Abstract
Objective:
To identify modifiable factors leading to unplanned readmission (UR) and characterize differences in adjusted UR rates across hospitals
Design:
Retrospective cohort study using prospectively collected clinical registry data
Setting:
Pediatric Cardiac Critical Care Consortium (PC4) clinical registry.
Patients:
Patients admitted to a pediatric cardiac intensive care unit (PCICU) at PC4 hospitals.
Interventions:
None.
Measurements and Main Results:
We examined PCICU encounters in the PC4 registry from October 2013 to March 2016. The primary outcomes were early (<48 hours from PCICU transfer) and late (2–7 days) UR. Generalized logit models identified independent predictors of UR. We then calculated observed-to-expected (O/E) ratios of UR, and identified higher-than or lower-than-expected UR rates for those with an O/E > or < 1, respectively, and a 95% confidence interval that did not cross 1. Of 11,301 PCICU encounters (16 hospitals), 62% were surgical and 18% were neonates. There were 175 (1.6%) early UR, and 300 (2.7%) late UR, most commonly for respiratory (31%) or cardiac (28%) indications. In multivariable analysis, unique modifiable factors were associated with UR. While shorter time between discontinuation of vasoactive infusions and PCICU transfer was associated with early UR, nighttime discharge was independently associated with a greater likelihood of late UR. Two hospitals had lower-than-expected UR in both the early and late categories, whereas two other hospitals were higher-than-expected in both.
Conclusions:
This analysis demonstrated time from discontinuation of critical care therapies to PCICU transfer as a significant, modifiable predictor of UR. We identified two hospitals with lower-than-expected adjusted rates of both early and late UR, suggesting that their systems are well-designed to prevent UR. This offers the possibility of disseminating best practices to other hospitals through collaborative learning.
Keywords: Cardiovascular Surgical Procedures; Heart Defects, Congenital; Intensive Care Units, Pediatric; Patient Readmission
Introduction
Unplanned readmissions (UR) to intensive care units are uncommon, but associated with longer length of stay and greater mortality.(1, 2) One analysis of patients cared for in nearly one hundred intensive care units suggested a more than two-fold increase in hospital length of stay and a four-fold increase in mortality.(3) Some advocate to use UR rates as a quality of care measure in critical care, but controversy remains with respect to the utility of UR rates as a performance metric.(1, 2, 4, 5)
Despite reports of the impact of UR in many adult critical care populations, less is known with respect to incidence of UR in children, particularly among pediatric patients with heart disease.(6–9) One single-center series reported a PCICU UR rate of 5.3% and a mortality rate of 16% in such admissions (relative to a mortality rate of 0.5% among those not readmitted).(9) A second single-center series reported a 2.4% readmission rate within 72 hours of discharge, also associated with a greater than two-fold increase in mortality.(10) To date, the single-center nature of these investigations has encumbered an understanding of factors that may contribute to UR in the PCICU. Identification of both patient and hospital-level contributions to UR and their outcomes may provide insight into modifiable factors to prevent UR and improve outcomes. Furthermore, developing a method to calculate case mix-adjusted UR rates across hospitals could identify variation in performance, and provide the opportunity to study high-performing hospitals.
In this context, we used data from the Pediatric Cardiac Critical Care Consortium (PC4) registry to define predictors of UR to a PCICU.(11) We hypothesized that patient, PCICU practice, and hospital factors would associate with both early and late UR. We then developed a case mix-adjusted model to study variation in UR rates and identify high-performing hospitals with low UR rates.
Methods
Data Source
The Pediatric Cardiac Critical Care Consortium is a quality improvement collaborative that collects data on all patients with primary cardiac disease admitted to the PCICU service of participating hospitals.(12) PC4 maintains a clinical registry to support research and quality improvement initiatives. At the time of this analysis, 16 centers were submitting cases to the PC4 Registry.
Each participating center has a data manager who collects data in accordance with the standardized PC4 Data Definitions Manual. The PC4 registry shares terminology and definitions with applicable data points from the International Pediatric and Congenital Cardiac Code (IPCCC), Society of Thoracic Surgeons (STS) Congenital Heart Surgery Database, and American College of Cardiology Improving Pediatric and Adult Congenital Treatment (IMPACT) Registry, as previously described(12). Participating centers are audited on a regular schedule and audit results suggest complete, accurate and timely submission of data across centers.(11) The University of Michigan Institutional Review Board provides oversight for the PC4 Data Coordinating Center; this study was reviewed and approved with waiver of informed consent.
Inclusion and Exclusion Criteria
All initial PCICU encounters in a hospitalization recorded in the PC4 registry were considered for inclusion in this analysis. The study period spanned from October 2013 through March 2016. Encounters were not considered at risk for readmission and excluded if (1) the encounter concluded with death, or if (2) the patient was admitted to the PCICU for comfort care. All other initial encounters were considered at risk for readmission, including those where the patient was discharged from the PCICU to home or to an outside hospital. We excluded all encounters from one hospital that does not physically discharge patients to another ward from the PCICU, and those from hospitals with less than 100 encounters in the database at the time of analysis.
Outcomes
Primary outcomes were early (<48 hours form PCICU transfer) and late (2–7 days) PCICU UR. A PCICU readmission was considered “unplanned” if it was noted as unplanned by the PC4 data collector according to the registry definition; the registry defines an unplanned admission as that which is not planned at the time of morning bed meeting. Admissions to the PCICU for treatment of an acute medical condition were also coded as unplanned. Readmissions to the PCICU following an unplanned reintervention, while potentially an “unplanned” aspect of the overall treatment plan, were not included unless the encounter also met definitional criteria for an UR as described above. A cut point of 7 days was utilized a priori in comparisons associated with late UR performance; this time duration has been utilized by others in the validation of predictive models for UR among adult ICU patients.(13, 14)
Predictor variables
We analyzed patient and PCICU index encounter characteristics, including demographics, critical care therapies, and time of therapy discontinuation prior to PCICU transfer, for association with UR. We considered complications encountered during the index PCICU encounter as possible predictors of UR. Weight-for-age z score was calculated utilizing the World Health Organization and Centers for Disease Control standards.(15) A surgical encounter was defined by an STS index operation immediately preceding or during the PCICU encounter. To account for surgical complexity, index operations were classified into a Society of Thoracic Surgeons-European Association for Cardiothoracic Surgery (STAT) mortality category where appropriate.(16) Institutional organizational structure and practices were also identified from each participating center through a questionnaire issued to participating centers in 2015, with 100% response rate on all items.
Statistical Analysis
Patient characteristics, PCICU encounter characteristics, and outcomes were described using standard measures of central tendency. Univariate analyses were used to determine associations between each candidate predictor variable and the multinomial outcome consisting of 3 categories: no readmission, early UR, and late UR. All variables associated with the outcome at p<0.1 were included in the subsequent multivariable analyses.
Polytomous logistic regression was used to model the multinomial outcome as a function of the aforementioned predictor variables. We formally tested for the proportional odds assumption in the logistic model. Based on the result, we fitted two separate generalized logit model to the 3-category outcome (i.e. no readmission vs. early UR, and vs. late UR, respectively) using no readmission as the reference category. Generalized estimating equation (GEE) was used to account for clustering of patients within hospitals and obtain robust (sandwich estimators) standard errors. The treating hospital was included as a fixed effect in the model since our goal was to evaluate the performance of the PC4 hospitals. Multicollinearity was assessed using variance inflation factors, and the final model was selected using a stepwise selection procedure. Variables associated with readmission at p<0.05 are reported as independent predictors of UR, as appropriate. We performed bootstrap resampling (based on 1000 resamples) to empirically derive optimism-corrected 95% confidence intervals around the odds ratio for each predictor.
We then calculated case-mix adjusted UR rates for each hospital. Patient and PCICU encounter factors identified in multivariable analysis were used to determine the expected UR rate for each outcome category. Variables thought to be related to hospital and PCICU quality or hospital structure were excluded from the adjustment model. Using expected UR rates, we calculated observed-to-expected ratios (O/E) of early and late UR for each hospital. Based on the bootstrap resamples, we obtained 95% confidence intervals around the O/E ratios. Those hospitals whose confidence interval did not cross one were considered statistical outliers. Of these outliers, hospitals with an O/E less than 1 were classified as lower-than-expected, and those with an O/E greater than 1 were classified as higher-than-expected UR. All others were considered to have as expected UR rates. All analyses were performed using SAS Version 9.4 (SAS Institute, Cary, NC) or STATA Version 14 (Stata Corp, College Station, TX).
Results
There were 11,301 PCICU encounters that met criteria as at risk for readmission within 7 days from 16 hospitals. Demographic characteristics and complications associated with each initial PCICU encounter are summarized in Table 1 and Supplemental Table 1 respectively. Among this cohort, there were 475 UR (4.2%) within 7 days, with 175 (1.6%) early and 300 (2.7%) late. Hospital and organizational factors, including 24/7 in-house PCICU attending presence, ward nursing hours per patient day, shared nursing staff between ward and PCICU, and use of early warning scores on ward units were not associated with UR. Indications for, as well as outcomes associated with PCICU UR are summarized in Table 2. Among index encounters associated with early UR, 53% (n=93) occurred within 24 hours. Indications for UR were most commonly classified as respiratory or cardiac in origin. Furthermore, both early and late UR was associated with similar rates of cardiac surgery, cardiac catheterization, as well as PCICU mortality.
Table 1.
Characteristics of PCICU encounters by readmission outcome, N=11,301
| Unplanned Readmission | ||||
|---|---|---|---|---|
| No UR | UR at 0–2 days | UR at 2–7 days | p-value¶ | |
| Characteristic | 10826(95.8%) | 175 (1.6%) | 300 (2.7%) | |
| Patient Characteristics | ||||
| Age at PCICU admission | ||||
| Neonate (0–30 days) | 1934 (17.9%) | 36 (20.6%) | 73 (24.3) | 0.0006 |
| Infant (1 month-1 year) | 3077 (28.4%) | 54 (30.9%) | 91 (30.3%) | |
| Child (1–18 years) | 4942 (45.7%) | 65 (37.1%) | 103 (34.3%) | |
| Adult (>18 years) | 873 (8.1%) | 20 (11.4%) | 33 (11%) | |
| Weight-for-age z-score | ||||
| Underweight | 2272(21%) | 47(26.9%) | 88(29.3%) | 0.0005 |
| Normal weight | 8086(74.7%) | 119(68%) | 193(64.3%) | |
| Overweight | 468(4.3%) | 9(5.1%) | 19(6.3%) | |
| Male gender | 6048(55.9%) | 104(59.4%) | 177(59%) | 0.37 |
| Anomalies | ||||
| Extracardiac/chromosomal abnormality | 3578(33%) | 75(42.9%) | 121(40.3%) | 0.0009 |
| Trisomy 21/Down syndrome | 788(7.3%) | 15(8.6%) | 14(4.7%) | 0.18 |
| DiGeorge syndrome | 351(3.2%) | 5(2.9%) | 10(3.3%) | 0.96 |
| Encounter type | <0.0001 | |||
| Medical | 4049(37.4%) | 75(42.9%) | 159(53%) | |
| Surgical | 6777(62.6%) | 100(57.1%) | 141(47%) | |
| STAT Category of index operation | <0.0001 | |||
| STAT 1 | 2126(31.4%) | 16(16%) | 15(10.6%) | |
| STAT 2 | 2253(33.2%) | 32(32%) | 41(29%) | |
| STAT 3 | 882(13%) | 14(14%) | 17(12.1%) | |
| STAT 4 | 1198(17.7%) | 26(26%) | 47(33.3%) | |
| STAT 5 | 215(3.2%) | 9(9%) | 15(10.6%) | |
| Not categorized | 103(1.5%) | 3(3%) | 6(4.3%) | |
| Time (days) from end of intervention to CICU discharge | ||||
| Last operation | 3(2,5) | 3(2,6) | 7(3,13) | <0.0001 |
| All vasoactive infusions | 1(1,3) | 1(0,4) | 2(1,6) | 0.003 |
| Mechanical ventilation | 2(1,4) | 2(1,4) | 4(2,8) | <0.0001 |
| NIPPV | 2(1,4) | 1(0,2) | 3(1,6) | <0.0001 |
| Discharge characteristics | ||||
| Critical care length of stay, days | 2(1,6) | 3(1,8) | 5(2,13) | <0.0001 |
| Night discharge | 2388(22.1%) | 40(22.9%) | 86(28.7%) | 0.03 |
| Weekend discharge | 2984(27.6%) | 46(26.3%) | 86(28.7%) | 0.85 |
| Number of admissions on discharge date | 2(1,3) | 2(1,3) | 2(1,3) | 0.75 |
| Number of discharges/deaths on discharge date | 3(2,4) | 2(2,3) | 3(2,3) | 0.44 |
Continuous variables are reported as Median (25th, 75th percentile). Categorical variables are reported as Frequency (%)
%s are column percentages, STAT category percentages for surgical patients only.
Weight categories were based on Weight-for-age Z-score/ BMI from WHO (2 yrs or below) or CDC (>2yrs).
Univariate comparisons describing association between candidate predictor characteristic and a multinomial outcome (no UR, UR at 0–2 days, and UR at 2–7 days),
PCICU: Pediatric Cardiac Intensive Care Unit; UR: Unplanned readmission; NIPPV: Noninvasive Positive Pressure Ventilation; STAT: Society of Thoracic Surgeons and the European Association for Cardiothoracic Surgery (STS-EACTS) Congenital Heart Surgery Mortality Category
Table 2.
Characteristics of unplanned readmissions <7 days following PCICU discharge
| Unplanned Readmission Characteristic | <2d (N=175) |
2–7 d (N=300) |
|---|---|---|
| Indication for unplanned readmission | ||
| Respiratory | 56 (32%) | 89 (30%) |
| Cardiac | 51 (29%) | 80 (27%) |
| Infection | 15 (9%) | 25 (8%) |
| Neurologic | 3 (2%) | 10 (3%) |
| Other medical condition | 37 (21%) | 62 (21%) |
| Unplanned procedure | 13 (7%) | 34 (11%) |
| Interventions Following Readmission | ||
| Cardiac surgery | 31 (18%) | 57 (19%) |
| Cardiac catheterization (any) | 18 (10%) | 39 (13%) |
| Cardiac catheterization (interventional) | 9 (5%) | 21 (7%) |
| Mortality during readmission encounter | 8 (5%) | 19 (6%) |
Categorical variables are reported as frequency (%).
PCICU: Pediatric Cardiac Intensive Care Unit
Covariates significantly associated with UR in the univariate analyses were included in multivariable models for both early UR and late UR. Independent predictors of early UR are detailed in Table 3. Factors associated with increased odds of UR included presence of an extracardiac anomaly and complications (presence of paralyzed diaphragm, cardiac arrest). Discontinuation of vasoactive infusions ≤24 hours prior to discharge conferred a 60% increase in odds of early UR, while low complexity surgical encounters were associated with a 50% lower odds of readmission.
Table 3.
Independent predictors of early (<48 hour) unplanned readmission
| Variable | Adjusted Odds Ratio (OR)¶ | 95% Confidence Interval | p-value |
|---|---|---|---|
| Patient and Encounter Characteristics | |||
| Extracardiac anomaly | 1.5 | 1.1–2.0 | 0.007 |
| Medical vs. Surgical encounter* | |||
| Low complexity surgery | 0.5 | 0.3–0.9 | 0.03 |
| High complexity surgery | 1.0 | 0.5–2.0 | 0.90 |
| Medical | REF | ||
| Time of discontinuation of vasoactive infusions† | |||
| ≤24 hours prior to discharge/transfer | 1.6 | 1.03–2.4 | 0.04 |
| >24 hours prior to discharge/transfer | 1.2 | 0.7–1.9 | 0.48 |
| Complications during encounter | |||
| Paralyzed diaphragm | 2.9 | 1.2–6.7 | 0.01 |
| Cardiac arrest | 2.1 | 1.2–3.8 | 0.01 |
Low complexity surgical PCICU encounters include index operations classified into STAT categories 1–3. High complexity surgical PCICU encounters include index operations classified into STAT categories 4–5 or unclassified. Medical encounters do not include an index cardiothoracic operation.
Model covariates include age at PCICU admission, weight-for-age z-score at admission, presence of an extracardiac or chromosomal anomaly, STAT category of index operation, cardiac arrest, use of mechanical circulatory support, arrhythmia, seizure, infection, extubation failure, diaphragm paralysis, chylothorax, unplanned reintervention, time elapsed between end of critical care intervention [vasoactive medication, mechanical ventilation, noninvasive positive pressure ventilation] and PCICU discharge, PCICU length of stay prior to discharge, and nighttime discharge.
Compared to encounters where therapy was not administered as referent group
Independent predictors of late UR are detailed in Table 4. The administration of both vasoactive infusions and noninvasive ventilation during the index admission, regardless of timing of discontinuation, were independently associated with late UR. Conversely, those separated from mechanical ventilation during the index PCICU encounter ≤24 hours prior to PCICU discharge demonstrated a reduced likelihood of late UR, relative to patients not mechanically ventilated during their encounter. As seen in early UR, low complexity surgical encounters were associated with reduced odds of readmission relative to medical encounters.
Table 4.
Independent predictors of late (2–7 days) unplanned readmission
| Variable | Adjusted Odds Ratio (OR)¶ | 95% Confidence Interval | p-value |
|---|---|---|---|
| Patient and Encounter Characteristics | |||
| Underweight status |
0.6 | 0.5–0.7 | <0.0001 |
| Medical vs. Surgical encounter* | |||
| Low complexity surgery | 0.3 | 0.2–0.5 | <0.0001 |
| High complexity surgery | 0.7 | 0.5–1.2 | 0.20 |
| Medical | REF | ||
| Time of discontinuation of vasoactive infusions† | |||
| ≤24 hours prior to discharge/transfer | 1.6 | 1.02–2.5 | 0.04 |
| >24 hours prior to discharge/transfer | 1.9 | 1.1–3.4 | 0.02 |
| Time of discontinuation of mechanical ventilation† | |||
| ≤24 hours prior to discharge/transfer | 0.6 | 0.4–0.9 | 0.008 |
| >24 hours prior to discharge/transfer |
0.6 | 0.3–1.3 | 0.19 |
| Time of discontinuation of non-invasive ventilation† | |||
| ≤24 hours prior to discharge/transfer | 1.4 | 1.2–1.8 | 0.004 |
| >24 hours prior to discharge/transfer | 1.4 | 0.6–3.4 | 0.46 |
| Nighttime discharge | 1.4 | 1.05–1.8 | 0.02 |
| PCICU length of stay prior to discharge/transfer (days) |
1.01 | 1.01–1.02 | <0.0001 |
| Complications during encounter | |||
| Chylothorax | 1.7 | 1.1–2.8 | 0.03 |
Low complexity surgical PCICU encounters include index operations classified into STAT categories 1–3. High complexity surgical PCICU encounters include index operations classified into STAT categories 4–5 or unclassified. Medical encounters do not include an index cardiothoracic operation.
Model covariates include age at PCICU admission, weight-for-age z-score at admission, presence of an extracardiac or chromosomal anomaly, STAT category of index operation, cardiac arrest, use of mechanical circulatory support, arrhythmia, seizure, infection, extubation failure, diaphragm paralysis, chylothorax, unplanned reintervention, time elapsed between end of critical care intervention [vasoactive medication, mechanical ventilation, noninvasive positive pressure ventilation] and PCICU discharge, PCICU length of stay prior to discharge, and nighttime discharge.
Compared to encounters where therapy was not administered as referent group
Case-mix adjusted UR rates by hospital are detailed in Figure 1. With respect to early UR, we observed four-fold variation in adjusted rates of early UR, ranging from 0.7% to 3.1% across the sixteen participating centers with O/E ratios of early UR ranging from 0.41 (95%CI 0.28–0.59) to 1.79 (95%CI 1.21–2.59). Case-mix adjustment also demonstrated wide variation in O/E ratios of late UR, ranging from 0.64 (95%CI 0.47–0.86) to 1.61 (95%CI 1.21–2.18) across the same centers. There were two hospitals with higher-than-expected adjusted rates of both early and late UR, and two centers with lower-than-expected adjusted rates of both early and late UR.
Figure 1.
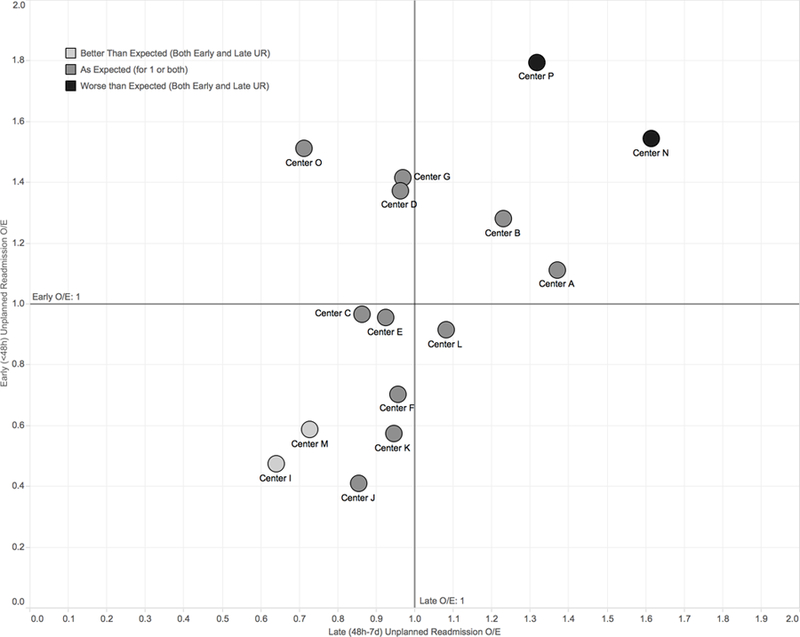
Scatterplot relating early (vertical axis) and late (horizontal axis) case-mix adjusted unplanned readmission rates with respect to PC4 participating center. Centers are considered lower or higher-than-expected if both lower and upper 95% confidence intervals do not cross a case-mix adjusted observed-to-expected (O/E) ratio of 1. Centers I and M demonstrate lower-than-expected case-mix adjusted rates of both early and late UR, while centers P and N demonstrate higher-than expected case-mix adjusted rates of both early and late UR.
Discussion
To our knowledge, this is the first multi-center description of patient and institution-level predictors of unplanned readmission to the pediatric cardiac intensive care unit. We report modifiable factors that are independently associated with PCICU UR and we demonstrate clinically important variations in UR rates across sixteen participating hospitals, while identifying hospitals that appear to be high-performing as evidenced by lower-than-expected adjusted rates of both early and late UR.
ICU UR has been proposed as a performance measure by the Society for Critical Care Medicine and European Society of Intensive Care Medicine.(17–19) Early UR may be the most accurate measure of critical care quality and the ICU team’s decision making; readmissions within 48 hours are more likely to reflect unrecognized conditions present at ICU discharge. Others contend that ICU UR rates do not reflect ICU quality of care, but instead serve as an indicator of variation in critical care resources between hospitals. (20–22) While resources no doubt impact how PCICU patients are cared for within and across hospitals, we found no association between certain hospital organizational variables and UR. We assessed readmissions after 48 hours to determine if some hospitals were able to delay, but not avoid, UR in part because of their available resources in non-ICU wards.
We assessed variation in UR across PC4 hospitals using O/E rates and accounting for case-mix differences. There were important differences in both early and late UR rates when considering each outcome separately. While 2 of the 16 hospitals demonstrated higher-than-expected early and late UR rates suggesting an opportunity for UR reduction among some institutions, we also identified two hospitals with lower O/E UR rates in both outcome categories. These hospitals could serve as model organizations providing operational insight on how to reduce UR to the PCICU.
Critical care literature to date has identified largely non-modifiable factors independently associated with early UR, including age, admission diagnoses, and the presence of comorbid conditions. (1, 3, 6, 23) Importantly, our analysis also identified several modifiable PCICU practices associated with UR. Previous literature suggests occupancy at time of ICU discharge and measures of ICU capacity strain are associated with UR.(8–10, 20, 24) We evaluated many of these variables, and only nighttime discharge was associated with late UR. We also found associations between time from discontinuation of critical care therapies and UR; discontinuation of vasoactive infusions ≤24h prior to ICU discharge were associated with early UR. Hospitals looking to reduce early UR might consider timing of de-escalation as an important factor in transfer readiness. While not practical among all patients, those at greatest risk for UR based upon identified predictors may benefit from prolonged observation in the ICU or employing objective means of monitoring patient stability following ICU discharge.(25) Curiously, exposure to inotropes or mechanical ventilation was associated with a decreased risk of late UR. While difficult to explain clinically, it is possible that patients who receive critical care for reasons other than for receipt of vasoactive infusions and/or mechanical ventilation have complex medical needs placing them at risk for repeated admissions.
Researchers must contextualize UR with other PCICU quality metrics including mortality and length-of-stay to determine whether UR truly reflects differential quality. Mortality among our readmitted cohort was 6%, greater than an overall hospital mortality rate of 2.9%, and consistent with increases described elsewhere.(9, 10) These data support an important, but ill-defined association between PCICU UR and mortality. While as much as a 10-fold increased mortality has been described in ICU readmissions, others suggest no association between readmission and mortality or length of stay after case-mix adjustment.(1, 26) Similarly, it remains unclear in our hospital cohort whether PCICU length of stay and UR are related. It is possible that hospitals achieve lower UR rates by holding patients in their PCICU longer before discharge. It will be necessary to develop methods to adjust PCICU length of stay accounting for patient factors. Though these analyses were beyond the scope of our investigation, assessing PCICU quality across multiple domains may provide insight on whether high-performing PCICUs with low case-mix adjusted mortality and length of stay also demonstrate lower UR rates.
Limitations.
We recognize limitations in this investigation. Defining an “unplanned” encounter in accordance with PC4 operational definition fails to identify patients readmitted following an intervention after a prior PCICU discharge. While these situations are “unplanned” readmissions in that they are not anticipated at the time of PCICU discharge, this operational definition for the PC4 registry more closely reflects PCICU operational decision-making. Furthermore, while we investigated the contribution of several institutional factors, limitations in modeling an infrequent outcome among 16 hospitals reduced our ability to assess an exhaustive collection of hospital-level covariates potentially related to UR; additionally these institutional characteristics, while accurate at the time of survey collection, may not have remained consistent across the entire study period. Furthermore, the PC4 database currently excludes most information related to non-ICU care. A partnership between PC4 and the Pediatric Acute Cardiac Care Collaborative (PAC3) will soon provide access to more information related to non-ICU care, which will be important in assessing UR in follow-up studies. Finally, this study investigated UR among patients with an initial cardiac ICU encounter who survived to ICU discharge, excluding those readmitted previously. This approach may raise concern with respect to selection bias when comparing center UR rates, by considering only those well enough to survive to discharge from an index PCICU encounter. Our analysis included GEE modeling which may provide less reliable estimates of hospital performance when the sample of hospitals is low.(27) As with any observational study, we cannot eliminate the possibility of residual confounding; some of our measured variables may not completely capture illness severity factors that predict readmission.
Conclusions.
We report the first multicenter investigation of PCICU UR, and find that adjusted rates of UR vary substantially across hospitals in PC4. We describe both patient factors and modifiable PCICU practices independently associated with UR. We must uncover the hospital practices affecting variation, and determine whether UR truly serves as a reliable indicator of PCICU practice quality. With these data, hospitals looking to reduce UR will have an evidence base and the collaborative learning network of PC4 to provide models for practice change.
Supplementary Material
Acknowledgements
We acknowledge the data collection teams at all of the participating centers.
Financial Support:
This study was supported in part by funding from the University of Michigan Congenital Heart Center, CHAMPS for Mott, and the Michigan Institute for Clinical and Health Research (NIH/NCATS UL1TR002240).
Copyright form disclosure: Drs. Smith and Gaies received support for article research from the National Institutes of Health (NIH). Dr. Gaies’ institution received funding from the NIH (K08 Award).
Footnotes
The remaining authors have disclosed that they do not have any potential conflicts of interest.
References
- 1.Rosenberg AL, Watts C: Patients readmitted to ICUs* : a systematic review of risk factors and outcomes. Chest 2000; 118:492–502 [DOI] [PubMed] [Google Scholar]
- 2.Rosenberg AL, Hofer TP, Hayward RA, et al. : Who bounces back? Physiologic and other predictors of intensive care unit readmission. Crit Care Med 2001; 29:511–8 [DOI] [PubMed] [Google Scholar]
- 3.Kramer AA, Higgins TL, Zimmerman JE: Intensive care unit readmissions in U.S. hospitals: patient characteristics, risk factors, and outcomes. Crit Care Med 2012; 40:3–10 [DOI] [PubMed] [Google Scholar]
- 4.Edwards JD, Lucas AR, Stone PW, et al. : Frequency, Risk Factors, and Outcomes of Early Unplanned Readmissions to PICUs. Crit Care Med 2013; 41:2773–2783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Renton J, Pilcher DV, Santamaria JD, et al. : Factors associated with increased risk of readmission to intensive care in Australia. Intensive Care Med 2011; 37:1800–1808 [DOI] [PubMed] [Google Scholar]
- 6.Brown SES, Ratcliffe SJ, Kahn JM, et al. : The epidemiology of intensive care unit readmissions in the United States. Am J Respir Crit Care Med 2012; 185:955–964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Penk JS, Loke Y-H, Waloff KR, et al. : Unplanned admissions to a pediatric cardiac critical care unit: a review of 2 years’ experience. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 2015; 16:155–160 [DOI] [PubMed] [Google Scholar]
- 8.Odetola FO, Clark SJ, Dechert RE, et al. : Going back for more: an evaluation of clinical outcomes and characteristics of readmissions to a pediatric intensive care unit. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 2007; 8:343–347; CEU quiz 357 [DOI] [PubMed] [Google Scholar]
- 9.Brunetti MA, Glatz AC, McCardle K, et al. : Unplanned Readmission to the Pediatric Cardiac Intensive Care Unit: Prevalence, Outcomes, and Risk Factors. World J Pediatr Congenit Heart Surg 2015; 6:597–603 [DOI] [PubMed] [Google Scholar]
- 10.Bastero-Miñón P, Russell JL, Humpl T: Frequency, characteristics, and outcomes of pediatric patients readmitted to the cardiac critical care unit. Intensive Care Med 2012; 38:1352–1357 [DOI] [PubMed] [Google Scholar]
- 11.Gaies M, Donohue JE, Willis GM, et al. : Data integrity of the Pediatric Cardiac Critical Care Consortium (PC4) clinical registry. Cardiol Young 2016; 26:1090–1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaies M, Cooper DS, Tabbutt S, et al. : Collaborative quality improvement in the cardiac intensive care unit: development of the Paediatric Cardiac Critical Care Consortium (PC4). Cardiol Young 2015; 25:951–957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gajic O, Malinchoc M, Comfere TB, et al. : The Stability and Workload Index for Transfer score predicts unplanned intensive care unit patient readmission: initial development and validation. Crit Care Med 2008; 36:676–682 [DOI] [PubMed] [Google Scholar]
- 14.Kastrup M, Powollik R, Balzer F, et al. : Predictive ability of the stability and workload index for transfer score to predict unplanned readmissions after ICU discharge. Crit Care Med 2013; 41:1608–15 [DOI] [PubMed] [Google Scholar]
- 15.Growth Charts - Z-score Data Files [Internet]. [cited 2017 Oct 31] Available from: https://www.cdc.gov/growthcharts/zscore.htm
- 16.Jacobs JP, Jacobs ML, Maruszewski B, et al. : Initial application in the EACTS and STS Congenital Heart Surgery Databases of an empirically derived methodology of complexity adjustment to evaluate surgical case mix and results. Eur J Cardio-Thorac Surg Off J Eur Assoc Cardio-Thorac Surg 2012; 42:775–779; discussion 779–780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.SCCM Quality Indicators Committee: Candidate Critical Care Quality Indicators. 1995;
- 18.NQF: NQF Endorses All-Cause Unplanned Readmissions Measures [Internet]. [cited 2017 Jan 9] Available from: http://www.qualityforum.org/News_And_Resources/Press_Releases/2012/NQF_Endorses_All-Cause_Unplanned_Readmissions_Measures.aspx
- 19.Rhodes A, Moreno RP, Azoulay E, et al. : Prospectively defined indicators to improve the safety and quality of care for critically ill patients: a report from the Task Force on Safety and Quality of the European Society of Intensive Care Medicine (ESICM). Intensive Care Med 2012; 38:598–605 [DOI] [PubMed] [Google Scholar]
- 20.Wagner J, Gabler NB, Ratcliffe SJ, et al. : Outcomes among patients discharged from busy intensive care units. Ann Intern Med 2013; 159:447–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown SES, Ratcliffe SJ, Halpern SD: An empirical comparison of key statistical attributes among potential ICU quality indicators. Crit Care Med 2014; 42:1821–1831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maharaj R, Terblanche M, Vlachos S: The Utility of ICU Readmission as a Quality Indicator and the Effect of Selection. Crit Care Med 2018; 46:749–756 [DOI] [PubMed] [Google Scholar]
- 23.Litmathe J, Kurt M, Feindt P, et al. : Predictors and outcome of ICU readmission after cardiac surgery. Thorac Cardiovasc Surg 2009; 57:391–4 [DOI] [PubMed] [Google Scholar]
- 24.Chrusch CA, Olafson KP, McMillan PM, et al. : High occupancy increases the risk of early death or readmission after transfer from intensive care. Crit Care Med 2009; 37:2753–8 [DOI] [PubMed] [Google Scholar]
- 25.Kroeger AR, Morrison J, Smith AH: Predicting unplanned readmissions to a pediatric cardiac intensive care unit using predischarge Pediatric Early Warning Scores. Congenit Heart Dis 2018; 13:98–104 [DOI] [PubMed] [Google Scholar]
- 26.Kramer AA, Higgins TL, Zimmerman JE: The association between ICU readmission rate and patient outcomes. Crit Care Med 2013; 41:24–33 [DOI] [PubMed] [Google Scholar]
- 27.McNeish D, Stapleton LM: Modeling Clustered Data with Very Few Clusters. Multivar Behav Res 2016; 51:495–518 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


