohol) and marijuana users compared to female users of these products. Although the gender interactions for the bidirectional associations between e-cigarette use and any drug use differed by the inclusion and exclusion of alcohol, the associations in both directions were stronger for male compared to female users. The differing findings for gender by tobacco product suggest that male and female youth may benefit from targeted interventions based on the types of products they use.
Overall, the strengths of the bidirectional associations were similar across tobacco products and substances. Although many of the associations between ever tobacco use and subsequent alcohol use were not significant compared to the associations in the opposite direction (i.e., ever alcohol use and subsequent tobacco use), formally testing the magnitude and significance of these bidirectional associations with additional waves of PATH Study data represents an area of future research. Nevertheless, the findings of bidirectional associations among tobacco use and substance use among youth can be interpreted in several ways. First, the use of one drug (e.g., nicotine) may increase the probability of using another drug (e.g., marijuana) via biological mechanisms such as priming (Kandel and Kandel, 2015; Kandel et al., 1992). Indeed, preclinical studies have shown biological interactions between nicotine and alcohol as well as drugs (marijuana, opioids, and cocaine and other stimulants) whereby the use of one specific substance influences the use of another (Cross et al., 2017; Kohut, 2017; Spear, 2016). Second, initiation and progression of tobacco and substance use may reflect common underlying factors such as genetic predispositions (Hines et al., 2015; Vanyukov et al., 2012), environmental factors that increase risk of use (Hines et al., 2015; Vanyukov et al., 2012), or problem behaviors (Jessor, 1991). The order of use, from this perspective, may reflect unmeasured risk factors (e.g., vulnerability traits [other than sensation seeking], opportunities to use, peer use) that are shared across the use of tobacco, alcohol, and drugs. The plausibility of common factors underlying these bidirectional associations is supported by twin studies. Whereas some studies (Vrieze et al., 2012; Waaktaar et al., 2018) show that the comorbidity in youth tobacco use and substance use is largely due to a common genetic liability, other studies (Han et al., 1999; Koopmans et al., 1997) attribute the observed comorbidity to shared environmental factors. Therefore, consistent with an integrated risk-prevention perspective (Hale et al., 2014) our findings point to two promising directions for prevention and intervention efforts: (1) comprehensive screening of alcohol, tobacco, and any drug use among youth, and (2) addressing modifiable risk factors common to multiple forms of substance use.
This study has both strengths and limitations. It is the first to longitudinally describe tobacco use and substance use among U.S. youth across a range of tobacco products including emerging non-cigarette tobacco products. The analyses also included several important covariates (e.g., demographics, mental health, sensation seeking) that help mitigate confounding. Ever use of any tobacco and alcohol or any drugs emerged as the strongest predictors of subsequent tobacco use and substance use, respectively. Sensation seeking was consistently associated with use across all substances but not all tobacco products. Demographic characteristics and mental health problems predicted both tobacco use and substance use; however, associations varied by tobacco products and substances. Nonetheless, these findings reinforce the need for controlling for these covariates in analyses examining tobacco and substance use behaviors. The use of past 12-month assessments for Wave 2 tobacco use and substance use maximized the capture of behaviors that are intermittent in this age group. It remains a possibility that the associations could differ among more frequent or regular users; however, adjusting for Wave 1 past 30-day use or the number of days of use in the past 30 days had no substantial impact on the observed associations. Some cigar users may be blunt-only users, thus potentially overestimating the associations between cigar use and marijuana use; yet, exclusion of past 12-month blunt-only users did not substantially affect estimates. Additionally, although longitudinal associations were identified between tobacco and substance use, causality cannot be established. The role of several common underlying factors associated with youth tobacco use and substance use (e.g., family history, peer influence) were not included in this study; this is an important area for future research. The PATH Study lacked data on synthetic drugs (e.g., spice); therefore, associations for this class of drugs could not be examined. Finally, the relatively short period of follow-up may have limited statistical power to detect some associations for less frequently used tobacco products and substances, however presenting estimates across a wide range of tobacco products addresses an important gap in the literature that has predominantly focused on cigarette use. Further, these estimates provide a foundation for monitoring changes in tobacco and substance use patterns over time. Future assessments of tobacco, alcohol, and drug use across additional data-collection waves in the PATH study can inform how onset and progression evolve over longer periods of time.
5. Conclusion
In summary, bidirectional longitudinal associations were observed between the use of tobacco products, alcohol, and drugs among U.S. youth. Preventive and intervention efforts may benefit from a comprehensive screening of tobacco, alcohol, and drug use among youth. In addition to screening, future research should identify risk factor(s) shared across substances that when mitigated most effectively prevent the onset of substance use in youth.
Supplementary Material
Highlights.
Any tobacco use predicted subsequent substance (alcohol or drug) use.
E-cigarette use predicted substance use except non-prescribed painkillers/sedatives.
Substance use consistently predicted tobacco use across products.
Marijuana use predicted use of all tobacco products except smokeless tobacco.
Targeting risk factors shared across tobacco and substances may be beneficial.
Acknowledgements
The authors would also like to acknowledge Drs. Kathryn Edwards and Kevin Frissel for their assistance with deriving the variables and Drs. Heather D’Angelo and Yan Zhuang for completing quality control re-analyses. This article was prepared while Dr. Kevin Conway was employed at the National Institute on Drug Abuse, National Institutes of Health, Bethesda, MD and Drs. Amy Cohn and Raymond S. Niaura were employed at the Schroeder Institute for Tobacco Research and Policy Studies, Truth Initiative, Washington, DC.
Role of Funding Source
This manuscript is supported with Federal funds from the National Institute on Drug Abuse, National Institutes of Health, and the Food and Drug Administration, Department of Health and Human Services, under a contract to Westat (Contract No. HHSN271201100027C). Staff from the NIDA and the FDA contributed to the design and conduct of the study; management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; and the decision to submit the manuscript for publication. The NIDA and the FDA were not directly involved in the collection of study data. The views and opinions expressed in this manuscript are those of the authors only and do not necessarily represent the views, official policy or position of the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies.
Footnotes
Conflict of Interest
Dr. Compton reports holding stock in General Electric, the 3M Companies, and Pfizer; Dr. Cummings reports receiving grant support from Pfizer and receiving fees as a paid expert witness in litigation filed against the tobacco industry; Dr. Niaura reports having been a witness for plaintiffs vs. tobacco companies, receiving speaker fees, receiving honoraria, sitting on advisory boards, being a site PI, and consulting for pharmaceutical companies testing and marketing smoking cessation aids, but not in the last 6 years. No other potential conflict of interest relevant to this manuscript was reported.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: ...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: ...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: ...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: ...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: ...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: ...
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arrazola RA, Singh T, Corey CG, Husten CG, Neff LJ, Apelberg BJ, Bunnell RE, Choiniere CJ, King BA, Cox S, McAfee T, Caraballo RS, 2015. Tobacco use among middle and high school students - United States, 2011–2014. MMWR Morb. Mortal. Wkly. Rep 64, 381–385. [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2016. 2015 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf. [Google Scholar]
- Centers for Disease Control and Prevention (CDC), 2011–2012. National Health and Nutrition Examination Survey Questionnaire (NHANES). In: National Center for Health Statistics; (Ed.), Hyattsville, MD: https://www.cdc.gov/nchs/nhanes/index.htm [Google Scholar]
- Conway KP, Green VR, Kasza KA, Silveira ML, Borek N, Kimmel HL, Sargent JD, Stanton CA, Lambert E, Hilmi N, Reissig CJ, Jackson KJ, Tanski SE, Maklan D, Hyland AJ, Compton WM, 2018. Co-occurrence of tobacco product use, substance use, and mental health problems among youth: Findings from wave 1 (2013–2014) of the population assessment of tobacco and health (PATH) study. Addict. Behav 76, 208–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross SJ, Lotfipour S, Leslie FM, 2017. Mechanisms and genetic factors underlying co-use of nicotine and alcohol or other drugs of abuse. Am. J. Drug Alcohol Abuse 43, 171–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H, Catley D, Richter KP, Goggin K, Ellerbeck EF, 2018. Electronic cigarettes and future marijuana use: A Longitudinal Study. Pediatrics 141. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Chan YF, Funk RR, 2006. Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. Am. J. Addict 15, 80–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner BR, Belur VK, Dennis ML, 2013. The GAIN Short Screener (GSS) as a predictor of future arrest or incarceration among youth presenting to Substance Use Disorder (SUD) treatment. Subst. Abuse 7, 199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale DR, Fitzgerald-Yau N, Viner RM, 2014. A systematic review of effective interventions for reducing multiple health risk behaviors in adolescence. Am. J. Public Health 104, e1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton CM, Strader LC, Pratt JG, Maiese D, Hendershot T, Kwok RK, Hammond JA, Huggins W, Jackman D, Pan H, Nettles DS, Beaty TH, Farrer LA, Kraft P, Marazita ML, Ordovas JM, Pato CN, Spitz MR, Wagener D, Williams M, Junkins HA, Harlan WR, Ramos EM, Haines J, 2011. The PhenX Toolkit: Get the most from your measures. Am. J. Epidemiol 174, 253–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han C, McGue MK, Iacono WG, 1999. Lifetime tobacco, alcohol and other substance use in adolescent Minnesota twins: Univariate and multivariate behavioral genetic analyses. Addiction 94, 981–993. [DOI] [PubMed] [Google Scholar]
- Hines LA, Morley KI, Mackie C, Lynskey M, 2015. Genetic and environmental interplay in adolescent substance use disorders. Curr. Addict. Rep 2, 122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyle RH, Stephenson MT, Palmgreen P, Lorch EP, Donohew RL, 2002. Reliability and validity of a brief measure of sensation seeking. Pers. Individ. Dif 32, 401–414. [Google Scholar]
- Hyland A, Ambrose BK, Conway KP, Borek N, Lambert E, Carusi C, Taylor K, Crosse S, Fong GT, Cummings KM, Abrams D, Pierce JP, Sargent J, Messer K, BansalTravers M, Niaura R, Vallone D, Hammond D, Hilmi N, Kwan J, Piesse A, Kalton G, Lohr S, Pharris-Ciurej N, Castleman V, Green VR, Tessman G, Kaufman A, Lawrence C, van Bemmel DM, Kimmel HL, Blount B, Yang L, O’Brien B, Tworek C, Alberding D, Hull LC, Cheng YC, Maklan D, Backinger CL, Compton WM, 2017. Design and methods of the Population Assessment of Tobacco and Health (PATH) study. Tob. Control 26, 371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessor R, 1991. Risk behavior in adolescence: A psychosocial framework for understanding and action. J. Adolesc. Health 12, 597–605. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE, 2017. Monitoring the Future National Survey results on drug use, 1975–2016: Overview, key findings on adolescent drug use. Institute for Social Research, The University of Michigan, Ann Arbor: http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2016.pdf [Google Scholar]
- Judkins DR, 1990. Fay’s method for variance estimation. J. Off. Stat 6, 223–239. [Google Scholar]
- Kandel D, Kandel E, 2015. The Gateway Hypothesis of substance abuse: Developmental, biological and societal perspectives. Acta Paediatr. 104, 130–137. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Yamaguchi K, Chen K, 1992. Stages of progression in drug involvement from adolescence to adulthood: further evidence for the gateway theory. J Stud. Alcohol 53, 447457. [DOI] [PubMed] [Google Scholar]
- Kasza KA, Ambrose BK, Conway KP, Borek N, Taylor K, Goniewicz ML, Cummings KM, Sharma E, Pearson JL, Green VR, Kaufman AR, Bansal-Travers M, Travers MJ, Kwan J, Tworek C, Cheng YC, Yang L, Pharris-Ciurej N, van Bemmel DM, Backinger CL, Compton WM, Hyland AJ, 2017. Tobacco-Product Use by Adults and Youths in the United States in 2013 and 2014. N. Engl. J. Med 376, 342–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Cerdá M, Brady JE, Havens JR, Galea S, 2013. Understanding the rural–urban differences in nonmedical prescription opioid use and abuse in the United States. Am. J. Public Health 104, e52–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein RJ, Proctor SE, Boudreault MA, Turczyn KM, 2002. Healthy People 2010 criteria for data suppression. Healthy People 2010 Stat. Notes 1–12. [PubMed] [Google Scholar]
- Kohut SJ, 2017. Interactions between nicotine and drugs of abuse: A review of preclinical findings. Am. J. Drug Alcohol Abuse 43, 155–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopmans JR, van Doornen LJP, Boomsma DI, 1997. Association between alcohol use and smoking in adolescent and young adult twins: A bivariate genetic analysis. Alcohol. Clin. Exp. Res 21, 537–546. [PubMed] [Google Scholar]
- Leon KS, Martinez DE, 2017. To Study, to Party, or Both? Assessing risk factors for nonprescribed stimulant use among middle and high school students. J. Psychoactive Drugs 49, 22–30. [DOI] [PubMed] [Google Scholar]
- McCabe SE, West BT, Veliz P, Boyd CJ, 2017. E-cigarette use, cigarette smoking, dual use, and problem behaviors among U.S. adolescents: Results From A National Survey. J. Adolesc. Health 61, 155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy PJ, 1969. Pseudoreplication: Further evaluation and applications of the balanced halfsample technique. Vital Health Stat 2 1–24. [PubMed] [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2012. Preventing tobacco use among youth and young adults: A Report of the Surgeon General. Centers for Disease Control and Prevention (US), Atlanta (GA). [PubMed] [Google Scholar]
- National Institutes of Health (NIH), 2004–2005. National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). In: National Institute on Alcohol Abuse and Alcoholism (NIAAA) (Ed.), Rockville, MD: https://www.surgeongeneral.gov/library/reports/preventing-youth-tobacco-use/fullreport.pdf. [Google Scholar]
- Palamar JJ, Zhou S, Sherman S, Weitzman M, 2014. Hookah use among U.S. high school seniors. Pediatrics 134, 227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Liu H, Prochaska JJ, 2012. Tobacco and marijuana use among adolescents and young adults: A systematic review of their co-use. Clin. Psychol. Rev 32, 105–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter L, Pugh BS, Smith PH, Ball SA, 2017. The co-occurrence of nicotine and other substance use and addiction among youth and adults in the United States: Implications for research, practice, and policy. Am. J. Drug Alcohol Abuse 43, 132–145. [DOI] [PubMed] [Google Scholar]
- Schuster RM, Hertel AW, Mermelstein R, 2013. Cigar, cigarillo, and little cigar use among current cigarette-smoking adolescents. Nicotine Tob. Res 15, 925–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, Yang J, Primack BA, Andrews JA, Miech RA, Spindle TR, Dick DM, Eissenberg T, Hornik RC, Dang R, Sargent JD, 2017. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: A systematic review and meta-analysis. JAMA Pediatr. 171, 788–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP, 2016. Consequences of adolescent use of alcohol and other drugs: Studies using rodent models. Neurosci. Biobehav. Rev 70, 228–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone AL, Becker LG, Huber AM, Catalano RF, 2012. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict. Behav 37, 747775. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, 2014. The health consequences of smoking—50 years of progress: A report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Atlanta, GA: https://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf. [Google Scholar]
- U.S. Department of Health and Human Services (HHS), Office of the Surgeon General, 2016. Facing addiction in America: The Surgeon General’s report on alcohol, drugs, and health. HHS, Washington, DC: https://www.surgeongeneral.gov/library/2016alcoholdrugshealth/index.html. [PubMed] [Google Scholar]
- United States Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse, and United States Department of Health and Human Services, Food and Drug Administration, Center for Tobacco Products., 2018. Population Assessment of Tobacco and Health (PATH) study [United States] restricted-use files, User Guide. ICPSR36231-v13 Inter-university Consortium for Political and Social Research [distributor], Ann Arbor, MI: https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/36231 [Google Scholar]
- Vanyukov MM, Tarter RE, Kirillova GP, Kirisci L, Reynolds MD, Kreek MJ, Conway KP, Maher BS, Iacono WG, Bierut L, Neale MC, Clark DB, Ridenour TA, 2012. Common liability to addiction and “gateway hypothesis”: theoretical, empirical and evolutionary perspective. Drug Alcohol Depend. 123, S3–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrieze SI, Hicks BM, Iacono WG, McGue M, 2012. Decline in genetic influence on the cooccurrence of alcohol, marijuana, and nicotine dependence symptoms from age 14 to 29. Am. J. Psychiatry 169, 1073–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waaktaar T, Kan KJ, Torgersen S, 2018. The genetic and environmental architecture of substance use development from early adolescence into young adulthood: a longitudinal twin study of comorbidity of alcohol, tobacco and illicit drug use. Addiction 113, 740–748. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.