Abstract
Objective To analyze the current clinical use of navigation at the lateral skull base among skull base surgeons in Germany.
Methods A web-based questionnaire was provided to surgeons being head of the department and member of one of the following scientific societies: German Society of Head and Neck Surgery, Maxillo-Facial Surgery, Neurosurgery, and German Skull Base Society. Replies were recorded anonymously. The questionnaire included the estimated case load per year and percent of surgery performed with navigation (middle and posterior fossa), type of navigation, estimates of intraoperative inaccuracy, and reasons for not using navigation.
Results Eighty nine out of 99 replies met requirements for final analysis. Overall, 37% of skull base surgeons use navigation on a regular basis (15% use no navigation). Optical tracking is more frequently used than magnetic tracking (71 vs 19). At the middle fossa, ENT surgeons split into routine users ( n = 10/36) and rare users ( n = 16/36), the latter stating navigation inaccuracy as a major reason for neglecting navigation. Neurosurgeons use navigation at the middle fossa significantly more often and criticize navigation inaccuracy less. At the posterior fossa, navigation is used less frequently by both ENT and neurosurgeons with similar rates of estimated inaccuracy.
Conclusions A moderate use of navigation at the lateral skull base was demonstrated. Insufficient accuracy causes ENT surgeons to frequently omit navigation at the middle fossa (not neurosurgeons) and posterior fossa (also neurosurgeons). Higher intraoperative navigation accuracy is needed to enhance the use of navigation at the lateral skull base.
Keywords: skull base, navigation, middle fossa, posterior fossa, accuracy, survey
Introduction
Surgical navigation has gained wide clinical appreciation. Targeting anatomical structures or pathological lesions around the skull base promises to be highly useful, because shift of soft tissue during surgery (as in brain surgery) usually does not occur due to fixation of the targets within or at the rigid bony structure. For clinical acceptance, not only technical accuracy of the navigation device but also the robustness and effectiveness of a perioperative workflow as well as the impression of the surgeons whether the technical adjunct supports his/her surgical goal with an acceptable amount of time for setup might influence the implementation of skull base navigation for routine use. Therefore, we asked skull base surgeons in Germany for their habits and indications for skull base navigation in their respective departments.
Methods
We defined nine questions regarding the routine use of navigation at the lateral skull base as a web-based electronic questionnaire (Survey Monkey, Appendix A ). The presidents of the German Societies of Maxillo-Facial Surgery, ENT-Head and Neck Surgery, Neurosurgery, and the German Skull Base Society agreed to address this questionnaire to all their respective members classified as head of department. These members were contacted directly by their societies and a detailed instruction was offered along with the link to the web-based questionnaire. Data entry was anonymous. Members were instructed to answer the questionnaire only once in case of membership in more than one of the involved societies.
Statistics
The database was analyzed by explorative statistical analysis (JMP 12.1.0, SAS, Cary, North Carolina, United States). Correlations were calculated using logistic regression models. Intergroup analysis of quantitative data was calculated using least squares F test. Categorical response analysis was used to analyze multiple items from different data categories for potential clusters. Level of error p < 0.05 was accepted as significant.
Results
Replies from 99 colleagues were entered into the database. Data sets with missing information were excluded from the final analysis ( n = 10; drop outs due to missing specialty: n = 1, missing information on surgery estimates: n = 9 [ENT: 7; neurosurgery: 1; maxillofacial surgery, MaxFacs: 1]). Eighty nine datasets were used for final analysis.
Basic Information (Q1, Q2)
Head of departments of 43 neurosurgical departments (48.3%), 36 ENT departments (40.4%), and 10 MaxFacs departments (11.2%) replied. Departments were located at university hospitals (46), academic teaching hospitals (39), and other institutions (4). In neurosurgery, more academic teaching hospitals contributed to the survey compared with university hospitals, whereas university hospitals dominated replies in ENT and maxillofacial departments ( p = 0.004; nominal logistic regression; Fig. 1 ).
Fig. 1.
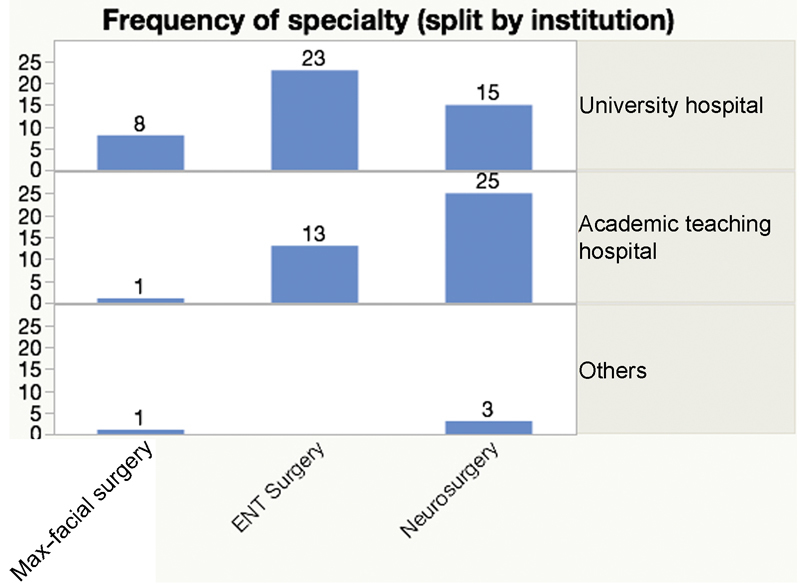
Counts of contributions of each specialty (maxillofacial surgery; ENT surgery; neurosurgery), split by the institution.
Type of Navigation Used (Q7)
Optic navigation is preferred over magnetic navigation over all (71 and 19, respectively) and within each specialty ( Fig. 2 ). In addition, integration of the surgical microscope into navigation is used in 34 departments (38%). Thirty seven percent of surgeons use navigation on a routine basis (neurosurgery: 15/43; ENT: 13/36, MaxFacs: 5/10), whereas 15% of participants do not use navigation at all in lateral skull base surgery.
Fig. 2.

Counts of type of navigation system used (magnetic tracking; optical tracking; microscope integration), split by specialty.
Middle Fossa Surgery and Navigation (Q3, Q5)
The estimated surgical case load at the middle fossa was significantly different between specialties with a higher case load in neurosurgery compared with ENT and MaxFacs ( p < 0.001, ordinal logistic model) as well as between institutions with a higher case load in university hospitals (ENT) and academic teaching hospitals compared with other hospitals ( p = 0.005, ordinal logistic model) ( Fig. 3 ).
Fig. 3.
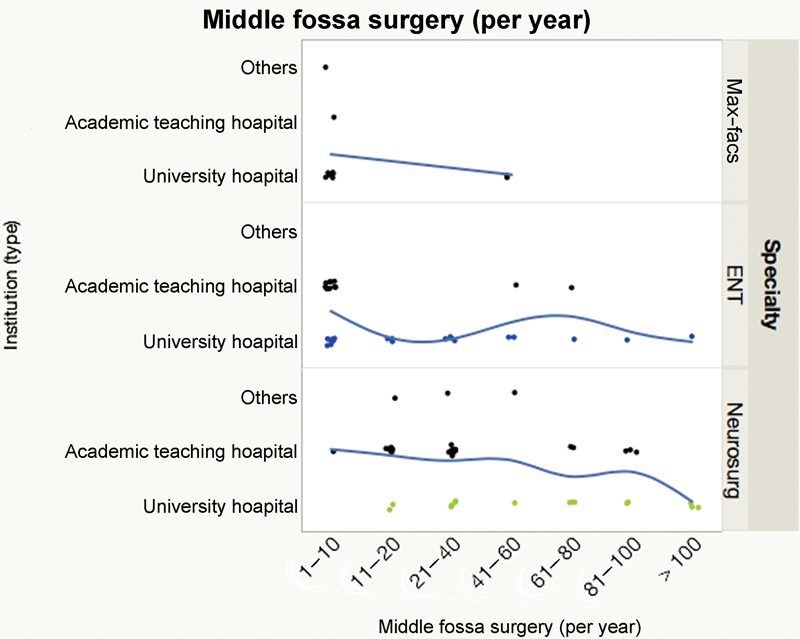
Estimated case load per year per department at the middle fossa (x-axis: ranges in absolute number), split by specialty and institution. The spline indicates the relative proportion between institutions at a given case load interval.
Correlation of estimated surgical case load and percent navigation used revealed a bimodal distribution at ENT centers with either rare use of navigation or near routine use of navigation at the middle fossa ( Fig. 4 ). In neurosurgery, the percent use of navigation was higher and independent from the estimated case load ( Fig. 4 ).
Fig. 4.
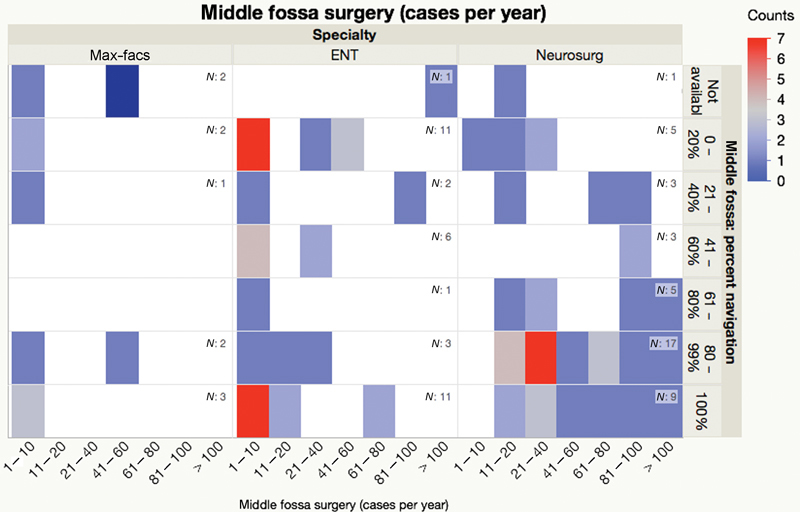
Heat map of estimated case load per year per department at the middle fossa (x-axis: ranges in absolute number), split by specialty and estimated percent of cases treated with navigation guidance (y-axis). Counts per field are color-coded.
Posterior Fossa Surgery and Navigation (Q4, Q6)
The estimated surgical case load at the posterior fossa was significantly different between specialties with higher case load in neurosurgery compared with ENT and MaxFacs ( p < 0.001, ordinal logistic model) as well as between institutions with higher case load in university hospitals (neurosurgery) compared with academic teaching and other hospitals ( p < 0.001, ordinal logistic model). ( Fig. 5 )
Fig. 5.
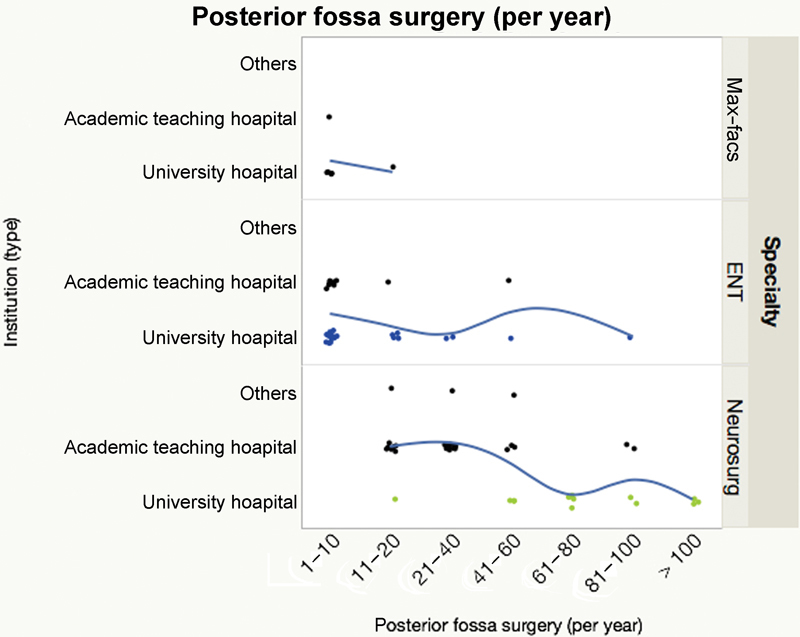
Estimated case load per year per department at the posterior fossa (x-axis: ranges in absolute number), split by specialty and institution. The spline indicates the relative proportion between institutions at a given case load interval.
Correlation of estimated surgical caseload and percent navigation used revealed a bimodal distribution at ENT centers with lower caseload, but low percentage of navigation in larger centers ( Fig. 6 ). In neurosurgery, the use of navigation was low with only 10 centers using navigation in more than 60% of cases ( Fig. 6 ).
Fig. 6.
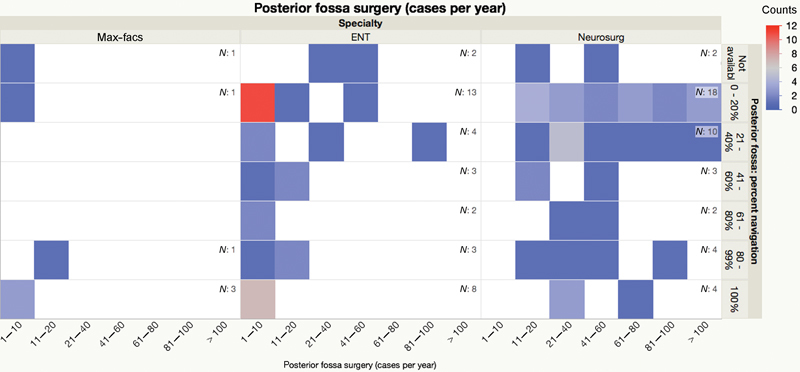
Heat map of estimated case load per year per department at the posterior fossa (x-axis: ranges in absolute number), split by specialty and estimated percent of cases treated with navigation guidance (y-axis). Counts per field are color-coded.
Reasons for Omission of Navigation (Q9)
Asked for reasons for not using navigation (at all or in certain cases), insufficient intraoperative support by navigation (“doesńt help”) was reported mostly by neurosurgeons. Inaccuracy was mentioned more often by ENT compared with neurosurgeons (trend; p = 0.068; Poisson Chi 2 ). The ENT group significantly more often classified navigation as “complicated” compared with neurosurgery ( p = 0.038; Poisson Chi 2 ). A positive vote as “always using navigation” was chosen by 15 neurosurgeons (34.9%), 13 ENT surgeons (36.1%), and 5 MaxFacs (50%) ( Fig. 7 ).
Fig. 7.
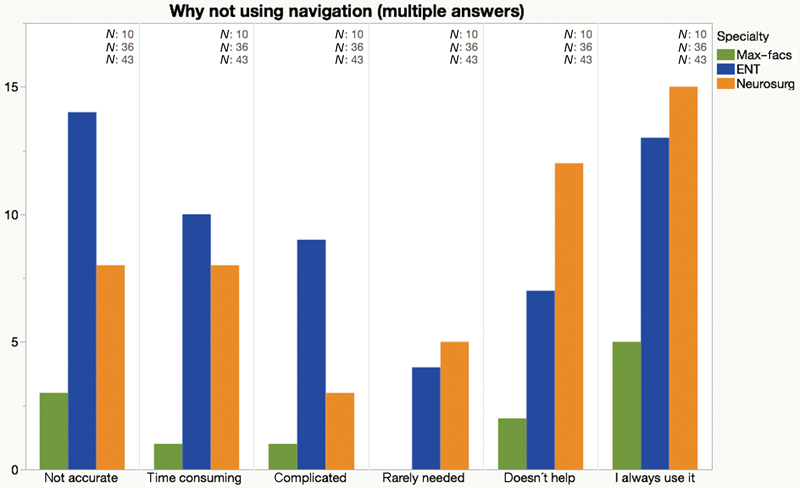
Relation of reasons for not using navigation, split by specialty. Absolute number of answers (multiple answers possible).
Estimation of Navigation Inaccuracy (Q8)
Objections to the use of navigation because of the impression of inaccuracy were significantly higher in the ENT group compared with neurosurgeons ( p = 0.017; least squares F-Test). Within each specialty, there was no significant difference between institutions. Departments that do not use navigation report a significantly higher rate of inaccuracy compared with departments using navigation ( p = 0.032; least squares F-Test) ( Fig. 8 ). Type of navigation (i.e., magnetic vs optical tracking) did not relate to the estimation of inaccuracy (data not shown).
Fig. 8.
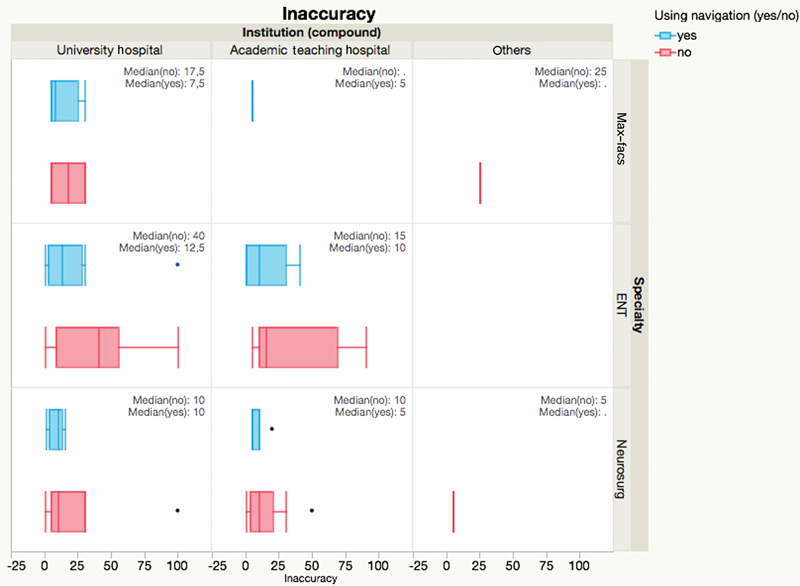
Estimation of inaccuracy (in percent of cases), split by specialty and institution. Box-and-whisker plot; blue: departments using navigation. Red: departments not using navigation.
Descriptions of inaccuracy (“not accurate,” “doesn't help”; Q9, multiple answers possible ) were predominant in the ENT group using navigation rarely (in < 40% of cases) at the middle fossa ( n = 16/56) and posterior fossa ( n = 16/55), whereas 10 ENT and neurosurgeons stated using navigation “always” reported to use navigation in more than 60% of cases ( Figs. 9 and 10 ).
Fig. 9.
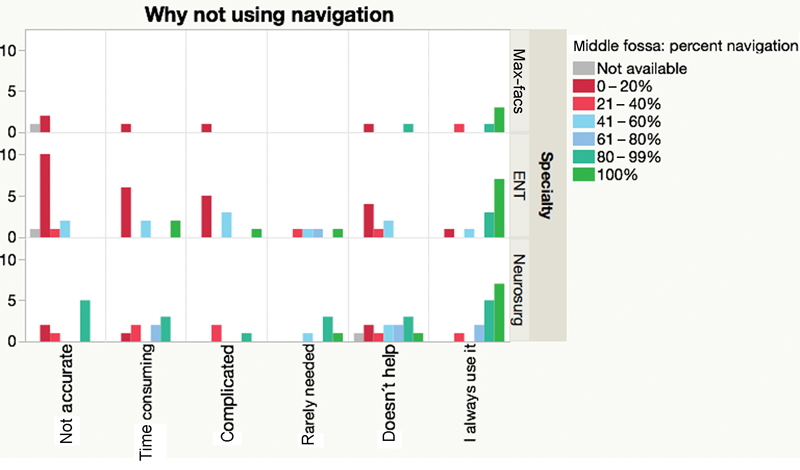
Middle fossa surgery: Relation of reasons for not using navigation, split by specialty and estimated percent of cases treated with navigation guidance (y-axis). Red bars indicate low percentage of navigation, green high percentage. Absolute number of answers (multiple answers possible).
Fig. 10.
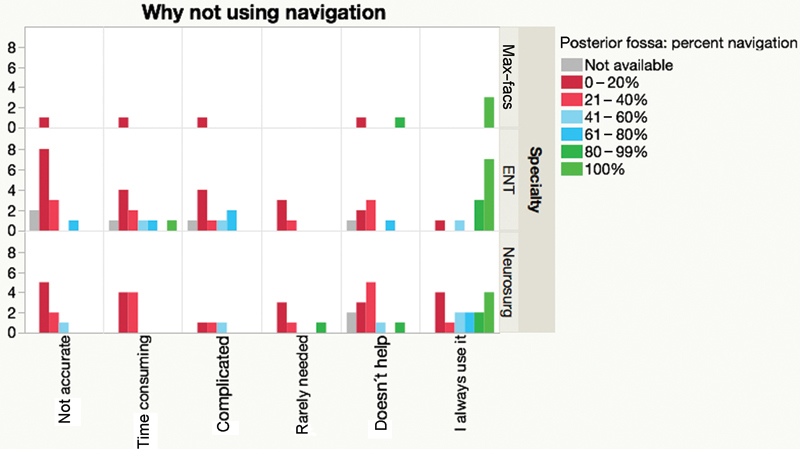
Posterior fossa surgery: Relation of reasons for not using navigation, split by specialty and estimated percent of cases treated with navigation guidance (y-axis). Red bars indicate low percentage of navigation, green high percentage. Absolute number of answers (multiple answers possible).
In neurosurgery, terms of inaccuracy as described above are reported rarely ( n = 6/51) at the middle fossa, but more often at the posterior fossa ( n = 15/51). Interestingly, five neurosurgeons stating routine use of navigation at the posterior fossa also state to use it in less than 40% or 20% of cases, which points toward incoherent comments to similar questions ( Figs. 9 and 10 ).
Multidimensional Analysis (Correlation of Specialty, Type of Institution, and Reported Need of Navigation)
Categorical response analysis was used to analyze the relation of types of specialty, institution, and statement for not using navigation as reported by the heads of department for potential clusters. Visual three-dimensional analysis revealed two clusters. Cluster 1 comprises of “ENT” close to the navigation items “complicated” and “not accurate” and the navigation type “magnetic.” Cluster 2 comprises of “neurosurgery” close to the navigation item “doesńt help” and the navigation type “optic” and “scope integration.” The type of institution and the specialty of MaxFacs did not relate to distinctable clusters in this analysis ( Fig. 11A , B )
Fig. 11.
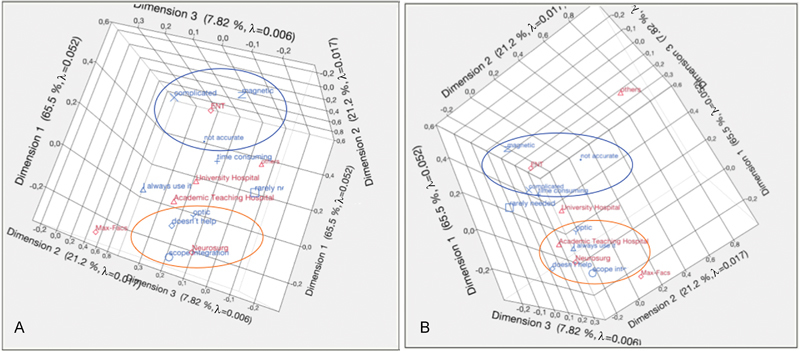
( A , B ) Three-dimensional relation of categorical response analysis of items: Specialty (red), institution (red), type of navigation (blue), reasons for not using navigation (blue). Part ( A ) view along dimension 2 and part (B) view along dimension 3 (90° flip). Group of items clustered in both views are marked with circles (orange: neurosurgery centered; blue: ENT centered).
Discussion
Based on estimates within the respondent group of surgeons clinically active at the lateral skull base in Germany, surgery at the middle and posterior fossa is more often performed in neurosurgical departments compared with ENT departments. This estimation, however, looks skewed. Given that mastoidectomies in ENT are performed in high numbers on a daily and routine basis without the need for navigation, navigation is reserved for special complex cases (e.g., cholesteatoma with extension to the petrous apex or complex tumors). Also, extended skull base procedures are performed in a limited number of ENT departments, only.
Therefore, this difference of case load between specialties might be interpreted as looking at a specific group of patients within each specialty, in which navigation might be considered as a valid option and addition to the surgeons' needs, but not all patients with skull base procedures. This consideration might complicate the discussion of case load, but does not affect the analysis of philosophy to use of navigation and reason for or against this technology in different departments and specialties. The survey data from MaxFacs are relatively sparse and are, therefore, not discussed in detail. It seems that navigation at the lateral skull base has its place in this specialty, but mainly in a few university centers.
Magnetic navigation was less used compared with optic systems, but the estimation of the proportion of cases with inaccurate navigation did not differ between both navigation systems (data not shown). Inferior laboratory accuracy has been published for magnetic tracking at the lateral skull base, 1 but identification of 45% (middle fossa) and 65% (translabyrinthine approach) of landmarks with less than 0.5 mm target registration error in cadavers was recently reported. 2
In this survey, navigation is reported to be used more often at the lateral skull base in neurosurgery, especially at the middle fossa. The difference to the percentage of navigation used in posterior fossa surgery is striking, where navigation is less in favor. This differentiation of the use of navigation between lateral skull base areas is reflected by neurosurgery as a relatively homogenous group. At the posterior fossa, inaccuracy issues are prominent within the group of neurosurgeons using navigation in less than 20% to 40% of cases, and this is reflected within the ENT group as well. Middle fossa, however, is completely different. Inaccuracy is less an issue and the proportion of neurosurgeons using navigation often is high.
ENT surgeons, however, are “split” in two groups. This is more prominent in middle fossa compared with posterior fossa procedures. At the middle fossa, inaccuracy is clearly an argument of a group ENT surgeons using navigation in less than 20% to 40% of cases. This may reflect findings from a retrospective study on 41 patients with temporal bone navigation, where intraoperative support by navigated distance control or navigated control of the drill was reported as necessary for the surgery by the ENT surgeon in 17% of cases. 3 However, those using navigation often or always do not point out accuracy problems in our survey.
Despite a lot of possible interpretations for this difference at the middle fossa, two hypotheses can be put forward.
Neurosurgeons might be less experienced in the complex anatomy of the middle fossa and, therefore, might rely more on image guidance support than ENT surgeons. This would explain the difference in the proportion of navigation, but not in the perception of potential or real inaccuracy.
The strategic concept of each surgery (i.e., removal of tumors attached to the middle fossa as meningiomas or petrous apex “transit” to retroclival targets vs facial nerve decompression at the geniculate ganglion or targeting of the cochlea for cochlea implant positioning) was not analyzed in this survey. This might influence the purpose of using navigation significantly. Navigation accuracy might be sufficient for a middle fossa approach to a small petroclival meningioma for a neurosurgical purpose, but insufficient for drilling the internal acoustic canal safely without blue-lining the superior semicircular canal in a flat middle fossa for an ENT purpose. This example may illustrate a potential difference of expectations on navigation depending on the surgical goal: to “get safely around” or to “stay out” of an anatomical detail in lesions on the surface of the middle fossa (i.e., meningioma) versus to “precisely encounter” the lesion within the lateral skull base (i.e., semicircular canal/cochlea).
In our interpretation, there is not a single concept of “the navigation.” It is a surgical tool with a different supportive impact to the skull base surgeon depending on the surgical goal and strategy—there are many “navigation scenarios.” In cases of a regular anatomy, navigation with average accuracy based on surface matching might speed up the surgical procedure (i.e., suboccipital craniotomy 4 ) while protecting eloquent anatomy (in combination with neuromonitoring). It is important to note that the registration error at known targets, not the overall root mean square error, helps to estimate the actual accuracy. 5 Dental splints, showing improved accuracy in laboratory tests, may improve the clinical accuracy while using preoperative image data. 6 In other cases, accuracy based on surface laser scanning or oral splint technologies may be not sufficient 7 without improved registration procedures such as intraoperative C-arm flat panel imaging 8 or intraoperative high-resolution imaging such as digital volume tomography 9 10 or additional integration of electrophysiological monitoring. 11 As this add on in accuracy might be costly or time consuming, this kind of advanced navigation might be limited in use until the workflow and health care funding may be optimized. 12
This “hesitation” of implementation of navigation in ENT departments due to restrictions in accuracy calls for further improvements in the field of image guidance registration to the patient. Since empowered surgical assistance devices gain more acceptances in surgery, 13 the topic of high accuracy image guided surgery in clinical routine at the lateral skull base might warrant even more attention. 10
Conclusions
This survey demonstrates a moderate clinical use of navigation at the lateral skull base. Estimation of insufficient accuracy leads a large part of ENT surgeons to refrain from navigation at the middle fossa (but not neurosurgeons) and posterior fossa (also neurosurgeons). Higher intraoperative navigation accuracy in the clinical setting is needed to spread the use of navigation (and other image-guided technologies such as assistance systems or robotics) at the lateral skull base.
Acknowledgments
The authors thank the members of the German Societies of Maxillofacial Surgery, ENT-Head and Neck Surgery, Neurosurgery, and Skull Base Surgery and their presidents and executive boards for their active support.
Conflict of Interests All authors indicate no conflict of interest.
Note
Presented at the 12 th Congress of the European Skull Base Society, May 26 to 28, 2016, Berlin, Germany.
Appendix A.
Questionnaire
Q1: What is your specialty?
Neurosurgery
ENT head and neck surgery
Maxillofacial surgery
Q2: Please specify the institution you are working in
University hospital
Academic teaching hospital
Nonacademic hospital, main department
Occupancy ward
Q3: How many operations at the middle fossa do you perform in your department each year (time interval for estimation: 2013 to 2015)
1 to 10
11 to 20
21 to 40
41 to 60
61 to 80
81 to 100
More than 100
Q4: How many operations at the posterior fossa do you perform in your department each year (time interval for estimation: 2013–2015)
1 to 10
11 to 20
21 to 40
41 to 60
61 to 80
81 to 100
More than 100
Q5: For middle fossa surgery, how often (in percent of cases) do you use navigation?
We don't use navigation
0% to 20%
21% to 40%
41% to 60%
61% to 80%
More than 80%
Always (100%)
Q6: For posterior fossa surgery, how often (in percent of cases) do you use navigation?
We don't use navigation
0 to 20%
21 to 40%
41 to 60%
61 to 80%
More than 80%
Always (100%)
Q7: What type of navigation technology do you use (multiple answers possible)?
Optical navigation
Magnetic navigation
With integration of the surgical microscope
Q8: How often (in percent of navigated surgery) did you estimate the navigation accuracy as not sufficient?
Free text, Arabic numbers in percent requested
Q9: Why don't you use navigation in all cases on a routine basis (multiple answers possible)?
I always use navigation on a routine basis
Insufficient intraoperative support in orientation (“I better get along without it,” “does not help”)
Time consuming
Insufficient accuracy (inaccurate)
Complicated setup
Other reason (free text statement)
References
- 1.Kral F, Puschban E J, Riechelmann H, Freysinger W. Comparison of optical and electromagnetic tracking for navigated lateral skull base surgery. Int J Med Robot. 2013;9(02):247–252. doi: 10.1002/rcs.1502. [DOI] [PubMed] [Google Scholar]
- 2.Komune N, Matsushima K, Matsuo S, Safavi-Abbasi S, Matsumoto N, Rhoton A L., Jr The accuracy of an electromagnetic navigation system in lateral skull base approaches. Laryngoscope. 2017;127(02):450–459. doi: 10.1002/lary.25998. [DOI] [PubMed] [Google Scholar]
- 3.Strauß G, Schaller S, Nowatschin S et al. [Clinical experience with navigation functions for temporal bone surgery: interim result after 40 patients] HNO. 2012;60(12):1115–1121. doi: 10.1007/s00106-012-2558-2. [DOI] [PubMed] [Google Scholar]
- 4.Gharabaghi A, Rosahl S K, Feigel G C, Mirzayan J M, Samii M, Tatagiba M.Impact of image guidance on complication rates and operation time in lateral suboccipital approaches Skull Base 200717(S1):A367 [Google Scholar]
- 5.Kral F, Riechelmann H, Freysinger W. Navigated surgery at the lateral skull base and registration and preoperative imagery: experimental results. Arch Otolaryngol Head Neck Surg. 2011;137(02):144–150. doi: 10.1001/archoto.2010.249. [DOI] [PubMed] [Google Scholar]
- 6.Ledderose G J, Hagedorn H, Spiegl K, Leunig A, Stelter K. Image guided surgery of the lateral skull base: testing a new dental splint registration device. Comput Aided Surg. 2012;17(01):13–20. doi: 10.3109/10929088.2011.632783. [DOI] [PubMed] [Google Scholar]
- 7.Grauvogel T D, Soteriou E, Metzger M C, Berlis A, Maier W. Influence of different registration modalities on navigation accuracy in ear, nose, and throat surgery depending on the surgical field. Laryngoscope. 2010;120(05):881–888. doi: 10.1002/lary.20867. [DOI] [PubMed] [Google Scholar]
- 8.Grauvogel T D, Becker C, Hassepass F, Arndt S, Laszig R, Maier W. Comparison of 3D C-arm-based registration to conventional pair-point registration regarding navigation accuracy in ENT surgery. Otolaryngol Head Neck Surg. 2015;152(02):266–271. doi: 10.1177/0194599814561175. [DOI] [PubMed] [Google Scholar]
- 9.Stelter K, Ledderose G, Hempel J M et al. Image guided navigation by intraoperative CT scan for cochlear implantation. Comput Aided Surg. 2012;17(03):153–160. doi: 10.3109/10929088.2012.668937. [DOI] [PubMed] [Google Scholar]
- 10.Majdani O, Rau T, Weber C, Würfel W, Lenarz T.Intraoperative use of digital volume tomography (DVT) for navigation-assisted resection of the anterior and lateral skull base pathologies J Neurol Surg B Skull Base 201273(S2):A424 [Google Scholar]
- 11.Shi J, Strauss G, Heininger S, Lueth T C. Surgical assistance for instruments' power control based on navigation and neuromonitoring. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:2115–2118. doi: 10.1109/IEMBS.2011.6090394. [DOI] [PubMed] [Google Scholar]
- 12.Rotter N, Schmitz B, Sommer F et al. First use of flat-panel computed tomography during cochlear implant surgery: perspectives for the use of advanced therapies in cochlear implantation. HNO. 2017;65(01):61–65. doi: 10.1007/s00106-016-0213-z. [DOI] [PubMed] [Google Scholar]
- 13.Majdani O, Rau T, Eilers H, Baron S, Lenarz T, Leinung M.Robot-assisted surgery at the lateral skull base Skull Base 200717(S1):A213 [Google Scholar]


