Abstract
BACKGROUND:
Myofascial pain is characterized by the presence of trigger points, tenderness to palpation, and local or referred pain, and commonly involves the pelvic floor muscles in men and women. Pelvic floor myofascial pain in the absence of local or referred pain has also been observed in patients with lower urinary tract symptoms (LUTS), and we have found that many patients report an improvement in these symptoms after receiving myofascial-targeted pelvic floor physical therapy.
OBJECTIVE:
To systematically review the literature for examination techniques used to assess pelvic floor myofascial pain in women.
STUDY DESIGN:
We performed a systematic literature search using strategies for the concepts of pelvic floor disorders, myofascial pain, and diagnosis in Ovid Medline 1946-, Embase 1947-, Scopus 1960-, Cochrane Central Register of Controlled Trials, Database of Abstracts of Reviews of Effects, and Cochrane Database of Systematic Reviews. Articles were screened by three authors and included if they contained a description of a pelvic myofascial physical examination.
RESULTS:
Fifty-five studies met our inclusion criteria. Overall, examination components varied significantly among the included studies and were frequently undefined. A consensus examination guideline was developed based on the available data and includes use of a single digit (62%, 34/55) to perform transvaginal palpation (75%, 41/55) of the levator ani (LA; 87%, 48/55) and obturator internus (OI; 45%, 25/55) muscles with a patient-reported scale to assess the level of pain to palpation (51%, 28/55).
CONCLUSIONS:
Physical examination methods to evaluate pelvic musculature for presence of myofascial pain varied significantly and were often undefined. Given the known role of pelvic floor myofascial pain in chronic pelvic pain and link between pelvic floor myofascial pain and lower urinary tract symptoms, physicians should be trained to evaluate for pelvic floor myofascial pain as part of their physical examination in patients presenting with these complaints. Therefore, the development and standardization of a reliable and reproducible examination is needed.
Keywords: Pelvic floor myofascial pain, physical examination, lower urinary tract symptoms
INTRODUCTION
Myofascial pain arising from the pelvic [levator ani (LA)] and internal hip [obturator internus (OI)] muscles and connective tissue is common in patients with chronic pelvic pain (CPP) and pelvic floor disorder symptoms1–3. It has also been observed in men with chronic prostatitis, men and women with bladder pain syndrome/interstitial cystitis, and women with vulvar pain4. Myofascial pain is characterized by the presence of trigger points1, tenderness to palpation, and local or referred pain4, which can result in debilitating CPP. In one study, 60–85% of patients with CPP reported tenderness upon physical examination of the LA and OI muscles5,6.
Multiple theories exist regarding the etiology of myofascial pain though none have been validated in the literature. One theory suggests that myofascial pain derives from metabolic changes occurring at the level of the motor endplate that causes hyperactivity of the muscle or microscopic muscle damage4. It has also been proposed that myofascial pain involves changes, such as glial cell proliferation and neuronal cell loss, in the central nervous system, which could explain the referred pain patterns seen in myofascial pain pathology7. Finally, the chronic muscle contraction/spasm associated with myofascial pain has been theorized to be a compensatory mechanism for impairments in the levator ani architecture or high functional demands on the pelvic floor4.
Pelvic floor myofascial pain in the absence of local or referred pain has also been observed in patients with lower urinary tract symptoms (LUTS) and other pelvic floor disorders like pelvic organ prolapse2,3,5,8. Preliminary data from our institution also support a correlation between the presence of myofascial pain in the LA and OI muscles and the degree of lower urinary tract symptom bother9,10. We have found that these patients often report significant improvement in their LUTS after receiving myofascial-targeted pelvic floor physical therapy. As the possibility of an association between subclinical pelvic floor myofascial pain (i.e. pelvic floor myofascial pain identified on physical examination but not associated with symptomatic pelvic pain) and LUTS has received little study to date, few physicians may be trained to assess pelvic floor myofascial pain in the differential diagnosis for patients presenting with these symptoms. LUTS and other visceral symptoms are often attributed solely to the end organ (bladder, bowel, uterus, and ovaries) and the pelvic floor muscles are not explored.
Unfortunately, a standardized and reproducible protocol for assessing LA and OI myofascial pain does not currently exist, and few providers evaluate for pelvic floor myofascial pain even in patients presenting with pelvic pain. Considering the growing evidence correlating myofascial pain with chronic pelvic pain syndromes and emerging data suggesting a link between subclinical myofascial pain and LUTS, as well as the availability of myofascial-targeted therapies, a thorough and evidence based physical examination for myofascial pain is necessary. As we are primarily interested in further understanding the relationship between pelvic floor myofascial pain and LUTS in patients who may seek care from general or subspecialist gynecologists, we sought examination strategies for the assessment of myofascial pain in adult women. Furthermore, although some components of the pelvic floor myofascial examination may be similar in males and females, the approach to access these muscles is different so we chose to focus on examination strategies in women for this systematic review. This will both aid in assessment of and guide treatment for patients presenting with pelvic floor symptoms including pelvic pressure, heaviness, and lower urinary tract symptoms. The objective of our study is to systematically review the literature on examination techniques for the diagnosis of LA and OI myofascial pain in women.
MATERIALS AND METHODS
A comprehensive literature search was performed using strategies created by a medical librarian for the concepts of pelvic floor disorders, myofascial pain, and diagnosis using the following terms for: 1) pelvic floor disorders: “pelvic floor disorders,” “disorders of the pelvic floor,” “pelvic floor dysfunctions,” “dysfunctions of the pelvic floor,” “pelvic floor diseases,” “diseases of the pelvic floor,” and “syndrome of the pelvic floor”; 2) myofascial pain: “myofascial pain syndromes,” “spasm,” “trigger points,” “pain,” “ache,” “myalgia,” “chronic pain,” “myofascial pain,” “painful defecation,” “dysuria,” “pelvic girdle pain,” “pelvic pain,” “perineal pain,” “postoperative pain,” “vaginal pain,” “vulvodynia,” “muscle spasm,” “myofascial syndrome,” “muscle soreness,” “muscle tenderness,” and “pelvic pain syndrome”; and 3) assessment methodology: “diagnosis,” “differential diagnosis,” “sensitivity and specificity,” “physical examination,” “evaluation,” and “assessment”. Studies containing any of the terms for all three concepts (pelvic floor disorders, myofascial pain, and assessment) were captured and reviewed for eligibility. These strategies were implemented in Ovid Medline 1946-, Embase 1947-, Scopus 1960-, Cochrane Central Register of Controlled Trials, Database of Abstracts of Reviews of Effects, and Cochrane Database of Systematic Reviews. We reviewed the references of the identified studies to add any additional relevant studies.
All searches were completed in June 2017 and results were exported to EndNote. The full strategies for Ovid Medline, Embase, Cochrane Library, and Scopus are available in the supplementary material. We defined the following inclusion criteria: 1) adults (>18 years), 2) majority female (>50% of study population), and 3) studies reporting a description of the pelvic floor myofascial examination.
The results of the systematic search were screened independently by two authors (MM, NS) and were included if there was any mention of a pelvic examination used to assess pelvic muscle pain. The resulting studies were then reviewed thoroughly and independently by three authors (MM, NS, JL) and were included if they met the aforementioned inclusion criteria. All study designs that included a pelvic floor myofascial pain examination as part of their protocol were included. Articles were excluded if they exclusively reported on children/adolescents, males constituted more than 50% of the studied population, or the study described pelvic pain in the setting of a known mesh complication. In the event of a disagreement, the authors reviewed the study together and came to a consensus regarding whether it satisfied criteria for inclusion. Data extracted from included studies were study design, year of publication, study objective, inclusion criteria, exclusion criteria, concomitant pelvic floor disorders, primary diagnosis, diagnostic tools utilized, measured outcomes and results, and specific characteristics of the physical examination. Data extraction was performed in duplicate by two authors (MM, NS) independently. Disagreements were resolved through discussion and consensus. From these data, a recommended examination sequence was developed that incorporated components when used by multiple studies. In the event that examination components differed among included studies, the component cited in the majority of the studies was selected for inclusion in the recommended examination sequence. In order to assess the quality of examination descriptions and procedures, a scoring system was developed whereby studies were given one point for each key examination component reported in the study. The conduct and reporting of this systematic review closely adhered to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. This study was prospectively registered with PROSPERO (registration number CRD42017073701) and was exempt from IRB review.
RESULTS
The initial search identified 5,112 publications, 2,075 of which were duplicates: 1,823 removed by the automatic duplicate finder in EndNote and 252 duplicates removed by a medical librarian. We screened the resulting 3,037 publications and excluded 2,633 based on predefined inclusion and exclusion criteria, resulting in 404 full-text articles reviewed. As very few of these studies were performed to evaluate the pelvic floor myofascial examination itself, but instead used this examination as part of their research protocol for other study goals, we included all article types(from randomized controlled trials to expert opinion and review articles) to capture as many examination descriptions as possible. This resulted in a total sample size of 55 studies, including 9460 patients of which 9437 (99.8%) were women (Table 1, Figure 1).
Table 1.
Physical examination characteristics of studies that assessed pelvic myofascial pain in adult women, published 1997–2017.
| Reference | Study Type | Patient Position | Route | Digits | Clock-face orientation (Y/N) | Order of exam specified (Y/N) | Palpation technique | Vaginal algometer (Y/N) | Pain scale | Strength Assessment (Y/N) |
|---|---|---|---|---|---|---|---|---|---|---|
| Carrico et al, 200811 | RCT | NS | TV | 1 | N | N | S | N | 0–10, VAS | N |
| Fitzgerald et al, 200912 | RCT | NS | NS | NS | N | N | NS | N | None | N |
| De Souza Montenegro et al, 2010b13 | PC | DL | TV | 1 | N | N | NS | N | 0–2*, NRS | N |
| Lamvu et al, 201514 | PC | DL | TV | 1 | Y | Y | S | N | 0–10, VAS | Y |
| Langford et al, 200715 | PC | DL | TV | 1 | N | Y | L | N | 0–100, VAS | N |
| Morrissey et al, 201516 | PC | NS | TV | 1 | N | N | NS | N | 0–4, NRS | Y |
| Oyama et al, 200417 | PC | NS | NS | NS | N | N | NS | N | 0–4, NRS | N |
| Sillem et al, 201618 | PC | DL | TV | 1 | N | N | NS | N | None | N |
| Adelowo et al, 201319 | RC | NS | TV | 1 | N | N | NS | N | 0–10, NRS | N |
| Bassaly et al, 201120 | RC | NS | NS | NS | N | N | NS | N | 0–10, VAS | N |
| Bedaiwy et al, 201321 | RC | NS | TV | NS | N | N | NS | N | 0–10, NRS | N |
| Bendana et al, 200922 | RC | DL | TV | 2 | Y | Y | L | N | None | N |
| Goetsch, 200723 | RC | NS | TV | NS | N | N | NS | N | None | N |
| Dos Bispo et al, 201624 | CC | DL | TV | 1 | N | Y | NS | N | None | Y |
| Williams et al, 201525 | CC | NS | NS | NS | N | N | NS | N | 0–10, NRS | N |
| Zolnoun et al, 201226 | CC | NS | TV | 1 | Y | Y | S | Y | None | N |
| Kavvadias et al, 201327 | CS | DL | TV | 1 | N | Y | S | N | 0–10, VAS | Y |
| Fenton et al, 201328 | CS | DL | TV | 1 | Y | Y | S | Y | 0–10, NRS | N |
| Peters et al, 200729 | CS | NS | NS | NS | N | N | S | N | 0–10, VAS | N |
| Phillips et al, 201630 | CS | NS | TV | NS | N | N | S | N | 0–10, NRS | N |
| Adams et al, 20132 | CS | NS | NS | NS | N | N | NS | N | None | N |
| Adams et al, 201431 | CS | NS | NS | NS | N | N | NS | N | None | Y |
| Bhide et al, 201532 | CS | DL | TV | 1 | N | N | S | N | 1–10, VAS | N |
| De Souza Montenegro et al, 2010a33 | CS | DL | TV | 1 | N | N | NS | N | 0–2*, NRS | N |
| Fitzgerald et al, 201134 | CS | DR | TV | 1 | Y | N | L | N | None | Y |
| Hellman et al, 201535 | CS | NS | TV | NS | N | N | S | Y | 0–10, NRS | N |
| Loving et al, 201436 | CS | DL | TV | 1 | Y | N | S | Y | 0–10, NRS | Y |
| Peters et al, 200837 | CS | NS | TV | NS | N | N | S | N | 0–10, VAS | N |
| Tu et al, 200738 | CS | DL | TV | 1 | Y | N | S | N | None | N |
| Tu et al, 2008a39 | CS | DL | TV | 1 | Y | N | L | N | 0–3*, NRS | Y |
| Tu et al, 2008b40 | CS | DL | TV | 1 | Y | N | S | Y | 0–100, NRS | Y |
| Tu et al, 200641 | CS | NS | TV | 1 | N | N | NS | N | 0–10, VAS | N |
| Witzeman et al, 201542 | CS | NS | TV | 1 | N | Y | S | Y | None | N |
| Yong et al, 201443 | CS | NS | NS | 1 | N | N | NS | N | A/M/M/S | N |
| Reissing et al, 200544 | CS | NS | Both | 1/2 | Y | Y | S | N | None | Y |
| Albrecht et al, 201545 | EO | NS | TV | 1 | N | Y | L | N | None | Y |
| Pastore & Katzman, 20123 | EO | SHL | TV | 1 | Y | Y | S | N | None | N |
| Sarton, 201046 | EO | NS | TV | 1 | N | Y | L | N | None | N |
| Steege, 199747 | EO | NS | TV | 1 | Y | Y | S | N | None | N |
| Haylen et al, 201048 | EO | NS | TV | NS | N | N | S | N | None | Y |
| Messelink et al, 200549 | EO | DLƚ | NS | NSƚƚ | N | N | NS | N | None | Y |
| Apte et al, 201250 | R | SHL | Both | 1 | Y | Y | NS | N | None | Y |
| Aredo et al, 201751 | R | NS | NS | 1 | N | N | L | N | None | N |
| Butrick, 200952 | R | NS | TV | 1 | N | N | NS | N | None | Y |
| Faubion et al, 201253 | R | NS | Both | 2 | N | N | NS | N | None | Y |
| Fitzgerald & Kotarinos, 200354 | R | NS | TV | NS | N | Y | L | N | 0–10, NRS | Y |
| Gyang et al, 201355 | R | NS | TV | 1 | Y | Y | S | N | None | Y |
| Hartmann, 201056 | R | NS | TV | 1 | N | N | NS | N | None | Y |
| Peters & Carrico, 200657 | R | NS | TV | 1 | Y | N | S | N | 0–10, VAS | N |
| Prather & Camacho-Soto, 201458 | R | NS | NS | 1 | N | N | NS | N | None | Y |
| Prather et al, 200759 | R | NS | NS | NS | N | Y | NS | N | None | Y |
| Prather et al, 200960 | R | NS | Both | NS | Y | N | S/L | N | None | Y |
| Prendergast & Weiss, 200361 | R | DL | Both | 1 | N | N | NS | N | None | Y |
| Spitznagle, 20144 | R | NS | NS | NS | N | N | NS | Y | None | N |
| Vercellini et al, 200962 | R | NS | Both | 1 | N | N | NS | N | None | N |
CC, case-control; CS, cross-sectional; PC, prospective cohort; RCT, randomized controlled trial; RC, retrospective cohort; EO, expert opinion; R, review; DL, dorsal lithotomy; DR, dorsal recombinant; SHL, supine hook-lying; NS, not specified; 1, single digit; 2, two digits; 1/2 choice of 1 or 2 digits; S, single site within the muscle; L, along the length of the muscle belly; TV, transvaginal; TR, transrectal; Y, yes; N, no; NRS, numeric rating scale; VAS, visual analogue scale; A/M/M/S, absent, mild, moderate, or severe.
Three studies used physician-reported scales rather than patient-reported.
Figure 1:
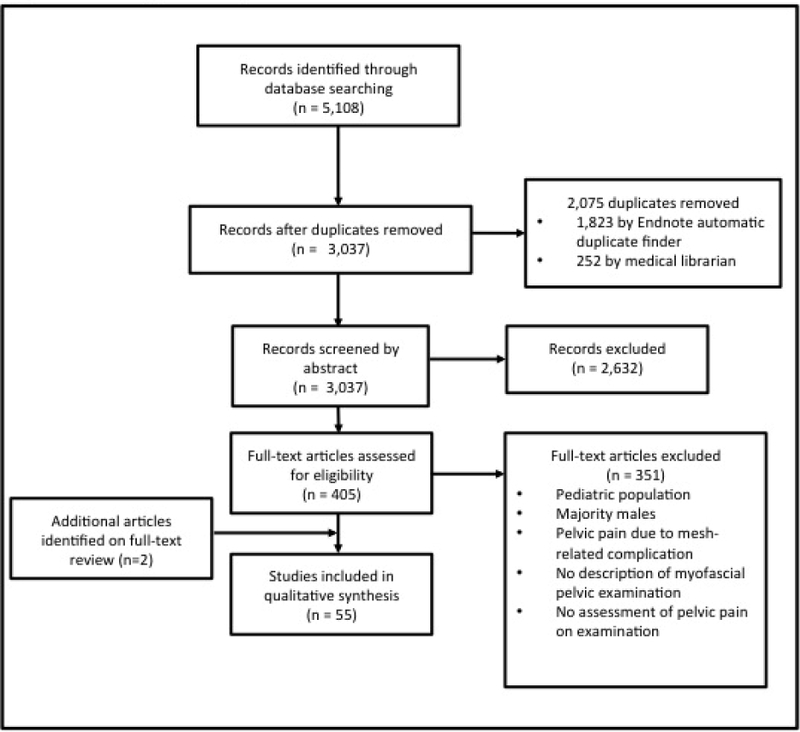
PRISMA diagram for study selection
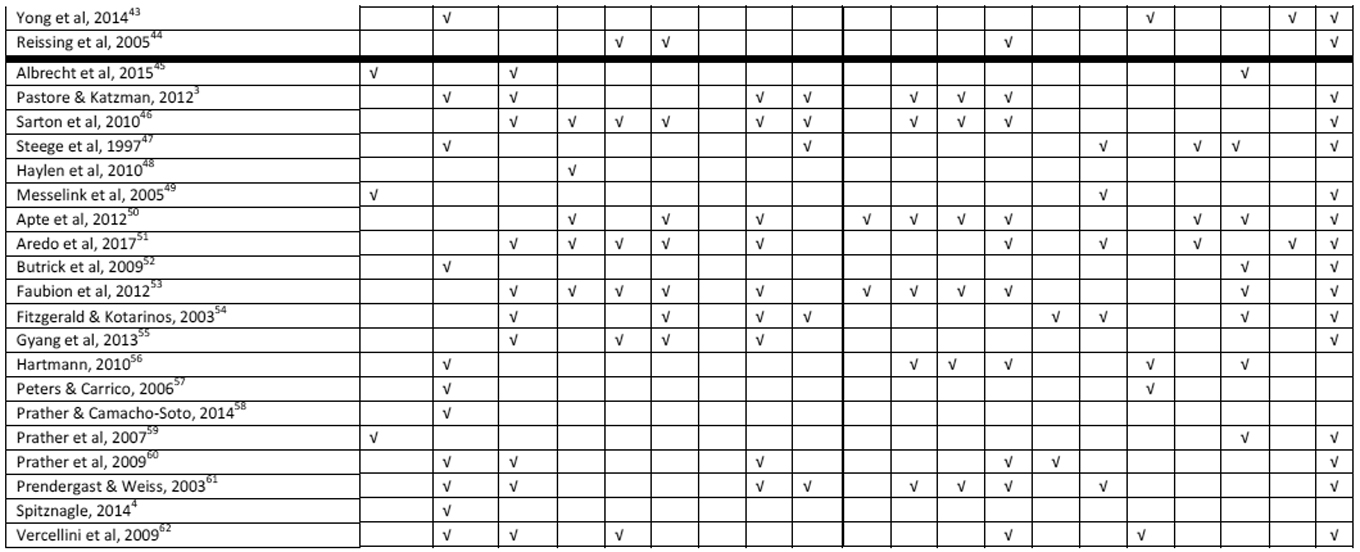
Of the 55 included studies, examination technique details were extracted from two randomized controlled trials, six prospective cohort studies, eight retrospective cohort and case-control studies, 19 cross sectional studies, and 20 general review articles or expert opinion pieces (Table 1). There were no systematic reviews. Objectives of the included studies varied widely with 11 testing an intervention, 21 reporting on diagnostic criteria/pathology, and 23 evaluating findings/symptoms upon examination. Only two of the 55 included manuscripts, only two studied the examination itself. One study defined terminology for investigators studying and reporting pelvic floor muscle evaluation, and specified that patient positioning and number of digits used in palpation should be reported49.
The level of detail for included examination components varied greatly among the studies. Most (49/55, 89.0%) did not document counseling or consent prior to beginning the pelvic examination. Likewise, the majority of studies did not describe the position of the patient during the examination. Only 19/55 (34.5%) reported patient positioning, and of those, the majority (15/19, 78.9%) were dorsal lithotomy. Many studies (13/55; 23.6%) did not describe whether the examination was approached transvaginally or transrectally. The majority that did specify route suggested using a transvaginal examination (36/42, 85.7%). No studies included an isolated transrectal approach, but six (14.3%) recommend both transvaginal and transrectal approaches for the complete examination. Most authors used a single digit for palpation (34/55, 61.8%), but many (19/55,34.5%) did not specify the number of digits to use on palpation, and most (38/55, 69.1%) did not explicitly mention use of gloves or lubrication.
The majority of studies (39/55, 70.9%) lacked a description of the method used to orient the examiner to the relevant muscles (Table 1). Of the 16 studies that did describe a specific method for orientation, all (16/16, 100%) used the clock-face method with the introitus at the center, the pubic bone at 12 o’clock and the anus at 6 o’clock.
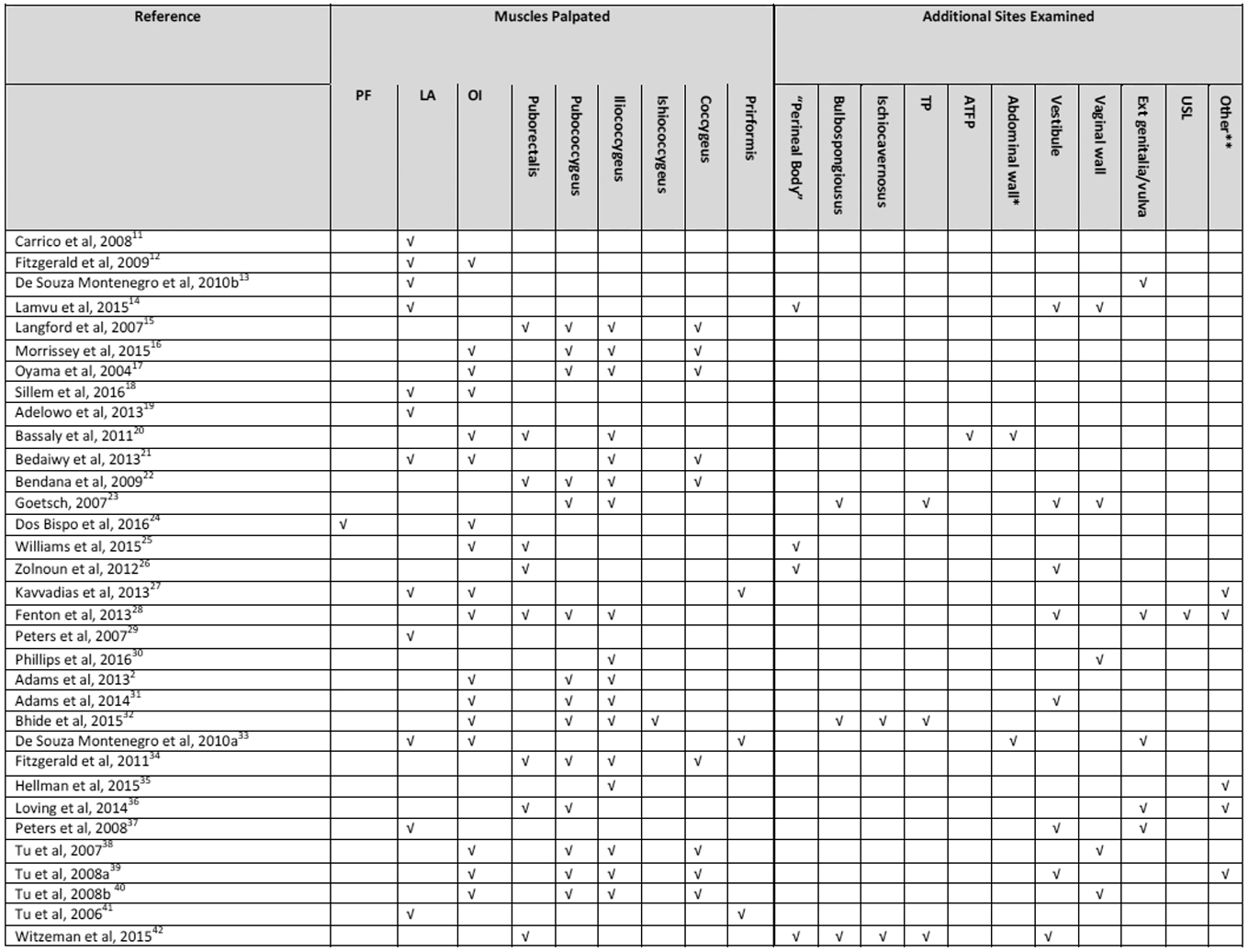
Among the included studies, there was a general agreement that the LA should be examined in some capacity (48/55, 87.3%), but the inclusion of the OI, piriformis, and other sites was variable (Table 2). Less than half (27/55, 49.1%) specified whether the OI should be included in the examination, and seven (12.7%) included palpation of the piriformis. Nearly one-third of the studies (17/55, 30.9%) recommended palpating the LA muscles only or did not specify any particular muscle sites beyond “pelvic floor muscles”. Of the studies that recommended examination of the LA muscles, some suggested palpation of the LA in general (23/55, 41.8%) whereas others specified which muscular components of the LA should be identified and palpated (28/55, 50.9%). Additionally, studies differed in the order and method of palpation of the various pelvic floor muscles. Only 17/55 studies (30.9%) recommended a preferred order of palpation. Of those, 6 (35.3%) described muscle palpation beginning with the superficial muscles (bulbospongiosus, ischiocavernosus, and superficial transverse perineal muscles) then proceeding to the deeper muscles (pubococcygeus, iliococcygeus, and coccygeus). Twenty-six out of 55 studies (47.3%) lacked instruction on the technique of palpating muscles, specifically, whether the muscle should be palpated at an isolated location or along the length of the muscle. Of the 29 studies that did specify a technique, the majority (20/29, 69.0%) recommended palpation of an isolated location.
Table 2.
Sites designated as part of the physical examination in studies that assessed pelvic myofascial pain in adult women, published 1997–2017.
 |
 |
PF, pelvic floor; LA, levator ani; OI, obturator internus; TP, transverse perineal muscles; ATFP, arcus tendineus fascia pelvis; USL, uterosacral ligament.
Abdominal wall includes rectus abdominis.
Other sites examined include the adnexa28,47,52, bladder and urethra27,35,43,51,52,55,58,62 anorectal raphae35, anus/rectum36,44,50,53,55,59,60, pelvis39, buttock39, sacroiliac joint39,55, Iliopsoas39, hamstring39, hip flexor39, and coccyx44,50,59,60, sphincter urethra and compressor urethra3,46, cervix47,52,53, adductor muscles49, clitoris50, pubovaginalis50,54 , uterus51, sacrococcygeus ligaments53,59,60, urogenital triangle53, quadratus lumborum54,61, gluteal muscles49,54,59,61, pubic symphysis55,59,60, anterior superior iliac spines55, iliopsoas61, anal sphincter60,61,62.
There was also variation in the use of instruments to standardize pressure and measure pain/pressure thresholds. Most studies (49/55, 89.1%) did not attempt to standardize the amount of pressure applied to muscle. More recent studies (6/55, 10.9%) incorporated vaginal pressure algometers in an effort to increase inter-rater reliability and define pain/pressure thresholds (Table 1).
Twenty-eight studies (50.9%) assessed pain on palpation of the pelvic floor muscles as part of the physical examination, and most 17 (60.7%) used a 0–10 patient-reported scale (0–10; 0=None, 1–3=mild pain, 4–6=moderate pain, and 7–10= severe pain; Table 1). Additional sites that were often examined included external genitalia, vestibule, urethra, bladder, anus, abdomen, and vaginal wall. Twenty-three articles (41.8%) also included evaluation of pelvic floor musculature strength in addition to pelvic pain.
Table 3 outlines our recommended examination sequence based on the little consensus reported in the literature. The recommended examination includes counseling for the patient prior to the examination, identifying muscle location based on a clock-face method, palpating muscles at single sites mid-muscle belly using a single digit, and quantifying self-reported pain upon palpation using a 0–10 validated scale (0–10; 0=No pain, 1–3=Mild pain, 4–6=Moderate pain, and 7–10=Severe pain). Specifically, muscle palpation should include the bilateral LA and OI muscles, and trigger points should be noted. A vaginal pressure algometer can be considered in an attempt to standardize pressure applied on examination. Visual inspection and observation of the function of the pelvic floor should occur throughout the examination.
Table 3:
Recommended Structure for Physical Examination of Pelvic Myofascial Pain
| Examination Method | Supporting References |
|---|---|
| 1) Provide counseling to patient about the pelvic examination process. Explain thoroughly the steps that are a part of the examination and pay particular attention in trying to ease the fear and hesitancy that the patient may have. Finally obtain consent to begin physical examination. | 6/55 studies documented counseling and/or consent of patient prior to start of physical examination |
| 2) Ask patient to sit in the lithotomy position for examination | 14/55 studies used the lithotomy position for examination of pelvic musculature |
| 3) Begin the unidigital transvaginal examination by inserting a gloved, lubricated index finger into the vaginal introitus | 34/55 studies palpated muscles with single digit Of these, 19/34 studies palpated muscles with palmar side of the index finger |
| 42/55 studies performed a transvaginal exam for the pelvic musculature | |
| 17/55 studies explicitly mentioned gloving and/or lubrication of examining digit | |
| 4) Utilize clock face orientation with the pubic symphysis at 12 o clock and the anus at 6 o clock to localize pelvic floor muscles | 16/55 studies utilized clock face orientation to locate pelvic floor muscles |
| 5) Start with unidigital palpation of superficial pelvic floor musculature and then proceed to deep pelvic floor musculature. | 17/55 studies specified order for pelvic muscle palpation Of these, 6/17 studies started with superficial PFM and then moved to deep PFM palpation |
| 6) Use the following clock face positions to palpate the superficial and then deep PFM. | |
| Superficial Layer: Bulbospongiosus (2 and 10 o clock), Ischiocavernosus (1 and 11 o clock), Superficial transverse perineal muscles (3 and 9 o clock) | Number of studies that assessed superficial muscles: bulbospongiosus (12/55), ischiocavernosus (9/55), superficial transverse perineal muscles (13/55) |
| Deep Layer: Pubococcygeus (7 and 11 o clock for left side; 1 and 5 o clock for right side), Iliococcygeus (4 and 8 o clock), Coccygeus (5 and 7 o clock; requires deeper digital insertion) | Number of studies that assessed deep muscles: pubococcygeus (22/55), iliococcygeus (24/55), coccygeus (18/55), unspecified levator ani (25/55) |
| 7) Then palpate obturator internus at 2 and 10 o clock | 25/55 studies palpated obturator internus for tenderness Of these, 5/25 studies specified palpating obturator internus after palpating pelvic floor muscles |
| 8) During palpation, apply pressure to specific sites predefined on each of the pelvic floor muscles and obturator internus. Consider vaginal pressure algometer to standardize amount of pressure being applied to each site. | 21/55 studies used site specific palpation and did not palpate along length of muscle |
| 6/55 studies used a vaginal pressure algometer | |
| 9) Use a graded scale (either NRS or VAS) to assess patient reported pain after palpation of each site | 28/55 studies used patient reported scores to assess muscle tenderness |
| 25/55 studies used graded scale to assess muscle tenderness | |
| 9/55 studies used visual analogue scale and 15/55 studies use numerical rating scale | |
| 10) Additional items that can be included in examination: | |
| external genitalia, vestibule, urethra, bladder, anus, abdomen, vaginal wall | 31/55 studies that assessed additional non-muscular sites for tenderness |
| strength of pelvic floor musculature | 23/55 studies evaluated the strength of the pelvic floor musculature |
We assessed study quality based on whether or not studies reported eight key examination components. Studies were given one point for each key component reported and were then ranked by score with higher scores representing “higher quality” studies (Table 4). Only one study reported all 8 key components while three studies did not report any of the key components.
Table 4.
Assessment of the quality of pelvic floor myofascial pain examination descriptions among studies included in the systematic review.
| Reference | Patient Position | Route | Single or double digit palpation | Orientation to identify muscles | Order of exam | Palpation technique | Pain scale | Strength Assessment | Score (8 max) |
|---|---|---|---|---|---|---|---|---|---|
| Lamvu et al, 201514 | X | X | X | X | X | X | X | X | 8 |
| Kavvadias et al, 201327 | X | X | X | X | X | X | X | 7 | |
| Fenton et al, 201328 | X | X | X | X | X | X | X | 7 | |
| Loving et al, 201436 | X | X | X | X | X | X | X | 7 | |
| Tu et al, 2008a39 | X | X | X | X | X | X | X | 7 | |
| Tu et al, 2008b40 | X | X | X | X | X | X | X | 7 | |
| Langford et al, 200715 | X | X | X | X | X | X | 6 | ||
| Bendana et al, 200922 | X | X | X | X | X | X | 6 | ||
| Fitzgerald et al, 201134 | X | X | X | X | X | X | 6 | ||
| Reissing et al, 200544 | X | X | X | X | X | X | 6 | ||
| Pastore & Katzman, 20123 | X | X | X | X | X | X | 6 | ||
| Apte et al, 201250 | X | X | X | X | X | X | 6 | ||
| Gyang et al, 201355 | X | X | X | X | X | X | 6 | ||
| Dos Bispo et al, 201624 | X | X | X | X | X | 5 | |||
| Zolnoun et al, 201226 | X | X | X | X | X | 5 | |||
| Bhide et al, 201532 | X | X | X | X | X | 5 | |||
| Albrecht et al, 201545 | X | X | X | X | X | 5 | |||
| Tu et al, 200738 | X | X | X | X | X | 5 | |||
| Steege, 199747 | X | X | X | X | X | 5 | |||
| Fitzgerald & Kotarinos, 20 0354 | X | X | X | X | X | 5 | |||
| Peters & Carrico, 20 0657 | X | X | X | X | X | 5 | |||
| Morrissey et al, 201516 | X | X | X | X | 4 | ||||
| Carrico et al, 200811 | X | X | X | X | 4 | ||||
| De Souza Montenegro et al, 2010b13 | X | X | X | X | 4 | ||||
| De Souza Montenegro et al, 2010a33 | X | X | X | X | 4 | ||||
| Witzeman et al, 201542 | X | X | X | X | 4 | ||||
| Sarton, 201046 | X | X | X | X | 4 | ||||
| Prather et al, 200960 | X | X | X | X | 4 | ||||
| Prendergast & Weiss, 20 0361 | X | X | X | X | 4 | ||||
| Sillem et al, 201618 | X | X | X | 3 | |||||
| Adelowo et al, 201319 | X | X | X | 3 | |||||
| Phillips et al, 201630 | X | X | X | 3 | |||||
| Hellman et al, 201535 | X | X | X | 3 | |||||
| Peters et al, 200837 | X | X | X | 3 | |||||
| Tu et al, 200641 | X | X | X | 3 | |||||
| Haylen et al, 201048 | X | X | X | 3 | |||||
| Butrick, 200952 | X | X | X | 3 | |||||
| Faubion et al, 201253 | X | X | X | 3 | |||||
| Hartmann, 201056 | X | X | X | 3 | |||||
| Bedaiwy et al, 201321 | X | X | 2 | ||||||
| Peters et al, 200729 | X | X | 2 | ||||||
| Yong et al, 201443 | X | X | 2 | ||||||
| Messelink et al, 200549 | X | X | 2 | ||||||
| Aredo et al, 201751 | X | X | 2 | ||||||
| Prather & Camacho-Soto, 201458 | X | X | 2 | ||||||
| Prather et al, 20 0759 | X | X | 2 | ||||||
| Vercellini et al, 200962 | X | X | 2 | ||||||
| Oyama et al, 200417 | X | 1 | |||||||
| Bassaly et al, 201120 | X | 1 | |||||||
| Goetsch, 200723 | X | 1 | |||||||
| Williams et al, 201525 | X | 1 | |||||||
| Adams et al, 201431 | X | 1 | |||||||
| Adams et al, 20132 | 0 | ||||||||
| Spitznagle, 20144 | 0 | ||||||||
| Fitzgerald et al, 200912 | 0 |
Studies received one point for each examination component specified in the description of the examination. Studies with the highest scores included the most specific examination description and were judged to be of higher quality of examination reporting.
CONCLUSIONS
Despite the prevalence of pelvic floor myofascial pain in patients with CPP, no standardized protocol for the physical examination of myofascial pelvic pain currently exists. Findings from this systematic review illustrate that techniques for pelvic myofascial examination vary significantly and commonly are poorly defined among both investigational studies and clinical reviews. Furthermore, the overall level of evidence to guide standardization of a pelvic myofascial examination is poor. As a result, it is difficult to draw conclusions about the best methods to execute the myofascial pelvic pain examination, but here we recommend an examination sequence based upon the limited consensus within the literature to date.
As with all systematic reviews, this review is limited by the quality of the studies available for inclusion. Very few studies evaluated the examination itself, and no studies tested the validity or reproducibility of the examination for pelvic floor myofascial pain. Additionally, very few studies utilized vaginal pressure algometers or other methods to standardize the pressure applied during palpation, or consistent anatomic landmarks for identification of the ideal sites for palpation are lacking. Finally, as no quality appraisal tool exists to evaluate pelvic floor (or other) myofascial pain examination techniques, we had to generate an informal tool based on key examination components. This tool assigned points to studies based on whether or not key components were included within the examination description.
Despite the aforementioned limitations, we believe the common elements of previous examinations – i.e., our consensus-based guidelines – provide a good foundation upon which to build an evidence-based protocol for the assessment of pelvic myofascial pain. Going forward, these examination elements should be tested and validated as reliable indicators of the presence and severity of pelvic floor myofascial pain in women. A standardized, evidence-based examination protocol is necessary to reduce misclassification as investigators begin studying the association between pelvic floor myofascial pain and other pelvic floor disorders like CPP and LUTS. Clinically, a standardized pelvic floor myofascial examination will improve the identification of patients with pelvic floor myofascial pain as a contributing factor in their CPP, LUTS, or other pelvic floor disorder symptoms and who may benefit from myofascial-targeted therapies. Once this evidence-based, standardized examination is established, efforts can then turn to promoting physician education regarding the importance of assessing pelvic floor myofascial pain in women presenting with pelvic floor disorder symptoms.
Acknowledgements
The authors would like to acknowledge Michelle Doering for her assistance with development of the systematic literature search strategy and implementation.
Dr. Meister is supported by an NIH Reproductive Epidemiology Training Grant (T32HD055172–08) and a Clinical and Translational Science Award held at Washington University in St. Louis (UL1 TR002345).
Appendix
PICO Question: What evidence-based examination strategies exist in the literature for the assessment of pelvic floor myofascial pain in adult women?
P (patients): Adult women
I (intervention): Examination strategies
C (comparison, optional): none
O (outcome): diagnosis/assessment of pelvic floor myofascial pain
Complete Search Strategy
Ovid Medline
06/06/17
929 results
(Exp Pelvic Floor Disorders/OR “pelvic floor disorder”.mp. OR pelvic floor disorders.mp. OR disorder of the pelvic floor.mp. OR disorders of the pelvic floor.mp. OR myofascial pelvic pain syndrome.mp. OR pelvic floor dysfunction.mp. OR pelvic floor dysfunctions.mp. OR dysfunctions of the pelvic floor.mp. OR dysfunction of the pelvic floor.mp. OR pelvic floor disease.mp. OR pelvic floor diseases.mp. OR diseases of the pelvic floor.mp. OR pelvic floor syndrome.mp. OR pelvic floor syndromes.mp. OR syndromes of the pelvic floor.mp. OR syndrome of the pelvic floor.mp. OR (myofascial adj2 (pelvic OR pelvis)).mp. OR Exp Pelvic Floor/OR (pelvi* adj3 (floor or levator or diaphragm* OR coccygeus)).mp. AND (Exp Pain/OR Exp myofascial pain syndromes/OR Exp Spasm/OR Exp Trigger Points/OR (trigger adj1 (point* or area*)).mp. OR spasm*.mp. OR pain*.mp. or ache*.mp. or myalgia*.mp. OR (muscle adj1 (soreness or tenderness)).mp.) OR (exp myofascial pain syndromes/or myofascial pain syndromes.mp. or myofascial pain syndrome.mp.) and (pelvis.mp. or pelvic.mp.) OR (pelvic pain syndrome.mp. AND (myalgia.mp. OR myofascial.mp.)) AND (Exp diagnosis/or Exp differential diagnosis/or Exp “Sensitivity and specificity”/or (sensitivity adj2 specificity).mp. or Exp Physical examination/or exam*.mp. or Diagnos*.mp. OR diagnosis.fs. OR symptom*.mp. OR evaluat*.ti. OR evaluat*.ab. or assessment*.mp. OR map*.mp.)) not (exp Male/not (exp Female/and exp Male/))
Embase
06/06/17
2,417 results
'pelvic floor disorder'/exp OR 'pelvic floor disorder' OR 'pelvic floor disorders' OR 'disorder of the pelvic floor' OR 'disorders of the pelvic floor' OR 'pelvic floor dysfunction':ti,ab,de OR 'pelvic floor dysfunctions' OR 'dysfunctions of the pelvic floor' OR 'dysfunction of the pelvic floor' OR 'pelvic floor disease' OR 'pelvic floor diseases' OR 'diseases of the pelvic floor' OR 'pelvic floor syndrome' OR 'pelvic floor syndromes' OR 'syndromes of the pelvic floor' OR 'syndrome of the pelvic floor' OR myofascial NEAR/2 pelvic OR myofascial NEAR/2 pelvis OR 'pelvis floor'/exp OR (pelvi* NEAR/3 (floor OR levator OR diaphragm* OR coccygeus)):ti,ab,de AND ('pain'/de OR 'abdominal pain'/de OR 'cystalgia'/de OR 'inflammatory pain'/exp OR 'inguinal pain'/exp OR 'myalgia'/exp OR 'chronic pain'/de OR 'myofascial pain'/exp OR 'painful defecation'/exp OR 'dysuria'/exp OR 'pelvic girdle pain'/exp OR 'pelvic pain'/exp OR 'perineal pain'/exp OR 'postoperative pain'/exp OR 'vaginal pain'/exp OR 'vulvodynia'/exp OR 'muscle spasm'/exp OR 'trigger point'/exp OR 'myofascial syndrome' OR trigger NEAR/1 (point* OR area*) OR spasm* OR pain*:ti,ab OR ache* OR myalgia* OR muscle NEAR/1 (soreness OR tenderness)) OR (‘myofascial pain syndrome’:ti,ab AND (‘pelvis’:ti,ab,de OR ‘pelvic’:ti,ab,de)) OR ('pelvis pain syndrome'/exp AND (myalgia OR myofascial)) AND ('diagnosis'/exp OR 'differential diagnosis'/exp OR 'sensitivity and specificity'/exp OR 'physical examination'/exp OR exam*:ti,ab,de OR diagnos*:ti,ab,de OR symptom*:ti,ab,de OR evaluat*:ti,ab,de OR assessment*:ti,ab,de OR map*:ti,ab,de) NOT ('male'/exp NOT ('female'/exp AND 'male'/exp))
Cochrane Library
06/06/17
Cochrane Database of Systematic Reviews– 135 results
Cochrane Central Register of Controlled Trials – 11 results
Database of Abstracts of Reviews of Effect – 206 results
(((([mh “Pelvic Floor Disorders”] or “pelvic floor disorder” or “pelvic floor disorders” or “disorder of the pelvic floor” or “disorders of the pelvic floor” or “myofascial pelvic pain syndrome” or “pelvic floor dysfunction” or “pelvic floor dysfunctions” or “dysfunctions of the pelvic floor” or “dysfunction of the pelvic floor” or “pelvic floor disease” or “pelvic floor diseases” or “diseases of the pelvic floor” or “pelvic floor syndrome” or “pelvic floor syndromes” or “syndromes of the pelvic floor” or “syndrome of the pelvic floor” or (myofascial near/2 (pelvic OR pelvis)) OR [mh “Pelvic Floor”] or (pelvi* near/3 (floor or levator or diaphragm* or coccygeus)))
AND
([mh Pain] or [mh “myofascial pain syndromes”] or [mh Spasm] or [mh “Trigger Points”] or (trigger near/1 (point* or area*)) or spasm* or pain* or ache* or myalgia* or (muscle near/1 (soreness or tenderness))))
OR ([mh “myofascial pain syndromes”] AND (pelvis OR pelvic)) or (“pelvic pain syndrome” AND (myalgia OR myofascial)))
and
([mh diagnosis] or [mh “differential diagnosis”] or [mh “Sensitivity and specificity”] or (sensitivity near/2 specificity) or [mh “Physical examination”] or exam* or Diagnos* or [mh diagnosis/ae] or symptom* or evaluat*.ti,ab. or assessment* or map*.ti,ab.))
not ([mh Male] not ([mh Female] and [mh Male]))
Scopus
06/09/17
1,380 results
(((((TITLE-ABS-KEY (“pelvic floor disorder”)) OR (TITLE-ABS-KEY (“pelvic floor disorders”)) OR (TITLE-ABSKEY (“disorder of the pelvic floor”)) OR (TITLE-ABS-KEY (“disorders of the pelvic floor”)) OR (TITLE-ABS-KEY (“myofascial pelvic pain syndrome”)) OR (TITLE-ABS-KEY (“pelvic floor dysfunction”)) OR (TITLE-ABS-KEY (“pelvic floor dysfunctions”)) OR (TITLE-ABS-KEY (“dysfunctions of the pelvic floor”)) OR (TITLE-ABS-KEY (“dysfunction of the pelvic floor”)) OR (TITLE-ABS-KEY (“pelvic floor disease”)) OR (TITLE-ABS-KEY (“pelvic floor diseases”)) OR (TITLE-ABS-KEY (“diseases of the pelvic floor”)) OR (TITLE-ABS-KEY (“pelvic floor syndrome”)) OR (TITLE-ABS-KEY (“pelvic floor syndromes”)) OR (TITLE-ABS-KEY (“syndromes of the pelvic floor”)) OR (TITLE-ABS-KEY (“syndrome of the pelvic floor”)) OR (TITLE-ABS-KEY (myofascial W/2 (pelvic OR pelvis))) OR (TITLE-ABS-KEY (pelvi* W/3 (floor OR levator OR diaphragm* OR coccygeus)))) AND ((TITLE-ABS-KEY (“myofascial syndrome”)) OR (TITLE-ABS-KEY (trigger W/1 (point* OR area*))) OR (TITLEABS-KEY (spasm*)) OR (TITLE-ABS-KEY (pain*)) OR (TITLE-ABS-KEY (ache*)) OR (TITLE-ABS-KEY (myalgia*)) OR (TITLE-ABS-KEY (muscle W/1 (soreness OR tenderness))))) OR (((TITLE-ABS-KEY (“myofascial pain syndromes”)) AND ((TITLE-ABS-KEY (pelvis OR pelvic))) OR (TITLE-ABS-KEY (“pelvic pain syndrome”)) AND (TITLE-ABS-KEY (myalgia OR myofascial))))) AND ((TITLE-ABS-KEY (sensitivity W/2 specificity)) OR (TITLEABS-KEY (exam*)) OR (TITLE-ABS-KEY (diagnos*)) OR (TITLE-ABS-KEY (symptom*)) OR (TITLE (evaluat*))OR (KEY (evaluat*)) OR (TITLE-ABS-KEY (assessment*)) OR (TITLE-ABS-KEY (map*)))) AND NOT (((KEY (male)) AND NOT ((KEY (male)) AND (KEY (female)))))
06/06/17
34 results
pelvic floor disorders AND pain AND diagnosis AND EXACT NOT “Male” [GENDER]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflict of interest
CONDENSATION: This systematic review investigates published examination techniques for assessment of myofascial pelvic pain, and offers a recommended examination based upon consensus within the literature.
This work was accepted for poster presentation at the 44th annual scientific meeting of the Society of Gynecologic Surgeons, Orlando, Florida, March, 2018.
Contributor Information
R. MEISTER Melanie, St. Louis, Missouri; Obstetrics & Gynecology, Division of Female Pelvic Medicine and Reconstructive Surgery, Washington University in St. Louis.
SHIVAKUMAR Nishkala, St. Louis, Missouri; Washington University School of Medicine.
SUTCLIFFE Siobhan, St. Louis, Missouri; Department of Surgery, Division of Public Health Sciences, Washington University in St. Louis.
SPITZNAGLE Theresa, St. Louis, Missouri; Department of Physical Therapy, Washington University in St. Louis.
LOWDER Jerry, St. Louis, Missouri; Obstetrics & Gynecology, Division of Female Pelvic Medicine and Reconstructive Surgery, Washington University in St. Louis.
References
- 1.Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, Bortolini M, Dumoulin C, Gomes M, McClurg D, Meijlink J, Shelly E, Trabuco E, Walker C, Wells A. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Neurourol Urodynam 2017; 36:221–244. [DOI] [PubMed] [Google Scholar]
- 2.Adams K, Gregory WT, Osmundsen B, Clark A. Levator myalgia: why bother? Int Urogynecol J 2013; 24:1687–1693 [DOI] [PubMed] [Google Scholar]
- 3.Pastore EA, Katzman WB. Recognizing myofascial pelvic pain in the female patient with chronic pelvic pain. J Obstet Gynecol Neonatal Nurs 2012; 41(5):680–691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spitznagle TM, Robinson CM. Myofascial pelvic pain. Obstet Gynecol Clin N Am 2014; 41:409–432 [DOI] [PubMed] [Google Scholar]
- 5.Moldwin RM, Fariello JY. Myofascial trigger points of the pelvic floor: associations with urological pain syndromes and treatment strategies including injection therapy. Curr Urol Rep 2013; 14:409–417 [DOI] [PubMed] [Google Scholar]
- 6.Sanses TV, Chelimsky G, McCabe NP, Zolnoun D, Janata J, Elston R, Buffington CA, Simpson P, Zhang L, Chelimsky T. The pelvis and beyond: musculoskeletal tender points in women with chronic pelvic pain. Clin J Pain 2016; 32(8): 659–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuner R Central mechanisms of pathological pain. Nat Med 2010; 16(11):1258–1266 [DOI] [PubMed] [Google Scholar]
- 8.Peters KM, Carrico DJ, Kalinowski SE, Ibrahim IA, Diokno AC. Prevalence of pelvic floor dysfunction in patients with interstitial cystitis. Urology 2007; 70(1): 16–18. [DOI] [PubMed] [Google Scholar]
- 9.Meister M, Sutcliffe S, Badu A, Ghetti C, Lowder JL. Pelvic floor and obturator internus myofascial pain is common in patients with pelvic floor symptoms. Female Pelvic Med Reconstr Surg 2017; 23(5):S33. [Google Scholar]
- 10.Meister M, Sutcliffe S, Badu A, Ghetti C, Lowder JL. Pelvic floor and obturator internus myofascial pain is correlated with lower urinary tract symptom severity. Female Pelvic Med Reconstr Surg 2017; 23(5):S34. [Google Scholar]
- 11.Carrico DJ, Peters KM, Diokno AC. Guided imagery for women with interstitial cystitis: results of a prospective, randomized controlled pilot study. J Altern Complement Med 2008; 14(1): 53–60 [DOI] [PubMed] [Google Scholar]
- 12.FitzGerald MP, Anderson RU, Potts J, Payne CK, Peters KM, Clemens JQ, Kotarinos R, Fraser L, Cosby A, Fortman C, Neville C, Badillo S, Odabachian L, Sanfield A, O’Dougherty B, Halle-Podell R, Cen L, Chuai S, Landis JR, Kusek JW, Nyberg LM. Randomized multicenter feasibility trial of myofascial physical therapy for treatment of urologic chronic pelvic pain syndrome. J Urol 2009; 182(2): 570–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Souza Montenegro M, Lemes E, Mateus-Vasconcelos, Silva J, Nogueira A, Dos Reis F, Neto O. Importance of pelvic muscle tenderness evaluation in women with chronic pelvic pain. Pain Med 2010; 11: 224–228 [DOI] [PubMed] [Google Scholar]
- 14.Lamvu G, Nguyen R, Burrows LJ, Rapkin A, Witzeman K, Marvel RP, Hutchins D, Witkin SS, Veasley C, Fillingim R, Zolnoun D. The evidence-based vulvodynia assessment project. J Reprod Med 2015; 60:223–235 [PubMed] [Google Scholar]
- 15.Langford CF, Nagy SU, Ghoniem GM. Levator ani trigger point injections: an underutilized treatment for chronic pelvic pain. Neurourol Urodynam 2007; 26:59–62 [DOI] [PubMed] [Google Scholar]
- 16.Morissey D, El-Khawand D, Ginzburg N, Wehbe S, O’Hare P, Whitmore K Botulinum toxin A injections into pelvic floor muscles under electromyographic guidance for women with refractory high-tone pelvic floor dysfunction: a 6-month prospective pilot study. Female Pelvic Med Reconstr Surg 2015; 21: 277–282 [DOI] [PubMed] [Google Scholar]
- 17.Oyama IA, Rejba A, Lukban JC, Fletcher E, Kellogg-Spadt S, Holzberg AS, Whitmore KE. Modified thiele massage as therapeutic intervention for female patients with interstitial cystitis and high-tone pelvic floor dysfunction. Urology 2004; 64:862–865 [DOI] [PubMed] [Google Scholar]
- 18.Sillem M, Juhasz-Boss I, Klausmeier I, Mechsner S, Siedentopf F, Solomayer E. Osteopathy for endometriosis and chronic pelvic pain – a pilot study. Geburtsh Fauenheilk 2016; 76:960–963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adelowo A, Hacker MR, Shapiro A, Modest AM, Elkadry E. Botulinum toxin type A (BOTOX) for refractory myofascial pelvic pain. Female Pelvic Med Reconstr Surg 2013; 19(5): 288–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bassaly R, Tidwell N, Bertolino S, Hoyte L, Downes K, Hart S. Myofascial pain and pelvic floor dysfunction in patients with interstitial cystitis. Int Urogynecol J 2011; 22: 413–418 [DOI] [PubMed] [Google Scholar]
- 21.Bedaiwy MA, Patterson B, Mahajan S. Prevalence of myofascial chronic pelvic pain and the effectiveness of pelvic floor physical therapy. J Reprod Med 2013; 58: 504–510 [PubMed] [Google Scholar]
- 22.Bendana EE, Belarmino JM, Dinh JH, Cook CL, Murray BP, Feustel PJ, De EJB. Efficcacy of transvaginal biofeedback and electrical stimulation in women with urinary urgency and frequency and associated pelvic floor muscle spasm. Urol Nurs 2009; 29: 171–176 [PubMed] [Google Scholar]
- 23.Goetsch MF. Surgery compared with muscle therapy for dyspareunia from vulvar vestibulitis. J Reprod Med 2007; 52: 597–603 [PubMed] [Google Scholar]
- 24.Dos Bispo AP, Ploger C, Loureiro AF, Sato H, Kolpeman A, Girao MJ, Schor E. Assessment of the pelvic floor muscles in women with deep endometriosis. Arch Gynecol Obstet 2016; 294:519–523. [DOI] [PubMed] [Google Scholar]
- 25.Williams DP, Chelimsky G, McCabe NP, Koenig J, Singh P, Janata J, Thayer JF, Buffington CA, Chelimsky T. Effects of chronic pelvic pain on heart rate variability in women. J Urol 2015; 194:1289–1294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zolnoun D, Bair E, Essicks G, Gracely R, Goyal V, Maixner W. Reliability and reproducibility of novel methodology for assessment of pressure pain sensitivity in pelvis. J Pain 2012; 13(9): 910–920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kavvadias T, Pelikan S, Roth P, Baessler K, Schuessler B. Pelvic floor muscle tenderness in asymptomatic, nulliparous women: topographical distribution and reliability of a visual analogue scale. Int Urogynecol J 2013; 24: 281–286 [DOI] [PubMed] [Google Scholar]
- 28.Fenton BW, Grey SF, Reichenbach M, McCarroll M, Von Gruenigen V. Phenotyping chronic pelvic pain based on latent class modeling of physical examination. Pain Research and Treatment 2013; 1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peters KM, Carrico DJ, Kalinowski SE, Ibrahim IA, Diokno AC. Prevalence of pelvic floor dysfunction in patients with interstitial cystitis. Urology 2007; 70:16–18 [DOI] [PubMed] [Google Scholar]
- 30.Phillips N, Brown C, Bachmann G, Wan J, Wood R, Ulrich D, Bachour C, Foster D. Relationship between nongenital tender point tenderness and intravaginal muscle pain intensity: ratings in women with provoked vestibulodynia and implications for treatment. Am J Obstet Gynecol 2016; 215: 751e1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adams K, Osmundsen B, Gregory WT. Does fibromyalgia influence symptom bother from pelvic organ prolapse? Int Urogynecol J 2014; 25: 677–682 [DOI] [PubMed] [Google Scholar]
- 32.Bhide AA, Puccini F, Bray R, Khullar V, Digesu A. The pelvic floor muscle hyperalgesia (PFMH) scoring system: a new classification tool to assess women with chronic pelvic pain: multicenter pilot study of validity and reliability. Eur J Obstet Gynecol Reprod Biol 2015; 193: 111–113 [DOI] [PubMed] [Google Scholar]
- 33.De Souza Montenegro M, Mateus-Vasconcelos E, dos Reis FJ, Silva J, Nogueira A, Neto O. Thiele massage as a therapeutic option for women with chronic pelvic pain caused by tenderness of pelvic floor muscles. J Eval Clin Pract 2010; 16: 981–982 [DOI] [PubMed] [Google Scholar]
- 34.Fitzgerald CM, Neville CE, Mallinson T, Badillo SA, Hynes CK, Tu FF. Pelvic floor muscle examination in female chronic pelvic pain. J Reprod Med 2011; 56: 117–122 [PubMed] [Google Scholar]
- 35.Hellman KM, Patanwala IY, Pozolo KE, Tu FF. Multimodal nociceptive mechanisms underlying chronic pelvic pain. Am J Obstet Gynecol 2015; 213(6): 827e1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loving S, Thomsen T, Jaszczak P, Nordling J. Pelvic floor muscle dysfunctions are prevalent in female chronic pelvic pain: a cross-sectional population-based study. Eur J Pain 2014; 18: 1259–1270 [DOI] [PubMed] [Google Scholar]
- 37.Peters K, Girdler B, Carrico D, Ibrahim I, Diokno A. Painful bladder syndrome/interstitial cystitis and vulvodynia: a clinical correlation. Int Urogynecol J 2008; 19: 665–669 [DOI] [PubMed] [Google Scholar]
- 38.Tu FF, Fitzgerald CM, Kuiken T, Farrell T, Norman HR. Comparative measurement of pelvic floor pain sensitivity in chronic pelvic pain. Obstet Gynecol 2007; 110(6): 1244–1248 [DOI] [PubMed] [Google Scholar]
- 39.Tu FF, Holt J, Gonzales J, Fitzgerald CM. Physical therapy evaluation of patients with chronic pelvic pain: a controlled study. Am J Obstet Gynecol 2008; 198: 272e1–7 [DOI] [PubMed] [Google Scholar]
- 40.Tu FF, Fitzgerald CM, Kuiken T, Farrell T, Harden RN. Vaginal pressure-pain thresholds: initial validation and reliability assessment in healthy women. Clin J Pain 2008; 24(1): 45–50 [DOI] [PubMed] [Google Scholar]
- 41.Tu FF, As-Sanie S, Steege JF. Prevalence of pelvic musculoskeletal disorders in a female chronic pelvic pain clinic. J Reprod Med 2006; 51: 185–189 [PubMed] [Google Scholar]
- 42.Witzeman K, Nguyen R, Eanes A, As-Sanie S, Zolnoun D. Mucosal versus muscle pain sensitivity in provoked vestibulodynia. J Pain Res 2015; 8:549–555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yong PJ, Mui J, Allaire C, Williams C. Pelvic floor tenderness in the etiology of superficial dyspareunia. J Obstet Gynaecol Can 2014; 36(11):1002–1009 [DOI] [PubMed] [Google Scholar]
- 44.Reissing ED, Brown C, Lord MJ, Binik YM, Khalife S. Pelvic floor muscle functioning in women with vulvar vestibulitis syndrome. J Psychosom Obstet Gynaecol 2005; 26(2): 107–113 [DOI] [PubMed] [Google Scholar]
- 45.Albrecht KB. “How-To” Guide to pelvic floor muscle dysfunction. Clin Obstet Gynecol 2015;58: 546–550 [DOI] [PubMed] [Google Scholar]
- 46.Sarton J Assessment of the pelvic floor muscles in women with sexual pain. J Sex Med 2010; 7: 3526–3529 [DOI] [PubMed] [Google Scholar]
- 47.Steege JF. Office assessment of chronic pelvic pain. Clin Obstet Gynecol 1997; 40(3): 554–563 [DOI] [PubMed] [Google Scholar]
- 48.Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN. An International Urogynecologic Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 2010; 29: 4–20 [DOI] [PubMed] [Google Scholar]
- 49.Messelink B, Benson T, Berghmans B, Bo K, Corcos J, Fowler C, Laycock J, Lim P, van Lunsen R, Nijeholt G, Pemberton J, Wang A, Watier A, Van Kerrebroeck P. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the pelvic floor clinical assessment group of the International Continence Society. Neurourol Urodyn 2005; 24: 374–380 [DOI] [PubMed] [Google Scholar]
- 50.Apte G, Nelson P, Brismee JM, Dedrick G, Justiz R, Sizer PS. Chronic female pelvic pain – Part 1: clinical pathoanatomy and examination of the pelvic region. Pain Practice 2012; 12(2): 88–110 [DOI] [PubMed] [Google Scholar]
- 51.Aredo JV, Heyrana KJ, Karp BI, Shah JP, Stratton P. relating chronic pelvic pain and endometriosis to signs of sensitization and myofascial pain and dysfunction. Semin Reprod Med 2017; 35:88–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Butrick CW. Pelvic floor hypertonic disorders: identification and management. Obstet Gynecol Clin N Am 2009; 36: 707–722 [DOI] [PubMed] [Google Scholar]
- 53.Faubion SS, Shuster LT, Bharucha AE. Recognition and management of nonrelaxing pelvic floor dysfunction. Mayo Clin Proc 2012; 87(2): 187–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.FitzGerald MP, Kotarinos R. Rehabilitation of the short pelvic floor I: background and patient evaluation. Int Urogynecol J 2003; 14: 261–268 [DOI] [PubMed] [Google Scholar]
- 55.Gyang A, Hartman M, Lamvu G. Musculoskeletal causes of chronic pelvic pain. Obstet Gynecol 2013; 121: 645–650 [DOI] [PubMed] [Google Scholar]
- 56.Hartmann D Chronic vulvar pain from a physical therapy perspective. Dermatologic Therapy 2010; 23: 505–513 [DOI] [PubMed] [Google Scholar]
- 57.Peters KM, Carrico DJ. Frequency, urgency, and pelvic pain: treating the pelvic floor versus the epithelium. Curr Urol Rep 2006; 7:450–455 [DOI] [PubMed] [Google Scholar]
- 58.Prather H, Camacho-Soto A. Musculoskeletal etiologies of pelvic pain. Obstet Gynecol Clin N Am 2014; 41: 433–442 [DOI] [PubMed] [Google Scholar]
- 59.Prather H, Spitznagle TM, Dugan SA. Recognizing and treating pelvic pain and pelvic floor dysfunction. Phys Med Rehabil Clin N Am 2007; 18: 477–496 [DOI] [PubMed] [Google Scholar]
- 60.Prather H, Dugan S, Fitzgerald C, Hunt D. Review of anatomy, evaluation, and treatment of musculoskeletal pelvic floor pain in women. PM&R 2009; 1: 346–358 [DOI] [PubMed] [Google Scholar]
- 61.Prendergast SA, Weiss JM. Screening for musculoskeletal causes of pelvic pain. Clin Obstet Gynecol 2003; 46(4): 773–782 [DOI] [PubMed] [Google Scholar]
- 62.Vercellini P, Somigliana E, Vigano P, Abbiati A, Barbara G, Fedele L. Chronic pelvic pain in women: etiology, pathogenesis and diagnostic approach. Gynecol Endocrinol 2009; 25(3): 149–158 [DOI] [PubMed] [Google Scholar]


