Abstract
Female sex workers (FSWs) in sub-Saharan Africa are disproportionately affected by HIV and gender-based violence (GBV). Substance use overlaps with these co-occurring epidemics to further increase FSWs’ risk for negative health outcomes. We explored the relationship between substance use, GBV, and consistent condom use utilizing baseline data from a cohort of 496 FSWs in Tanzania. Results demonstrate high levels of alcohol use and GBV, and low levels of consistent condom use. Frequent intoxication during sex work was associated with increased odds of recent GBV (aOR: 1.64, 95% CI: 1.07, 2.49; p-value: 0.02) and reduced odds of consistent condom use with clients (aOR: 0.58, 95% CI: 0.37, 0.92; p-value: 0.02). We adapt the Risk Environment Framework to contextualize our findings in the social and structural context and to gain insight into intervention approaches to address the intersecting challenges of substance use, GBV, and HIV among FSWs in Tanzania and similar settings.
Keywords: Sub-Saharan Africa, Female Sex Workers, Gender-Based Violence, Substance Use, HIV
Introduction
Female sex workers (FSWs) bear a disproportionate burden of HIV globally. In low and middle-income countries, FSWs have 13.5 times the odds of HIV infection compared to the general female population (1). FSWs in sub-Saharan Africa (SSA) have the highest burden of HIV, with an HIV prevalence of 29% (2).
The high burden of HIV among FSWs in SSA is shaped by the social and structural context in which sex work occurs. Criminalization of sex work, which fosters stigma and discrimination towards FSWs (3–5), poverty (6–8), and gender inequality (9, 10), all inhibit HIV preventative behaviors such as condom use (4, 11).
High rates of gender-based violence (GBV) (i.e. physical or sexual violence) against FSWs may also contribute to increased risk for HIV among this population (12, 13). Globally, FSWs experience a disproportionate burden of GBV due to their marginalized status in society (4, 14). Violence can increase FSWs’ risk for HIV directly, through forced sex, and indirectly through increased HIV risk behaviors including unprotected sex (15).
Substance use is associated with both GBV and unprotected sex among FSWs in SSA (16–19). Alcohol is the most common substance used among FSWs in SSA, and has been shown to limit FSWs’ ability to successfully negotiate and use condoms, ultimately increasing their risk for HIV (16–18). Evidence also suggests that alcohol use increases FSWs’ risk for GBV (16, 20, 21). Qualitative research describes how clients encourage FSWs to drink to the point where they lose consciousness, which renders them vulnerable to rape (22, 23). Alcohol consumption may also impair FSWs’ ability to detect the risk of violence and escape a risky situation (17, 24).
While research from SSA has examined how substance use, including alcohol use/abuse, is associated with both GBV and HIV risk among FSWs (16, 18–21), few studies have examined the intersection of substance use, GBV and the potential for increased HIV risk among this population. To enhance our understanding of these dynamics, this paper examines the relationship between substance use, GBV, and consistent condom use with clients among FSWs in Iringa, Tanzania.
Prior interventions have sought to address the overlapping epidemics of substance use, violence and HIV among FSWs (25, 26), and have demonstrated promise in reducing short-term alcohol consumption. However, these individual-level interventions did not consistently reduce violence or unprotected sex among FSWs. To achieve substantial and sustainable reductions in alcohol consumption, violence, and unprotected sex, interventions may need to address the social and structural context in which sex work occurs (24). As a first step in developing an effective solution to the overlapping epidemics of substance use, violence, and HIV among FSWs, we must understand how aspects of the sex work environment impact alcohol consumption, violence, and HIV risk behaviors among FSWs and their clients. To this end, we explore the social and structural factors associated with violence and condom use among FSWs, and utilize an adapted version of the risk environment framework (27) to contextualize our findings in the social and structural context in which sex work occurs.
The Risk Environment Framework
The Risk Environment Framework was originally developed to understand how social and structural factors shape individual’s risk for drug use and HIV (27). Although this framework was conceptualized in relation to drug use, the core principles of this framework can be applied to understand other health issues. We adapt this framework to contextualize our findings in the broader social and structural environment and gain insight into potential interventions to limit substance use, and prevent GBV, and HIV among FSWs in Tanzania and similar settings
Methods
Study Setting
This study was conducted in the Iringa region of Tanzania, which is bifurcated by the Tanzanian-Zambian (Tan-Zam) highway. The majority of FSWs in Iringa are employed as barmaids in the bars that line the Tan-Zam highway, where they sell alcohol to migrant workers/truck drivers and meet clients. Evidence suggests that FSWs in Iringa have some of the highest rates of alcohol consumption and GBV in the country (28). With an HIV prevalence of 32.9%, FSWs in Iringa are also one of the FSW populations most impacted by HIV in Tanzania (28).
Sampling
This study utilized baseline data from 496 FSWs enrolled in a phase II community-randomized controlled trial of a community-based combination HIV prevention model, Project Shikamana (Kiswahili for ‘stick together’), in Iringa, Tanzania (29).
Two geographically distant communities, matched on demographic characteristics and level of HIV risk, were randomized to either the intervention or the control condition. FSWs were recruited from entertainment venues in the two participating communities, including bars, guesthouses, and clubs. Venue-based time location sampling (TLS) was used to enroll a cohort of 203 HIV-infected and 293 HIV-uninfected women. Women were eligible to participate in the study if they were: ≥18 years, reported exchanging sex for money in the last month, worked at an identified venue in one of the two study communities, and provided informed consent.
Data Collection
Eligible participants provided informed consent and completed baseline surveys in a private location in or near the venue where they work, or at the study’s local office. The interviewer-administered survey was conducted in Kiswahili and assessed HIV risk behaviors, experiences with GBV, and substance use. Responses were recorded onto a secure tablet and uploaded to a secure database upon completion of the survey. All data were de-identified using unique participant identifiers. Finally, consenting participants were counseled and tested for HIV following the Tanzanian National guidelines.
Measures
Outcome variables
Outcome variables included recent experiences of physical or sexual GBV from any perpetrator, defined as occurring in the past 6 months, and consistent condom use with all clients in the past 30 days. GBV was measured using the previously validated 16-item World Health Organization (WHO) scale measuring experiences of physical and sexual violence against women (30), adapted for the Tanzanian context based on our formative work. The scale measured 7 types of physical violence, ranging from being slapped to having a weapon used against you, as well as sexual violence. For each type of violence, participants were asked if they had experienced that type of violence ever and in the past 6 months. Responses to items regarding experiences of physical or sexual violence in the past 6 months were summed and dichotomized to represent any or no recent experiences of violence.
Consistent condom use was measured using two questions adapted from the previously validated assessment from the NIMH-Project Accept Study (31). Participants were asked how often they use condoms during vaginal sex with new and regular clients in the past 30 days. Answer choices ranged from 0 (never) to 4 (always). Responses for regular and new clients were combined to create a dichotomized variable indicating consistent (always) or inconsistent condom use (less than always) with all client types.
Independent variables
The main independent variable of interest was substance use, which was operationalized as the frequency of intoxication from either drugs or alcohol during sex work in the past 30 days. This was measured by the question ‘In the past 30 days, out of all the times you exchanged money for sex, how often were you intoxicated (i.e. drunk or high)?’ Response options ranged from 0 (never intoxicated) to 5 (always intoxicated). Infrequent intoxication was defined as never/rarely/sometimes being intoxicated during sex work, and frequent intoxication was defined as almost always/always. We collapsed sparse categories of the original variable to determine the cutoff for dichotomization.
Additional independent factors included internalized sex work stigma, social cohesion, as well as socio-demographic and work environment characteristics. Internalized sex work stigma, which refers to FSWs’ acceptance of the negative attitudes society holds about them, was measured using a reliable (α=0.86) and valid (32) 13-item scale adapted from an internalized HIV stigma measure informed by the work of Berger (33). The same questions asked in the HIV self-stigma measure were re-worded in relation to sex work. Participants rated how much they agreed with each statement using a 4-point Likert scale. Scores on each item were summed to obtain the overall continuous internalized sex work stigma score.
Social cohesion (α=0.86) was measured using a 9-item scale developed by the last author and previously validated among FSWs in Brazil (34, 35). Participants rated their agreement with statements related to mutual aid, support, and trust among their sex worker colleagues, using a 4-point Likert scale. Scores on each item were summed to obtain the overall continuous social cohesion score.
Socio-demographic characteristics assessed included age, average monthly income, and knowledge of HIV serostatus. Age was a continuous variable, and average monthly income was dichotomized at the median such that those earning 120,000Tsh (~54USD) or more were compared to those earning less than 120,000Tsh per month. Knowledge of HIV status was assessed by comparing self-reported HIV status to the result from the rapid HIV test administered at enrollment (29). A categorical variable was created to represent HIV negative status (0), tested HIV positive but did not report HIV positive status (not aware of status or unwilling to report) (1), and tested HIV positive and reported HIV positive status (aware of status and willing to report) (2).
Work environment covariates included having ever been denied payment for sex work, frequency of clients expecting FSWs to consume alcohol/drugs during sex work, and access to condoms. Participants reported whether they had ever been denied payment from a client. Client expectations of FSW substance use during sex work was measured by the question: ‘In the past 30 days, how often does a client want or expect you to drink or use drugs with him?’ Answer choices ranged from 0 (never)-4 (always). Based on the distribution of the original categorical variable, this measure was dichotomized so FSWs who said clients almost always/always expected them to use substances were compared to FSWs who said this never/rarely/sometimes happened. Access to condoms was measured by asking women if they felt they had access to condoms when they needed them in the past 6 months. Answer choices ranged from 0 (no access)-3(somewhat easy access). This variable was dichotomized to represent difficult or no access (0) and somewhat easy access (1), based on the distribution of the original categorical variable.
Data Analysis
Bivariate logistic regression models were used to determine the association between the independent variables and the outcomes of interest. We initially sought to explore whether GBV mediated the relationship between substance use and consistent condom use. However, in the bivariate analysis, recent GBV was not significantly associated with consistent condom use with clients in the past 30 days, making us unable to conduct a mediation analysis (36). An interaction term between frequency of intoxication during sex work and recent GBV on consistent condom use was also explored. However, it was not significant, and was therefore not included in the multivariable analysis.
Ultimately, two separate analyses were conducted, with recent GBV as the outcome for the first model, and consistent condom use with all clients in the past 30 days as the outcome for the second model. Frequency of intoxication during sex work was the main independent variable for both models.
The two multivariable models controlled for socio-demographic characteristics and independent variables of interest. Variables were included in the multivariable model if they had a p-value less than or equal to 0.1 or were deemed theoretically important. Community was included in the multivariate models because the study design was based on the purposive selection of the two communities. Generalized estimating equations (GEE) with robust variance estimates were used to adjust for the within-venue, intra-class correlation related to our outcomes of interest (37, 38).
To better understand the overlapping relationships between GBV, intoxication and condom use we conducted additional sensitivity analyses by stratifying the adjusted analysis of intoxication during sex work on consistent condom use by recent GBV. Data analysis was conducted using STATA 13 (39).
This study received human subjects research approval from the Institutional Review Boards (IRBs) of the Johns Hopkins Bloomberg School of Public Health, the Muhimbili University of Health and Allied Sciences Directorate of Research and Publications, and the National Institute for Medical Research of Tanzania. All procedures performed in this study were conducted in accordance with the principles outlined in the Declaration of Helsinki.
RESULTS
Sample Characteristics
The median age of the sample was 25 years old (Interquartile range (IQR): 22–30 years) (Table I). Over half of the sample (62%) were employed as barmaids by a venue that sells alcohol, and 91% met their clients in these venues. Forty percent of the participants reported that they were frequently intoxicated during sex work in the past 30 days. Alcohol consumption was more common than drug use among this sample: 97% reported drinking at least one alcoholic beverage during a typical day at work, while 7% had ever used drugs. The median internalized sex work stigma score was 39 (IQR: 35, 44), and the median social cohesion score was 21 (IQR: 18–24). The HIV prevalence at baseline was 41%. Of the 203 women who tested positive for HIV, 31% (n=63) were aware of their HIV positive status. Physical or sexual violence was experienced by 40% of FSWs in the past 6 months. Finally, 32% of the sample reported consistent condom use with all clients in the past 30 days.
Table I.
Demographic Characteristics of the cohort at baseline (N=496)
| Characteristics | N (%) |
|---|---|
| Individual level | |
| Age, years, median (IQR) | 25 (22,30) |
| Monthly income > 120,000 Tsh/$55 | 244 (49) |
| Education | |
| No formal schooling | 27 (5) |
| Some primary school | 325 (66) |
| Some secondary or higher | 144 (29) |
| HIV positive (laboratory confirmed) | 203 (41) |
| Knowledge of HIV status | |
| HIV negative | 293 (59) |
| HIV positive but unaware/not willing to report | 140 (28) |
| HIV positive and aware and willing to report | 63 (13) |
| Relationship status | |
| Single | 78 (16) |
| In a steady relationship but not married | 329 (66) |
| Married | 89 (18) |
| Responsible for one or more children | 449 (91) |
| Number of years in sex work, median (IQR) | 5 (2,10) |
| Full-time or part-time employment with a salary | 301 (61) |
| Frequency of sex work | |
| Once a week or less | 165 (34) |
| A few times a week but not every day | 287 (58) |
| Once a day or more | 40 (8) |
| Work Environment/Structural level | |
| Frequent intoxication during sex work, past 30 days | 207 (42) |
| Drink one or more drinks on a typical day of work | 408 (97) |
| Ever used drugs | 34 (7) |
| Clients expect FSW to consume alcohol during sex work | 324 (66) |
| Earn ≥ 15,000 Tsh/$7 per sex act | 266 (54) |
| Ever denied payment for sex work completed | 158 (32) |
| Employed by a venue that sells alcohol | 301 (62) |
| Meet clients in bars | 449 (91) |
| Internalized sex work stigma, median (IQR) | 39 (35,44) |
| Social cohesion among sex workers in venue, median (IQR) | 21 (18,24) |
| Consistent condom use with all clients, past 30 days | 158 (32) |
| Somewhat easy access to condoms, past 6 months | 400 (82) |
| Any GBV (physical or sexual), ever | 254 (51) |
| Recent GBV (physical or sexual), past 6 months | 197 (40) |
| Physical GBV, ever | 232 (47) |
| Recent Physical GBV, past 6 months | 175 (35) |
| Sexual GBV, ever | 109 (22) |
| Recent Sexual GBV, past 6 months | 86 (17) |
Results from model 1: Recent GBV as the outcome
Results from the bivariate and multivariable logistic regression analyses with recent GBV as the outcome are displayed in Table II. In the multivariable logistic regression, frequent intoxication during sex work was associated with increased odds of recent GBV (aOR: 1.64, 95% CI: 1.07, 2.49; p-value: 0.02). Having ever been denied payment for sex work by clients (aOR: 1.74, 95% CI: 1.15, 2.64; p-value: 0.01), social cohesion (aOR: 1.06, 95% CI: 1.01, 1.10; p-value: 0.01), internalized sex work stigma (aOR: 1.03, 95% CI: 1.00, 1.07; p-value: 0.03), and knowledge of HIV positive status (aOR: 1.96, 95% CI: 1.02, 3.78; p-value: 0.04) were also associated with increased odds of recent GBV. Older age (aOR 0.96, 95% CI: 0.93, 0.99; p-value: 0.04) and residing in the Mafinga study community (aOR: 0.59, 95% CI: 0.38, 0.94; p-value: 0.03) were associated with reduced odds of recent GBV.
Table II.
Unadjusted and Adjusted associations between intoxication during sex work and recent GBV (N=496)
| Characteristics | Bivariatea | Multivariablea | ||
|---|---|---|---|---|
| OR (95% CI) | p-value | AOR (95% CI) | p-value | |
| Age | 0.98 (0.95, 1.01) | 0.13 | 0.96 (0.93, 0.99) | 0.04 |
| Earn an average of 120,000 Tsh or more per month (~$55 USD) | 1.42 (0.99, 2.04) | 0.06 | 1.29 (0.86, 1.92) | 0.21 |
| Relationship status | ||||
| Single | (reference) | -- | (reference) | -- |
| In a steady relationship but not married | 1.04 (0.63, 1.72) | 0.88 | 1.07 (0.62, 1.85) | 0.82 |
| Married | 0.87 (0.46, 1.64) | 0.67 | 1.03 (0.50, 2.11) | 0.94 |
| Knowledge of HIV status | ||||
| HIV negative | (reference) | -- | (reference) | -- |
| HIV positive unaware | 0.98 (0.65, 1.48) | 0.92 | 0.96 (0.61, 1.52) | 0.87 |
| HIV positive aware | 1.65 (0.95, 2.86) | 0.08 | 1.96 (1.02, 3.78) | 0.04 |
| Meet clients in bars | 0.82 (0.45, 1.51) | 0.53 | 0.66 (0.33, 1.31) | 0.23 |
| Frequent intoxication druing sex work in the past 30 days | 1.84 (1.28, 2.66) | 0.001 | 1.64 (1.07, 2.49) | 0.02 |
| Clients expect FSW to consume alcohol during sex work | 1.42 (0.96, 2.08) | 0.08 | 1.24 (0.79, 1.94) | 0.35 |
| Ever denied payment for sex work completed | 2.16 (1.46, 3.18) | <0.001 | 1.74 (1.15, 2.64) | 0.01 |
| Social cohesion among sex workers in venue | 1.07 (1.02, 1.11) | 0.002 | 1.06 (1.01, 1.10) | 0.01 |
| Internalized sex work stigma | 1.03 (1.00, 1.06) | 0.036 | 1.03 (1.00, 1.07) | 0.03 |
| Mafinga study community | 0.83 (0.56, 1.24) | 0.367 | 0.59 (0.38, 0.94) | 0.03 |
Adjusted for intraclass correlation due to clustering in venues
Results from model 2: Consistent condom use with all clients in the past 30 days as the outcome
Results from the bivariate and multivariable logistic regression analyses with consistent condom use with all clients in the past 30 days as the outcome are displayed in Table III. In the multivariable logistic regression, frequency of intoxication during sex work was significantly associated with reduced odds of consistent condom use with all clients (aOR: 0.58, 95% CI: 0.37, 0.92; p-value: 0.02). Older age was also associated with reduced odds of consistent condom use with all clients (aOR: 0.96, 95% CI: 0.93, 0.99; p-value: 0.04). Earning higher average monthly income (aOR: 1.65, 95% CI: 1.09, 2.51; p-value: 0.02) and knowledge of HIV positive status (aOR: 2.39, 95% CI: 1.23, 4.66; p-value: 0.01) were associated with increased odds of consistent condom use with all clients. The relationship between GBV and consistent condom use was not significant in the multivariable model.
Table III.
Unadjusted and adjusted odds of consistent condom use with all clients in the past 30 days among the cohort at baseline (N=496)
| Characteristics | Bivariatea | Multivariablea | ||
|---|---|---|---|---|
| OR (95% CI) | p-value | AOR (95% CI) | p-value | |
| Age | 0.98 (0.95, 1.01) | 0.22 | 0.96 (0.93, 0.99) | 0.04 |
| Earn an average of 120,000 Tsh or more per month (~$55 USD) | 1.53 (1.04, 2.24) | 0.03 | 1.65 (1.09, 2.51) | 0.02 |
| Relationship status | ||||
| Single | (reference) | -- | (reference) | -- |
| In a steady relationship but not married | 1.68 (0.95, 2.96) | 0.07 | 1.73 (0.93, 3.19) | 0.08 |
| Married | 2.04 (1.03, 4.03) | 0.04 | 2.06 (0.95, 4.25) | 0.07 |
| Knowledge of HIV status | ||||
| HIV negative | (reference) | -- | (reference) | -- |
| HIV positive unaware | 0.95 (0.62, 1.47) | 0.83 | 1.17 (0.72, 1.88) | 0.53 |
| HIV positive aware | 1.68 (0.96, 2.94) | 0.07 | 2.39 (1.23, 4.66) | 0.01 |
| Recent GBV | 0.95 (0.65, 1.39) | 0.78 | 0.92 (0.60, 1.42) | 0.72 |
| Frequent intoxication druing sex work in the past 30 days | 0.54 (0.36, 0.79) | 0.002 | 0.58 (0.37, 0.92) | 0.02 |
| Clients expect FSW to consume alcohol during sex work | 0.69 (0.47, 1.01) | 0.06 | 0.91 (0.58, 1.44) | 0.69 |
| Meet clients in bars | 0.55 (0.30, 1.00) | 0.05 | 0.61 (0.31, 1.22) | 0.16 |
| Social cohesion among sex workers in venue | 0.99 (0.95, 1.03) | 0.61 | 0.98 (0.94, 1.03) | 0.44 |
| Sex work stigma | 1.03 (0.99, 1.06) | 0.06 | 1.03 (0.99, 1.06) | 0.12 |
| Somewhat easy access to condoms in the past 6 months | 1.36 (0.82, 2.28) | 0.24 | 1.45 (0.82, 2.55) | 0.20 |
| Mafinga study community | 1.39 (0.91, 2.12) | 0.13 | 1.26 (0.78, 2.03) | 0.25 |
Adjusted for intraclass correlation due to clustering in venues
In the stratified analysis (Table IV), frequent intoxication during sex work was significantly associated with reduced odds of consistent condom use with clients among women who experienced recent violence (aOR: 0.37; 95% CI: 0.17, 0.77; p-value: 0.01), but not among those who did not recently experience violence. Women who were aware of their HIV positive status and had experienced recent GBV had significantly increased odds of consistent condom use with clients (aOR: 2.63, 95% CI: 1.03, 6.70; p-value: 0.04) compared to women who were HIV-negative and had experienced recent GBV. Among women who did not recently experienced violence, older age was associated with reduced odds of consistent condom use with clients (aOR: 0.95, 95% CI: 0.90, 0.99; p-value: 0.03), and being in a steady relationship and being married was associated with increased odds of consistent condom use with clients.
Table IV.
Adjusted odds of consistent condom use with all clients in the past 30 days, stratified by experiences of recent GBV
| Characteristics | No recent GBV (n=299) | Recent GBV (n=197) | ||
|---|---|---|---|---|
| AOR (95% CI)a | AOR (95% CI)a | |||
| p-value | p-value | |||
| Age | 0.95 (0.90, 0.99) | 0.03 | 0.98 (0.92, 1.04) | 0.55 |
| Earn an average of 120,000 Tsh or more per month (~$55 USD) | 1.58 (0.91, 2.74) | 0.10 | 1.87 (0.93, 3.75) | 0.08 |
| Relationship status | ||||
| Single | (reference) | -- | (reference) | -- |
| In a steady relationship but not married | 2.46 (1.03, 5.89) | 0.04 | 1.06 (0.39, 2.82) | 0.91 |
| Married | 4.02 (1.43, 11.32) | 0.01 | 0.74 (0.19, 2.74) | 0.65 |
| Knowledge of HIV status | ||||
| HIV negative | (reference) | -- | (reference) | -- |
| HIV positive unaware | 1.63 (0.89, 3.01) | 0.12 | 0.53 (0.22, 1.28) | 0.16 |
| HIV positive aware | 2.18 (0.80, 3.01) | 0.13 | 2.63 (1.03, 6.70) | 0.04 |
| Frequent intoxication druing sex work in the past 30 days | 0.74 (0.39, 1.37) | 0.34 | 0.37 (0.17, 0.77) | 0.01 |
| Clients expect FSW to consume alcohol during sex work | 0.86 (0.47, 1.56) | 0.62 | 0.81 (0.37, 1.76) | 0.59 |
| Meet clients in bars | 0.95 (0.36, 2.50) | 0.91 | 0.41 (0.14, 1.2) | 0.10 |
| Social cohesion among sex workers in venue | 0.97 (0.92, 1.04) | 0.41 | 0.97 (0.90, 1.05) | 0.45 |
| Sex work stigma | 1.03 (0.98, 1.07) | 0.21 | 1.03 (0.97, 1.08) | 0.33 |
| Somewhat easy access to condoms in the past 6 months | 1.20 (0.54, 2.67) | 0.65 | 1.72 (0.73, 4.08) | 0.22 |
| Mafinga study community | 1.58 (0.89, 2.78) | 0.11 | 0.89 (0.44, 1.80) | 0.75 |
Adjusted for intraclass correlation due to clustering in venues
Discussion
Findings from this study suggest that frequent intoxication during sex work is associated with increased risk for both recent GBV and unprotected sex among FSWs in Iringa, Tanzania. Results also suggest that aspects of the sex work environment, including denial of payment for sex work completed, internalized sex work stigma, and monthly income, are associated with GBV and consistent condom use with clients among FSWs in this setting.
Interestingly, findings from the sensitivity analysis suggest that frequent intoxication during sex work is associated with significantly reduced odds of consistent condom use with clients among women who experience recent GBV, but not among those who have not experienced recent GBV. This finding suggests that the overlapping experience of GBV and frequent intoxication may place FSWs at heightened risk for unprotected sex. Prior research has demonstrated that GBV is associated with unprotected sex with regular non-paying partners among FSWs who abuse alcohol (13). Our findings build upon this past research by suggesting that the intersection of GBV and alcohol use may also influence condom use among clients. This is of particular importance given prior work suggesting that alcohol use plays a central role in the sex work negotiation process with clients in this context (40)
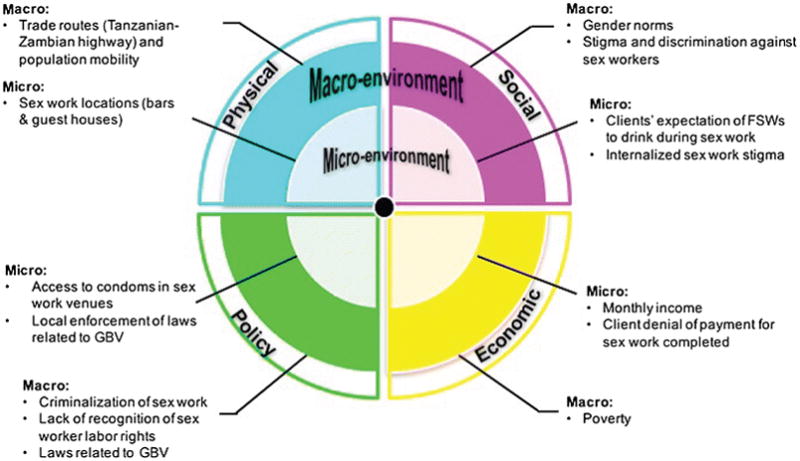
In the following section, we apply an adapted version of the risk environment framework to contextualize our findings in the broader social and structural sex work environment and gain insight into intervention approaches to limit substance use and prevent GBV and HIV among FSWs in Tanzania and similar contexts (27). Figure 1 outlines a risk environment that comprises four types of environments (physical, social, economic, and policy) that intersect with levels of environments (micro and macro) to increase risk or protective factors for substance use, GBV, and HIV among FSWs in Iringa, Tanzania (27).
Figure 1.
Policy Environment
Sex work is criminalized in Tanzania, as in many other African countries, which has broad reaching implications for FSWs’ ability to access their human and labor rights (3–5). The International Labor Organization (ILO), under labor code 200, recognizes sex work as a legitimate form of work entitled to the right to fair wages and a safe work environment, including access to HIV prevention and treatment and freedom from violence (41). However, when sex work is not viewed as a legitimate form of work under the eyes of the law, FSWs have limited ability to demand these rights. Evidence suggests that criminalization limits FSWs’ ability to demand condom use with their clients and payment for sex work (5, 42). It is possible that these factors contribute to our findings that only 32% of FSWs in this sample consistently use condoms with their clients in the last 30 days, and over one third have been denied payment for sex work they have already completed.
Furthermore, FSWs face significant barriers to accessing justice for violence perpetrated against them due to the criminalization of their work and their marginalized status in society (3). Although laws that provide protection to survivors of violence exist in Tanzania (43), their effectiveness is undermined by inconsistent enforcement (3). When perpetrators are not held accountable for violence against FSWs, abuses are allowed to continue with impunity. Such dynamics may have contributed to the high rates of violence reported in this study.
Criminalization of sex work also limits FSWs’ access to HIV services such as HIV testing, due to fear or actual experiences of stigma and discrimination or denial of services by health care providers (42, 44). Prior research has demonstrated the positive effects HIV testing can have on condom use and other HIV prevention behaviors (45, 46). In this sample, only 31% of the FSWs who tested positive for HIV were aware of their status, suggesting very low rates of HIV testing or, possibly, an unwillingness to disclose. Yet the few FSWs who were aware of their HIV positive status were significantly more likely to engage in consistent condom use with their clients, even in the context of recent GBV. This finding supports the importance of HIV testing services to be made widely available to FSWs, as it may contribute to improved condom use among this population, in addition to serving as a gateway to treatment services. Further research is also needed to understand how FSWs living with HIV are able to engage in consistent condom use with clients even when they experience GBV. Such research could shed important insights into potential intervention strategies.
Physical Environment
Iringa’s location along the Tan-Zam highway brings high levels of mobility and migration through the region, increasing the demand for sex work (47). The majority of sex workers in this sample work as barmaids in the modern and traditional bars that line the highway where they sell alcohol and meet their sex work clients. Prior qualitative work in Iringa suggests that clients typically buy FSWs alcoholic beverages in order to initiate the sex exchange process (44). Indeed, 66% of the women in our sample reported that their clients expect them to consume alcohol during sex work. These dynamics illustrate how the physical sex work environment (i.e. bars along the Tan-Zam highway) may intersect with the social environment (i.e. norms about alcohol consumption during work) to facilitate alcohol consumption during sex work. As our findings suggest, intoxication during sex work is associated with increased risk for both GBV and HIV among this population.
Social Environment
Criminalization of sex work fosters stigma and discrimination towards sex workers (3–5). Our findings suggest that some FSWs internalize this stigma, and that this is associated with increased risk for violence. Few studies have explored the relationship between internalized sex work stigma and GBV (14). However, in a qualitative study among FSWs living with HIV in Canada, Logie and colleagues found that FSWs with internalized HIV-related stigma frequently reported being in, and remaining in, violent relationships (48). In a similar vein, our findings suggest that internalized sex work stigma is associated with increased risk for GBV. It is also possible that the positive relationship between internalized sex work stigma and GBV reflects the emergence of internalized sex work stigma as a result of experiences with GBV. In contexts where sex work is criminalized and highly stigmatized, violence against FSWs is often a form of enacted sex work stigma, and regularly occurs with impunity (4, 49).
Our findings also suggest that FSWs who were aware of their HIV-positive serostatus had significantly increased odds of recent GBV compared to HIV-negative FSWs. This finding is supported by prior research among the general female population, which indicates that women living with HIV are at increased risk for GBV due to HIV stigma and relationship conflict brought on by partner disclosure (50, 51). It is possible that stigma and discrimination towards sex workers intersects with HIV stigma to place FSWs living with HIV at increased risk for GBV. It is also possible that a similar mechanism described by Logie and colleagues (48) is at play; namely, FSWs may be internalizing HIV-related stigma and staying in abusive relationships.
Although we did not measure gender norms in our study, it is important to acknowledge that inequitable gender norms intersect with stigma and discrimination against sex workers to place FSWs at increased risk for GBV (52, 53).
At the micro-level, we also found that FSWs who had not experienced recent GBV and were in a steady relationship or married had significantly increased odds of consistent condom use with clients, compared to FSWs who were single. It is possible that women who were in steady relationships were engaging in HIV prevention behavior with their clients in order to protect their steady partners. While this relationship did not persist among FSWs who experienced recent GBV, it is worth further research as it could inform future HIV prevention interventions among FSWs.
Economic Environment
As described above, criminalization of sex work compromises FSWs’ labor rights, as defined by the ILO, including access to fair wages and a safe work environment (41). Our findings suggest that denial of payment for sex work already completed is associated wtih increased risk for GBV. In contrast, earning a higher monthly income is associated with significantly increased odds of consistent condom use with clients. Taken together, these findings suggest that labor rights, including access to payment for sex work, might play a critical role in reducing FSWs’ risk for HIV and GBV.
We had two unexpected findings. First, we found that social cohesion was associated with increased odds of recent GBV. This finding is not in line with prior research, which suggests that social cohesion among FSW communities facilitates violence prevention (35, 54, 55). However, due to the cross-sectional nature of this study we are unable to determine temporal order. It is therefore possible that our finding reflects an organic emergence of mutual aid and support (i.e. social cohesion) that resulted from experiences with GBV. Further research, including longitudinal analyses, is needed to explore this relationship.
Second, GBV was not significantly associated with consistent condom use in this study. This finding held when we stratified by demographic variables, as well as severity and frequency of violence. This is contrary to prior research, which suggests that GBV is associated with inconsistent condom use among FSWs and their sexual partners (12, 15). Importantly, some of this work has yielded partner-specific results related to violence and condom use (13, 56, 57). Unfortunately, our data lacked specificity regarding perpetrator type (e.g. non-paying partner, new client etc.), which may have weakened our ability to detect a significant relationship between GBV and consistent condom use with clients. Future studies should assess whether perpetrator type influences the relationship between GBV and consistent condom use among this population.
Implications for a rights-based approach to prevent HIV and GBV among FSWs
The risk environment framework emphasizes the potential for creating safe and supportive environments by addressing the social situations and structures that promote risk (27). Rights-based, community empowerment approaches, which provide opportunities for sex workers to come together in solidarity to address the social and structural barriers they face to their health and human rights, have shown promise in addressing the social and structural factors described above that increase FSWs’ risk for GBV and HIV. Interventions that have adopted this approach have reduced violence and increased condom use among FSWs across a number of contexts (58, 60–62). However, few community empowerment approaches in the literature have explicitly addressed the overlapping epidemics of substance use, violence, and HIV among FSWs (5, 58). Our findings suggest the need for future community empowerment initiatives to address the role substance use, particularly alcohol use, plays in increasing FSWs’ risk for GBV and unprotected sex in SSA.
Strengths and limitations
It is important to acknowledge the limitations of this study. First, the cross-sectional nature of this study limits our ability to establish temporal order, and therefore draw causal conclusions about the relationship between substance use, GBV, and consistent condom use. Furthermore, the self-report of GBV, consistent condom use, and substance use, may have introduced some social desirability bias into our findings. To minimize this potential bias, interviewers were trained to establish trust and rapport with participants, and ask questions about GBV in a sensitive manner. Finally, as described above, our inability to account for perpetrator type in our analysis of the relationship between GBV and consistent condom use with clients is another limitation of this study.
Despite these limitations, this study has a number of strengths. This is study contributes to our knowledge regarding the way in which substance use influences the co-occurring epidemics of GBV and HIV among FSWs in SSA. Additionally, our study sheds light on the important role of internalized sex work stigma on the experiences of violence against FSWs in this setting, something that has previously been unexplored.
Conclusion
Results from this study demonstrate that intoxication during sex work is associated with increased risk for both GBV and HIV among FSWs. Findings also suggest that internalized sex work stigma, and denial of payment for sex work are associated with increased risk for GBV, while earning a higher average monthly income is associated with increased odds of consistent condom use with clients. Drawing upon the Risk Environment Framework, we argue that a rights-based community empowerment approach is needed to address the effects of the sex work environment on FSWs’ risk for substance use, GBV, and HIV. Such approaches should facilitate the opportunity for sex workers to come together as a community to mobilize their collective power and resources to fight for their right to a safe and supportive working environment.
Acknowledgments
We would like to thank the women who participated in the study and the efforts of the research staff. This work was supported by the National Institutes of Mental Health R01MH104044 and F31MH110303. The content in this paper is solely the responsibility of the authors and does not necessarily represent the official views of the sponsors.
Funding
This work was supported by the National Institutes of Mental Health R01MH104044 and F31MH110303. The content in this paper is solely the responsibility of the authors and does not necessarily represent the official views of the sponsors.
Footnotes
Compliance with ethical standards
Disclosure of potential conflicts of interest
The authors declare that they have no conflict of interests.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. The LancetInfectious diseases. 2012;12(7):538–49. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- 2.Beyrer C, Crago AL, Bekker LG, Butler J, Shannon K, Kerrigan D, et al. An action agenda for HIV and sex workers. Lancet (London, England) 2015;385(9964):287–301. doi: 10.1016/S0140-6736(14)60933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Human Rights Watch. “Treat us like human beings”: Discrimination against sex workers, sexual and gender minorities, and people who use drugs in Tanzania. Washington D.C., USA: Human Rights Watch; 2013. [Google Scholar]
- 4.Decker MR, Crago AL, Chu SK, Sherman SG, Seshu MS, Buthelezi K, et al. Human rights violations against sex workers: burden and effect on HIV. Lancet (London, England) 2015;385(9963):186–99. doi: 10.1016/S0140-6736(14)60800-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kerrigan D, Wirtz A, Baral S, Decker M, Murray L, Poteat T, et al. The global HIV epidemics among sex workers. Washington, D.C: World Bank; 2013. [Google Scholar]
- 6.Fielding-Miller R, Mnisi Z, Adams D, Baral S, Kennedy C. “There is hunger in my community”: a qualitative study of food security as a cyclical force in sex work in Swaziland. BMC Public Health. 2014;14:79. doi: 10.1186/1471-2458-14-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ntumbanzondo M, Dubrow R, Niccolai LM, Mwandagalirwa K, Merson MH. Unprotected intercourse for extra money among commercial sex workers in Kinshasa, Democratic Republic of Congo. AIDS Care. 2006;18(7):777–85. doi: 10.1080/09540120500412824. [DOI] [PubMed] [Google Scholar]
- 8.Beckham SW, Shembilu CR, Winch PJ, Beyrer C, Kerrigan DL. ‘If you have children, you have responsibilities’: motherhood, sex work and HIV in southern Tanzania. Culture, health & sexuality. 2015;17(2):165–79. doi: 10.1080/13691058.2014.961034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pettifor AE, Measham DM, Rees HV, Padian NS. Sexual power and HIV risk, South Africa. Emerging infectious diseases. 2004;10(11):1996–2004. doi: 10.3201/eid1011.040252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shai NJ, Jewkes R, Levin J, Dunkle K, Nduna M. Factors associated with consistent condom use among rural young women in South Africa. AIDS Care. 2010;22(11):1379–85. doi: 10.1080/09540121003758465. [DOI] [PubMed] [Google Scholar]
- 11.Open Society Foundations Sexual Health and Rights Project. Criminalizing condoms. New York: Open Society Foundations (OSF); 2012. [Google Scholar]
- 12.Tounkara FK, Diabate S, Guedou FA, Ahoussinou C, Kintin F, Zannou DM, et al. Violence, condom breakage, and HIV infection among female sex workers in Benin, West Africa. Sexually transmitted diseases. 2014;41(5):312–8. doi: 10.1097/OLQ.0000000000000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mooney A, Kidanu A, Bradley HM, Kumoji EK, Kennedy CE, Kerrigan D. Work-related violence and inconsistent condom use with non-paying partners among female sex workers in Adama City, Ethiopia. BMC public health. 2013;13 doi: 10.1186/1471-2458-13-771. 771-2458-13-771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deering KN, Amin A, Shoveller J, Nesbitt A, Garcia-Moreno C, Duff P, et al. A systematic review of the correlates of violence against sex workers. Am J Public Health. 2014;104:e42–e54. doi: 10.2105/AJPH.2014.301909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dunkle KL, Decker MR. Gender-based violence and HIV: reviewing the evidence for links and causal pathways in the general population and high-risk groups. American journal of reproductive immunology (New York, NY: 1989) 2013;69(Suppl 1):20–6. doi: 10.1111/aji.12039. [DOI] [PubMed] [Google Scholar]
- 16.Chersich MF, Luchters SM, Malonza IM, Mwarogo P, King’ola N, Temmerman M. Heavy episodic drinking among Kenyan female sex workers is associated with unsafe sex, sexual violence and sexually transmitted infections. International Journal of STD & AIDS. 2007;18(11):764–9. doi: 10.1258/095646207782212342. [DOI] [PubMed] [Google Scholar]
- 17.Li Q, Li X, Stanton B. Alcohol use among female sex workers and male clients: an integrative review of global literature. Alcohol and Alcoholism (Oxford, Oxfordshire) 2010;45(2):188–99. doi: 10.1093/alcalc/agp095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chersich MF, Bosire W, King’ola N, Temmerman M, Luchters S. Effects of hazardous and harmful alcohol use on HIV incidence and sexual behaviour: a cohort study of Kenyan female sex workers. Global Health. 2014;10:22. doi: 10.1186/1744-8603-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wechsberg WM, Luseno WK, Lam WK. Violence against substance-abusing South African sex workers: intersection with culture and HIV risk. AIDS Care. 2005;17(Suppl 1):S55–64. doi: 10.1080/09540120500120419. [DOI] [PubMed] [Google Scholar]
- 20.Schwitters A, Swaminathan M, Serwadda D, Muyonga M, Shiraishi RW, Benech I, et al. Prevalence of rape and client-initiated gender-based violence among female sex workers: kampala, Uganda, 2012. AIDS and behavior. 2015;19(Suppl 1):68–76. doi: 10.1007/s10461-014-0957-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Micheni M, Rogers S, Wahome E, Darwinkel M, van der Elst E, Gichuru E, et al. Risk of sexual, physical and verbal assaults on men who have sex with men and female sex workers in coastal Kenya. AIDS (London, England) 2015;29(Suppl 3):S231–6. doi: 10.1097/QAD.0000000000000912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Panchanadeswaran S, Johnson SC, Sivaram S, Srikrishnan AK, Latkin C, Bentley ME, et al. Intimate partner violence is as important as client violence in increasing street-based female sex workers’ vulnerability to HIV in India. The International journal on drug policy. 2008;19(2):106–12. doi: 10.1016/j.drugpo.2007.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schulkind J, Mbonye M, Watts C, Seeley J. The social context of gender-based violence, alcohol use and HIV risk among women involved in high-risk sexual behaviour and their intimate partners in Kampala, Uganda. Culture, health & sexuality. 2016;18(7):770–84. doi: 10.1080/13691058.2015.1124456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lancaster KE, MacLean SA, Lungu T, Mmodzi P, Hosseinipour MC, Hershow RB, et al. Socioecological Factors Related to Hazardous Alcohol use Among Female Sex Workers in Lilongwe, Malawi: A Mixed Methods Study. Subst Use Misuse. 2017:1–10. doi: 10.1080/10826084.2017.1365088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.L’Engle KL, Mwarogo P, Kingola N, Sinkele W, Weiner DH. A randomized controlled trial of a brief intervention to reduce alcohol use among female sex workers in Mombasa, Kenya. J Acquir Immune Defic Syndr. 2014;67(4):446–53. doi: 10.1097/QAI.0000000000000335. [DOI] [PubMed] [Google Scholar]
- 26.Wechsberg WM, Luseno WK, Lam WK, Parry CD, Morojele NK. Substance use, sexual risk, and violence: HIV prevention intervention with sex workers in Pretoria. AIDS Behav. 2006;10(2):131–7. doi: 10.1007/s10461-005-9036-8. [DOI] [PubMed] [Google Scholar]
- 27.Rhodes T. Risk environments and drug harms: A social science for harm reduction approach. International Journal of Drug Policy. 2009;20:193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 28.National AIDS Commission. HIV and STI Biological and Behavioral Survey, 2013: A study of Female Sex workers in seven Regions: Dar es Salaam, Iringa, Mbeya, Mwanza, Shinyanga, Tabora and Mara. Dar es Salaam; Tanzania: 2014. [Google Scholar]
- 29.Kerrigan D, Mbwambo J, Likindikoki S, Beckham S, Mwampashi A, Shembilu C, et al. Project Shikamana: Baseline Findings From a Community Empowerment-Based Combination HIV Prevention Trial Among Female Sex Workers in Iringa, Tanzania. Journal of acquired immune deficiency syndromes (1999) 2017;74(Suppl 1):S60–S8. doi: 10.1097/QAI.0000000000001203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization. WHO multi-country study on women’s health and domestic violence against women: summary report of initial results on prevalence, health outcomes and women’s responses. Geneva, Switzerland: 2005. [Google Scholar]
- 31.Genberg BL, Kulich M, Kawichai S, Modiba P, Chingono A, Kilonzo GP, et al. HIV risk behaviors in sub-Saharan Africa and Northern Thailand: baseline behavioral data from Project Accept. Journal of acquired immune deficiency syndromes (1999) 2008;49(3):309–19. doi: 10.1097/QAI.0b013e3181893ed0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zulliger R, Maulsby C, Barrington C, Holtgrave D, Donastorg Y, Perez M, et al. Retention in HIV Care Among Female Sex Workers in the Dominican Republic: Implications for Research, Policy and Programming. AIDS and behavior. 2015;19(4):715–22. doi: 10.1007/s10461-014-0979-5. [DOI] [PubMed] [Google Scholar]
- 33.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Research in nursing & health. 2001;24(6):518–29. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 34.Kerrigan D, Telles P, Torres H, Overs C, Castle C. Community development and HIV/STI-related vulnerability among female sex workers in Rio de Janeiro, Brazil. Health Education Research. 2008;23(1):137–45. doi: 10.1093/her/cym011. [DOI] [PubMed] [Google Scholar]
- 35.Lippman SA, Donini A, Diaz J, Chinaglia M, Reingold A, Kerrigan D. Social-environmental factors and protective sexual behavior among sex workers: the Encontros intervention in Brazil. American Journal of Public Health. 2010;100(Suppl 1):S216–23. doi: 10.2105/AJPH.2008.147462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51(6):1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 37.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. American Journal of Epidemiology. 2003;157(4):364–75. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 38.Zeger SL, Liang K, Albert PS. Models for Longitudinal Data: A Generalized Estimating Equation Approach. Biometrics. 1988;44(4):1049–60. [PubMed] [Google Scholar]
- 39.StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- 40.Leddy A, Kerrigan D, Kennedy C, Mbwambo J, Likindikoki S, Underwood C. ‘You already drank my beers, I can decide anything’: Using structuration theory to explore the dynamics of alcohol use, gender-based violence, and HIV risk among female sex workers in Iringa, Tanzania. Cult Health Sex. 2018 doi: 10.1080/13691058.2018.1438667. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.International Labour Organization. HIV and AIDS recommendation: Recommendation concerning HIV and AIDS and the world of work. Geneva, Switzerland: 2010. [Google Scholar]
- 42.Shannon K, Strathdee SA, Goldenberg SM, Duff P, Mwangi P, Rusakova M, et al. Global epidemiology of HIV among female sex workers: influence of structural determinants. Lancet. 2015;385(9962):55–71. doi: 10.1016/S0140-6736(14)60931-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.USAID. Gender-based violence in Tanzania: An assessment of policies, services, and promising interventions. 2008 [Google Scholar]
- 44.Strategic assessment to define a comprehensive response to HIV in Iringa, Tanzania research brief: Female Sex Workers. USAID; 2013. Research to Prevention. [Google Scholar]
- 45.Dokubo EK, Shiraishi RW, Young PW, Neal JJ, Aberle-Grasse J, Honwana N, et al. Awareness of HIV status, prevention knowledge and condom use among people living with HIV in Mozambique. PLoS One. 2014;9(9):e106760. doi: 10.1371/journal.pone.0106760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bunnell R, Opio A, Musinguzi J, Kirungi W, Ekwaru P, Mishra V, et al. HIV transmission risk behavior among HIV-infected adults in Uganda: results of a nationally representative survey. AIDS (London, England) 2008;22(5):617–24. doi: 10.1097/QAD.0b013e3282f56b53. [DOI] [PubMed] [Google Scholar]
- 47.Strategic assessment to define a comprehensive response to HIV in Iringa, Tanzania research brief: Summary of findings. USAID; 2013. Research to Prevention. [Google Scholar]
- 48.Logie CH, James L, Tharao W, Loutfy MR. HIV, gender, race, sexual orientation, and sex work: a qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS medicine. 2011;8(11):e1001124. doi: 10.1371/journal.pmed.1001124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sallmann J. Living With Stigma: Women’s Experiences of Prostitution and Substance Use. Journal of Women and Social Work. 2010;25(2):146–59. [Google Scholar]
- 50.Mulrenan C, Colombini M, Howard N, Kikuvi J, Mayhew SH, Integra I. Exploring risk of experiencing intimate partner violence after HIV infection: a qualitative study among women with HIV attending postnatal services in Swaziland. BMJ open. 2015;5(5):e006907–2014. doi: 10.1136/bmjopen-2014-006907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hatcher AM, Woollett N, Pallitto CC, Mokoatle K, Stockl H, MacPhail C, et al. Bidirectional links between HIV and intimate partner violence in pregnancy: implications for prevention of mother-to-child transmission. Journal of the International AIDS Society. 2014;17:19233. doi: 10.7448/IAS.17.1.19233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beckham S. “Like any other woman”? Pregnancy, motherhood, and HIV among sex workers in Southern Tanzania. Baltimore, MD, USA: Johns Hopkins Bloomberg School of Public Health; 2013. [Google Scholar]
- 53.Scorgie F, Chersich MF, Ntaganira I, Gerbase A, Lule F, Lo YR. Socio-demographic characteristics and behavioral risk factors of female sex workers in sub-saharan Africa: a systematic review. AIDS and behavior. 2012;16(4):920–33. doi: 10.1007/s10461-011-9985-z. [DOI] [PubMed] [Google Scholar]
- 54.Fonner VA, Kerrigan D, Mnisi Z, Ketende S, Kennedy CE, Baral S. Social cohesion, social participation, and HIV related risk among female sex workers in Swaziland. PloS one. 2014;9(1):e87527. doi: 10.1371/journal.pone.0087527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Argento E, Reza-Paul S, Lorway R, Jain I, Bhagya M, Fathima M, et al. Confronting structural violence in sex work: lessons from a community-led HIV prevention project in Mysore, India. AIDS Care. 2011;23(1):69–74. doi: 10.1080/09540121.2010.498868. [DOI] [PubMed] [Google Scholar]
- 56.Wirtz AL, Schwartz S, Ketende S, Anato S, Nadedjo FD, Ouedraogo HG, et al. Sexual violence, condom negotiation, and condom use in the context of sex work: results from two West African countries. Journal of acquired immune deficiency syndromes (1999) 2015;68(Suppl 2):S171–9. doi: 10.1097/QAI.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 57.Muldoon KA, Akello M, Muzaaya G, Simo A, Shoveller J, Shannon K. Policing the epidemic: High burden of workplace violence among female sex workers in conflict-affected northern Uganda. Glob Public Health. 2017;12(1):84–97. doi: 10.1080/17441692.2015.1091489. [DOI] [PubMed] [Google Scholar]
- 58.Kerrigan D, Kennedy CE, Morgan-Thomas R, Reza-Paul S, Mwangi P, Thi Win K, et al. A community empowerment approach to the HIV response among sex workers: eff ectiveness, challenges, and considerations for implementation and scale-up. Lancet. 2015;385:172–85. doi: 10.1016/S0140-6736(14)60973-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


